1. Introduction
Calcaneal fractures, which account for 2% of all bodily fractures and 60% of tarsal fractures, are frequently caused by high axial energy trauma. Of these, 75% are intra-articular fractures, which greatly influence postoperative results [
1]. Displaced intra-articular calcaneus fractures (DIACF) typically stem from high-energy trauma, and optimal surgical outcomes necessitate a deep understanding of calcaneal anatomy, fracture characteristics, and associated soft tissue injuries [
2]. How best to treat DIACF remains a contentious issue. The two main treatment options are open reduction and internal fixation (ORIF), where injuries are reduced with plates and screws, and minimally invasive osteosynthesis (MIOS), which uses percutaneous reduction and external fixation. The choice depends on the patient’s particulars, such as age, functional expectations, existing health issues, degree of injury, and convalescence factors [
3]. More surgeons are now leaning towards minimally invasive methods due to fewer soft tissue complications and improved postoperative recovery [
2]. Nevertheless, these methods might result in inadequate anatomical reduction and inaccurate restoration of the Böhler angle, which is crucial for the functional recovery of the heel [
4,
5].
This research aims to outline the advantages and disadvantages of each treatment method for DIACF, as well as provide insights into patient satisfaction and the rate of complications. By utilizing the most recent scientific literature, our study offers critical guidance for therapeutic decision-making in treating DIACF.
2. Materials and Methods
2.1. Demographic Data
This comparative retrospective cohort study involved 70 patients who underwent surgery for DIACF displaced > 2 mm at the Orthopedics and Traumatology Unit, A.O.U. Policlinico “G. Rodolico”, University of Catania, Italy, between January 2018 and September 2022.
The inclusion criteria included patients over 18 years of age who were hospitalized between January 1, 2018, and September 30, 2022. These patients had intra-articular calcaneal fractures treated by specific methods and may or may not have had bone grafts. Polytraumatized patients were also included.
The exclusion criteria included: a history of trauma or foot surgery, open or beak fractures, fractures outside the joint, Sanders type I fractures, and cases treated with primary arthrodesis. We invited all patients via phone to participate anonymously in a survey that aimed to evaluate three main topics.
Risk factors and health status prior to the trauma: The presence of decompensated diabetes, diabetic foot, hypertension, smoking, autoimmune diseases, immunodeficiencies, coagulopathies, peripheral arteriopathies, and other pathologies affecting performance status.
Anthropometric parameters: weight, height, and age at the time of the operation.
Information relating to the fracture: causes, the eventuality of polytrauma, treatment performed, waiting time for the operation, and time to weight-bearing.
2.2. Surgical Techniques
2.2.1. The Conventional Approach of Internal Fixation with Plate and Screws
Patients were positioned on their side with a thigh tourniquet. A capital “L” shaped incision was created vertically between the fibula and Achilles tendon and horizontally at the base of the fifth metatarsal. A full-thickness flap was then lifted, ensuring the preservation of vascularization and the sural nerve. This flap was temporarily secured in place.
During the surgery, the peroneal retinaculum was split, and both the fibulo-calcaneal and talo-calcaneal ligaments were removed to reveal the fracture site and the sunken posterior facet’s depth. The posterior tuberosity fragment was aligned with the medial fragment using an osteotome and a Shantz screw, temporarily secured with K-wires. This process made provision for the reduction and elevation of the posterior facet fragments with K-wires, aiding in the correction of heel height and subtalar depression. After thorough radiographic confirmation of precise reduction, a proper rearfoot alignment, and the absence of varus, internal fixation began. A subchondral screw was inserted from lateral to medial up to the sustentaculum tali, ensuring not to insert the screw too deep to avoid tendinitis or neurovascular damage on the medial side. Then, a plate, molded based on fracture comminution, was put in place and secured with several angular stability screws. In a few cases (noted twice in our study), a synthetic bone graft was used to rebuild the depressed joint surface. The final reduction was checked, and the K-wires were removed. A final radiographic review confirmed the reduction. The ankle was immobilized with a knee-high pinstripe cast for a month; partial weight-bearing was allowed after 6 weeks, and full weight-bearing after 8 weeks [
5].
2.2.2. Minimally Invasive Osteosynthesis with Triplane External Fixator
Once the patient was positioned in lateral decubitus, opposite the fracture site, and under loco-regional anesthesia, the lateral aspect of the heel was exposed. This allowed for full lateral and axial fluoroscopic visualization of the hindfoot without obstructing the surgical field. Two K-wires were inserted through the heel to rectify the length and varus to achieve reduction. The proper restoration of the bone fragments and Böhler’s angle was confirmed with an image intensifier. The application of external fixation succeeded in this.
A minifixator was used for external fixation, composed of three clamps and six grippers fitted with self-drilling bone screws. The fixator features a uniplanar articulated clamp designed for thalamic fragments. This is connected to two compression-distraction units, which is useful when two counterbalancing points are needed for fragment reduction.
