Figure 1 An abdominal radiograph showed pneumobilia and an enlarged gastric bubble of a 81-year-old man presented to the emergency department with epigastric pain, vomiting, anorexia and obstipation for 3 days. Physical examination was notable for a painful epigastric tenderness. Laboratory examinations revealed a white blood cell count of 22.1 (3.4-9.7)(10*9/L).
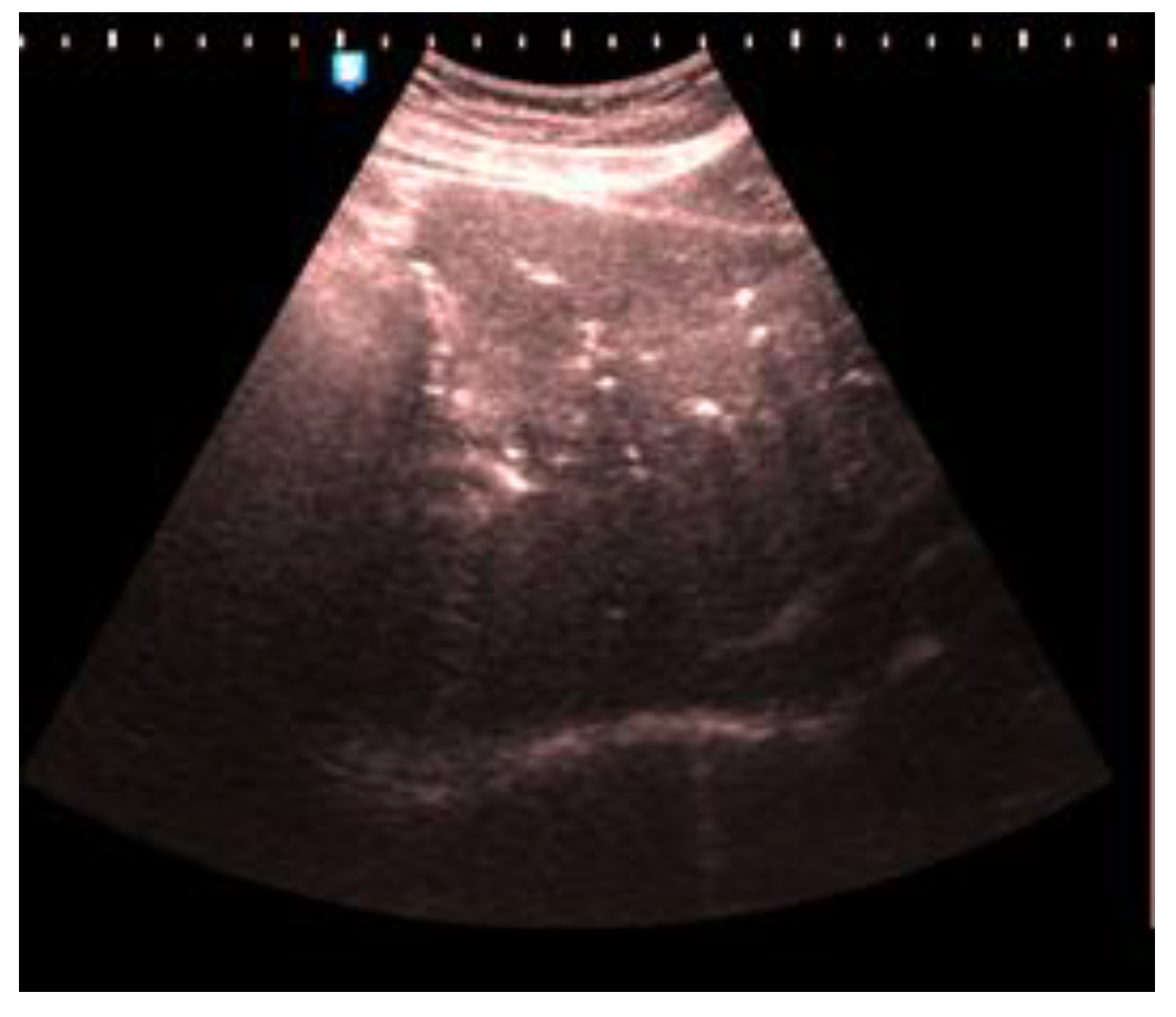
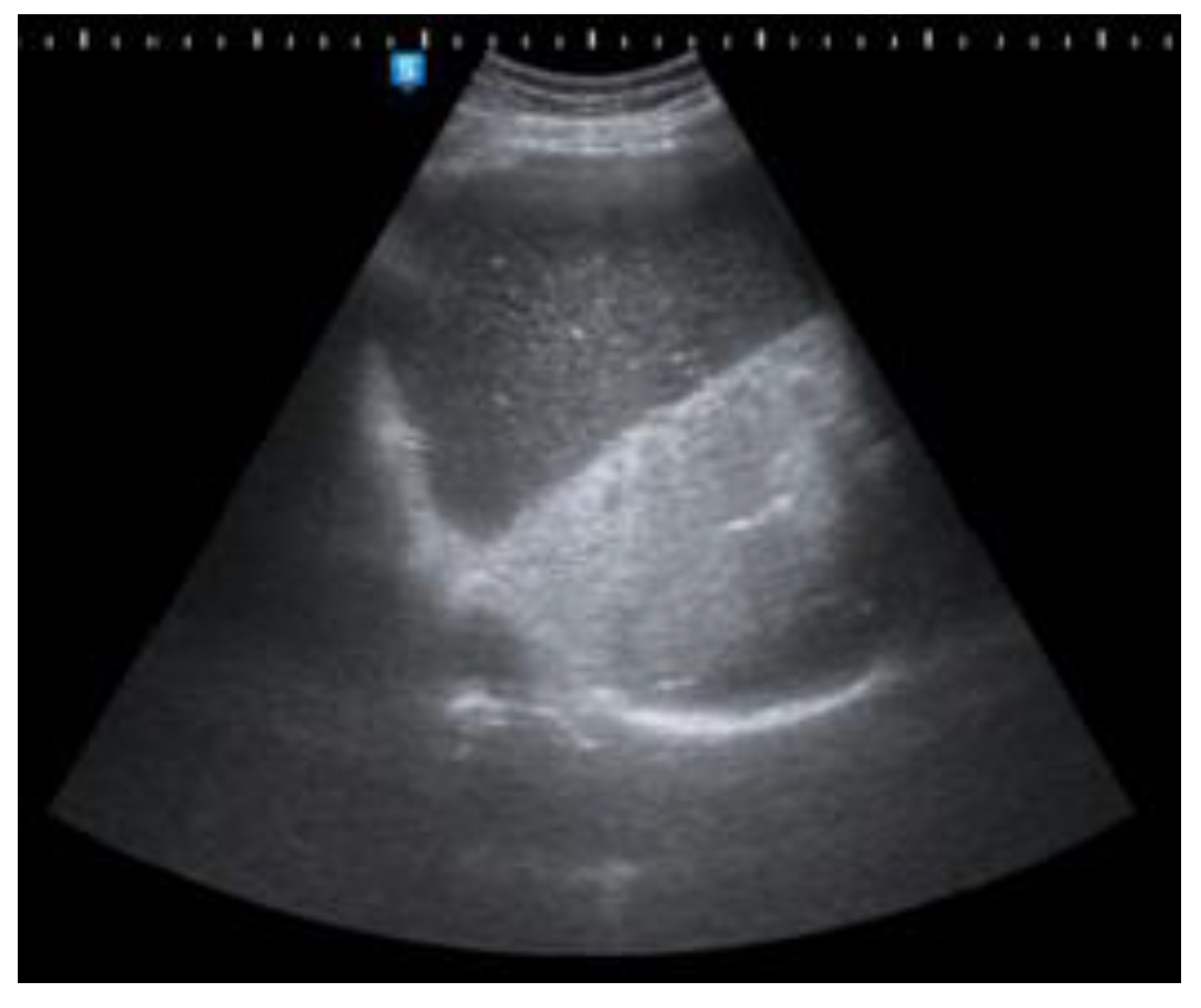
Figure 2,
Figure 3 and
Figure 4 Abdominal ultrasound (US) also demonstrated an enlarged stomach, a curvilinear focus of increased echogenicity with posterior shadowing in duodenal bulb which corresponds to a gallstone (long arrow) and ultrasound signs of pneumobilia. The leading diagnosis of a new finding of pneumobilia on ultrasonography with elevated white blood cell count is cholangitis. However, poor visualization of gallbladder and distended stomach can not be explained by cholangitis so CT scan has been useful as an imaging modality for diagnosis of cholecystoduodenal fistula. The other causes of pneumobilia are biliodigestive anastomosis or post-ERCP conditions.
