Background
Osteoarthritis (OA) is a painful and debilitating condition and is the most common musculoskeletal condition in older adults [
1]. According to Arthritis Research UK, in England, approximately 1 in 5 adults over 45 years have OA of the knee and 1 in 9 OA of the hip [
2], while another study claimed that the overall prevalence of OA of the hip and knee was higher (knee: 2.9%, 95%CI: 2.7 to 2.9 and hip: 1.5%, 95%CI: 1.4 to 1.5) [
3].
Furthermore, OA stands a strain on scarce resources. In the UK, the total healthcare cost of OA is estimated to be over £1 billion [
4]. Based on an observational retrospective study designed to estimate resource utilisation and costs in UK patients with moderate to severe OA pain, direct cost of healthcare at 12 months was £2,519 in patients with moderate to severe OA pain and £3,389 for those with severe OA pain [
5].
Whilst treatment and management of OA involve a multidisciplinary approach and various management options, including patient education and self-management, and pharmacological and non-pharmacological treatments [
6], individuals diagnosed with this condition frequently progress to needing a joint arthroplasty.
There is strong published evidence showing that THA and TKA are highly effective, in reducing pain symptoms and functional limitations in most patients [
7,
8], in addition to being cost-effective [
9,
10]. Over 100,000 THA and TKA operations are carried out each year in the UK [
11]. These numbers are projected to increase with both an increase in national life expectancy and in the prevalence of obesity adding even further pressure on NHS funding and capacity [
12]. Additionally, 10% of patients who have received a THA or TKA have gait abnormalities one-year post-operation [
13].
This is a result of a lack of objective assessment data of post-operation gait, leaving patients to continue the walking pattern they had adapted before the operation to avoid pain in the arthritic joint thereby creating abnormalities in their gait post-operation. Patients need to retrain their walking by strengthening weakened muscles, as by continuing the incorrect walking pattern, many continue to strain the joints and use muscles incorrectly [
14]. This can lead to falls, reduced activity, or pain in other joints.
GS is a digital medical device (CE-marked class 1M medical device) that uses patient-connected motion sensors and an artificial intelligence algorithm to provide objective gait data from which personalised rehabilitation can be effectively delivered and monitored. This study aimed to conduct an economic evaluation to determine the cost-effectiveness of the GS system compared with the current SoC in people undergoing THA or TKA with gait and mobility issues.
Methods
We estimated the cost-effectiveness of the GS system compared with the current SoC in people undergoing THA or TKA with gait and mobility issues in the UK. The main aspects of the analysis were summarised according to the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 statement to increase the transparency of the proposed study [
15].
The pilot randomized controlled trial (RCT) was funded by Innovate UK under the Digital Health programme, whose role was to ensure the project was correctly managed. This pilot study was designed as a parallel group RCT to assess how a fully automated personalised exercise intervention (using GS) compared to standard physiotherapy (SoC) as defined in National Institute for Health Care and Excellence (NICE) Guideline QS206 [
16]. Patients were recruited from Norfolk and Norwich University Hospital (NNUH) and approved by the institutional ethics committee. All subjects had undergone hip or knee replacement using standard implants and surgical techniques. Furthermore, all patients received routine inpatient physiotherapy until discharged and then up to 6-8 weeks post-operatively. Patients were screened for eligibility criteria at 6-8 weeks post-operatively. The primary outcome measure was the change in the patient's gait speed. This is a universally recognised measure, with established values for Mean Detectable Change (MDC) of 0.05m/s and minimally clinically significant change of 0.1m/s [
17].
We conducted an economic evaluation using data from the pilot RCT. Clinical outcome at the start of the trial (17 weeks) was measured by the change in the patient's gait speed. Health utilities were used to calculate quality-adjusted life-years (QALYs) over the clinical trial period. Resource use estimates collected during the trial included physiotherapy, follow-up cost, and cost of treatment with GS and best SoC. Unit costs were obtained from the Personal Social Services Research Unit (PSSRU) [
18] and applied to resource use. All the cost were inflated to 2023 GBP for the analyses.
The study population comprised participants who were approached at their pre-operative appointment by a member of the research team and consented to participate in the GS RCT. The target population was adults who met the following criteria: patients aged 18 years or older, undergoing THA or TKA with gait and mobility issues.
