Introduction
Stones are the most common gallbladder disease, afflicting a median of 6-22% of population in European Countries, with higher prevalence in females (14,6%) than males (6,7%) [
1]. In 80% of cases the patients stay asymptomatic throughout their life, whereas 20% of patients with cholelithiasis can develop a complication such as acute cholecystitis, acute pancreatitis and in a 5-20% of cases, choledocholithiasis [
2].
Until about 20 years ago the classical approach to the cholecysto-choledocholithiasis (CCL) was open cholecystectomy with intraoperative cholangiography followed by open common bile duct clearance. With the increased use of advanced laparoscopy and operative pancreaticobiliary endoscopy, the management has profoundly changed [
3,
4,
5,
6].
Actually, the two stage technique combining ERCP and common bile duct (CBD) clearance before a cholecistectomy represents the most common approach for CBD stones [
3,
7]. Although ERCP still remains the gold standard method of treatment for choledocholithiasis, it can be challenging to cannulate the papilla in some cases and the technique carries the burden of post-operative complications such as pancreatitis, stenosis of the ampulla and recurrent choledocolithiasis [
8,
9].
Different techniques have been proposed to manage CCL in a single operative session, including laparoscopic cholecistectomy (LC) along with laparoscopic common bile duct exploration (LCBDE), LC plus trans-cystic bile duct exploration, LC plus intraoperative ERCP, and laparo- endoscopic rendez vous (LERV). Laparoscopic CBD exploration and trans cystic CBD clearance are not currently widely used, due to the need of advanced laparoscopic skills and long learning curve [
10].
In 1993, Deslandres proposed a technique that combined LC with intraoperative cholangiography (IOC) and subsequent endoscopic stone removal in a single-stage and the procedure was termed Laparo-Endoscopic Rendez-Vous (LERV) [
11]. Thereafter, many authors explored this type of approach highlighting the significant improvement in CBD clearance rate, post-operative pancreatitis occurrence and length of stay when adopting LERV compared to the conventional two- stage approach [
12,
13]. However, since there is no clear consensus about the optimal method of management of concomitant gallstones and CBD stones, we aim to evaluate the role of LERV for the treatment of CCL in this retrospective multicentric study.
Materials and Methods
A retrospective observational review of clinical cases of CCL observed in General Surgery Units of “F. Renzetti” Hospital in Lanciano (Chieti, Italy) and “Casa di Cura Luigi Pierangeli” (Pescara, Italy) was carried out.
The surgical and endoscopical equipes involved in the study have performed in their career at least 30 LERVs and 50 ERCP procedures respectively, having both almost 10 years-experience in complex hepatopancreaticobiliary procedures.
From January 2018 to December 2023, 1554 consecutive LCs for gallstones were performed in the two above mentioned facilities. When the preoperative work up was indicative for concomitant choledocolithiasis, a single-stage approach was routinely planned after multidisciplinary meeting with endoscopists, surgeons and radiologists, regardless of the elective or urgent setting. The diagnosis was based on clinical and radiological features, including the presence of altered liver function tests and typical findings of CCL at ultrasound (CBD diameter greater than 10mm or direct visualization of stones), CT scan and/or magnetic resonance cholangiography (cMRI). Patients with clinical diagnosis of acute cholangitis with septic shock, impacted choledocal stones (diameter of stones > 1.5 cm) or suspected malignant stenosis were scheduled for pre-operative ERCP and excluded from our analysis.
The collection of demographic data included age, gender and ASA (American Society of Anaesthesiologists) score. The primary end-point was to evaluate the efficacy in obtaining the CBD complete clearance. The secondary end-point were morbidity, mortality, operative time, conversion rate, in-hospital stay and late recurrence of CBD stones. Evaluating morbidity, Clavien-Dindo score system of complications after surgery was applied and included post-procedural pancreatitis, perforation, bleeding, intra-abdominal or port-site infections, bile leak, cholangitis, residual choledocholithiasis, thromboembolism [
14].