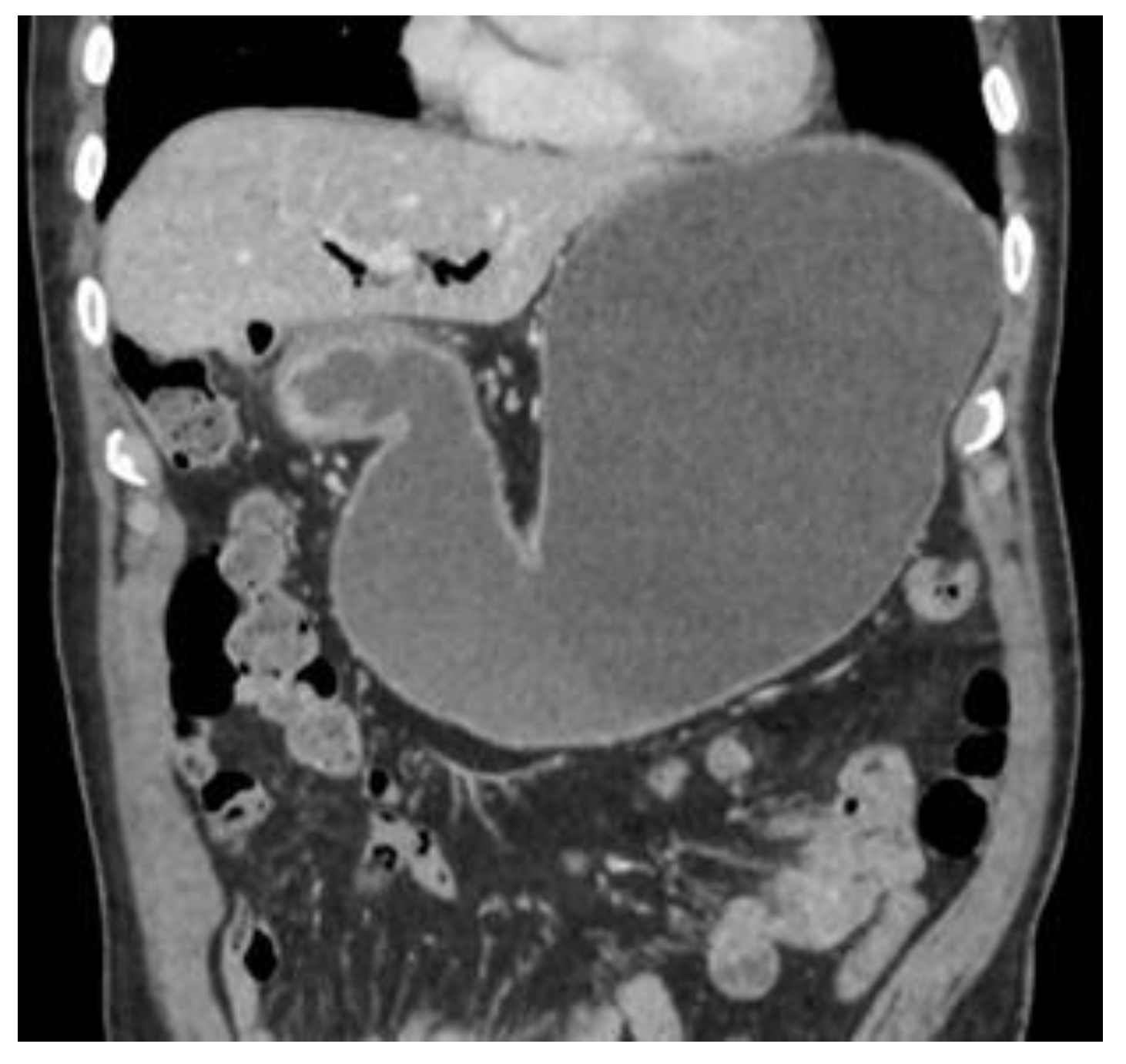
Figure 5 and
Figure 6 Subsequent computed tomography with intravenous contrast material confirmed pneumobilia with direct visualization of a tract between the gallbladder and the duodenum and a 25 mm gallstone impacted in the duodenal bulb (long arrow) causing gastric distention so diagnosis of cholecystoduodenal fistula was made. Bouveret’s syndrome is characterized by gastric outlet obstruction (GOO) secondary to cholecystoduodenal fistula. [
1,
2] Fistula formation is favoured by the long history of cholelithiasis, the repeated episodes of acute cholecystitis, the large size of the gallstones (2–8 cm), the female gender and advanced age ( > 60 years ). Morbidity and mortality rates are high, estimated at 60% and 12%–30% respectively, due to the advanced age and the comorbidities of the patients. [
3] Patients usually present with non-specific signs and symptoms of GOO, including nausea and vomiting in 87%, abdominal pain in 71%, hematemesis in 15%, weight loss in 14% and anorexia in 13%. [
