1. Introduction
Temporomandibular disorders (TMDs) include a group of clinical signs and symptoms in the temporomandibular joints, masticatory system, and related structures [
1]. TMD affects 5-12% of the population [
2]; in addition, it has been confirmed that more women suffer from TMDs than men, with a prevalence of 6.3%, compared to 2.8% [
3]. Symptoms of TMD include pain and/or changes to temporomandibular joint (TMJ) functions; specifically, pain in the jaw joint and/or masticatory muscles, limited mobility and joint crepitus are the three most representative symptoms [
4]. The causes of TMD include structural factors (e.g., skeletal, neural, muscular), functional factors (e.g., posture, lifestyle), and psychological factors (e.g., stress), or any combination of them [
1].
The evaluation of TMD typically involves a multifaceted approach that integrates various clinical assessments, imaging techniques, and subjective patient-reported measures [
5]. Clinical examination typically includes: (i) the assessment of jaw mobility and function; (ii) palpation of the TMJ and surrounding muscles to identify tenderness, swelling, or muscle spasms; (iii) evaluation of occlusion; and (iv) assessment of associated symptom. Imaging modalities may include X-rays, magnetic resonance imaging (MRI) and computed tomography (CT) providing valuable information about the TMJ and surrounding structures [
6]. However, the risks associated with radiological exposure and the costs of these types of assessments cannot be overlooked, as well as the availability of specialized clinical laboratories, also in consideration of the need to be able to monitor rehabilitation treatments [
7]. In addition to instrumented-based approach, patient-reported outcome measures can provide valuable information about the impact of TMD on daily functioning, quality of life, and psychological factors such as anxiety or depression [
8]. Common questionnaires include the Oral Health Impact Profile (OHIP), Jaw Function Limitation Scale (JFLS), and TMD-specific questionnaires like the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD). By combining these various assessment methods, clinicians can obtain a comprehensive understanding of the patient's TMDs presentation, allowing for accurate diagnosis and appropriate treatment planning [
9]. These rating scales, despite being considered the gold standard for more than 25 years, are continually placed under review for their validity and reliability [
10] and questioned among clinical operators [
11].
Aiming to improve the quality of the diagnosis and monitoring, much attention in recent years has been paid to the postural assessment of people affected by TMDs. Many studies have focused on the evaluation of posture and mobility of the cervical spine, whereas others have focused on the quality of balance management and ground support. Walczyńska-Dragon et al. evaluate the influence of TMDs therapy on cervical spine range of movement (ROM), analyzed by an ultrasound device, and reduction of spinal pain [
12]. After 3 months of therapy the results showed a significant improvement in TMJ function, cervical spine ROM, and a reduction of spinal pain demonstrating a significant association between TMDs treatment and reduction of cervical spine pain, as far as improvement of cervical spine mobility. Grondin et al. used an inclinometer to evaluate cervical ROM measures in twenty asymptomatic subjects compared with 37 subjects with pain attributed to TMDs [
13]. The researchers highlighted significant differences between groups indicating that’s subjects with TMDs had signs of upper cervical spine ROM impairment. Regarding body posture, Nota et al. have highlighted that there is a significant difference in the postural stability of the body between subjects suffering from myogenic TMD and healthy controls [
14]. In particular, the postural parameters of the oscillation area and of the oscillation speed were increased when gathered from participants affected by TMDs. Souza et al. evaluated body posture through photogrammetry and the distribution of plantar pressure, with a pressure platform, at physiologic rest of the mandible and during maximal intercuspal positions in subjects with and without TMDs [
15]. They found more pronounced cervical distance, valgus of the right calcaneus, and lower pelvic tilt in the photogrammetric analysis and a higher rearfoot and lower forefoot distribution for the TMD subjects, while no differences were verified in maximal intercuspal position in the between-group analysis and between the two mandibular positions in the within-group analysis. In contrast, Scharnweber et al. did not find evidence of correlations between the parameters provided by a pressure platform during a static and dynamic examination in subjects with different dental occlusions, concluding that postural control and plantar pressure distribution are independent of each other [
16]. Despite the plethora of studies published on the topic, the correlation between postural assessments and TMDs remains unclear [
17,
18,
19].
Considering these aspects, as well as the notable advances in artificial intelligence (AI), the application of machine learning algorithms appears to be a promising approach for diagnosis in clinics, such as for TMDs [
20], and in sports [
21,
22]. In particular, AI algorithms can analyse medical imaging data gathered by MRI, CT scans, and X-rays to identify anatomical abnormalities, joint degeneration, or structural irregularities indicative of TMDs. Machine learning models, particularly convolutional neural networks (CNNs), have been demonstrated to excel in image recognition tasks and can assist in automating the detection and classification of TMD-related pathologies. Reda et al. proposed an architecture based on commercially available cognitive computing services, trained using scientific documents and interviews with experienced professionals regarding the diagnosis of TMDs. They give preliminary proof of the feasibility of implementing an AI-based system to support untrained dentists in the recognition of TMDs. Furthermore, the work conducted by Lee et al. aimed to identify contributing biological and psychosocial factors and their relative importance as risk factors for the development of TMDs using artificial intelligence methodologies on a nationwide sample of 4744 participants [
23]. They used six artificial intelligence approaches, SVM, Artificial Neural Network (ANN), Random Forest, Naïve Bayes, Decision Tree and Logistic Regression for identifying the factors associated with TMDs. Their results highlighting the importance of obesity, general health, stress, socioeconomic status, and working conditions in the management of TMDs.
Although the promising usefulness of artificial intelligence in providing automatic information for the diagnosis and classification of TMDs is evident, the already published papers, to the best of authors' knowledge, are focused on data gathered from high-cost and not-portable technologies, such as MRI and CT, or not associated with physical functions. Thus, the aim of the present study is to propone a sensor system based on low-cost and portable technologies, such as inertial sensors and baropodometric platform, in order to gather data to fed machine-learning algorithms for the identification of TMDs. From this perspective, we performed a comparative analysis among the most widely used machine-learning algorithms fed with data related to baropodometric analysis and cervical mobility to define the best performing one.
The findings of the study can represent a starting point to foster the use of portable sensor system to objectivize the identification of TMDs in clinical settings.
2. Materials and Methods
2.1. Participants
Fifty subjects (20 males and 30 females) were involved in the study. They were divided into two homogeneous groups of 10 males and 15 females; a group of healthy subjects acting as control group (CG) (height = 172±8 cm, body mass = 68±13 kg, age = 31±6 years) and a group with TMD (TMD) (height = 172±10 cm, body mass = 69±14 kg, age = 32±7 years). The division into the two groups was carried out through a clinical examination performed by an experienced operator in combination with two questionnaires on anxiety and depression. For recruitment the exclusion criteria were the following: a) No orthodontic treatment in progress; b) Not having undergone orthognathic surgery; c) Diagnosis of other painful orofacial conditions; d) Primary disorder of the cervical spine such as herniated disc or significant degenerative changes in the spine; e) Systemic disease that could compromise the mobility of the spine such as spondylitis; f) Reported injuries, accidents involving the head or vertebral column. All participants were initially informed about the purpose of the study and asked to sign a written consent. The experimental procedures were in accordance with the principles set out in the Declaration of Helsinki. The study has been approved by the approved by the Institutional Review Board of the Ovidius University of Constanta (Romania) with the protocol n. 45 in date 23.01.2024.
2.2. Experimental Protocol and Setup
The experimental protocol was composed of two distinct evaluations: the first consisted in the clinical evaluation of the subjects, whereas in the second part the instrumental evaluation was carried out. Both assessments were carried out on the same day and the complete protocol lasted approximately 30 minutes per participant.
2.2.1. Clinical Assessment
The clinical evaluation protocol was structured in two parts. The first part focused on the physical aspects of the patient and was based on the recent review of Malgorzata et al. on the Diagnostic of Temporomandibular Disorders and Other Facial Pain Conditions [
24]. The protocol was carried out by a physiotherapist with advanced training in manual therapy of the TMJ and cervical spine. The second part consisted of the administration of two questionnaires: the Patient Health Quality 9-item (PHQ-9) and the Generalized Anxiety Disorder 7-item (GAD-7). These questionnaires are part of Annex II of the Diagnostic Criteria for Temporomandibular Disorder (DCTMD) [
25], which is the standard tool used to assess TMD both the physical and psychosocial aspects of the patient.
The first part of the clinical evaluation involves 5 steps:
Mouth opening (MO)
The operator asked the subject to open and close the mouth three times, evaluating only the opening phase [
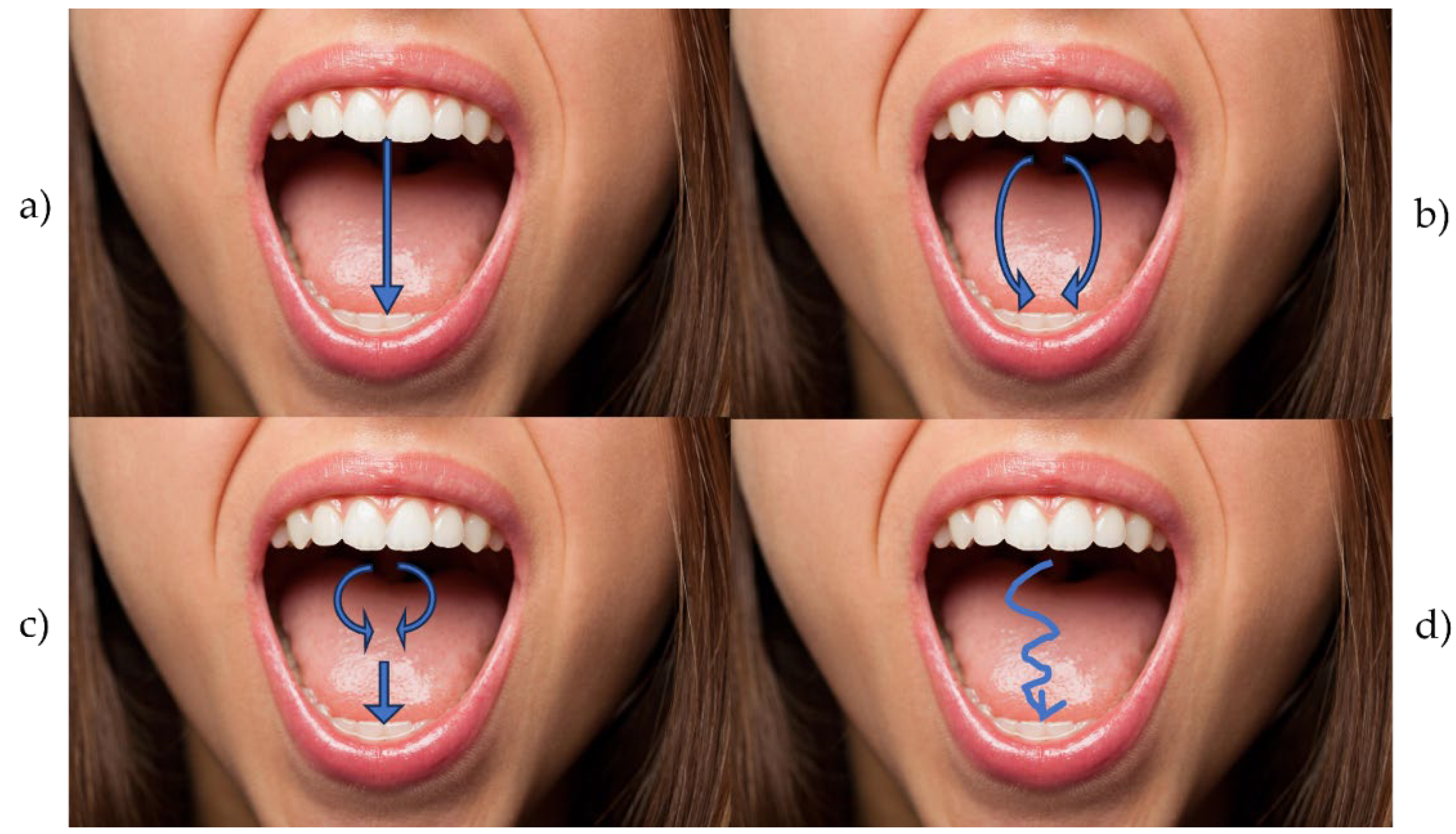
24] (
Figure 1). The movement was recorded with a smartphone so that it could be reviewed in post-processing analysis, if needed. If the participant had several opening modalities, he/she was asked to repeat the three openings and was then classified according to the following criteria:
Straight (S). No deviation is observed.