Laparoendoscopic Rendez-Vous: Technical Details
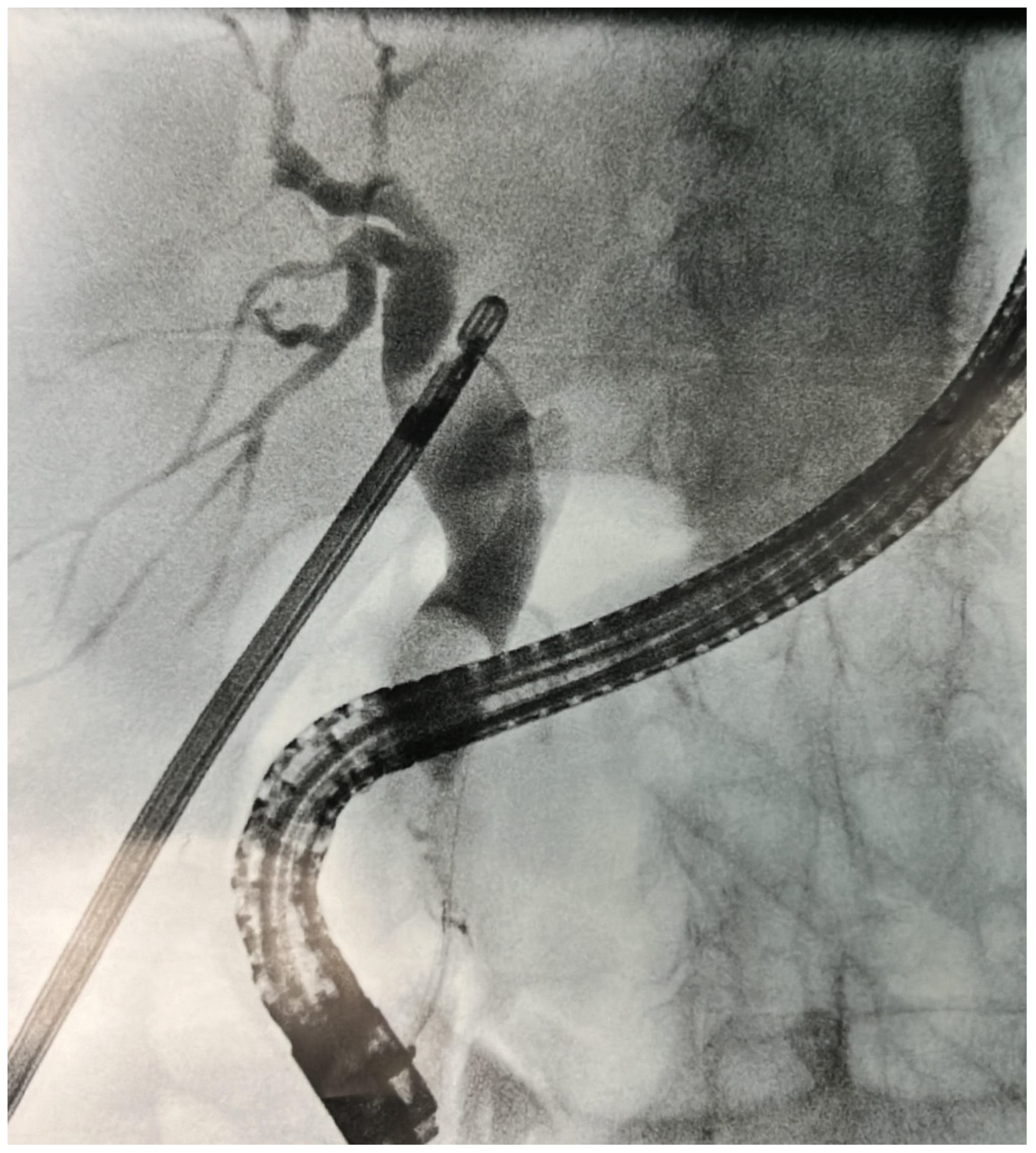
LC was performed with standard 4-port technique; the first surgeon operating between the patient’s legs and the assistant surgeon on the left side (French position). After a careful identification of the Calot’s triangle, dissection and division of the cystic artery was carried out. This step was then followed by the incision of the cystic duct and insertion of a 5F urological catheter (Bracci-catheter) through the cut for intra-operative cholangiography using an Olsen clamp. After completing the cholangiography, an hydrophilic guidewire (Jagwire™, Boston Scientific©, Massachussets, USA) was advanced through the catheter, sticking out through the sphincter of Oddi in the duodenum as reported in
Figure 1. The endoscopic phase undertook when the tip of the wire was identified through scope, grabbed with a snare and carefully pulled out of patient’s oral cavity. A sphincterotome was introduced along the guide, allowing the direct and selective cannulation of the papilla. Choledochal cannulation was then followed by a traditional sphincterotomy or papillary balloon dilatation (papilloplasty) when necessary. After CBD exploration, the stones were removed using a Fogarty angioplasty catheter and/or Dormia basket in case of larger calculi. Complete removal of obstruction was finally confirmed by an endoscopic cholangiography. In case of suspected incomplete clearance or intraprocedural endoscopic bleeding, a biliary plastic or uncovered metallic stent was introduced in CBD. After the endoscopic phase of the procedure, the laparoscopic procedure was completed by clipping cystic duct, dissecting the gallbladder from the liver bed and placing in the retrieval bag for extraction. Before wound closure, an intraabdominal drainage was placed in all cases.