First, two self-drilling bone screws, with a diameter of 4 mm and a length of 70–90 mm, were inserted into the subthalamic fragments; guide K-wires and screws may or may not have been used and removed prior to this step. Additional screws were inserted into the anterior and/or posterior calcaneal processes, depending on the fracture variety and severity. Furthermore, for cases needing increased stability, such as severe comminution of the anterior apophysis, screws were additionally implanted into both these locations and the cuboid.
Fluoroscopic verification affirmed the realignment of the calcaneal body and the adjustment of varus-valgus deviations. Following this, the external fixator was secured onto the screws. Postoperatively, the patient was barred from weight-bearing for 4 weeks; nevertheless, immediate active and passive ankle movements were initiated. The patient was directed to clean the external fixator pins with saline and antiseptic solution twice a day [
6].
2.3. Clinical and Radiographic Assessment
This study followed the STROBE guidelines. We have attached the STROBE Statement - checklist.
For a thorough final functional assessment, this study defined two types of endpoints for each patient, providing an in-depth insight into their postoperative and ongoing conditions.
We addressed immediate, early, and late postoperative complications. Immediate complications included traumatic or hemorrhagic shock and vascular and nerve injuries. Early complications were thromboembolism, dehiscence and/or infection of surgical wounds, delays in wound healing time with or without Vacuum Assisted Closure (VAC) Therapy, compartment syndrome, and cutaneous necrosis. Late complications included pneumonia, bedsores, chronic pain and swelling, peroneal tendinitis and/or tendon dislocation, joint stiffness, arthritis and/or arthrosis, algodystrophy resistant to painkillers, pseudoarthrosis and/or consolidation defects at the 6-month control radiograph, and any other disorders related to recovery [
7,
8].
Two functional outcomes assessment scales were used: The Maryland Foot Score and the Creighton-Nebraska Health Foundation Assessment Scale (CNHFAS) for calcaneal fractures [
9]. These scales evaluate crucial aspects of the patient’s performance status following a heel fracture, including the presence of chronic/sporadic pain with/without painkillers and whether it is associated with rest/work/daily activities, motor function including distance and surfaces navigable, joint function specifically internal and external rotation of the rear foot and flexion-extension, the necessity for support devices, limping, difficulties in climbing stairs, abnormal hindfoot loading, aesthetic deformities, and same/different work recovery with/without restrictions.
The cohort of patients received uniform treatment within 15 days after the trauma. This was preceded by thorough radiographic analyses in Antero-Posterior, Lateral, and Axial Projections, as well as preoperative CT scans. These evaluations helped detect changes in the Böhler and Gissane angles, heel height and volume, degree of comminution, and displacement based on the Sanders classification.
After treatment, all patients were subject to follow-up appointments as outpatients, during which radiographic evaluations were performed at 1, 3, 6, and 12 months. These visits were aimed at assessing the functional scales and confirming adequate postoperative recovery. Aspects examined included heel load uniformity, stability of the ankle and hindfoot with or without valgus or varus, and the degrees of flexion, extension, and internal and external rotation in the back foot.
2.4. Statistical Analysis
Statistical analyses were conducted using SPSS software, version 25.0 (IBM Corp., Armonk, NY, USA). We began with the Shapiro-Wilk test to examine the normal distribution of functional outcome scores. These scores included the Maryland Foot Score (MFS) and the CNHFAS in both ORIF and MIOS groups. After confirming a normal distribution, we used independent sample t-tests to compare means between the two groups.
