Introduction
Cervical cancer is the fourth most common cancer in women globally [
1]. Unfortunately, cervical cancer primarily affects medically underserved women and is disproportionately higher in low and lower middle-income countries, accounting for 85% of the cases worldwide and 90% of deaths [
1]. While there has been a reduction in cervical cancer prevalence rates since the introduction of Pap smears in the mid-20th century, healthcare systems and care vary across the globe [
2]. This trend was not observed in low and lower-middle-income countries (LMICs), due to a lack of health and human resources for screening implementation and low population coverage [
2].
In 2020, The WHO launched a global strategy to accelerate the elimination of cervical cancer by 2030 [
3]. The goals include 1) vaccinating 90% of eligible girls against Human Papillomavirus (HPV); 2) screening 70% of eligible women at least twice in their lifetimes (ideally at age 35 and 45 years); and 3) effectively treating 90% of those with a positive screening test or a cervical lesion, including palliative care when needed [
3]. Presently, the WHO recommends using HPV DNA sampling as the primary screening test as opposed to visual inspection with/through acetic acid (VIA) or cytology for screening and treatment purposes among both the general population, as well as women living with HIV [
4]. However, it is also stated that where HPV DNA testing is not yet feasible (i.e., resource-limited settings such as Tanzania), a regular screening interval of every 3 years when using VIA or cervical cytology may suffice [
4]. This is supported by a 2012 study as part of a “screen and treat" pilot program that was deemed effective in six African countries and demonstrated that VIA and cryotherapy are effective and feasible for this population as a screening modality [
5]. This screening method can be easily performed by mid-level providers and allows for immediate ablative treatment of amenable precancerous lesions [
6]. However, despite being inexpensive and feasible to implement, it has relatively low sensitivity compared to other methods such as cervical cytology or HPV DNA testing [
7,
8]. Tanzania plans to begin the implementation of HPV testing as a primary screening modality in a pilot program in 2024, but VIA will remain the primary screening modality in the national cervical cancer prevention program until this program can be fully brought to scale nationally [
9].
Notably, cervical cancer has been identified as the most common cancer among women in Tanzania, resulting in about 9772 new cases and 6695 deaths each year [
2]. This is especially alarming, given that over 60% of the population is under the age of 25 [
2]. Unfortunately, insufficient surgical equipment, medications, and imaging capabilities are only a few of the reasons to explain this statistic [
2]. Research has identified that a lack of awareness and knowledge of cervical cancer risk and available screening methods is a major contributor to the low screening uptake [
2]. Studies in Tanzania suggest several barriers to screening uptake among women at risk and these include knowledge of cervical cancer and related risk and the role of screening in prevention, knowledge among health care providers (HCPs) regarding cervical cancer risk and prevention, and misconceptions and beliefs regarding cervical cancer risk and the role of screening [
2]. In addition, financial barriers for women who undergo screening and have access to preventive services at a higher level of care or travel long distances to receive these services continue to exist [
2]. Many women have received education on cervical cancer risk and the role of screening in secondary prevention of cervical cancer and/or the role of HPV vaccination as primary prevention (i.e. among younger women) through radio and television awareness campaigns [
10]. Among these women, one-third knew someone who suffered from cervical cancer [
10]. Notably, predictors of awareness of cervical cancer and the role of screening included having a secondary education or higher, having 1-4 children, being 30-44 years old, living in an urban household, and obtaining a reasonable income [
10]. Despite urban status being a predictor of awareness, outcomes from a community-based cross-sectional study conducted in five municipalities of Dar es Salaam, the largest urban center in Tanzania, found that the three predictors of cervical cancer screening were knowledge level, screening intention, and health beliefs [
11]. It was found that 53% of participants had inadequate knowledge of cervical cancer and cervical cancer screening, with 91.8% of the overall population having never previously been screened for cervical cancer [
11].
While prior studies on the effects of knowledge levels on cervical cancer screening uptake in rural and semi-rural Tanzania have been explored, there is scant literature on the perspectives of not only women at risk, but also other health system stakeholders (e.g., policymakers, program managers, and HCPs) [
12]. Several studies have suggested that many women, particularly those with low levels of knowledge about cervical cancer and screening, may not recognize the benefit of screening over the possible consequences of forgoing screening [
12]. In one study, it was determined that while the majority of the women had heard of cervical cancer, only 6-21% had ever been screened [
2]. Interestingly, women from more developed regions in Tanzania were more likely to be screened if they had some form of health insurance, were older, or had some prior knowledge of cervical cancer [
2]. In addition, across seven studies that have been conducted regarding cervical cancer prevention among Tanzanian women, it was identified that 80% of women had heard of cervical cancer, although knowledge levels surrounding specific prevention methods and risk factors were low [
2]. Lack of knowledge and awareness regarding cervical cancer risk and the role of screening and preventive services extends beyond women at risk, with prior studies demonstrating a lack of HCP knowledge regarding cervical cancer in the region [
13]. For example, one study found that, before a 1-day cancer training symposium conducted amongst 43 clinicians, 69% had reported never receiving any training regarding cervical cancer and cervical cancer screening in the past [
13].
Given the existing evidence, we designed and conducted a cross-sectional research study using semi-structured interviews. Most HCPs and women interviewed resided and worked in rural or semi-rural locations in the Northern Zone of Tanzania (Arusha, Kilimanjaro and Tanga Regions). For representation from the national screening program and national cancer experts, we also sought key informants to participate in interviews at the National Cancer Hospital in Dar es Salaam, (Ocean Road Cancer Institute (ORCI)). We developed our methodology from the HSA framework that had been previously utilized in LMICs for assessing multi-level health system barriers and enablers for the screening, diagnosis, and management of chronic diseases (such as hypertension and diabetes) [
14,
15].
Methods
Theoretical Framework
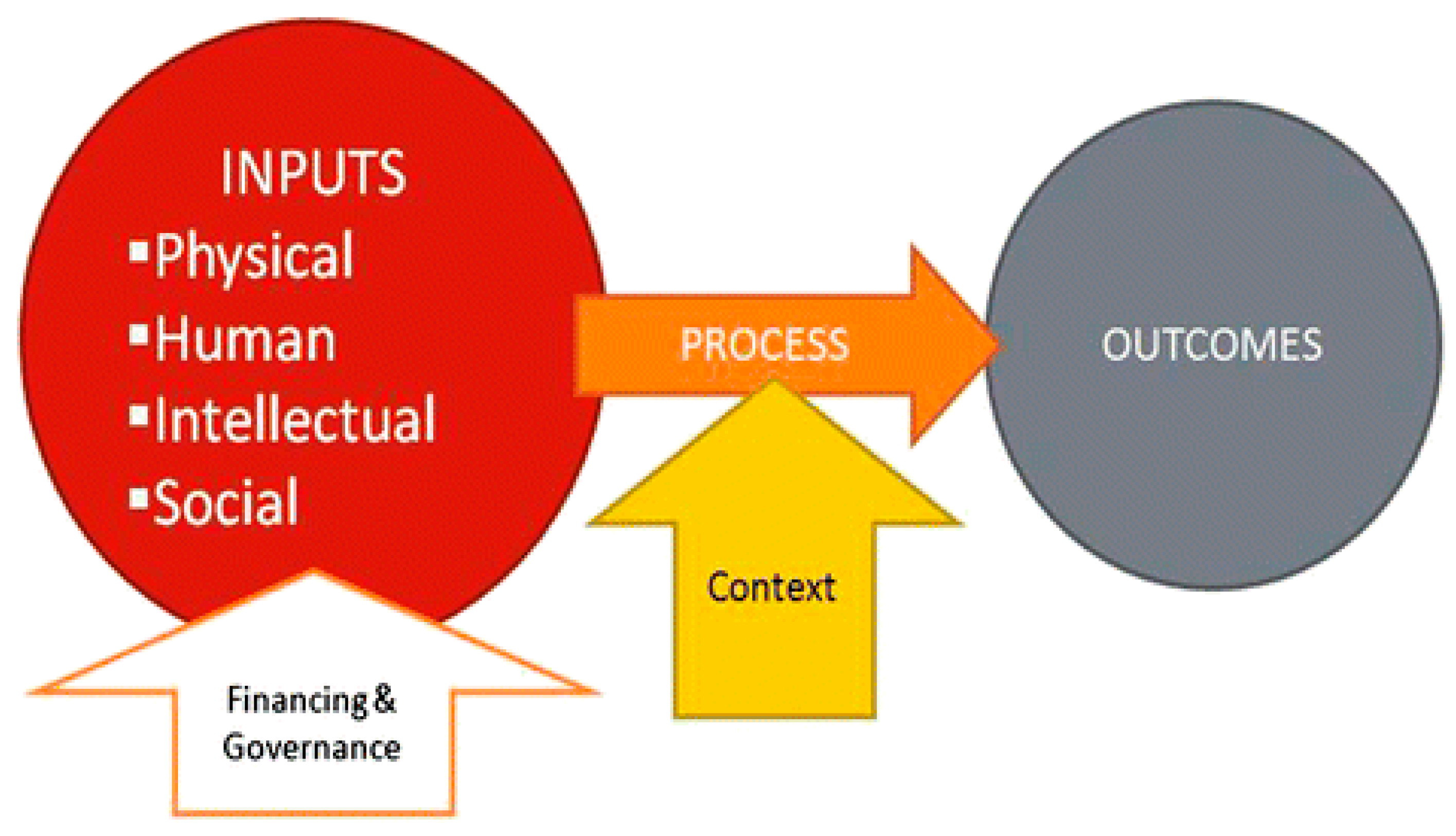
The approach to the health systems assessment is described in
Figure 1 (below) and underpinned by a conceptual framework developed by Risso-Gill and colleagues [
14,
15]. The conceptual framework draws on constructs proposed in World Health Report 2000 [
16]. The report highlights that good performance of a health system depends critically on the delivery of high-quality services and on the ability of each system to carry out four main functions: service provision, resource generation, financing, and stewardship [
16]. The framework incorporates the WHO health system building blocks and recognizes that the building blocks (leadership and governance, service delivery, health system financing, health workforce, medical products, vaccines and technologies, and health information systems) exist in a complex ‘system’ and different components may influence outcomes of another and allows identification of how resource inputs may influence outcomes in another [
16].
