Submitted:
29 May 2024
Posted:
30 May 2024
You are already at the latest version
Abstract
Keywords:
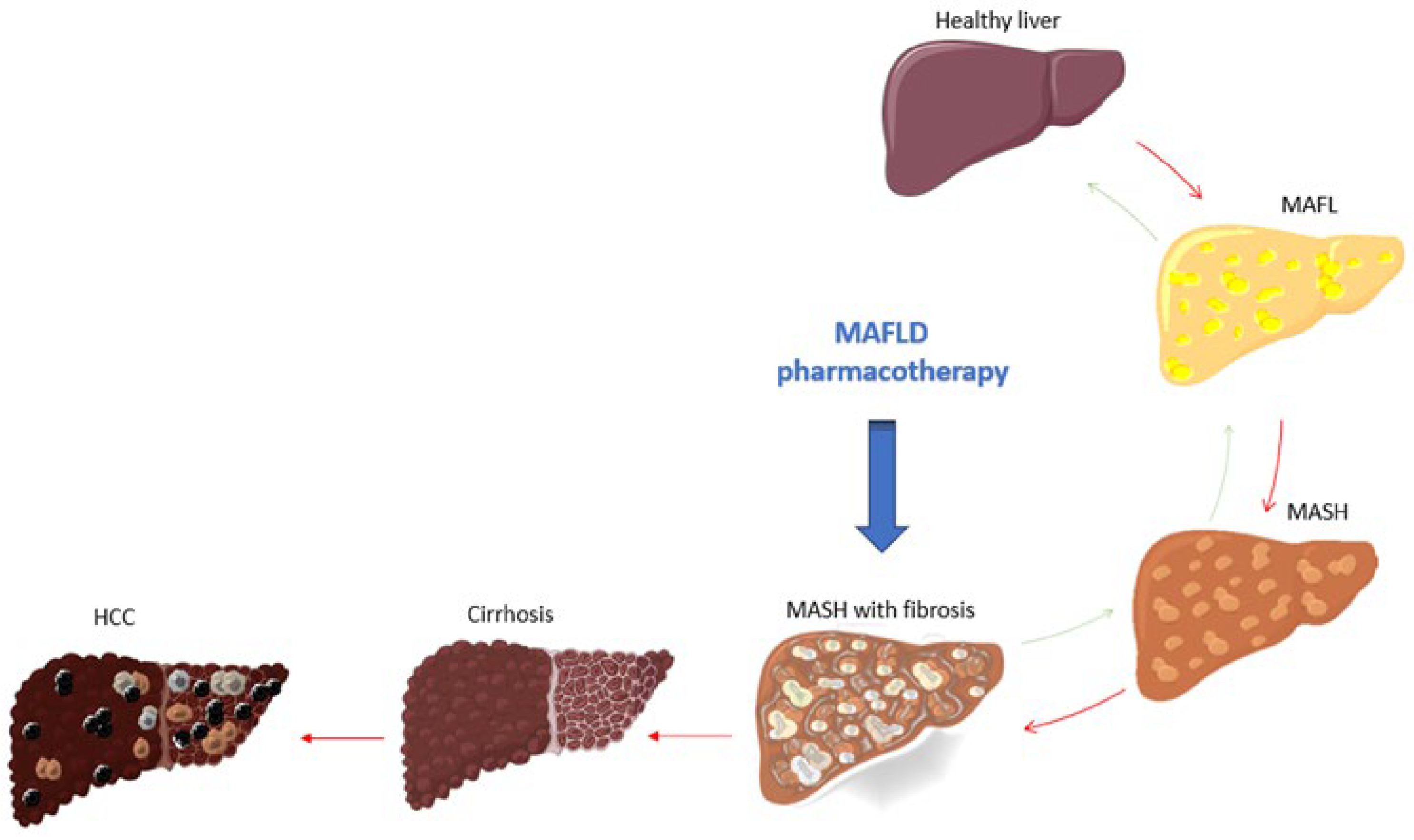
1. Introduction
1.1. Pathophysiology of Liver Fibrosis
2. Latest Updates in MAFLD Treatment
2.1. Thyroid hormone receptor β (THR-β) Agonists
2.2. Fibroblast Growth Factor 21 (FGF-21) Agonists
2.3. Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors
2.4. Incretin and Glucagon Receptor Agonists
2.5. Peroxisome Proliferator-Activated Receptor (PPAR) Agonists
3. Future Directions
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mirarchi, L.; Amodeo, S.; Citarrella, R.; Licata, A.; Soresi, M.; Giannitrapani, L. SGLT2 Inhibitors as the Most Promising Influencers on the Outcome of Non-Alcoholic Fatty Liver Disease. Int. J. Mol. Sci. 2022, 23, 3668. [CrossRef]
- Roeb, E.; Geier, A. Nonalcoholic steatohepatitis (NASH) – current treatment recommendations and future developments. Z. Gastroenterol. 2019, 57, 508–517. [CrossRef]
- Moon, J.S.; Hong, J.H.; Jung, Y.J.; Ferrannini, E.; Nauck, M.A.; Lim, S. SGLT-2 inhibitors and GLP-1 receptor agonists in metabolic dysfunction-associated fatty liver disease. Trends Endocrinol. Metab. 2022, 33, 424–442. [CrossRef]
- Parlati, L.; Régnier, M.; Guillou, H.; Postic, C. New targets for NAFLD. JHEP Rep. 2021, 3, 100346. [CrossRef]
- Badmus, O.O.; Hillhouse, S.A.; Anderson, C.D.; Hinds, T.D.; Stec, D.E. Molecular mechanisms of metabolic associated fatty liver disease (MAFLD): functional analysis of lipid metabolism pathways. Clin. Sci. 2022, 136, 1347–1366. [CrossRef]
- Sakurai, Y.; Kubota, N.; Yamauchi, T.; Kadowaki, T. Role of Insulin Resistance in MAFLD. Int. J. Mol. Sci. 2021, 22, 4156. [CrossRef]
- Eslam, M.; Sanyal, A.J.; George, J.; on behalf of theInternational Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease. Gastroenterology 2020, 158, 1999–2014.e1991. [CrossRef]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wong, V.W.-S.; Dufour, J.-F.; Schattenberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020, 73, 202–209. [CrossRef]
- Gofton C, Upendran Y, Zheng MH, George J. MAFLD: How is it different from NAFLD? Clin Mol Hepatol. 2023;29(Suppl):S17-S31.
