Introduction
Total hip arthroplasty stands as a pivotal recourse for numerous conditions including traumas, malignancies, and rheumatological diseases that impair the hip joint, particularly end-stage osteoarthritis [
1]. With the aging demographic and the rise of contributory factors like obesity and sedentary lifestyles posing a threat to joint health, its application continues to escalate. In the United States alone, over 250,000 procedures are performed annually [
2]. The outcomes of this prevalent surgical intervention exhibit commendable success, yielding favorable functional improvements and in-hospital recovery [
3].
The concept of same-day discharge holds significant advantages for both healthcare services and physicians, serving as a boon both economically and medically [
4]. Particularly in the current landscape where hospital bed costs and the prevalence of resistant infections are on the rise, the adoption of same-day discharge stands as a strategic response [
5,
6]. This approach, recognized for its applicability across various procedures including spinal surgery, has gained traction in recent years, especially within the realm of arthroplasty surgery [
7,
8,
9]. With its implementation and widespread adoption steadily increasing, the same-day discharge model presents a promising avenue for enhancing efficiency and reducing healthcare-associated risks.
We conducted an analysis of same-day discharge outcomes and trends in total hip arthroplasty cases registered within the American College of Surgeons NSQIP registry between 2016 and 2021.
Methods
1. Study Design
This retrospective analysis utilized data from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) Participant Use File spanning 2016 to 2021. The focus was on patients undergoing total hip arthroplasty, identified by CPT code 27130.
CPT code 27130 corresponds to "arthroplasty, acetabular and proximal femoral prosthetic replacement (total hip arthroplasty), with or without autograft or allograft."
The primary aim of this study was to demonstrate the outcomes of patients discharged on the same day following total hip arthroplasty.
2. Database
This retrospective analysis utilized data from the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) Participant Use File, spanning the period from 2016 to 2021. ACS NSQIP is a comprehensive initiative focused on collecting and assessing preoperative risk factors and 30-day postoperative outcomes in surgical patients [
10]. It provides a standardized, risk-adjusted approach for comparing outcomes across different hospitals. The data, meticulously compiled by specialized surgical reviewers, undergoes rigorous auditing processes to ensure accuracy and consistency. The study specifically focused on individuals who underwent CPT code 27130 procedures, encompassing 235,393 patients from a large pool of over 5.5 million.
3. Current Procedural Terminology Codes (CPTs)
CPT code 27130 denotes "arthroplasty, acetabular and proximal femoral prosthetic replacement (total hip arthroplasty), with or without autograft or allograft." This procedure involves the precise surgical replacement of the acetabulum and proximal femur with prosthetic components, tailored to the patient's specific anatomical needs[
11]. Autograft or allograft may be incorporated to augment bone structure, enhancing stability and long-term functionality.
Perioperative Factors:
In our study, we utilized a comprehensive array of perioperative factors to discern differences between patients discharged on the same day of surgery and those requiring hospitalization. These factors encompassed various demographic characteristics, including gender, age, and ethnic background, alongside medical comorbidities such as diabetes mellitus, smoking status, hypertension, and chronic pulmonary conditions. Additionally, we examined functional status prior to surgery as well as operative time and the year of operation to capture temporal trends. Notably, urgent surgeries were also considered, reflecting the acuity of the surgical interventions.
Postoperative 30-Day Outcomes
In the study, we utilized a comprehensive set of variables to discern 30-day outcomes disparities between patients discharged on the same day of hip surgery and those requiring hospitalization. These variables encompassed critical aspects of postoperative care, including the mean length of stay, 30-day readmission rates for any reason, 30-day readmission specifically related to the procedure, 30-day reoperation rates, occurrences of more than two reoperations within 30 days, and 30-day mortality rates.
1. Statistical Analysis
In the univariate analysis, categorical variables were presented as numbers and percentages (n, %). Statistical significance was determined using the Chi-square test and Fisher's exact test, maintaining a significance level of 0.05. This analysis allowed for the examination of the relationship between each individual variable and the outcomes of interest, providing initial insights into potential associations.