Results
A total of 120 patients presenting CCL were treated with LERV between January 2018 and December 2023. Emergency cases was medically treated and scheduled for elective procedure during the same hospitalization according to the Tokyo guidelines [
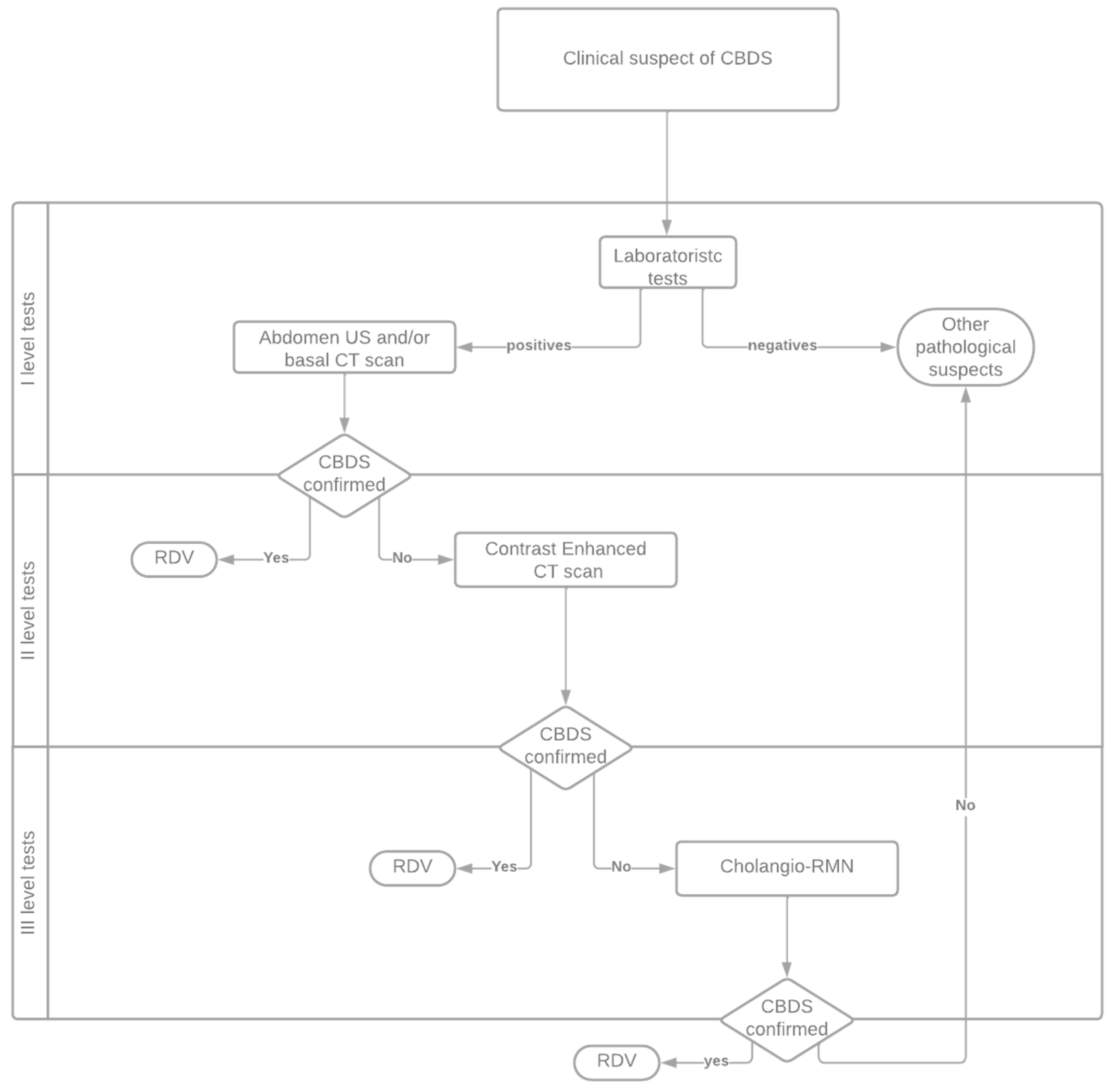
15]. Preoperative assessment of patient was carried out with a personalised diagnostic/therapeutical flowchart based on European Society of Gastroenterology (ESGE) [
16] indications as showed in
Figure 2. Any previous abdominal surgery was not an exclusion criteria for a laparoscopic approach. Eight patients had a previous Billroth-2 partial gastrectomy and in two of these a previous failed ERCP due to difficult CBD cannulation was reported.
Demographical data, patients characteristics and post-operative characteristics are summarised in
Table 1.
The median operative time was 122 (range 95-220) min. The median hospital stay was 4 days (range 2-38). No post-operative mortality was observed. The overall morbidity was 15% (18/120 pts). In detail, 10 mild post-operative pancreatitis and 1 surgical site infection occurred. In one case a patient who experienced mild pancreatitis required a prolonged antibiotics treatment due to concomitant cholangitis. Two severe surgical complications occurred both requiring a laparoscopic re-operation: in one case a postoperative intraperitoneal bleeding due to wide adhesiolysis was reported, in the other case a bile leak due to unrecognized Luschka duct lead to a intraabdominal abscess and bilioma. Bleeding after endoscopic sphincterotomy occurred in 4 cases, requiring blood transfusions in 3 cases and endoscopic haemostasis in 1 case, respectively. Conversion to open surgery was necessary in 2 patients: one patient because of adhesions after partial gastrectomy and one for abnormal bowel distension after ERCP which prevented completion of LC.