The Cervical Cancer Prevention Program of Tanzania
Tanzania has a “multi-tiered, comprehensive cervical cancer control programme” [
17].
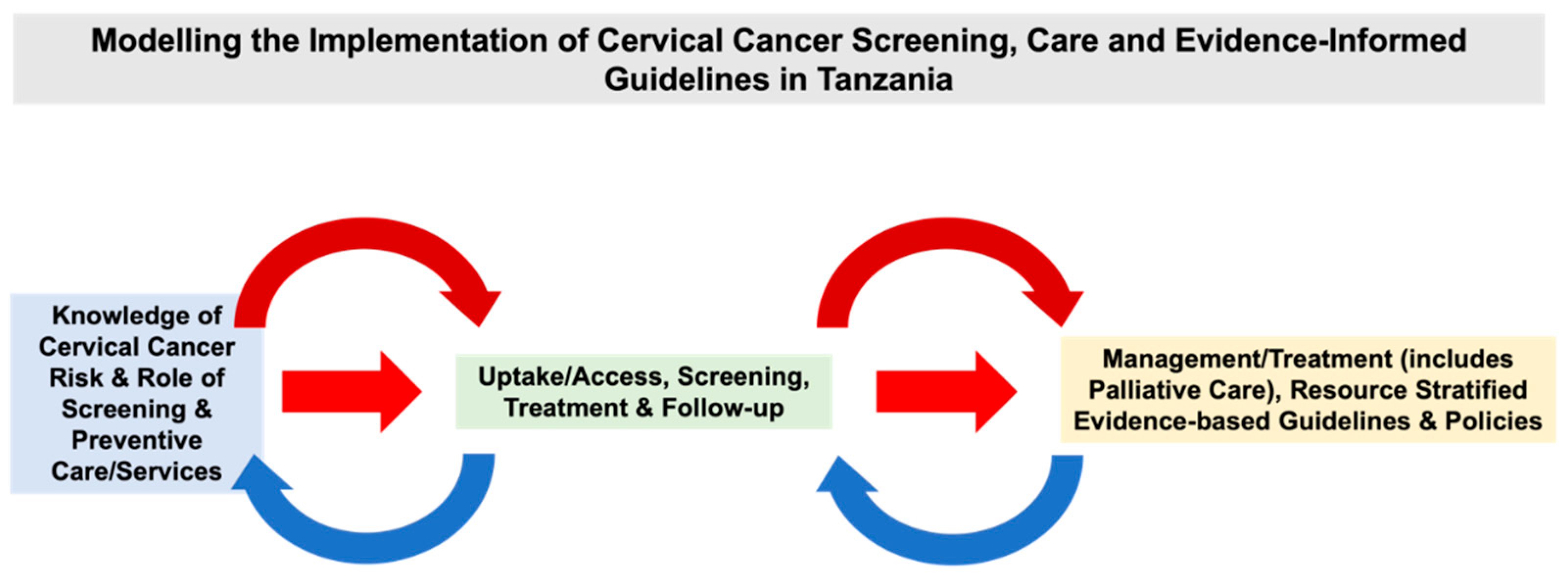
Figure 2 demonstrates components embedded across Tanzania’s screening and treatment pathway. There has been significant progress in cervical cancer screening progress. Since 2010, the government has established a national Cervical Cancer Prevention (CECAP) program offering VIA through a single visit approach as a national strategy [
18,
19]. Tanzania’s CECAP program includes a mHealth supported quality assurance program developed by Dr. Karen Yeates and colleagues (formerly known as the ’SEVIA’ application) [
18,
19]. Eligible women are screened for cervical cancer using VIA [
20]. VIA is free, and treatment of pre-cancerous lesions (e.g., thermal ablation and LEEP) are at no cost through the program [
20]. Unfortunately, there is a low cryotherapy rate, as a result of a lack of resources and insufficient equipment [
20]. Notably, there are costs involved for diagnostic services [
20]. Comprehensive services that include diagnostic, radiotherapy, chemotherapy, and palliative care, are offered in two public sector institutions [
20]. There are costs for further assessment and higher-level of treatment (e.g., cervical biopsy and surgery) [
20].
This research study is part of a series of studies evaluating HCP, women at risk, and other stakeholder perspectives on determinants of the cervical cancer screening and preventive treatment program in Tanzania.
We adapted the HSA framework, conceptualized by Risso-Gill, Balabanova and colleagues for hypertension control (
Figure 1) [
14,
15]. The health systems assessment has been leveraged in other low-resource settings (including Malaysia and Columbia) to understand the health system barriers to hypertension diagnosis and management [
14,
15]. While cervical cancer screening and prevention services are dissimilar to the diagnosis and management of hypertension, the HSA framework captures multiple levels of health system components and inputs required for screening, diagnosis, and management of almost any chronic, non-communicable disease [
14,
15]. This allows for ease of adaptation and significant overlap with the concept of cervical cancer screening and the ‘care pathway’ for cervical cancer prevention services and required follow-up in almost any health care system [
14,
15]. Therefore, we used the foundations of this model/framework to inform our research approach and evaluate policy maker, health system leadership, patient and HCPs' perspective of the extent to which health system requirements for effective cervical cancer screening, prevention, and control are in place in Tanzania [
14,
15]. The framework posits that a coordinated investment that includes physical resources (e.g. diagnostic equipment), human resources (e.g. trained healthcare staff), intellectual resources (e.g. evidence-based guidelines), and social resources (e.g. patient support systems) are necessary inputs for achieving clinical outcomes [
14,
15]. Further, additional contextual factors (e.g. attitudes and beliefs among providers and women at risk) may modify the impact of those inputs on the implementation process [
14,
15]. The inputs and context will be evaluated from the perspective of women at risk (patients) and HCPs and health system stakeholders (in our case cervical cancer screening providers, program managers, policymakers, and other health providers who perform roles in cervical cancer prevention services) to better understand the full range of barriers and facilitators regarding cervical cancer screening uptake and access to preventive services in Tanzania.
Using previous studies as a guide, the HSA framework informed the design of this study, providing a structured process by which to identify critical strengths and weaknesses in the management of cervical cancer screening and preventive treatment services in Tanzania and subsequently to identify feasible strategies that offer the possibility of improving or optimizing cervical cancer control at a national level while also considering service delivery and uptake among women at risk who reside in rural or semi-rural locations [
14,
15]. The data was analyzed using thematic analysis methodology [
21,
22].
We adapted interview topic guides for cervical cancer screening and preventive treatment services using the HSA framework [
14,
15]. The following are the main themes for each of the interviews that were explored: 1) pathways to care, 2) access to care, 3) cervical cancer control, 4) physical resources, 5) financing, 6) patient communication and empowerment, 7) human resources, 8) knowledge and information resources, 9), policy and governance, and 10) cervical cancer screening strategies.
Study Participants
Field work was undertaken by local researcher team members who received training in health systems appraisal at a workshop held in Moshi, Tanzania, using a detailed manual (HSA Toolkit) adapted from the one developed for hypertension that contained sampling frameworks and assessment tools to better standardize the participant recruitment and the interviews and data collection across sites. At each site, researchers identified the main health facilities where women would seek cervical cancer screening and treatment services in the national screening program.