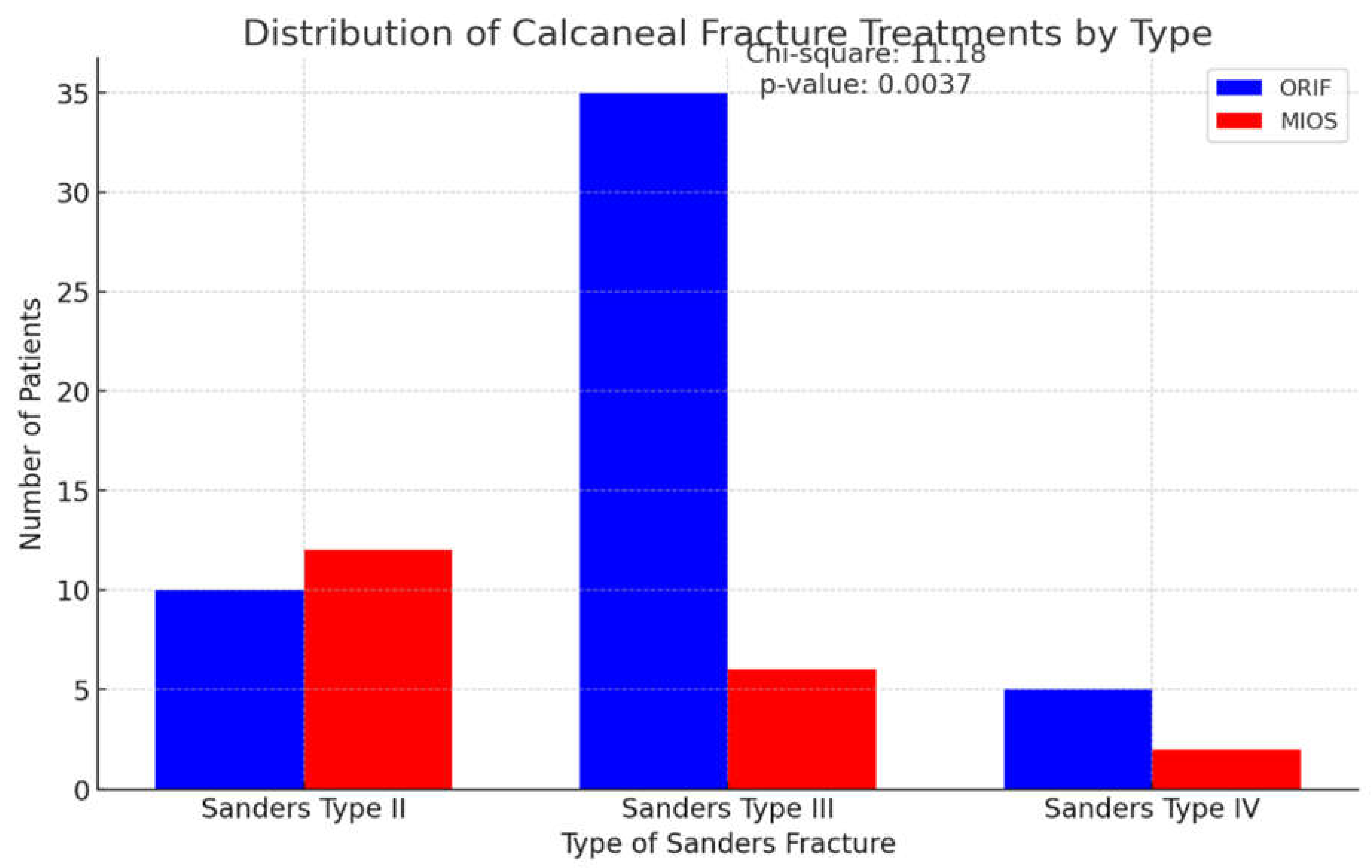
Chi-square tests were used to assess the significance of differences in categorical outcomes between groups, focusing on postoperative complications like tendinitis, chronic pain and swelling, algodystrophy, and surgical wound infections. Additionally, the distribution of patients by Sanders classification in the study, shown in
Table 1, was analyzed using the chi-square tests. This analysis was important in determining if the choice of treatment techniques had a bias toward specific fracture types.
A p-value below 0.05 indicated statistical significance in all tests. Continuous variables are presented as mean ± standard deviation and categorical variables as frequencies (percentages). This comprehensive statistical analysis robustly evaluates the efficacy and safety of ORIF and MIOS techniques in managing calcaneal fractures.
3. Results
3.1. Simple
In the Orthopedics and Traumatology Unit, a cohort of 201 patients was treated for calcaneal fractures. Only 70 patients met the study’s criteria, and they were treated either with ORIF (50 patients) or MIOS (20 patients). The severity of the fractures was categorized as Sanders type II (22 cases), type III (41 cases), and type IV (7 cases). The retrospective study included patients admitted between January 2018 and September 2022 and entailed a follow-up period of 9 months.
We conducted a chi-square test to determine whether the choice of treatment—either ORIF or MIOS—significantly varied based on the Sanders classification of calcaneal fractures. The patient distributions for these treatment techniques are shown in
Figure 1.
The test resulted in a chi-square value of 11.18 and a p-value of 0.0037, suggesting significant differences in the application frequency of the two treatment methods for different fracture types.
The average age of the group studied was 47.8 years, with falls from a height being the most frequently identified cause of trauma. The study also evaluated risk factors that could potentially hinder healing or pose as objections to invasive treatments, such as diabetic foot, hypertension, peripheral arterial disease, and coronary artery disease. The group showed 32 cases of smoking risk conditions, with ten individuals having smoked a pack a day for at least 10 years. Interestingly, all smokers refrained from smoking during their recovery period. The group also included four cases of immunodeficiency, one case of coagulopathy, and five incidents of multiple traumas (
Table 1).
