Submitted:
19 May 2024
Posted:
20 May 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
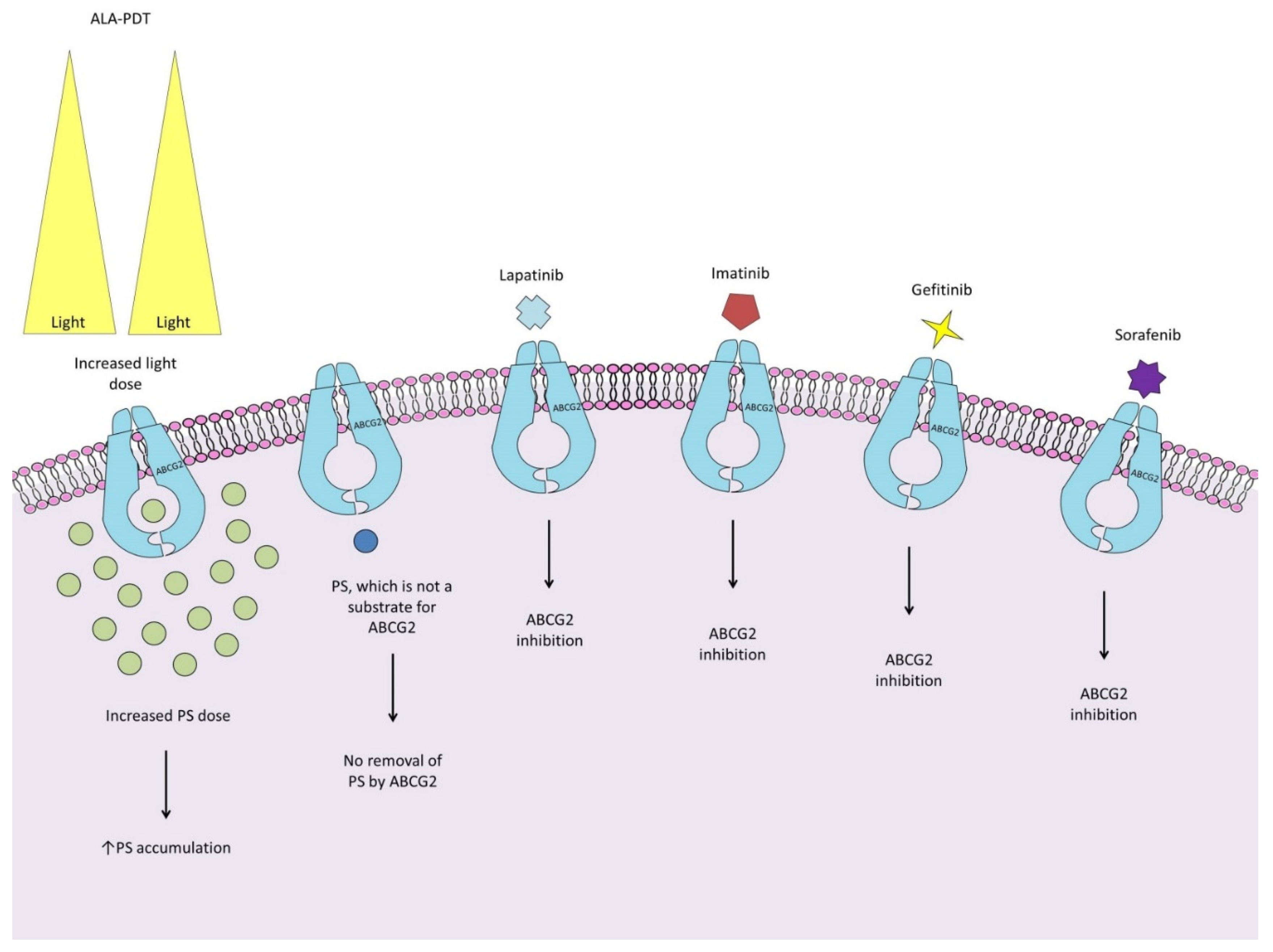
2. Adenosine Triphosphate (ATP)-Binding Cassette Efflux Transporter G2
3. Glutathione
4. Ferrochelatase
5. Heme Oxygenase 1
6. Hypoxia-Inducible Factor 1 α
7. Histone Deacetylases
8. Protein Kinase C
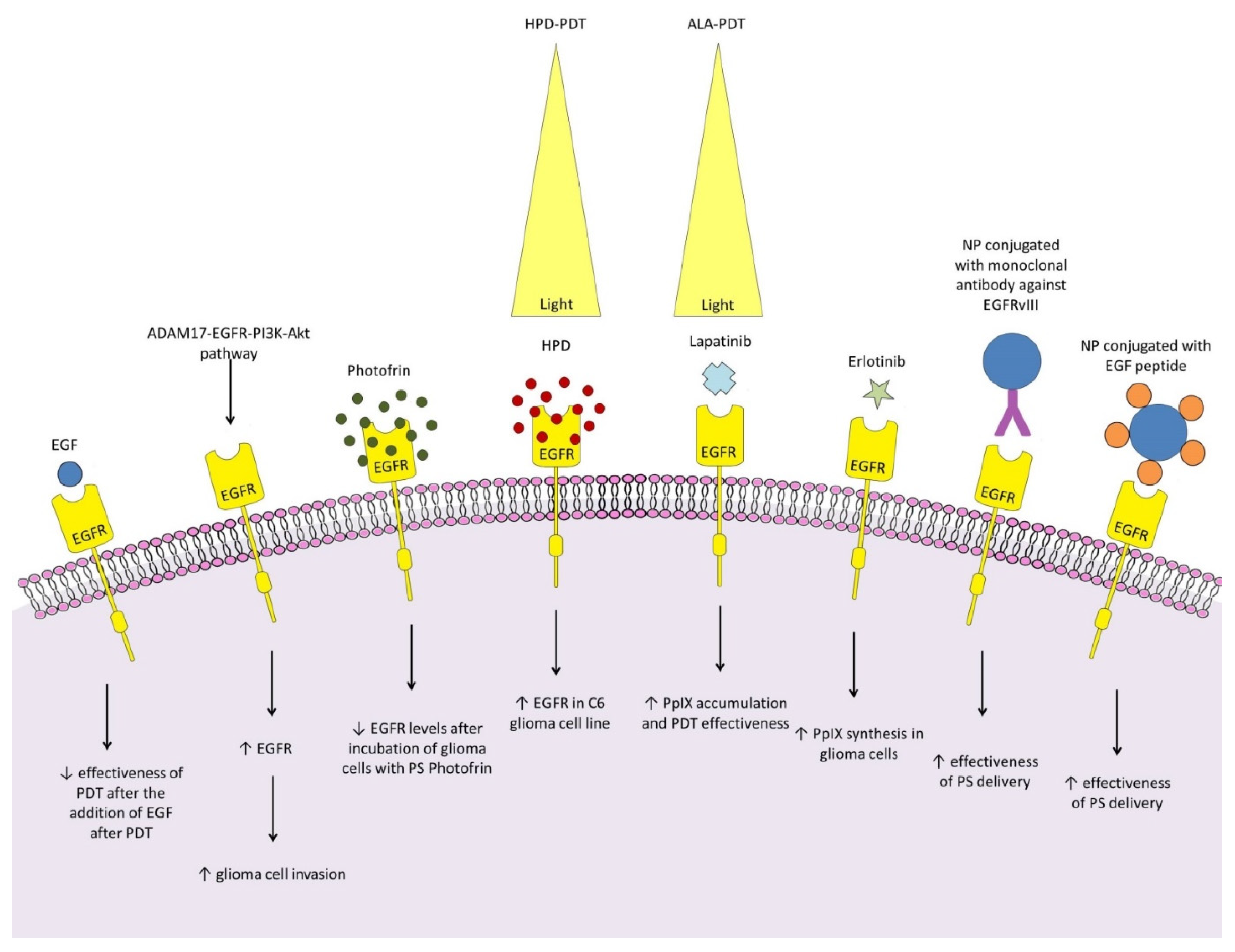
9. Epidermal Growth Factor Receptor
10. Fibroblast Growth Factors
11. Hepatocyte Growth Factor
12. Vascular Endothelial Growth Factor
13. Neuropilin-1
| Molecular target | Targeting method | Article |
|---|---|---|
| EGFR | Monoclonal antibody against EGFRvIII | Jamali et al. [103] |
| EGFR | EGF peptide | Meyers JD et al. [104] |
| Neuropilin-1 | ATWLPPR heptapeptide targeting NRP-1 | Thomas et al. [137] Tirand et al. [138] Bechet et al. [139] Tirand et al. [142] Thomas et al. [143] |
| Neuropilin-1 | KDKPPR peptide targeting NRP-1 | Gries et al. [140] Thomas et al. [141] |
| Neuropilin-1 Integrin αvβ3 Integrin αvβ5 |
RGD internalizing peptide targeting NRP1, INT αvβ3 and αvβ5 | Lu et al. [144] |
| Integrin αvβ3 | Modified monoclonal antibody against INT αvβ3 | Wei et al. [157] |
| Neuropeptide Y receptor 1 | Neuropeptide Y type D | He et al. [255] |
| Low-density lipoprotein receptor | Low density lipoprotein | Andreazza et al. [269] Huntosova et al. [270] |
| Extra domain A of fibronectin (ED A) | Ligand targeting epitope ED A small immunoprotein antibody F8 | Acker et al. [281] |
| US28 protein | Nanoprotein binding discontinuous epitope US28 with high affinity | De Groof et al. [282] |
| Nucleolin | Single-stranded DNA aptamer AS1411 with high affinity for nucleolin | Zhu et al. [283] |
| Transferrin receptor | Transferrin | Zhu et al. [283] |
| Cell nucleus | T-ag antigen variants of SV40 virus | Akhlynina et al. [284] |
14. Vascular Cell Adhesion Protein 1
15. Integrins
16. Matrix Metalloproteinases
17. Glial Fibrillary Acidic Protein
18. Na+ /H+ Exchanger Isoform 1
19. Nuclear Factor kB
20. Transporter Associated with Antigen Processing 1
21. PD-L1/PD-1
22. Nitric Oxide Synthase
23. Glutamate
24. Peripheral-Type Benzodiazepine Receptors
25. Neuropeptide Y Receptors
| Neurotransmitter | NS levels | Receptor expression | Impact on the effectiveness of PDT | Tested therapeutic approach |
|---|---|---|---|---|
| NO | Increase [231,232,233] | No data available | Increased resistance, survival and migration of glioma cells after PDT [191,231,232,233] | Association of PDT with iNOS inhibitors reduces NO levels and glioma cell growth and invasion after PDT [232] |
| Glutaminian | Increase [237] | Increase in AMPAR expression [237,239] | Increase in apoptosis of glioma cells [237,239] | No data available |
| GABA | No data available | Increase in PBR expression [245] | Increased production of PpIX and phototoxic effect against glioma cells (via increase in PBR) [245] | Association of PDT with diazepam enhances apoptosis of glioma cells [247] |
| Neuropeptide Y | No data available | No data available | No data available | NP coupling with NPY improves targeting and PS delivery in the glioma [255] |
26. Receptor-Interacting Serine/Threonine Kinases
27. Low-Density Lipoprotein Receptor
28. GLUT Glucose Transporters
29. Other Molecules and Pathways
Author Contributions
Conflicts of Interest
References
- Schwartz, S.M. Epidemiology of Cancer. Clinical Chemistry 2024, 70, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Laversanne, M.; Weiderpass, E.; Soerjomataram, I. The ever-increasing importance of cancer as a leading cause of premature death worldwide. Cancer. 2021, 127, 3029–3030. [Google Scholar] [CrossRef] [PubMed]
- Vigneswaran, K.; Neill, S.; Hadjipanayis, C.G. Beyond the World Health Organization grading of infiltrating gliomas: Advances in the molecular genetics of glioma classification. Ann Transl Med. 2015, 3, 95. [Google Scholar] [PubMed]
- Davis, M.E. Epidemiology and Overview of Gliomas. Semin Oncol Nurs. 2018, 34, 420–429. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.M.; Englander, Z.K.; Miller, M.L.; Bruce, J.N. Malignant Glioma. Adv Exp Med Biol. 2023, 1405, 1–30. [Google Scholar] [PubMed]
- Jakola, A.S.; Myrmel, K.S.; Kloster, R.; Torp, S.H.; Lindal, S.; Unsgård, G.; Solheim, O. Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA. 2012, 308, 1881–1888. [Google Scholar] [CrossRef] [PubMed]
- Stupp, R.; Taillibert, S.; Kanner, A.; Read, W.; Steinberg, D.; Lhermitte, B.; Toms, S.; Idbaih, A.; Ahluwalia, M.S.; Fink, K.; Di Meco, F.; Lieberman, F.; Zhu, J.J.; Stragliotto, G.; Tran, D.; Brem, S.; Hottinger, A.; Kirson, E.D.; Lavy-Shahaf, G.; Weinberg, U.; Kim, C.Y.; Paek, S.H.; Nicholas, G.; Bruna, J.; Hirte, H.; Weller, M.; Palti, Y.; Hegi, M.E.; Ram, Z. Effect of Tumor-Treating Fields Plus Maintenance Temozolomide vs Maintenance Temozolomide Alone on Survival in Patients With Glioblastoma: A Randomized Clinical Trial. JAMA. 2017, 318, 2306–2316. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Wee, C.W. Treatment of Adult Gliomas: A Current Update. Brain Neurorehabil. 2022, 15, e24. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Wu, Z.; Zhang, H.; Zhang, N.; Wu, W.; Wang, Z.; Dai, Z.; Zhang, X.; Zhang, L.; Peng, Y.; Ye, W.; Zeng, W.; Liu, Z.; Cheng, Q. Glioma targeted therapy: Insight into future of molecular approaches. Mol Cancer. 2022, 21, 39. [Google Scholar] [CrossRef]
- Bush, N.A.; Chang, S.M.; Berger, M.S. Current and future strategies for treatment of glioma. Neurosurg Rev. 2017, 40, 1–14. [Google Scholar] [CrossRef]
- Vermandel, M.; et al. Standardized intraoperative 5-ALA photodynamic therapy for newly diagnosed glioblastoma patients: A preliminary analysis of the INDYGO clinical trial. Journal of neuro-oncology 2021, 152, 501–514. [Google Scholar] [CrossRef] [PubMed]
- Kwiatkowski, S.; Knap, B.; Przystupski, D.; Saczko, J.; Kędzierska, E.; Knap-Czop, K.; Kotlińska, J.; Michel, O.; Kotowski, K.; Kulbacka, J. Photodynamic therapy - mechanisms, photosensitizers and combinations. Biomed Pharmacother. 2018, 106, 1098–1107. [Google Scholar] [CrossRef] [PubMed]
- Mansoori, B.; Mohammadi, A.; Amin Doustvandi, M.; Mohammadnejad, F.; Kamari, F.; Gjerstorff, M.F.; Baradaran, B.; Hamblin, M.R. Photodynamic therapy for cancer: Role of natural products. Photodiagnosis Photodyn Ther. 2019, 26, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Aebisher, D.; Przygórzewska, A.; Myśliwiec, A.; Dynarowicz, K.; Krupka-Olek, M.; Bożek, A.; Kawczyk-Krupka, A.; Bartusik-Aebisher, D. Current Photodynamic Therapy for Glioma Treatment: An Update. Biomedicines 2024, 12, 375. [Google Scholar] [CrossRef] [PubMed]
- Kukal, S.; Guin, D.; Rawat, C.; Bora, S.; Mishra, M.K.; Sharma, P.; Paul, P.R.; Kanojia, N.; Grewal, G.K.; Kukreti, S.; Saso, L.; Kukreti, R. Multidrug efflux transporter ABCG2: Expression and regulation. Cell Mol Life Sci. 2021, 78, 6887–6939. [Google Scholar] [CrossRef] [PubMed]
- Morgan, J.; Petrucci, C.M. The effect of ALA/PpIX PDT on putative cancer stem cells in tumor side populations. Kessel D, editor. 12TH WORLD CONGRESS OF THE INTERNATIONAL PHOTODYNAMIC ASSOCIATION: PHOTODYNAMIC THERAPY: BACK TO THE FUTURE. 1000 20TH ST, PO BOX 10, BELLINGHAM, WA 98227-0010 USA: SPIE-INT SOC OPTICAL ENGINEERING; 2009. (Proceedings of SPIE; vol. 7380).
