1. Introduction
Lack of regular toothbrushing leads to the accumulation of dental biofilm and gingivitis develops within three weeks. The first clinical sign is bleeding on positive probing (BoP), demonstrated by Löe [
1]. Thus, before the onset of clinical signs, an inflammatory gingival response has already been initiated as a reaction to bacterial invasion. Chronic inflammation causes not only inflammation in the gingiva but also destruction of the alveolar bone, leading to periodontitis [
2,
3]. It can be said that dental plaque is a necessary and sufficient causative factor for the development of gingivitis; however, the mature biofilm itself is not a sufficient causative factor in the pathogenesis of destructive periodontal disease. Periodontal chart scores (FMPS, FMBS) are available for the diagnosis of plaque-induced inflammation. New diagnostic devices are also available to diagnose inflammatory processes in interdental spaces (BOB) [
4,
5].
On the other hand, human saliva as a biological fluid can be a non-invasive diagnostic approach in oral and systematic diseases [
6]. It is rich in disease-related biomarkers such as matrix metalloproteinases, which can be used to detect early stage periodontal disease detection [
7,
8]. Matrix metalloproteinases obviously play a decisive role in pathological inflammatory processes and malignant tissue destruction [
9,
10,
11,
12]. It has been shown that matrix metalloproteinase-8 (MMP-8), as a collagenase in gingival connective tissue, is an early biomarker of periodontitis which can be measured not only with laboratory methods but also with chair-side tests. These techniques use the same monoclonal antibodies [
13,
14,
15]. Lysosomal enzymes released during phagocytosis, such as MMP-8, are discharged into the oral cavity with the sulcus fluid and no tissue damage occurs [
16,
17].
The aim of our study was to evaluate the effectiveness of individualized oral hygiene education and its role in oral prevention in patients visiting our Institute (Department of Community Dentistry, Semmelweis University) with various dental problems. Furthermore, we compared four oral hygiene devices (Solo Prophylaxis, toothbrush and commercially available interdentalbrushes as well as electric and manual toothbrush) thus subgrouping them according to the most common tooth cleaning devices used in the clinical study. Finally, to find out what motivational techniques our patients need to continue to maintain good oral hygiene.
Our hypothesis is that a well-constructed dental hygiene concept with education and lifelong follow-up can reduce and stop oral inflammatory processes, thus preventing gingival and periodontal diseases at an early stage.
2. Materials and Methods
The study was conducted at the Department of Community Dentistry, Semmelweis University, Hungary between 1 September 2020 and 30 April 2023. The examination was conducted by a team of dentists and dental hygienists from the Prevention and Periodontology Department of the Department of Community Dentistry, Semmelweis University. The measurements of the six-person investigation team were standardized using the Fleiss kappa test (0.9) before the start of the investigation [
18]. Subjects were selected from patients presenting to the Periodontology and Prevention Department of the Department of Community Dentistry. Participation in the study was voluntary, with a total of 102 subjects included. The study was approved by the Regional and Institutional Committee of Science and Research Ethics and the Hungarian Office of Health Authorization and Administrative Procedures, and was conducted in accordance with the Declaration of Helsinki. (Nr: ETT-TUKEB IV/9854-1/2021/EKU) All patients provided written informed consent prior to participation. All authors had access to information that could be used to identify individual participants during data collection between 1 September 2020 and 30 April 2023.
After an initial stomato-oncology, clinical and radiological examination, four main parameters were recorded during appointments at fixed times. The first of the four measurements was Bleeding on Brushing index (BOB), a new measurement method to determine how many interdental spaces in the mouth bleed as a result of stimulation. Bleeding is a clinical sign of the presence of an inflammatory process. The measuring and stimulating tool was a custom-designed interdental brush called DiagnoSTIX, manufactured by SOLO-MED GmbH, which created the concept of SOLO Prophylaxis, referred to as Prophylaxis Concept. DiagnoSTIX was applied one by one to each interdental space, and it was observed how many interdental spaces were bleeding compared to the total number of interdental spaces. (e.g., 20/13) [
19]. BOB is expressed as the percentage of bleeding interdental spaces of the patient.
The second of the four measurements was MMP-8, which is a neutrophil collagenase, involved in types I, II and III of collagen breakdown. An early marker of periodontal tissue destruction, its elevated level indicates inflammation before inflamed gingival margin is clinically detectable. The measuring device was the PerioSafe PRO DRS Test System, a chair-side test based on enzyme-linked immunosorbent assay (ELISA). The device measures the quantitative level of MMP-8 in the saliva and displays this as a numerical value in ng/ml. On the basis of these data, an interval table for the system determined whether collagenolysis was minimal, elevated, or whether it was advanced and severe. The only objectively monitorable marker of the extent of inflammation was the concentration of MMP-8 in the sulcus inflammatory exudate, measured in ng/ml [
20,
21].
The third and fourth measurements were based on the periodontal chart used as a reference by the School of Dental Medicine of the University of Bern (
periodontalchart-online.com), measurements were also conducted during the appointments of each patient. The full mouth bleeding score (FMBS) is a percentage value, calculated from the bleeding. Bleeding on probing (BoP) values were recorded at six points on each tooth when the full periodontal status was taken. The measuring device was the PCPUNC 15 periodontal probe [
22,
23].
The full mouth plaque score (FMPS) is a percentage value calculated from the plaque index (PI) values at six points on each tooth when the full periodontal status is taken. The measuring device was also the PCPUNC 15 periodontal probe [
22,
23]. The data of all patients participating in the long-term follow-up study were recorded in an application designed in collaboration by the University of Obuda for easier documentation.