Study participant categories and recruitment are displayed below in
Table 1. The eligibility criteria and recruitment of participants were completed through consultation with stakeholders (e.g., Tanzanian Ministry of Health officials). Enrolment was performed opportunistically (e.g., the study team visited health facilities that had cervical cancer screening sites that were supported by the national Cervical Cancer Prevention Program to invite participants for interviews with the consideration of sampling across various roles and cadres of healthcare, and specific sampling of rural and semi-rural sites where possible. This included cervical cancer screening program leadership (rural/urban; private/public) whose work is related to the provision of cervical cancer screening and preventive treatment services and women at risk. Key stakeholders were divided into four main categories: program leadership/policy makers, HCPs, women at risk, and non-physician HCPs. We recruited 8 program leadership/policy maker participants that comprised national and district-level government officials, donor agency leaders, non-governmental organizations, health facility managers, pharmaceutical company representatives, and academia (who know cervical cancer screening and cancer care). We recruited 15 HCPs from primary care/outpatient clinics and village dispensaries where cervical cancer screening may or may not be provided, secondary (health centers) and tertiary (hospitals), health facility-based medical doctors, and clinical officers. We recruited 9 non-physician HCPs including matrons, nurses, and nurse assistants. Women at risk of cervical cancer (women at risk/clients) included 39 women from various districts, from screening sites at differing health system levels including up to the national cancer hospital. A total of
71 Interviews were conducted between 2014-2018. A large proportion of the HCPs and women at risk are from rural or semi-rural locations (
Table 1).
Table 1.
List of Interviewed Participants (e.g., Location, Number Interviewed Per Group, Median Age). Assistant Medical Officer – AMO; Clinical Officer – CO; Medical Doctor – MD; Medical Officer – MO; Regional Reproductive and Child Health Coordinator – RRCHCo.
Table 1.
List of Interviewed Participants (e.g., Location, Number Interviewed Per Group, Median Age). Assistant Medical Officer – AMO; Clinical Officer – CO; Medical Doctor – MD; Medical Officer – MO; Regional Reproductive and Child Health Coordinator – RRCHCo.
| Interview Participants |
|---|
| Group |
Location |
No. Interviewed |
Median Age |
No. Females |
No. Males |
| Cervical cancer screening program leadership |
KCMC, ORCI, Bombo Referral Hospital |
8 (1 = Senior Lecturer and Senior Consultant for Gynecology and Obstetrics, 2 = Specialist (Oncology), 1 = Professor Gynecology and Obstetrics, 1= Gynecologist, 1= Cervical Cancer Focal Person MOH, 1= RRCHCo, 1= In Charge of Clinic |
Not collected |
4 |
4 |
| Healthcare Providers |
Mt Meru, Marangu Hospital, Meru District Hospital, Pasua Health Center, TPC Hospital, Kibosho Hospital, ORCI, Kilema, SEVIA Screening Sites, KCMC, Bombo Referral Hospital |
24 (AMO = 2, MD = 12, MO = 1, Nurse = 9) |
Not collected |
13 |
11 |
| Women at Risk of Cervical Cancer (Women at Risk/Clients) |
ORCI, Kilema, TPC, Pamoja Tunaweza Women’s Centre, SEVIA Screening Sites |
39 |
46 (18-80 years old, 50 years old as the most common age, three unknown ages) |
39 |
0 |
Table 2.
Health Facilities Sampled by Site Characteristics (Rural/Semi-Rural vs. Urban; Private vs. Public vs. Faith-Based).
Table 2.
Health Facilities Sampled by Site Characteristics (Rural/Semi-Rural vs. Urban; Private vs. Public vs. Faith-Based).
| Location |
Rural/Urban |
Private/Public/Faith-Based |
| Kilimanjaro Christian Medical Center (KCMC) |
Urban |
Faith-Based/Public Hybrid |
| Mt. Meru Hospital |
Urban |
Public |
| Ocean Road Cancer Institute (ORCI) |
Urban |
Public |
| Kilema Hospital |
Rural |
Faith-Based |
| TPC Hospital |
Rural |
Private |
| Marangu Hospital |
Rural |
Faith-Based |
| Meru District Hospital |
Urban |
Public |
| Pasua Health Center |
Urban |
Public |
| Kibosho Hospital |
Rural |
Faith-Based |
| Bombo Regional Referral Hospital |
Semi-Rural |
Public |
Data Collection
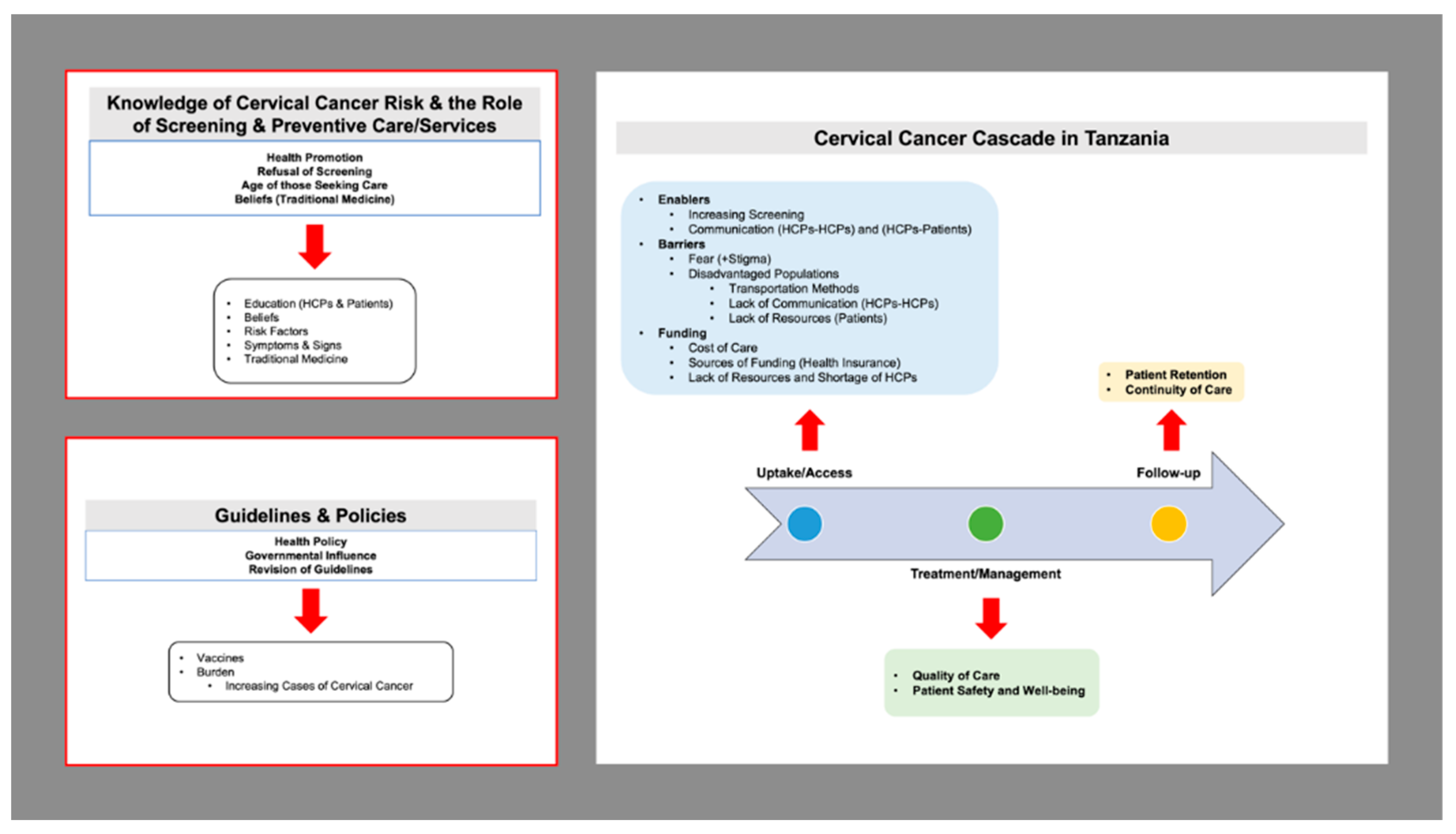
Semi-structured individual interviews were conducted using an interview guide derived from the Health Systems Appraisal Toolkit provided to our research team by Risso-Gill. A purposive sampling technique was used to recruit key stakeholders involved in cervical cancer screening program leadership and policy (including policymakers and HCPs) and to ensure a range of experiences regarding optimal management and control of cervical cancer within Tanzania were captured. In addition, women at risk of cervical cancer were recruited for semi-structured interviews to share their own perspectives and knowledge on cervical cancer risk and cervical cancer prevention services in Tanzania. An open-ended semi-structured interview guide, which included items that explored the availability of physical resources, human resources, intellectual resources, and social resources necessary for optimal management and control of cervical cancer was utilized. The open-ended questions allowed participants to elaborate on issues they considered important or relevant, particularly about these categories. All participants described their role and position within the health systems and in the context of cervical cancer screening and preventive treatment/management. Participants shared their perceptions on how women at risk are diagnosed with cervical precancer or invasive cervical cancer within the health care system and the pathways for preventive treatment, referrals for required management, preventive follow-up care, access to cervical cancer treatment, lifestyle counseling, and support with patient-centered care for cervical cancer control (
Figure 3). All interviews were audio recorded with written consent from participants. Interviews lasted between 30 to 45 minutes and were conducted in a health facility.