In all patients CBD’s cannulation with hydrophilic jag wire through the cystic duct was obtained. A successful duct clearance was acquired in 97%, in 4 patients a redo-ERCP was necessary during the same hospitalization.
Eleven patients (9%) required a biliary plastic stents positioning for preventive purpose only (intraoperative papillary bleeding or suspected impacted stones / incomplete clearance). In all cases the subsequent biliary stent removal and cholangiography showed no persistent CBD stones. At a median follow up of 14 months (range 3-59), five patients experienced stone recurrence, requiring in 2 cases a redo-ERCP.
Discussion
CCL implies the concomitant presence of stones in both the gallbladder and the common bile duct. Most patients remain asymptomatic for a long time, and over a 15 year long follow up only 25% of patients will develop overt disease.
Surgical or endoscopic CBD clearance with simultaneous (one-stage technique) or delayed (two-stage technique) LC are the strategies of choice for CCL management, but according to current literature there is still no agreement yet on which is indisputably the most successful technique.
A single procedure is definitely convenient for the patient and it means that in one hospital stay CCL can be thoroughly addressed. Among the one-stage procedures, the LERV technique combines laparoscopic and endoscopic treatment of CCL [
11,
17], but in the last 20 years the evolution of laparoscopic surgery and the expanded skills of some surgeons especially in Eastern countries, have brought up an another one-stage feasible option in the treatment of CCL: the laparoscopic common bile duct exploration (LCBDE). Many studies comparing LCBDE with LERV or two-stage technique showed that the first one is associated to a shorter in-hospital stay, lower post-operative pancreatitis, higher CBD stone clearance rate, higher post-operative bile leakage rate. Despite this, limitations to the diffusion of the LCBDE are the logistic feasibility in clinical practice requiring also expertise and advanced laparoscopic skills. Among European countries, Alexakis eth al reported in his metanalysis that in Germany the two-stage management was the preferred method in 99% of patients with suspected CBD stones and there was a conversion rate in the 43% of patients when LCBDE was attempted. On the other hand, in UK about 61% of upper-gastrointestinal or hepatobiliarypancreatic surgeons performed laparoscopic CBD exploration (LCBDE) when a single-stage technique was pursued, 25% demanding postoperative ERCP and 13% performing either LCBDE or ERCP when they encountered CBD stones [
18]. Nevertheless, the trend over the last decade continues not so much towards LCBDE utilisation in favour of endoscopic only (two-stage sequential approach) or LERV procedures, resulting in a decreased familiarity with LCBDE by senior surgeons and their trainees [
10,
19,
20,
21,
22].
Compared to the two stage approach (LC plus ERCP), LERV can be associated to higher efficacy and a better safety profile [
23,
24,
25,
26]. In one of the most significant research in literature, Ricci et al. reported that the combined LC and intraoperative ERCP approach (LERV) has the greatest odd to be the safest and the most successful choice [
22]. Regarding the post-ERCP pancreatitis rate, literature reports that it ranges between 1.6 to 15.1%, meaning that widely adopted sequential approach (pre-ERCP plus LC) is less beneficial [
17,
22]
However, not all authors of the current literature confirm a superiority of the single stage approach compared to the two-stage one [
3,
27,
28,
29,
30].
Our experience showed results in line with those reported by the current literature. LERV technique was effective allowing a CBD clearance in 116 cases (97% success rate). Despite that, four patients required a redo-ERCP for incomplete CBD clearance due to impacted stones. In all cases a successful cannulation of CBD was accomplished, that was in significantly contrast with the current rate of 5-20% of failed biliary cannulation during ERCP. Furthermore, this aspect is even more interesting considering that 8 patients had a surgically altered anatomy (previous Billroth-2 partial gastrectomy) and in two of these cases a previous failed ERCP was reported due to difficult CBD cannulation. During LERV, a higher rate of selective CBD cannulation and the avoidance of high pressure injection of the contrast medium into the pancreatic duct are directly related with the lower rate of post-ERCP pancreatitis [
30,
31,
32]. Preventing redo-ERCP after failed biliary cannulation allows lower complications rate and patient’s discomfort compared to the two-stage approach [
33,
34].
Our series showed a 15 % of overall morbidity, that was an interesting safety profile. As reported in
Table 1, only 2.5% of patients experienced severe complications requiring intervention or reoperation (Clavien-Dindo 3a or 3b). Almost of patients who experienced complications had mainly mild (or biochemical) post-operative pancreatitis which did not affect the post-operative course.
Confirming the effectiveness of LERV in CBD clearance, in the subgroup of patients (9%) that required a preventive positioning of biliary plastic stents during LERV, ended up with the stent removal and verification through cholangiography of no persistent CBD stones. Moreover, at a median follow up of 14 months (range 3-59), only five patients experienced stone recurrence, requiring in 2 cases a redo-ERCP.