- Lin, S.; Huang, J.; Wang, M.; Kumar, R.; Liu, Y.; Liu, S.; Wu, Y.; Wang, X.; Zhu, Y. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020, 40, 2082–2089. [CrossRef]
- Suzuki, K.; Tamaki, N.; Kurosaki, M.; Takahashi, Y.; Yamazaki, Y.; Uchihara, N.; Tanaka, Y.; Miyamoto, H.; Yamada, M.; Keitoku, T.; et al. Concordance between metabolic dysfunction-associated steatotic liver disease and nonalcoholic fatty liver disease. Hepatol. Res. 2024. [CrossRef]
- Sumida, Y.; Yoneda, M. Current and future pharmacological therapies for NAFLD/NASH. J. Gastroenterol. 2017, 53, 362–376. [CrossRef]
- Younossi, Z.M.; Stepanova, M.; Ong, J.; Trimble, G.; AlQahtani, S.; Younossi, I.; Ahmed, A.; Racila, A.; Henry, L. Nonalcoholic Steatohepatitis Is the Most Rapidly Increasing Indication for Liver Transplantation in the United States. Clin. Gastroenterol. Hepatol. 2020, 19, 580–589.e5. [CrossRef]
- Gao, F.; Chen, G.; Byrne, C.D.; Targher, G.; Cheung, T.T.; Zheng, M.-H. Metabolic dysfunction-associated fatty liver disease and hepatocellular carcinoma: present and future. HepatoBiliary Surg. Nutr. 2023, 12, 945–948. [CrossRef]
- Heyens, L.J.M.; Busschots, D.; Koek, G.H.; Robaeys, G.; Francque, S. Liver Fibrosis in Non-alcoholic Fatty Liver Disease: From Liver Biopsy to Non-invasive Biomarkers in Diagnosis and Treatment. Front. Med. 2021, 8. [CrossRef]
- Nassir F. NAFLD: Mechanisms, Treatments, and Biomarkers. Biomolecules. 2022;12(6).
- Dong, Q.; Bao, H.; Wang, J.; Shi, W.; Zou, X.; Sheng, J.; Gao, J.; Guan, C.; Xia, H.; Li, J.; et al. Liver fibrosis and MAFLD: the exploration of multi-drug combination therapy strategies. Front. Med. 2023, 10. [CrossRef]
- Alonso-Peña, M.; Del Barrio, M.; Peleteiro-Vigil, A.; Jimenez-Gonzalez, C.; Santos-Laso, A.; Arias-Loste, M.T.; Iruzubieta, P.; Crespo, J. Innovative Therapeutic Approaches in Non-Alcoholic Fatty Liver Disease: When Knowing Your Patient Is Key. Int. J. Mol. Sci. 2023, 24, 10718. [CrossRef]
- Sato-Espinoza K, Chotiprasidhi P, Huaman MR, Díaz-Ferrer J. Update in lean metabolic dysfunction-associated steatotic liver disease. World J Hepatol. 2024;16(3):452-64.
- Madrigal Pharmaceuticals Announces FDA Approval of Rezdiffra™ (resmetirom) for the Treatment of Patients with Noncirrhotic Nonalcoholic Steatohepatitis (NASH) with Moderate to Advanced Liver Fibrosis 2024 [Available from: https://ir.madrigalpharma.com/news-releases/news-release-details/madrigal-pharmaceuticals-announces-fda-approval-rezdiffratm.