Data Analysis
We analyzed the data using an iterative process. Transcripts from interviews were transcribed verbatim and translated (if conducted in Kiswahili) and exported to NVivo for Mac v11.4.0 (QSR International, Melbourne, Australia) for analysis, where two of the authors independently became familiar with and reviewed the data in depth. A deductive approach was utilized based on the health systems assessment framework by Risso-Gill and colleagues. Statements related to physical, human, intellectual, and social resources were coded, and a detailed thematic analysis was performed to extract the salient themes. Upon completion of individual coding, the two coders (MC and SK) convened on multiple occasions to discuss the coding process and explore emerging themes. This was done until coding saturation was achieved, and discrepancies in coding were discussed until consensus was reached. Quotes reported in the results represent statements that are highly representative of each theme and are cited as indicated by key stakeholders (cervical cancer screening program leadership), HCPs, non-physician HCPs, and women at risk.
Results
Thematic analysis based on initial coding and development of a codebook was used to identify emergent themes and triangulate the information collected, facilitated by NVivo for Mac v11.4.0 (QSR International, Melbourne, Australia). This inductive approach allowed for links between research objectives and findings from raw data (
Figure 1). It helped develop a deeper understanding of emergent themes’ underlying experiences and processes. Verbatim quotations were frequently used to illustrate the responses of the respondents on important themes and sub-themes. Seven themes emerged from our analysis: knowledge of cervical cancer risk and the role of screening and preventive care/services (e.g., prevention, risks, signs, etiology, and treatment), training and knowledge of HCPs, knowledge of women at risk, beliefs about cervical cancer screening, traditional medicine, risk factors, and symptoms and signs.
Table 3.
Seven Identified Themes and Examples of Evidence.
Table 3.
Seven Identified Themes and Examples of Evidence.
| Themes |
Examples of Evidence |
| Knowledge of cervical cancer risk and the role of screening and preventive care/services |
“’Awareness should be spread in different areas…Most people don’t know anything about cervical cancer. So, awareness should be provided.” (Patient) |
| Knowledge and Training (HCPs) |
“I don’t think even among the health profession… that people know exactly how to walk through it (HCP)." |
| Knowledge (Women at Risk) |
"Provision of education is needed... [healthcare providers] are supposed to [provide education]. [If we can educate men], a lot of women would be willing to go for screening (HCP)." |
| Beliefs on Cervical Cancer Screening |
"She said that contraception can cause cervical cancer" (Patient) |
| Traditional Medicine |
"They want to go to a traditional attendant or a traditional doctor who can say, 'This is just someone [who has] bewitched you. I can take care of you'" (HCP) |
| Risk Factors |
"They mentioned.. that [those who are] HIV-positive are at risk of getting cervical cancer" (Patient) |
| Symptoms and Signs |
"[Elderly] women come and complain about... bleeding, post-bleeding and... discharge. When you insert the speculum... there is cancer" (HCP) |
The first theme investigated awareness and knowledge levels among women at risk and HCPs regarding cervical cancer risk and the role of preventive services. Sub-themes included the importance of health promotion, methods of raising awareness such as word of mouth and radio, and underlying reasons behind the refusal of screening. The second theme was the education of HCPs. A relevant sub-theme was the relation of training to the capability and knowledge that HCPs possessed. The third theme was the education level of women at risk and opportunities for improving awareness through education. The fourth theme that emerged was beliefs on cervical cancer screening among women and HCPs. The fifth major theme addressed traditional healers and traditional medicine and its relevance to cervical cancer screening amongst the population. The sixth theme addressed common risk factors related to cervical cancer. Sub-themes that emerged in the analysis include HIV and early sexual intercourse. Finally, the seventh theme discussed the signs and symptoms women at risk experience with cervical cancer and/or HCPs commonly identify. Pain was identified as a sub-theme of interest.
Knowledge of Cervical Cancer Risk and the Role of Screening and Preventive Care/Services
Many women at risk expressed a lack of awareness surrounding cervical cancer prevention, risks, signs/symptoms, etiology, and treatment, and overall, the importance of screening.
"Women are not so much aware of cervical cancer so it will take time for them to become aware about understand the importance of screening for their health. I just educate them and then it will take time for them to think and to prepare themselves, and then they will come - so it takes time."
The need for more education surrounding the disease and prevention was highlighted.
"So, she said that awareness should be spread in different areas. Because she mentioned the village that she comes from, most of the people don't know anything about cervical cancer. So, awareness should be provided."
Interviewers asked HCPs if there was a reason that women didn’t come in for screening. The HCP compared health promotion for HIV vs. cervical cancer. They discussed the need to implement more initiatives that will educate women on the disease and the need to be screened. Other factors, such as transportation and distance were identified as additional barriers to health promotion.
“So, it just started, and people are not that well informed. And the project, is not that well, not that well organized, compared to maybe ctc [HIV clinic] when we can go to the villages and talk to people about HIV, reach out to them. For cervical cancer it is different, we don't have such activities going on, or such organized procedures or activities. For maybe a certain period you have screened a certain number of people or go to the villages to talk to them so they can come to be screened – they are not that established. So, you’ve got to get a larger number of people and also difficult to get the information to the people if you are not going to them. Because they won’t come here, you have to go to them. It is different in the town, where people are well informed about their health, and they have to follow. But in the villages, you have to follow them – tell them, teach them.”
- 2.
Word of Mouth
Word of mouth was identified as the primary means of spreading awareness. Once women attended their screening visit, they would often share their experiences with their family, friends, neighbors, and community.
"The ones who have already come are the ones who will go back and tell like she was told by the neighbor that it’s fine, there’s no problem. So, when they go back and tell them, they will come."
"She says that not everyone knows, but a lot of them know. Mostly because if they come here then they're told about it, and then those who go back actually tell their colleagues about it. She's even been told by some of her colleagues that she should bring them here."
- 3.
Radio
Awareness and information surrounding cervical cancer are largely spread through announcements made on the radio or TV.
"From the radio, I heard that cervical cancer is a dangerous disease, so it is good to do screening at the earlier stage. So that is why I decided to go to the clinic for the check-up."
"Almost everyone in this country, in Africa has a radio. Or radio access. So, you cannot be scared they'll get your information- then comes, of course, the TV, which is not all that, not everyone has a TV, but many people have TVs."
- 4.
Refusal of Screening
Some women who are already at the clinic refuse to be screened and receive treatment, due to fear or lack of understanding about the role of screening and treatment for cervical cancer prevention.
"Of course, yea challenges – they may refuse treatment like cryotherapy – like one client refused cryotherapy. – and others when you refer them to KCMC don't go. But most they agree to be screened."
"Most women, accept this screening only a few have not already decided about screening. From today, only three women refused to do the screening, so I'm not sure if they are going to accept or they will just leave."
Another woman described her thoughts on the refusal of screening:
"Some they are afraid, ignorance..... we are going into the church, we are giving information to the church. Even to the market, the schools, but others are not coming."
Education (HCPs)
A lack of education surrounding cervical cancer exists at the HCP level. The level of knowledge is often variable among HCPs of different ages, experience levels, and professional levels.
"I don’t think even among the health profession, that, I don’t know which percentage I should mention. But I don’t think that people know quite – that people know exactly how to walk through it."
"Updating, more education to the community and also training more staff to know about cervical cancer."
"So, you have these young, young doctors, only the old doctors don't know, old nurses who have trained twenty years ago, they are probably not very aware about cervical cancer. They are aware of cervical cancer but, screening and a lot of information about it, no. In terms of patients, the population I don't think they have a lot of information on cervical cancer, no."
- 5.
Training
HCPs highlighted the need for HCPs across all levels to be trained to conduct cervical cancer screening to improve reach and uptake.