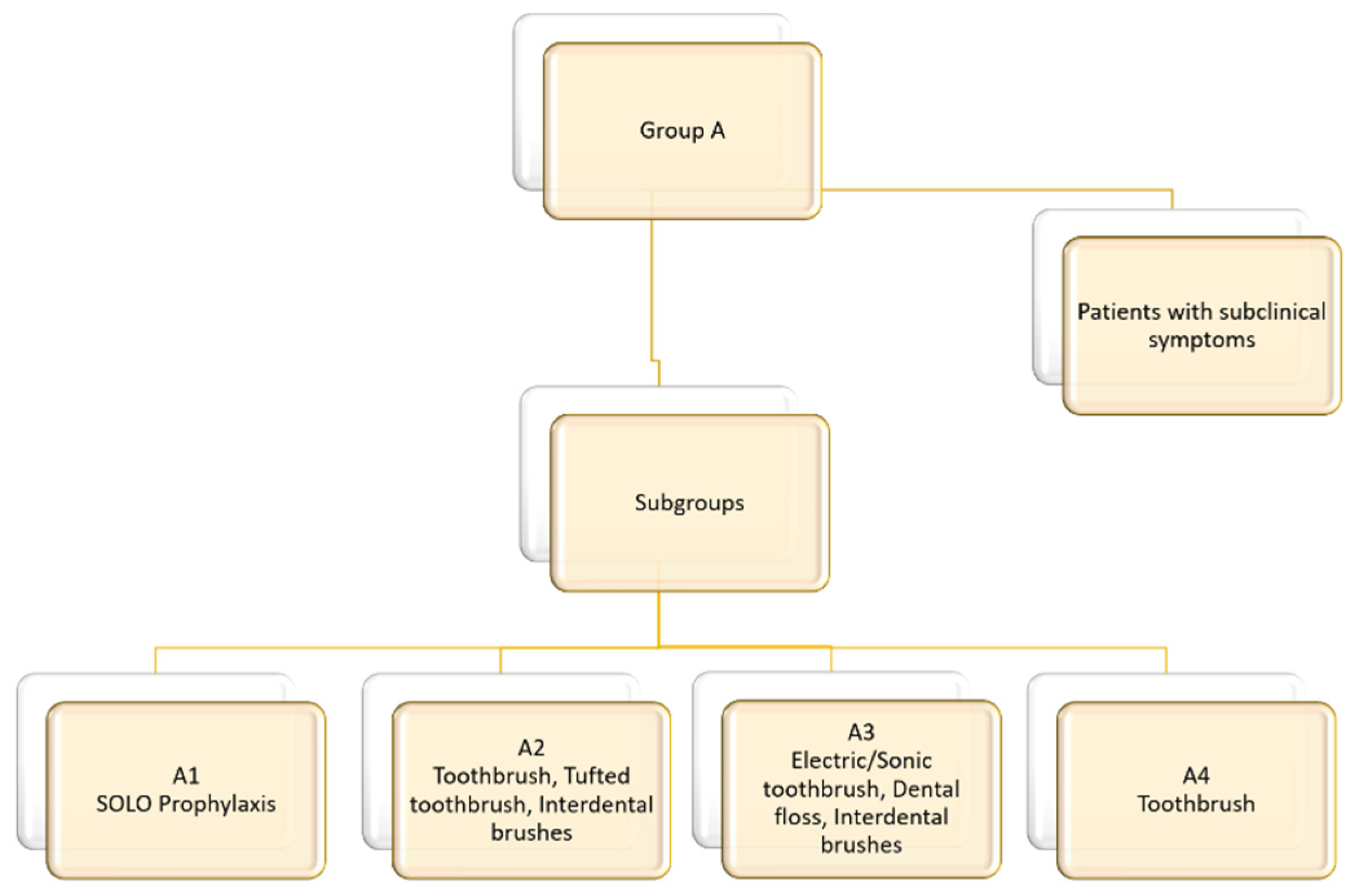
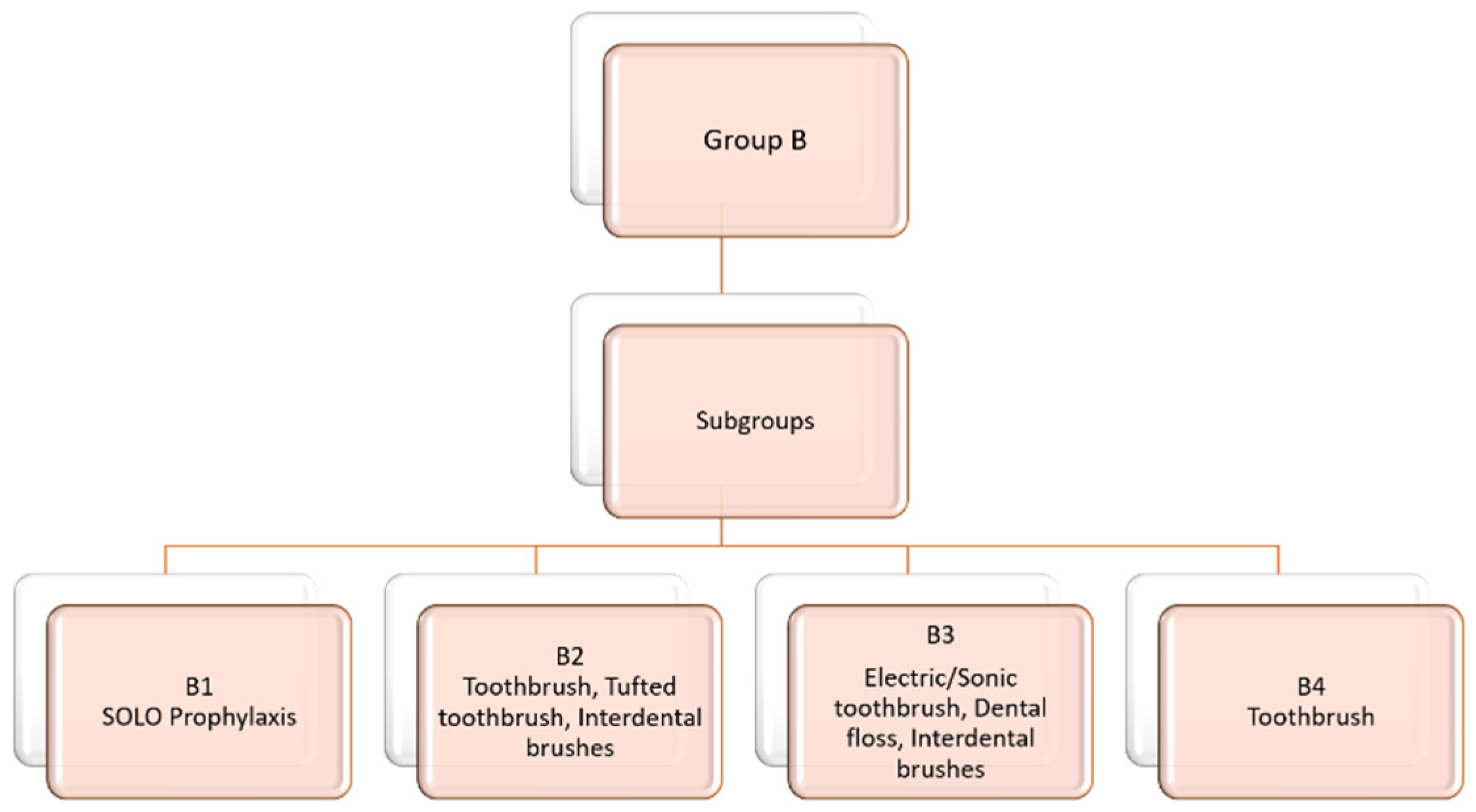
Participants received the patient information sheet and the patient consent form, and if they accepted the conditions, they signed them. After signing, subjects were assigned to two groups (A or B) based on their periodontal status, each group containing four subgroups (1, 2, 3 and 4) based on their oral hygiene habits and the tools used for tooth cleaning (A1, A2, A3, A4, B1, B2, B3 and B4). Before group assignment, all oral hygiene toolkits were presented during the first examination. Patients selected the toolkits they would use during the study. Patients were instructed on the correct use of the chosen toolkit. At the end of the study, all patients in the groups received our preferred oral hygiene education, thus avoiding discrimination.
According to their radiological and clinical examination, patients in group A had neither periodontal damage nor bone loss, only clinical symptoms of gingivitis. Within group A and beside the four subgroups (A1, A2, A3 and A4), there was an individual group called ”Patients with subclinical symptoms”, who had PPD (periodontal probing depth) anywhere less than or equal to 4 mm, and FMPS and FMBS values below 35%. There were no clinical signs of gingivitis so BOB and MMP-8 values could be detected and a pre-existing inflammatory process could be diagnosed. Bone loss in subjects in group B could be determined using the radiological and clinical examination, and PPD values of 5 mm or more. Patients in subgroupsA1 and B1 attended a lecture on the Prophylaxis Concept, during which they were introduced to the Solo Prophylaxis philosophy