1. Introduction
The American Hospital Association defines sustainability in healthcare, sas “the integration of environmental stewardship, social equity and fiduciary responsibility to support healthy, equitable and resilient environments and communities over time” [
https://www.aha.org/sustainability] Despite unprecedented investments in healthcare, lack of capacity and timeliness are still problems affecting every country, even the wealthier ones [Gustavo et. al. 2022]. Leadership in many countries holds the opinion that a lockdown (full or partial) is the only way to prevent the collapse of the healthcare system during conditions of drastic increases in Covid19 pathology. The argument states that such an event will flood hospitals with patient volumes that they will not be able to handle. Indeed, in some countries, the lockdown was the case: China, India, Brazil, Spain, Italy, parts of the U.S., and others.
This paper presents a resource-based approach to the problem using the Theory-of-Constraints (TOC). The TOC’s focus on effective and efficient resource utilization goes hand in hand with the objective to reduce the hospital’s ecological footprint.
Section 2 presents the Theory-of-Constraints and its application in healthcare management.
Section 3 defines three potential hospital load scenarios; section 4 presents a case that will accompany the application of the various scenarios;
Section 5 presents the evolutionary methodologies to cope with these scenarios; section 6 presents the disruptive (revolutionary) methodology; section 7 concludes the analysis and provides effective tools for the management of future pandemics and suggestions for future research. This paper presents an innovative sustainable managerial methodology in health crisis management.
2. Theory-of-Constraints and Its Application in Healthcare Management
TOC is a managerial approach developed by Goldratt [Goldratt and Cox, 1988] that was applied successfully in hundreds of organizations, many of which in healthcare systems, leading to rapid and significant results. TOC was conceived in manufacturing settings and from there it moved to project management [Goldratt, 1997] and to service organizations. In the last twenty years, TOC has been applied in complex healthcare systems around the world [Ronen et. al., 2018; Cox and Schleier, 2010; Ikeziri et. al., 2019; Groop et. al. 2017; Rodriguez et. al., 2022; Stratton and Knight, 2010; Stratton and West, 2014]. TOC focuses the organization’s attention on the few resources – Bottlenecks - that prevent the organization from reaching its goal. Gustavo et. al., 2022 analyzed 42 TOC implementations (15 full-text articles, 12 video proceedings, and 2 theses/dissertations) from major scientific electronic databases and TOC International Certification Organization Conferences. All implementations reported positive outcomes, both tangible and intangible. The two main improvements reported by the authors were productivity (98%; n = 41) – more patients treated – and the timeliness of care (83%; n = 35). Furthermore, the selected studies reported dramatic improvements: 50% reductions in mean patient waiting times; 38% reduction in patient length of stay; 43% mean increase in operating room productivity and 34% mean increase in throughput. TOC implementations attained positive results at all levels of the health and social care chain. Most TOC recommendations and changes showed almost immediate results and required little or no additional costs to implement. Evidence supports TOC as a promising solution for the chronic healthcare problem, improving quality and timeliness, both necessary conditions for providing effective healthcare. One of TOC’s most effective tools is hereby presented in the “Seven focusing steps”. Orderly application of these seven steps results in significant improvement in throughput and in lead-time reduction while at the same time improving clinical and service qualities. TOC’s seven steps are based on Operations Research tools such as Linear Programming [Ronen and Starr, 1990]. TOC was adapted to healthcare management as outlined hereby. TOC methodology uses the Satisficer approach as it produces sufficiently acceptable solutions that result in significant improvement of the organization’s performance and are achieved in a relatively short time span. Gustavo et. al. [2022] and Mabin et. al. [2018] and Mabin and Balderstone [2003] provide more successful application of TOC in healthcare.