Following the univariate analysis, multivariate regression techniques were employed to further explore the relationship between the categorical variables and various clinical outcomes. Logistic regression analysis was utilized to assess the impact of different preoperative and postoperative factors on clinical outcomes while adjusting for potential confounding variables. This approach enabled the identification of independent predictors of adverse events and other outcomes following revision total hip arthroplasty. By incorporating multiple variables simultaneously, the multivariate regression analysis provided a more comprehensive understanding of the factors influencing patient outcomes, contributing to the robustness of the study findings.
Results
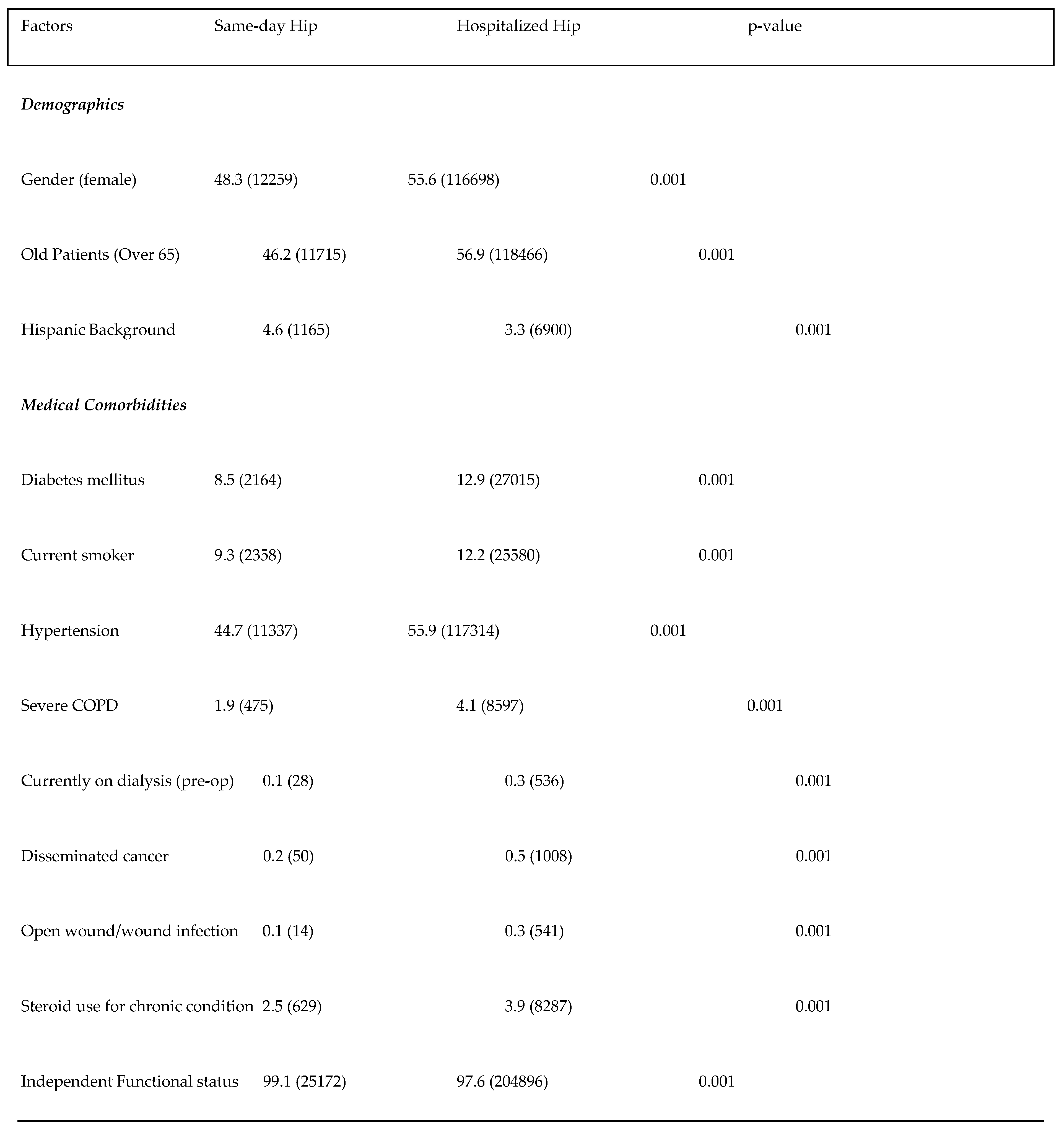
The preoperative status analysis, as summarized in
Table 1, revealed notable differences between patients undergoing same-day hip surgery and those requiring hospitalization. In terms of demographics, a higher proportion of female patients underwent hospitalized hip surgery compared to same-day hip surgery (55.6% vs. 48.3%, p < 0.001). Similarly, a greater percentage of older patients (over 65 years) and individuals with a Hispanic background were observed in the hospitalized hip group compared to the same-day hip group (p < 0.001 for both). Regarding medical comorbidities, hospitalized hip patients exhibited higher rates of diabetes mellitus, current smoking, hypertension, severe COPD, current dialysis, disseminated cancer, open wound or wound infection, and steroid use for chronic conditions compared to same-day hip patients (p < 0.001 for all). However, independent functional status prior to surgery was notably high in both groups, with a slightly higher percentage observed in the same-day hip cohort (99.1% vs. 97.6%, p < 0.001).