3.2. Treatment with MIOS
Twenty patients underwent minimally invasive surgery employing an external tripolar fixator. The fractures were classified as follows: 60% as Sanders type II (comprising four Sanders IIA and eight Sanders IIB), 30% as Sanders type III (which included two III AB, one III AC, and three III BC), and 10% as Sanders type IV. The average wait time prior to surgery was 3 days, with a range of up to 10 days. Patients were permitted partial and full weight-bearing at 2 and 4 weeks post-surgery, respectively. The external fixator was removed 6 weeks post-surgery. X-Ray follow-ups at the first, third, sixth, and twelfth postoperative months showed successful recovery of the Böhler angle within a range of 20° to 40°. However, two cases had a recovery below the physiological value of 20° and were coupled with chronic pain. Complications included 25% incidences of tendinitis, 50% of osteoarthritis, and 37% with chronic pain. Local infections were detected at the sites of self-drilling screw insertion in 12.5% (three cases) of the total cohort, which were addressed using local and oral antibiotics. There were no reports of deep infections or premature removals of the external fixator.
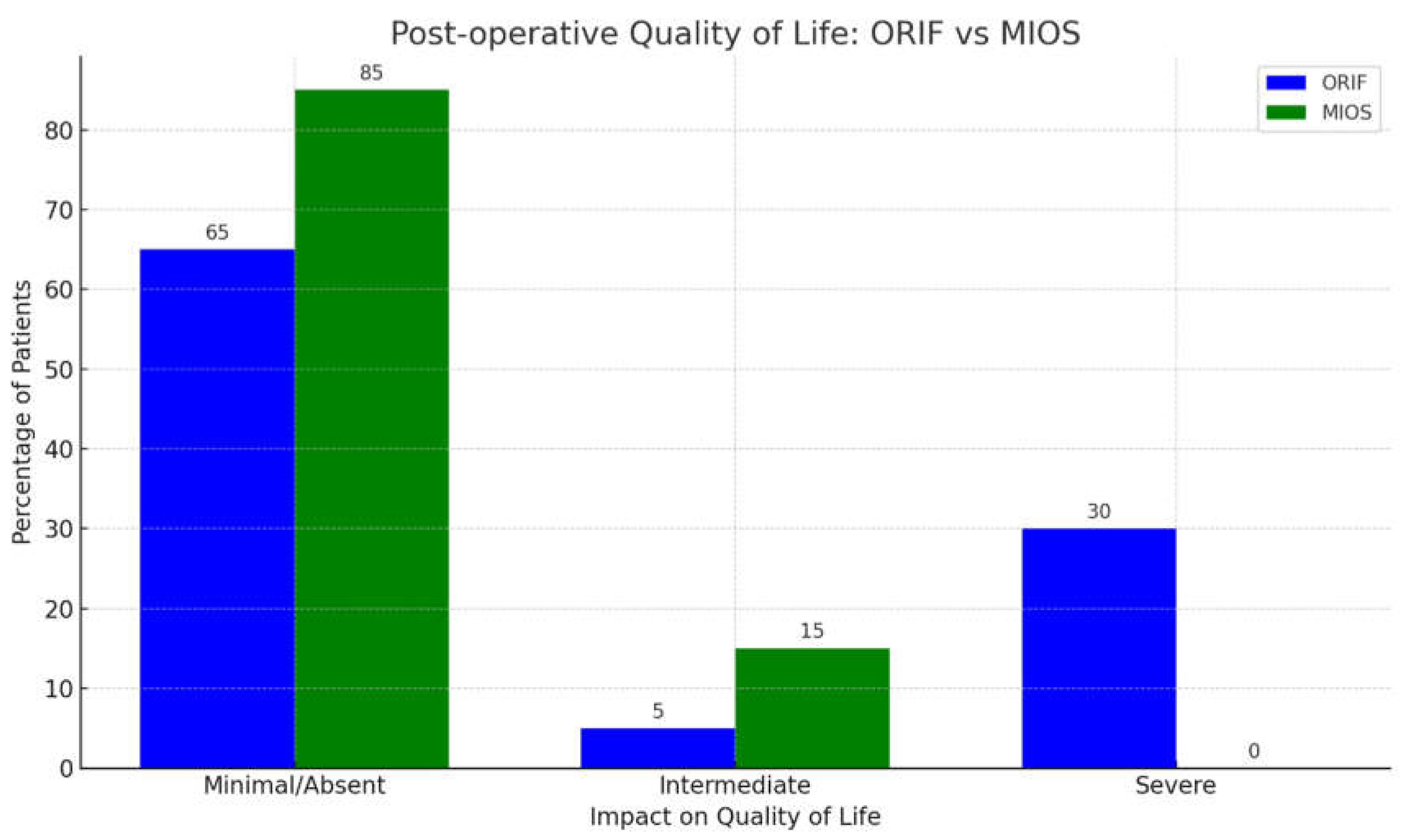
The postoperative quality of life assessment findings are reported in
Figure 2. A significant portion of patients, 85% of them (17 out of 20), reported minimal to no postoperative issues, enjoying an excellent or good quality of life as per the MFS (90–100 points for excellent, 75–89 points for good) and the Creighton-Nebraska Health Foundation assessment scales (100–90 excellent, 89–80 good). These individuals experienced only sporadic neurological symptoms, such as tingling upon insertion of one self-healing screw, and tendon disorders, managed effectively with massage therapy. They faced no limitations in activities like walking more than 1 km, navigating uneven surfaces or stairs, and required no aids. Aesthetic deformities were absent, joint function remained normal, weight-bearing favored the inside of the heel, and any type of footwear was comfortable. Returning to previous full-time jobs, including sports activities, was accomplished without the need for hospital visits beyond routine follow-up. For 15% of patients (3 cases), complications moderately impacted convalescence due to superficial infections at screw sites and calcaneal arthrosis. Though they reported chronic pain, they abstained from analgesics, opting for orthotic shoes and cryotherapy post-exertion. No cases exhibited severe impact with values falling below thresholds (MFS below 50, CNHFA below 64).