"They should educate more people on the job training we're two…. when we will train more staff here our services will improve….and in the rural areas we need to train more staff and home service care providers…. of course, when you talk with them they don't know so much about the cervical cancer screening."
"I think that we have to train people in different categories, yeah. Train the specialists, train the other nurse- the other doctors, sorry, the other practitioners, the nurses, the advanced medical officers, so that every person can screen."
Education (Women at Risk)
There is a pressing need for education related to cervical cancer, including the reasons for development and the importance of being screened.
"They come from their home to here, and we give them the education…. health education……the general issues about cervical cancer and after that for those who are willing to screen their health…. they are screened….and then they get their result if it is positive or negative. If it is negative, we give them the next date for check, but for those whom the problem is so big and we feel we can't solve, we refer to other places."
One woman described how she believes women can be better reached and provided with cervical cancer screening and care:
“Provision of education is needed. And also, on that education, they are supposed to give so that they can get it even through men. So, if they know that, a lot of women would be willing to go for screening.”
Beliefs on Cervical Cancer Screening
Several misconceptions related to the cause of cervical cancer continue to exist. Some women believed that using contraceptives or consuming certain foods resulted in the development of cervical cancer.
"She said that this contraception can cause cervical cancer."
Another woman described her thoughts on cervical cancer and women’s health.
“Before I knew about cervical cancer, I knew it's a disease you can get from different medicines which a lot of women like to use. Or you can get different types of food, which you like to eat. Also, I didn’t know if this disease if you can get it from men. I thought maybe it was only for women. Before I know that."
Traditional Medicine
A large dependence and belief surrounding the efficacy of traditional medicine continues to exist. A combination of beliefs and financial strains cause many women to use local herbs, instead of chemotherapy to treat their cancer. One HCP mentioned:
"They want to go to a traditional attendant (inaudible 38:20) or a traditional doctor who can say, this is just someone who has bewitched you, I can take care of you. They can understand."
Another HCP explained:
"One patient came and said if you diagnosed with cervical cancer in KCMC she used the local herbs, but they don’t treat anything?"
"The education provided by KCMC helped us, and we got no disturbance and when you go there with your husband, they give you priority. (move that to another theme- treatment?)."
One woman discussed the financial burden of chemotherapy:
“If I go to a traditional doctor and they say, ‘bring on God I can take care of this’ and a god will cost about 150-200,000 Tanzanian shillings. And you go to Ocean Road [National Cancer Hospital of Tanzania]. One course of chemotherapy will cost 400,000. Okay? So which options will you take? If you are my relative looking after me? You going to take the easiest option available. So, that’s still a big gap.”
Risk Factors
HCPs explain the role of HIV in cervical cancer.
"High risk – patients with- who are HIV positive. And the screening, because there is no formal clinic, we usually do screening based on request patients who have requested, and then we have other satellite screening sites. They refer like this patient has a problem, please take a look at her – we'll do that."
One woman explained her knowledge surrounding HIV.
"They mentioned about HIV. That the one who has HIV-positive are at risk of getting this cervical cancer."
HCPs highlighted HIV as a significant risk factor for cervical cancer.
"Yeah, there are so many risk factors. HIV is just one of them and it has been publicized because with HIV the disease progression is very fast, but there are many other risk factors for getting cervical cancer."
"The low immunity, and for those who start sexual intercourse from the beginning are in risk to get the cervical cancer…and also those who get the human papillomaviruses…they are also at risk to get the cervical cancer."
- 6.
Early Sexual Intercourse
Implementing sexual reproductive health classes for young girls may educate women on the importance of using contraceptives and prevent the development of cervical cancer.
"Yeah, and also another challenge is for young kids. Before they are grown up, sometimes they have a lot of – they have multiple partners, for them, they don’t know it is risky. Or whatever, for cervical cancer."
"We have to intensify this sexual reproductive health to these young ladies so that they can delay sexual intercourse so if we manage to go directly to the school to input information for cervical cancer prevention it will be better than staying until you get suffer then you look for the service."- use a narrative to explain more."
Symptoms and Signs
Pain is one of the most common symptoms of cervical cancer.
"I visited before, I was getting pain in the stomach and then I went to the hospital and then the doctor recommended to me to do cervical cancer screening."
Other complications women described included bleeding and discharge.
"You can see the elder women come to you and complain about the PV bleeding, post coital-bleeding and follow the discharge and when you insert the speculum you see there is cancer."
- 7.
Pain
Common symptoms women reported included abnormal or pelvic pain and bleeding. These were often the first few signs women experienced before going to get screened.
"Because I have this abnormal stomach frequently, that is why also I decided to do screening."
Another woman shared her experience:
"Symptoms caught me when I was at home it started by getting abdomen pain and when I had sex, I felt pain and blood coming out when I was on my period the period lasted for long like a month, I went to Mawenzi hospital and got medication."
Discussion
The findings highlight existing challenges in cervical cancer screening across Tanzania. Rural areas particularly struggle with numerous barriers that limit not only access to cervical cancer screening services, but also access to multiple healthcare services [
23]. Lower health literacy and limited knowledge regarding screening services or insufficient infrastructure also play a role [
23]. Moreover, cultural beliefs significantly shape health seeking behaviour with respect to cervical cancer screening uptake [
23]. Women who reside in urban locations may be more acquainted with where to access specific healthcare services [
23]. Addressing these issues requires targeted efforts, especially in rural regions, including the implementation of mobile screening initiatives, enhanced health education campaigns, integration of community health workers or other extenders of the health workforce who can provide health promotion at the community level and health system infrastructure strengthening and enhancements. These measures are crucial for ensuring equitable access to cervical cancer screening services throughout the country.
The findings of our study intersect and overlap with the theoretical framework, which incorporates the WHO health system building blocks (leadership and governance, service delivery, health system financing, health workforce, medical products, vaccines and technologies, and health information systems) [
14,
15,
16]. This framework allows for a comprehensive analysis of the associations and relationships between the resources and components of a health system [
14,
15,
16]. This approach considers the perspectives of patients and HCPs and allows for the identification of how resource inputs may influence outcomes in another [
14,
15,
16]. There is a significant need for an increase in political governance regarding cervical cancer screening services. The results of our study further inform the conceptual framework. Women at risk and HCPs indicate the importance of education (input) and informed knowledge on cervical cancer and risk factors (desired outcome) to increase the uptake of cervical cancer screening in Tanzania.
Strategies for Increasing Knowledge of Cervical Cancer Risk and the Role of Screening and Preventive Care/Services
HCPs interviewed in our study emphasized the importance of education in increasing knowledge about the importance of cervical cancer screening and treatment services among women at risk, especially in rural settings. They also highlighted the importance of informed decision-making. Many HCPs agreed that providing women with the knowledge surrounding cervical cancer screening would increase knowledge of cervical cancer risk and the importance of screening and preventive treatment, which may lead to an increase in screening rates. This is congruent with the findings of a 2012 study that evaluated determinants of acceptance of cervical cancer screening in Dar es Salaam, Tanzania [
24]. Women who had attended at least primary school were more likely to attend screening in comparison with women who had never attended school [
24]. The education gap is also evident in the reasons for which women present at the clinic [
24]. One study found that of the women presenting for screening at ORCI, 90.7% had at least some education compared to only 43.1% of women presenting for treatment [
25].
Health promotion plays a significant role in increasing the uptake of cervical cancer screening and treatment services among women in Tanzania. It is of particular importance to establish a greater number of programs that educate a large number of individuals in close vicinity to where they reside. This is to optimize convenience and reduce barriers such as transportation and distance. This is evident in studies, which show that differences in knowledge have been found between rural and urban areas in Tanzania, with generally lower knowledge and greater issues accessing cancer screening services in remote areas [
25]. Other studies have found that women who are least likely to be aware of cervical cancer are rural women, less affluent women, those with limited education, and those with limited access to the formal economy [
10]. In the aforementioned study conducted at the OCRI, women in the treatment clinic had to travel significantly further at a much greater cost than women in the screening clinic [
25]. In another study, women having to come a long distance before reaching centers for cervical cancer screening was seen as a barrier by 58.7% of participants [
26]. An example of a successful intervention for health promotion in Tanzania is, in fact, OCRI, which began a mobile screening clinic in 2001, which travels to various satellite clinics throughout the country [
25]. This mobile clinic screens approximately 1,500 women during the 2-week outreach session and trains HCPs to continue screening services upon completion of the outreach program [
25]. Above all, it has shown to be a cost-effective method in successfully reaching rural populations and providing education to thousands of women who would otherwise not receive appropriate care [
25].