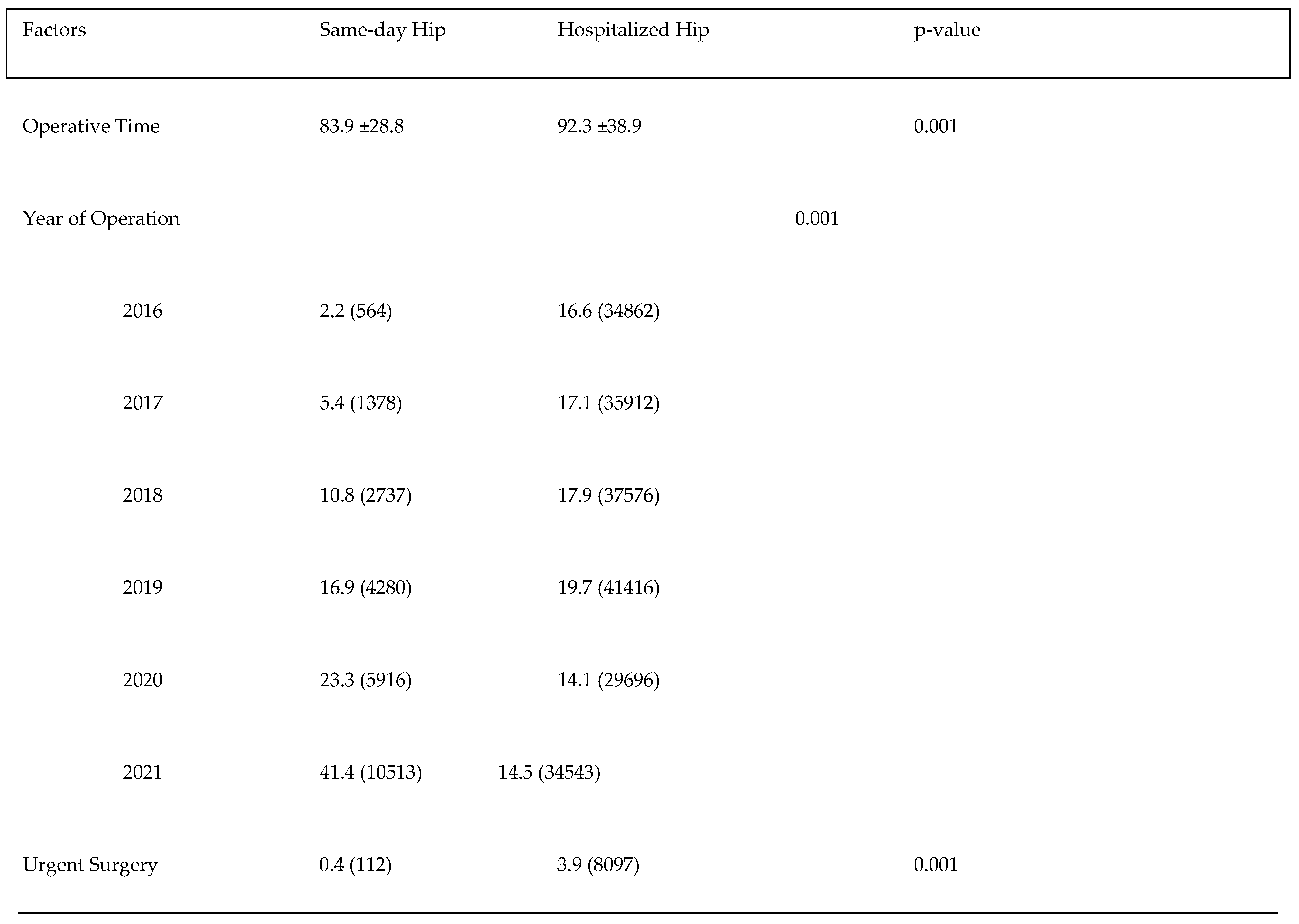
The analysis presented in
Table 2 highlights significant differences between patients undergoing same-day hip surgery and those requiring hospitalization, particularly regarding operative factors. Operative time was notably shorter for same-day hip surgery patients compared to hospitalized hip patients (83.9 ± 28.8 minutes vs. 92.3 ± 38.9 minutes, p < 0.001), indicating a streamlined surgical process for same-day procedures. Moreover, the year of operation demonstrated a significant association with discharge status (p < 0.001), with a notable increase in same-day hip surgeries observed over the years. Specifically, there was a gradual rise in the proportion of same-day hip surgeries from 2016 to 2021, reflecting a trend towards greater adoption of this approach. Conversely, urgent surgeries were more common among hospitalized hip patients compared to those undergoing same-day surgery (3.9% vs. 0.4%, p < 0.001), suggesting that urgent cases may necessitate hospitalization for further observation and management.
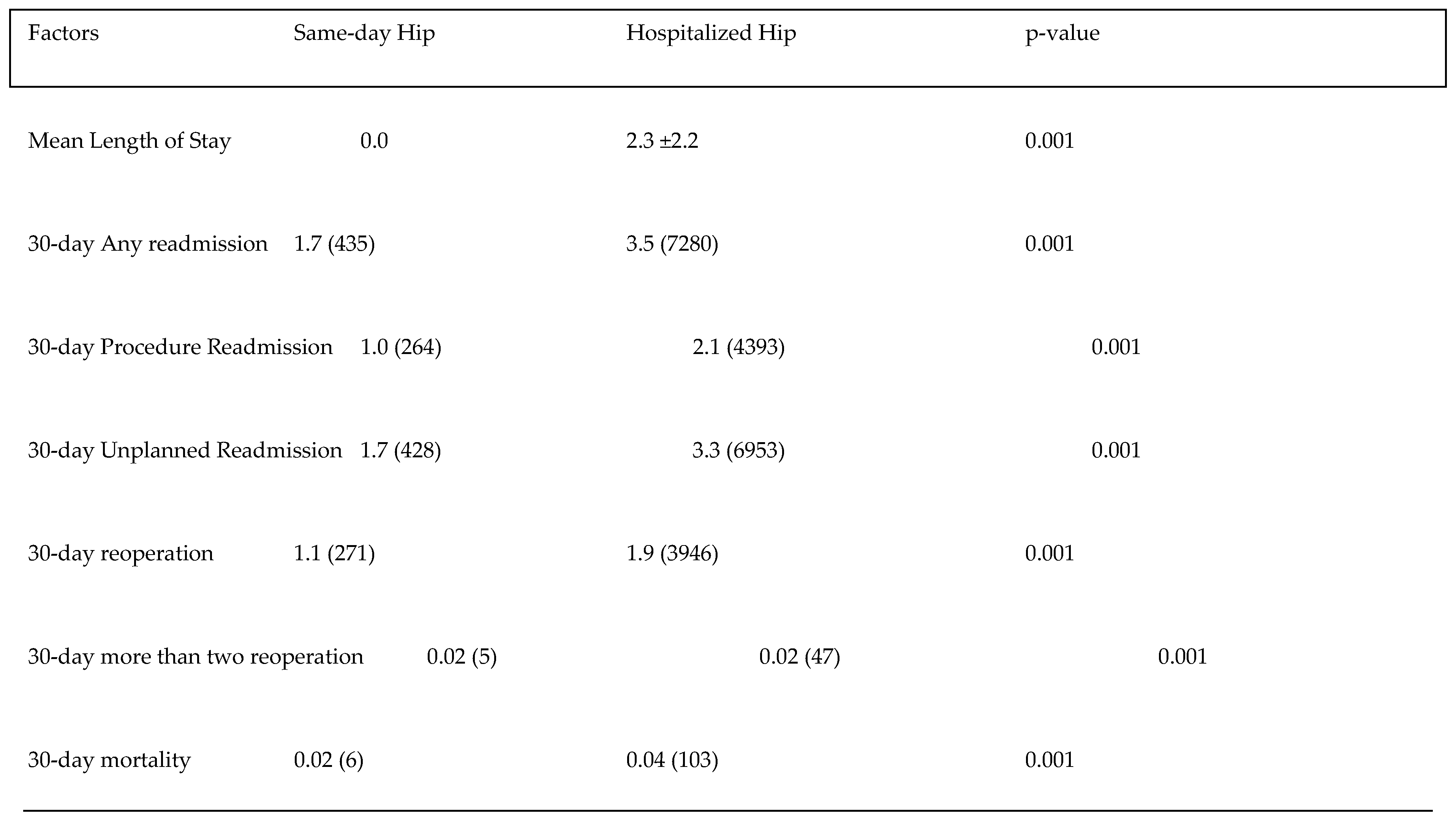