and the use of individualized oral hygiene tools. These patients used the oral hygiene devices included in the system. Patients in subgroups A2 and B2 used any other commercially available interdental brushes, possibly tufted toothbrushes, and manual toothbrushes. Patients in subgroups A3 and B3 used electric or sonic toothbrushes, any other commercially available interdental brushes and/or dental floss. Patients in subgroups A4 and B4 used only manual toothbrushes. (
Figure 1 and
Figure 2) All patients in each group attended the examinations at the first appointment, and then 2, 4 and 12 weeks after the first appointment. At each test time, subjects participating in the study received professional oral hygiene treatment after the measurements.
Exclusion factors included smoking, mental and physical disabilities, patients under 18 years of age, patients undergoing orthodontic treatment, pregnancy, patients with less than six interdental spaces, oncological diseases, hematological diseases, genetic disorders, diabetes, bisphosphonate consumption, pacemaker, and infectious diseases.
2.1. Data Collection
The study was conducted on 102 patients (38 male and 66 female). The number of patients in the subroups was in A1:12; A2: 1; A3: 17; A4: 16; B1: 17; B2: 15, B3: 9; and B4: 5. During the first examination, study team members educated patients on how to optimize the use of devices according to their oral hygiene habits, and introduced the Prophylaxis Concept to them. Patients returned 2, 4 and 12 weeks after the first visit to be re-assessed, and to recieve professional oral hygiene treatment. MMP-8, BOB, FMPS and FMBS values were recorded at each visit.