The study managed to recruit 44 participants, with 22 allocated to the intervention group (average age: 67.4 years, male proportion: 50%, average BMI: 31.05) and 22 allocated to the SoC group (average age: 72.3 years, male proportion: 50%, average BMI: 29.08).
From the NHS perspective, the economic model estimated the relative cost-effectiveness of GS compared with SoC for improving gait and mobility issues in people undergoing THA or TKA, adhering to good practice guidelines [
15] and the NICE reference case [
19]. Therefore, only healthcare costs (direct medical costs) related to the disease were included.
The GS is a sensor-based digital medical device (CE Marked Class 1M Medical Device). Using an algorithm, GS provides a detailed and objective measure of a patient's walking ability, in which the collected data are used to automatically define a personalized exercise program. Patients assigned to the intervention group (GS) were monitored four times during the implementation of the intervention, three weeks apart. All exercises were recommended either in the Otago Exercise Program (OEP) or in the NHS older people guidance, as per current appropriate practice. All interventions were delivered by the research team. Training of the research team was undertaken by Dynamic Metrics. To deliver the intervention, a 20-metre quiet (discrete) straight corridor was used, and patients wore flat or low-heeled shoes with proper support. Patients were instructed to use the same footwear at each appointment when possible.
Patients in the SoC group received postoperative rehabilitation according to the NICE Quality Standard (QS 206) [
16]. All patients were advised on self-directed rehabilitation. Those who had difficulties managing activities of daily living with an ongoing functional impairment or felt that they were not achieving their goals through self-directed rehabilitation were offered group or individual outpatient rehabilitation.