Table 3 presents the postoperative outcomes for patients undergoing same-day hip surgery compared to those requiring hospitalization. Significant differences were observed across various metrics. 30-day readmission rates were lower among same-day hip surgery patients compared to hospitalized patients, both for any reason (1.7% vs. 3.5%, p < 0.001) and specifically related to the procedure (1.0% vs. 2.1%, p < 0.001). Reoperation rates within 30 days were also lower for same-day hip surgery patients compared to the hospitalized group (1.1% vs. 1.9%, p < 0.001), as were instances of more than two reoperations within the same timeframe (0.02% vs. 0.02%, p < 0.001). Furthermore, although both cohorts experienced low mortality rates within 30 days post-surgery, the same-day hip surgery patients exhibited a slightly lower incidence compared to the hospitalized group (0.02% vs. 0.04%, p < 0.001).
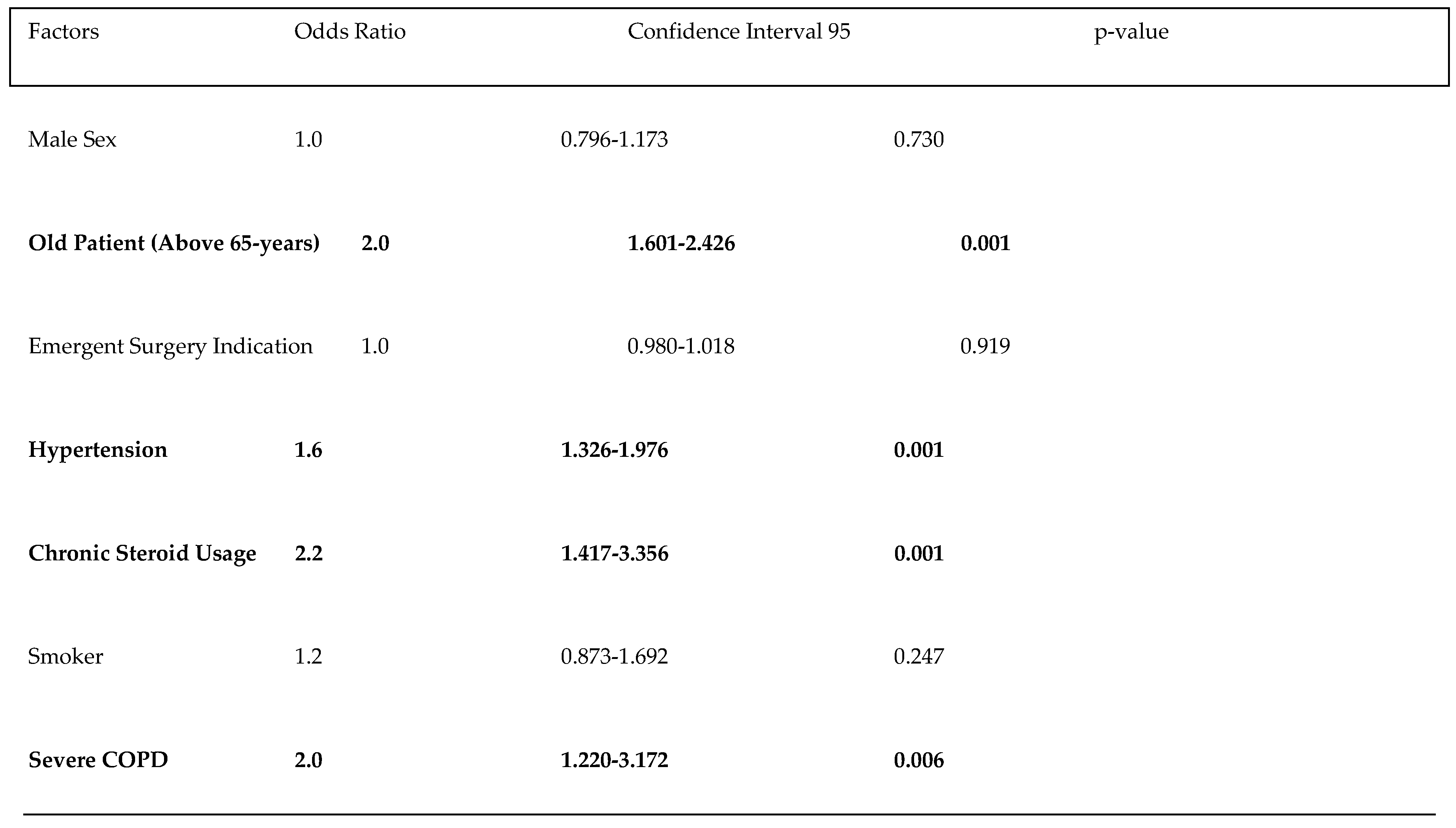
Table 4 presents the independent predictors of unplanned readmission within the same-day group, highlighting several factors with varying levels of statistical significance. Male sex was not a significant predictor, with an odds ratio (OR) of 1.0 (95% CI: 0.796-1.173, p=0.730). In contrast, patients older than 