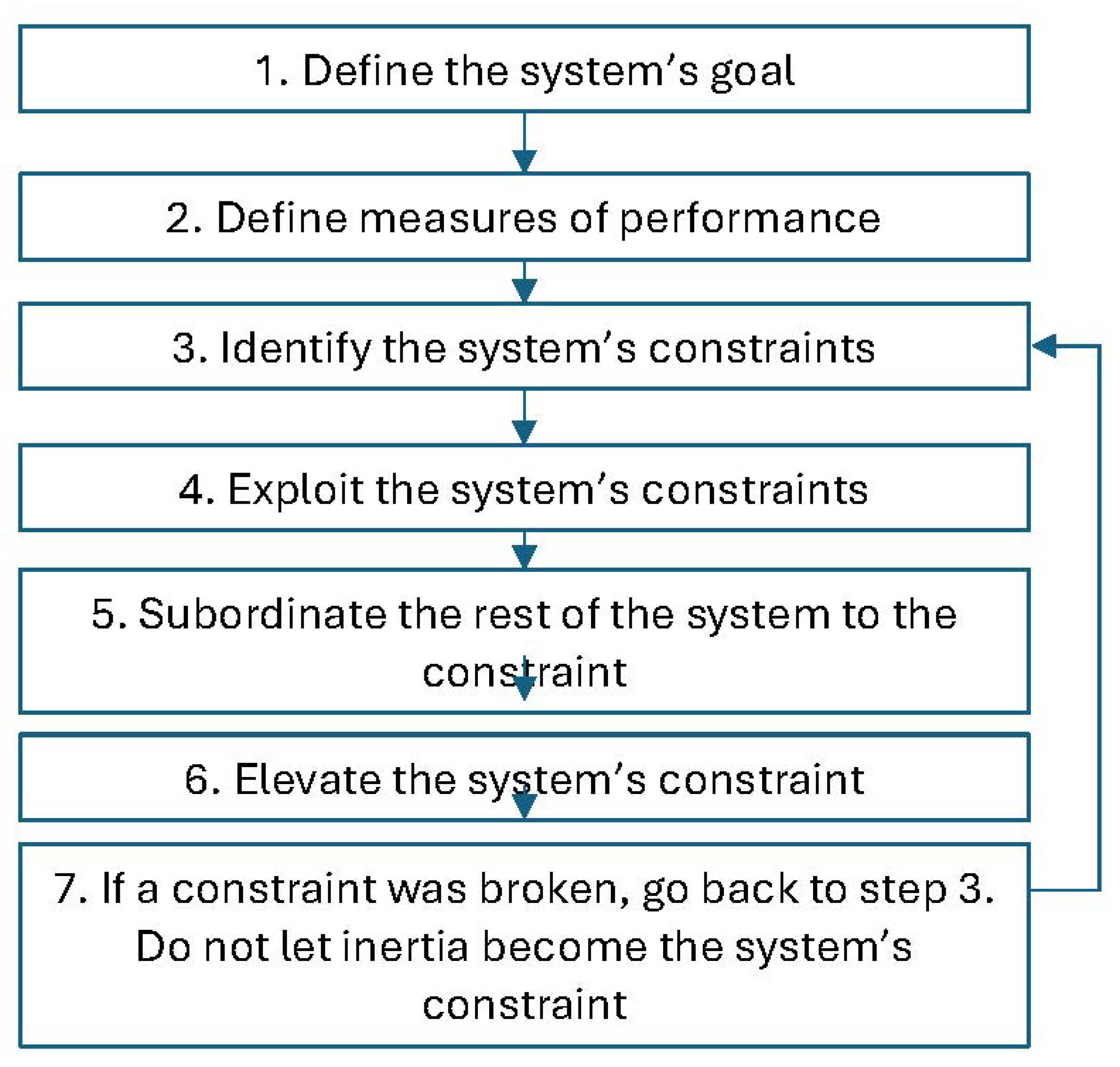
The Seven focusing steps
The seven steps of TOC’s application in healthcare are (
Figure 1):
Define the system’s goal(s): when defining the system’s goal, one must identify the system being analyzed. In the case of the Covid19 pandemic, we analyze the national healthcare system and its economic arena. Thus, the goals are to treat Covid19 patients best as possible, prevent contamination, and provide continuous treatment to the whole patient population, while monitoring the cost to the economy. During crises, there is a tendency to skip the definition of the goal, as it seems obvious, and to move straight to problem solutions. Defining the Goal is of great importance, particularly in not-for-profit organizations.
Define measures of performance: a system behaves according to its Key Performance Indicators (KPIs). The following KPIs should be focal when confronting the Covid19 pandemic:
Number of Covid19 patients;
Number of new Covid19 patients during the measurement period;
Average number of Covid19 patients infected by each Covid19 patient (Ro);
Number of relevant medical teams (defined later);
Number of carriers identified by tests;
Covid19 death toll;
Amount of waste generated by the system;
Increase in Carbon emissions.
Lead time measures: time from contamination to identification; and from identification to patient release;
Number of patients on ventilators.
The role of the KPIs is to help decision-making by providing decision-makers with feedback to identify successes and failures in system management. In most cases, the system must compete versus itself and perform continuous improvement in a Satisficer approach by setting challenging, achievable objectives. The common approach of setting challenging benchmarks derived from other countries or organizations does not lead to the coveted result. Setting objectives should take into account the system’s condition on one hand and the medical requirements on the other.
- 3.
Identify the system’s constraints: a constraint is defined as a resource in shortage preventing the system from achieving a better performance level relative to the goal [
6].
A process flow chart of the system should be drawn [Ronen et. al. p. 48, 2018] to better analyze and understand the patient treatment flow.
There are four constraint types:
Resource constraint – Bottleneck. A resource constraint is the most loaded resource so that it cannot perform all tasks assigned to it. This is the resource that constrains the performance of the whole system. The bottleneck is usually the most expensive and scarce resource. During “peaceful times” habitually, the bottlenecks in surgery are anesthetists, and in Emergency Departments (EDs) ED experts are the bottleneck. In imaging institutions, we often identify the constraint as the MRI machines or imaging analysts. During “War times”, as is the case today as we fight Covid19, internal medicine experts, anesthetists, intensive care (ICU) nurses and ED surgeons (hereby defined as medical teams) constitute the system’s bottleneck. The number of medical teams keeps shrinking due to the contamination of medical teams by the virus and the need for quarantine. Other resources must not become bottlenecks: test kits, laboratories, ventilators, and personal protective equipment. It is highly probable that in future crises, medical teams will likewise constitute the system’s bottleneck.