Cost-effectiveness was expressed as the incremental cost-effectiveness ratio (ICER). Monte Carlo simulation was used to calculate 95% confidence intervals for the estimated difference in mean cost and QALYs between intervention groups.
As the benefit of the GS system is usually seen over a short-term, our analysis was performed over a seventeen-week time horizon - alongside the pilot GS RCT to estimate the cost-effectiveness results. This time horizon was also chosen because it is similar to the time frame in which patients receive physiotherapy (SoC) in current practice after THA and TKA. Given that our analytic time horizon was lower than 12 months, a discount rate was not applied to the costs and benefits.
The economic model informed by a previously published early economic model [
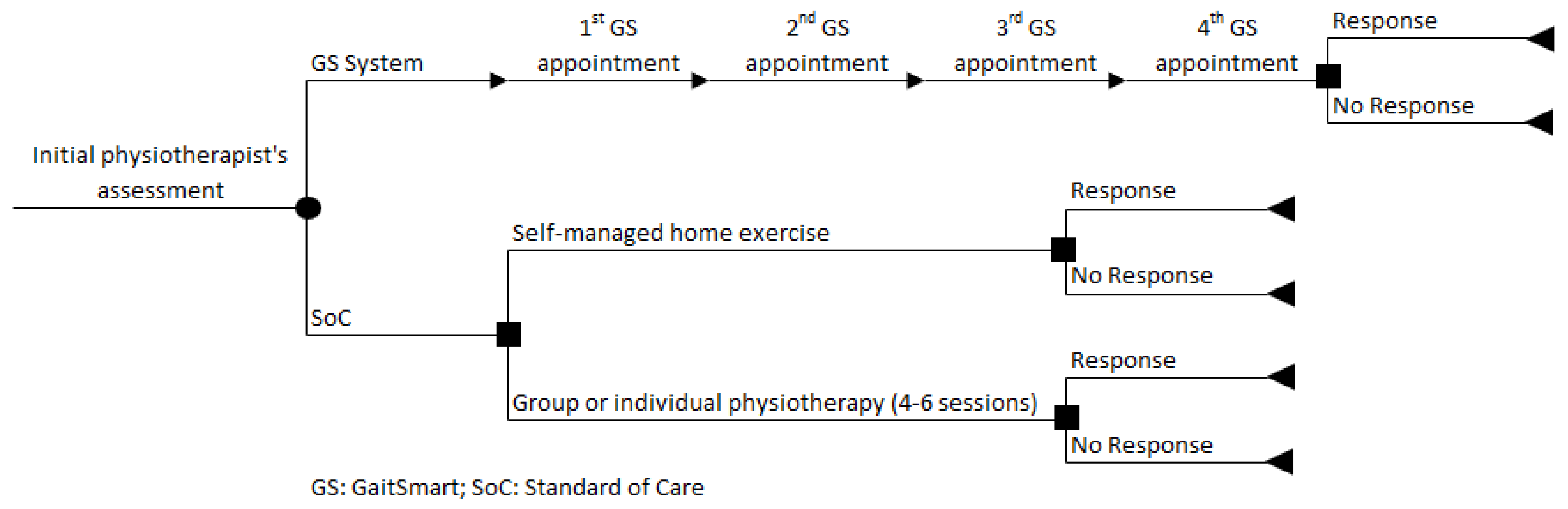
20] and is in line with the current clinical pathway described for patients undergoing THA or TKA who are eligible for SoC, according to the guidance set out by NICE (
Figure 1). The seventeen weeks (GS RCT period) are represented by a decision tree model, developed in Microsoft Excel 2013. In summary, patients assigned to the GS group were monitored four times, three weeks apart, while patients assigned to the SoC group were not monitored with GS and could be allocated to receive either self-managed home exercise or group or individual physiotherapy (4-6 sessions). At the end of the path, each branch of the decision tree provides the outcomes of the model (response or no response).
The decision tree modelling approach was considered appropriate as, according to expert opinion, there were no recurrent physiotherapy sessions if the patients did not respond to the initial sessions after the operation.
Results
Cost-effectiveness results found that GS compared to the SoC had a total cost of £67.00, compared to the SoC total cost of £517.56 (