65 years had a significantly increased risk of readmission, with an OR of 2.0 (95% CI: 1.601-2.426, p=0.001). Emergent surgery indication did not significantly affect readmission likelihood (OR: 1.0, 95% CI: 0.980-1.018, p=0.919). Hypertension was associated with a 1.6 times higher risk of readmission (95% CI: 1.326-1.976, p=0.001). Chronic steroid usage markedly increased the risk, with an OR of 2.2 (95% CI: 1.417-3.356, p=0.001). Smoking status, however, was not a significant predictor (OR: 1.2, 95% CI: 0.873-1.692, p=0.247). Finally, severe chronic obstructive pulmonary disease (COPD) was associated with a significantly higher risk of readmission, with an OR of 2.0 (95% CI: 1.220-3.172, p=0.006). These findings underscore the importance of age, hypertension, chronic steroid usage, and severe COPD as significant predictors of unplanned readmissions.
The Figure 1, illustrates a notable shift in the percentage of same-day discharge compared to hospitalization rates over the years for hip surgeries. In 2016, only 1.5% of patients were discharged on the same day, while the vast majority, 97.5%, required hospitalization. However, this trend gradually evolved, with an increasing proportion of patients being discharged on the same day in subsequent years. By 2021, the percentage of same-day discharges had risen to 25.6%, while the percentage of hospitalized patients decreased to 73.4%.
Discussion
The main outcomes of this study underscored the feasibility and safety of same-day discharge following total hip arthroplasty, even among patients with comorbidities. The research revealed that individuals with underlying health conditions could undergo same-day discharge without compromising safety or outcomes. Additionally, the study identified an increasing trend in same-day discharge rates over the study period, indicating a growing acceptance and adoption of this practice in clinical settings. Furthermore, we have determined that potential predictors of risk of unplanned readmission after same-day discharge. These findings collectively highlighted the potential benefits of same-day discharge, not only in terms of resource optimization but also in enhancing patient experience and improving healthcare efficiency. In addition, these findings also provide insight into predicting potential readmissions in same-day discharge patients.