Market constraint (excess capacity). A market constraint occurs when the system has extra capacity and is capable of treating additional patients.
Dummy constraint. A dummy constraint is a case when the system’s bottleneck is an extremely inexpensive resource relative to the other resources in the system. This is a situation where the system’s capacity is constrained by a resource of negligible cost. For example, shortage in janitors or operating room patient transporters, or a shortage in Covid19 testing swabs. Shortages in testing kits and personal protection equipment are defined as dummy constraints since they are relatively inexpensive resources that are meant to be in excess. Dummy constraints must be resolved in haste.
Policy constraint. A policy constraint is the adoption of an inappropriate policy constraining the system’s performance and achievement of the goal, and at times operates dramatically against the organization’s goals. This is a situation where inappropriate policy is the system constraint. Policy, as a rule, is a positive element, every organization must set policies on a range of important issues. However, a policy that was excellent in the past (as well as in “peaceful times”), may become a policy constraint once environmental changes occur (“War times”). The Covid19 system is afflicted by multiple policy constraints. Most policy constraints emanate from the application of a uniform policy in all conditions and from inappropriate KPIs. For example, applying the “number of tests performed” as a performance indicator will result in a loss of focus on the test targets, which are to perform sampling testing on one hand, and identifying virus carriers on the other. This is therefore not a measure that should not be maximized or minimized. The “number of tests” is a measure of input rather than a measure of the system’s output. Appropriate throughput measures are the number of new patients and the number of severely ill patients. Another policy constraint is failure to test all suspected patients and failure to train enough teams and labs to perform tests. Labs must work three shifts per day, if required, to establish protective capacity. Protective capacity takes into account fluctuations in the process. These are disturbances, mishaps, and uncertainty hindering performance. An excellent example of a policy constraint is the Ministry of Health’s insistence to perform all tests in the ministry’s labs rather than using dozens of other labs. At many hospitals around the world, ventilators are a bottleneck, and efforts are made to increase their quantity.
It is of utmost importance to identify the constraints of complex health systems on the one hand and where the constraint should be, on the other. Focusing on the bottleneck of complex systems frees managerial attention to important issues and the promotion of the goal.
- 4.
-
Exploit the system’s constraint: once a bottleneck is identified it should be exploited in two modes:
“Medical teams” are a bottleneck, and they are the expensive resource that management attention should be dedicated to. To achieve healthcare effectiveness, two treatment entities must be established: one for Covid19 patients hospitalized in separate wards and the other for the rest of the routine patients. A minimal number of bottleneck physicians will be dedicated to serious Covid19 cases. Most medical teams would be assigned to the treatment of “regular” patients. To ascertain that the bottleneck functions with efficiency and safety, a demonstrated procedure is to prevent staff from one shift from overlapping with other shifts. To minimize exposure, physicians will be selected from the hospital’s regular staff and will support Covid19 departments as consultants, as is the practice with the ICU or the ED. Only a small percentage of Covid19 patients require the attention of a physician, and most of them require a nurse or paramedic trained to treat them. Since medical teams are susceptible to Covid19 infection, particular attention should be devoted to their protection through routine tests and protective gear. It is imperative that medical teams do not deteriorate to fatigue or exhaustion. Shortage of people and testing swabs is a “policy constraint”. It happens in complex health systems where the focus is lost in an attempt to simultaneously maximize utilization of all resources. We advise creating excess (protective redundancy) of all resources and striving to reach a situation of a single bottleneck – physicians, which can be managed effectively and safely.
- 5.
-
Subordinate the rest of the system to the constraint (the bottleneck): all non-bottleneck resources (other physicians, nurses, physician assistants, technicians, paramedics, logistic decisions, patient prioritization, etc.) are subordinated to the medical teams. The “Covid19 wards” will be subordinated to the hospital’s routine management. In case of conflict, treatment should be prioritized according to the medical condition and bottleneck availability. Subordination should be performed according to the Pareto methodology. Many are familiar with the Pareto rule (the 20/80 principle) and the Pareto methodology is a practical extension of this rule [
6]:
Classification
Differentiation
Resource allocation.
Classification will break patients into two groups:
High-risk Covid19 patients, and elderly, non-Covid19 patients with background afflictions. These patients constitute around 10% of the Covid19 population and consume 90% of the bottleneck resources. This population includes patients in geographic regions with high local contamination rates; and –
Low-risk patients who constitute 90% of the Covid19 patients and consume merely 10% of bottleneck resources.
The significance of the differentiation is in forming a different treatment policy for each group. Group A will be treated by expert internal medicine doctors, anesthetists, and ICU physicians. Group B will be treated mainly by non-bottleneck doctors and nurses.
- 6.