- Guo, X.; Yin, X.; Liu, Z.; Wang, J. Non-Alcoholic Fatty Liver Disease (NAFLD) Pathogenesis and Natural Products for Prevention and Treatment. Int. J. Mol. Sci. 2022, 23, 15489. [CrossRef]
- Tanase, D.M.; Gosav, E.M.; Costea, C.F.; Ciocoiu, M.; Lacatusu, C.M.; Maranduca, M.A.; Ouatu, A.; Floria, M. The Intricate Relationship between Type 2 Diabetes Mellitus (T2DM), Insulin Resistance (IR), and Nonalcoholic Fatty Liver Disease (NAFLD). J. Diabetes Res. 2020, 2020, 1–16. [CrossRef]
- Xian, Y.-X.; Weng, J.-P.; Xu, F. MAFLD vs. NAFLD: shared features and potential changes in epidemiology, pathophysiology, diagnosis, and pharmacotherapy. Chin. Med J. 2020, 134, 8–19. [CrossRef]
- Huang, X.; Chen, H.; Wen, S.; Dong, M.; Zhou, L.; Yuan, X. Therapeutic Approaches for Nonalcoholic Fatty Liver Disease: Established Targets and Drugs. Diabetes, Metab. Syndr. Obesity: Targets Ther. 2023, ume 16, 1809–1819. [CrossRef]
- Peiseler, M.; Schwabe, R.; Hampe, J.; Kubes, P.; Heikenwälder, M.; Tacke, F. Immune mechanisms linking metabolic injury to inflammation and fibrosis in fatty liver disease – novel insights into cellular communication circuits. J. Hepatol. 2022, 77, 1136–1160. [CrossRef]
- Qu, W.; Ma, T.; Cai, J.; Zhang, X.; Zhang, P.; She, Z.; Wan, F.; Li, H. Liver Fibrosis and MAFLD: From Molecular Aspects to Novel Pharmacological Strategies. Front. Med. 2021, 8. [CrossRef]
- Li, W.; Chang, N.; Li, L. Heterogeneity and Function of Kupffer Cells in Liver Injury. Front. Immunol. 2022, 13, 940867. [CrossRef]
- Ginès P, Krag A, Abraldes JG, Solà E, Fabrellas N, PS. K. Liver cirrhosis. Lancet. 2021;398(10308):1359–76.
- Parola, M.; Pinzani, M. Liver fibrosis in NAFLD/NASH: from pathophysiology towards diagnostic and therapeutic strategies. Mol. Asp. Med. 2024, 95, 101231. [CrossRef]
- Colosimo, S.; Ravaioli, F.; Petroni, M.L.; Brodosi, L.; Marchignoli, F.; Barbanti, F.A.; Sasdelli, A.S.; Marchesini, G.; Pironi, L. Effects of antidiabetic agents on steatosis and fibrosis biomarkers in type 2 diabetes: A real-world data analysis. Liver Int. 2021, 41, 731–742. [CrossRef]
- Kowalik, M.A.; Columbano, A.; Perra, A. Thyroid Hormones, Thyromimetics and Their Metabolites in the Treatment of Liver Disease. Front. Endocrinol. 2018, 9, 382. [CrossRef]
- Huang, S.; Deng, Z.; Wang, W.; Liao, G.; Zhao, Y.; Zhong, H.; Zhang, Q.; Liu, J.; Mao, X.; Chen, B.; et al. CS27109, A Selective Thyroid Hormone Receptor-β Agonist Alleviates Metabolic-Associated Fatty Liver Disease in Murine Models. Int. J. Endocrinol. 2023, 2023, 1–11. [CrossRef]
- Kizivat, T.; Maric, I.; Mudri, D.; Curcic, I.B.; Primorac, D.; Smolic, M. Hypothyroidism and Nonalcoholic Fatty Liver Disease: Pathophysiological Associations and Therapeutic Implications. J. Clin. Transl. Hepatol. 2020, 8, 1–7. [CrossRef]
- Harrison, S.A.; Bashir, M.; Moussa, S.E.; McCarty, K.; Frias, J.P.; Taub, R.; Alkhouri, N. Effects of Resmetirom on Noninvasive Endpoints in a 36-Week Phase 2 Active Treatment Extension Study in Patients With NASH. Hepatol. Commun. 2021, 5, 573–588. [CrossRef]
- Rojas, .; Lara-Romero, C.; Muñoz-Hernández, R.; Gato, S.; Ampuero, J.; Romero-Gómez, M. Emerging pharmacological treatment options for MAFLD. Ther. Adv. Endocrinol. Metab. 2022, 13. [CrossRef]
- Tanase, D.M.; Gosav, E.M.; Neculae, E.; Costea, C.F.; Ciocoiu, M.; Hurjui, L.L.; Tarniceriu, C.C.; Floria, M. Hypothyroidism-Induced Nonalcoholic Fatty Liver Disease (HIN): Mechanisms and Emerging Therapeutic Options. Int. J. Mol. Sci. 2020, 21, 5927. [CrossRef]
- Karim G, Bansal MB. Resmetirom: An Orally Administered, Smallmolecule, Liver-directed, β-selective THR Agonist for the Treatment of Non-alcoholic Fatty Liver Disease and Non-alcoholic Steatohepatitis. touchREV Endocrinol. 2023;19(1):60-70.