3.3. Treatment with ORIF
A group of 50 patients suffering from substantial bone fragmentation (comprising 25% Sanders type II [IIB], 92.5% Sanders type III [IIIBC], and 12.5% Sanders type IV) were treated using ORIF through an Extensile Lateral Approach (ELA). The usual delay before surgery was 3 days for minor trauma and 15 days for major fractures, averaging out to 9 days, allowing time for the resolution of edema and soft tissue injury - shown by a positive Wrinkle sign. On average, weight-bearing recovery occurred at 3 months with the help of crutches, while complete functional recovery occurred in 6 months. X-ray follow-ups demonstrated recovery of the Böhler angle within a range of 20° to 40° (average recovery: 29.5°), starting from initial preoperative values of 0–10°.
The reported postoperative complications included tendinitis in 44% of patients, chronic pain and swelling in 55%, painkiller-resistant algodystrophy in 33%, and joint stiffness in 44%. Twenty percent of the cohort (8 cases) developed surgical wound infections and showed poor healing despite receiving VAC therapy. These patients required the removal of synthetic materials due to subsequent osteomyelitis [
10]. Multiple overlapping complications were experienced by 44% of the cohort. In 50 cases treated with ORIF, 16 (32%) reported a complete absence of complications.
In 65% of cases (32 out of 50), patients experienced minimal or absent impact on their convalescence, excluding Achilles tendon impairment occurring at the time of trauma (
Figure 2). They occasionally reported pain without requiring analgesics, had unrestricted mobility even on challenging surfaces or distances exceeding 1 km, and lacked joint stiffness. Normal plantar flexion, dorsiflexion, and rear foot rotation were observed without the need for support devices or limping. Stair navigation was unassisted, and weight distribution favored the back foot with slight outside heel loading in 11% of cases. They comfortably wore any shoe without orthosis or size alteration, showed minimal aesthetic deformities, and resumed their previous full-time jobs. Intermediate impact was observed in 5% of patients who experienced persistent swelling and chronic pain during daily activities a year post-operation. They faced stiffness and joint restrictions but managed without aids or lameness, though descending stairs required railing support. Uneven back foot support, shoe insoles, slight scar deformities, and job restrictions were noted. Severe impact was reported by 30% of patients (12 out of 40), characterized by algodystrophy, acute postoperative pain requiring daily analgesics, joint stiffness, and tendinitis. Panic attacks and depression necessitated neurological consultation. Chronic pain affected daily and recreational activities, with reduced walking distances, instability, abnormal gait, and moderate limping. Aesthetic deformity, shoe size increase, fatigue leading to part-time work for four cases, and inability to return to previous jobs for eight cases were evident.
Using the Shapiro-Wilk test, we determined that the MFS and the CNHFAS distributions in both ORIF and MIOS groups were normal (p > 0.05). Later analyses through independent t-tests showed no noteworthy differences in these functional outcomes between the groups (p > 0.20). This indicates that the two treatments had a comparable efficiency regarding functional recovery (
Figure 3).