Lateral deviation to the right (RDEV) or to the left (LDEV). For deviations that are observed in the maximum aperture on one side only, operator determined which side of the face the deviation is directed to and noted it.
Corrected deviation (CDEV). The patient has a slight deviation, to the right or to the left, which are corrected either at the midline or when the maximum unguided opening is reached.
Other (O). Participant showed a discontinuous or different opening than those listed.
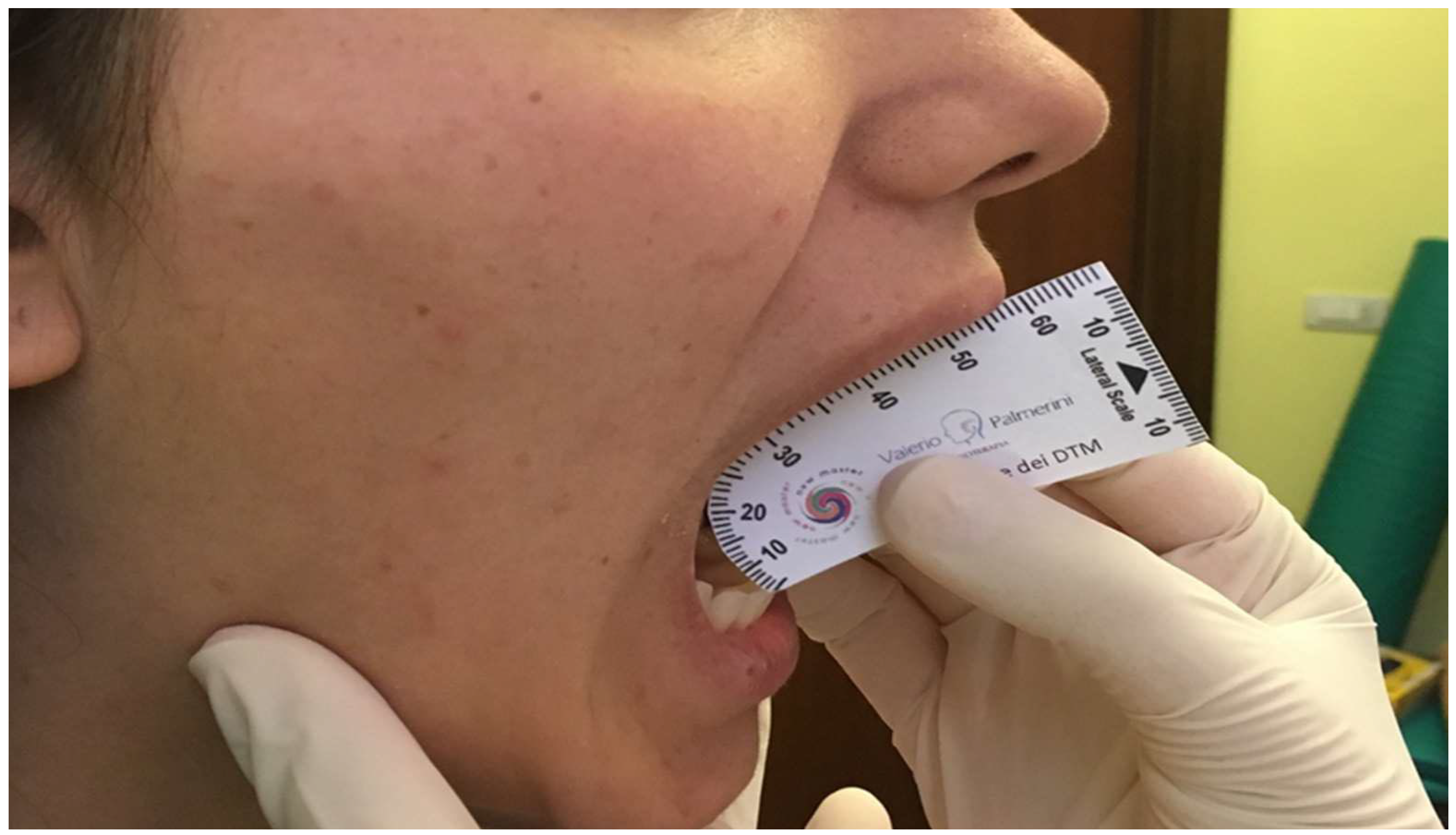
Opening Width (OW)
The operator asked the participant to place the lower jaw in a comfortable position and open the mouth as wide as possible until no pain is felt [
24]. At this point, the operator positioned the ruler vertically by measuring the distance between the edge of the upright upper incisor and the edge of the corresponding lower incisor as shown in
Figure 2.
If the opening was less than 30 mm, the measurement was repeated twice. If the aperture is less than 30 mm the second time, it was recorded.
Joint noises (JN)
The operator identified the presence and type of noise when opening the mouth. The operator placed the left index finger on the right TMJ and the right index finger on the left TMJ in front of the tragus [
24]. He/she then asked the participant to slowly open his/her mouth as much as possible, even in the presence of pain, and then to close his mouth so as to bring the teeth into maximum intercuspation. The movement was repeated three times. The operator noted the outcome of the examination according to three criteria:
0 = No noise.
1 = Click. A defined noise, of very short duration, with a distinct beginning and end, which is usually felt as a click. This noise was only noted if the shot could be reproduced in two of the three opening and closing movements.
2 = Crepitus. Continuous noise, which lasts longer than the click. Present for a longer period during the opening and closing movement. Crackling can manifest itself as continuous, overlapping noises. This noise is not muffled and can be described as the sound of bone rubbing against bone.
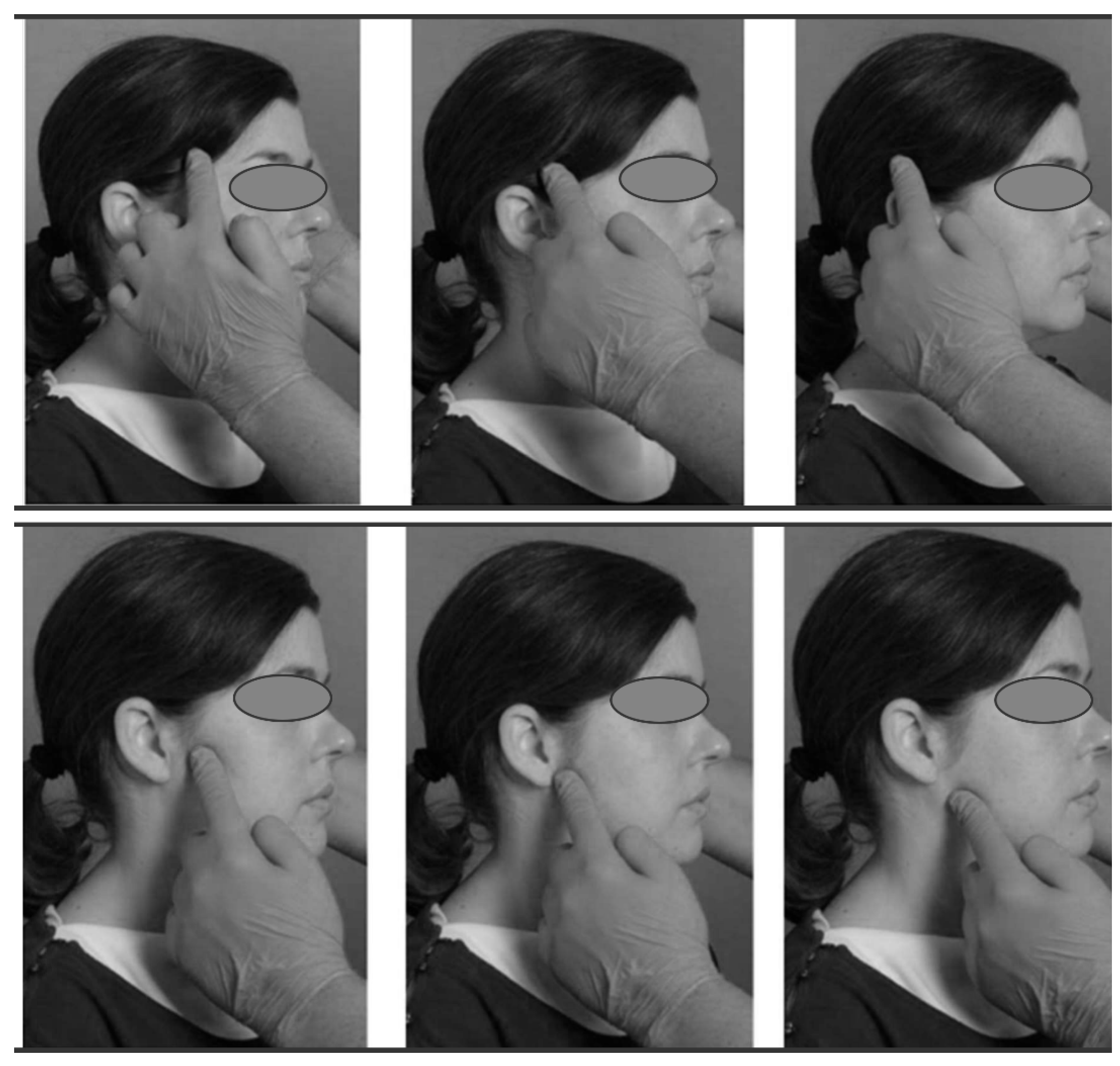
Muscle Palpation (MP)
Muscle palpation was performed by pressing with the tip of the index finger on the site of interest while with the other hand the operator held the subject's head on the side opposite to the one examined. The lower jaw had to be in a resting position, with the teeth exposed. To locate the muscle site well, the operator asked the participant to clench his/her teeth slightly and then relax the muscles [
24]. Since areas of maximum pain are variable from patient to patient, different areas of the muscle were palpated to determine if pain was present as shown in
Figure 3. The muscles evaluated were the temporalis muscle and the masseter muscle.