- FDA Approves First Treatment for Patients with Liver Scarring Due to Fatty Liver Disease 2024 [Available from: https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-patients-liver-scarring-due-fatty-liver-disease.
- Harrison, S.A.; Bedossa, P.; Guy, C.D.; Schattenberg, J.M.; Loomba, R.; Taub, R.; Labriola, D.; Moussa, S.E.; Neff, G.W.; Rinella, M.E.; et al. A Phase 3, Randomized, Controlled Trial of Resmetirom in NASH with Liver Fibrosis. New Engl. J. Med. 2024, 390, 497–509. [CrossRef]
- Harrison, S.A.; Taub, R.; Neff, G.W.; Lucas, K.J.; Labriola, D.; Moussa, S.E.; Alkhouri, N.; Bashir, M.R. Resmetirom for nonalcoholic fatty liver disease: a randomized, double-blind, placebo-controlled phase 3 trial. Nat. Med. 2023, 29, 2919–2928. [CrossRef]
- Rubin, V.R.; Bojanic, K.; Smolic, M.; Rubin, J.; Tabll, A.; Smolic, R. An Update on Efficacy and Safety of Emerging Hepatic Antifibrotic Agents. J. Clin. Transl. Hepatol. 2021, 000, 1–11. [CrossRef]
- 2809; 42. VK2809 Selective Thyroid Receptor-β Agonist 2024.
- Available from: https://vikingtherapeutics.com/pipeline/metabolic-disease-program/vk2809/.
- Safety and Tolerability of VK2809 in Patients With Primary Hypercholesterolemia and Non-Alcoholic Fatty Liver Disease 2024 [Available from: https://classic.clinicaltrials.gov/ct2/show/NCT02927184.
- A Study to Assess the Efficacy and Safety of VK2809 for 52 Weeks in Subjects With Biopsy Proven NASH (VOYAGE) 2024 [Available from: https://classic.clinicaltrials.gov/ct2/show/NCT04173065.
- Bhatt DL, Bays HE, Miller M, Cain JE, Wasilewska K, Andrawis NS, et al. The FGF21 analog pegozafermin in severe hypertriglyceridemia: a randomized phase 2 trial. Nat Med. 2023;29(7):1782-92.
- Ciardullo, S.; Muraca, E.; Vergani, M.; Invernizzi, P.; Perseghin, G. Advancements in pharmacological treatment of NAFLD/MASLD: a focus on metabolic and liver-targeted interventions. Gastroenterol. Rep. 2023, 12, goae029. [CrossRef]
- Kounatidis, D.; Vallianou, N.G.; Geladari, E.; Panoilia, M.P.; Daskou, A.; Stratigou, T.; Karampela, I.; Tsilingiris, D.; Dalamaga, M. NAFLD in the 21st Century: Current Knowledge Regarding Its Pathogenesis, Diagnosis and Therapeutics. Biomedicines 2024, 12, 826. [CrossRef]
- Loomba, R.; Sanyal, A.J.; Kowdley, K.V.; Bhatt, D.L.; Alkhouri, N.; Frias, J.P.; Bedossa, P.; Harrison, S.A.; Lazas, D.; Barish, R.; et al. Randomized, Controlled Trial of the FGF21 Analogue Pegozafermin in NASH. New Engl. J. Med. 2023, 389, 998–1008. [CrossRef]
- Amatya, R.; Lee, D.; Min, K.A.; Shin, M.C. Pharmaceutical Strategies to Improve Druggability of Potential Drug Candidates in Nonalcoholic Fatty Liver Disease Therapy. Pharmaceutics 2023, 15, 1963. [CrossRef]
- A Harrison, S.; Frias, J.P.; Neff, G.; A Abrams, G.; Lucas, K.J.; Sanchez, W.; Gogia, S.; Sheikh, M.Y.; Behling, C.; Bedossa, P.; et al. Safety and efficacy of once-weekly efruxifermin versus placebo in non-alcoholic steatohepatitis (HARMONY): a multicentre, randomised, double-blind, placebo-controlled, phase 2b trial. Lancet Gastroenterol. Hepatol. 2023, 8, 1080–1093. [CrossRef]
- Brennan, P.N.; Elsharkawy, A.M.; Kendall, T.J.; Loomba, R.; Mann, D.A.; Fallowfield, J.A. Antifibrotic therapy in nonalcoholic steatohepatitis: time for a human-centric approach. Nat. Rev. Gastroenterol. Hepatol. 2023, 20, 679–688. [CrossRef]
- CLINICAL TRIALS OVERVIEW: We have designed a robust clinical development program to deliver EFX, if approved, as quickly as possible to patients in need.: Akero.
- Therapeutics, Inc; 2024 [Available from: https://akerotx.com/clinical-trials/.