- Mueller, P.; Gaber, S.A.A.; Zimmermann, W.; Wittig, R.; Stepp, H. ABCG2 influence on the efficiency of photodynamic therapy in glioblastoma cells. Vol. 210, JOURNAL OF PHOTOCHEMISTRY AND PHOTOBIOLOGY B-BIOLOGY. PO BOX 564, 1001 LAUSANNE, SWITZERLAND: ELSEVIER SCIENCE SA; 2020.
- Pan, L.; Lin, H.; Tian, S.; Bai, D.; Kong, Y.; Yu, L. The Sensitivity of Glioma Cells to Pyropheophorbide-αMethyl Ester-Mediated Photodynamic Therapy Is Enhanced by Inhibiting ABCG2. Vol. 49, LASERS IN SURGERY AND MEDICINE. 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY; 2017. p. 719–26.
- Weidner, L.D.; Zoghbi, S.S.; Lu, S.; Shukla, S.; Ambudkar, S.V.; Pike, V.W.; Mulder, J.; Gottesman, M.M.; Innis, R.B.; Hall, M.D. The Inhibitor Ko143 Is Not Specific for ABCG2. J Pharmacol Exp Ther. 2015, 354, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Wang W, Tabu K, Hagiya Y, Sugiyama Y, Kokubu Y, Murota Y, Ogura S ichiro, Taga T. Enhancement of 5-aminolevulinic acid-based fluorescence detection of side population-defined glioma stem cells by iron chelation. vol. 7, scientific reports. macmillan building, 4 crinan st, london n1 9xw, england: Nature publishing group; 2017.
- Abdel Gaber, S.A.; Müller, P.; Zimmermann, W.; Hüttenberger, D.; Wittig, R.; Abdel Kader, M.H.; Stepp, H. ABCG2-mediated suppression of chlorin e6 accumulation and photodynamic therapy efficiency in glioblastoma cell lines can be reversed by KO143. J Photochem Photobiol B. 2018, 178, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Hamid, S.A.; Zimmermann, W.; Huettenberger, D.; Wittig, R.; Kader, M.A.; Stepp, H. In vitro Study for Photodynamic Therapy using Fotolon® in Glioma Treatment. Lilge L, Sroka R, editors. MEDICAL LASER APPLICATIONS AND LASER-TISSUE INTERACTIONS VII. 1000 20TH ST, PO BOX 10, BELLINGHAM, WA 98227-0010 USA: SPIE-INT SOC OPTICAL ENGINEERING; 2015. (Proceedings of SPIE; vol. 9542).
- Selbo, P.K.; Weyergang, A.; Eng, M.S.; Bostad, M.; Maelandsmo, G.M.; Hogset, A.; Berg, K. Strongly amphiphilic photosensitizers are not substrates of the cancer stem cell marker ABCG2 and provides specific and efficient light-triggered drug delivery of an EGFR-targeted cytotoxic drug. Vol. 159, JOURNAL OF CONTROLLED RELEASE. RADARWEG 29, 1043 NX AMSTERDAM, NETHERLANDS: ELSEVIER; 2012. p. 197–203.
- Sun, W.; Kajimoto, Y.; Inoue, H.; Miyatake, S.I.; Ishikawa, T.; Kuroiwa, T. Gefitinib enhances the efficacy of photodynamic therapy using 5-aminolevulinic acid in malignant brain tumor cells. Vol. 10, PHOTODIAGNOSIS AND PHOTODYNAMIC THERAPY. RADARWEG 29, 1043 NX AMSTERDAM, NETHERLANDS: ELSEVIER; 2013. p. 42–50.
- Mansi, M.; Howley, R.; Chandratre, S.; Chen, B. Inhibition of ABCG2 transporter by lapatinib enhances 5-aminolevulinic acid-mediated protoporphyrin IX fluorescence and photodynamic therapy response in human glioma cell lines. Vol. 200, BIOCHEMICAL PHARMACOLOGY. THE BOULEVARD, LANGFORD LANE, KIDLINGTON, OXFORD OX5 1GB, ENGLAND: PERGAMON-ELSEVIER SCIENCE LTD; 2022.
- Bansal, A.; Simon, M.C. Glutathione metabolism in cancer progression and treatment resistance. J Cell Biol. 2018, 217, 2291–2298. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Du, S.; Du, Y.; Ren, J.; Ying, G.; Yan, Z. Glutathione reductase mediates drug resistance in glioblastoma cells by regulating redox homeostasis. J Neurochem. 2018, 144, 93–104. [Google Scholar] [CrossRef]
- Edano, M.; Kanda, T.; Tarumoto, R.; Hamamoto, W.; Hasegawa, T.; Mae, Y.; Onoyama, T.; Takata, T.; Sugihara, T.; Isomoto, H. Intracellular glutathione levels affect the outcomes of verteporfin-mediated photodynamic therapy in esophageal cancer cells. Photodiagnosis Photodyn Ther. 2022, 40, 103090. [Google Scholar] [CrossRef]
- Mastrangelopoulou, M.; Grigalavicius, M.; Raabe, T.H.; Skarpen, E.; Juzenas, P.; Peng, Q.; Berg, K.; Theodossiou, T.A. Predictive biomarkers for 5-ALA-PDT can lead to personalized treatments and overcome tumor-specific resistances. Cancer Rep (Hoboken). 2022, 5, e1278. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Robin, A.M.; Katakowski, M.; Tong, L.; Espiritu, M.; Singh, G.; Chopp, M. Photodynamic therapy with photofrin in combination with Buthionine Sulfoximine (BSO) of human glioma in the nude rat. Lasers Med Sci. 2003, 18, 128–133. [Google Scholar] [CrossRef] [PubMed]
- dos Reis Oliveira, C.; Pereira, J.C.; Barros Ibiapina, A.; Roseno Martins, I.R.; de Castro e Sousa, J.M.; Ferreira, P.M.P.; Carneiro da Silva, F.C. Buthionine sulfoximine and chemoresistance in cancer treatments: A systematic review with meta-analysis of preclinical studies. Journal of Toxicology and Environmental Health, Part B 2023, 26, 417–441. [Google Scholar] [CrossRef] [PubMed]
- Hwang, B.; Kim, T.I.; Kim, H.; Jeon, S.; Choi, Y.; Kim, Y. Ubiquinone-BODIPY nanoparticles for tumor redox-responsive fluorescence imaging and photodynamic activity. J Mater Chem B. 2021, 9, 824–831. [Google Scholar] [CrossRef] [PubMed]
- An, R.; Liu, L.; Wei, S.; Huang, Z.; Qiu, L.; Lin, J.; Liu, H.; Ye, D. Controlling Disassembly of Paramagnetic Prodrug and Photosensitizer Nanoassemblies for On-Demand Orthotopic Glioma Theranostics. ACS Nano. 2022, 16, 20607–20621. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.-Y.; Ye, Y.-X.; Zhang, Q.; Kang, Q.-J.; Xu, Z.-M.; Ren, S.-Z.; Lin, F.; Duan, Y.-T.; Xu, H.-J.; Hu, Z.-Y.; Yang, S.-S.; Zhu, H.-L.; Zou, M.-J.; Wang, Z.-C. , Multifunctional Protein Hybrid Nanoplatform for Synergetic Photodynamic-Chemotherapy of Malignant Carcinoma by Homologous Targeting Combined with Oxygen Transport. Adv. Sci. 2023, 10, 2203742. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Li, S.; Chen, W.; Lu, H.; Ye, L.; Min, Z.; Sun, S.; Teng, C.; Yin, H.; Zhang, Q.; He, W.; Wang, X.; Lv, W.; Lv, L.; Xin, H. Multifunctional Hybrid Hydrogel System Enhanced the Therapeutic Efficacy of Treatments for Postoperative Glioma. ACS Appl Mater Interfaces. 2022, 14, 27623–27633. [Google Scholar] [CrossRef]
- Obi, C.D.; Bhuiyan, T.; Dailey, H.A.; Medlock, A.E. Ferrochelatase: Mapping the Intersection of Iron and Porphyrin Metabolism in the Mitochondria. Front Cell Dev Biol. 2022, 10, 894591. [Google Scholar] [CrossRef] [PubMed]
- Briel-Pump, A.; Beez, T.; Ebbert, L.; Remke, M.; Weinhold, S.; Sabel, M.C.; Sorg, R.V. Accumulation of protoporphyrin IX in medulloblastoma cell lines and sensitivity to subsequent photodynamic treatment. J Photochem Photobiol B. 2018, 189, 298–305. [Google Scholar] [CrossRef]
- Ihata, T.; Nonoguchi, N.; Fujishiro, T.; Omura, N.; Kawabata, S.; Kajimoto, Y.; Wanibuchi, M. The effect of hypoxia on photodynamic therapy with 5-aminolevulinic acid in malignant gliomas. Photodiagnosis Photodyn Ther. 2022, 40, 103056. [Google Scholar] [CrossRef]
- Reburn, C.; Anayo, L.; Magnussen, A.; Perry, A.; Wood, M.; Curnow, A. Experimental findings utilising a new iron chelating ALA prodrug to enhance protoporphyrin IX-induced photodynamic therapy. Hasan T, editor. 17TH INTERNATIONAL PHOTODYNAMIC ASSOCIATION WORLD CONGRESS. 1000 20TH ST, PO BOX 10, BELLINGHAM, WA 98227-0010 USA: SPIE-INT SOC OPTICAL ENGINEERING; 2019. (Proceedings of SPIE; vol. 11070).