-
Elevate the system’s constraint: offloading implies the creation of additional medical resources by transferring some of the bottleneck tasks to other resources:
Define “Covid19 supporters” who are not bottlenecks: medical assistants, paramedics, military medical teams, and medical students;
Transfer medical tasks from hospital physicians to ”Covid19 supporters”;
Prepare for home quarantine of Covid19 patients through telemedicine, and self-test kits.
Transfer those exposed to patients to home quarantine.
Train non-Covid19 professional physicians to perform some “medical team” duties.
The Offload mechanism encapsulates significant potential to elevate bottleneck resources. The application of remote monitoring reduces the burden on hospitals. Patients receive equipment that reports their medical status via the web and they are treated remotely as long as their condition is sound. Experience shows that during “peaceful times”, offloading physician duties to nurses constitutes a win/win solution for both: decreasing the burden on doctors and professional empowerment to nurses.
The offloading mechanism must also be applied in decisions pertaining to the purchase of critical equipment. Simple, available equipment can be used for light patients, thus freeing sophisticated equipment for patients requiring it.
The offloading mechanism should also be applied in decision-making processes. During the current crisis, most decisions were made by excessively senior ranks, both in “peaceful times” and “war times”. For example, exit from lockdown characterization was determined by the Covid19 regulator. Decision makers should delegate authority to lower professional cadres. Otherwise, the decision-making process itself will become the bottleneck paralyzing the whole system.
- 7.
If the constraint is broken, return to step 3: identifying the new constraint, do not let inertia become the next constraint: once medical teams cease being bottlenecks, there is a new resource that takes their place. In the Covid19 crisis, we have observed a decline in the number of afflicted, thus turning bottlenecks (medical teams) into resources with protective capacity. In such situations, the number of medical teams dedicated to the treatment of Covid19 patients should be reduced and they should be freed to treat routine patients. During the crisis, 80%-90% of medical personnel should be allocated to the treatment of regular patients and only 10%-20% to Covid19 patients. Many policymakers made the opposite decision: release regular patients and convert more and more wards to Covid19 wards. As long as the above-mentioned differentiation between A-type patients (severe Covid19 patients) and B-type patients (light Covid19 patients) is maintained, there is no need to establish more and more Covid19 wards and there is no need to allocate bottlenecks to the treatment of patients in these wards.
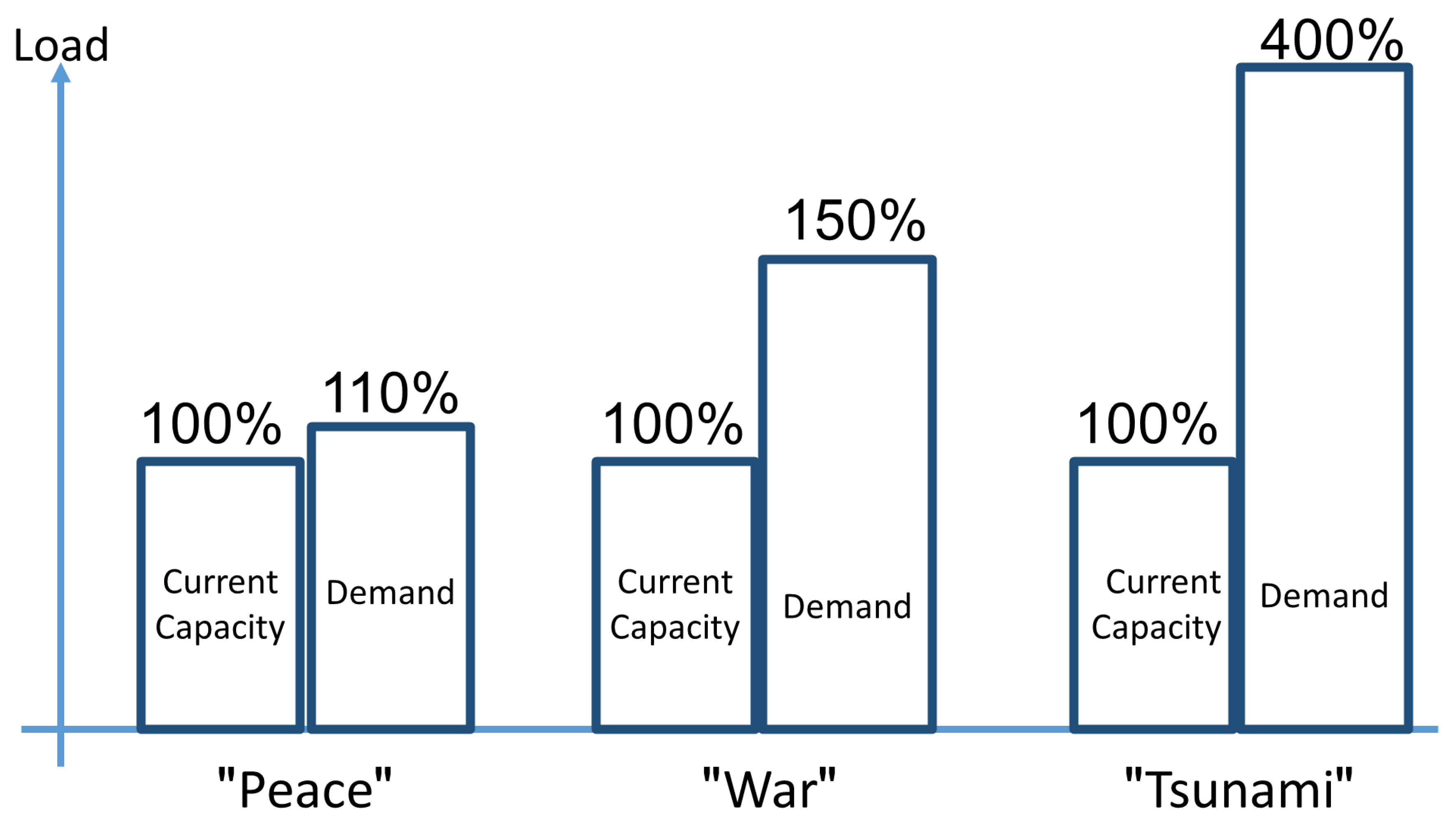
3. Resource Load Scenarios
Figure 2 presents the three load/capacity scenarios for hospitals: “Peace”, “War” and “Tsunami”. Increase in resource load/capacity results in a corresponding increase in environmental footprint. Resources operating beyond their capacity generate significantly greater amounts of waste and harmful environmental impact. The Peacetime scenario is the normal overload situation in a hospital.