2.2. Statistical Analysis
To assess the effects of different oral hygiene methods on MMP-8, BOB, FMPS and FMBS, we applied generalized linear mixed-effects models (GLMMs) [
24] using R 4.3.3 [
25] with the glmmTMB package [
26]. Patients in groups A and B as well asa group of patients with subclinical symptoms were analyzed separately. MMP-8 levels, BOB, FMPS and FMBS were analyzed as dependent variables in separate models and time (first appointment, 2, 4 and 12 weeks later) and subgroups (1, 2, 3 and4) and their interaction were included in all models. To view individual changes, patient ID was included as a random factor in all models. When analyzing MMP-8, we used models with Gamma-distribution and log-link function. Six patients (four from B2, two from B1) had values above 400 ng/ml and three patients (one each from A2, A4 and B2) had values under 10 ng/ml value at some point, and were excluded from the analysis of MMP-8. For the analysis, we modeled the percentages of BOB, FMPS and FMPS binomially (bleeding or presence of plaque and the assessed sites in absence of bleeding or plaque). To avoid overdispersion, we used the betabinomial model family. Our model selection approach was based on the Akaike Information Criterion (AIC) for all models [
27]. We removed explanatory variables one by one, and chose the candidate model with the lowest AIC value. We considered a model to be a better fit if the AIC value was lower by 2. We did not remove main effects before their interactions. If the AIC value of two or more models differed by 2 or less, we chose the simpler model. We repeated this, until we achieved an optimal model fit. We used a deviance-ratio test to test the significance of the fixed terms in the final models. All models run can be viewed in the Appendix, with detailed results of the final models. Residual analysis and model validation were performed using the Dharma package [
28], as described by Smith and Warren (2023) [
29]. Post-hoc contrasts were calculated with the emmeans package [
30], using Sidak correction to adjust for multiple comparisons.
3. Results
3.1. Patients with Subclinical Symptoms
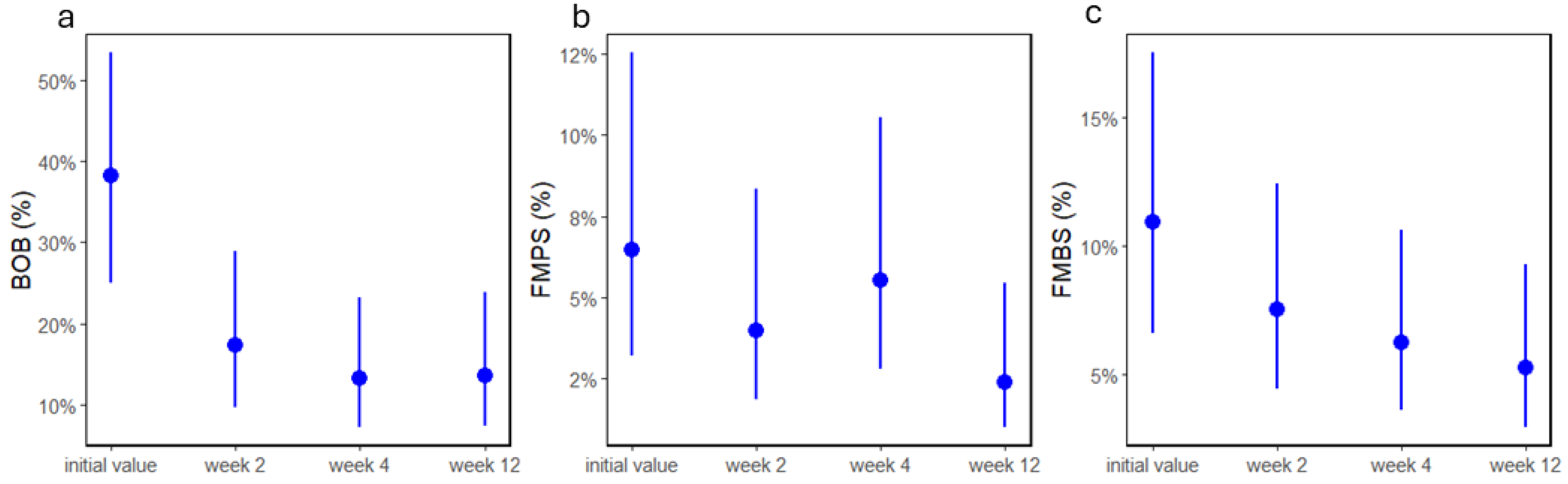
Alltogether, 29 patients had subclinical symptoms (19 female, 10 male; 7 in subgroup A1, 6 in A2, 10 in A3, the only patient in B3 was removed from further analyses). After model selection, BOB showed a significant time effect (p>0.0001,
Figure 3a). Post-hoc analyses revealed that after the first treatment, BOB significantly decreased (all adj. p<0.005, and remained at this level (all adj. p>0.77). When analyzing MMP-8, we found that two patients had values under 10 ng/ml, therefore they were removed from the analyses. There were no significant effects of time or subgroup on MMP-8 (all p>0.5). Time had a significant effect on FMPS (p=0.036;
Figure 3b), whereas FMBS only marginally decreased in time (p=0.055,
Figure 3c). Post-hoc tests revealed that there were differences only between the initial and week 12 values of both FMBS (adj. p=0.027) and FMPS (adj. p=0.054), all other adj. p>0.95.