- Blake, E.; Curnow, A. The hydroxypyridinone iron chelator CP94 can enhance PpIX-induced PDT of cultured human glioma cells. Photochem Photobiol. 2010, 86, 1154–1160. [Google Scholar] [CrossRef] [PubMed]
- Blake, E.; Allen, J.; Curnow, A. An in vitro comparison of the effects of the iron-chelating agents, CP94 and dexrazoxane, on protoporphyrin IX accumulation for photodynamic therapy and/or fluorescence guided resection. Photochem Photobiol. 2011, 87, 1419–1426. [Google Scholar] [CrossRef] [PubMed]
- Teng, L.; Nakada, M.; Zhao, S.G.; Endo, Y.; Furuyama, N.; Nambu, E.; Pyko, I.V.; Hayashi, Y.; Hamada, J.I. Silencing of ferrochelatase enhances 5-aminolevulinic acid-based fluorescence and photodynamic therapy efficacy. Br J Cancer. 2011, 104, 798–807. [Google Scholar] [CrossRef] [PubMed]
- Chau, L.Y. Heme oxygenase-1: Emerging target of cancer therapy. J Biomed Sci. 2015, 22, 22. [Google Scholar] [CrossRef] [PubMed]
- Kyriakis, J.M.; Avruch, J. Mammalian mitogen-activated protein kinase signal transduction pathways activated by stress and inflammation. Physiol Rev. 2001, 81, 807–869. [Google Scholar] [CrossRef] [PubMed]
- Sigaud, R.; Rösch, L.; Gatzweiler, C.; Benzel, J.; von Soosten, L.; Peterziel, H.; Selt, F.; Najafi, S.; Ayhan, S.; Gerloff, X.F.; Hofmann, N.; Büdenbender, I.; Schmitt, L.; Foerster, K.I.; Burhenne, J.; Haefeli, W.E.; Korshunov, A.; Sahm, F.; van Tilburg, C.M.; Jones, D.T.W.; Pfister, S.M.; Knoerzer, D.; Kreider, B.L.; Sauter, M.; Pajtler, K.W.; Zuckermann, M.; Oehme, I.; Witt, O.; Milde, T. The first-in-class ERK inhibitor ulixertinib shows promising activity in mitogen-activated protein kinase (MAPK)-driven pediatric low-grade glioma models. Neuro Oncol. 2023, 25, 566–579. [Google Scholar] [CrossRef] [PubMed]
- Haller, V.; Nahidino, P.; Forster, M.; Laufer, S.A. An updated patent review of p38 MAP kinase inhibitors (2014-2019). Expert Opin Ther Pat. 2020, 30, 453–466. [Google Scholar] [CrossRef] [PubMed]
- Chédeville, A.L.; Madureira, P.A. The Role of Hypoxia in Glioblastoma Radiotherapy Resistance. Cancers (Basel). 2021, 13, 542. [Google Scholar] [CrossRef] [PubMed]
- Pezzuto, A.; Carico, E. Role of HIF-1 in Cancer Progression: Novel Insights. A Review. Curr Mol Med. 2018, 18, 343–351. [Google Scholar] [CrossRef]
- Albert, I.; Hefti, M.; Luginbuehl, V. Physiological oxygen concentration alters glioma cell malignancy and responsiveness to photodynamic therapy in vitro. Neurol Res. 2014, 36, 1001–1010. [Google Scholar] [CrossRef]
- Broekgaarden, M.; Weijer, R.; van Gulik, T.M.; Hamblin, M.R.; Heger, M. Tumor cell survival pathways activated by photodynamic therapy: A molecular basis for pharmacological inhibition strategies. Cancer Metastasis Rev. 2015, 34, 643–690. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, M.J.; Pansa, M.F.; Vera, R.E.; Fernández-Zapico, M.E.; Rumie Vittar, N.B.; Rivarola, V.A. Transcriptional activation of HIF-1 by a ROS-ERK axis underlies the resistance to photodynamic therapy. PLoS ONE. 2017, 12, e0177801. [Google Scholar] [CrossRef] [PubMed]
- Weijer, R.; Broekgaarden, M.; van Golen, R.F.; Bulle, E.; Nieuwenhuis, E.; Jongejan, A.; Moerland, P.D.; van Kampen, A.H.; van Gulik, T.M.; Heger, M. Low-power photodynamic therapy induces survival signaling in perihilar cholangiocarcinoma cells. BMC Cancer. 2015, 15, 1014. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Q.; Yue, W.; Hu, S. Effect of photodynamic therapy and endostatin on human glioma xenografts in nude mice. Vol. 8, PHOTODIAGNOSIS AND PHOTODYNAMIC THERAPY. RADARWEG 29, 1043 NX AMSTERDAM, NETHERLANDS: ELSEVIER; 2011. p. 314–20.
- Sun, Y.; Zhang, X.; Liu, W. Effect of low energy ALA-PDT on angiogenesis and glioma growth in brain. Zhongguo Jiguang/Chinese Journal of Lasers [Internet]. 2012;39(8).
- Zheng, X.; Jiang, F.; Katakowski, M.; Zhang, X.; Jiang, H.; Zhang, Z.G.; Chopp, M. Sensitization of cerebral tissue in nude mice with photodynamic therapy induces ADAM17/TACE and promotes glioma cell invasion. Cancer Lett. 2008, 265, 177–187. [Google Scholar] [CrossRef] [PubMed]
- Ji, Z.; Yang, G.; Shahzidi, S.; Tkacz-Stachowska, K.; Suo, Z.; Nesland, J.M.; Peng, Q. Induction of hypoxia-inducible factor-1alpha overexpression by cobalt chloride enhances cellular resistance to photodynamic therapy. Cancer Lett. 2006, 244, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, M.E.; Catrinacio, C.; Ropolo, A.; Rivarola, V.A.; Vaccaro, M.I. A novel HIF-1α/VMP1-autophagic pathway induces resistance to photodynamic therapy in colon cancer cells. Photochem Photobiol Sci. 2017, 16, 1631–1642. [Google Scholar] [CrossRef] [PubMed]
- Wan, Y.; Fu, L.H.; Li, C.; Lin, J.; Huang, P. Conquering the Hypoxia Limitation for Photodynamic Therapy. Adv Mater. 2021, 33, e2103978. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, D.; Zhang, Z.; Wang, Y.; Zhang, Z.; Liang, Z.; Liu, F.; Chen, L. Photodynamic therapy enhances the cytotoxicity of temozolomide against glioblastoma via reprogramming anaerobic glycolysis. Photodiagnosis Photodyn Ther. 2023, 42, 103342. [Google Scholar] [CrossRef]
- Xu, D.; Chen, X.; Peng, Y.; Chen, W.; Li, Y.; Wang, X.; Bui, B.; Chen, K.; Zhou, M.; Kawai, N.; Tamiya, T. Effects of Phthalocyanine-Based Molecular Beacon-Mediated Photodynamic Therapy on U251 Cells. Vol. 8, NANOSCIENCE AND NANOTECHNOLOGY LETTERS. 26650 THE OLD RD, STE 208, VALENCIA, CA 91381-0751 USA: AMER SCIENTIFIC PUBLISHERS; 2016. p. 714–22.
- Cao, X.; Liu, Q.; Adu-Frimpong, M.; Shi, W.; Liu, K.; Deng, T.; Yuan, H.; Weng, X.; Gao, Y.; Yu, Q.; Deng, W.; Yu, J.; Wang, Q.; Xiao, G.; Xu, X. Microfluidic Generation of Near-Infrared Photothermal Vitexin/ICG Liposome with Amplified Photodynamic Therapy. AAPS PharmSciTech. 2023, 24, 82. [Google Scholar] [CrossRef]
- Ma, S.; Wang, F.; Dong, J.; Wang, N.; Tao, S.; Du, J.; Hu, S. Inhibition of hypoxia-inducible factor 1 by acriflavine renders glioblastoma sensitive for photodynamic therapy. J Photochem Photobiol B. 2022, 234, 112537. [Google Scholar] [CrossRef]
- Lv, Z.; Jin, L.; Gao, W.; Cao, Y.; Zhang, H.; Xue, D.; Yin, N.; Zhang, T.; Wang, Y.; Zhang, H. Novel YOF-Based Theranostic Agents with a Cascade Effect for NIR-II Fluorescence Imaging and Synergistic Starvation/Photodynamic Therapy of Orthotopic Gliomas. ACS Appl Mater Interfaces. 2022, 14, 30523–30532. [Google Scholar] [CrossRef] [PubMed]
- Song, R.; Hu, D.; Chung, H.Y.; Sheng, Z.; Yao, S. Lipid-Polymer Bilaminar Oxygen Nanobubbles for Enhanced Photodynamic Therapy of Cancer. ACS Appl Mater Interfaces. 2018, 10, 36805–36813. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Li, J.M.; Yu, H.; Deng, K.; Zhou, W.; Wang, C.X.; Zhang, Y.; Li, K.H.; Zhuo, R.X.; Huang, S.W. Fluorinated polymeric micelles to overcome hypoxia and enhance photodynamic cancer therapy. Vol. 6, BIOMATERIALS SCIENCE. THOMAS GRAHAM HOUSE, SCIENCE PARK, MILTON RD, CAMBRIDGE CB4 0WF, CAMBS, ENGLAND: ROYAL SOC CHEMISTRY; 2018. p. 3096–107.
- Xu, H.; Han, Y.; Zhao, G.; Zhang, L.; Zhao, Z.; Wang, Z.; Zhao, L.; Hua, L.; Naveena, K.; Lu, J.; Yu, R.; Liu, H. Hypoxia-Responsive Lipid-Polymer Nanoparticle-Combined Imaging-Guided Surgery and Multitherapy Strategies for Glioma. Vol. 12, ACS APPLIED MATERIALS & INTERFACES. 1155 16TH ST, NW, WASHINGTON, DC 20036 USA: AMER CHEMICAL SOC; 2020. p. 52319–28.
- Rroji, O.; Kumar, A.; Karuppagounder, S.S.; Ratan, R.R. Epigenetic regulators of neuronal ferroptosis identify novel therapeutics for neurological diseases: HDACs, transglutaminases, and HIF prolyl hydroxylases. Neurobiol Dis. 2021, 147, 105145. [Google Scholar] [CrossRef] [PubMed]
- Shen, L.; Li, Y.; Li, N.; Shen, L.; Li, Z. Comprehensive analysis of histone deacetylases genes in the prognosis and immune infiltration of glioma patients. Aging (Albany NY). 2022, 14, 4050–4068. [Google Scholar] [CrossRef] [PubMed]
- Li, P.T.; Tsai, Y.J.; Lee, M.J.; Chen, C.T. Increased Histone Deacetylase Activity Involved in the Suppressed Invasion of Cancer Cells Survived from ALA-Mediated Photodynamic Treatment. Int J Mol Sci. 2015, 16, 23994–24010. [Google Scholar] [CrossRef] [PubMed]
- Demyanenko, S.V.; Uzdensky, A.B.; Sharifulina, S.A.; Lapteva, T.O.; Polyakova, L.P. PDT-induced epigenetic changes in the mouse cerebral cortex: A protein microarray study. Biochim Biophys Acta. 2014, 1840, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Zhang, M.; Zhou, Y.; Guo, W.; Yi, M.; Zhang, Z.; Ding, Y.; Wang, Y. The application of histone deacetylases inhibitors in glioblastoma. J Exp Clin Cancer Res. 2020, 39, 138. [Google Scholar] [CrossRef] [PubMed]
- Sawa, H.; Murakami, H.; Ohshima, Y.; Sugino, T.; Nakajyo, T.; Kisanuki, T.; Tamura, Y.; Satone, A.; Ide, W.; Hashimoto, I.; Kamada, H. Histone deacetylase inhibitors such as sodium butyrate and trichostatin A induce apoptosis through an increase of the bcl-2-related protein Bad. Brain Tumor Pathol. 2001, 18, 109–114. [Google Scholar] [CrossRef]
- Sawa, H.; Murakami, H.; Ohshima, Y.; Murakami, M.; Yamazaki, I.; Tamura, Y.; Mima, T.; Satone, A.; Ide, W.; Hashimoto, I.; Kamada, H. Histone deacetylase inhibitors such as sodium butyrate and trichostatin A inhibit vascular endothelial growth factor (VEGF) secretion from human glioblastoma cells. Brain Tumor Pathol. 2002, 19, 77–81. [Google Scholar] [CrossRef]
- Nör, C.; Sassi, F.A.; de Farias, C.B.; Schwartsmann, G.; Abujamra, A.L.; Lenz, G.; Brunetto, A.L.; Roesler, R. The histone deacetylase inhibitor sodium butyrate promotes cell death and differentiation and reduces neurosphere formation in human medulloblastoma cells. Mol Neurobiol. 2013, 48, 533–543. [Google Scholar] [CrossRef]
- Bueno-Carrazco, J.; Castro-Leyva, V.; García-Gomez, F.; Solís-Paredes, M.; Ramon-Gallegos, E.; Cruz-Orea, A.; Eguía-Aguilar, P.; Arenas-Huertero, F. Sodium butyrate increases the effect of the photodynamic therapy: A mechanism that involves modulation of gene expression and differentiation in astrocytoma cells. Childs Nerv Syst. 2012, 28, 1723–1730. [Google Scholar] [CrossRef] [PubMed]
- Flores-Ancona, R.M.; García-Gómez, F.Y.; Jiménez-Betanzos, A.M.; Solis-Paredes, M.; Castro-Leyva, V.; Cruz-Orea, A.; Arenas-Huertero, F.; Ramón-Gallegos, E. Effects of sodium butyrate on cell death induced by photodynamic therapy in U373-MG and D54-MG astrocytoma cell lines. Photochem Photobiol. 2009, 85, 1182–1188. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Huang, C.; Zhang, J.; Chen, Q.; Liu, Z.; Ren, X.; Gan, S.; Wu, P.; Wang, D.; Tang, B.Z.; Sun, H. HDAC6-Activatable Multifunctional Near-Infrared Probe for Glioma Cell Detection and Elimination. Anal Chem. 2024, 96, 2406–2414. [Google Scholar] [CrossRef] [PubMed]
- do Carmo, A.; Balça-Silva, J.; Matias, D.; Lopes, M.C. PKC signaling in glioblastoma. Cancer Biol Ther. 2013, 14, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Couldwell, W.T.; Uhm, J.H.; Antel, J.P.; Yong, V.W. Enhanced protein kinase C activity correlates with the growth rate of malignant gliomas in vitro. Neurosurgery. 1991, 29, 880–886. [Google Scholar] [CrossRef]
- Couldwell, W.T.; Antel, J.P.; Yong, V.W. Protein kinase C activity correlates with the growth rate of malignant gliomas: Part II. Effects of glioma mitogens and modulators of protein kinase C. Neurosurgery. 1992, 31, 717–724. [Google Scholar] [CrossRef]
- Huntosova, V.; Stroffekova, K. Hypericin in the Dark: Foe or Ally in Photodynamic Therapy? Cancers 2016, 8, 93. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, I.; Nakanishi, S.; Kobayashi, E.; Nakano, H.; Suzuki, K.; Tamaoki, T. Hypericin and pseudohypericin specifically inhibit protein kinase C: Possible relation to their antiretroviral activity. Biochem Biophys Res Commun. 1989, 165, 1207–1212. [Google Scholar] [CrossRef]
- Uzdensky, A.; Kristiansen, B.; Moan, J.; Juzeniene, A. Dynamics of signaling, cytoskeleton and cell cycle regulation proteins in glioblastoma cells after sub-lethal photodynamic treatment: Antibody microarray study. Biochim Biophys Acta. 2012, 1820, 795–803. [Google Scholar] [CrossRef]
- Dzurová, L.; Petrovajova, D.; Nadova, Z.; Huntosova, V.; Miskovsky, P.; Stroffekova, K. The role of anti-apoptotic protein kinase Cα in response to hypericin photodynamic therapy in U-87 MG cells. Photodiagnosis Photodyn Ther. 2014, 11, 213–226. [Google Scholar] [CrossRef]
- Pevna, V.; Wagnières, G.; Huntosova, V. Autophagy and Apoptosis Induced in U87 MG Glioblastoma Cells by Hypericin-Mediated Photodynamic Therapy Can Be Photobiomodulated with 808 nm Light. Biomedicines. 2021, 9, 1703. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Cho, K.K.; Mikkelse, T.; Tong, L.; Lew, Y.S.; Hochbaum, N.; Shargorodsky, J.; Chop, M. Tamoxifen increases photodynamic therapeutic response of U87 and U25ln human glioma cells. J Neurooncol. 2002, 56, 51–58. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Liu, R.; Yang, S.H.; Yuan, F. Chemotherapeutic effect of tamoxifen on temozolomide-resistant gliomas. Anticancer Drugs. 2015, 26, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.; DiBiase, S.; Meisenberg, B.; Flannery, T.; Patel, A.; Dhople, A.; Cheston, S.; Amin, P. Phase I clinical trial assessing temozolomide and tamoxifen with concomitant radiotherapy for treatment of high-grade glioma. Int J Radiat Oncol Biol Phys. 2012, 82, 739–742. [Google Scholar] [CrossRef] [PubMed]
- Misuth, M.; Horvath, D.; Miskovsky, P.; Huntosova, V. Synergism between PKCδ regulators hypericin and rottlerin enhances apoptosis in U87 MG glioma cells after light stimulation. Vol. 18, PHOTODIAGNOSIS AND PHOTODYNAMIC THERAPY. PO BOX 211, 1000 AE AMSTERDAM, NETHERLANDS: ELSEVIER SCIENCE BV; 2017. p. 267–74.