- Jasleen, B.; Vishal, G.K.; Sameera, M.; Fahad, M.; Brendan, O.; Deion, S.; Pemminati, S. Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors: Benefits Versus Risk. Cureus 2023, 15, e33939. [CrossRef]
- Sangro, P.; Aláez, M.d.l.T.; Sangro, B.; D’avola, D. Metabolic dysfunction–associated fatty liver disease (MAFLD): an update of the recent advances in pharmacological treatment. J. Physiol. Biochem. 2023, 79, 869–879. [CrossRef]
- Xu, B.; Li, S.; Kang, B.; Zhou, J. The current role of sodium-glucose cotransporter 2 inhibitors in type 2 diabetes mellitus management. Cardiovasc. Diabetol. 2022, 21, 1–21. [CrossRef]
- Kansara, A.; Mubeen, F.; Shakil, J. SGLT2 Inhibitors in Patients with Chronic Kidney Disease and Heart Disease: A Literature Review. Methodist DeBakey Cardiovasc. J. 2022, 18, 62–72. [CrossRef]
- Ala, M. SGLT2 Inhibition for Cardiovascular Diseases, Chronic Kidney Disease, and NAFLD. Endocrinology 2021, 162. [CrossRef]
- Androutsakos, T.; Nasiri-Ansari, N.; Bakasis, A.-D.; Kyrou, I.; Efstathopoulos, E.; Randeva, H.S.; Kassi, E. SGLT-2 Inhibitors in NAFLD: Expanding Their Role beyond Diabetes and Cardioprotection. Int. J. Mol. Sci. 2022, 23, 3107. [CrossRef]
- Yaribeygi, H.; Maleki, M.; Jamialahmadi, T.; Moallem, S.A.; Sahebkar, A. HEPATIC BENEFITS OF SODIUM-GLUCOSE COTRANSPORTER 2 INHIBITORS IN LIVER DISORDERS. 2023, 22, 403–414. [CrossRef]
- He, K.; Li, J.; Xi, W.; Ge, J.; Sun, J.; Jing, Z. Dapagliflozin for nonalcoholic fatty liver disease: A systematic review and meta-analysis. Diabetes Res. Clin. Pr. 2022, 185, 109791. [CrossRef]
- Clayton-Chubb D, Kemp W, Majeed A, Lubel JS, Hodge A, Roberts SK. Understanding NAFLD: From Case Identification to Interventions, Outcomes, and Future Perspectives. Nutrients. 2023;15(3).
- Weng TM. A Single Center, Randomized, Open Label, Parallel Group, Phase 3 Study to Evaluate the Efficacy of Dapagliflozin in Subjects With Nonalcoholic Fatty Liver Disease National Taiwan University Hospital: ClinicalTrials.gov; 2024 [NCT05308160]. Available from: https://clinicaltrials.gov/study/NCT05308160?a=1.
- Zhang H. Dapagliflozin Efficacy and Action in NASH (DEAN) Nanfang Hospital, Southern Medical University: ClinicalTrials.gov; 2024 [Available from: https://clinicaltrials.gov/study/NCT03723252?a=3.
- Fraile JM, Palliyil S, Barelle C, Porter AJ, Kovaleva M. Non-Alcoholic Steatohepatitis (NASH) - A Review of a Crowded Clinical Landscape, Driven by a Complex Disease. Drug Des Devel Ther. 2021;15:3997-4009.
- Sumida, Y.; Yoneda, M.; Tokushige, K.; Kawanaka, M.; Fujii, H.; Yoneda, M.; Imajo, K.; Takahashi, H.; Eguchi, Y.; Ono, M.; et al. Antidiabetic Therapy in the Treatment of Nonalcoholic Steatohepatitis. Int. J. Mol. Sci. 2020, 21, 1907. [CrossRef]
- Sinakos E, Liava C, Loomba R. Emerging advances in the pharmacologic treatment of nonalcoholic steatohepatitis and related cirrhosis. Ann Gastroenterol. 2022;35(3):213-25.
- Fu, Y.; Zhou, Y.; Shen, L.; Li, X.; Zhang, H.; Cui, Y.; Zhang, K.; Li, W.; Chen, W.-D.; Zhao, S.; et al. Diagnostic and therapeutic strategies for non-alcoholic fatty liver disease. Front. Pharmacol. 2022, 13, 973366. [CrossRef]
- Werida R. Dapagliflozin in Type 2 Diabetes Mellitus Patients (T2DM) With Nonalcoholic Fatty Liver Disease (NAFLD) University of Alexandria2024 [NCT05459701]. Available from: https://classic.clinicaltrials.gov/ct2/show/study/NCT05459701.
- Cheung, K.S.; Ng, H.Y.; Hui, R.W.H.; Lam, L.K.; Mak, L.Y.; Ho, Y.C.; Tan, J.T.; Chan, E.W.; Seto, W.K.; Yuen, M.F.; et al. Effects of empagliflozin on liver fat in metabolic-dysfunction associated steatotic liver disease patients without diabetes mellitus: A randomized, double-blind, placebo-controlled trial. Hepatology 2024. [CrossRef]
- Cheung KS. Effect of Empagliflozin on Liver Fat in Non-diabetic Patients The University of Hong Kong: ClinicalTrials.gov; 2024 [NCT04642261]. Available from: https://clinicaltrials.gov/study/NCT04642261.