During “Peace” times, hospitals are usually 10%-20% short in resources. To overcome bottlenecks, managers apply evolutionary methods such as constraint management, the complete kit concept, etc. This is the normal condition in hospitals where there are fluctuations in supply and demand. Bottlenecks in this situation are typically medical crews: senior physicians and experienced nurses.
During “War” times, such as during the Covid19 pandemic, the need for resources exceeds capacity by over 50%. To overcome this shortage, managers use the above-mentioned evolutionary methods but must also apply revolutionary methods. Here too, system bottlenecks are typically the medical crews. The first step is to create a protective capacity by rapid deployment of auxiliary hospitals. Converting internal medicine wards to Covid19 wards, postponing elective surgeries, etc. Medical crews work significantly harder and effort must be made to offload them through nurses, paramedics, physician assistants, etc. War scenarios require a hybrid application of evolutionary and revolutionary actions.
During “Tsunami” times, thousands of patients storm hospital emergency departments. In this scenario, revolutionary methods must be applied. Since the bottlenecks remain in medical crews, the policy should be to hospitalize a minimum number of patients and send the majority back to their communities. Evolutionary steps in the Tsunami scenario are a waste of managerial energy as they focus on double-digit improvement rather than on “order of magnitude” increase. Anyway, for Peace and War scenarios, the Theory of Constraints (TOC) can serve as an effective tool to increase capacity. During “peace” times, evolutionary strategies handle the excess demand peaks. During “war” times, a hybrid evolutionary/disruptive (revolutionary) strategy should be applied. During “Tsunami” times, a disruptive (revolutionary) strategy should be applied exclusively.
TOC has proved an effective tool for increasing capacity in crisis situations. Mark Woepple [2011] was hired by BP to fight the oil spill in the Gulf of Mexico. Some other supplies were the constraint. He had a couple of TOC experts go to suppliers around the globe and increased their capacity (of an already engineered production system) by up to 400% in a matter of days.
4. A Case Study
Medical center X is a large Israeli university medical center consisting of over 1,000 beds. Each year, patients from the area and beyond entrust their health to the Medical Center’s dedicated team of medical professionals. Annually the medical center treats 400,000 patients, performs 36,000 surgeries, and accepts 1.8 million patient visits, 220,000 ED visits, and 12,000 births.
The management team was knowledgeable of TOC methodology either from their studies at the university’s Healthcare Management program or through dedicated workshops given at the hospital. During the Covid19 pandemic, three additional workshops were conducted specifically for this purpose.
The campus spans over 2.7 million square feet (250,000 square meters). The Medical Center features a General Hospital, a Medical Tower, a Children’s Hospital, a Heart and Brain Building, and a Maternity and Women’s Hospital.
The following is based on our close acquaintance with the medical center before and during the Covid19 pandemic.
During “peace” times, some of the units handle 100%-120% loads. During the Covid19 “war” lockdown, demand exceeded the hospital capacity by about 50%. The medical center has prepared itself for the “tsunami” scenario but did not encounter it.
5. Evolutionary Methodologies
There are several tools to cope with each scenario. These tools fall into one of two categories: Evolutionary and Disruptive (revolutionary) change. Evolutionary change or “hill climbing” optimizes performance within given processes. Such evolutionary tools include the Theory of Constraints (TOC) seven-step methodology and the Compete Kit concept.
The disruptive (revolutionary) change consists of radical changes to processes (even up to cancellation) that will bring significant results. The “Disruptive Methodology” is a tool used to achieve revolutionary change.