During palpation, the operator asked if pain or pressure was felt on certain parts of the head or face. The goal was to stimulate, during palpation, the familial pain, that is, a pain that the subject knows well and can recognize as his own. Each muscle palpation lasted 5 s for each point.
Joint Palpation (JP)
For joint palpation, the operator placed the index finger immediately in front of the tragus and above the temporomandibular joint, applying a slight pressure as shown in
Figure 4, at the same time with the other hand on the opposite side holding the head he asked to open and close the mouth [
24]. During palpation, the operator asked if pain or pressure was felt on the joint in its back or front.
PHQ-9 and GAD-7
The Patient Health Questionnaire 9-item Depression Scale (PHQ-9) and the 7-item Generalized Anxiety Disorder Scale (GAD-7) are among the best-validated and most commonly used measures of depression and anxiety, which represent two psychological variables affecting the occurrence of TMDs [
26]. They have been used in hundreds of research studies, incorporated into numerous clinical practice guidelines, and adopted by a variety of medical practice and mental health settings.
The PHQ-9 consists of 9 items that represent symptoms for DSM 5 major depressive disorder. Respondents are asked how much each symptom has bothered them over the past 2 weeks.
The GAD-7 has 7 items. Although originally developed as a measure to detect generalized anxiety disorder, the operational features of GAD-7 are almost as valid for other anxiety disorders common in clinical practice such as panic disorder, social anxiety disorder, and post-traumatic stress disorder. PHQ-9 and GAD-7 have strong internal and test-retest reliability, as well as construct validity and factor structure [
27].
2.2.2. Instrumental Assessment
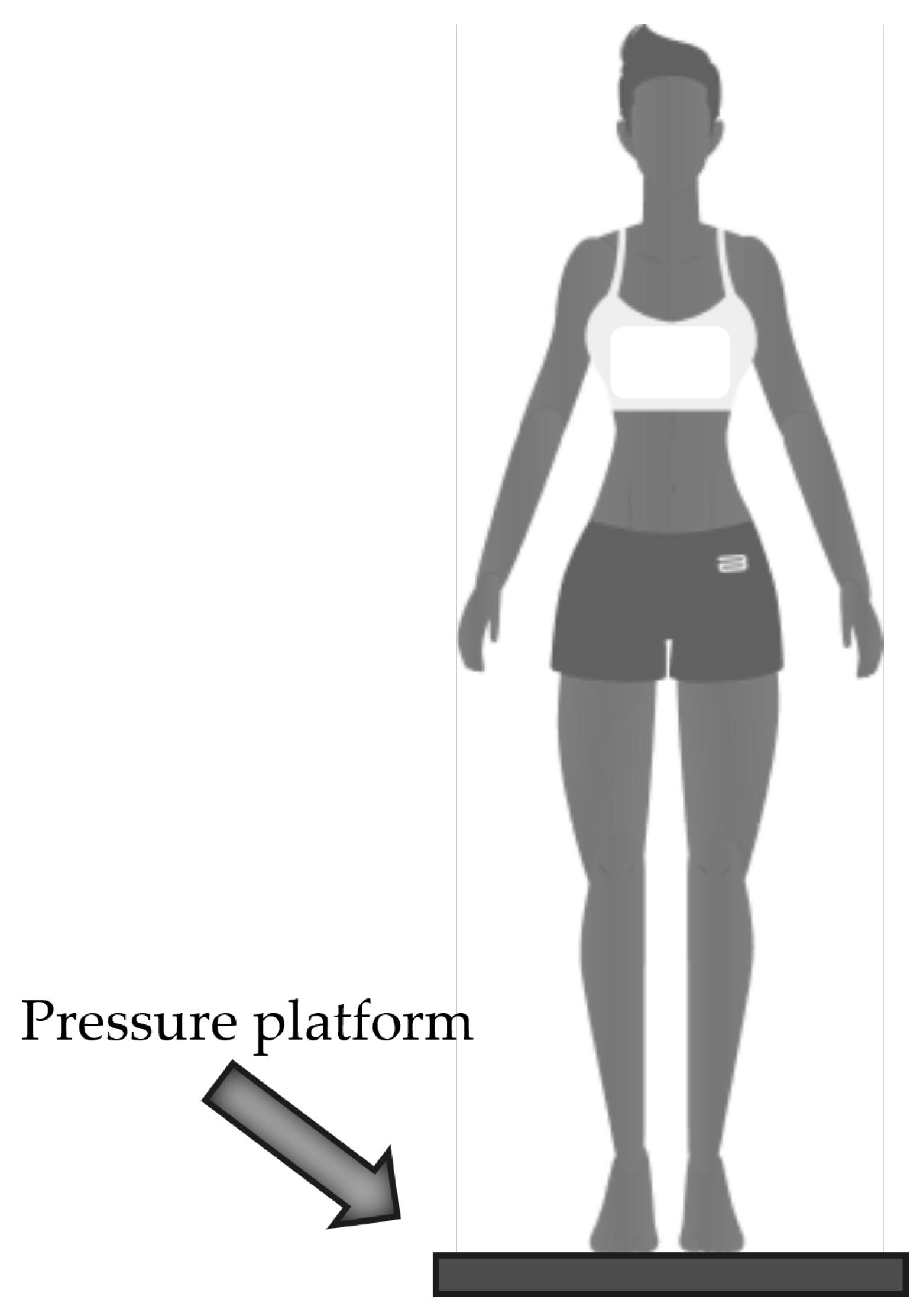
Baropodometric analysis
The freeMed BASIC 40x40 platform (Sensor Medica, Guidonia Montecelio, Italy) was used for the acquisition of baropodometric data. The platform is composed of 2.400 resistive 24k coated gold sensors arranged according to 40 rows and 40 columns for a total area of 398 x 318 mm2. The full scale of the sensors is 150 N/cm2 with an acquisition frequency up to 400 Hz and the sensitive area of each sensor is 1 x 1 cm2. The matrix is covered with a conductive synthetic rubber material in socaprene and is connected to the PC via USB cable and interfaces with the freeSTEP 2.0 software (version 2.00.010). The pressure platform is widely used in both clinical and sports applications [
28,
29,
30] and its reliability and repeatability has already been analyzed by the same authors [
31]. Experimental protocol consisted in a static task, where participants were asked to take off their footwear and step on the platform with a self-selected position of the feet. Once the subject was positioned on the platform, with relaxed arms, was asked to look forward towards a target, which was placed at a distance of 5 m, in order to stabilize the posture (
Figure 5). The duration of the static test was 5 s and was repeated three times with a 30-sbreak between trials. Once the acquisition was completed, the participant stepped off the platform and then repositioned him/herself on it. The test was repeated three times. Data was collected at a 50 Hz.
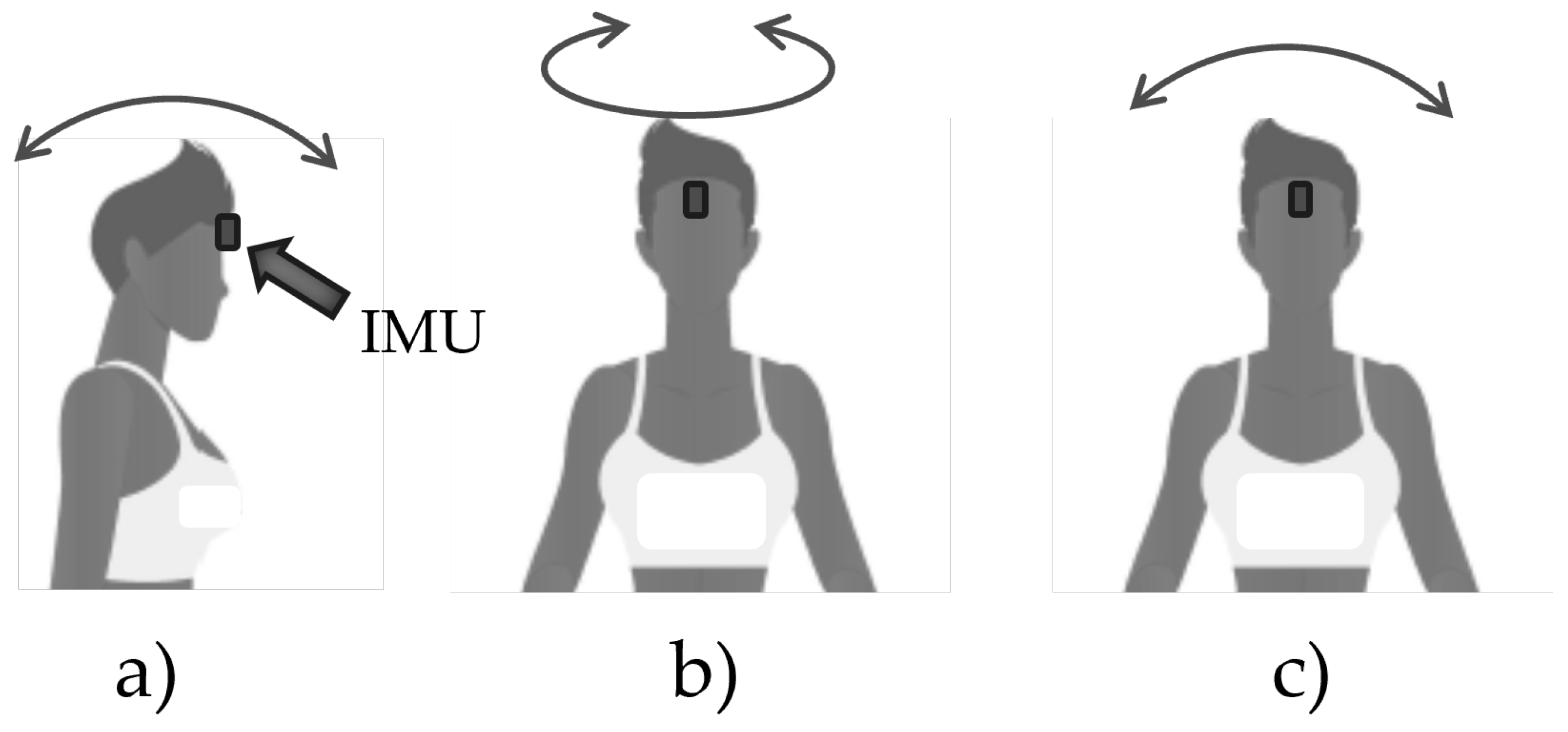
Cervical rom analysis
Cervical mobility tests were acquired with the Moover sensor (Sensor Medica, Guidonia Montecelio, Italy). The Moover device consists of an inertial measurement unit (IMU), with dimensions: 65 × 45 × 18 mm, and mass 28 g, which contains a triaxial accelerometer, gyroscope and magnetometer with full scale of ± 16 g, ± 2000 °/s and ± 4800 µT respectively. The device is equipped with an internal 32-bit processor with floating point unit that processes the data and sends the results via Bluetooth 4.0 connection to the PC and stored using the freeSTEP 2.0 software (version 2.00.010). The sampling frequency was set at 200 Hz. The validity of the device for the evaluation of cervical ROMs was analyzed in a recent article [
32]. The device was fixed on the head, in particular on the forehead, using a special semi-elastic belt equipped with specific device support to avoid relative movements during the execution of the task. The elastic waistband ensures subject comfort and reduces motion artifacts during task performance. The cervical mobility assessment was carried out standing with arms relaxed at the sides, participants were asked to fix a target placed 5 m away in front to standardize the starting position and to acquire a static phase of the inertial sensor. At this point three distinct movements were carried out as shown in
Figure 6: a) flexion-extension of the head; b) rotation of the head towards the two sides; c) inclination of the head to both sides. Each test included a total of eight movements with four repetitions performed for both sides. Participants were free to start towards whichever side they preferred. An expert operator paid attention to any compensatory movements of the body, in which case participant was asked to repeat the test.