Word-of-mouth and radio were identified as successful techniques in raising awareness about the existence of screening services amongst the population. This strongly aligns with research from high and low health resource countries where strategies that delivered health promotion messaging via word of mouth and audio-visual channels is effective in making women more informed [
27]. In contrast, research undertaken while implementing a human papillomavirus video education program for women participating large cervical cancer screening campaigns in Tanzania found that education provided to women via word of mouth resulted in the inconsistent spreading of information among women and inefficient use of HCPs time [
28]. It was enforced that educational interventions must be appropriately designed for the specific population of interest to see long-lasting changes in health-seeking behavior [
28]. However, there is uncertainty amongst these findings: another study found that the influence of family and friends was found to be the second largest source of information and that friends and family were the most trustworthy stakeholders in improving knowledge, a concept that was reinforced in a study evaluating health promotion strategies for HPV vaccination for prevention of cervical cancer [
29]. As for the use of radio in health promotion, a 2013 study found that compared with women who did not attend the screening service, women who attended listened regularly to the radio (OR 24.76; 95% CI, 11.49–53.33) [
30]. Another study conducted in Zanzibar, Tanzania found that integration of health awareness themes into popular television and radio dramas might be effective in such promotion and prevention [
31].
Our research identified fear as a primary reason for the refusal of screening amongst participants interviewed. In the aforementioned study conducted in Zanzibar, Tanzania, fear of screening and inconvenience were the primary concerns among the Zanzibari interviewees [
31]. Another study conducted in Addis Ababa, Ethiopia also found that perceived fear of positive results and the perceived pain and discomfort experienced with undergoing screening were mentioned as a barrier to seeking screening services [
32]. A Kenyan study found that female participants stated fear and shame, or embarrassment related to the screening procedure as a barrier [
33]. Specifically, participants were worried about being fully or partially nude during screening, especially with a male doctor [
33]. To combat this, participants suggest that women should be screened where possible by a female health provider for screening to be more acceptable to women, although they may still fear being “judged” by the physician [
33].
Education
Our study found that the level of training and breadth of knowledge among HCPs was felt to be integral to increasing rates of health promotion and uptake of screening services among women at risk. This is supported by a study that found that women undergoing cervical cancer screening at a health clinic reported that they had heard about cervical cancer screening from a HCP [
34]. This is congruent with other studies, which have shown that HCP recommendations may positively influence the uptake of cervical cancer screening [
35]. A cross-sectional study conducted in urban Tanzania found that those who received information about cervical cancer from HCPs were 1.569 times more likely to have adequate knowledge of cervical cancer as compared to respondents who did not receive cervical cancer information [
11]. If women at risk are seeking knowledge from HCPs to ensure informed decision-making, it is integral that HCPs (doctors and nurses) are knowledgeable and resourceful. HCPs are pivotal in encouraging women to adopt protective health behaviors and health seeking behaviours and in correcting misconceptions of screening tests and providing targeted comprehensive health education [
35]. Our study is not the first to document the importance of knowledge and screening skills/competence among health providers as a barrier to cancer screening [
35]. A 2018 study addressing barriers and facilitators to screening found that only approximately 70% of clinicians had performed cervical cancer screenings [
36]. Of those that did receive training, most only received a 2-hour orientation, which took place 2 to 5 years prior [
36]. Participants were primarily trained to do Pap smears, VIA, and visual inspection with Lugol's iodine (VILI) [
36]. As a result, most participants felt that the training they received in screening and treating precancerous lesions was insufficient and contributed to a lack of confidence in performing screening procedures and preventive treatment [
36].
Knowledge levels among women at risk were found to be an integral factor regarding cervical cancer screening uptake. This aligns with the results of similar studies conducted in Tanzania, which found that screening acceptance is associated with knowing about cervical cancer, its risk factors, and the role of prevention [
24]. The need for education regarding cervical cancer prevention exists across sub-Saharan Africa, as several studies have found that women who lack knowledge of cervical cancer risk and the role of screening (especially in rural locations) are less likely to participate in screening services and are at greater risk for developing invasive cervical cancer [
24].
The provision of health education with the end goal of disseminating information to male partners was highlighted as a topic of importance by one woman. One study highlighted the importance of male involvement in the cervical cancer cascade, as it found that, of the women presenting for screening, 43.6% came alone, and 12.8% were accompanied by at least one male relative [
25]. Opposingly, in the treatment group, 16.3% came alone, and 44.9% were accompanied by a male [
25]. Thus, it is evident that men play a role in their partner’s reproductive health experiences in many ways: shared decision-making, granting permission services, or providing financial support and transport for health services [
37].
Knowledge levels before screening also significantly affected women's screening acceptance in other studies. It was discovered that women who had attended at least primary school were more likely to attend screening than women who had never attended school [
38]. It is thus evident that more work is required to address gaps in patient education at an earlier age as this will lead to better acceptance of cervical cancer screening services in the future.
Beliefs on Cervical Cancer Screening
Our research found that women believed that cervical cancer was caused by a variety of causes including contraceptives/medications, food, fate, and karma. There continues to be a lack of adequate knowledge surrounding cervical cancer among Tanzanian women and HCPs, serving as a barrier to cervical cancer screening. During a Prevention and Awareness Campaign in Northern Tanzania (2017-2019), a series of multiple-choice questions were distributed to participants to identify their beliefs and misbeliefs about the etiology and causes of cervical cancer [
39]. A concerning number of women attributed the cause to using contraceptives (20%), while others selected it to be a result of a curse (14%), receiving the vaccine (5.8%), or through direct contact with a cancer patient (2.8%) [
39]. Interestingly, incorrect responses were positively correlated with women living in rural regions of Tanzania [
39].
In another study, a community-based cross-sectional was performed to gather predictors of cervical cancer screening [
11]. A striking 1013 (91.8%) of the respondents had not been screened for cervical cancer [
11]. Notably, screening intention, health beliefs, and knowledge level were identified as predictors for cervical cancer screening [
11]. Interestingly, 53% had inadequate knowledge of cervical cancer and screening, 54.4% had no screening intention, 50% had negative health beliefs, and 53% had inadequate knowledge of cervical cancer and screening [
11]. It was determined that respondents who had no intention to screen were less likely to uptake cervical cancer screening [
11]. Respondents suffered many gaps surrounding the knowledge about VIA, especially in terms of its purpose, suggested age for screening, and the appropriate screening intervals [
11]. There is a clear need to conduct community-awareness-raising campaigns and knowledge-raising campaigns to increase cervical cancer knowledge and establish peer-supporting screening programs in communities. It might be beneficial to explore peer-led navigation to promote cervical cancer screening knowledge, intention, and practices among urban women in Tanzania. Specifically, it is a form of task sharing that delegates cervical-cancer-related tasks from HCPs to community health workers.
The lack of knowledge surrounding cervical cancer extends across various levels of Tanzania’s health system. Specifically, there continues to be a lack of education even among HCPs. In one study, it was identified that less than half of the nurses had adequate knowledge regarding cervical cancer [
40]. Specifically, knowledge levels of causes of cervical cancer and transmission of HPV and age demonstrated a significant correlation [
40]. Interestingly, levels of knowledge ranged across the levels of HCPs, although seemed to be more adequate among young nurses [
40]. In terms of screening intervals being aware of the HPV vaccine, it was identified that registered nurses had more knowledge than enrolled nurses [
40]. Notably, 84.6% of the nurses had never had a Pap smear examination [
40]. Moreover, the results of this study indicate the pressing need to continue medical education and awareness across all levels of Tanzania’s healthcare sector.
Traditional Medicine
Reasons for seeking traditional medicine treatment may be an amalgamation of beliefs and financial strains, causing women to use local herbs rather than seek appropriate treatment for signs and symptoms that may be due to cervical cancer. A study of 655 adults in Northern Tanzania found that a majority of respondents use traditional medicines due to lower cost, fewer side effects, ease of access, and perceived safety and efficacy [
41]. Importantly, it is not the inadequacy of the modern health system alone that influences women to seek traditional medicine, but rather a combination of factors related to cultural beliefs, past experiences, financial considerations and potentially residing in a more rural location versus urban where use of traditional healers may be less prevalent and health literacy may be higher especially with respect to screening services [
41]. The use of traditional healers, particularly when signs and symptoms may already be present (and diagnosis is needed instead of screening) may be influenced by external factors such as fear of a cancer diagnosis and fear of the financial implications this may have on the family [
41]. In some cases, traditional healers may deliberately promote the use of traditional medicines and their effectiveness at curing cancers [
42]. This belief was the same in rural and urban sites as per a 2014 study conducted in northern Uganda [
42].