Not less important, many studies stated that LERV is associated to a shorter hospital stay when compared with the traditional two stage treatment [
22,
35,
36,
37,
38,
39,
40]. These data are confirmed by our experience, where a median of 4 (2-38) days hospital stay was reported. Also, the two stage approach presents the drawback of the waiting period required to ensure that no post-ERCP complication has occurred before proceeding to cholecystectomy.
Despite the numerous
pros of the LERV, two-stage approach (pre-operative ERCP followed by LC) still remains the treatment of choice in many facilities [
5,
17,
18,
22,
27,
28,
41]. The feasibility of a one-stage procedures such as LERV is not straightforward, it requires a good operating room organisation and coordination of the dedicated surgical and endoscopic equipes, also in emergency settings.
Therefore is not unforeseen that scheduling separately the two teams seems easier to manage. Moreover, the shortage of skilled biliary endoscopists and the difficulties or even the lack of cooperation between endoscopic and surgical teams pushes the decision towards the two stage technique [
25,
42]. In our work, we endeavour to manage and organise the operating rooms and the teamwork in the best way possible to achieve close collaboration and improved outcomes in the long run [
43]. Besides that, it is important to underline that LERV needs only basic and cheap laparoscopic equipment and the ability to perform an intraoperative cholangiography [
26,
44,
45].
Definitely, LERV approach also allows to treat patients in a single hospital admission and with a single general anesthesia, with greater acceptance by patients as well as lower risk of possible related complications. Current evidence demonstrates that LERV has shorter hospital stay and less complication compared to the two stage, even in emergency setting.
The limitations of the study are its retrospective nature and the relative limited sample size. Future prospective, multicenter randomized controlled study should be conducted.
Author Contributions
RP, PP contributed to the conception and writing of the study and they should be considered co-first authors. All others authors contributed to the data acquisition, analysis, and interpretation of data. PDS and FFDM critically reviewed the submitted version of paper.
Funding
No funding to declare.
Institutional Review Board Statement
The study protocol was carried out in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki Declaration and its later amendments. No Ethics Committee review was needed.
Informed Consent Statement
Since this was a retrospective study, formal consent was not required and approval of the institutional research committee was not needed.
Data Availability Statement
The original contributions presented in the study are included in the article.
Conflicts of Interest
The authors declare no conflict of interest.
Cover Letter
Please find enclosed our manuscript entitled “LAPAROENDOSCOPIC RENDEZ-VOUS: AN EFFECTIVE AND SAFE APPROACH IN THE MANAGEMENT OF CHOLECYSTO-CHOLEDOCHOLITHIASIS” by Percario R, Panaccio P et al. which we would like to submit for publication.
We believe our findings would appeal to the readership of Journal of Clinical Medicine, enlighting the readers about the optimal therapeutical strategy in the management of cholecysto-choledocolithiasis.
The goal of this study was to evaluate the efficacy and safeness of LERV procedure recording complications and to compare our results to what is known in the surgical community.
We confirm that neither the manuscript nor any parts of its content are currently under consideration or published in another journal.
All authors have approved the manuscript and agree with its submission to Journal of Clinical Medicine.
We look forward to hearing from you at a suitable time.
Thank you for your consideration of my work. Please address all correspondence to paolo.panaccio@gmail.com
Sincerely,
Rossana Percario, MD
Paolo Panaccio, MD
Fabio Francesco Di Mola, MD PhD
References
- Barbara, L.; Sama, C.; Labate, A.M.M.; Taroni, F.; Rusticali, A.G.; Festi, D.; Sapio, C.; Roda, E.; Banterle, C.; Puci, A.; Formentini, F.; Colasanti, S.; Nardin, F. A Population Study on the Prevalence of Gallstone Disease: The Sirmione Study. Hepatology 1987, 7 (5).
- Lammert, F.; Acalovschi, M.; Ercolani, G.; van Erpecum, K.J.; Gurusamy, K.S.; van Laarhoven, C.J.; Portincasa, P. EASL Clinical Practice Guidelines on the Prevention, Diagnosis and Treatment of Gallstones. J. Hepatol. 2016, 65 (1).