2.3. Data Analysis and Feature Extraction
2.3.1. Clinical Assessment
The clinical assessment has been conducted in order to have the categorize each subject and to have the label for the supervised application of machine-learning algorithms. Each item of the DCTMD protocol has been analyzed independently.
Concerning the mouth opening (MO), a score of 0 or 1 has been assigned, following the rules reported in
Table 1. Thus, each subject could obtain a minimum score equal to 0 and a maximum score equal to 4.
Moving to the analysis of opening width (OW), the index reported is the millimeters measured through the proper graduated ruler, whereas the join noise (JN) task has been analyzed according to the values reported in
Table 2, with the score ranging from 0 to 2.
Considering the muscle and joint palpation, MP and JP, respectively
, the operator can assign 0 or 1 for each specific muscle/joint, where 0 and 1 indicate the absence and presence of the pain, respectively, as in
Table 3. Thus, each subject could obtain a minimum score equal to 0 and a maximum score equal to 3.
PHQ-9 and GAD-7
Finally, the analysis of the two administrated questionnaire the PHQ-9 and GAD-7 questionnaires followed the indications reported in
Table 4 and
Table 5 respectively.
The PHQ-9 can be assessed as a continuous variable from 0 to 27 (with higher scores representing more severe depression) or categorically using a diagnostic algorithm for major depression or other depressive disorders [
27]. GAD-7 presents identical responses to the PHQ-9 and therefore can be assessed as a continuous variable from 0 to 21 (with higher scores representing more severe anxiety). The most commonly used cut-off value on both PHQ-9 and GAD-7 for screening for depressive and anxiety disorders, respectively, is 10 or higher.
By combining the results of the clinical tests through the application of diagnostic decision trees reported in [
33], it is possible to diagnose the presence of TMD. The decision tree has been applied by the same skilled operator, who performed the clinical assessment.
2.3.2. Instrumental Assessment
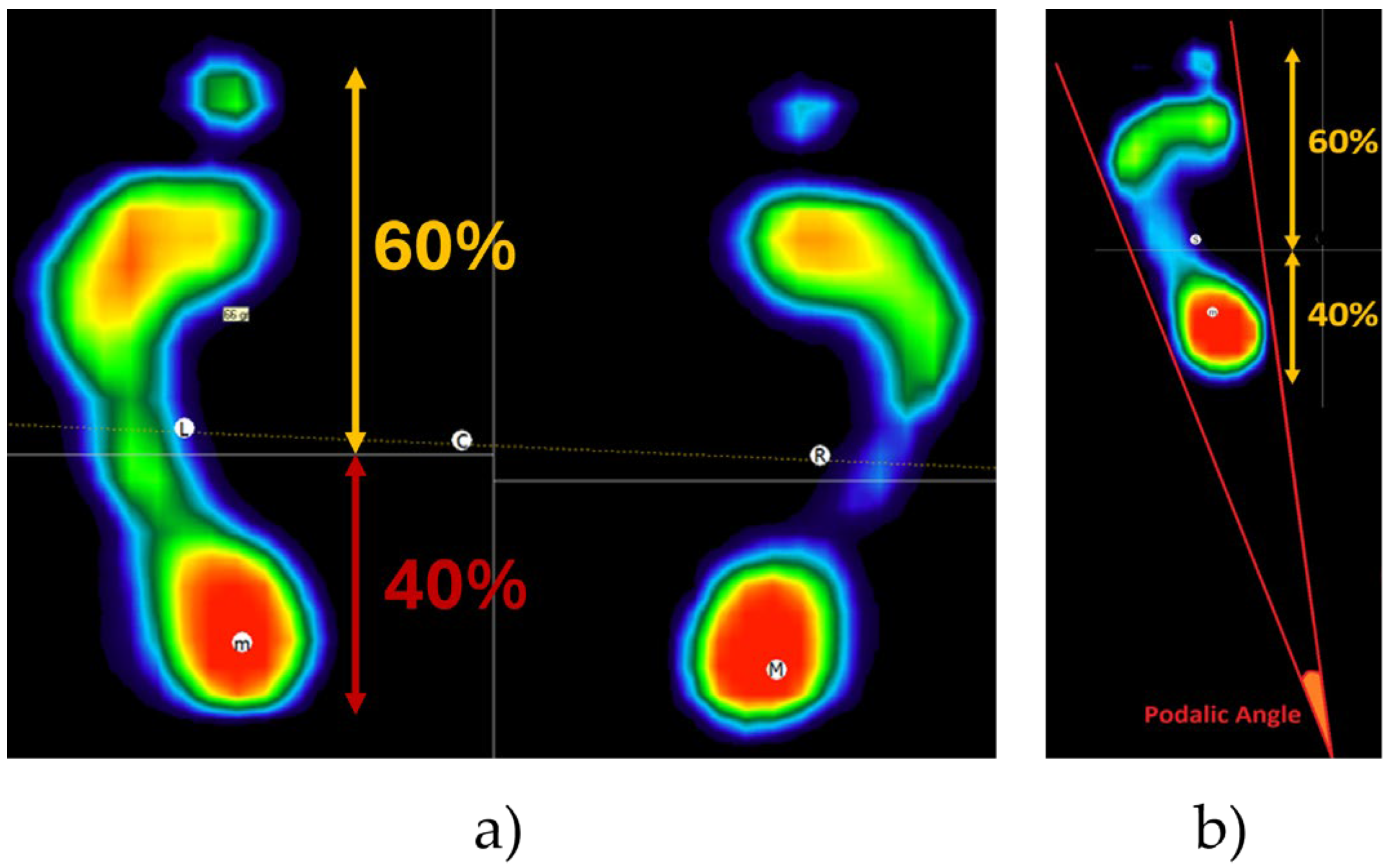
Baropodometric analysis
After placing the subject on the platform, the software automatically calibrates itself based on the subject's weight in order to avoid saturation of the platform amplifiers. Once the acquisition phase has been completed, the software automatically distinguishes between the right and left feet, dividing their footprint into forefoot and rearfoot regions based on pressure distribution, with 60% allocated to the forefoot and 40% to the rearfoot (
Figure 7a). The analysis focused on the following parameters:
the podalic angle (PA) is the angle formed by the intersection of the two lateral tangents of the footprint (
Figure 7b).
forefoot and rearfoot load percentage (FL and RL, respectively) computed as the load distribution on the forefoot and rearfoot estimated from the subject weight.
total load percentage between left and right foot (TL), indicating the percentage of the total weight distributed between the right and left side.
Each parameter was calculated for both the left and right footprint and the average value was calculated across the three repetitions, individually per each subject.
Cervical rom analysis
Regarding cervical mobility tests, the freeSTEP 2.0 software automatically realigned the Moover axes with the absolute reference system using data gathered during the initial static phase. The sensor's orientation was determined by merging linear accelerations and angular velocities using a fusion algorithm based on the Mahony filter [
34]. For each test, the first and last values of the 8 rotation movements were discarded. The average value, indicated with
θ, was then calculated, considering the following parameters, all expressed in degree:
Flexion [θFLEX]: value of the maximum angle reached in flexion.
Extension [θEXT]: value of the maximum angle reached in extension.
Total flexion-extension [θFLEX+EXT]: sum of the two angles of flexion and extension.
Right rotation [θR_ROT]: value of the maximum angle reached in rotation to the right.
Left rotation [θL_ROT]: value of the maximum angle reached in rotation to the left.
Total rotation [θTOT_ROT]: sum of the two right and left rotation angles.
Right inclination [θR_INC]: value of the maximum angle reached in the inclination to the right.
Left inclination [θL_INC]: value of the maximum angle reached when tilting to the left.
Total inclination [θTOT_INC]: sum of the two right and left inclination angles.
2.4. Machine-Learning Algorithms
To understand if a machine-learning-based approach can help to objectively assess the occurrence of TMD through the analysis of physical parameters associated with cervical mobility and baropodometric analysis, we conducted an investigation into two distinct categories of supervised machine learning algorithms: geometric and binary, as they are among the most commonly used algorithms for motion recognition [
35]. Within the geometric classifiers category, we chose to focus on the support vector machine (SVM) and the k-nearest neighbor (kNN), whereas the decision tree (DT) was selected from the binary algorithms.