- Kim, D.C.; Kim, S.H.; Jeong, M.W.; Baek, N.I.; Kim, K.T. Effect of rottlerin, a PKC-delta inhibitor, on TLR-4-dependent activation of murine microglia. Biochem Biophys Res Commun. 2005, 337, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Song, K.S.; Kim, J.S.; Yun, E.J.; Kim, Y.R.; Seo, K.S.; Park, J.H.; Jung, Y.J.; Park, J.I.; Kweon, G.R.; Yoon, W.H.; Lim, K.; Hwang, B.D. Rottlerin induces autophagy and apoptotic cell death through a PKC-delta-independent pathway in HT1080 human fibrosarcoma cells: The protective role of autophagy in apoptosis. Autophagy. 2008, 4, 650–658. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.H.; Park, J.W.; Choi, K.S.; Park, Y.B.; Kwon, T.K. Rottlerin induces apoptosis via death receptor 5 (DR5) upregulation through CHOP-dependent and PKC delta-independent mechanism in human malignant tumor cells. Carcinogenesis. 2009, 30, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Saadeh, F.S.; Mahfouz, R.; Assi, H.I. EGFR as a clinical marker in glioblastomas and other gliomas. Int J Biol Markers. 2018, 33, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Brennan, C.W.; Verhaak, R.G.; McKenna, A.; Campos, B.; Noushmehr, H.; Salama, S.R.; Zheng, S.; Chakravarty, D.; Sanborn, J.Z.; Berman, S.H.; et al. The somatic genomic landscape of glioblastoma. Cell. 2013, 155, 462–477. [Google Scholar] [CrossRef]
- Oprita, A.; Baloi, S.C.; Staicu, G.A.; Alexandru, O.; Tache, D.E.; Danoiu, S.; Micu, E.S.; Sevastre, A.S. Updated Insights on EGFR Signaling Pathways in Glioma. Int J Mol Sci. 2021, 22, 587. [Google Scholar] [CrossRef]
- Fanuel-Barret, D.; Patrice, T.; Foultier, M.T.; Vonarx-Coinsmann, V.; Robillard, N.; Lajat, Y. Influence of epidermal growth factor on photodynamic therapy of glioblastoma cells in vitro. Res Exp Med (Berl). 1997, 197, 219–233. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.W.; Hung, M.C.; Hsieh, C.Y.; Tung, E.C.; Wang, Y.H.; Tsai, J.C.; Lee, J.M. The effects of Photofrin-mediated photodynamic therapy on the modulation of EGFR in esophageal squamous cell carcinoma cells. Lasers Med Sci. 2013, 28, 605–614. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.; Ji, H.T.; Chiang, P.C.; Chou, R.H.; Chang, W.S.; Chen, C.T. ALA-PDT results in phenotypic changes and decreased cellular invasion in surviving cancer cells. Lasers Surg Med. 2009, 41, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Ulfo, L.; Costantini, P.E.; Di Giosia, M.; Danielli, A.; Calvaresi, M. EGFR-Targeted Photodynamic Therapy. Pharmaceutics. 2022, 14, 241. [Google Scholar] [CrossRef] [PubMed]
- Fisher, C.J.; Niu, C.J.; Lai, B.; Chen, Y.; Kuta, V.; Lilge, L.D. Modulation of PPIX synthesis and accumulation in various normal and glioma cell lines by modification of the cellular signaling and temperature. Lasers Surg Med. 2013, 45, 460–468. [Google Scholar] [CrossRef] [PubMed]
- Fisher, C.; Obaid, G.; Niu, C.; Foltz, W.; Goldstein, A.; Hasan, T.; Lilge, L. Liposomal Lapatinib in Combination with Low-Dose Photodynamic Therapy for the Treatment of Glioma. J Clin Med. 2019, 8, 2214. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, S.M.B.; Kamel, A.; Ciubotaru, G.V.; Onose, G.; Sevastre, A.S.; Sfredel, V.; Danoiu, S.; Dricu, A.; Tataranu, L.G. An Overview of EGFR Mechanisms and Their Implications in Targeted Therapies for Glioblastoma. Int J Mol Sci. 2023, 24, 11110. [Google Scholar] [CrossRef]
- Jamali, Z.; Khoobi, M.; Hejazi, S.M.; Eivazi, N.; Abdolahpour, S.; Imanparast, F.; Moradi-Sardareh, H.; Paknejad, M. Evaluation of targeted curcumin (CUR) loaded PLGA nanoparticles for in vitro photodynamic therapy on human glioblastoma cell line. Photodiagnosis Photodyn Ther. 2018, 23, 190–201. [Google Scholar] [CrossRef] [PubMed]
- Meyers, J.D.; Cheng, Y.; Broome, A.M.; Agnes, R.S.; Schluchter, M.D.; Margevicius, S.; Wang, X.; Kenney, M.E.; Burda, C.; Basilion, J.P. Peptide-Targeted Gold Nanoparticles for Photodynamic Therapy of Brain Cancer. Part Part Syst Charact. 2015, 32, 448–457. [Google Scholar] [CrossRef]
- Xie, Y.; Su, N.; Yang, J.; Tan, Q.; Huang, S.; Jin, M.; Ni, Z.; Zhang, B.; Zhang, D.; Luo, F.; Chen, H.; Sun, X.; Feng, J.Q.; Qi, H.; Chen, L. FGF/FGFR signaling in health and disease. Signal Transduct Target Ther. 2020, 5, 181. [Google Scholar]
- Klimaschewski, L.; Claus, P. Fibroblast Growth Factor Signalling in the Diseased Nervous System. Mol Neurobiol. 2021, 58, 3884–3902. [Google Scholar] [CrossRef] [PubMed]
- Wei, P.; Zhang, Z.; Lin, M.; Zhou, B.; Wang, Z. Bevacizumab has bidirectional regulatory effects on the secretion of basic fibroblast growth factor in glioma cells. Cytokine. 2020, 129, 155022. [Google Scholar] [CrossRef] [PubMed]
- Chai, N.; Stachon, T.; Berger, T.; Li, Z.; Seitz, B.; Langenbucher, A.; Szentmáry, N. Human corneal epithelial cell and fibroblast migration and growth factor secretion after rose bengal photodynamic therapy (RB-PDT) and the effect of conditioned medium. PLoS ONE. 2023, 18, e0296022. [Google Scholar] [CrossRef] [PubMed]
- LaMuraglia, G.M.; Adili, F.; Karp, S.J.; Statius van Eps, R.G.; Watkins, M.T. Photodynamic therapy inactivates extracellular matrix-basic fibroblast growth factor: Insights to its effect on the vascular wall. J Vasc Surg. 1997, 26, 294–301. [Google Scholar] [CrossRef]
- Vilchez, M.L.; Rodríguez, L.B.; Palacios, R.E.; Prucca, C.G.; Caverzán, M.D.; Caputto, B.L.; Rivarola, V.A.; Milla Sanabria, L.N. Isolation and initial characterization of human glioblastoma cells resistant to photodynamic therapy. Photodiagnosis Photodyn Ther. 2021, 33, 102097. [Google Scholar] [CrossRef] [PubMed]
- Tsai, J.; Hsiao, Y.; Teng, L.; Chen, C.; Kao, M. Comparative study on the ALA photodynamic effects of human glioma and meningioma cells. Vol. 24, LASERS IN SURGERY AND MEDICINE. DIV JOHN WILEY & SONS INC, 605 THIRD AVE, NEW YORK, NY 10158-0012 USA: WILEY-LISS; 1999. p. 296–305.
- Chakrabarti, M.; Banik, N.L.; Ray, S.K. Photofrin based photodynamic therapy and miR-99a transfection inhibited FGFR3 and PI3K/Akt signaling mechanisms to control growth of human glioblastoma In vitro and in vivo. PLoS ONE. 2013, 8, e55652. [Google Scholar] [CrossRef] [PubMed]
- Repetto, M.; Crimini, E.; Giugliano, F.; Morganti, S.; Belli, C.; Curigliano, G. Selective FGFR/FGF pathway inhibitors: Inhibition strategies, clinical activities, resistance mutations, and future directions. Expert Rev Clin Pharmacol. 2021, 14, 1233–1252. [Google Scholar] [CrossRef] [PubMed]
- Abounader, R.; Laterra, J. Scatter factor/hepatocyte growth factor in brain tumor growth and angiogenesis. Neuro Oncol. 2005, 7, 436–451. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.F.; Wang, X.B.; Tian, X.Y.; Li, Y.; Li, B.; Huang, Q.; Zhang, M.; Li, Z. Tumor-derived hepatocyte growth factor is associated with poor prognosis of patients with glioma and influences the chemosensitivity of glioma cell line to cisplatin in vitro. World J Surg Oncol. 2012, 10, 128. [Google Scholar] [CrossRef]
- Vogel, S.; Peters, C.; Etminan, N.; Börger, V.; Schimanski, A.; Sabel, M.C.; Sorg, R.V. Migration of mesenchymal stem cells towards glioblastoma cells depends on hepatocyte-growth factor and is enhanced by aminolaevulinic acid-mediated photodynamic treatment. Biochem Biophys Res Commun. 2013, 431, 428–432. [Google Scholar] [CrossRef]
- Matsumoto, K.; Umitsu, M.; De Silva, D.M.; Roy, A.; Bottaro, D.P. Hepatocyte growth factor/MET in cancer progression and biomarker discovery. Cancer Sci. 2017, 108, 296–307. [Google Scholar] [CrossRef] [PubMed]
- Weathers, S.P.; de Groot, J. VEGF Manipulation in Glioblastoma. Oncology (Williston Park). 2015, 29, 720–727. [Google Scholar]
- Seyedmirzaei, H.; Shobeiri, P.; Turgut, M.; Hanaei, S.; Rezaei, N. VEGF levels in patients with glioma: A systematic review and meta-analysis. Rev Neurosci. 2020, 32, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Onishi, M.; Ichikawa, T.; Kurozumi, K.; Date, I. Angiogenesis and invasion in glioma. Brain Tumor Pathol. 2011, 28, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Deininger, M.H.; Weinschenk, T.; Morgalla, M.H.; Meyermann, R.; Schluesener, H.J. Release of regulators of angiogenesis following Hypocrellin-A and -B photodynamic therapy of human brain tumor cells. Biochem Biophys Res Commun. 2002, 298, 520–530. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Chen, X.; Chen, K.; Peng, Y.; Li, Y.; Ke, Y.; Gan, D. Tetra-sulfonate phthalocyanine zinc-bovine serum albumin conjugate-mediated photodynamic therapy of human glioma. J Biomater Appl. 2014, 29, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Ke, Y.; Jiang, X.; Cai, Y.; Peng, Y.; Li, Y. In vitro photodynamic therapy on human U251 glioma cells with a novel photosensitiser ZnPcS4-BSA. Br J Neurosurg. 2010, 24, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Jiang, F.; Kalkanis, S.N.; Zhang, Z.; Hong, X.; Yang, H.; Chopp, M. Post-acute response of 9L gliosarcoma to Photofrin-mediated PDT in athymic nude mice. Lasers Med Sci. 2007, 22, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Zhang, Z.; Katakowski, M.; Robin, A.; Faber, M.; Zhang, F.; Chopp, M. Angiogenesis induced by photodynamic therapy in normal rat brain. Vol. 79, PHOTOCHEMISTRY AND PHOTOBIOLOGY. 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY-BLACKWELL; 2004. p. 494–8.