Table 2). Over a seventeen-week time horizon, the QALYs gained in the intervention group were 0.28, compared with 0.26 in the control group. This equates to a cost savings of £450.56 and an incremental 0.02 QALYs gained from the use of GS. . Therefore, the GS system is the dominant strategy because it shows to be more effective and less costly compared to the SoC for improving gait and mobility issues in people undergoing THA or TKA.
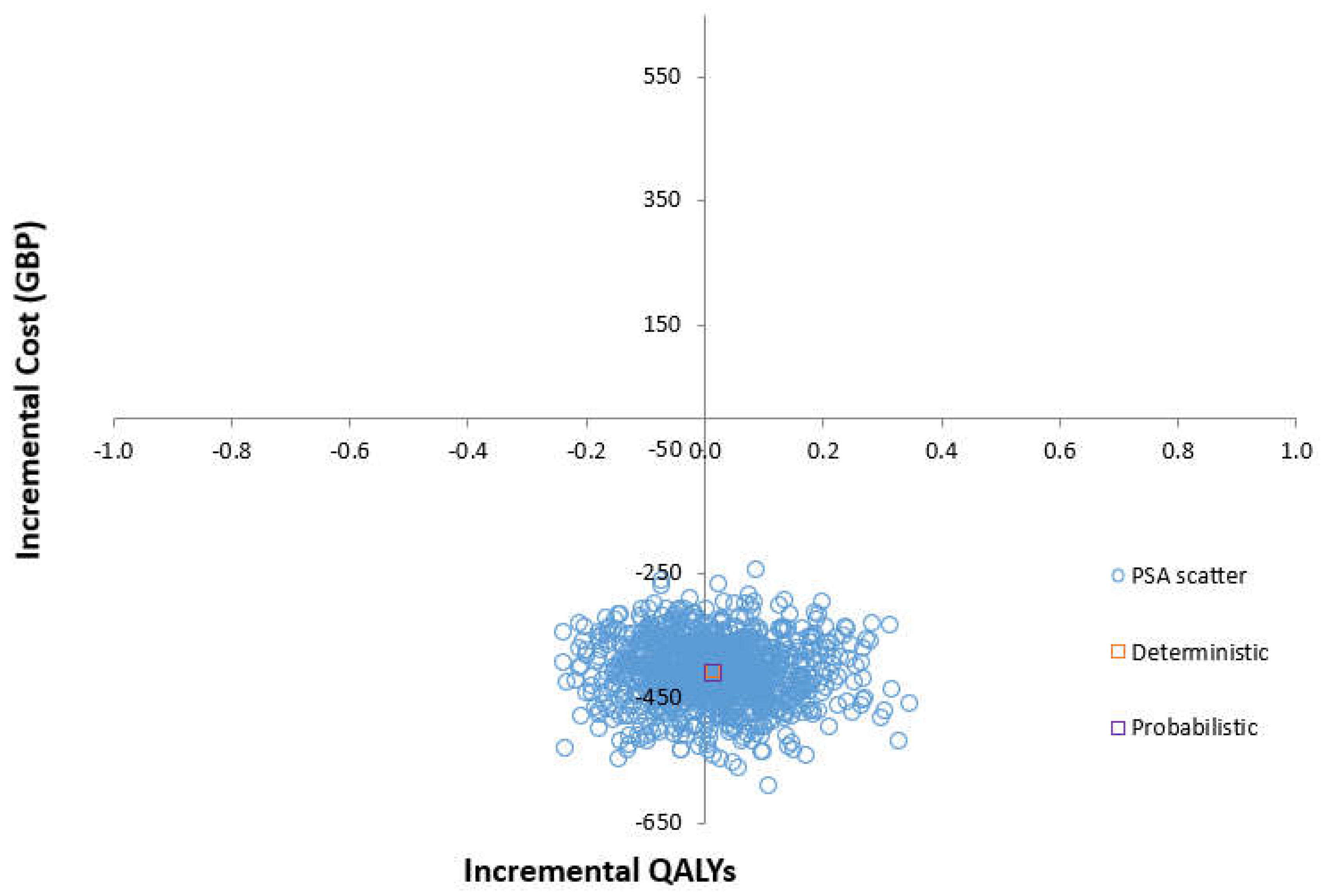
The cost-effectiveness plane shows the results of running the model 1000 times and recording the difference in cost and effectiveness between the GS and SoC (
Figure 2). Using 1,000 Monte-Carlo simulations, PSA has shown that at a willingness to pay (WTP) of £20,000, the GS system is dominant over SoC in improving gait and mobility issues in people undergoing THA and TKA (
Supplementary Table S1). Although most data points are observed in the southeast quadrant of the plane (representing the scenario of ‘less costly and more effective’, that is, a dominant strategy), there is considerable uncertainty surrounding the extent and existence of the additional expected costs and of the additional expected QALYs.
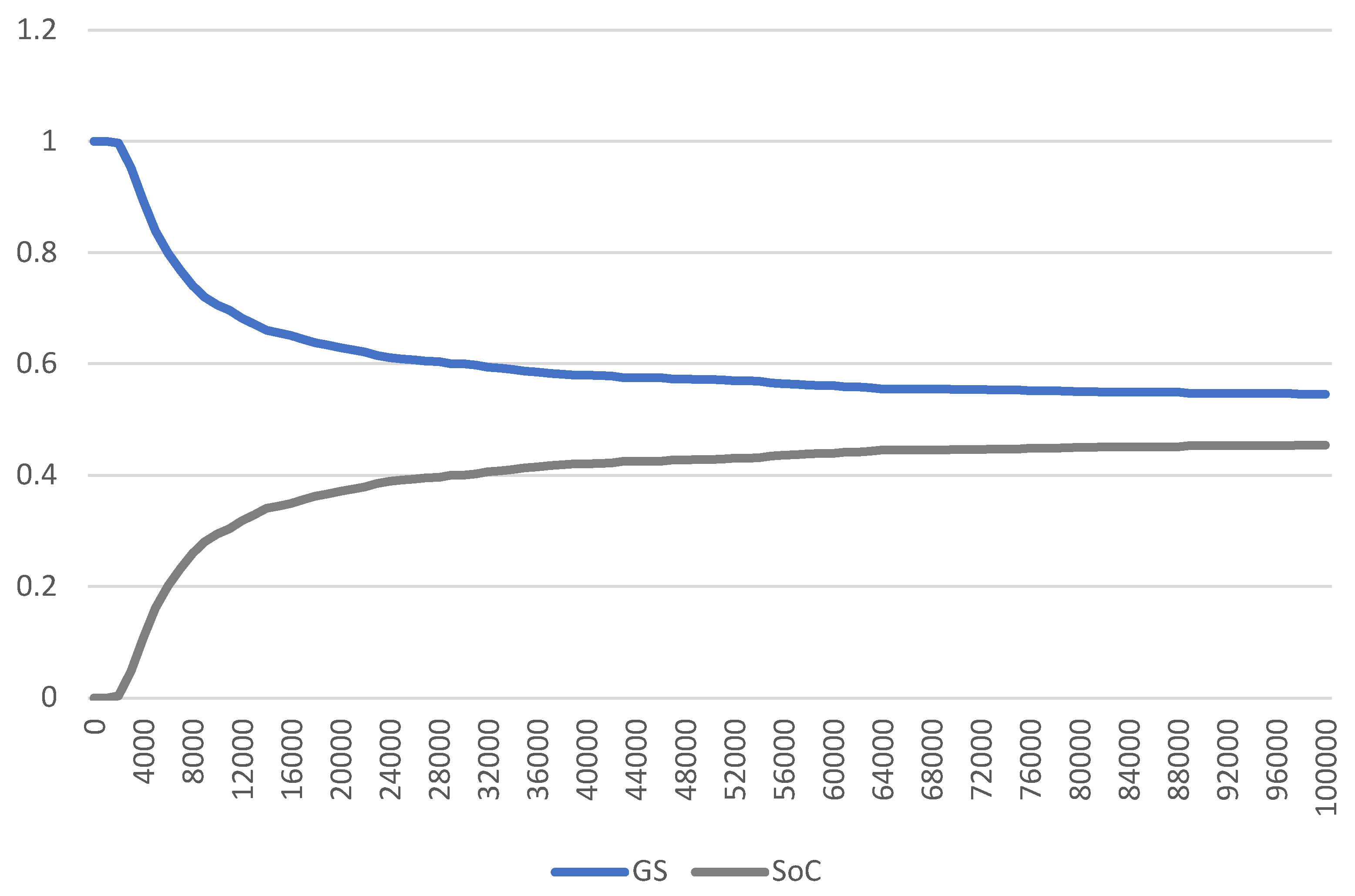
The CEAC shows the probability of GS being cost-effective for different levels of willingness-to-pay thresholds, compared with SoC (
Figure 3). The CEAC shows that, at a willingness-to-pay threshold of £20,000 per QALY gained, GS has a 60.9% probability of being cost-effective, compared with SoC.
Discussion
Our results indicate that the GS, compared with the SoC, meets the standard criteria to be considered a cost-effective use of resources in a UK health service setting. There are a limited number of studies focusing on the cost-effectiveness analysis of rehabilitation forms following THA or TKA. To the best of our knowledge, this is the first study assessing the cost-effectiveness of the GS system for THA or TKA patients, which limits the comparison of our