SVMs are geometric supervised machine-learning algorithms that aim to identify the hyperplane that best separates features belonging to different classes [
36]. The choice of kernel function, which linearizes the feature space, is crucial before initiating the classification process. Specifically, we tested three SVMs: linear (l-SVM), quadratic (q-SVM), and cubic (c-SVM).
kNNs are geometric supervised machine learning algorithms that make classification decisions by identifying the most frequent class among the k-nearest neighbors while maximizing the distance from other classes [
37]. The distance computation equation is a key parameter to select. We examined three kNN variants: fine kNN (f-kNN), employing Euclidean distance with one neighbor; cosine kNN (c-kNN), utilizing cosine distance with ten neighbors; and weighted kNN (w-kNN), employing weighted Euclidean distance with ten neighbors based on a squared inverse approach.
Finally, DTs are binary supervised machine learning algorithms that predict the most probable class by constructing a series of nodes, wherein classification occurs through specific splitting criteria. For this study, the split criterion was based on the Gini index. The maximum number of splits is a critical parameter to choose before classification. We tested three DT variations: coarse (c-DT), medium (m-DT), and complex DT (cx-DT), with maximum split numbers set at 4, 20, and 100, respectively [
22].
By summarizing, nine machine-learning algorithms have been tested and compared. Each algorithm has been fed by using the synthetic indices extracted from the baropodometric analysis, i.e. eight features, four per each foot, and the ones associated with the cervical mobility, i.e. nine features. To evaluate which is the best solution for the feature selection, three datasets of features were constructed by considering: (i) only the features obtained from the baropodometric test – condition B; (ii) only the features gathered from the cervical mobility analysis – condition M; and (iii) all features together, for a total of 17 features, condition MB.
The performance of the tested machine-learning algorithms has been evaluated by using a 10-fold cross-validation. Consequently, we divided the datasets into 40 subjects for training and the remaining ten for validation, in turn. Finally, the algorithms’ performance has been obtained by averaging across all folds.
2.4.1 Performance Metrics
The class “TMD”, which is subjects manifesting temporomandibular disorder, and “CG”, which is subjects belonging to control group, predicted by the aforementioned algorithms were compared to the reference values obtained through the analysis of the clinical assessment. For each classifier, a two-by-two confusion matrix was generated. Subsequently, algorithms performances were evaluated in terms of accuracy, F1-Score and goodness index. Accuracy (A) was calculated as the ratio of correctly predicted risk classes to the total predictions using the following Equation (1):
where TP, TN, FP, and FN denote true positive, true negative, false positive, and false negative, respectively. True positive and true negative were obtained when the algorithm correctly classified subject as "TMD" or "CG" (R), respectively, consistent with the clinical assessment. A value close to 1 indicates a perfect classifier, with 0.80 typically chosen as the threshold for an optimal classifier.
F1-score, a harmonic average of recall (Re) and precision (P), where recall is the ratio of true positive to the sum of true positive and false positive, and precision is the ratio of true positive to the sum of true positive and false positive, was computed as follows (Equation 2):
Similar to accuracy, F1-score ranges from zero to one, with a value close to 1 indicating a perfect classifier and a threshold of 0.80 indicating an optimal classifier. Additionally, the goodness index (G), representing the Euclidean distance in the receiver operating characteristic space between the tested classifier and the perfect one, was computed as follows (Equation 3):
G ranges from 0 to
, with the following goodness ranges: (i) optimum when G ≤ 0.25; (ii) good when 0.25 < G ≤ 0.70; (iii) random if G = 0.70; and (iv) bad if G > 0.70 [
38].
3. Results
The results of the clinical assessments led to the identification of twenty-five participants belonging to the TMD class and the remaining twenty-five to the CG. Specifically, the values gather from the clinical assessment were reported in Table 6.
Table 7.
Values of the scores associated with the clinical assessments for CG (control group) and TMD (temporomandibular disorders), respectively.
Table 7.
Values of the scores associated with the clinical assessments for CG (control group) and TMD (temporomandibular disorders), respectively.
| Parameters |
Related task
|
CG
|
TMD
|
| % of participants manifesting deviation |
MO |
4% |
100% |
| Mean value (SD) (mm) |
OW |
43.4 (2.8) |
35.4 (2.9) |
| % of participants manifesting noise |
JN |
8% |
100% |
| % of participants manifesting muscle pain |
MP |
40% |
100% |
| % of participants manifesting joint pain |
JP |
0% |
100% |
| Median score |
GAD-7 |
6 |
9 |
| Median score |
PHQ-9 |
3 |
8 |
It is clear how the TDM group was associated with a lower averaged value of the mouth opening, as well as to higher scores for both administered questionnaires in comparison of participants belonging to CG. In addition, all the participants belonging to the TDM groups manifested deviation during mouth opening, noise, and pain both at muscle and joint level.
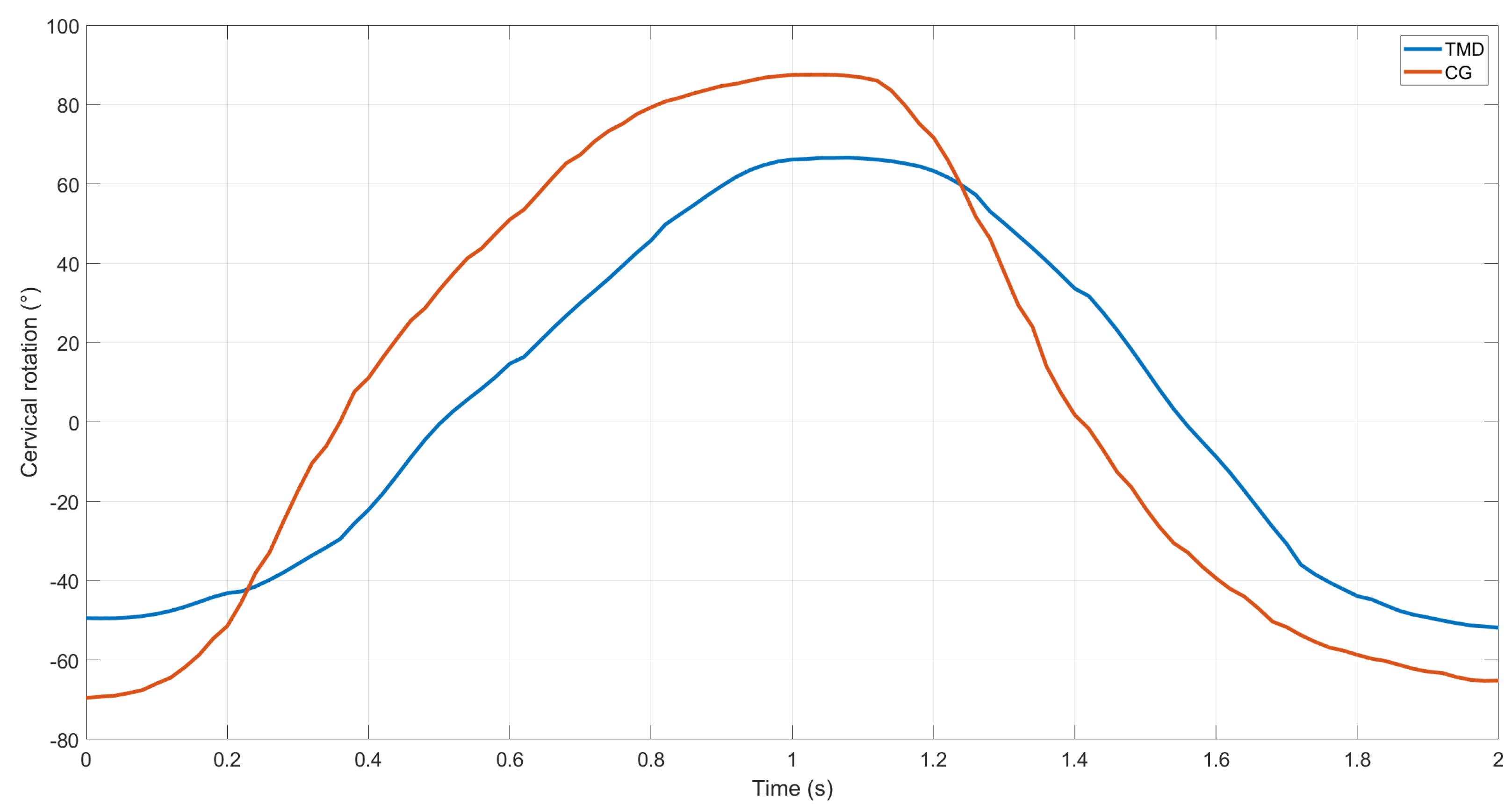
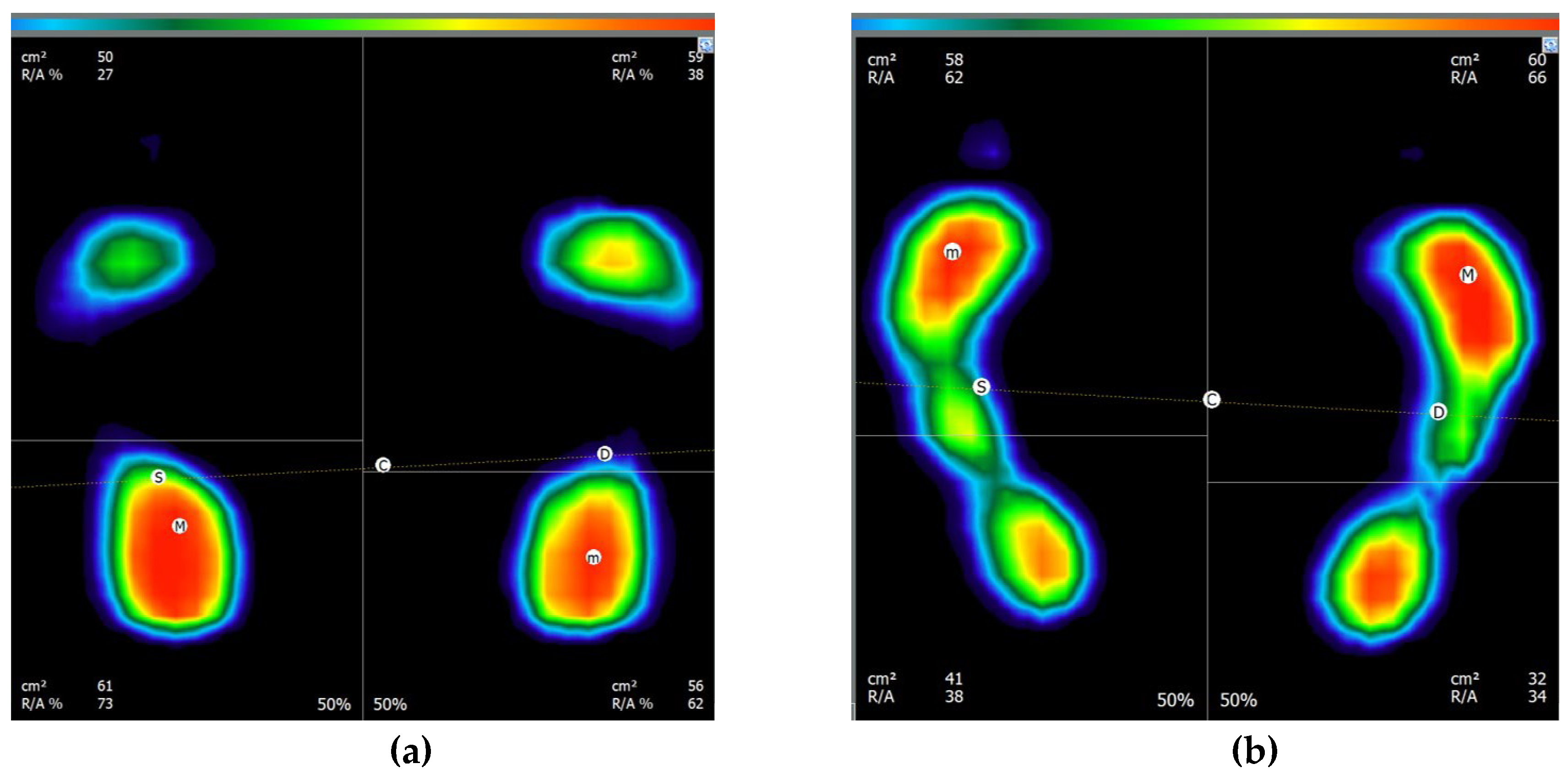
Moving to the instrumented analysis, as an example, the waveform associated with the cervical rotation belonging to either TMD and CG, as well as the graph of the baropodometric analysis, are reported in
Figure 8 and
Figure 9, respectively.