- Zhang, X.; Jiang, F.; Zhang, Z.G.; Kalkanis, S.N.; Hong, X.; deCarvalho, A.C.; Chen, J.; Yang, H.; Robin, A.M.; Chopp, M. Low-dose photodynamic therapy increases endothelial cell proliferation and VEGF expression in nude mice brain. Lasers Med Sci. 2005, 20, 74–79. [Google Scholar] [CrossRef]
- Tzerkovsky, D.A.; Osharin, V.V.; Istomin, Y.P.; Alexandrova, E.N.; Vozmitel, M.A. Fluorescent diagnosis and photodynamic therapy for C6 glioma in combination with antiangiogenic therapy in subcutaneous and intracranial tumor models. Exp Oncol. 2014, 36, 85–89. [Google Scholar]
- Jiang, F.; Zhang, X.; Kalkanis, S.N.; Zhang, Z.; Yang, H.; Katakowski, M.; Hong, X.; Zheng, X.; Zhu, Z.; Chopp, M. Combination therapy with antiangiogenic treatment and photodynamic therapy for the nude mouse bearing U87 glioblastoma. Photochem Photobiol. 2008, 84, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Tatar, O.; Shinoda, K.; Adam, A.; Eckert, T.; Eckardt, C.; Lucke, K.; Deuter, C.; Bartz-Schmidt, K.U.; Grisanti, S. Effect of verteporfin photodynamic therapy on endostatin and angiogenesis in human choroidal neovascular membranes. Br J Ophthalmol. 2007, 91, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Walia, A.; Yang, J.F.; Huang, Y.H.; Rosenblatt, M.I.; Chang, J.H.; Azar, D.T. Endostatin’s emerging roles in angiogenesis, lymphangiogenesis, disease, and clinical applications. Biochim Biophys Acta. 2015, 1850, 2422–2438. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.L.; Lin, H.C.; Chiang, W.L.; Shih, Y.H.; Chiang, P.F.; Luo, T.Y.; Cheng, C.C.; Shieh, M.J. Anti-angiogenic treatment (Bevacizumab) improves the responsiveness of photodynamic therapy in colorectal cancer. Photodiagnosis Photodyn Ther. 2018, 23, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Jo, J.; Wen, P.Y. Antiangiogenic Therapy of High-Grade Gliomas. Prog Neurol Surg. 2018, 31, 180–199. [Google Scholar] [PubMed]
- Zhang, G.; Chen, L.; Sun, K.; Khan, A.A.; Yan, J.; Liu, H.; Lu, A.; Gu, N. Neuropilin-1 (NRP-1)/GIPC1 pathway mediates glioma progression. Tumour Biol. 2016, 37, 13777–13788. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.K.; Miao, W.; Tang, X.Y.; Zhang, H.P.; Wang, S.Y.; Luo, F.H.; et al. The expression and significance of neuropilin-1 (NRP-1) on glioma cell lines and glioma tissues. J Biomed Nanotechnol. 2013, 9, 559–563. [Google Scholar] [CrossRef]
- Chen, L.K.; Miao, W.; Tang, X.Y.; Zhang, H.P.; Wang, S.Y.; Luo, F.H.; et al. Inhibitory effect of neuropilin-1 monoclonal antibody (NRP-1 MAb) on glioma tumor in mice. J Biomed Nanotechnol. 2013, 9, 551–558. [Google Scholar] [CrossRef]
- Caponegro, M.D.; Moffitt, R.A.; Tsirka, S.E. Expression of neuropilin-1 is linked to glioma associated microglia and macrophages and correlates with unfavorable prognosis in high grade gliomas. Oncotarget. 2018, 9, 35655–35665. [Google Scholar] [CrossRef]
- Thomas, N.; Tirand, L.; Chatelut, E.; Plénat, F.; Frochot, C.; Dodeller, M.; Guillemin, F.; Barberi-Heyob, M. Tissue distribution and pharmacokinetics of an ATWLPPR-conjugated chlorin-type photosensitizer targeting neuropilin-1 in glioma-bearing nude mice. Photochem Photobiol Sci. 2008, 7, 433–441. [Google Scholar] [CrossRef]
- Tirand, L.; Frochot, C.; Vanderesse, R.; Thomas, N.; Trinquet, E.; Pinel, S.; Viriot, M.L.; Guillemin, F.; Barberi-Heyob, M. A peptide competing with VEGF165 binding on neuropilin-1 mediates targeting of a chlorin-type photosensitizer and potentiates its photodynamic activity in human endothelial cells. J Control Release. 2006, 111, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Bechet, D.; Auger, F.; Couleaud, P.; Marty, E.; Ravasi, L.; Durieux, N.; Bonnet, C.; Plénat, F.; Frochot, C.; Mordon, S.; Tillement, O.; Vanderesse, R.; Lux, F.; Perriat, P.; Guillemin, F.; Barberi-Heyob, M. Multifunctional ultrasmall nanoplatforms for vascular-targeted interstitial photodynamic therapy of brain tumors guided by real-time MRI. Nanomedicine. 2015, 11, 657–670. [Google Scholar] [CrossRef] [PubMed]
- Gries, M.; Thomas, N.; Daouk, J.; Rocchi, P.; Choulier, L.; Jubréaux, J.; Pierson, J.; Reinhard, A.; Jouan-Hureaux, V.; Chateau, A.; Acherar, S.; Frochot, C.; Lux, F.; Tillement, O.; Barberi-Heyob, M. Multiscale Selectivity and in vivo Biodistribution of NRP-1-Targeted Theranostic AGuIX Nanoparticles for PDT of Glioblastoma. Int J Nanomedicine. 2020, 15, 8739–8758. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.; Colombeau, L.; Gries, M.; Peterlini, T.; Mathieu, C.; Thomas, N.; Boura, C.; Frochot, C.; Vanderesse, R.; Lux, F.; Barberi-Heyob, M.; Tillement, O. Ultrasmall AGuIX theranostic nanoparticles for vascular-targeted interstitial photodynamic therapy of glioblastoma. Int J Nanomedicine. 2017, 12, 7075–7088. [Google Scholar] [CrossRef] [PubMed]
- Tirand, L.; Bastogne, T.; Bechet, D.; Linder, M.; Thomas, N.; Frochot, C.; Guillemin, F.; Barberi-Heyob, M. Response surface methodology: An extensive potential to optimize in vivo photodynamic therapy conditions. Int J Radiat Oncol Biol Phys. 2009, 75, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Thomas, N.; Bechet, D.; Becuwe, P.; Tirand, L.; Vanderesse, R.; Frochot, C.; Guillemin, F.; Barberi-Heyob, M. Peptide-conjugated chlorin-type photosensitizer binds neuropilin-1 in vitro and in vivo. Vol. 96, JOURNAL OF PHOTOCHEMISTRY AND PHOTOBIOLOGY B-BIOLOGY. PO BOX 564, 1001 LAUSANNE, SWITZERLAND: ELSEVIER SCIENCE SA; 2009. p. 101–8.
- Lu, L.; Zhao, X.; Fu, T.; Li, K.; He, Y.; Luo, Z.; Dai, L.; Zeng, R.; Cai, K. An iRGD-conjugated prodrug micelle with blood-brain-barrier penetrability for anti-glioma therapy. Biomaterials. 2020, 230, 119666. [Google Scholar] [CrossRef] [PubMed]
- Kong, D.H.; Kim, Y.K.; Kim, M.R.; Jang, J.H.; Lee, S. Emerging Roles of Vascular Cell Adhesion Molecule-1 (VCAM-1) in Immunological Disorders and Cancer. Int J Mol Sci. 2018, 19, 1057. [Google Scholar] [CrossRef]
- Mäenpää, A.; Kovanen, P.E.; Paetau, A.; Jäáskeläinen, J.; Timonen, T. Lymphocyte adhesion molecule ligands and extracellular matrix proteins in gliomas and normal brain: Expression of VCAM-1 in gliomas. Acta Neuropathol. 1997, 94, 216–225. [Google Scholar] [CrossRef] [PubMed]
- Cheng, V.W.T.; de Pennington, N.; Zakaria, R.; Larkin, J.R.; Serres, S.; Sarkar, M.; Kirkman, M.A.; Bristow, C.; Croal, P.; Plaha, P.; Campo, L.; Chappell, M.A.; Lord, S.; Jenkinson, M.D.; Middleton, M.R.; Sibson, N.R. VCAM-1-targeted MRI Improves Detection of the Tumor-brain Interface. Clin Cancer Res. 2022, 28, 2385–2396. [Google Scholar] [CrossRef]
- Zhan, Q.; Yue, W.; Hu, S. The inhibitory effect of photodynamic therapy and of an anti-VCAM-1 monoclonal antibody on the in vivo growth of C6 glioma xenografts. Vol. 44, BRAZILIAN JOURNAL OF MEDICAL AND BIOLOGICAL RESEARCH. FACULDADE MEDICINA, CASA 10, 14049 RIBEIRAO PRETO, RIBEIRAO PRETO, SP 14049, BRAZIL: ASSOC BRAS DIVULG CIENTIFICA; 2011. p. 489–96.
- Volanti, C.; Gloire, G.; Vanderplasschen, A.; Jacobs, N.; Habraken, Y.; Piette, J. Downregulation of ICAM-1 and VCAM-1 expression in endothelial cells treated by photodynamic therapy. Oncogene. 2004, 23, 8649–8658. [Google Scholar] [CrossRef]
- Kawczyk-Krupka, A.; Czuba, Z.P.; Kwiatek, B.; Kwiatek, S.; Krupka, M.; Sieroń, K. The effect of ALA-PDT under normoxia and cobalt chloride (CoCl2)-induced hypoxia on adhesion molecules (ICAM-1, VCAM-1) secretion by colorectal cancer cells. Photodiagnosis Photodyn Ther. 2017, 19, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Takada, Y.; Ye, X.; Simon, S. The integrins. Genome Biol. 2007, 8, 215. [Google Scholar] [CrossRef]
- Liu, F.; Wu, Q.; Dong, Z.; Liu, K. Integrins in cancer: Emerging mechanisms and therapeutic opportunities. Pharmacol Ther. 2023, 247, 108458. [Google Scholar] [CrossRef]
- Ferrer, V.P.; Moura Neto, V.; Mentlein, R. Glioma infiltration and extracellular matrix: Key players and modulators. Glia. 2018, 66, 1542–1565. [Google Scholar] [CrossRef] [PubMed]
- Di Venosa, G.; Perotti, C.; Batlle, A.; Casas, A. The role of cytoskeleton and adhesion proteins in the resistance to photodynamic therapy. Possible therapeutic interventions. Photochem Photobiol Sci. 2015, 14, 1451–1464. [Google Scholar] [CrossRef]
- Au, C.M.; Luk, S.K.; Jackson, C.J.; Ng, H.K.; Yow, C.M.N.; To, S.S.T. Differential effects of photofrin, 5-aminolevulinic acid and calphostin C on glioma cells. Journal of Photochemistry and Photobiology B: Biology. 2006, 85, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Pacheco Soares, C.; Maftou Costa, M.; da Cunha Menezes Costa, C.G.; de Siqueira Silva, A.C.; Moraes, K.C. Evaluation of photodynamic therapy in adhesion protein expression. Oncology Letters 2014, 8, 714–718. [Google Scholar] [CrossRef]
- Wei, Y.; Zhou, F.; Zhang, D.; Chen, Q.; Xing, D. A graphene oxide based smart drug delivery system for tumor mitochondria-targeting photodynamic therapy. Nanoscale. 2016, 8, 3530–3538. [Google Scholar] [CrossRef]
- de Almeida, L.G.N.; Thode, H.; Eslambolchi, Y.; Chopra, S.; Young, D.; Gill, S.; Devel, L.; Dufour, A. Matrix Metalloproteinases: From Molecular Mechanisms to Physiology, Pathophysiology, and Pharmacology. Pharmacol Rev. 2022, 74, 712–768. [Google Scholar] [CrossRef]
- Zhou, W.; Yu, X.; Sun, S.; Zhang, X.; Yang, W.; Zhang, J.; Zhang, X.; Jiang, Z. Increased expression of MMP-2 and MMP-9 indicates poor prognosis in glioma recurrence. Biomed Pharmacother. 2019, 118, 109369. [Google Scholar] [CrossRef]
- Wang, L.; Yuan, J.; Tu, Y.; Mao, X.; He, S.; Fu, G.; Zong, J.; Zhang, Y. Co-expression of MMP-14 and MMP-19 predicts poor survival in human glioma. Clin Transl Oncol. 2013, 15, 139–145. [Google Scholar] [CrossRef]
- Chu, E.S.M.; Wong, T.K.S.; Yow, C.M.N. Photodynamic effect in medulloblastoma: Downregulation of matrix metalloproteinases and human telomerase reverse transcriptase expressions. Photochem Photobiol Sci. 2008, 7, 76–83. [Google Scholar] [CrossRef]
- Etminan, N.; Peters, C.; Ficnar, J.; Anlasik, S.; Bünemann, E.; Slotty, P.J.; Hänggi, D.; Steiger, H.J.; Sorg, R.V.; Stummer, W. Modulation of migratory activity and invasiveness of human glioma spheroids following 5-aminolevulinic acid-based photodynamic treatment. Laboratory investigation. J Neurosurg. 2011, 115, 281–288. [Google Scholar] [CrossRef]
- Li, J.; Tian, Y.; Zheng, T. A multifunctional nanoprobe for real-time SERS monitoring of invasion ability affected by photodynamic therapy. Chem Commun (Camb). 2022, 58, 6542–6545. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Lin, H.; Chen, Q.; Yu, L.; Bai, D. MPPa-PDT suppresses breast tumor migration/invasion by inhibiting Akt-NF-κB-dependent MMP-9 expression via ROS. BMC Cancer. 2019, 19, 1159. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Shen, B.; Swinarska, J.T.; Li, W.; Xiao, K.; He, P. 9-Hydroxypheophorbide α-mediated photodynamic therapy induces matrix metalloproteinase-2 (MMP-2) and MMP-9 down-regulation in Hep-2 cells via ROS-mediated suppression of the ERK pathway. Photodiagnosis Photodyn Ther. 2014, 11, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Li, B.O.; Meng, C.; Zhang, X.; Cong, D.; Gao, X.; Gao, W.; Ju, D.; Hu, S. Effect of photodynamic therapy combined with torasemide on the expression of matrix metalloproteinase 2 and sodium-potassium-chloride cotransporter 1 in rat peritumoral edema and glioma. Oncol Lett. 2016, 11, 2084–2090. [Google Scholar] [CrossRef]
- Lee, E.J.; Kim, S.Y.; Hyun, J.W.; Min, S.W.; Kim, D.H.; Kim, H.S. Glycitein inhibits glioma cell invasion through down-regulation of MMP-3 and MMP-9 gene expression. Chem Biol Interact. 2010, 185, 18–24. [Google Scholar] [CrossRef]
- Wang, X.; Chen, X.; Sun, L.; Bi, X.; He, H.; Chen, L.; Pang, J. MicroRNA 34a inhibits cell growth and migration in human glioma cells via MMP 9. Mol Med Rep. 2019, 20, 57–64. [Google Scholar] [CrossRef]
- Middeldorp, J.; Hol, E.M. GFAP in health and disease. Prog Neurobiol. 2011, 93, 421–443. [Google Scholar] [CrossRef]
- van Asperen, J.V.; Robe, P.A.J.T.; Hol, E.M. GFAP Alternative Splicing and the Relevance for Disease - A Focus on Diffuse Gliomas. ASN Neuro. 2022, 14, 17590914221102065. [Google Scholar] [CrossRef]
- van Bodegraven, E.J.; van Asperen, J.V.; Robe, P.A.J.; Hol, E.M. Importance of GFAP isoform-specific analyses in astrocytoma. Glia. 2019, 67, 1417–1433. [Google Scholar] [CrossRef] [PubMed]
- Uceda-Castro, R.; van Asperen, J.V.; Vennin, C.; Sluijs, J.A.; van Bodegraven, E.J.; Margarido, A.S.; Robe, P.A.J.; van Rheenen, J.; Hol, E.M. GFAP splice variants fine-tune glioma cell invasion and tumour dynamics by modulating migration persistence. Sci Rep. 2022, 12, 424. [Google Scholar] [CrossRef] [PubMed]
- Namatame, H.; Akimoto, J.; Matsumura, H.; Haraoka, J.; Aizawa, K. Photodynamic therapy of C6-implanted glioma cells in the rat brain employing second-generation photosensitizer talaporfin sodium. Vol. 5, PHOTODIAGNOSIS AND PHOTODYNAMIC THERAPY. RADARWEG 29, 1043 NX AMSTERDAM, NETHERLANDS: ELSEVIER; 2008. p. 198–209.