results with those from literature. However, our study results were consistent with other economic evaluations that evaluated different rehabilitation components for patients with THA or TKA, suggesting that the GS is more effective and cost saving for the health system compared to usual care [
22,
23,
24].
Overall, regardless of these limitations, the current study adds to this body of evidence that the use of GS in clinical practice for the rehabilitation of patients undergoing THA or TKA seems to be cost-effective. Sensitivity analysis performed to evaluate our assumptions regarding the input parameters indicated that even when we range the input values around the mean, the GS system remains a more cost-effective option.
The main strength of the study is that all input parameters used in the model, such as resource use, probabilities, and costs, are real-life parameters retrieved at the individual level from the GS RCT funded by Innovate UK, which supports the reliability and validity of these parameters. The main limitation of the study is that the GS RCT had low subject numbers included, which did not allow us to perform a subgroup analysis as the subgroups' statistical power would have been very low. Another limitation was the lack of follow-up protocol and data. These limitations should be addressed in future RCTs.
In the current study, healthcare costs per QALY were assessed over a 17-week horizon (GS RCT period). OA is a long-term chronic condition [
25], so analysing cost-effectiveness over a seventeen-week horizon is a relatively short time horizon, warranting further long-term cost-effectiveness analyses. However, a model-based cost-effectiveness analysis suggested that a physical activity program for patients with knee OA would lead to favourable long-term clinical and economic benefits. Therefore, the clinical and economic benefits observed in our study could be even greater over a longer-term horizon.
