Introduction
Peri operative visual impairment/Blindness as an isolated complication following cardiac surgery is known to occur in 0.05-0.1% of cases [
2]. Most common etiology is ischemic damage to retina / optic nerve/ occipital cortex [
2]. We report a case of bilateral cortical blindness due to unilateral subdural hematoma in occipital region with spontaneous remission after 4 weeks.
Case Report
20 months old child with tetralogy of fallot’s (TOF), weighing 10 kg and saturation of 82% underwent elective intracardiac repair. Repair was performed through median sternotomy. Trans right atrial VSD closure, right ventricular outflow tract resection along with limited transannular patch augmentation was performed on cardiopulmonary bypass (CPB). Aorto-Bicaval cannulation was performed and baby was cooled to 28 degree﮿C. Aortic X clamp time and CPB time were 180 min and 240 min respectively. On CPB,range of mean blood pressure, hematocrit, ACT and lactate were 50-65 mm Hg, 30-33%, 450-900 and 1-2mmlol/litre respectively . Arterial filter and hemofilter were part of CPB circuit.
Post repair, patient was rewarmed gradually to 36 degree C and CPB was weaned off on epinephrine 0.05 mcg/kg/hr, milrinone 0.25 mcg/kg/min and vasopressin 0.02U/kg/hr. Echocardiography showed good biventricular function, small residual VSD and RVOT gradient of 40 mmHg. Repair was accepted and patient shifted to intensive care unit (ICU). Baby was extubated on post operative day 1 and inotropes tapered off.
It was noticed that baby was irritable and not making eye contact. He was not able to locate mother but was responding to her voice. On examination, perception of light was negative in both the eyes but pupils were reacting to light. There was
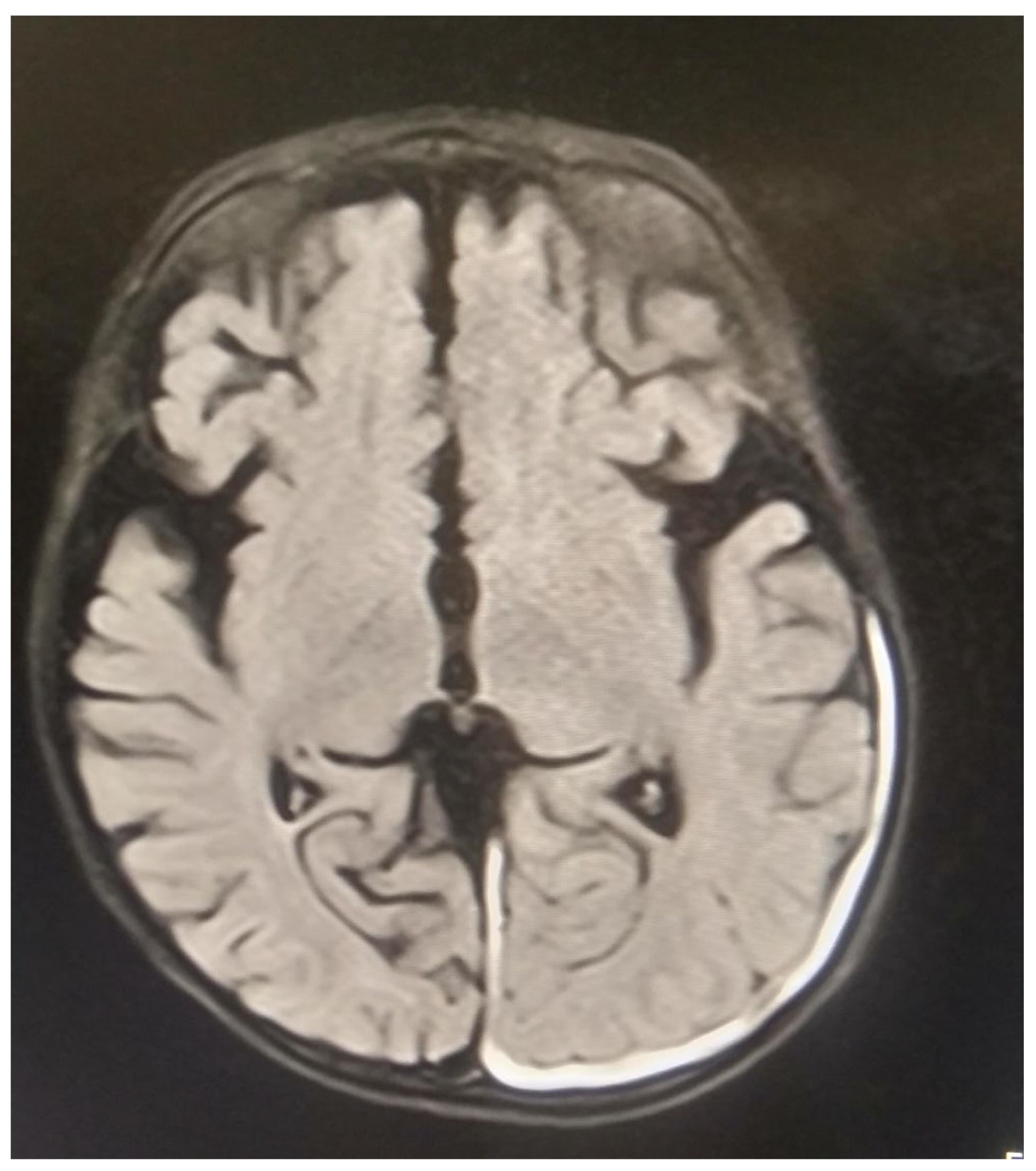
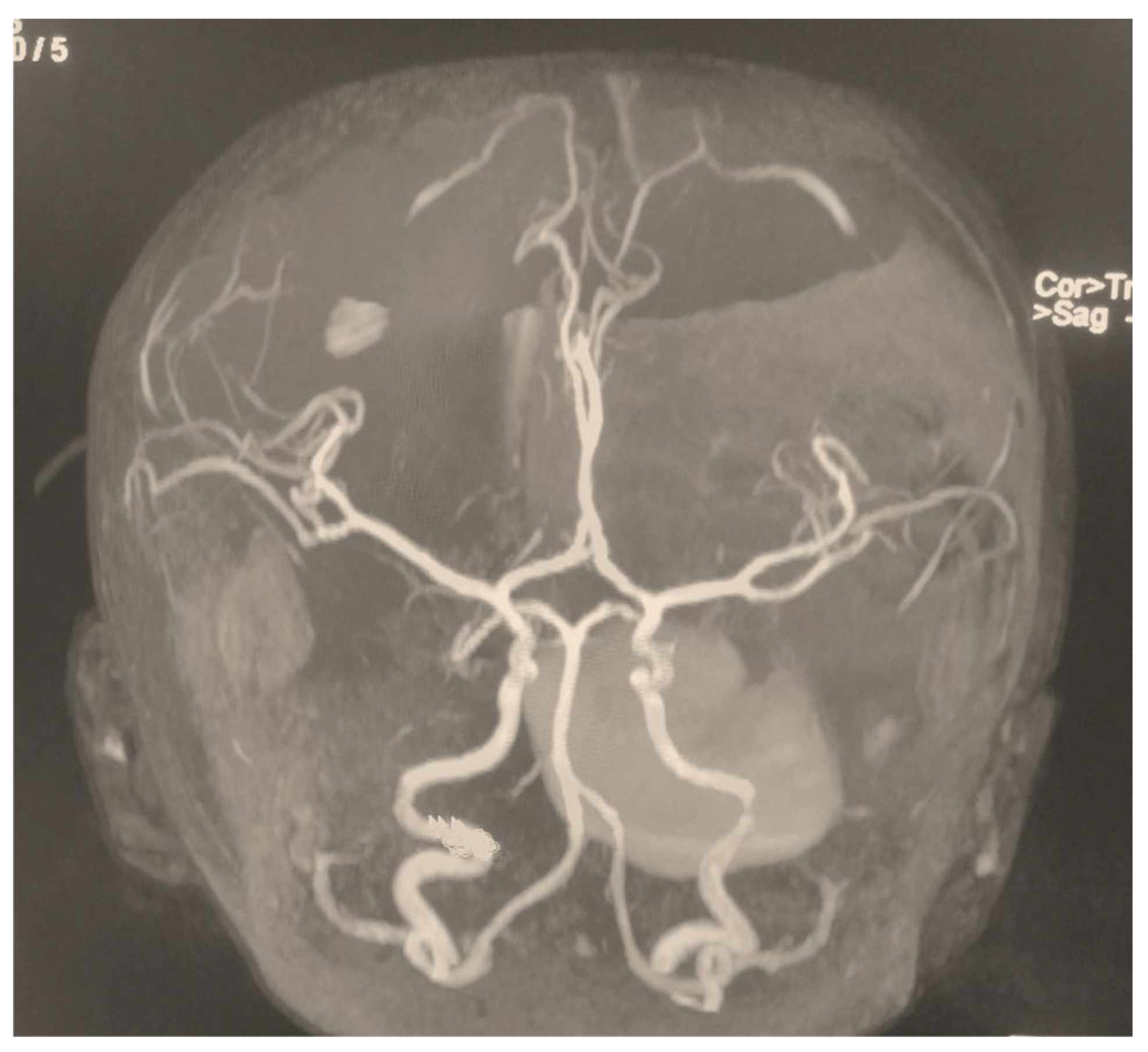
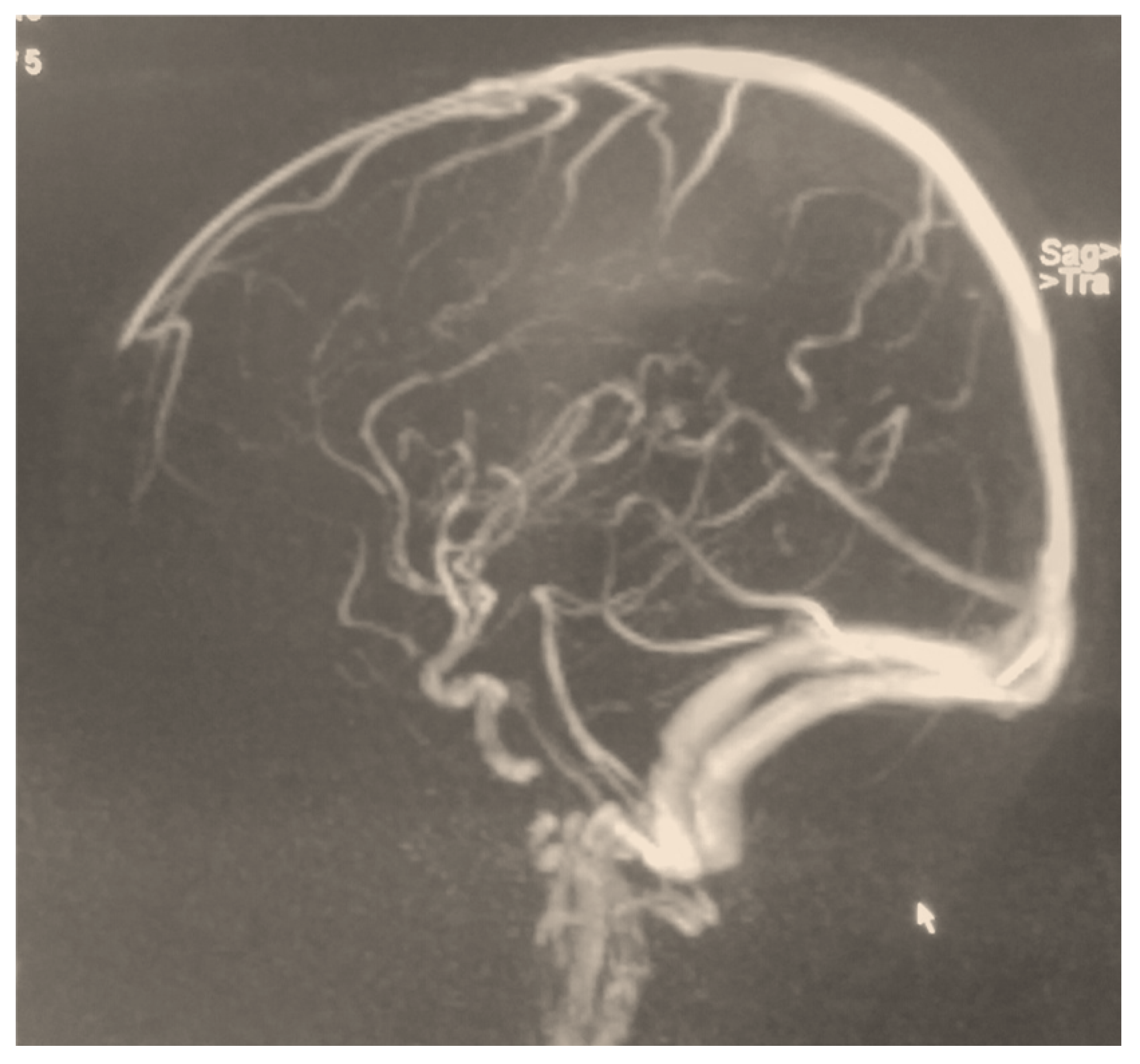
absence of lid reflex response to threat in both the eyes. Fundus examination was normal bilaterally. There was no other neurological abnormality. MRI brain with MR angiography revealed small subdural hematoma in left occipital cortex extending into interhemispheric fissure. It showed no evidence of embolism/diffusion restriction/ venous thrombosis/optic nerve damage. EEG was normal. Visual Evoked Potential (VEP) response to flash light was negative bilaterally. Diagnosis of cortical blindness was made. SDH remained nonexpanding with no midline shift on post op day 6 and 10. (
Figure 1,
Figure 2 and
Figure 3). Baby was discharged on post operative day 11. On Follow up after 4 weeks vision was normal and CT scan showed resolution of SDH.