- Hara, A.; Sakai, N.; Yamada, H.; Niikawa, S.; Ohno, T.; Tanaka, T.; Mori, H. Proliferative assessment of GFAP-positive and GFAP-negative glioma cells by nucleolar organizer region staining. Surg Neurol. 1991, 36, 190–194. [Google Scholar] [CrossRef]
- Hara, A.; Hirayama, H.; Sakai, N.; Yamada, H.; Tanaka, T.; Mori, H. Correlation between nucleolar organizer region staining and Ki-67 immunostaining in human gliomas. Surg Neurol. 1990, 33, 320–324. [Google Scholar] [CrossRef]
- Harmelin, A.; Zuckerman, A.; Nyska, A. Correlation of Ag-NOR protein measurements with prognosis in canine transmissible venereal tumour. J Comp Pathol. 1995, 112, 429–433. [Google Scholar] [CrossRef]
- Arden, K.C.; Pathak, S.; Frankel, L.S.; Zander, A. Ag-NOR staining in human chromosomes: Differential staining in normal and leukemic bone-marrow samples. Int J Cancer. 1985, 36, 647–649. [Google Scholar] [CrossRef]
- Schelling, J.R.; Abu Jawdeh, B.G. Regulation of cell survival by Na+/H+ exchanger-1. Am J Physiol Renal Physiol. 2008, 295, F625–F632. [Google Scholar] [CrossRef] [PubMed]
- Guan, X.; Hasan, M.N.; Begum, G.; Kohanbash, G.; Carney, K.E.; Pigott, V.M.; Persson, A.I.; Castro, M.G.; Jia, W.; Sun, D. Blockade of Na/H exchanger stimulates glioma tumor immunogenicity and enhances combinatorial TMZ and anti-PD-1 therapy. Cell Death Dis. 2018, 9, 1010. [Google Scholar] [CrossRef]
- Zhu, W.; Carney, K.E.; Pigott, V.M.; Falgoust, L.M.; Clark, P.A.; Kuo, J.S.; Sun, D. Glioma-mediated microglial activation promotes glioma proliferation and migration: Roles of Na+/H+ exchanger isoform 1. Carcinogenesis. 2016, 37, 839–851. [Google Scholar] [CrossRef]
- Hasan, M.N.; Luo, L.; Ding, D.; et al. Blocking NHE1 stimulates glioma tumor immunity by restoring OXPHOS function of myeloid cells. Theranostics. 2021, 11, 1295–1309. [Google Scholar] [CrossRef]
- Hou, K.; Liu, J.; Du, J.; Mi, S.; Ma, S.; Ba, Y.; Ji, H.; Li, B.; Hu, S. Dihydroartemisinin prompts amplification of photodynamic therapy-induced reactive oxygen species to exhaust Na/H exchanger 1-mediated glioma cells invasion and migration. J Photochem Photobiol B. 2021, 219, 112192. [Google Scholar] [CrossRef] [PubMed]
- Jia, Y.; Chen, L.; Chi, D.; Cong, D.; Zhou, P.; Jin, J.; Ji, H.; Liang, B.; Gao, S.; Hu, S. Photodynamic therapy combined with temozolomide inhibits C6 glioma migration and invasion and promotes mitochondrial-associated apoptosis by inhibiting sodium-hydrogen exchanger isoform 1. Photodiagnosis Photodyn Ther. 2019, 26, 405–412. [Google Scholar] [CrossRef]
- Shimoda, L.A.; Fallon, M.; Pisarcik, S.; Wang, J.; Semenza, G.L. HIF-1 regulates hypoxic induction of NHE1 expression and alkalinization of intracellular pH in pulmonary arterial myocytes. Am J Physiol Lung Cell Mol Physiol. 2006, 291, L941–L949. [Google Scholar] [CrossRef]
- Tamtaji, O.R.; Mirzaei, H.; Shamshirian, A.; Shamshirian, D.; Behnam, M.; Asemi, Z. New trends in glioma cancer therapy: Targeting Na⁺/H⁺ exchangers. J Cell Physiol. 2019, 235, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Dolcet, X.; Llobet, D.; Pallares, J.; Matias-Guiu, X. NF-kB in development and progression of human cancer. Virchows Arch. 2005, 446, 475–482. [Google Scholar] [CrossRef]
- Li, Y.; Zhou, Q.L.; Sun, W.; Chandrasekharan, P.; Cheng, H.S.; Ying, Z.; Lakshmanan, M.; Raju, A.; Tenen, D.G.; Cheng, S.Y.; Chuang, K.H.; Li, J.; Prabhakar, S.; Li, M.; Tergaonkar, V. Non-canonical NF-κB signalling and ETS1/2 cooperatively drive C250T mutant TERT promoter activation. Nat Cell Biol. 2015, 17, 1327–1338. [Google Scholar] [CrossRef]
- Hu, Y.H.; Jiao, B.H.; Wang, C.Y.; Wu, J.L. Regulation of temozolomide resistance in glioma cells via the RIP2/NF-κB/MGMT pathway. CNS Neurosci Ther. 2021, 27, 552–563. [Google Scholar] [CrossRef] [PubMed]
- Coupienne, I.; Bontems, S.; Dewaele, M.; Rubio, N.; Habraken, Y.; Fulda, S.; Agostinis, P.; Piette, J. NF-kappaB inhibition improves the sensitivity of human glioblastoma cells to 5-aminolevulinic acid-based photodynamic therapy. Biochem Pharmacol. 2011, 81, 606–616. [Google Scholar] [CrossRef]
- Piette, J. Signalling pathway activation by photodynamic therapy: NF-κB at the crossroad between oncology and immunology. Photochem Photobiol Sci. 2015, 14, 1510–1517. [Google Scholar] [CrossRef]
- Fahey, J.M.; Korytowski, W.; Girotti, A.W. Upstream signaling events leading to elevated production of pro-survival nitric oxide in photodynamically-challenged glioblastoma cells. Free Radic Biol Med. 2019, 137, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Karmakar, S.; Banik, N.L.; Patel, S.J.; Ray, S.K. 5-Aminolevulinic acid-based photodynamic therapy suppressed survival factors and activated proteases for apoptosis in human glioblastoma U87MG cells. Neurosci Lett. 2007, 415, 242–247. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Alqawi, O.; Espiritu, M. Metronomic PDT and cell death pathways. Methods Mol Biol. 2010, 635, 65–78. [Google Scholar] [PubMed]
- He, Y.; Duan, L.; Wu, H.; Chen, S.; Lu, T.; Li, T.; He, Y. Integrated Transcriptome Analysis Reveals the Impact of Photodynamic Therapy on Cerebrovascular Endothelial Cells. Front Oncol. 2021, 11, 731414. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, M.; Candido, M.F.; Valera, E.T.; Brassesco, M.S. The multifaceted NF-kB: Are there still prospects of its inhibition for clinical intervention in pediatric central nervous system tumors? Cell Mol Life Sci. 2021, 78, 6161–6200. [Google Scholar] [CrossRef] [PubMed]
- Kumthekar, P.; Grimm, S.; Chandler, J.; et al. A phase II trial of arsenic trioxide and temozolomide in combination with radiation therapy for patients with malignant gliomas. J Neurooncol 2017, 133, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Tu, Z.; Li, K.; Ji, Q.; Huang, Y.; Lv, S.; Li, J.; Wu, L.; Huang, K.; Zhu, X. Pan-cancer analysis: Predictive role of TAP1 in cancer prognosis and response to immunotherapy. BMC Cancer. 2023, 23, 133. [Google Scholar] [CrossRef]
- Satoh, E.; Mabuchi, T.; Satoh, H.; Asahara, T.; Nukui, H.; Naganuma, H. Reduced expression of the transporter associated with antigen processing 1 molecule in malignant glioma cells, and its restoration by interferon-gamma and -beta. J Neurosurg. 2006, 104, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Žilionytė, K.; Bagdzevičiūtė, U.; Mlynska, A.; Urbštaitė, E.; Paberalė, E.; Dobrovolskienė, N.; Krasko, J.A.; Pašukonienė, V. Correction to: Functional antigen processing and presentation mechanism as a prerequisite factor of response to treatment with dendritic cell vaccines and anti-PD-1 in preclinical murine LLC1 and GL261 tumor models. Cancer Immunol Immunother. 2022, 71, 2701. [Google Scholar] [CrossRef]
- Yang, W.; Li, Y.; Gao, R.; Xiu, Z.; Sun, T. MHC class I dysfunction of glioma stem cells escapes from CTL-mediated immune response via activation of Wnt/beta-catenin signaling pathway. Oncogene. 2020, 39, 1098–1111. [Google Scholar] [CrossRef]
- Yasinjan, F.; Xing, Y.; Geng, H.; Guo, R.; Yang, L.; Liu, Z.; Wang, H. Immunotherapy: A promising approach for glioma treatment. Front Immunol. 2023, 14, 1255611. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.Y.; Li, J.L.; Xu, X.K.; Zheng, M.G.; Wen, C.C.; Li, F.C. HMME-based PDT restores expression and function of transporter associated with antigen processing 1 (TAP1) and surface presentation of MHC class I antigen in human glioma. J Neurooncol. 2011, 105, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Han, Y.; Liu, D.; Li, L. PD-1/PD-L1 pathway: Current researches in cancer. Am J Cancer Res. 2020, 10, 727–742. [Google Scholar] [PubMed]
- Xue, S.; Hu, M.; Iyer, V.; Yu, J. Blocking the PD-1/PD-L1 pathway in glioma: A potential new treatment strategy. J Hematol Oncol. 2017, 10, 81. [Google Scholar] [CrossRef] [PubMed]
- Gurung, P.; Lim, J.; Shrestha, R.; et al. Chlorin e6-associated photodynamic therapy enhances abscopal antitumor effects via inhibition of PD-1/PD-L1 immune checkpoint. Sci Rep 2023, 13, 4647. [Google Scholar] [CrossRef] [PubMed]
- Lobo, C.S.; Mendes, M.I.P.; Pereira, D.A.; et al. Photodynamic therapy changes tumour immunogenicity and promotes immune-checkpoint blockade response, particularly when combined with micromechanical priming. Sci Rep 2023, 13, 11667. [Google Scholar] [CrossRef] [PubMed]
- Anand, S.; Shen, A.; Cheng, C.E.; Chen, J.; Powers, J.; Rayman, P.; Diaz, M.; Hasan, T.; Maytin, E.V. Combination of vitamin D and photodynamic therapy enhances immune responses in murine models of squamous cell skin cancer. Photodiagnosis Photodyn Ther. 2024, 45, 103983. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Tait, S.W.G. Targeting immunogenic cell death in cancer. Mol Oncol. 2020, 14, 2994–3006. [Google Scholar] [CrossRef] [PubMed]
- Nabrinsky, E.; Macklis, J.; Bitran, J. A Review of the Abscopal Effect in the Era of Immunotherapy. Cureus. 2022, 14, e29620. [Google Scholar] [CrossRef] [PubMed]
- Aebisher, D.; Woźnicki, P.; Bartusik-Aebisher, D. Photodynamic Therapy and Adaptive Immunity Induced by Reactive Oxygen Species: Recent Reports. Cancers 2024, 16, 967. [Google Scholar] [CrossRef]
- Turubanova, V.D.; Balalaeva, I.V.; Mishchenko, T.A.; Catanzaro, E.; Alzeibak, R.; Peskova, N.N.; Efimova, I.; Bachert, C.; Mitroshina, E.V.; Krysko, O.; Vedunova, M.V.; Krysko, D.V. Immunogenic cell death induced by a new photodynamic therapy based on photosens and photodithazine. J Immunother Cancer. 2019, 7, 350. [Google Scholar] [CrossRef]
- Shibata, S.; Shinozaki, N.; Suganami, A.; Ikegami, S.; Kinoshita, Y.; Hasegawa, R.; Kentaro, H.; Okamoto, Y.; Aoki, I.; Tamura, Y.; Iwadate, Y. Photo-immune therapy with liposomally formulated phospholipid-conjugated indocyanine green induces specific antitumor responses with heat shock protein-70 expression in a glioblastoma model. Oncotarget. 2019, 10, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Pangal, D.J.; Yarovinsky, B.; Cardinal, T.; Cote, D.J.; Ruzevick, J.; Attenello, F.J.; Chang, E.L.; Ye, J.; Neman, J.; Chow, F.; Zada, G. The abscopal effect: Systematic review in patients with brain and spine metastases. Neurooncol Adv. 2022, 4, vdac132. [Google Scholar] [CrossRef] [PubMed]