Clinical guidelines by the NICE in the UK recommend a multidisciplinary and integrated approach to the assessment and management of osteoarthritis [
6]. The guidelines advocate for patient education and self-management to enhance understanding of the condition and its management. Unfortunately, the information on economic analyses in the guidelines is restricted to pharmacological and conventional treatments. Therefore, it is recommended that guidelines should also include economic evaluations of interventions aimed at the rehabilitation of patients undergoing THA and TKA.
This study limited the analysis to the NHS perspective, following the NICE reference case [
19]. However, it should be noted that a large proportion of the economic burden of OA is related to indirect costs and productivity losses [
4]. Therefore, the societal perspective has the potential to capture all important impacts on the whole society. Some guidelines suggest that due to the chronic nature of OA, a broader societal perspective should be considered in the economic analyses [
26]. Thus, considering the societal perspective within the sensitivity analysis could provide a better picture of the true burden associated with OA.
Conclusion
Our economic evaluation results indicate that the GS system may be a dominant strategy (delivering lower costs and improving the quality-of-life outcomes) compared to the current SoC. Even under less favourable assumptions, where the parameters with the highest level of uncertainty were varied, the GS showed to be a cost-effective alternative, assuming a £20,000 WTP threshold.
Thus, our cost-effectiveness analysis suggests that GS in patients undergoing THA and TKA with gait and mobility issues is also potentially cost saving compared to SoC, reducing costs by £ £450.56 per patient. Policymakers and practitioners should consider the possible cost benefits of introducing GS as an alternative to the current practice and support further studies to strengthen the generalisability of the current findings.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Supplementary Table S1. Probabilistic sensitivity results comparing GS versus SoC.
Acknowledgements and Sources of Funding
We thank the Innovate UK for funding the GaitSmart randomised controlled trial. We would also like to thank DML for GaitSmart data and data collection. The funder did not have any role in the design, analysis, and interpretation of the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lee, W.; Nims, R.J.; Savadipour, A.; Zhang, Q.; Leddy, H.A.; Liu, F.; McNulty, A.L.; Chen, Y.; Guilak, F.; Liedtke, W.B. Inflammatory signaling sensitizes Piezo1 mechanotransduction in articular chondrocytes as a pathogenic feed-forward mechanism in osteoarthritis. Proceedings of the National Academy of Sciences 2021, 118, e2001611118. [Google Scholar] [CrossRef] [PubMed]
- Public Health England; Arthritis Research UK. Prevalence of osteoarthritis in England and local authorities: Birmingham; 2024 Feb 17, 2014.
- Swain, S.; Sarmanova, A.; Mallen, C.; Kuo, C.; Coupland, C.; Doherty, M.; et al. Trends in incidence and prevalence of osteoarthritis in the United Kingdom: findings from the Clinical Practice Research Datalink (CPRD). Osteoarthr Cartil 2020, 28, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.; Gupte, C.; Akhtar, K.; Smith, P.; Cobb, J. The Global Economic Cost of Osteoarthritis: How the UK Compares. Arthritis 2012, 2012, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Abraham, L.; Halsby, K.; Stein, N.; Wrona, B.; Emir, B.; Stevenson, H. An Observational Retrospective Matched Cohort Study of Healthcare Resource Utilisation and Costs in UK Patients with Moderate to Severe Osteoarthritis Pain. Rheumatol Ther 2022, 9, 851–874. [Google Scholar] [CrossRef] [PubMed]
- Health, N.I.f.; Excellence, C. Osteoarthritis in over 16s: diagnosis and management | Guidance. Availabe online: https://www.nice.org.uk/guidance/ng226 (accessed on.