Risk Factors/Symptoms and Signs
The HCPs interviewed in our study understood that HIV is a significant risk factor for cervical cancer. In one study, approximately four in ten Tanzanian women denied that they knew anything about the warning signs and risk factors for cervical cancer [
31]. Many women commonly believed that oral contraceptives, condom usage, and swimming in public pools were risk factors [
11]. Unfortunately, in a similar study, it was also identified that a high proportion of women were also completely ignorant about warning signs and risk factors [
11]. Interestingly, 83.7% of respondents were not aware that family history is a notable risk factor for cervical cancer [
11]. In addition, 83% and 78.4% were not aware that HIV/AIDS and pregnancies and deliveries, respectively, could increase the risk of disease [
11].
In a community-based study, many women (68.3%) were not able to identify bleeding and spotting after menopause as signs of cervical cancer and (72.1%) were not able to identify bleeding and feeling pain after intercourse, as possible signs of cervical cancer [
11]. In another community-based cross-sectional study in the Ilala municipality in Tanzania, a total of 210 women were interviewed [
43]. Among all responses, irregular vaginal bleeding was the most common symptom that was mentioned by participants (51.7%) [
43].
Strengths and Limitations
One strength of this study is its inclusion of perspectives from different domains of health care (key informants, women at risk, and HCPs). This provides us with a comprehensive understanding of awareness and knowledge surrounding cervical cancer screening in rural Tanzania, as compared to other studies, which limit their findings to solely women in the community [
31].
Another strength of the study was that semi-structured interviews were conducted to allow participants to better express their opinions and experiences in an open and free manner. This flexible interview protocol consists of open dialogue between the researcher and participant and encourages deeper conversations about personal and sensitive issues [
44]. Additionally, the incorporation of inter-coder reliability offers several benefits, such as improving the systematicity, communicability, and transparency of the coding process: promoting reflexivity and dialogue within the research team and strengthening the reliability of the analysis [
45].
A significant limitation of this study is its qualitative nature, resulting in an increased risk of error and bias and the potential for less internal validity.
Another limitation of this study is that we sampled participants from 8 districts in 4 regions in Tanzania. The results should be more generalizable to semi-rural and rural health facilities and communities and may have differed if we had sampled only urban locations or expanded our sampling to include a more equal distribution of urban and rural participants.
Conclusion
There is a low level of knowledge of cervical cancer risk and the role of screening and prevention services among HCPs and women at risk in rural and semi-rural Tanzania. There is a critical need to implement strategies among health providers, within health facilities, in health promotion and in rural communities to increase screening uptake and access to screening services among women at risk.
Funding Information
This research was funded by Grand Challenges Canada (Grant Number 0774-05: Transition to Scale: A smartphone-based task-sharing approach to breast and cervical cancer control in Tanzania: mPowering women to save lives).
Acknowledgments
We would like to thank all the participants, HCPs, and researchers for their contributions to this study. We would also like to acknowledge the team members who assisted with translating the semi-structured interview guides. We would also like to thank Isabell Risso-Gill for providing us with the Health Systems Appraisal Toolkit.
Author Contributions
Conceptualization, K.Y.; Methodology, K.Y.; Formal Analysis, M.C., S.K.; Writing – Original Draft Preparation, K.Y., M.C., S.K.; Writing – Review & Editing, K.Y., M.C., S.K., N.W., E.E., S.Y., K.M., J.S., D.S.; Visualization, M.C.; Supervision, K.Y.; Project Administration, N.W., K.Y.; Funding Acquisition, K.Y. The authors have reviewed and approved the final manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the National Institute of Medical Research.
Ethic Statements
This project was part of a larger implementation research project that received approval from Queen's University, Canada, and NIMR, Tanzania. Participants were informed that their responses would be completely confidential no identifying information about them would be recorded beyond the information collected and that all transcript data would be de-identified. Each participant was given a copy of the informed consent document. Consent was obtained in both verbal and written formats. Information regarding age (where provided), sex, marital and occupational status was collected. Informed consent was obtained from all subjects involved in the study.
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA. Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Runge, A.S.; Bernstein, M.E.; Lucas, A.N.; Tewari, K.S. Cervical Cancer in Tanzania: A Systematic Review of Current Challenges in Six Domains. Gynecol. Oncol. Rep. 2019, 29, 40–47. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Framework for Strengthening and Scaling-up of Services for the Management of Invasive Cervical Cancer; World Health Organization: Geneva, 2020; ISBN 978-92-4-000323-1. [Google Scholar]
- World Health Organization. New WHO Recommendations on Screening and Treatment to Prevent Cervical Cancer among Women Living with HIV: Policy Brief; World Health Organization: Geneva, 2021; ISBN 978-92-4-003096-1. [Google Scholar]
- World Health Organization; International Agency for Research on Cancer; African Population and Health Research Center Prevention of Cervical Cancer through Screening Using Visual Inspection with Acetic Acid (VIA) and Treatment with Cryotherapy. A Demonstration Project in Six African Countries: Malawi, Madagascar, Nigeria, Uganda, the United Republic of Tanzania, and Zambia; World Health Organization: Geneva, 2012; ISBN 978-92-4-150386-0. [Google Scholar]
- Mchome, B.; Swai, P.; Wu, C.; Katanga, J.; Kahesa, C.; Manongi, R.; Mwaiselage, J.D.; Kjaer, S.; Rasch, V.; Linde, D.S. Comprehensive Cervical Cancer Prevention in Tanzania (CONCEPT) Study: Cohort Profile. BMJ Open 2020, 10, e038531. [Google Scholar] [CrossRef] [PubMed]
- Adsul, P.; Manjunath, N.; Srinivas, V.; Arun, A.; Madhivanan, P. Implementing Community-Based Cervical Cancer Screening Programs Using Visual Inspection with Acetic Acid in India: A Systematic Review. Cancer Epidemiol. 2017, 49, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Katanga, J.; Kjaer, S.K.; Manongi, R.; Wu, C.S.; Iftner, T.; Waldstrom, M.; Pembe, A.B.; Mwaiselage, J.; Rasch, V. Performance of careHPV, Hybrid Capture 2 and Visual Inspection with Acetic Acid for Detection of High-Grade Cervical Lesion in Tanzania: A Cross-Sectional Study. PLOS ONE 2019, 14, e0218559. [Google Scholar] [CrossRef] [PubMed]
- Verbal communication from Dr. Safina Yuma, Focal Lead, Ministry of Health, Tanzania.
- Moshi, F.V.; Vandervort, E.B.; Kibusi, S.M. Cervical Cancer Awareness among Women in Tanzania: An Analysis of Data from the 2011-12 Tanzania HIV and Malaria Indicators Survey. Int. J. Chronic Dis. 2018, 2018, 2458232. [Google Scholar] [CrossRef] [PubMed]
- Mabelele, M.M.; Materu, J.; Ng’ida, F.D.; Mahande, M.J. Knowledge towards Cervical Cancer Prevention and Screening Practices among Women Who Attended Reproductive and Child Health Clinic at Magu District Hospital, Lake Zone Tanzania: A Cross-Sectional Study. BMC Cancer 2018, 18, 565. [Google Scholar] [CrossRef]
- Mboineki, J.F.; Wang, P.; Dhakal, K.; Getu, M.A.; Millanzi, W.C.; Chen, C. Predictors of Uptake of Cervical Cancer Screening among Women in Urban Tanzania: Community-Based Cross-Sectional Study. Int. J. Public Health 2020, 65, 1593–1602. [Google Scholar] [CrossRef] [PubMed]
- Yimer, N.B.; Mohammed, M.A.; Solomon, K.; Tadese, M.; Grutzmacher, S.; Meikena, H.K.; Alemnew, B.; Sharew, N.T.; Habtewold, T.D. Cervical Cancer Screening Uptake in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Public Health 2021, 195, 105–111. [Google Scholar] [CrossRef]
- Legido-Quigley, H.; Camacho Lopez, P.A.; Balabanova, D.; Perel, P.; Lopez-Jaramillo, P.; Nieuwlaat, R.; Schwalm, J.-D.; McCready, T.; Yusuf, S.; McKee, M. Patients’ Knowledge, Attitudes, Behaviour and Health Care Experiences on the Prevention, Detection, Management and Control of Hypertension in Colombia: A Qualitative Study. PloS One 2015, 10, e0122112. [Google Scholar] [CrossRef]
- Risso-Gill, I.; Balabanova, D.; Majid, F.; Ng, K.K.; Yusoff, K.; Mustapha, F.; Kuhlbrandt, C.; Nieuwlaat, R.; Schwalm, J.-D.; McCready, T.; et al. Understanding the Modifiable Health Systems Barriers to Hypertension Management in Malaysia: A Multi-Method Health Systems Appraisal Approach. BMC Health Serv. Res. 2015, 15, 254. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Report - Health Systems: Improving Performance. Geneva: WHO; 2000.