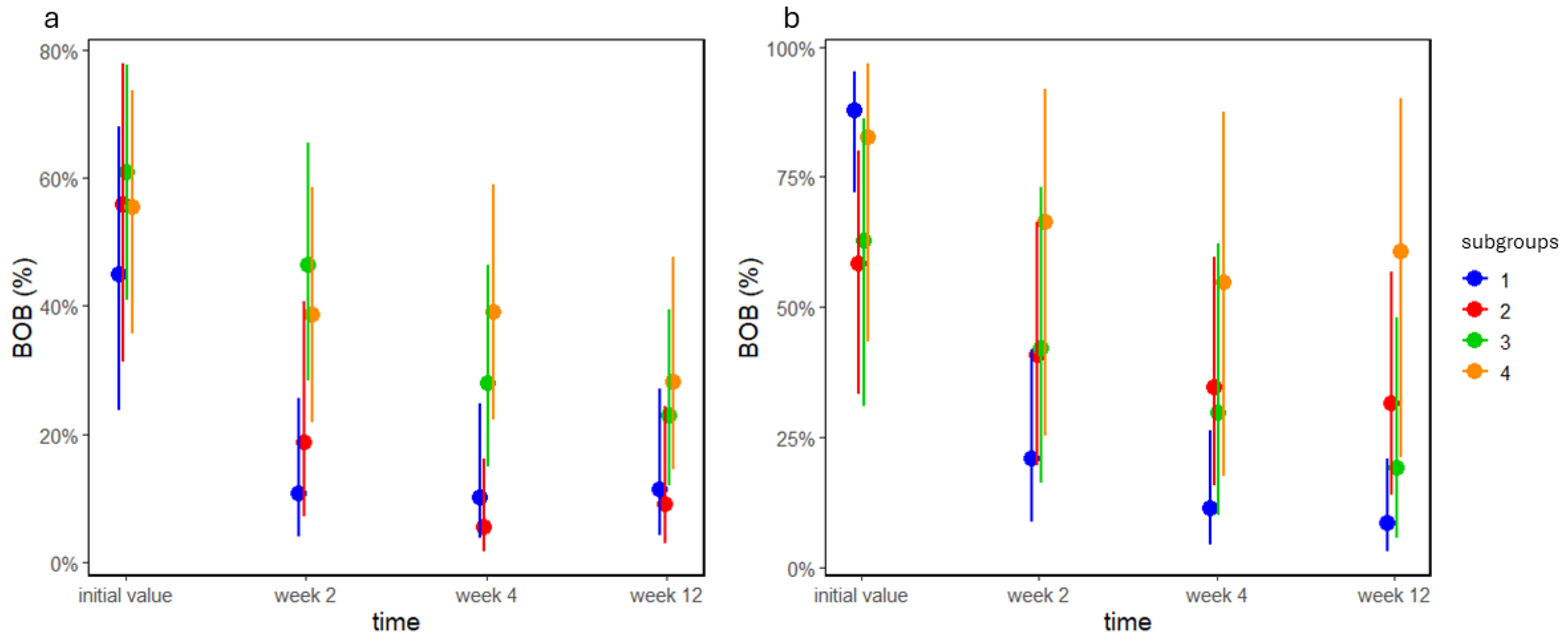
3.2. BOB
The analysis of BOB in group A revealed a significant interaction between time and subgroup (p=0.009;
Figure 4a). Post-hoc analysis by time revealed that BOB decreased in A1 and A2 after week 2 (all adj. p<0.006), and remained there (all adj. p>0.22). In subgroup A3, BOB decreased between weeks 2 and 4 (adj. p=0.001), whereas it did not change between the other appointments (all adj. p>0.88); however in A4, BOB differed only between the initial and week 12 adj. (p=0.034). Contrasts between groups showed that subgroups 1 and 3 were different marginally at week 2 (adj. p=0.07), whereas subgroups 2 and 4 were significantly different at week 4. In group B, the interaction between time and subgroup was also significant (p<0.0001;
Figure 4b). The post-hoc analysis by time showed that in B1, BOB significantly decreased after week 2 (adj. p<0.0001) and remained there (all adj p>0.75). In B2 and B3, BOB decreased only after week 4 (adj. p=0.027), and remained there (all adj p>0.55), whereas there was no change in B4 (all adj. p>0.31)
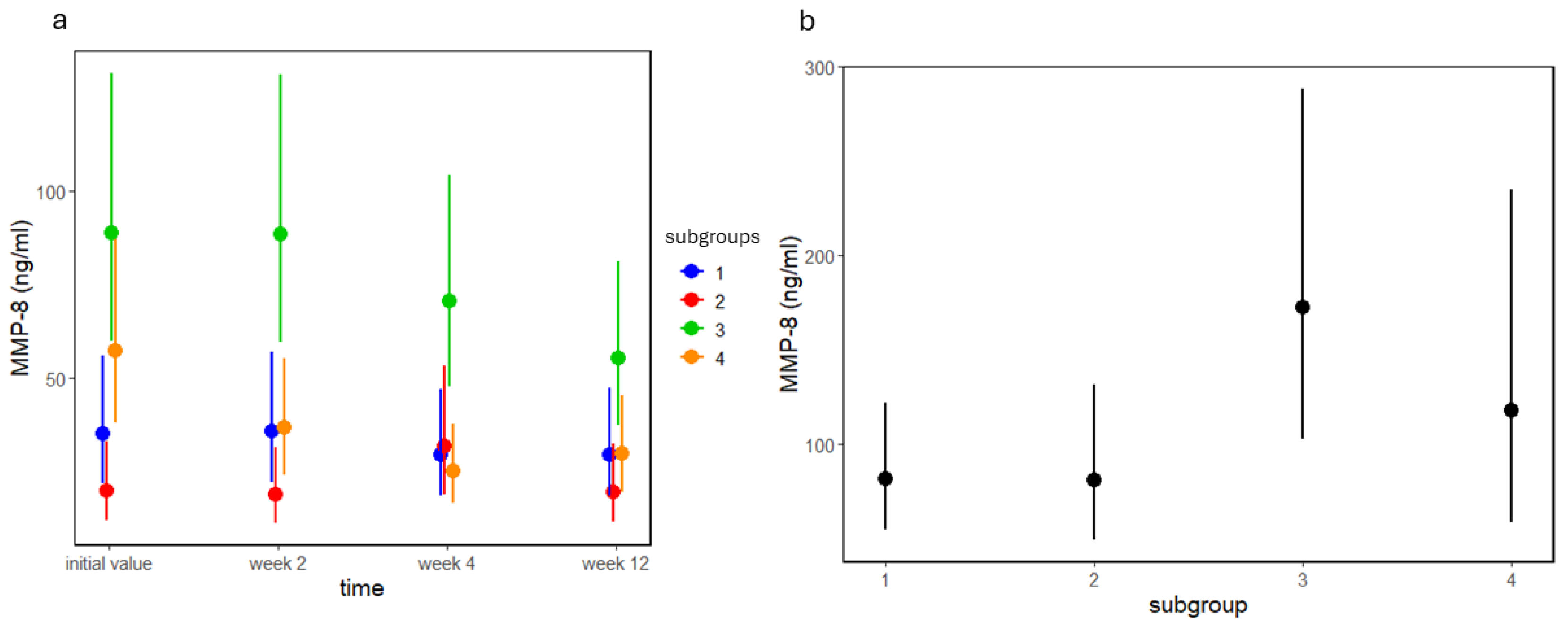
3.3. MMP-8
The analysis of MMP-8 in group A revealed a significant subgroup-time interaction (p=0.008;
Figure 5a). The post-hoc analysis by time showed that MMP-8 decreased only in A4 at week 4 (adj. p<0.0001), whereas in all other cases, it remained the same (all adj. p>0.21). The initial MMP-8 levels of A2 significantly differed from A3 (adj. p<0.0001) and A4 (adj. p=0.037), and A3 marginally differed from A1 (adj. p=0.064; all other adj. p>0.9). At week 2, there were marginal differences between A1 and A3 (p=0.077), whereas the difference was significant between A2-A3 (adj. p<0.0001) and A3-A4 (p=0.048; all other adj. p>0.69). At week 4, the difference between A3 and A4 remained (adj. p=0.006; all other adj. p>0.1). At week 12, there was a significant difference between A2 and A3 (adj. p=0.035; all other adj. p>0.52). In group B, there was a marginal subgroup effect (p=0.083), and the post-hoc analysis showed no significant contrasts (all adj. p>0.1;
Figure 5b).
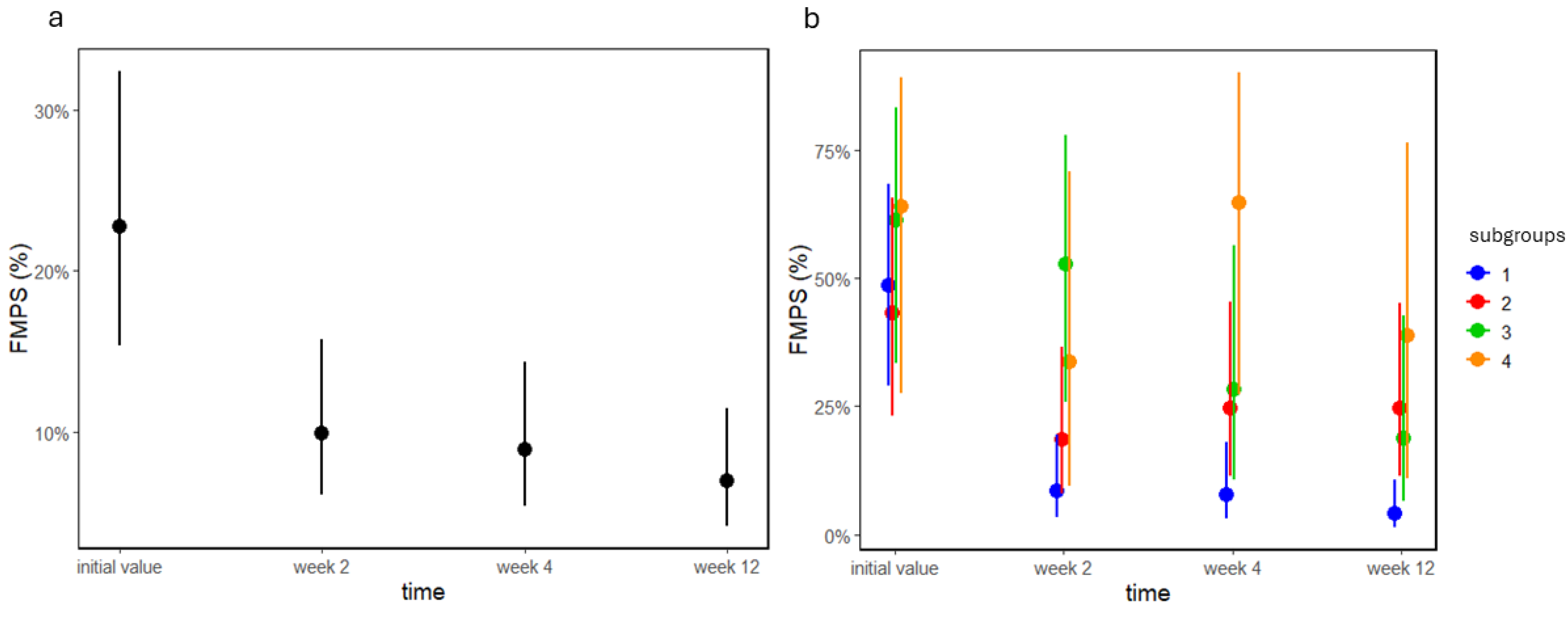
3.4. FMPS
In group A, there was a significant time effect on FMPS (p<0.0001;
Figure 6a). Post-hoc analysis revealed that FMPS significantly decreased at week 2 (adj. p<0.0001), and remained at that level until the end of the study (all adj. p>0.41). In groups B, the time-subroup interaction was significant (p=0.001;
Figure 6b). Contrasts by time showed that in B1, FMPS decreased at week 2 (adj. p<0.0001), and remained at this level (all adj. p>0.9). In B2, FMPS did not change (all adj. p>0.11), whereas in groups B3 and B4, the only difference was in B3 between the initial and week 12 values (adj. p=0.005; all other adj. p>0.6). At week 2, B1 had significantly lower FMPS than B3 (adj. p=0.028), whereas FMPS of B1 and B4 differed at week 4 (adj. p=0.023). There was a marginal difference between B1 and B2 at the end of the study.