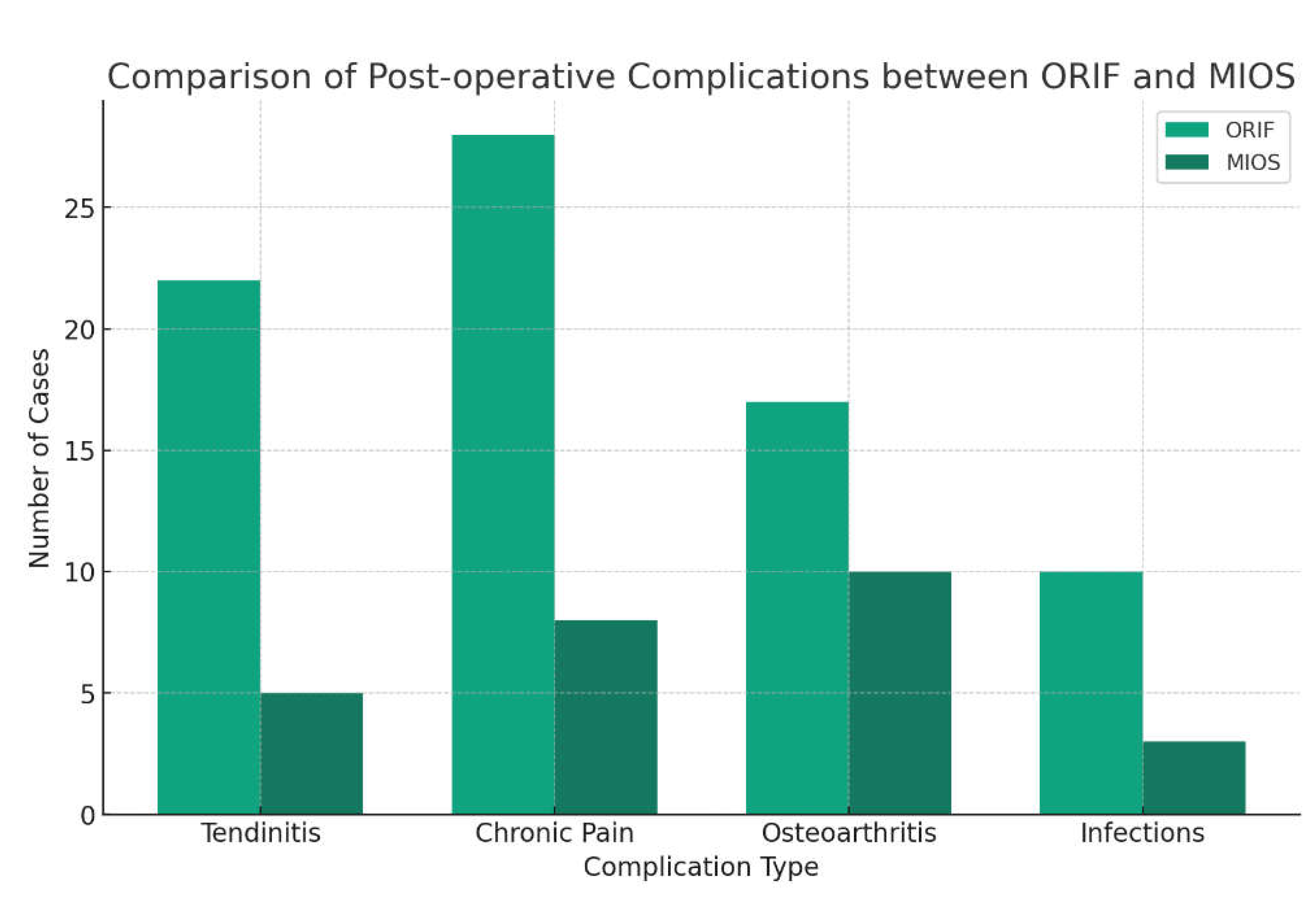
The chi-square test analysis of postoperative complications highlighted no substantial differences between the ORIF and MIOS groups in relation to tendinitis, chronic pain and swelling, algodystrophy, and surgical wound infections (p > 0.20 for all).
Figure 4 visually encapsulates these findings, presenting a comparison of the frequency of complications between the two groups.
4. Discussion
The treatment paradigm for calcaneal joint fractures (DIACF) has significantly changed in recent decades. The initial focus was on the precise anatomical reduction of the subtalar joint. However, the emphasis has now shifted towards restoring the three-dimensional height and correct alignment of the calcaneal body in axial and coronal planes. Modern strategies give more importance to postoperative care and its broader impact on the patients’ functional reintegration and future quality of life. This includes evaluating outcomes that extend beyond traditional measures like range of motion (ROM) and chronic pain, as well as considering complications in soft tissue healing [
2,
11].
Interest in minimally invasive techniques, such as percutaneous reduction and external fixation, is growing. These techniques are especially useful for treating high-energy fractures accompanied by severe soft tissue damage, as well as patients with added risk factors such as old age, immunosuppression, diabetes, smoking, coagulopathy, and high anesthetic risk [
10,
12].
While there is a lack of randomized clinical trials comparing ORIF to external limb alignment and MIOS with external fixation, meta-analyses indicate that there are no substantial outcome differences between these treatments. Although ORIF often results in better anatomical restoration of the Böhler angle, it matches the functional results of other methods. However, it is linked with a higher occurrence of postoperative complications such as surgical wound dehiscence, infections, neurovascular injuries, and early osteoarthritis. Conversely, MIOS with external fixation tends to yield fewer complications, which are also less severe. These include chronic pain, occasional infections at the screw insertion sites, inadequate reduction, and postoperative osteoarthritis [
1,
7,
8,
12].