- World Health Organization. A Cervical Cancer-Free Future for Women in Tanzania. 2023.
- Yeates KE, Sleeth J, Hopman W, Ginsburg O, Heus K, Andrews L, Giattas MR, Yuma S, Macheku G, Msuya A, Oneko O. Evaluation of a Smartphone-Based Training Strategy Among Health Care Workers Screening for Cervical Cancer in Northern Tanzania: The Kilimanjaro Method. J Glob Oncol. 2016 May 4;2(6):356-364. eCollection 2016 Dec. [CrossRef]
- Yeates and Ginsburg et al. A smartphone-enhanced training, QA, monitoring and evaluation platform for secondary prevention of cervical cancer: opportunities and challenges to successful large-scale implementation in Tanzania. Journal of Global Oncology. June 2020.
- United Republic of Tanzania - Ministry of Health, Community Development, Gender, Elderly and Children. Tanzania Service Delivery Guidelines for Cervical Cancer Prevention and Control Programme. 2nd Ed August 2021.
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Saunders, C.H.; Sierpe, A.; Plessen, C. von; Kennedy, A.M.; Leviton, L.C.; Bernstein, S.L.; Goldwag, J.; King, J.R.; Marx, C.M.; Pogue, J.A.; et al. Practical Thematic Analysis: A Guide for Multidisciplinary Health Services Research Teams Engaging in Qualitative Analysis. BMJ 2023, 381, e074256. [Google Scholar] [CrossRef] [PubMed]
- Rick, T.J.; Deming, C.M.; Helland, J.R.; Hartwig, K.A. Cancer Training for Frontline Healthcare Providers in Tanzania. J. Cancer Educ. 2019, 34, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Kahesa, C.; Kjaer, S.; Mwaiselage, J.; Ngoma, T.; Tersbol, B.; Dartell, M.; Rasch, V. Determinants of Acceptance of Cervical Cancer Screening in Dar Es Salaam, Tanzania. BMC Public Health 2012, 12, 1093. [Google Scholar] [CrossRef]
- Peters, L.M.; Soliman, A.S.; Bukori, P.; Mkuchu, J.; Ngoma, T. Evidence for the Need of Educational Programs for Cervical Screening in Rural Tanzania. J. Cancer Educ. 2010, 25, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Niyonsenga, G.; Gishoma, D.; Sego, R.; Uwayezu, M.G.; Nikuze, B.; Fitch, M.; Igiraneza, P.C. Knowledge, Utilization and Barriers of Cervical Cancer Screening among Women Attending Selected District Hospitals in Kigali - Rwanda. Can. Oncol. Nurs. J. 2021, 31, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Stewart, B.W.; Coates, A.S. Cancer Prevention: A Global Perspective. J. Clin. Oncol. 2005, 23, 392–403. [Google Scholar] [CrossRef]
- Cooper, E.C.; Maher, J.A.; Naaseh, A.; Crawford, E.W.; Chinn, J.O.; Runge, A.S.; Lucas, A.N.; Zezoff, D.C.; Bera, K.R.; Dinicu, A.I.; et al. Implementation of Human Papillomavirus Video Education for Women Participating in Mass Cervical Cancer Screening in Tanzania. Am. J. Obstet. Gynecol. 2021, 224, 105.e1–105e9. [Google Scholar] [CrossRef]
- Maharajan, M.K.; Rajiah, K.; Sze Fang, K.N.; Lui, L.Y. Cervical Cancer Prevention in Malaysia: Knowledge and Attitude of Undergraduate Pharmacy Students Towards Human Papillomavirus Infection, Screening and Vaccination in Malaysia. J. Cancer Educ. 2017, 32, 166–174. [Google Scholar] [CrossRef]
- Perng, P.; Perng, W.; Ngoma, T.; Kahesa, C.; Mwaiselage, J.; Merajver, S.D.; Soliman, A.S. Promoters of and Barriers to Cervical Cancer Screening in a Rural Setting in Tanzania. Int. J. Gynecol. Obstet. 2013, 123, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Weng, Q.; Jiang, J.; Haji, F.M.; Nondo, L.H.; Zhou, H. Women’s Knowledge of and Attitudes toward Cervical Cancer and Cervical Cancer Screening in Zanzibar, Tanzania: A Cross-Sectional Study. BMC Cancer 2020, 20, 63. [Google Scholar] [CrossRef]
- Shiferaw, S.; Addissie, A.; Gizaw, M.; Hirpa, S.; Ayele, W.; Getachew, S.; Kantelhardt, E.J.; Assefa, M.; Jemal, A. Knowledge about Cervical Cancer and Barriers toward Cervical Cancer Screening among HIV-positive Women Attending Public Health Centers in Addis Ababa City, Ethiopia. Cancer Med. 2018, 7, 903–912. [Google Scholar] [CrossRef]
- Buchanan Lunsford, N.; Ragan, K.; Lee Smith, J.; Saraiya, M.; Aketch, M. Environmental and Psychosocial Barriers to and Benefits of Cervical Cancer Screening in Kenya. The Oncologist 2017, 22, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Koneru, A.; Jolly, P.E.; Blakemore, S.; McCree, R.; Lisovicz, N.F.; Aris, E.A.; Mtesigwa, T.; Yuma, S.; Mwaiselage, J.D. Acceptance of Peer Navigators to Reduce Barriers to Cervical Cancer Screening and Treatment among Women with HIV Infection in Tanzania. Int. J. Gynecol. Obstet. 2017, 138, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Coronado Interis, E.; Anakwenze, C.P.; Aung, M.; Jolly, P.E. Increasing Cervical Cancer Awareness and Screening in Jamaica: Effectiveness of a Theory-Based Educational Intervention. Int. J. Environ. Res. Public. Health 2016, 13, 53. [Google Scholar] [CrossRef] [PubMed]
- Bateman, L.B.; Blakemore, S.; Koneru, A.; Mtesigwa, T.; McCree, R.; Lisovicz, N.F.; Aris, E.A.; Yuma, S.; Mwaiselage, J.D.; Jolly, P.E. Barriers and Facilitators to Cervical Cancer Screening, Diagnosis, Follow-Up Care and Treatment: Perspectives of Human Immunodeficiency Virus-Positive Women and Health Care Practitioners in Tanzania. The Oncologist 2019, 24, 69–75. [Google Scholar] [CrossRef]
- Muia, E.; Kimani, V.; Leonard, A. Integrating Men into the Reproductive Health Equation: Acceptability and Feasibility in Kenya; Population Council, 2000.
- Bradley, J.; Risi, L.; Denny, L. Widening the Cervical Cancer Screening Net in a South African Township: Who Are the Underserved? Health Care Women Int. 2004, 25, 227–241. [Google Scholar] [CrossRef]
- Henke, A.; Kluge, U.; Borde, T.; Mchome, B.; Serventi, F.; Henke, O. Tanzanian Women´s Knowledge about Cervical Cancer and HPV and Their Prevalence of Positive VIA Cervical Screening Results. Data from a Prevention and Awareness Campaign in Northern Tanzania, 2017 - 2019. Glob. Health Action 2021, 14, 1852780. [Google Scholar] [CrossRef]
- Urasa, M.; Darj, E. Knowledge of Cervical Cancer and Screening Practices of Nurses at a Regional Hospital in Tanzania. Afr. Health Sci. 2011, 11, 48–57. [Google Scholar]
- Stanifer, J.W.; Patel, U.D.; Karia, F.; Thielman, N.; Maro, V.; Shimbi, D.; Kilaweh, H.; Lazaro, M.; Matemu, O.; Omolo, J.; et al. The Determinants of Traditional Medicine Use in Northern Tanzania: A Mixed-Methods Study. PLOS ONE 2015, 10, e0122638. [Google Scholar] [CrossRef] [PubMed]
- Mwaka, A.D.; Okello, E.S.; Orach, C.G. Barriers to Biomedical Care and Use of Traditional Medicines for Treatment of Cervical Cancer: An Exploratory Qualitative Study in Northern Uganda. Eur. J. Cancer Care (Engl.) 2015, 24, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Chande, H.; Kassim, T. Assessment of Women‘s Knowledge and Attitude towards Carcinoma of the Cervix in Ilala Municipality. East Afr. J. Public Health 2011, 7. [Google Scholar] [CrossRef] [PubMed]
- DeJonckheere, M.; Vaughn, L.M. Semistructured Interviewing in Primary Care Research: A Balance of Relationship and Rigour. Fam. Med. Community Health 2019, 7, e000057. [Google Scholar] [CrossRef]
- O’Connor, C.; Joffe, H. Intercoder Reliability in Qualitative Research: Debates and Practical Guidelines. Int. J. Qual. Methods 2020, 19, 1609406919899220. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).