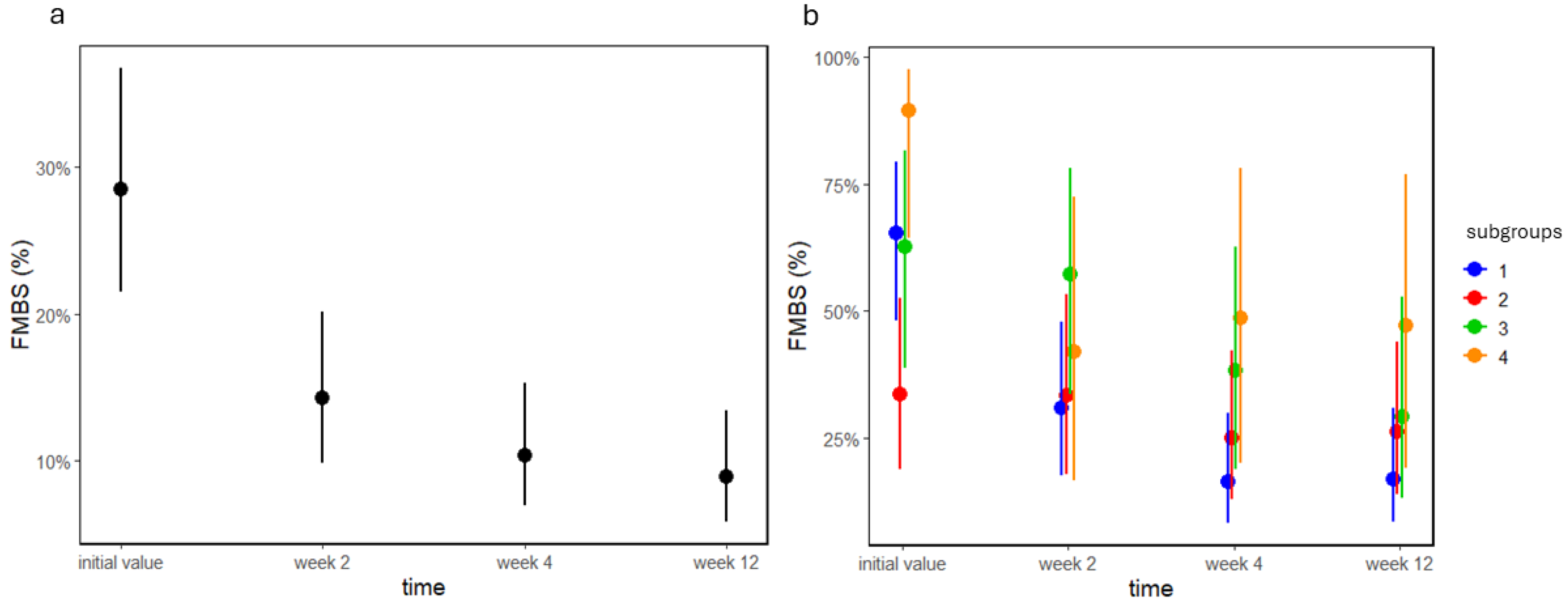
3.5. FMBS
In group A, time had a significant effect on FMBS (p<0.0001,
Figure 7a). Post-hoc analysis showed that FMBS significantly decreased at week 2 (adj. p<0.001), and stayed at this level (all adj. p>0.12). There was a significant interaction between subgroups and time in group B (p=0.005,
Figure 7b). Contrasts by time showed that in B1 FMBS significantly decreased at week 2 (adj. p<0.001), and remained at a low level (all adj. p>0.49). In B2, FMBS did not change (all adj. p>0.6); however, in both B3 and B4, there was a moderate decrease in FMBS at week 12 (all adj. p<0.084). This means that B2 started from a low level of FMBS, and remained there, and B1 caught up to this level, whereas B3 and B4 barely improved.