Theory of Constraints Covid19 application
In healthcare systems, we often face resource constraints – bottlenecks. Expensive resources or temporary loads during peak times create resource constraints in the system. A market constraint is a case when the system has excess capacity. Dummy constraints are extremely cheap bottlenecks that must be quickly eliminated. Policy constraints result from erroneous policies and rules set by the organization (usually out-of-date ones) that hinder performance.
Bottleneck identification is achieved by exploring the work areas, interviewing people, and using process flow diagrams, and load analysis.
Ronen et al. (2018) provide many examples of successful applications of these methods in healthcare systems. They all result in significant improvements in throughput, reduction of response times, increase in patient and worker satisfaction, and quality improvements. The use of TOC is very productive in “Peace” and “War” times.
During “peace”, the load is typically between 100%-120% and is concentrated in the Emergency Department (ED), internal medicine wards, and the imaging services. Using TOC, the bottlenecks were identified: experts and interns in emergency medicine in the ED, internal medicine experts and interns, and senior and experienced nurses. In the imaging services, the CT equipment was the bottleneck. During “peace” time these three bottlenecks can be overcome by offloading the physician load to experienced nurses, paramedics, etc.
During “war” time, as was the case during the recent lockdown, the bottlenecks were medical teams (emergency medicine experts, internal medicine experts, experienced nurses, intensive care experts, and anesthesiologists). All other resources could cope with their load. The amount of Covid19 patients in the critical condition determined the overall hospital load. The total number of hospitalized Covid19 patients reached 1,200. Healthcare leaders feared the occurrence of a “tsunami” scenario as was experienced in Italy and Spain. As a result, the lockdown in the country was determined by the total number of serious and critical patients. Even such a large and complex crisis situation can be simplified by TOC’s focusing mechanism. By increasing the capacity of small and well-defined resources, lockdown decisions can be reconsidered when compared with its dramatic impact on the economy.
The Complete Kit concept
The Complete Kit (CK) concept and its theoretical background are easy to understand and not too difficult to implement. This managerial tool has been implemented in various organizations with a high success rate. It is easy to adopt in every environment and situation, providing many benefits in relatively short time spans. We present here the concept of CK and show how it can be implemented in the health care system and demonstrate successful accomplishments in numerous medical processes such as emergency departments, operating rooms, and imaging departments. It is relatively easy to adopt in the healthcare environment and provides many benefits to healthcare organizations in a relatively short period of time, as in other industries today (for example, see Cox and Schleier, (2010); Ronen (1990)). This section discusses the complete kit concept and its implications for better health care management (Leshno and Ronen, 2001).
A complete kit in health care is the set of components and materials, medical documents, medical materials, laboratory results, and other information needed to complete a given medical procedure, process, or task.
In order to properly implement the complete kit concept, one has to train and educate executives, managers, physicians, nurses, and other paramedical staff. The complete kit concept was applied at Medical Center X in the ED when calling on expert consultants. During “peace” and “war” times, the complete kit halved waiting times for CT results, which is crucial for patient treatment decisions.
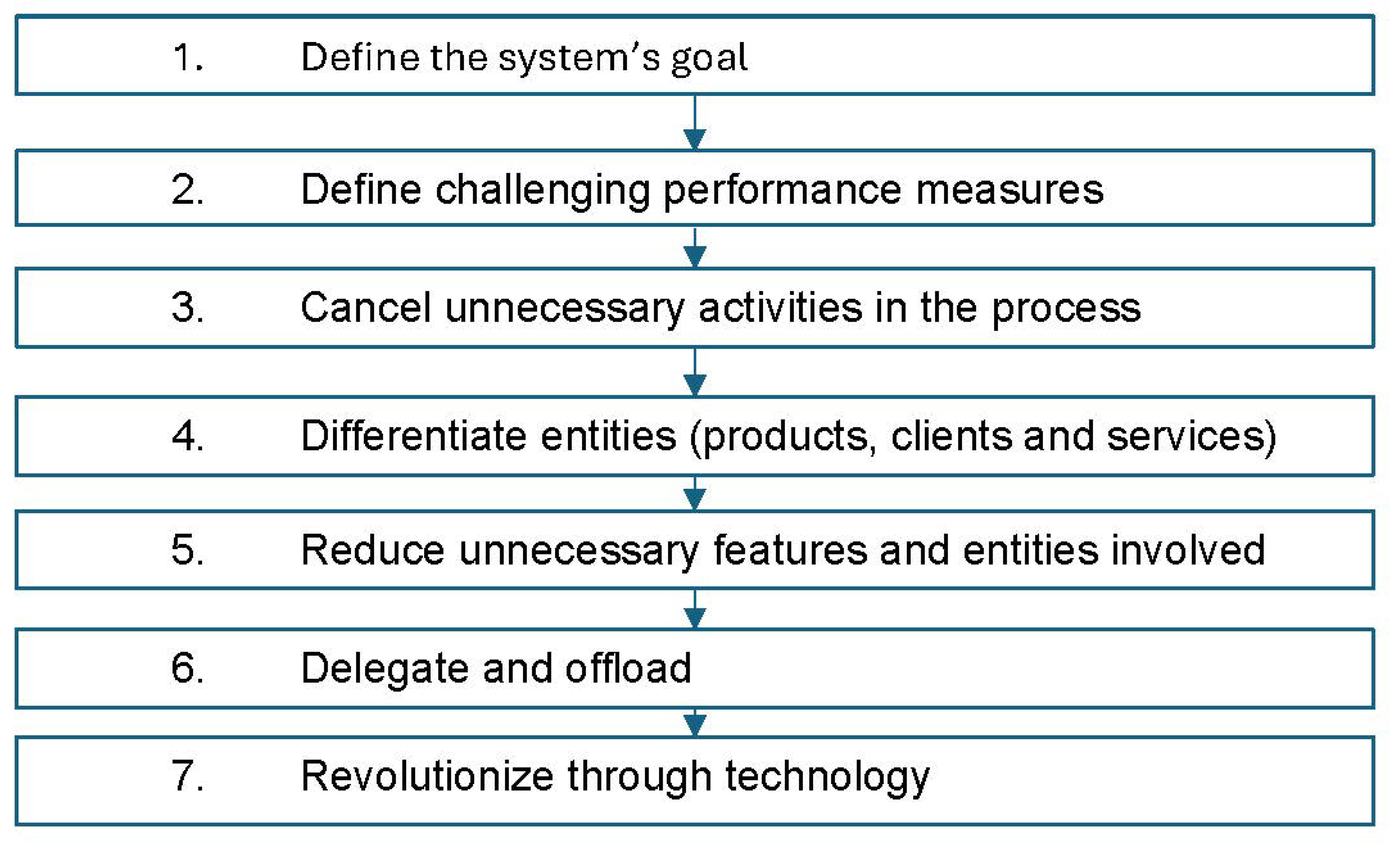
6. Disruptive (Revolutionary) Methodology