4] The radiologic features of gallstone ileus are the classical Rigler’s triad that consists of pneumobilia, dilated small bowel and an ectopic gallstone. [
5] A plain abdominal X- ray is diagnostic in about 50% of cases and may demonstrate intestinal obstruction, pneumobilia, an ectopic gallstone, alteration in the position of the previously observed stone or two air fluid levels in the right upper quadrant secondary to air in the gall bladder. [
6] US may show the gallstone sufficiently large to be apparent. The fistula may also be visualized if filled with fluid or air. Pneumobilia and a dilated stomach may also be seen with US. [
7,
8] CT is the best imaging technique used to search for Rigler’s triad that is specific to gallstone ileus and with it’s 93% sensitivity, 100% specificity, and 99% accuracy is needed for definitive diagnosis. [
9] Up to 20% of the gallstones may be isoattenuating when MRI is indicated because it detects Rigler’s triad in nearly all cases where it was present. [
10]
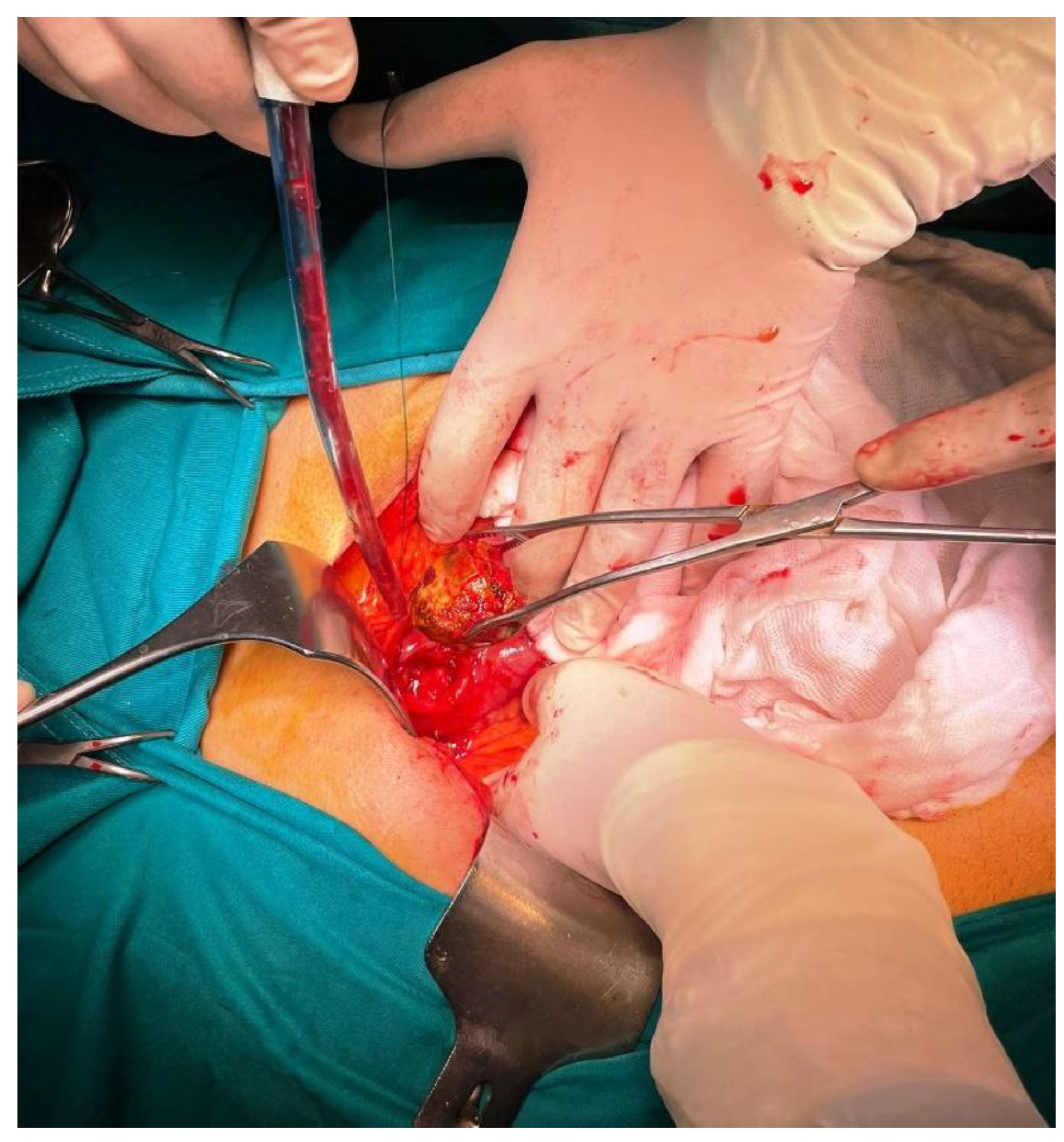