- Dasari, B.V.M.; Tan, C.J.; Gurusamy, K.S.; Martin, D.J.; Kirk, G.; McKie, L.; Diamond, T.; Taylor, M.A. Surgical versus Endoscopic Treatment of Bile Duct Stones. Cochrane database Syst. Rev. 2013, 12, CD003327. [Google Scholar]
- Hirota, W.K.; Zuckerman, M.J.; Adler, D.G.; Davila, R.E.; Egan, J.; Leighton, J.A.; Qureshi, W.A.; Rajan, E.; Fanelli, R.; Wheeler-Harbaugh, J.; Baron, T.H.; Faigel, D.O. ASGE Guideline: The Role of Endoscopy in the Surveillance of Premalignant Conditions of the Upper GI Tract. Gastrointest. Endosc. 2006. [CrossRef] [PubMed]
- Vettoretto, N.; Arezzo, A.; Famiglietti, F.; Cirocchi, R.; Moja, L.; Morino, M. Laparoscopic-Endoscopic Rendezvous versus Preoperative Endoscopic Sphincterotomy in People Undergoing Laparoscopic Cholecystectomy for Stones in the Gallbladder and Bile Duct. Cochrane Database of Systematic Reviews 2018. [CrossRef] [PubMed]
- Tranter, S.E.; Thompson, M.H. Comparison of Endoscopic Sphincterotomy and Laparoscopic Exploration of the Common Bile Duct. British Journal of Surgery 2002. [CrossRef] [PubMed]
- Ford, J.A.; Soop, M.; Du, J.; Loveday, B.P.T.; Rodgers, M. Systematic Review of Intraoperative Cholangiography in Cholecystectomy. British Journal of Surgery. 2012, pp 160–167.
- Rácz, I.; Rejchrt, S.; Hassan, M. Complications of ERCP: Ethical Obligations and Legal Consequences. Digestive Diseases 2007. [CrossRef] [PubMed]
- Rhodes, M.; Sussman, L.; Cohen, L.; Lewis, M.P. Randomised Trial of Laparoscopic Exploration of Common Bile Duct versus Postoperative Endoscopic Retrograde Cholangiography for Common Bile Duct Stones. Lancet 1998, 351 (9097).
- Lyu, Y.; Cheng, Y.; Li, T.; Cheng, B.; Jin, X. Laparoscopic Common Bile Duct Exploration plus Cholecystectomy versus Endoscopic Retrograde Cholangiopancreatography plus Laparoscopic Cholecystectomy for Cholecystocholedocholithiasis: A Meta-Analysis. Surg. Endosc. 2019, 33 (10).
- Deslandres, E.; Gagner, M.; Pomp, A.; Rheault, M.; Leduc, R.; Clermont, R.; Gratton, J.; Bernard, E.J. Intraoperative Endoscopic Sphincterotomy for Common Bile Duct Stones during Laparoscopic Cholecystectomy. Gastrointest. Endosc. 1993, 39 (1).
- Duncan, C.B.; Riall, T.S. Evidence-Based Current Surgical Practice: Calculous Gallbladder Disease. J. Gastrointest. Surg. 2012, 16 (11).
- Parra-Membrives, P.; Díaz-Gómez, D.; Vilegas-Portero, R.; Molina-Linde, M.; Gómez-Bujedo, L.; Lacalle-Remigio, J.R. Appropriate Management of Common Bile Duct Stones: A RAND Corporation/UCLA Appropriateness Method Statistical Analysis. Surg. Endosc. 2010, 24 (5).
- Clavien, P.A.; Barkun, J.; De Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; De Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; Graf, R.; Vonlanthen, R.; Padbury, R.; Cameron, J.L.; Makuuchi, M. The Clavien-Dindo Classification of Surgical Complications: Five-Year Experience. Annals of Surgery 2009. [CrossRef] [PubMed]
- Okamoto, K.; Suzuki, K.; Takada, T.; Strasberg, S.M.; Asbun, H.J.; Endo, I.; Iwashita, Y.; Hibi, T.; Pitt, H.A.; Umezawa, A.; Asai, K.; Han, H.S.; Hwang, T.L.; Mori, Y.; Yoon, Y.S.; Huang, W.S.W.; Belli, G.; Dervenis, C.; Yokoe, M.; Kiriyama, S.; Itoi, T.; Jagannath, P.; Garden, O.J.; Miura, F.; Nakamura, M.; Horiguchi, A.; Wakabayashi, G.; Cherqui, D.; de Santibañes, E.; Shikata, S.; Noguchi, Y.; Ukai, T.; Higuchi, R.; Wada, K.; Honda, G.; Supe, A.N.; Yoshida, M.; Mayumi, T.; Gouma, D.J.; Deziel, D.J.; Liau, K.H.; Chen, M.F.; Shibao, K.; Liu, K.H.; Su, C.H.; Chan, A.C.W.; Yoon, D.S.; Choi, I.S.; Jonas, E.; Chen, X.P.; Fan, S.T.; Ker, C.G.; Giménez, M.E.; Kitano, S.; Inomata, M.; Hirata, K.; Inui, K.; Sumiyama, Y.; Yamamoto, M. Tokyo Guidelines 2018: Flowchart for the Management of Acute Cholecystitis. J. Hepatobiliary. Pancreat. Sci. 2018, 25 (1).