To deal with the tsunami scenario we need revolutionary tools such as the disruptive seven steps (Ronen and Coman, 2020). We will demonstrate the application of the seven-step methodology by using it in a “tsunami” scenario.
The seven steps of the disruptive methodology in healthcare are (
Figure 3):
6.1. Define the System’s Goal
Organizational processes are created to increase the organization’s value. Value enhancement consists of more throughput, less operating expenses, and better quality. We should carefully define each process goal.
6.2. Define Challenging Performance Measures
Goals must be challenging yet achievable. A challenging goal forces executives to think outside the box and realize that the goals are unachievable in the current paradigm.
In many cases, we should challenge the set of proper performance measures and the definition of individual performance measures. For example, a hospital measured the efficiency of use of its operating rooms (OR) as the percentage of time that the room was utilized. This resulted in surgeons extending patient stays in the ORs rather than canceling unnecessary activities in the process, reducing interpatient setup times or other throughput-increasing actions.
In addition, many processes are complex and involve several service units. Measurement should include the entire process, even though each service/business unit is responsible for only part of it. Enforcing a single service level agreement (SLA) motivates cooperation to achieve the required one.
6.3. Cancel Unnecessary Activities in the Process
Canceling unnecessary activities is accomplished in two ways: using a process flowchart to analyze current activities and aggressively eliminate redundant activities; or, more effectively, building a new process from scratch. In some cases, the best way to improve a process is to cancel it altogether.
6.4. Differentiate Entities (Products, Clients, and Services)
One size does not fit all. The Pareto methodology consists of three steps: classification, differentiation, and resource allocation.
Classification means to classify products, clients, and services into three groups:
1. The A group consists of 20% of products, clients, or services that contribute 80% of the value. These are the vital few entities that generate most of the value.
2. The B group consists of 30% of products, clients, or services that account for 10% of the value.
3. The C group consists of 50% of products, clients, or services that account for 10% of the value.
Differentiation means different policies for each group.
Resource allocation implies that more resources are allocated to the A group, fewer to the B group, and even less to the C group.
6.4. Reduce Unnecessary Content and Entities Involved
The 25/25 principle states that 25% of projects should be eliminated or canceled. The remaining 75% must be tapered, and 25% of the content should be removed (see Ronen et al., 2012).
For example, the admission office in one hospital was dealing with both admission and discharge of patients. After analyzing the process using the disruptive methodology, they concluded that in 85% of the cases patients do not need to go through the admission office again.
6.5. Delegate and Offload
A significant part of the activities should be offloaded to other members of the team. Many processes can be delegated to the customer for self-service. This already is the case with digitalization, where many activities are available via mobile devices with no intervention by professionals.
6.6. Revolutionize through Technology
After following the first six steps, it is time to turn to technology for revolutionary impact. The dilemma is between the best-of-breed strategy, where optimal solutions are selected resulting in expensive and awkward integration, or best-of-suite, where solutions are less revolutionary but operate together seamlessly.
7. Discussion
The contribution of this paper is in managerial innovation focused on sustainability. We refute the belief that “overdoing” improves the system’s throughput. Overdoing dramatically increases the system’s environmental footprint, thus hurting sustainability.