- Kuhre RE, Deacon CF, Holst JJ, Petersen N. What Is an L-Cell and How Do We Study the Secretory Mechanisms of the L-Cell? Front Endocrinol (Lausanne). 2021;12:694284.
- Liarakos, A.L.; Koliaki, C. Novel Dual Incretin Receptor Agonists in the Spectrum of Metabolic Diseases with a Focus on Tirzepatide: Real Game-Changers or Great Expectations? A Narrative Review. Biomedicines 2023, 11, 1875. [CrossRef]
- Cigrovski Berkovic M, Rezic T, Bilic-Curcic I, Mrzljak A. Semaglutide might be a key for breaking the vicious cycle of metabolically associated fatty liver disease spectrum? World J Clin Cases. 2022;10(20):6759-68.
- Koureta, E.; Cholongitas, E. Evolving role of semaglutide in NAFLD: in combination, weekly and oral administration. Front. Pharmacol. 2024, 15, 1343587. [CrossRef]
- Wilding, J.P.H.; Batterham, R.L.; Calanna, S.; Davies, M.; Van Gaal, L.F.; Lingvay, I.; McGowan, B.M.; Rosenstock, J.; Tran, M.T.; Wadden, T.A.; et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N. Engl. J. Med. 2021, 384, 989–1002. [CrossRef]
- Zhu, K.; Kakkar, R.; Chahal, D.; Yoshida, E.M.; Hussaini, T. Efficacy and safety of semaglutide in non-alcoholic fatty liver disease. World J. Gastroenterol. 2023, 29, 5327–5338. [CrossRef]
- Newsome, P.N.; Buchholtz, K.; Cusi, K.; Linder, M.; Okanoue, T.; Ratziu, V.; Sanyal, A.J.; Sejling, A.-S.; Harrison, S.A. A Placebo-Controlled Trial of Subcutaneous Semaglutide in Nonalcoholic Steatohepatitis. New Engl. J. Med. 2021, 384, 1113–1124. [CrossRef]
- Flint, A.; Andersen, G.; Hockings, P.; Johansson, L.; Morsing, A.; Palle, M.S.; Vogl, T.; Loomba, R.; Plum-Mörschel, L. Randomised clinical trial: semaglutide versus placebo reduced liver steatosis but not liver stiffness in subjects with non-alcoholic fatty liver disease assessed by magnetic resonance imaging. Aliment. Pharmacol. Ther. 2021, 54, 1150–1161. [CrossRef]
- Romero-Gómez, M.; Shankar, R.R.; Chaudhri, E.; Liu, J.; Lam, R.L.; Kaufman, K.D.; Engel, S.S.; Bruzone, S.O.; Coronel, M.J.; Gruz, F.M.; et al. A phase IIa active-comparator-controlled study to evaluate the efficacy and safety of efinopegdutide in patients with non-alcoholic fatty liver disease. J. Hepatol. 2023, 79, 888–897. [CrossRef]
- Merck granted Fast Track Designation by the U.S. FDA for MK-6024 for the treatment of Nonalcoholic Steatohepatitis (NASH): Merck & Co., Inc.; 2023 [Available from: https://www.merck.com/news/merck-to-present-data-for-efinopegdutide-mk-6024-an-investigational-glp-1-glucagon-receptor-co-agonist-in-patients-with-nonalcoholic-fatty-liver-disease-nafld-at-easl-2023/.
- A Clinical Study of Efinopegdutide in Participants With Precirrhotic Nonalcoholic Steatohepatitis (NASH) (MK-6024-013): ClinicalTrials.gov; 2024 [NCT05877547, sponsor- Merck Sharp & Dohme LLC]. Available from: https://clinicaltrials.gov/study/NCT05877547.
- Forzano, I.; Varzideh, F.; Avvisato, R.; Jankauskas, S.S.; Mone, P.; Santulli, G. Tirzepatide: A Systematic Update. Int. J. Mol. Sci. 2022, 23, 14631. [CrossRef]
- Lilly Reports Strong Fourth-Quarter 2023 Financial Results and Provides 2024 Guidance: Eli Lilly and Company; February 6, 2024 [Available from: https://investor.lilly.com/news-releases/news-release-details/lilly-reports-strong-fourth-quarter-2023-financial-results-andAvailable from: https://investor.lilly.com/node/50281/pdf.