Most of previous reported cases of cortical blindness following cardiac surgery had evidence of infarcts on CT/MRI in occipital region and abnormal EEG changes. These were typically absent in our case, further suggesting that SDH was possible culprit of causing visual impairment in our patient.
The visual recovery after acquiring cortical blindness is reported to be between 2 weeks to 5 months. [
8] EEG has been found to be better predictor of visual recovery than VEP [
8]. Good prognostic factors for visual recovery include a) normal EEG b) focal / multifocal spike and wave discharge c) slow sharp wave discharges.
There was no positive correlation between VEP and recovery of vision [
8]. Normal CT/MRI were suggestive of possible visual recovery [
8].
Conclusions
Cortical blindness is a rare and devastating complication after congenital heart repair. It can be transient if underlying cause is reversible. Unilateral occipital SDH can result in bilateral cortical blindness in post operative period.
References
- Ferry PC. Neurologic sequelae of open heart surgery in children. Am J Dis Child 1990; 144: 369-73. [CrossRef]
- Shen Y, Drum M, Roth S. The prevalence of perioperative visual loss in the United States: A 10-year study from 1996 to 2005 of spinal, orthopedic, cardiac, and general surgery. Anesth Analg. 2009; 109(5) : 1534 -45. [CrossRef]
- Bharati S, Sharma MK, Chattopadhay A, Das D. Transient cortical blindness following intracardiac repair of congenital heart disease in an 11-year-old boy. Ann Card Anaesth 2017;20:256-8. [CrossRef]
- Tchantchaleishvili V, Dibardino DJ, Bolman RM 3rd. Transient bilateral blindness in a patient after cardiac surgery. Heart Surg Forum 2011;14:E198-9.
- Shin YD, Lim SW, Bae JH, Lee DH, Baek DH, Hong JS. Transient cortical blindness after heart surgery in a child patient – A case report. Korean J Anesthesiol 2010;59:61-4. [CrossRef]
- Scarpino, Maenia et al. Cortical Blindness After Cardiac Surgery: Just an Ischemic Mechanism? Journal of Cardiothoracic and Vascular Anesthesia, Volume 30, Issue 4, 1053 - 1056.
- Faried; et al. Cortical visual impairment as an initial clinical manifestation of post-traumatic brain injury: A case report and review of literature.Interdisciplinary Neurosurgery 18 (2019) 1004852. [CrossRef]
- Virginia C.N. Wong, Cortical blindness in children: A study of etiology and prognosis, Pediatric Neurology, Volume 7, Issue 3,1991,Pages 178-185,. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).