- Lin, R.A.; Lin, J.K.; Lin, S.Y. Mechanisms of immunogenic cell death and immune checkpoint blockade therapy. Kaohsiung J Med Sci. 2021, 37, 448–458. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Yu, S.; Wang, X.; Qian, Y.; Wu, W.; Zhang, S.; Zheng, B.; Wei, G.; Gao, S.; Cao, Z.; Fu, W.; Xiao, Z.; Lu, W. High Affinity of Chlorin e6 to Immunoglobulin G for Intraoperative Fluorescence Image-Guided Cancer Photodynamic and Checkpoint Blockade Therapy. ACS Nano. 2019, 13, 10242–10260. [Google Scholar] [CrossRef] [PubMed]
- Yin, N.; Wang, Y.; Liu, Y.; Niu, R.; Zhang, S.; Cao, Y.; Lv, Z.; Song, S.; Liu, X.; Zhang, H. A Cholesterol Metabolic Regulated Hydrogen-Bonded Organic Framework (HOF)-Based Biotuner for Antibody Non-Dependent Immunotherapy Tailored for Glioblastoma. Adv Mater. 2023, 35, e2303567. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Namkoong, H.; Doh, J.; Choi, J.C.; Yang, B.G.; Park, Y.; Chul Sung, Y. Negative role of inducible PD-1 on survival of activated dendritic cells. J Leukoc Biol. 2014, 95, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, M.; Hahn, M.; Michel, J.; Sankowski, R.; Kilian, M.; Kehl, N.; Günter, M.; Bunse, T.; Pusch, S.; von Deimling, A.; Wick, W.; Autenrieth, S.E.; Prinz, M.; Platten, M.; Bunse, L. Dysfunctional dendritic cells limit antigen-specific T cell response in glioma. Neuro Oncol. 2023, 25, 263–276. [Google Scholar] [CrossRef] [PubMed]
- Etminan, N.; Peters, C.; Lakbir, D.; Bünemann, E.; Börger, V.; Sabel, M.C.; Hänggi, D.; Steiger, H.J.; Stummer, W.; Sorg, R.V. Heat-shock protein 70-dependent dendritic cell activation by 5-aminolevulinic acid-mediated photodynamic treatment of human glioblastoma spheroids in vitro. Br J Cancer. 2011, 105, 961–969. [Google Scholar] [CrossRef]
- Rothe, F.; Patties, I.; Kortmann, R.D.; Glasow, A. Immunomodulatory Effects by Photodynamic Treatment of Glioblastoma Cells In Vitro. Molecules. 2022, 27, 3384. [Google Scholar] [CrossRef]
- Vedunova, M.; Turubanova, V.; Vershinina, O.; Savyuk, M.; Efimova, I.; Mishchenko, T.; Raedt, R.; Vral, A.; Vanhove, C.; Korsakova, D.; Bachert, C.; Coppieters, F.; Agostinis, P.; Garg, A.D.; Ivanchenko, M.; Krysko, O.; Krysko, D.V. DC vaccines loaded with glioma cells killed by photodynamic therapy induce Th17 anti-tumor immunity and provide a four-gene signature for glioma prognosis. Cell Death Dis. 2022, 13, 1062. [Google Scholar] [CrossRef] [PubMed]
- Redkin, T.S.; Sleptsova, E.E.; Turubanova, V.D.; Saviuk, M.O.; Lermontova, S.A.; Klapshina, L.G.; Peskova, N.N.; Balalaeva, I.V.; Krysko, O.; Mishchenko, T.A.; Vedunova, M.V.; Krysko, D.V. Dendritic Cells Pulsed with Tumor Lysates Induced by Tetracyanotetra(aryl)porphyrazines-Based Photodynamic Therapy Effectively Trigger Anti-Tumor Immunity in an Orthotopic Mouse Glioma Model. Pharmaceutics. 2023, 15, 2430. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Li, L.; Jia, M.; Liao, Q.; Peng, G.; Luo, G.; Zhou, Y. Dendritic cell vaccines improve the glioma microenvironment: Influence, challenges, and future directions. Cancer Med. 2023, 12, 7207–7221. [Google Scholar] [CrossRef] [PubMed]
- Mazurek, M.; Rola, R. The implications of nitric oxide metabolism in the treatment of glial tumors. Neurochem Int. 2021, 150, 105172. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.I.; Yin, J.H.; Mishra, S.; Mishra, R.; Hsu, C.Y. NO-mediated chemoresistance in C6 glioma cells. Ann N Y Acad Sci. 2002, 962, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.J.; Li, F.; Zhu, D.Y. nNOS and Neurological, Neuropsychiatric Disorders: A 20-Year Story. Neurosci Bull. 2023, 39, 1439–1453. [Google Scholar] [CrossRef] [PubMed]
- Kolluru, G.K.; Siamwala, J.H.; Chatterjee, S. eNOS phosphorylation in health and disease. Biochimie. 2010, 92, 1186–1198. [Google Scholar] [CrossRef] [PubMed]
- Lechner, M.; Lirk, P.; Rieder, J. Inducible nitric oxide synthase (iNOS) in tumor biology: The two sides of the same coin. Semin Cancer Biol. 2005, 15, 277–289. [Google Scholar] [CrossRef] [PubMed]
- Jahani-Asl, A.; Bonni, A. iNOS: A potential therapeutic target for malignant glioma. Curr Mol Med. 2013, 13, 1241–1249. [Google Scholar] [CrossRef] [PubMed]
- Maccallini, C.; Gallorini, M.; Cataldi, A.; Amoroso, R. Targeting iNOS As a Valuable Strategy for the Therapy of Glioma. ChemMedChem. 2020, 15, 339–344. [Google Scholar] [CrossRef]
- Fahey, J.M.; Emmer, J.V.; Korytowski, W.; Hogg, N.; Girotti, A.W. Antagonistic Effects of Endogenous Nitric Oxide in a Glioblastoma Photodynamic Therapy Model. Photochem Photobiol. 2016, 92, 842–853. [Google Scholar] [CrossRef] [PubMed]
- Fahey, J.M.; Stancill, J.S.; Smith, B.C.; Girotti, A.W. Nitric oxide antagonism to glioblastoma photodynamic therapy and mitigation thereof by BET bromodomain inhibitor JQ1. J Biol Chem. 2018, 293, 5345–5359. [Google Scholar] [CrossRef] [PubMed]
- Bazak, J.; Korytowski, W.; Girotti, A.W. Bystander Effects of Nitric Oxide in Cellular Models of Anti-Tumor Photodynamic Therapy. Cancers (Basel). 2019, 11, 1674. [Google Scholar] [CrossRef]
- Merenzon, M.A.; Hincapie Arias, E.; Bhatia, S.; Shah, A.H.; Higgins, D.M.O.; Villaverde, M.; Belgorosky, D.; Eijan, A.M. Nitric oxide synthase inhibitors as potential therapeutic agents for gliomas: A systematic review. Nitric Oxide. 2023, 138-139, 10–16. [Google Scholar] [CrossRef] [PubMed]
- de Groot, J.; Sontheimer, H. Glutamate and the biology of gliomas. Glia. 2011, 59, 1181–1189. [Google Scholar] [CrossRef]
- Pei, Z.; Lee, K.C.; Khan, A.; Erisnor, G.; Wang, H.Y. Pathway analysis of glutamate-mediated, calcium-related signaling in glioma progression. Biochem Pharmacol. 2020, 176, 113814. [Google Scholar] [CrossRef]
- Du, P.; Hu, S.; Cheng, Y.; Li, F.; Li, M.; Li, J.; Yi, L.; Feng, H. Photodynamic therapy leads to death of C6 glioma cells partly through AMPAR. Brain Res. 2012, 1433, 153–159. [Google Scholar] [CrossRef]
- Lyons, S.A.; Chung, W.J.; Weaver, A.K.; Ogunrinu, T.; Sontheimer, H. Autocrine glutamate signaling promotes glioma cell invasion. Cancer Res. 2007, 67, 9463–9471. [Google Scholar] [CrossRef]
- Hu, S.L.; Du, P.; Hu, R.; Li, F.; Feng, H. Imbalance of Ca2+ and K+ fluxes in C6 glioma cells after PDT measured with scanning ion-selective electrode technique. Lasers Med Sci. 2014, 29, 1261–1267. [Google Scholar] [CrossRef]
- Papadopoulos, V.; Lecanu, L.; Brown, R.C.; Han, Z.; Yao, Z.X. Peripheral-type benzodiazepine receptor in neurosteroid biosynthesis, neuropathology and neurological disorders. Neuroscience. 2006, 138, 749–756. [Google Scholar] [CrossRef]
- Starosta-Rubinstein, S.; Ciliax, B.J.; Penney, J.B.; McKeever, P.; Young, A.B. Imaging of a glioma using peripheral benzodiazepine receptor ligands. Proc Natl Acad Sci U S A. 1987, 84, 891–895. [Google Scholar] [CrossRef] [PubMed]
- Takada, A.; et al. Autoradiographic study of peripheral benzodiazepine receptors in animal brain tumor models and human gliomas. European Journal of Pharmacology: Environmental Toxicology and Pharmacology 1992, 228, 131–139. [Google Scholar]
- Veenman, L.; Levin, E.; Weisinger, G.; Leschiner, S.; Spanier, I.; Snyder, S.H.; Weizman, A.; Gavish, M. Peripheral-type benzodiazepine receptor density and in vitro tumorigenicity of glioma cell lines. Biochem Pharmacol. 2004, 68, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Corsi, L.; Geminiani, E.; Baraldi, M. Peripheral benzodiazepine receptor (PBR) new insight in cell proliferation and cell differentiation review. Curr Clin Pharmacol. 2008, 3, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Bisland, S.K.; Goebel, E.A.; Hassanali, N.S.; Johnson, C.; Wilson, B.C. Increased expression of mitochondrial benzodiazepine receptors following low-level light treatment facilitates enhanced protoporphyrin IX production in glioma-derived cells in vitro. Lasers Surg Med. 2007, 39, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Kessel, D.; Antolovich, M.; Smith, K.M. The Role of the Peripheral Benzodiazepine Receptor in the Apoptotic Response to Photodynamic Therapy. Photochemistry and Photobiology 2001, 74, 346–349. [Google Scholar] [CrossRef] [PubMed]
- Sarissky, M.; Lavicka, J.; Kocanová, S.; Sulla, I.; Mirossay, A.; Miskovsky, P.; Gajdos, M.; Mojzis, J.; Mirossay, L. Diazepam enhances hypericin-induced photocytotoxicity and apoptosis in human glioblastoma cells. Vol. 52, NEOPLASMA. BAJZOVA 7, BRATISLAVA, 821 08, SLOVAKIA: AEPRESS SRO; 2005. p. 352–9.
- Chen, J.; Ouyang, Y.; Cao, L.; Zhu, W.; Zhou, Y.; Zhou, Y.; Zhang, H.; Yang, X.; Mao, L.; Lin, S.; Lin, J.; Hu, J.; Yan, G. Diazepam inhibits proliferation of human glioblastoma cells through triggering a G0/G1 cell cycle arrest. J Neurosurg Anesthesiol. 2013, 25, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Lavicka, J.; Sarisský, M.; Mirossay, A.; Sulla, I.; Mojzis, J.; Mirossay, L. Diazepam enhances etoposide-induced cytotoxicity in U-87 MG human glioma cell line. Fundam Clin Pharmacol. 2001, 15, 201–207. [Google Scholar] [CrossRef]
- Drljača, J.; Popović, A.; Bulajić, D.; Stilinović, N.; Vidičević Novaković, S.; Sekulić, S.; Milenković, I.; Ninković, S.; Ljubković, M.; Čapo, I. Diazepam diminishes temozolomide efficacy in the treatment of U87 glioblastoma cell line. CNS Neurosci Ther. 2022, 28, 1447–1457. [Google Scholar] [CrossRef]
- Czarnecka, M.; Lu, C.; Pons, J.; Maheswaran, I.; Ciborowski, P.; Zhang, L.; Cheema, A.; Kitlinska, J. Neuropeptide Y receptor interactions regulate its mitogenic activity. Neuropeptides. 2019, 73, 11–24. [Google Scholar] [CrossRef]
- Körner, M.; Reubi, J.C. Neuropeptide Y receptors in primary human brain tumors: Overexpression in high-grade tumors. J Neuropathol Exp Neurol. 2008, 67, 741–749. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; He, X.; Wang, P.; Yuan, B.; Pan, Y.; Hu, X.; Lu, L.; Wu, A.; Li, J. A D-Y Shaped Neuropeptide Y Mimetic Peptide-Dye Self-Assembly with Maximal Emission Beyond 1300 nm and Glioma Mitochondrial Activity Modulation. Small. 2024, 20, e2308621. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Du, Y.; Jiang, Z.; Tian, Y.; Qiu, N.; Wang, Y.; Lqbal, M.Z.; Hu, M.; Zou, R.; Luo, L.; Du, S.; Tian, J.; Wu, A. Y1 receptor ligand-based nanomicelle as a novel nanoprobe for glioma-targeted imaging and therapy. Nanoscale. 2018, 10, 5845–5851. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Luo, Y.; Li, Y.; Pan, Y.; Kwok, R.T.K.; He, L.; Duan, X.; Zhang, P.; Wu, A.; Tang, B.Z.; Li, J. D-type neuropeptide decorated AIEgen/RENP hybrid nanoprobes with light-driven ROS generation ability for NIR-II fluorescence imaging-guided through-skull photodynamic therapy of gliomas. AGGREGATE. 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY; 2023.