From the above reported example, it is possible to observe how the subject belonging to TMD group was characterized by a lower value of the cervical rotation, both for the right and left direction,
i.e., the positive and negative values, respectively, in comparison of the CG behavior. Similarly, the two subjects are characterized by a different behavior focusing on the baropodometric analysis in terms of load distribution. Specifically, the greater amount of load was distributed on the forefoot for the TMD groups, whereas a greater load on the rearfoot was observed for CG. For sake of clarity,
Table 7 reports the mean values and stand standard deviations for all the computed feature for both groups.
Analyzing the values of the indices gathered from the baropodometric analysis, it is possible to affirm that CG participants tend, in general, to unload the weight more on the rearfoot, whereas the opposite behavior can be observed for TMD. Considering the PA, TMD groups was found to be characterized, in average, by a lower value of the podalic angle. Finally, no qualitative differences can be appreciated for the distribution of the weight between the left and right foot, considering the two groups.
By moving to the cervical mobility, it is evident how TMD group is always associated, in average, with a lower mobility for all the tested movements, with the greatest differences observed for the flexion/extension and left and right rotation.
Table 8 shows the results in terms of accuracy, F1-score and Goodness obtained for all the tested classifiers. By analyzing the results reported in the above table, it has been revealed as the best classifier is the one based on the c-kNN trained with the dataset composed of features gathered from both mobility and baropodometric analysis. In particular, the classifier is associated with an accuracy, F1-score and G-index equal to 0.94, 0.94 and 0.08, respectively. In general, algorithms based on the k-nearest neighbors were found to be associated with the greater performance, regardless the type of feature dataset. In addition, it can be also highlighted how no one of the classifiers trained with the dataset consisting in only baropodometric or mobility analysis achieved sufficient value in all the three parameters to be considered an optimum classifier. Just focusing on MB dataset, all the classifiers were able to overcome the optimal threshold for A and F1-score; however, only three classifiers fell into the optimum range of G-index, which are the three types of kNN.
4. Discussion
This paper proposes an analysis of the possibility to use machine-learning algorithms to support the clinical assessment of temporomandibular disorders. Within this aim, a comparison among nine machine-learning, each one trained with three datasets consisting in features gathered from baropodometric and mobility analysis performed with low-cost and portable sensor system.
By analyzing the general results shown in
Figure 8,
Figure 9 and Table 6, it is obtained qualitative differences associated with the two examined groups both concerning the baropodometric and mobility analysis. These findings suggest the potential use of such parameters as inputs for machine-learning algorithms since it is widely acknowledged that machine-learning algorithms exhibit greater performance when working with classes characterized by different motor patterns [
22].
Focusing on baropodometric analysis, our results confirm the evidence alterations in foot posture and gait mechanics may contribute to the development or exacerbation of TMD symptoms [
39]. As instance, individuals with abnormal foot posture or gait patterns may experience altered biomechanical forces transmitted through the body, potentially affecting the alignment and function of the temporomandibular joint [
40]. Similarly, imbalances in muscle activity or postural control associated with foot dysfunction could indirectly impact the muscles of the jaw [
40]. The different behavior in load distribution can be associated with the pain and discomfort experienced by patients with TMDs, who adjust their body to alleviate musculoskeletal tension and mitigate the pain [
39].
Similarly, the findings of the cervical mobility are in line with the ones already published in literature, where it is affirmed how the upper cervical range of motion is impaired in patient with temporomandibular disorders [
41]. In general, it can be discussed how the patients with TMD are more likely to experience significant cervical hypomobility since the well-known correlation between pain and motor limitations [
42]. The findings of lower mobility may be clarified by the convergence of the noxious stimuli from the neck and masticatory structure into the same neuroanatomical structure, known as the trigeminocervical complex. Consequently, experiencing pain in the masticatory system might influence the mobility and strength of the upper neck through mechanisms of somatic referred pain [
43]. In addition, the greater reduction in mobility observed for the rotation is confirmed in [
44].
Such differences between the two groups is confirmed by the good results achieved by the tested classifiers, especially when considering the ones trained with all the available features, i.e., the MB dataset. By analyzing the results of the performance indices, it can be affirmed how the selection of the model parameters, which are the kernel function for SVM, the distance equation for kNN and the number of splits in DT, seems to be a crucial step only when considering the baropodometric and mobility features separately, whereas no effects are observed when using the MB dataset. Such result is in contrast with the ones reported in previous studies, where the tuning of model parameters is considered fundamental in all applications [
45]. After the selection of the model parameters, by considering all the performance, we can affirm that no classifiers met all the optimal criteria when considering the B dataset, whereas only the c-kNN in case of M dataset. Conversely, all the tested classifiers achieved the optimal performance in case of MB dataset, with the kNN computed using the cosine distance revealing itself as the best performing. In addition to the best performance in terms of accuracy, F1-score and G-index, kNN could be preferred to support vector machine-based algorithms due to the: (i) easy implementation since the kNN is a straightforward algorithm; (ii) greater results interpretability since it is easy to understand how the algorithm arrive at its decision; and (iii) few mandatory operations for the training and parameter tuning [
46]. Furthermore, a geometric classifier, like the c-kNN, is generally more robust to inter-subject variability than decision trees [
47].
In summary, the method proposed here shows promise for integration into clinical assessment of temporomandibular disorders due to its simplicity and cost-effectiveness. Indeed, it requires only basic motor tasks, known to correlate with TMDs, and utilizes a low-cost sensors, which can be also portable to foster the applicability as telemedicine. By employing this protocol as a screening tool, tailored interventions can be devised for patient at early onset of the pathology. Clinicians are encouraged to incorporate this validated protocol and data analysis methodology into clinical assessment since it has been demonstrated as the early diagnosis and management of TMD can greatly improve prognosis and quality of life for patients [
48]. Moreover, this approach can also assess the effectiveness of customized interventions during the monitoring of the pathology to establish the most efficient care pathways. However, it is important to note that the results obtained in this study are specific to the tested cohort. Further research is needed to determine if this methodology can be applied to diverse demographic groups, including variations in age and comorbidities.
5. Conclusions
Aiming to understand if it is possible to use artificial intelligence for supporting the diagnosis of temporomandibular disorders, we compared nine machine-learning algorithms trained with data related to baropodometric analysis and cervical mobility. Data were gathered from 50 adult participants. The results reveal as participant affected by TMDs showed a lower cervical mobility, as well as a different behavior in weight distribution, by preferring to unload the weight on the rearfoot compared with the control group. Such differences were exploited by the machine-learning algorithms, with the one based on k-nearest neighbors with cosine distance found as the best performing both in terms of accuracy, F1-score and Goodness index. The obtained findings allow us to affirm the potentiality of artificial intelligence in providing useful information to be foreseen for the diagnosis of TMDs. Thus, the proposed methodology should be considered in the clinical assessment of the pathology, also considering the portability and low-cost of the used sensor systems.