- Ethgen, O.; Bruyerè, O.; Richy, F.; Dardennes, C.; Reginster, J. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 2004, 86, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.; Sledge, C. Total hip and total knee replacement (1). N Engl J Med 1990, 323, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Daigle, M.; Weinstein, A.; Katz, J.; Losina, E. The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best Pract Res Clin Rheumatol 2012, 26, 649–658. [Google Scholar] [CrossRef] [PubMed]
- Dakin, H.; Gray, A.; Fitzpatrick, R.; MacLennan, G.; Murray, D. Rationing of total knee replacement: a cost-effectiveness analysis on a large trial data set. BMJ Open 2012, 2. [Google Scholar] [CrossRef] [PubMed]
- Brittain, R.; Howard, P.; Lawrence, S.; Stonadge, J.; Wilkinson, M.; Wilton, T.; et al. NJR statistical analysis, support and associated services National Joint Registry | 19th Annual Report; 2024 Mar 1.
- Culliford, D.; Maskell, J.; Judge, A.; Cooper, C.; Prieto-Alhambra, D.; Arden, N. Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthr Cartil 2015, 23, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Heath, E.; Ackerman, I.; Cashman, K.; Lorimer, M.; Graves, S.; Harris, I. Patient-reported outcomes after hip and knee arthroplasty: results from a large national registry. Bone Jt Open 2021, 2, 422–432. [Google Scholar] [CrossRef] [PubMed]
- Dash, S.; Palo, N.; Arora, G.; Chandel, S.; Kumar, M. Effects of preoperative walking ability and patient’s surgical education on quality of life and functional outcomes after total knee arthroplasty. Rev Bras Ortop 2017, 52, 435. [Google Scholar] [CrossRef] [PubMed]
- Husereau, D.; Drummond, M.; Augustovski, F.; de Bekker-Grob, E.; Briggs, A.; Carswell, C.; et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) Statement: Updated Reporting Guidance for Health Economic Evaluations. Value Health 2022, 25, 3–9. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health Care Excellence. Joint replacement (primary): hip, knee and shoulder | Quality standards - 206. Availabe online: https://www.nice.org.uk/guidance/qs206 (accessed on.
- Abellan Van Kan, G.; Rolland, Y.; Andrieu, S.; Bauer, J.; Beauchet, O.; Bonnefoy, M.; et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging 2009, 13, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Curtis, L.A.; Burns, A. Unit Costs of Health and Social Care 2020 | PSSRU; 2024 Feb 22, 2020.
- National Institute for Health Care Excellence. NICE Health Technology Evaluations: The Manual | Guidance. Availabe online: https://www.nice.org.
- Zanghelini, F.; Xydopoulos, G.; Fordham, R.; Rodgers, G.; Khanal, S. Early economic evaluation of the digital gait analysis system for fall prevention–Preliminary analysis of the GaitSmart system. Aging Medicine 2024. [Google Scholar] [CrossRef] [PubMed]
- I, M.; CE, W.; N, W.; D, H.; R, W. Sensor Data-Driven Personalised Hip and Knee Replacement Rehabilitation Compared to Standard of Care, Pilot Randomized Trial. British Journal of Healthcare and Medical Research 2023, 10, 54–71. [Google Scholar] [CrossRef]
- Bolz, K.M.D.; Crawford, R.W.; Donnelly, B.; Whitehouse, S.L.; Graves, N. The cost-effectiveness of routine follow-up after primary total hip arthroplasty. The Journal of arthroplasty 2010, 25, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Fusco, F.; Campbell, H.; Barker, K. Rehabilitation after resurfacing hip arthroplasty: cost-utility analysis alongside a randomized controlled trial. Clinical Rehabilitation 2019, 33, 1003–1014. [Google Scholar] [CrossRef] [PubMed]
- Fusco, F.; Turchetti, G. Telerehabilitation after total knee replacement in Italy: cost-effectiveness and cost-utility analysis of a mixed telerehabilitation-standard rehabilitation programme compared with usual care. BMJ open 2016, 6, e009964. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; March, L.; Chew, M. Osteoarthritis in 2020 and beyond: a Lancet Commission. The Lancet 2020, 396, 1711–1712. [Google Scholar] [CrossRef] [PubMed]
- Hiligsmann, M.; Cooper, C.; Arden, N.; Boers, M.; Branco, J.C.; Brandi, M.L.; Bruyère, O.; Guillemin, F.; Hochberg, M.C.; Hunter, D.J. Health economics in the field of osteoarthritis: an expert's consensus paper from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). In Proceedings of Seminars in arthritis and rheumatism; pp. 303–313.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).