- Manes, G.; Paspatis, G.; Aabakken, L.; Anderloni, A.; Arvanitakis, M.; Ah-Soune, P.; Barthet, M.; Domagk, D.; Dumonceau, J.M.; Gigot, J.F.; Hritz, I.; Karamanolis, G.; Laghi, A.; Mariani, A.; Paraskeva, K.; Pohl, J.; Ponchon, T.; Swahn, F.; Ter Steege, R.W.F.; Tringali, A.; Vezakis, A.; Williams, E.J.; Van Hooft, J.E. Endoscopic Management of Common Bile Duct Stones: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2019, 51 (5).
- Arezzo, A.; Vettoretto, N.; Famiglietti, F.; Moja, L.; Morino, M. Laparoendoscopic Rendezvous Reduces Perioperative Morbidity and Risk of Pancreatitis. Surgical Endoscopy 2013. [CrossRef] [PubMed]
- Alexakis, N.; Connor, S. Meta-Analysis of One- vs. Two-Stage Laparoscopic/Endoscopic Management of Common Bile Duct Stones. HPB 2012, 14 (4), 254–259.
- Bansal, V.K.; Misra, M.C.; Rajan, K.; Kilambi, R.; Kumar, S.; Krishna, A.; Kumar, A.; Pandav, C.S.; Subramaniam, R.; Arora, M.K.; Garg, P.K. Single-Stage Laparoscopic Common Bile Duct Exploration and Cholecystectomy versus Two-Stage Endoscopic Stone Extraction Followed by Laparoscopic Cholecystectomy for Patients with Concomitant Gallbladder Stones and Common Bile Duct Stones: A Randomized Controlled Trial. Surg. Endosc. 2014, 28 (3).
- Bosley, M.E.; Zamora, I.J.; Neff, L.P. Choledocholithiasis-a New Clinical Pathway. Translational Gastroenterology and Hepatology 2021. [CrossRef] [PubMed]
- Bove, A.; Di Renzo, R.M.; Palone, G.; Testa, D.; Malerba, V.; Bongarzoni, G. Single-Stage Procedure for the Treatment of Cholecysto-Choledocolithiasis: A Surgical Procedures Review. Ther. Clin. Risk Manag. 2018, 14, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Ricci, C.; Pagano, N.; Taffurelli, G.; Pacilio, C.A.; Migliori, M.; Bazzoli, F.; Casadei, R.; Minni, F. Comparison of Efficacy and Safety of 4 Combinations of Laparoscopic and Intraoperative Techniques for Management of Gallstone Disease with Biliary Duct Calculi a Systematic Review and Network Meta-Analysis. JAMA Surg. 2018, 153 (7).
- La Greca, G.; Barbagallo, F.; Di Blasi, M.; Chisari, A.; Lombardo, R.; Bonaccorso, R.; Latteri, S.; Di Stefano, A.; Russello, D. Laparo-Endoscopic “Rendezvous” to Treat Cholecysto-Choledocolithiasis: Effective, Safe and Simplifies the Endoscopist’s Work. World J. Gastroenterol. 2008, 14(18), 2844–2850. [Google Scholar] [CrossRef] [PubMed]
- La Barba, G.; Gardini, A.; Cavargini, E.; Casadei, A.; Morgagni, P.; Bazzocchi, F.; D’Acapito, F.; Cavaliere, D.; Curti, R.; Tringali, D.; Cucchetti, A.; Ercolani, G. Laparoendoscopic Rendezvous in the Treatment of Cholecysto-Choledocholitiasis: A Single Series of 200 Patients. Surg. Endosc. 2018, 32 (9).
- Pizzicannella, M.; Barberio, M.; Lapergola, A.; Gregori, M.; Maurichi, F.A.; Gallina, S.; Benedicenti, P.; Viola, M.G. One-Stage Approach to Cholecystocholedocholithiasis Treatment: A Feasible Surgical Strategy for Emergency Settings and Frail Patients. Surg. Endosc. 2022, 36 (11).
- Bradley, A.; Sami, S.; Hemadasa, N.; Macleod, A.; Brown, L.R.; Apollos, J. Decision Analysis of Minimally Invasive Management Options for Cholecysto-Choledocholithiasis. Surgical Endoscopy 2020. [CrossRef] [PubMed]
- Costi, R.; Gnocchi, A.; Di Mario, F.; Sarli, L. Diagnosis and Management of Choledocholithiasis in the Golden Age of Imaging, Endoscopy and Laparoscopy. World J. Gastroenterol. 2014, 20(37), 13382–13401. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Su, Y.; Yan, J.; Li, X. Laparoendoscopic Rendezvous versus ERCP Followed by Laparoscopic Cholecystectomy in the Management of Cholecystocholedocholithiasis: A Systemic Review and Meta-Analysis. Surg. Endosc. 2020, 34 (9).
- Lu, J.; Xiong, X.Z.; Cheng, Y.; Lin, Y.X.; Zhou, R.X.; You, Z.; Wu, S.J.; Cheng, N.S. One-Stage versus Two-Stage Management for Concomitant Gallbladder Stones and Common Bile Duct Stones in Patients with Obstructive Jaundice. Am. Surg. 2013, 79(11), 1142–1148. [Google Scholar] [CrossRef] [PubMed]
- Schacher, F.C.; Giongo, S.M.; Teixeira, F.J.P.; Mattos, Â.Z. Endoscopic Retrograde Cholangiopancreatography versus Surgery for Choledocholithiasis – A Meta-Analysis. Ann. Hepatol. 2019, 18 (4).