The lack of a universally accepted diagnostic and therapeutic algorithm hampers the prediction and planning of individual recovery outcomes. Factors such as fracture type, patient characteristics, and the expertise of the surgical team affect treatment decisions. This is evidenced in our study of 70 patients, where those with severe comorbidities, conditions like smoking or diabetes, older individuals, victims of high-energy trauma, and those with significant soft tissue damage typically undergo treatment with a triplanar external fixator. On the other hand, younger patients with fewer comorbidities are usually directed toward ORIF via a comprehensive lateral approach. Though ORIF tends to have a higher complication rate, it is often seen as a worthwhile compromise to achieve accurate and long-term bone reconstruction [
3,
5,
7,
12,
13].
The operative approach, according to the Sanders classification, includes: Sanders type I (conservative treatment), Sanders type II and III (choice between ORIF or MIOS, depending on comorbidities and future motor requirements), and Sanders type IV (ORIF treatment or primary arthrodesis).
The chi-square analysis depicts a significant correlation between treatment selection and Sanders classification (chi-square = 11.18, p = 0.0037). This indicates that more invasive procedures, such as ORIF, are favored for complex fractures (Type III and IV). Thus, it reflects a deliberate strategy depending on the fracture’s severity and complexity.
Our department’s comparison of the ORIF and MIOS groups, which were selected based on the criteria above, supports the idea that the type of fracture impacts the choice of surgical treatment. The preference for ORIF in more severe fractures could indicate the need for a stronger approach to ensure precise anatomical repair. On the other hand, MIOS might be chosen for less complicated fractures to reduce the chances of postoperative complications in cases viewed as more manageable.
Radiographic Outcomes: The Böhler and Gissane angles, as well as the height, width, and calcaneal length, are consistently restored in both operations. ORIF treatments tend to reconstruct the Böhler angle more accurately on average. However, a high rate of postoperative complications shows that accurate anatomical reduction does not always lead to positive postoperative outcomes. This reduction is aimed at ensuring prolonged functionality and reducing the risk of postoperative osteoarthritis, a common long-term complication of MIOS treatments. This benefit is particularly significant for younger patients with Sanders II and III fractures in ORIF treatment.
Clinical and Functional Outcomes: Both the Maryland Foot Scale and CNHFA show skewed results of negative outcomes in ORIF treatments. There has been significantly lower functionality experienced in 12 of 40 cases (30%), even years after the operation. Caution should be noted, as this group included five patients with Sanders type IV fractures, a potential limiting factor. Current studies [
14] recommend percutaneous reduction using only K-wires and external fixators, as screws paired with plates frequently have difficulty grasping osteopenic or osteoporotic bone fragments.
Our t-tests revealed no significant differences in functional outcomes between ORIF and MIOS treatments, indicating that these two techniques are similarly effective in managing calcaneal fractures. The parity in functional scores suggests the choice between ORIF and MIOS may be influenced more by factors such as surgeon preference, equipment availability, or considerations relating to the patient’s specific circumstances.
Complications Impacting Quality of Life: Different types and frequencies of complications are observed in the two groups. The MIOS group has a higher frequency of osteoarthritis and chronic pain, while the ORIF group primarily faces algodystrophic, tendon, and osteomyelitis complications. Invasive hospital interventions are mainly required for the ORIF cohort. Notably, 20% of the ORIF patients over 65 with a Sanders IV classification needed reintervention for osteomyelitis, which included the removal of synthetic means. Such interventions typically follow initial treatment for surgical wound dehiscence using VAC therapy and antibiotic prophylaxis. Despite MIOS surgeries also having complications (50% osteoarthritis, 37% chronic pain), it is essential to note that these issues tend to have a chronic and slow progression compared to the ORIF group’s more acute and invasive complications.
This study examined complications arising within 5 years in ORIF and MIOS groups using an external fixator. However, long-term complications, like subtalar osteoarthritis and chronic pain in the ORIF group, were somewhat overlooked. As the referenced studies indicated, such adverse outcomes tended to surface earlier in traffic accident victims compared to those who had fallen, particularly if achieving joint congruence or restoring the Böhler angle failed. This suggests that in MIOS treatments, where the anatomical reduction often falls short, the onset of osteoarthritis can be sooner than in ORIF treatments. It is projected that if the same patients were tracked over the ensuing decade, the prevalence of complications like subtalar and calcaneo-cuboid osteoarthritis and chronic pain, currently more common in the population treated with external fixators, would equalize between the ORIF and MIOS cohorts.
Our chi-square analysis reveals comparable rates of postoperative complications between the two surgical groups, suggesting equal safety in both approaches. While minimally invasive techniques like MIOS are theoretically superior in lessening soft tissue complications, our findings fail to show a statistically significant drop in issues like tendinitis or infections. These data question the commonly held belief that minimally invasive surgery invariably leads to fewer complications, emphasizing the importance of meticulous patient selection and surgical technique.