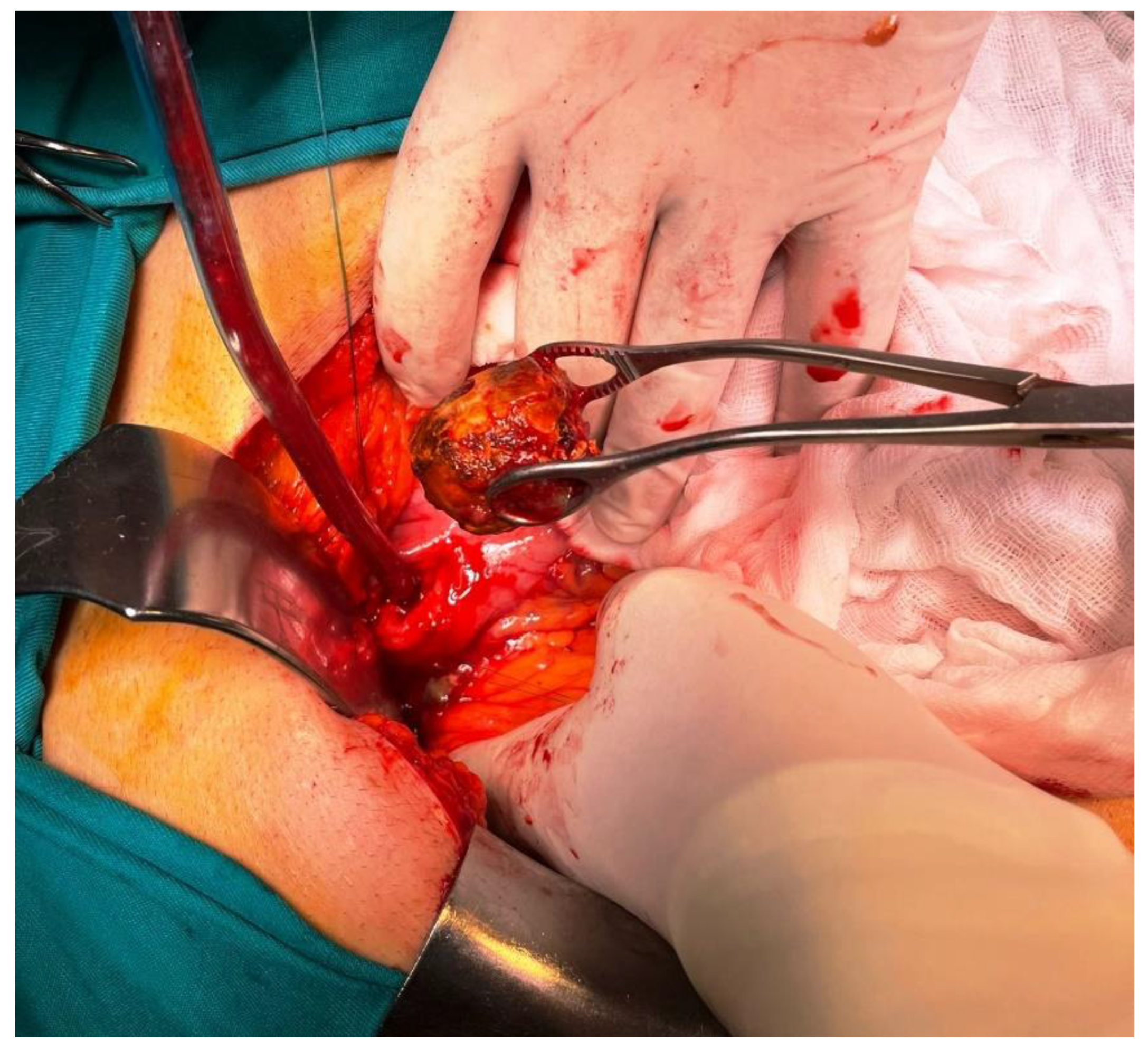
Figure 7,
Figure 8 and
Figure 9 Patient immediately have been treated by open surgery including gallstone extraction, gastrotomy, duodenal suture and cholecystectomy (Figures 7,8,9). Both parenteral nutrition and antibiotics were introduced during the postoperative period so patient was discharged after 7 days. Enterotomy or gastrotomy with or without cholecystectomy and fistula repair remains the treatment of choice. It has high success rate, with acceptable surgical morbidity and mortality [
11]. It is still a matter of debate whether cholecystectomy and repair of the fistula should be performed, due to spontaneous closure of fistulas in some cases [
9,
12,
13]
Author Contributions
All authors (Dragan Vasin, Sabina Sadović, Katarina Trajković, Tarik Plojović, Danilo Marković, Dušan Micić, Ksenija Mijović, Aleksandar Pavlović, Dragan Mašulović) have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to it is a retrospective case report, which did not impact the management of the patient.