The concept of same-day discharge traditionally suggests selecting patients who are in better clinical condition and can tolerate surgery more effectively. However, our study challenges this notion by revealing that patients with severe comorbidities, such as severe COPD, dialysis dependence, and even disseminated cancer, were discharged on the same day of surgery. While there may be a selection bias inherent in the concept and same-day discharge may seem advantageous in terms of comorbidities, it is crucial to highlight the significance of being able to discharge patients with severe comorbidities on the same day. Another noteworthy aspect is that approximately 12,000 patients over the age of 65 were discharged on the same day. These findings not only underscore the need for careful consideration of patient selection criteria but also signifies a significant advancement in the implementation of same-day discharge protocols, even for high-risk/frail patients.
Numerous recent studies in the current literature, same-day discharge has been found to be superior to hospitalization in terms of readmission rates, revision surgeries, and functional outcomes [
8,
9,
12,
13,
14,
15]. However, it is important to remember that same-day discharge patients are selected based on surgical preference, introducing potential bias. In our study, out of 25,388 patients discharged on the same day, only 264 of them returned to the hospital for procedure-related reasons; this rate is significantly lower than the hospitalized patients. Additionally, 30-day mortality was significantly lower compared to hospitalization, with only six cases observed out of nearly 25,000 patients. These findings suggest that while same-day discharge may offer advantages over hospitalization, careful patient selection and close postoperative monitoring remain essential to ensure optimal outcomes.
Few previous studies have focused on predicting patient readmissions. Identifying patients who will be readmitted to the hospital on the same day as their discharge is crucial for effective patient selection and the development of home follow-up strategies and protocols [
12,
13,
14,
15,
16,
17,
18]. Previous research has indicated that cardiovascular issues and certain systemic comorbidities serve as predictors of unplanned readmission following same-day discharge [
16,
17]. While secondary medical causes are recognized as significant risk factors, our study also highlights the importance of lifestyle and demographic factors, such as chronic steroid use, in predicting readmissions. Our study also demonstrated that emergent surgery is not an independent risk factor for unplanned readmissions following same-day discharge. This is also important for decision making for emergent THA patients.
The increasing trend towards same-day discharge following total hip arthroplasty, as evidenced by numerous studies and reports, including those from the American Academy of Orthopedic Surgeons (AAOS), underscores a paradigm shift in surgical practices and healthcare delivery [
18,
19]. Our study corroborates this trend, revealing a substantial rise in the proportion of patients discharged on the same day over the study period. In 2016, only a small fraction of patients underwent same-day discharge, with the vast majority necessitating hospitalization. However, by 2021, this landscape had transformed significantly, with a notable increase in the percentage of same-day discharges and a corresponding decrease in the proportion of hospitalized patients. This shift reflects the growing acceptance and adoption of same-day discharge protocols among clinicians and healthcare institutions, driven by advancements in surgical techniques, anesthesia protocols, and perioperative care pathways.
Conclusions
In conclusion, the findings of this study underscore the feasibility and safety of same-day discharge following total hip arthroplasty, even among patients with comorbidities. Our research reveals that individuals with underlying health conditions can undergo same-day discharge without compromising safety or outcomes. Moreover, the increasing trend in same-day discharge rates over the study period highlights the growing acceptance and adoption of this practice in clinical settings. These findings collectively emphasize the potential benefits of same-day discharge, not only in terms of resource optimization but also in enhancing patient experience and improving healthcare efficiency.
Funding
This study was not supported by any funding.
Authors' contributions
H.B conceived and designed the study. D.T. extracted the data. H.B analyzed the data. H.B, M.M, and D.T interpreted the data and wrote the manuscript. H.B and D.T contributed to the critical revision of the manuscript for important intellectual content. All authors approved the final version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Availability of data and material
The data for this study were taken from the NSQIP database.
Ethics approval and consent to participate
Not applicable; for this type of study due to NSQIP database nature.