- Williams, E.J.; Taylor, S.; Fairclough, P.; Hamlyn, A.; Logan, R.F.; Martin, D.; Riley, S.A.; Veitch, P.; Wilkinson, M.; Williamson, P.R.; Lombard, M. Are We Meeting the Standards Set for Endoscopy? Results of a Large-Scale Prospective Survey of Endoscopic Retrograde Cholangio-Pancreatograph Practice. Gut 2007, 56 (6).
- Swan, R.; Miner, T.J. Current Role of Surgical Therapy in Gastric Cancer. World Journal of Gastroenterology 2006. [CrossRef] [PubMed]
- Van Dijk, A.H.; de Reuver, P.R.; Boermeester, M.A. Evidence in Cholecysto – and Choledocholithiasis: A Systematic Review of Guidelines. HPB 2016, 18. [Google Scholar] [CrossRef]
- Pavlidis, E.T.; Pavlidis, T.E. Current Management of Concomitant Cholelithiasis and Common Bile Duct Stones. World J. Gastrointest. Surg. 2023, 15 (2).
- Morino, M.; Baracchi, F.; Miglietta, C.; Furlan, N.; Ragona, R.; Garbarini, A. Preoperative Endoscopic Sphincterotomy versus Laparoendoscopic Rendezvous in Patients with Gallbladder and Bile Duct Stones. Ann. Surg. 2006, 244 (6), 889–893; discussion 893-896.
- La Greca, G.; Barbagallo, F.; Sofia, M.; Latteri, S.; Russello, D. Simultaneous Laparoendoscopic Rendezvous for the Treatment of Cholecystocholedocholithiasis. Surgical Endoscopy and Other Interventional Techniques. 2010, pp 769–780.
- El-Geidie, A.A.-R. Laparoendoscopic Management of Concomitant Gallbladder Stones and Common Bile Duct Stones: What Is the Best Technique? Surg. Laparosc. Endosc. Percutan. Tech. 2011, 21(4), 282–287. [Google Scholar] [CrossRef] [PubMed]
- Tzovaras, G.; Baloyiannis, I.; Zachari, E.; Symeonidis, D.; Zacharoulis, D.; Kapsoritakis, A.; Paroutoglou, G.; Potamianos, S. Laparoendoscopic Rendezvous versus Preoperative ERCP and Laparoscopic Cholecystectomy for the Management of Cholecysto-Choledocholithiasis: Interim Analysis of a Controlled Randomized Trial. Ann. Surg. 2012, 255(3), 435–439. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Wang, Y.; Shu, G.; Lou, C.; Zhang, J.; Du, Z. Laparoscopic versus Endoscopic Management of Choledocholithiasis in Patients Undergoing Laparoscopic Cholecystectomy: A Meta-Analysis. J. Laparoendosc. Adv. Surg. Tech. A 2014, 24(5), 287–294. [Google Scholar] [CrossRef] [PubMed]
- Guan, G.; Sun, C.; Ren, Y.; Zhao, Z.; Ning, S. Comparing a Single-Staged Laparoscopic Cholecystectomy with Common Bile Duct Exploration versus a Two-Staged Endoscopic Sphincterotomy Followed by Laparoscopic Cholecystectomy. Surg. (United States) 2018, 164 (5).
- Bencini, L. Modern Approach to Cholecysto-Choledocholithiasis. World J. Gastrointest. Endosc. 2014, 6 (2).
- Noel, R.; Arnelo, U.; Swahn, F. Intraoperative versus Postoperative Rendezvous Endoscopic Retrograde Cholangiopancreatography to Treat Common Bile Duct Stones during Cholecystectomy. Dig. Endosc. 2019, 31 (1).
- Lella, F.; Bagnolo, F.; Rebuffat, C.; Scalambra, M.; Bonassi, U.; Colombo, E. Use of the Laparoscopic-Endoscopic Approach, the so-Called “Rendezvous” Technique, in Cholecystocholedocholithiasis: A Valid Method in Cases with Patient-Related Risk Factors for Post-ERCP Pancreatitis. Surg. Endosc. Other Interv. Tech. 2006, 20 (3).
- Cianci, P.; Restini, E. Management of Cholelithiasis with Choledocholithiasis: Endoscopic and Surgical Approaches. World Journal of Gastroenterology 2021. [CrossRef] [PubMed]
- Baloyiannis, I.; Tzovaras, G. Current Status of Laparoendoscopic Rendezvous in the Treatment of Cholelithiasis with Concomitant Choledocholithiasis. World J. Gastrointest. Endosc. 2015, 7 (7).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).