Informed Consent Statement
Written informed consent has been obtained from the patient and parents to publish this paper.
Acknowledgments
There is no acknowledgemnts.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Djuric-Stefanovic, A.; Pesko, P.; Saranovic, D. Education and imaging. Hepatobiliary and pancreatic: Bouveret's syndrome. J Gastroenterol Hepatol 2011, 26, 1216. [Google Scholar] [CrossRef] [PubMed]
- Wickbom, G. Mannen bakom syndromet: Léon Bouveret. Internmedicinaren som stödde kirurgin [The man behind the syndrome: Leon Bouveret. The internist who supported surgery]. Lakartidningen 1993, 90, 162–165. [Google Scholar] [PubMed]
- Mavroeidis, V.K.; Matthioudakis, D.I.; Economou, N.K.; Karanikas, I.D. Bouveret Syndrome—The Rarest Variant of Gallstone Ileus: A Case Report and Literature Review. Case Reports in Surgery 2013, 839370. [Google Scholar] [CrossRef] [PubMed]
- Cappell, M.S.; Davis, M. Characterization of Bouveret’s Syndrome: A Comprehensive Review of 128 Cases. American Journal of Gastroenterology 2006, 101, 2139–2146. [Google Scholar] [CrossRef]
- Gijon-de-la-Santa, L.; Camarero-Miguel, A.; Perez-Retortillo, J.A.; Ramia-Angel, J.M. Bouveret's syndrome: evaluation with multidetector CT. Rev Esp Enferm Dig. 2014, 106, 283–284. [Google Scholar]
- Masannat, Y. A. A rare complication of a common disease: Bouveret syndrome, a case report. World Journal of Gastroenterology 2016, 12, 2620. [Google Scholar] [CrossRef] [PubMed]
- Brennan, G.B.; Rosenberg, R.D.; Arora, S. Bouveret syndrome. RadioGraphics 2004, 24, 1171–1175. [Google Scholar] [CrossRef] [PubMed]
- Ripollés, T.; Miguel-Dasit, A.; Errando, J.; Morote, V.; Gómez-Abril, S.A.; Richart, J. Gallstone ileus: increased diagnostic sensitivity by combining plain film and ultrasound. Abdominal imaging 2001, 26, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Haddad, F.G.; Mansour, W.; Deeb, L. Bouveret’s Syndrome: Literature Review. Cureus 2018, 10, e2299. [Google Scholar] [CrossRef] [PubMed]
- Osman, K.T.; Wahba, A.; Farhoud, A.; Abdelfattah, A.M.; Maselli, D.B. Bouveret’s Syndrome: An Extensive Summary of the Literature. Arch Gastroenterol Res. 2020, 1, 40–46. [Google Scholar]
- Koulaouzidis, A.; Moschos, J. Bouveret's syndrome. Narrative review. Annals of hepatology 2007, 6, 89–91. [Google Scholar] [CrossRef] [PubMed]
- Mavroeidis, V.K.; Matthioudakis, D.I.; Economou, N.K.; Karanikas, I.D. Bouveret syndrome – the rarest variant of gallstone ileus: a case report and literature review. Case Rep Surg. 2013, 839370. [Google Scholar] [CrossRef]
- Saponjski, D.; Djuric Stefanovic, A.; Jankovic, A.; Mitrovic Jovanovic, M.; Kmezic, S.; Mihajlovic, S.; et al. Spontaneous cholecystoduodenal fistula – spectrum of complications. Srp Arh Celok Lek. 2019, 147, 628–631. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).