Consent for publication
Not applicable; for this type of study consent for publication is not required.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Abbreviations
ACS NSQIP - American College of Surgeons National Surgical Quality Improvement Program: THA - Total Hip Arthroplasty: CPT - Current Procedural Terminology: COPD - Chronic Obstructive Pulmonary Disease: BMI - Body Mass Index: AAOS - American Academy of Orthopedic Surgeon
References
- Karachalios T, Komnos G, Koutalos A (2018) Total hip arthroplasty. In: EFORT open reviews. [CrossRef]
- Shichman I, Roof M, Askew N, et al (2023) Projections and Epidemiology of Primary Hip and Knee Arthroplasty in Medicare Patients to 2040-2060. JBJS Open Access 8:. [CrossRef]
- Shapira J, Chen SL, Rosinsky PJ, et al (2020) Outcomes of outpatient total hip arthroplasty: A systematic review. HIP International 31:4–11. [CrossRef]
- Lutz RW, Post ZD, Thalody HS, et al (2024) Success of Same-Day Discharge Total Hip and Knee Arthroplasty: Does Location Matter? The Journal of Arthroplasty 39:8–12. [CrossRef]
- Shi Y, Zhu P, Jia J, et al (2022) Cost-effectiveness of Same-day Discharge Surgery for Primary Total Hip Arthroplasty: A Pragmatic Randomized Controlled Study. Frontiers in Public Health 10:. [CrossRef]
- Perencevich EN, Sands KE, Cosgrove SE, et al (2003) Health and Economic Impact of Surgical Site Infections Diagnosed after Hospital Discharge. Emerging Infectious Diseases 9:196–203. [CrossRef]
- Basil GW, Wang MY (2019) Trends in outpatient minimally invasive spine surgery. Journal of Spine Surgery 5:S108–S114. [CrossRef]
- Meding JB, Berend ME (2015) Outpatient total joint arthroplasty: Is the paradigm changing? Seminars in Arthroplasty 26:210–212. [CrossRef]
- DeCook CA (2019) Outpatient Joint Arthroplasty: Transitioning to the Ambulatory Surgery Center. The Journal of Arthroplasty 34:S48–S50. [CrossRef]
- Jones RS, Brown C, Opelka F (2005) Surgeon compensation: “Pay for performance,” the American College of Surgeons National Surgical Quality Improvement Program, the Surgical Care Improvement Program, and other considerations. Surgery 138:829–836. [CrossRef]
- Article - Billing and Coding: Total Hip Arthroplasty (A57683). https://www.cms.gov/medicare-coverage-database/view/article.aspx?articleId=57683.
- Migliorini F, Cipollaro L, Cuozzo F, et al (2021) Outpatient Total Hip Arthroplasty: A Meta-Analysis. Applied Sciences 11:6853. [CrossRef]
- Pansard E, Klouche S, Bauer T, et al (2020) Can primary total hip arthroplasty be performed in an outpatient setting? Prospective feasibility and safety study in 321 patients in a day-surgery unit. Orthopaedics & Traumatology: Surgery & Research 106:551–555. [CrossRef]
- Verdier N, Boutaud B, Ragot P, et al (2022) Same-day discharge to home is feasible and safe in up to 75% of unselected total hip and knee arthroplasty. International Orthopaedics 46:1019–1027. [CrossRef]
- Dove JH, Laperche JM, Kutschke MJ, et al (2024) The Effect of Surgical Approach on the Outcomes of Same-Day Discharge Outpatient Total Hip Arthroplasty at a Single Ambulatory Surgery Center. The Journal of Arthroplasty 39:398–401. [CrossRef]
- Foley DP, Ghosh P, Ziemba-Davis M, et al (2023) Predictors of Failure to Achieve Planned Same-Day Discharge after Primary Total Joint Arthroplasty: A Multivariable Analysis of Perioperative Risk Factors. Journal of the American Academy of Orthopaedic Surgeons 32:e219–e230. [CrossRef]
- Gazendam AM, Tushinski D, Patel M, et al (2022) Causes and predictors of failed same-day home discharge following primary hip and knee total joint arthroplasty: A Canadian perspective. HIP International 33:576–582. [CrossRef]
- Pasqualini I, Turan O, Emara AK, et al (2024) Outpatient Total Hip Arthroplasty Volume up Nearly 8-Fold After Regulatory Changes With Expanding Demographics and Unchanging Outcomes: A 10-Year Analysis. The Journal of Arthroplasty. [CrossRef]
- Center NLM (2020) Same Day Discharge Arthroplasty: The Time is Now. https://www.aaos.org/videos/video-detail-page/22868__Videos.
Table 1.
Preoperative status.
Table 1.
Preoperative status.
Table 3.
Postoperative Outcomes.
Table 3.
Postoperative Outcomes.
Table 4.
Independent Predictors of Unplanned Readmission in Same-day Group.
Table 4.
Independent Predictors of Unplanned Readmission in Same-day Group.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).