- Qiu, Y.-Y.; Zhang, J.; Zeng, F.-Y.; Zhu, Y.Z. Roles of the peroxisome proliferator-activated receptors (PPARs) in the pathogenesis of nonalcoholic fatty liver disease (NAFLD). Pharmacol. Res. 2023, 192, 106786. [CrossRef]
- Vitulo, M.; Gnodi, E.; Rosini, G.; Meneveri, R.; Giovannoni, R.; Barisani, D. Current Therapeutical Approaches Targeting Lipid Metabolism in NAFLD. Int. J. Mol. Sci. 2023, 24, 12748. [CrossRef]
- Staels, B.; Butruille, L.; Francque, S. Treating NASH by targeting peroxisome proliferator-activated receptors. J. Hepatol. 2023, 79, 1302–1316. [CrossRef]
- Mazhar, I.J.; Yasir, M.; Sarfraz, S.; Shlaghya, G.; Narayana, S.H.; Mushtaq, U.; Ameen, B.S.; Nie, C.; Nechi, D.; Penumetcha, S.S. Vitamin E and Pioglitazone: A Comprehensive Systematic Review of Their Efficacy in Non-alcoholic Fatty Liver Disease. Cureus 2023, 15, e43635. [CrossRef]
- Lee, K.-C.; Wu, P.-S.; Lin, H.-C. Pathogenesis and treatment of non-alcoholic steatohepatitis and its fibrosis. Clin. Mol. Hepatol. 2023, 29, 77–98. [CrossRef]
- Kamata, S.; Honda, A.; Ishii, I. Current Clinical Trial Status and Future Prospects of PPAR-Targeted Drugs for Treating Nonalcoholic Fatty Liver Disease. Biomolecules 2023, 13, 1264. [CrossRef]
- Lange, N.F.; Graf, V.; Caussy, C.; Dufour, J.-F. PPAR-Targeted Therapies in the Treatment of Non-Alcoholic Fatty Liver Disease in Diabetic Patients. Int. J. Mol. Sci. 2022, 23, 4305. [CrossRef]
- Huang, J.-F.; Dai, C.-Y.; Huang, C.-F.; Tsai, P.-C.; Yeh, M.-L.; Hsu, P.-Y.; Huang, S.-F.; Bair, M.-J.; Hou, N.-J.; Huang, C.-I.; et al. First-in-Asian double-blind randomized trial to assess the efficacy and safety of insulin sensitizer in nonalcoholic steatohepatitis patients. Hepatol. Int. 2021, 15, 1136–1147. [CrossRef]
- Lian, J.; Fu, J. Pioglitazone for NAFLD Patients With Prediabetes or Type 2 Diabetes Mellitus: A Meta-Analysis. Front. Endocrinol. 2021, 12. [CrossRef]
- Rong, L.; Zou, J.; Ran, W.; Qi, X.; Chen, Y.; Cui, H.; Guo, J. Advancements in the treatment of non-alcoholic fatty liver disease (NAFLD). Front. Endocrinol. 2023, 13, 1087260. [CrossRef]
- Tidwell, J.; Balassiano, N.; Shaikh, A.; Nassar, M. Emerging therapeutic options for non-alcoholic fatty liver disease: A systematic review. World J. Hepatol. 2023, 15, 1001–1012. [CrossRef]
- Gawrieh S, Noureddin M, Loo N, Mohseni R, Awasty V, Cusi K, et al. Saroglitazar, a PPAR-α/γ Agonist, for Treatment of NAFLD: A Randomized Controlled Double-Blind Phase 2 Trial. Hepatology. 2021;74(4):1809-24.
- Aggarwal, M.; Lindenmeyer, C.C. From cause to consequence: Insights into incident diabetes mellitus after hepatic steatosis. Clin. Liver Dis. 2023, 21, 41–46. [CrossRef]
- Gastaldelli, A. Is it necessary to target lipid metabolism in different organs for effective treatment of NASH?—the results of the Pan-PPAR Lanifibranor trial. HepatoBiliary Surg. Nutr. 2022, 11, 481–484. [CrossRef]
- Kamata S, Honda A, Ishikawa R, Akahane M, Fujita A, Kaneko C, et al. Functional and Structural Insights into the Human PPARα/δ/γ Targeting Preferences of Anti-NASH Investigational Drugs, Lanifibranor, Seladelpar, and Elafibranor. Antioxidants (Basel). 2023;12(8).
- Lefere, S.; Puengel, T.; Hundertmark, J.; Penners, C.; Frank, A.K.; Guillot, A.; de Muynck, K.; Heymann, F.; Adarbes, V.; Defrene, E.; et al. Differential effects of selective- and pan-PPAR agonists on experimental steatohepatitis and hepatic macrophages. J. Hepatol. 2020, 73, 757–770. [CrossRef]
- Mollerhoj, M.B.; Veidal, S.S.; Thrane, K.T.; Oro, D.; Overgaard, A.; Salinas, C.G.; Madsen, M.R.; Pfisterer, L.; Vyberg, M.; Simon, E.; et al. Hepatoprotective effects of semaglutide, lanifibranor and dietary intervention in the GAN diet-induced obese and biopsy-confirmed mouse model of NASH. Clin. Transl. Sci. 2022, 15, 1167–1186. [CrossRef]
- Francque, S.M.; Bedossa, P.; Ratziu, V.; Anstee, Q.M.; Bugianesi, E.; Sanyal, A.J.; Loomba, R.; Harrison, S.A.; Balabanska, R.; Mateva, L.; et al. A Randomized, Controlled Trial of the Pan-PPAR Agonist Lanifibranor in NASH. New Engl. J. Med. 2021, 385, 1547–1558. [CrossRef]
- Paternostro, R.; Trauner, M. Current treatment of non-alcoholic fatty liver disease. J. Intern. Med. 2022, 292, 190–204. [CrossRef]
- Machado, M.V. MASLD treatment—a shift in the paradigm is imminent. Front. Med. 2023, 10, 1316284. [CrossRef]
- Driessen, S.; Francque, S.M.; Anker, S.D.; Cabezas, M.C.; Grobbee, D.E.; Tushuizen, M.E.; Holleboom, A.G. Metabolic dysfunction-associated steatotic liver disease and the heart. Hepatology 2023. [CrossRef]
- Wang, X.; Wu, S.; Yuan, X.; Chen, S.; Fu, Q.; Sun, Y.; Lan, Y.; Hu, S.; Wang, Y.; Lu, Y.; et al. Metabolic Dysfunction-associated Fatty Liver Disease and Mortality Among Chinese Adults: a Prospective Cohort Study. J. Clin. Endocrinol. Metab. 2021, 107, e745–e755. [CrossRef]
- Zhang, B.; Feng, Y.; Lu, J. Progress in the Treatment of Metabolic-Related Fatty Liver Disease. Altern Ther Health Med. 2023, 29, 86–93.