5. Conclusions
Both ORIF and MIOS with external fixators effectively manage calcaneal fractures. Choosing between these techniques should hinge on a thorough assessment of the patient’s anatomy, clinical situation, and unique considerations. For patients having polytrauma or significant comorbidities, MIOS, particularly with external fixators, is beneficial as it limits the necessity for subsequent surgery and lowers the associated anesthesia risks. ORIF is better for patients who have a lower risk of infection complications as it allows for more accurate anatomical reconstruction and potentially decreases the occurrence of postoperative osteoarthritis. Further research with larger patient groups and extended follow-up time is needed to create precise, evidence-backed guidelines for fracture management in diverse patient populations, thereby improving long-term results and quality of life.
Author Contributions
Conceptualization, M.S. and G.T.; methodology, G.L.; software, G.M.; validation, G.T.; formal analysis, D.D.V.; investigation, F.S.; resources, M.C.; data curation, M.S.V.; writing—original draft preparation, G.L.; writing—review and editing, M.S.; visualization, G.T.; supervision, V.P.; project administration, V.P.; funding acquisition, V.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to retrospective nature of the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Schepers, T. Calcaneal Fractures: Looking Beyond the Meta-Analyses. The Journal of Foot and Ankle Surgery 2016, 55, 897–898. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, B.G.; Marsh, J.L. Minimally Invasive Treatment of Displaced Intra-Articular Calcaneal Fractures. Orthopedic Clinics of North America 2020, 51, 325–338. [Google Scholar] [CrossRef] [PubMed]
- Rammelt, S.; Swords, M.P. Calcaneal Fractures—Which Approach for Which Fracture? Orthopedic Clinics of North America 2021, 52, 433–450. [Google Scholar] [CrossRef] [PubMed]
- Shi, F.; Wu, S.; Cai, W.; Zhao, Y. Comparison of 5 Treatment Approaches for Displaced Intra-Articular Calcaneal Fractures: A Systematic Review and Bayesian Network Meta-Analysis. The Journal of Foot and Ankle Surgery 2020, 59, 1254–1264. [Google Scholar] [CrossRef] [PubMed]
- Sharr, P.J.; Mangupli, M.M.; Winson, I.G.; Buckley, R.E. Current Management Options for Displaced Intra-Articular Calcaneal Fractures: Non-Operative, ORIF, Minimally Invasive Reduction and Fixation or Primary ORIF and Subtalar Arthrodesis. A Contemporary Review. Foot and Ankle Surgery 2016, 22, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Giannini, S.; Cadossi, M.; Mosca, M.; Tedesco, G.; Sambri, A.; Terrando, S.; Mazzotti, A. Minimally-Invasive Treatment of Calcaneal Fractures: A Review of the Literature and Our Experience. Injury 2016, 47, S138–S146. [Google Scholar] [CrossRef] [PubMed]
- Lim, E.V.A.; Leung, J.P.F. Complications of Intraarticular Calcaneal Fractures: Clinical Orthopaedics and Related Research 2001, 391, 7–16. 391. [CrossRef]
- Clare, M.P.; Crawford, W.S. Managing Complications of Calcaneus Fractures. Foot and Ankle Clinics 2017, 22, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Schepers, T.; Van Lieshout, E.M.M.; Ginai, A.Z.; Mulder, P.G.H.; Heetveld, M.J.; Patka, P. Calcaneal Fracture Classification: A Comparative Study. The Journal of Foot and Ankle Surgery 2009, 48, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Majeed, H.; Barrie, J.; Munro, W.; McBride, D. Minimally Invasive Reduction and Percutaneous Fixation versus Open Reduction and Internal Fixation for Displaced Intra-Articular Calcaneal Fractures: A Systematic Review of the Literature. EFORT Open Reviews 2018, 3, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Kline, A.J.; Anderson, R.B.; Davis, W.H.; Jones, C.P.; Cohen, B.E. Minimally Invasive Technique Versus an Extensile Lateral Approach for Intra-Articular Calcaneal Fractures. Foot Ankle Int. 2013, 34, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Vicenti, G.; Carrozzo, M.; Solarino, G.; Caizzi, G.; De Crescenzo, A.; Portaluri, M.; Mori, C.M.; Vittore, D.; Moretti, B. Comparison of Plate, Calcanealplasty and External Fixation in the Management of Calcaneal Fractures. Injury 2019, 50, S39–S46. [Google Scholar] [CrossRef] [PubMed]
- Selim, A.; Ponugoti, N.; Chandrashekar, S. Systematic Review of Operative vs Nonoperative Treatment of Displaced Intraarticular Calcaneal Fractures. Foot & Ankle Orthopaedics 2022, 7, 24730114221101609. [Google Scholar] [CrossRef] [PubMed]
- Wei, N.; Zhou, Y.; Chang, W.; Zhang, Y.; Chen, W. Displaced Intra-Articular Calcaneal Fractures: Classification and Treatment. Orthopedics 2017, 40. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).