The “peace” scenario was the routine condition in which medical centers were operating prior to the Covid19 pandemic – hospital demand slightly exceeded the available resource capacity. In this scenario, hospitals confronted known bottlenecks, which were the primarily continuous shortage of medical teams and experienced nurses. Hospitals have been confronting this situation throughout the year, including during the flu epidemic, using established bottleneck management techniques and the application of the complete kit concept.
The “war” scenario was the situation experienced when rising numbers of Covid19 patients led to the first two lockdowns in Israel. During “war” scenarios, medical center X encountered peaks when demand exceeded capacity by 50% to 150%. Here the medical center implemented disruptive (revolutionary) strategies such as converting internal medicine wards into Covid19 wards and opening provisional “field hospitals” in parking lots. During the “war” scenarios, the bottlenecks were still medical crews and experienced nurses. The medical center passed these difficult times without collapsing thanks to focused management of the bottlenecks and laudable devotion, leadership, and tenacity vis-à-vis formidable individual and systemic loads. Experience gained during the pandemic demonstrates that the agility of the human resource in the healthcare system is impressive and throughput increased dramatically without experiencing a collapse of medical crews. A synthesis of authority and duty delegation from physicians to nurses and from nurses to assistants accompanied by resource pooling significantly increases capacity without medical crew attrition.
The real concern arises from the “tsunami” scenario where demand grows by hundreds of percent and the system faces the threat of collapse – as was the situation in Italy and Spain. In the “tsunami” scenario, the system must switch to crisis mode and apply a disruptive (revolutionary) strategy: establishing a broad home-care system, creation of emergency medical services, postponing elective surgeries, increasing the capacity of alternative hostels, and national initiatives to accelerate rapid discharge, etc. Some of these strategies were successfully applied during the lockdown periods and demonstrated that the systems did not reach a point of collapse.
This paper deals with healthcare crisis management during pandemic times. The leader must diagnose the condition the organization is in and act accordingly. The concept is applicable in other “code brown” crisis management scenarios such as chemical or nuclear massive accidents, natural disasters, etc. Many leaders respond intuitively to such crises. By establishing a resource management methodology, we strive to facilitate the dialogue within the team and also among teams that have not worked together in the past.
References
- Cox III, J. and Schleier, J., (2010). Theory of Constraints Handbook. New York: McGraw-Hill.
- Goldratt, E.M. , (1997), Critical Chain, Croton-on-Hudson, NY: North River Press.
- Goldratt, E.M. , and Cox, J., (1988) The Goal, North River Press, 2nd Revised Edition Croton–on-Hudson, NY.
- Groop, J. , Ketokivi, M., Gupta, M. and Holmström, J. (2017). Improving home care: Knowledge creation through engagement and design. Journal of Operations Management, 53–56(1), 9–22.
- Gustavo, M. B., J. F. Cox III and P. P. Rodrigues. Outcomes of managing healthcare services using the Theory of Constraints: A systematic review. Health Systems 2022, 11, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Ikeziri, L.M. de Souza, F.B., Gupta M.C. and Fiorini, P.C. Theory of constraints: review and bibliometric analysis. International Journal of Production Research 2019, 57. [Google Scholar]
- Mabin, V. and Balderstone, S. J. The performance of the theory of constraints methodology: Analysis and discussion of successful TOC applications. International Journal of Operations and Production Management 2003, 23, 568–595. [Google Scholar] [CrossRef]
- Mabin, V., Yee, J., Babington, S., Caldwell, V., and Moore, R. Using the theory of constraints to resolve long-standing resource and service issues in a large public hospital. Health Systems 2018, 7, 230–249. [Google Scholar] [CrossRef] [PubMed]
- Woeppel, M, (2011) TOC Tapped to Accelerate Gulf of Mexico Cleanup, Video presented at TOCICO, https://cdn.ymaws.com/www.tocico.org/resource/collection/7A232B11-402E-4DCE-B5CA-C33D88A0B713/Woeppel,_Mark_ToC_Tapped_to_Accelerate_Cleanup_rev_b_(FINAL).
- Rodriguez D. R., W. Silva, Savachkin A., Das T., Daza J. (2022) Resilience as a measure of preparedness for pandemic influenza outbreaks, Health Systems, Published online , 2022. 12 April.
- Ronen, B., and Coman, A. Are you passing by your digitalization opportunities? Reengineering for the digitalization age. Quality Progress 2020, 53, 26–31. [Google Scholar]
- Ronen, B. , Pliskin, J.S., and Pass, S., (2018) “The Hospital and Clinic Improvement Handbook: Using Lean and the Theory of Constraints for Better Healthcare Delivery”. Oxford University Press, 2018, NY NY.
- Ronen, B., and Starr, M.K. Synchronized Manufacturing as in OPT: From Practice to Theory. Computers and Industrial Engineering 1990, 18, 585–600. [Google Scholar] [CrossRef]
- Stratton, R. and Knight, A. ( 21(4), 484–498.
- Stratton, R. and West, B. (2014). A holistic solution for community health and social care. TOCICO Conference 2014: 12th Annual Worldwide Gathering of TOC Professionals, 12.
- https://www.aha.org/sustainability April.4.2024.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).