- Ratziu, V.; Charlton, M. Rational combination therapy for NASH: Insights from clinical trials and error. J. Hepatol. 2023, 78, 1073–1079. [CrossRef]
- Jeeyavudeen, M.S.; Khan, S.K.; Fouda, S.; Pappachan, J.M. Management of metabolic-associated fatty liver disease: The diabetology perspective. World J. Gastroenterol. 2023, 29, 126–143. [CrossRef]
| STUDY DRUG | RCT | SPONSOR | COUNTRY | STUDY END | RESULTS |
|---|---|---|---|---|---|
| RESMETIROM (MGL-3196) |
NCT02912260 (OLE) | Madrigal Pharmaceuticals, Inc. | United States | 2018. | Reduction in fibrosis, LDL and TG levels. |
| NCT03900429 (MAESTRO-NASH) | Ongoing | N/A | |||
| VK2809 | NCT02927184 | Viking Therapeutics, Inc | United States | 2019. | Reduction in LDL-C, other hepatic lipid content and ALT |
| NCT04173065 (VOYAGE) | Ongoing | Reduction of hepatic fat content1. | |||
| PEGOZAFERMIN (BIO89-100) |
NCT04929483 (ENLIVEN) | 89bio, Inc. | United States | Ongoing | Reduction of fibrosis. |
| NCT06318169 (ENLIGHTEN-Fibrosis) |
Ongoing | N/A | |||
| EFRUXIFERMIN | NCT04767529 (HARMONY) | Akero Therapeutics, Inc | United States | 2022. | Improvement of liver fibrosis by at least one stage, without MASH worsening. |
| NCT06215716 (SYNCHRONY Histology) |
Ongoing | N/A | |||
| NCT06161571(SYNCHRONY Real-World) | Ongoing | N/A | |||
| DAPAGLIFLOZIN | NCT05308160 | National Taiwan University Hospital | Taiwan | Ongoing | N/A |
| NCT03723252 (DEAN) | Nanfang Hospital, Southern Medical University | China | 2024. | N/A | |
| NCT05459701 | Rehab Werida | Egypt | Ongoing | N/A | |
| EMPAGLIFLOZIN | NCT04642261 | The University of Hong Kong | China | 2023. | Reduction of body weight, waist circumference, fasting blood glucose. |
| SEMAGLUTIDE | NCT02970942 | Novo Nordisk A/S | United States | 2020. | Reduction of ALT level, liver inflammation and steatosis. |
| NCT03357380 | Germany | 2020. | |||
| NCT04822181 (ESSENCE) | United States | Ongoing | N/A | ||
| EFINOPEGDUTIDE (MK-6024) |
NCT04944992 (MK-6024-001) | Merck Sharp & Dohme LLC | United States | 2022. | Reduction in hepatic fat. |
| NCT05877547 (MK-6024-013) | Ongoing | N/A | |||
| TIRZEPATIDE | NCT04166773 (SYNERGY-NASH) | Eli Lilly and Company | United States | 2024. | Resolution of MASH and no worsening of fibrosis.2 |
| SAROGLITAZAR | NCT03061721 (EVIDENCES IV) | Zydus Therapeutics Inc. | United States | 2020. | Reduction of liver fat content, ALT, triglycerides, adiponectin and insulin resistance. |
| NCT05011305 | Ongoing | N/A | |||
| PIOGLITAZONE | NCT01068444 | Kaohsiung Medical University Chung-Ho Memorial Hospital | Taiwan | 2020. | Reduction of liver fat content and inflammation. MASH resolution without fibrosis worsening. |
| NCT04501406 | University of Florida | United States | Ongoing | N/A | |
| LANIFIBRANOR (IVA 337) |
NCT03008070 (NATIVE) | Inventiva Pharma | United States | 2020. | Reduction of the SAF-A score by at least 2 points without fibrosis worsening. |
| NCT04849728 (NATIV3) | Ongoing | N/A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