Author Contributions
Conceptualization, L.M., J.T and V.P.; methodology, L.M., J.T., L.R., and S.R.; software, L.M and J.T.; formal analysis, L.M., L.R. and A.L; data curation, L.M. and J.T.; writing—original draft preparation, L.M., J.T., L.R. and V.P.; writing—review and editing, L.M., J.T., L.R. and S.R.; supervision, J.T., A.L. and S.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the Ovidius University of Constanta (Romania) with the protocol n. 45 in date 23.01.2024.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
For data availability, please refer to the corresponding authors.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Romero-Reyes, M.; Uyanik, J.M. Orofacial Pain Management: Current Perspectives. J Pain Res 2014, 99. [Google Scholar] [CrossRef] [PubMed]
- Ohrbach, R.; Dworkin, S.F. The Evolution of TMD Diagnosis. J Dent Res 2016, 95, 1093–1101. [Google Scholar] [CrossRef] [PubMed]
- Mogil, J.S. Pain Genetics: Past, Present and Future. Trends in Genetics 2012, 28, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Greenbaum, T.; Dvir, Z.; Reiter, S.; Winocur, E. Cervical Flexion-Rotation Test and Physiological Range of Motion – A Comparative Study of Patients with Myogenic Temporomandibular Disorder versus Healthy Subjects. Musculoskelet Sci Pract 2017, 27, 7–13. [Google Scholar] [CrossRef] [PubMed]
- LIST, T.; AXELSSON, S. Management of TMD: Evidence from Systematic Reviews and Meta-Analyses. J Oral Rehabil 2010, 37, 430–451. [Google Scholar] [CrossRef] [PubMed]
- Suenaga, S.; Nagayama, K.; Nagasawa, T.; Indo, H.; Majima, H.J. The Usefulness of Diagnostic Imaging for the Assessment of Pain Symptoms in Temporomandibular Disorders. Japanese Dental Science Review 2016, 52, 93–106. [Google Scholar] [CrossRef]
- Robinson de Senna, B.; Kelma dos Santos Silva, V.; Petruceli Franca, J.; Silva Marques, L.; Pereira, L.J. Imaging Diagnosis of the Temporomandibular Joint: Critical Review of Indications and New Perspectives. Oral Radiol 2006, 25, 8698. [Google Scholar]
- Ohrbach, R.; Dworkin, S.F. The Evolution of TMD Diagnosis. J Dent Res 2016, 95, 1093–1101. [Google Scholar] [CrossRef]
- Schiffman, E.; Ohrbach, R. Executive Summary of the Diagnostic Criteria for Temporomandibular Disorders for Clinical and Research Applications. The Journal of the American Dental Association 2016, 147, 438–445. [Google Scholar] [CrossRef]
- Steenks, M.; Türp, J.; de Wijer, A. Reliability and Validity of the Diagnostic Criteria for Temporomandibular Disorders Axis I in Clinical and Research Settings: A Critical Appraisal. J Oral Facial Pain Headache 2018, 32, 7–18. [Google Scholar] [CrossRef]
- Steenks, M.H.; Turp, J.C.; Habil, M.D.; Anton de Wijer, R.P.T.; Steenks, M.H. Reliability and Validity of the DC/TMD Axis I. J Oral Facial Pain Headache 2018, 32, 27–28. [Google Scholar] [CrossRef] [PubMed]
- Walczyńska-Dragon, K.; Baron, S.; Nitecka-Buchta, A.; Tkacz, E. Correlation between TMD and Cervical Spine Pain and Mobility: Is the Whole Body Balance TMJ Related? Biomed Res Int 2014, 2014, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Grondin, F.; Hall, T.; Laurentjoye, M.; Ella, B. Upper Cervical Range of Motion Is Impaired in Patients with Temporomandibular Disorders. CRANIO® 2015, 33, 91–99. [Google Scholar] [CrossRef]
- Nota, A.; Tecco, S.; Ehsani, S.; Padulo, J.; Baldini, A. Postural Stability in Subjects with Temporomandibular Disorders and Healthy Controls: A Comparative Assessment. Journal of Electromyography and Kinesiology 2017, 37, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Souza, J.A.; Pasinato, F.; Corrêa, E.C.R.; da Silva, A.M.T. Global Body Posture and Plantar Pressure Distribution in Individuals With and Without Temporomandibular Disorder: A Preliminary Study. J Manipulative Physiol Ther 2014, 37, 407–414. [Google Scholar] [CrossRef]
- Scharnweber, B.; Adjami, F.; Schuster, G.; Kopp, S.; Natrup, J.; Erbe, C.; Ohlendorf, D. Influence of Dental Occlusion on Postural Control and Plantar Pressure Distribution. CRANIO® 2017, 35, 358–366. [Google Scholar] [CrossRef]
- Cuenca-Martínez, F.; Herranz-Gómez, A.; Madroñero-Miguel, B.; Reina-Varona, Á.; La Touche, R.; Angulo-Díaz-Parreño, S.; Pardo-Montero, J.; del Corral, T.; López-de-Uralde-Villanueva, I. Craniocervical and Cervical Spine Features of Patients with Temporomandibular Disorders: A Systematic Review and Meta-Analysis of Observational Studies. J Clin Med 2020, 9, 2806. [Google Scholar] [CrossRef]
- Rocha, C.P.; Croci, C.S.; Caria, P.H.F. Is There Relationship between Temporomandibular Disorders and Head and Cervical Posture? A Systematic Review. J Oral Rehabil 2013, 40, 875–881. [Google Scholar] [CrossRef]
- Sambataro, S.; Cervino, G.; Bocchieri, S.; La Bruna, R.; Cicciù, M. TMJ Dysfunctions Systemic Implications and Postural Assessments: A Review of Recent Literature. J Funct Morphol Kinesiol 2019, 4, 58. [Google Scholar] [CrossRef]
- Claudino, J.G.; Capanema, D. de O.; de Souza, T.V.; Serrão, J.C.; Machado Pereira, A.C.; Nassis, G.P. Current Approaches to the Use of Artificial Intelligence for Injury Risk Assessment and Performance Prediction in Team Sports: A Systematic Review. Sports Med Open 2019, 5, 28. [Google Scholar] [CrossRef]
- Chidambaram, S.; Maheswaran, Y.; Patel, K.; Sounderajah, V.; Hashimoto, D.A.; Seastedt, K.P.; McGregor, A.H.; Markar, S.R.; Darzi, A. Using Artificial Intelligence-Enhanced Sensing and Wearable Technology in Sports Medicine and Performance Optimisation. Sensors 2022, 22, 6920. [Google Scholar] [CrossRef] [PubMed]
- Taborri, J.; Molinaro, L.; Santospagnuolo, A.; Vetrano, M.; Vulpiani, M.C.; Rossi, S. A Machine-Learning Approach to Measure the Anterior Cruciate Ligament Injury Risk in Female Basketball Players. Sensors 2021, 21, 3141. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-S.; Jha, N.; Kim, Y.-J. Risk Factor Assessments of Temporomandibular Disorders via Machine Learning. Sci Rep 2021, 11. [Google Scholar] [CrossRef] [PubMed]
- Małgorzata, P.; Małgorzata, K.-M.; Karolina, C.; Gala, A. Diagnostic of Temporomandibular Disorders and Other Facial Pain Conditions—Narrative Review and Personal Experience. Medicina (B Aires) 2020, 56, 472. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Dworkin, S.F.; Sherman, J.; Mancl, L.; Ohrbach, R.; LeResche, L.; Truelove, E. Reliability, Validity, and Clinical Utility of the Research Diagnostic Criteria for Temporomandibular Disorders Axis II Scales: Depression, Non-Specific Physical Symptoms, and Graded Chronic Pain. J Orofac Pain 2002, 16, 207–220. [Google Scholar] [PubMed]
- Kroenke, K.; Wu, J.; Yu, Z.; Bair, M.J.; Kean, J.; Stump, T.; Monahan, P.O. Patient Health Questionnaire Anxiety and Depression Scale: Initial Validation in Three Clinical Trials. Psychosom Med 2016, 78, 716–727. [Google Scholar] [CrossRef] [PubMed]
- Hawrylak, A.; Brzeźna, A.; Chromik, K. Distribution of Plantar Pressure in Soccer Players. Int J Environ Res Public Health 2021, 18, 4173. [Google Scholar] [CrossRef] [PubMed]
- Matla, J.; Filar-Mierzwa, K.; Ścisłowska-Czarnecka, A.; Jankowicz-Szymańska, A.; Bac, A. The Influence of the Physiotherapeutic Program on Selected Static and Dynamic Foot Indicators and the Balance of Elderly Women Depending on the Ground Stability. Int J Environ Res Public Health 2021, 18, 4660. [Google Scholar] [CrossRef]
- Molinaro, L.; Taborri, J.; Pauletto, D.; Guerra, V.; Molinaro, D.; Sicari, G.; Regina, A.; Guerra, E.; Rossi, S. Measuring the Immediate Effects of High-Intensity Functional Training on Motor, Cognitive and Physiological Parameters in Well-Trained Adults. Sensors 2023, 23, 3937. [Google Scholar] [CrossRef]
- Molinaro, L.; Taborri, J.; Rossi, S. Baropodometric Analysis in Different Feet Positions: Reliability and Repeatability Evaluation. In Proceedings of the 2021 IEEE International Workshop on Metrology for Industry 4.0 & IoT (MetroInd4.0&IoT); IEEE, June 7 2021; pp. 295–300. [Google Scholar]
- Russo, L.; Panessa, T.; Bartolucci, P.; Raggi, A.; Migliaccio, G.M.; Larion, A.; Padulo, J. Elastic Taping Application on the Neck: Immediate and Short-Term Impacts on Pain and Mobility of Cervical Spine. J Funct Morphol Kinesiol 2023, 8, 156. [Google Scholar] [CrossRef] [PubMed]
- Ohrbach, R.; Gonzalez, Y.; List, T.; Michelotti, A.; Shiffman, E. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) Clinical Examination Protocol; Available online at: www. rdc-tmdinternational. org, 2014. [Google Scholar]
- Mahony, R.; Hamel, T.; Pflimin, J.-M. Non-Linear Complementary Filters on the Special Orthogonal Group. IEEE Transactions on Automatic Control, Institute of Electrical and Electronics Engineers 2008, 53, 1203–1217. [Google Scholar] [CrossRef]
- Preece, S.J.; Paul, L.; Kenney, J.; Meijer, K.; Crompton, R.H.; Goulermas, J.Y.; Kenney, L.P.J.; Howard, D.; Crompton, R. Activity Identification Using Body-Mounted Sensors-A Review of Classification Techniques. Physiol. Meas 2009, 30, 1–33. [Google Scholar] [CrossRef] [PubMed]
- Hearst, M.A.; Dumais, S.T.; Osuna, E.; Platt, J.; Scholkopf, B. Support Vector Machines. IEEE Intelligent Systems and their Applications 1998, 13, 18–28. [Google Scholar] [CrossRef]
- Altman, N.S. An Introduction to Kernel and Nearest-Neighbor Nonparametric Regression. Am Stat 1992, 46, 175–185. [Google Scholar] [CrossRef]
- Taborri, J.; Scalona, E.; Palermo, E.; Rossi, S.; Cappa, P. Validation of Inter-Subject Training for Hidden Markov Models Applied to Gait Phase Detection in Children with Cerebral Palsy. Sensors (Switzerland) 2015, 15. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.B.B.; Araujo, C.C. de; Antonio, T.T. Del; Folster, N.M.; Silva, J.K.M. Da Prevalence of Temporomandibular Disorder and Its Relation with Plantar Pressures in University Students of Health-Related Courses. Manual Therapy, Posturology & Rehabilitation Journal, 2020; 1–15. [Google Scholar] [CrossRef]
- Souza, J.A.; Pasinato, F.; Corrêa, E.C.R.; da Silva, A.M.T. Global Body Posture and Plantar Pressure Distribution in Individuals With and Without Temporomandibular Disorder: A Preliminary Study. J Manipulative Physiol Ther 2014, 37, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Grondin, F.; Hall, T.; Laurentjoye, M.; Ella, B. Upper Cervical Range of Motion Is Impaired in Patients with Temporomandibular Disorders. CRANIO® 2015, 33, 91–99. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, S.; Falla, D.; Elliott, J.M.; Jull, G. Muscle Dysfunction in Cervical Spine Pain: Implications for Assessment and Management. Journal of Orthopaedic & Sports Physical Therapy 2009, 39, 324–333. [Google Scholar] [CrossRef]
- Haldeman, S.; Dagenais, S. Cervicogenic Headaches. The Spine Journal 2001, 1, 31–46. [Google Scholar] [CrossRef]
- Amaral, F.A.; Dall’Agnol, S.M.; Socolovski, G.; Kich, C.; Franco, G.C.N.; Bortoluzzi, M.C. Cervical Spine Range of Motion, Posture and Electromyographic Activity of Masticatory Muscles in Temporomandibular Disorders. Fisioterapia em Movimento 2020, 33. [Google Scholar] [CrossRef]
- Tjärnberg, A.; Mahmood, O.; Jackson, C.; Saldi, G.-A.; Cho, K.; Christiaen, L.; Bonneau, R. Optimal Tuning of Weighted KNN- and Diffusion-Based Methods for Denoising Single Cell Genomics Data. 2020. [CrossRef]
- Taunk, K.; De, S.; Verma, S.; Swetapadma, A. A Brief Review of Nearest Neighbor Algorithm for Learning and Classification. In Proceedings of the 2019 International Conference on Intelligent Computing and Control Systems (ICCS); IEEE, May 2019; pp. 1255–1260. [Google Scholar]
- Mannini, A.; Sabatini, A.M. Machine Learning Methods for Classifying Human Physical Activity from On-Body Accelerometers. Sensors 2010, 10, 1154–1175. [Google Scholar] [CrossRef] [PubMed]
- Palmer, J.; Durham, J. Temporomandibular Disorders. BJA Educ 2021, 21, 44–50. [Google Scholar] [CrossRef] [PubMed]
Figure 1.