- Moriwaki, K.; Chan, F.K. RIP3: A molecular switch for necrosis and inflammation. Genes Dev. 2013, 27, 1640–1649. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, T.; Lei, T.; Zhang, D.; Du, S.; Girani, L.; Qi, D.; Lin, C.; Tong, R.; Wang, Y. RIP1/RIP3-regulated necroptosis as a target for multifaceted disease therapy (Review). Int J Mol Med. 2019, 44, 771–786. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Zheng, S.Y.; Jiang, R.L.; Wu, H.D.; Li, Y.A.; Lu, J.L.; Xiong, Y.; Han, B.; Lin, L. Necroptosis signaling and mitochondrial dysfunction cross-talking facilitate cell death mediated by chelerythrine in glioma. Free Radic Biol Med. 2023, 202, 76–96. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Wang, W.; Zhang, Y.; Fu, X.; Ping, K.; Zhao, J.; Lei, Y.; Mou, Y.; Wang, S. Synthesis and biological evaluation of celastrol derivatives as potential anti-glioma agents by activating RIP1/RIP3/MLKL pathway to induce necroptosis. Eur J Med Chem. 2022, 229, 114070. [Google Scholar] [CrossRef]
- Zhou, J.; Li, G.; Han, G.; Feng, S.; Liu, Y.; Chen, J.; Liu, C.; Zhao, L.; Jin, F. Emodin induced necroptosis in the glioma cell line U251 via the TNF-α/RIP1/RIP3 pathway. Invest New Drugs. 2020, 38, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; McDonald, D.G.; Dixon-Mah, Y.N.; Jacqmin, D.J.; Samant, V.N.; Vandergrift, W.A., 3rd; Lindhorst, S.M.; Cachia, D.; Varma, A.K.; Vanek, K.N.; Banik, N.L.; Jenrette, J.M., 3rd; Raizer, J.J.; Giglio, P.; Patel, S.J. RIP1 and RIP3 complex regulates radiation-induced programmed necrosis in glioblastoma. Tumour Biol. 2016, 37, 7525–7534. [Google Scholar] [CrossRef]
- Coupienne, I.; Fettweis, G.; Rubio, N.; Agostinis, P.; Piette, J. 5-ALA-PDT induces RIP3-dependent necrosis in glioblastoma. Photochem Photobiol Sci. 2011, 10, 1868–1878. [Google Scholar] [CrossRef]
- Fettweis, G.; Di Valentin, E.; L’homme, L.; Lassence, C.; Dequiedt, F.; Fillet, M.; Coupienne, I.; Piette, J. RIP3 antagonizes a TSC2-mediated pro-survival pathway in glioblastoma cell death. Biochim Biophys Acta Mol Cell Res. 2017, 1864, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Maletínská, L.; Blakely, E.A.; Bjornstad, K.A.; Deen, D.F.; Knoff, L.J.; Forte, T.M. Human glioblastoma cell lines: Levels of low-density lipoprotein receptor and low-density lipoprotein receptor-related protein. Cancer Res. 2000, 60, 2300–2303. [Google Scholar] [PubMed]
- Han, L.; Jiang, C. Evolution of blood-brain barrier in brain diseases and related systemic nanoscale brain-targeting drug delivery strategies. Acta Pharm Sin B. 2021, 11, 2306–2325. [Google Scholar] [CrossRef] [PubMed]
- Pawar, S.; Koneru, T.; McCord, E.; Tatiparti, K.; Sau, S.; Iyer, A.K. LDL receptors and their role in targeted therapy for glioma: A review. Drug Discov Today. 2021, 26, 1212–1225. [Google Scholar] [CrossRef] [PubMed]
- Buzova, D.; Huntosova, V.; Kasak, P.; Petrovajova, D.; Joniova, J.; Dzurova, L.; Nadova, Z.; Sureau, F.; Miskovsky, P.; Jancura, D. Towards increased selectivity of drug delivery to cancer cells: Development of a LDL-based nanodelivery system for hydrophobic photosensitizers. Mohseni H, Agahi M, Razeghi M, editors. BIOSENSING AND NANOMEDICINE V. 1000 20TH ST, PO BOX 10, BELLINGHAM, WA 98227-0010 USA: SPIE-INT SOC OPTICAL ENGINEERING; 2012. (Proceedings of SPIE; vol. 8460).
- Huntosova, V.; Alvarez, L.; Bryndzova, L.; Nadova, Z.; Jancura, D.; Buriankova, L.; Bonneau, S.; Brault, D.; Miskovsky, P.; Sureau, F. Interaction dynamics of hypericin with low-density lipoproteins and U87-MG cells. Int J Pharm. 2010, 389, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Luiza Andreazza, N.; Vevert-Bizet, C.; Bourg-Heckly, G.; Sureau, F.; José Salvador, M.; Bonneau, S. Berberine as a photosensitizing agent for antitumoral photodynamic therapy: Insights into its association to low density lipoproteins. Int J Pharm. 2016, 510, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Huntosova, V.; Nadova, Z.; Dzurova, L.; Jakusova, V.; Sureau, F.; Miskovsky, P. Cell death response of U87 glioma cells on hypericin photoactivation is mediated by dynamics of hypericin subcellular distribution and its aggregation in cellular organelles. Photochem Photobiol Sci. 2012, 11, 1428–1436. [Google Scholar] [CrossRef]
- Song, L.; Li, H.; Sunar, U.; Chen, J.; Corbin, I.; Yodh, A.G.; Zheng, G. Naphthalocyanine-reconstituted LDL nanoparticles for in vivo cancer imaging and treatment. Int J Nanomedicine. 2007, 2, 767–774. [Google Scholar]
- Chen, L.Q.; Cheung, L.S.; Feng, L.; Tanner, W.; Frommer, W.B. Transport of sugars. Annu Rev Biochem. 2015, 84, 865–894. [Google Scholar] [CrossRef]
- Nabavizadeh, A.; Zhao, C.; Martinez, D.; Familiar, A.; Koptyra, M.; Ippolito, J.; Rubin, J.; Storm, P.B.; Resnick, A.C.; Santi, M. TMET-37. SODIUM-DEPENDENT GLUCOSE TRANSPORTER 2 (SGLT2) IS OVEREXPRESSED IN THE MAJORITY OF ATRTS AND A SUBSET OF PEDIATRIC PATIENTS WITH HIGH-GRADE GLIOMA; A POTENTIAL IMAGING AND THERAPEUTIC TARGET. Neuro Oncol. 2022 Nov 14;24(Suppl 7):vii270.
- Liu, Y.; Li, Y.M.; Tian, R.F.; Liu, W.P.; Fei, Z.; Long, Q.F.; Wang, X.A.; Zhang, X. The expression and significance of HIF-1alpha and GLUT-3 in glioma. Brain Res. 2009, 1304, 149–154. [Google Scholar] [CrossRef]
- Jensen, R.L.; Chkheidze, R. (2011). The Role of Glucose Transporter-1 (GLUT-1) in Malignant Gliomas. In: Hayat, M. (eds) Tumors of the Central Nervous System, Volume 1. Tumors of the Central Nervous System, vol 1. Springer, Dordrecht.
- Han, W.; Shi, J.; Cao, J.; Dong, B.; Guan, W. Emerging Roles and Therapeutic Interventions of Aerobic Glycolysis in Glioma. Onco Targets Ther. 2020, 13, 6937–6955. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhang, Z.; Blessington, D.; Li, H.; Busch, T.M.; Madrak, V.; Miles, J.; Chance, B.; Glickson, J.D.; Zheng, G. Pyropheophorbide 2-deoxyglucosamide: A new photosensitizer targeting glucose transporters. Bioconjug Chem. 2003, 14, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Guo, K.; Huang, B.; Lin, Z.; Cai, Z. Role of Glucose Transporters in Drug Membrane Transport. Curr Drug Metab. 2020, 21, 947–958. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Kataoka, H.; Yano, S.; Ohi, H.; Moriwaki, K.; Akashi, H.; Taguchi, T.; Hayashi, N.; Hamano, S.; Mori, Y.; Kubota, E.; Tanida, S.; Joh, T. Antitumor effects in gastrointestinal stromal tumors using photodynamic therapy with a novel glucose-conjugated chlorin. Mol Cancer Ther. 2014, 13, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Nishie, H.; Kataoka, H.; Yano, S.; Kikuchi, J.I.; Hayashi, N.; Narumi, A.; Nomoto, A.; Kubota, E.; Joh, T. A next-generation bifunctional photosensitizer with improved water-solubility for photodynamic therapy and diagnosis. Oncotarget. 2016, 7, 74259–74268. [Google Scholar] [CrossRef] [PubMed]
- Acker, G.; Palumbo, A.; Neri, D.; Vajkoczy, P.; Czabanka, M. F8-SIP mediated targeted photodynamic therapy leads to microvascular dysfunction and reduced glioma growth. J Neurooncol. 2016, 129, 33–38. [Google Scholar] [CrossRef] [PubMed]
- De Groof, T.W.M.; Mashayekhi, V.; Fan, T.S.; Bergkamp, N.D.; Sastre Toraño, J.; van Senten, J.R.; Heukers, R.; Smit, M.J.; Oliveira, S. Nanobody-Targeted Photodynamic Therapy Selectively Kills Viral GPCR-Expressing Glioblastoma Cells. Mol Pharm. 2019, 16, 3145–3156. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Zhou, H.; Liu, Y.; Wen, Y.; Wei, C.; Yu, Q.; Liu, J. Transferrin/aptamer conjugated mesoporous ruthenium nanosystem for redox-controlled and targeted chemo-photodynamic therapy of glioma. Acta Biomater. 2018, 82, 143–157. [Google Scholar] [CrossRef] [PubMed]
- Akhlynina, T.V.; Jans, D.A.; Statsyuk, N.V.; Balashova, I.Y.; Toth, G.; Pavo, I.; Rosenkranz, A.A.; Naroditsky, B.S.; Sobolev, A.S. Adenoviruses synergize with nuclear localization signals to enhance nuclear delivery and photodynamic action of internalizable conjugates containing chlorin e6. Int J Cancer. 1999, 81, 734–740. [Google Scholar] [CrossRef]
- Wu, D.P.; Bai, L.R.; Lv, Y.F.; Zhou, Y.; Ding, C.H.; Yang, S.M.; Zhang, F.; Huang, J.L. A novel role of Cx43-composed GJIC in PDT phototoxicity: An implication of Cx43 for the enhancement of PDT efficacy. Int J Biol Sci. 2019, 15, 598–609. [Google Scholar] [CrossRef]
- An, Y.W.; Liu, H.Q.; Zhou, Z.Q.; Wang, J.C.; Jiang, G.Y.; Li, Z.W.; Wang, F.; Jin, H.T. Sinoporphyrin sodium is a promising sensitizer for photodynamic and sonodynamic therapy in glioma. Oncol Rep. 2020, 44, 1596–1604. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Luk, S.K.; Chuang, C.P.; Yip, S.P.; To, S.S.; Yung, Y.M. TP53 regulates human AlkB homologue 2 expression in glioma resistance to Photofrin-mediated photodynamic therapy. Br J Cancer. 2010, 103, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Oh, S.J.; Shim, J.K.; Ji, Y.B.; Moon, J.H.; Kim, E.H.; Huh, Y.M.; Suh, J.S.; Chang, J.H.; Lee, S.J.; Kang, S.G. C5α secreted by tumor mesenchymal stem-like cells mediates resistance to 5-aminolevulinic acid-based photodynamic therapy against glioblastoma tumorspheres. J Cancer Res Clin Oncol. 2023, 149, 4391–4402. [Google Scholar] [CrossRef] [PubMed]
- Shahmoradi Ghahe, S.; Kosicki, K.; Wojewódzka, M.; Majchrzak, B.A.; Fogtman, A.; Iwanicka-Nowicka, R.; Ciuba, A.; Koblowska, M.; Kruszewski, M.; Tudek, B.; Speina, E. Increased DNA repair capacity augments resistance of glioblastoma cells to photodynamic therapy. DNA Repair (Amst). 2021, 104, 103136. [Google Scholar] [CrossRef]
- Li, F.; Cheng, Y.; Lu, J.; Hu, R.; Wan, Q.; Feng, H. Photodynamic therapy boosts anti-glioma immunity in mice: A dependence on the activities of T cells and complement C3. J Cell Biochem. 2011, 112, 3035–3043. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