a) Straight opening; (b) lateral deviation; (c) correct deviation; (d) Other.
Figure 1.
a) Straight opening; (b) lateral deviation; (c) correct deviation; (d) Other.
Figure 2.
Figure 2. Measuring the width of the opening.
Figure 2.
Figure 2. Measuring the width of the opening.
Figure 3.
Muscle palpation; in the upper the palpation of the temporal muscle, in the lower the masseter one.
Figure 3.
Muscle palpation; in the upper the palpation of the temporal muscle, in the lower the masseter one.
Figure 4.
Joint palpation.
Figure 4.
Joint palpation.
Figure 5.
Baropodometric setup.
Figure 5.
Baropodometric setup.
Figure 6.
Cervical mobility with Moover sensor. a) Flexion-extension of the head; b) Head rotation; c) Head inclination.
Figure 6.
Cervical mobility with Moover sensor. a) Flexion-extension of the head; b) Head rotation; c) Head inclination.
Figure 7.
a) Representation of static test and the division of the forefoot and rearfoot; b) Calculation of the podalic angle.
Figure 7.
a) Representation of static test and the division of the forefoot and rearfoot; b) Calculation of the podalic angle.
Figure 8.
Example of left cervical rotation, expressed in degree, of a single repetition for CG (red line) and TMD (blue line).
Figure 8.
Example of left cervical rotation, expressed in degree, of a single repetition for CG (red line) and TMD (blue line).
Figure 9.
Example of baropodometric result for CG (figure a) and TMD (figure b). Color scale represents the amount of load, with greater load associated with red color.
Figure 9.
Example of baropodometric result for CG (figure a) and TMD (figure b). Color scale represents the amount of load, with greater load associated with red color.
Table 1.
Mouth opening classification.
Table 1.
Mouth opening classification.
| Classification |
No |
Yes |
| 1 |
Straight (S) |
0 |
1 |
| 2 |
Lateral deviation to the right (RDEV) or to the left (LDEV) |
0 |
1 |
| 3 |
Corrected deviation (CDEV) |
0 |
1 |
| 4 |
Other (O) |
0 |
1 |
Table 2.
Joint noises classification.
Table 2.
Joint noises classification.
| Classification |
Value |
| No noise |
0 |
| Click |
1 |
| Crepitus |
2 |
Table 3.
Muscle palpation and Joint palpation classification.
Table 3.
Muscle palpation and Joint palpation classification.
| Classification |
Pain |
| No |
Yes |
| Temporal Muscle |
0 |
1 |
| Massetere Muscle |
0 |
1 |
| Temporomandibular Joint |
0 |
1 |
Table 4.
PHQ-9 questionnaire.
Table 4.
PHQ-9 questionnaire.
| Over the last 2 weeks, on how many days have you been bothered by any of the following problems? |
Not at all |
Several days |
More than half the days |
Nearly every day |
| 1 |
Little interest or pleasure in doing things |
0 |
1 |
2 |
3 |
| 2 |
Feeling down, depressed or hopeless |
0 |
1 |
2 |
3 |
| 3 |
Trouble falling or staying asleep, or sleeping too much |
0 |
1 |
2 |
3 |
| 4 |
Feeling tired or having little energy |
0 |
1 |
2 |
3 |
| 5 |
Poor appetite or overeating |
0 |
1 |
2 |
3 |
| 6 |
Feeling bad about yourself – or that you are a failure or have let yourself or your family down |
0 |
1 |
2 |
3 |
| 7 |
Trouble concentrating on things, such as reading the newspaper or watching television |
0 |
1 |
2 |
3 |
| 8 |
Moving or speaking so slowly that other people could have noticed, or the opposite – being so fidgety or restless that you have been moving around a lot more than usual |
0 |
1 |
2 |
3 |
| 9 |
Thoughts that you would be better off dead or of hurting yourself in some way |
0 |
1 |
2 |
3 |
Table 5.
GAD-7 questionnaire.
Table 5.
GAD-7 questionnaire.
| Over the last 2 weeks, on how many days have you been bothered by any of the following problems? |
Not at all |
Several days |
More than half the days |
Nearly every day |
| 1 |
Feeling nervous, anxious or on edge |
0 |
1 |
2 |
3 |
| 2 |
Not being able to stop or control worrying |
0 |
1 |
2 |
3 |
| 3 |
Worring too much about different things |
0 |
1 |
2 |
3 |
| 4 |
Trouble relaxing |
0 |
1 |
2 |
3 |
| 5 |
Being so restless it is hard to sit still |
0 |
1 |
2 |
3 |
| 6 |
Becoming easily annoyed or irritable |
0 |
1 |
2 |
3 |
| 7 |
Feeling afraid as if something awful might happen |
0 |
1 |
2 |
3 |
Table 7.
Mean (standard deviation) of the computed features for the two tested groups, CG (control group) and TMD (temporomandibular disorders), respectively.
Table 7.
Mean (standard deviation) of the computed features for the two tested groups, CG (control group) and TMD (temporomandibular disorders), respectively.
| Task |
|
Features |
CG
|
TMD
|
| Baropodometric analysis |
Right foot |
PA (°) |
7.5 (1.0) |
6.0 (0.8) |
| FL (%) |
19.8 (1.2) |
28.5 (1.1) |
| RL (%) |
31.0 (2.2) |
26.2 (1.0) |
| TL (%) |
52.0 (1.2) |
54.4 (1.3) |
Left
foot |
PA (°) |
5.4 (0.8) |
4.4 (1.1) |
| FL (%) |
19.8 (0.7) |
24.6 (1.1) |
| RL (%) |
29.4 (1.4) |
21.4 (1.2) |
| TL (%) |
48.0 (1.1) |
45.6 (1.2) |
| Cervical mobility |
θFLEX (°) |
55.9 (4.2) |
53.8 (2.2) |
|
θEXT (°) |
60.9 (2.9) |
52.2 (4.4) |
|
θFLEX+EXT (°) |
116.8 (4.4) |
106.0 (3.6) |
|
θR_ROT (°) |
72.5 (4.3) |
67.1 (2.6) |
|
θL_ROT (°) |
75.3 (3.9) |
70.7 (3.3) |
|
θTOT_ROT (°) |
147.7 (4.4) |
137.8 (2.2) |
|
θR_INC (°) |
43.4 (3.2) |
40.5 (3.3) |
|
θL_INC (°) |
40.1 (2.3) |
40.4 (4.9) |
|
θTOT_INC (°) |
83.5 (3.3) |
80.5 (3.3) |
Table 8.
Accuracy (A), F1-score (F1) and goodness index (G) achieved by the nine tested classifiers in the three datasets, where B stands for features related to only baropodometric analysis, M stands for only mobility parameters, whereas MB refer to all the features used together.
Table 8.
Accuracy (A), F1-score (F1) and goodness index (G) achieved by the nine tested classifiers in the three datasets, where B stands for features related to only baropodometric analysis, M stands for only mobility parameters, whereas MB refer to all the features used together.
| Classifiers |
B |
M |
MB |
| A |
F1 |
G |
A |
F1 |
G |
A |
F1 |
G |
| l-SVM |
0.65 |
0.76 |
0.29 |
0.75 |
0.77 |
0.27 |
0.84 |
0.80 |
0.23 |
| q-SVM |
0.77 |
0.77 |
0.31 |
0.78 |
0.81 |
0.26 |
0.83 |
0.84 |
0.22 |
| c-SVM |
0.69 |
0.71 |
0.30 |
0.79 |
0.82 |
0.26 |
0.80 |
0.84 |
0.23 |
| f-kNN |
0.73 |
0.79 |
0.29 |
0.79 |
0.81 |
0.28 |
0.91 |
0.93 |
0.11 |
| c-kNN |
0.74 |
0.72 |
0.33 |
0.82 |
0.83 |
0.22 |
0.94 |
0.94 |
0.08 |
| w-kNN |
0.72 |
0.71 |
0.32 |
0.75 |
0.77 |
0.33 |
0.93 |
0.92 |
0.10 |
| c-DT |
0.66 |
0.69 |
0.45 |
0.71 |
0.72 |
0.30 |
0.84 |
0.80 |
0.24 |
| m-DT |
0.65 |
0.65 |
0.44 |
0.74 |
0.75 |
0.32 |
0.82 |
0.83 |
0.23 |
| cx-DT |
0.70 |
0.77 |
0.34 |
0.79 |
0.80 |
0.26 |
0.86 |
0.82 |
0.23 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).