4. Discussion
According to Scandinavian studies in the 1970s, oral hygiene programs brought significant improvements in the first period, but did not have the expected long-term follow-up effect. In the last decade, attention has focused mainly on interproximal areas, as it has been proven that the most effective manual toothbrush, but not even the electric toothbrush, provides sufficient interproximal cleaning. The regular use of dental floss and custom-sized proximal toothbrushes are recommended for older people or for those with open interdental spaces [
31,
32].
It has become clear that only individual motivation, professional oral hygiene chairside treatment and regular supportive treatment 1-4 times a year, depending on the skill of the patient and potential risk factors, can reduce the rate of periodontal damage progression in high-risk groups [
32,
33].
The Prophylaxis Concept places a high priority on cleaning in cole area and the cervical zone. To achieve this, it provides patients with special tools, as well as a theoretical background, to help patients achieve individualized and appropriate oral health. The Prophylaxis Concept philosophy is based on the reduction of bacteria growth on non-self-cleaning surfaces of the teeth, using techniques and tools adapted to the given task. Patients who have understood the paramount importance of maintaining oral hygiene and have received the necessary education and practice from dentists and dental hygienists trained for this purpose can maintain good oral health not only during the examination, but also in the long term with smaller FMBS and FMPS index, MMP-8 and BOB [
19].
In this study, the group of patients with subclinical symptoms in group A were examined as a separate group, as subjects had no clinical symptoms of gingivitis, although they cleaned their teeth with different methods. In this case, the traditional indeces (FMPS and FMBS) did not provide any differences at different appointments, but BOB was able to diagnose contrast at an early stage, showing a significant reduction at week 2. This means that at an early stage, when no clinical sypmtoms of gingivitis are visible, BOB can clinically detect the inflammatory process. This represents a new opportunity for early diagnosis in preventive dentistry. MMP-8 can also show similar results, but there were not enough patients in the study to see significant differences. For groups A and B, the results of t the four measurements suggested a different approach to dental prevention. BOB level in groups A, A1 and A2 significantly decreased at week 2 and remained low until week 12. A3 decreased continuously, but there were no differences between weeks 4 and 12. Due to the professional oral hygiene treatments, A4 values were decreased after the first appointment, but then stagnated. All these mean that the oral hygiene concepts of subgroups A1 and A2 lead to more effective oral hygiene results than in subgroups where interdental cleaning is not a daily habit. There is also a minimal improvement in subgroups A3 and A4 with common professional oral hygiene treatment, but BOB cannot decrease as much as in other subgroups due to the lack of daily interdental cleaning. In group B, there are different time and group effects. Subgroup B1 shows significant improvement. The values decrease sharply from the intitial appointment to week 2 and slowly towards weeks 4 and 12. This means that proper daily interdental cleaning leads rapidly to a non-inflammatory oral status at week 2. In subgroup B2, significant improvement is only observed at weeks 4 and 12. The values a week 2 decreased but not as much as in subgroup B1. This means that it is not only the use of interdental brushes that leads to a non-inflammatory oral status, but also the use of the right size of interdental brushes by a dental health care professional. In subgroup B4, there is a decrease in scores from the initial appointment to week 4, but scores increase again at week 12. This means that without interdental cleaning, only regular professional oral hygiene treatment will not maintain adequate inflammation-free oral hygiene.
In group A, subjects using interdental brushes had lower MMP-8 values at the initital appointment than subjects without proximal cleaning habits, and their MMP-8 levels significantly decreased after week 2 of follow-up. Subgroup A4 showed a decrease in levels from the first appointment to week 12, but only regular professional oral hygiene treatments without interdental cleaning led to an improvement. In group B, in patients with periodontitis, MMP-8 levels were shown to be much higher than in patients with gingivitis, and their values also decreased more when regular interdental cleaning was performed.
Overall, it can be said that patients who used electric or ultrasonic toothbrushes, despite their dental education, did not use interdental brushes regularly because they felt their mouths much cleaner than with normal tootbrushes and lost their motivation to spend time with interdental brushing. A comparison of BOB and MMP-8 with FMPS and FMBS in group A makes it evident that FMPS and FMBS indeces cannot show significant differences between the different oral hygiene habit groups during the 12-week period. All subgroups showed improvement at week 2. This implies that the involvement of patients in dental education and regular follow-up led to a reduction in dental plaque and bleeding.
In group B, FMPS and FMBS levels decreased significantly in subgroup B1 and remained there for 12 weeks. This led to a fast and effective oral hygiene treatment that prepared patients with periodontitis for successful periodontal therapy. There were no significant changes in subgroups B3 and B4 because the main improvement in these subgroups was only due to regular professional cleaning during the examinations.
5. Conclusions
During the study, all patients consistently attended the examinations and all groups diligently used oral hygiene devices as expected. The results indicated a significant improvement in the oral hygiene of patients in the Prophylaxis Concept groups, leading to sustainable oral health without inflammation. This improvement was confirmed by the elevated values of BOB, MMP-8, FMBS and FMPS. The use of these values not only reduced the time for conservative therapy, but also facilitated short- and long-term follow-up while maintaining patient motivation. The study suggests that, in addition to FMPS, FMBS, MMP-8 and BOB may serve as an effective early diagnostic tools to assess oral hygiene and periodontal status. Due to their chair-side nature, these measurements can be easily applied in a clinical setting, providing patients with new diagnostic options and potentially reducing the burden of periodontitis. The objective, diagnostic value of BOB and MMP-8 from subclinical symptoms to severe periodontitis may offer a new perspective in the early detection of periodontitis.
Author Contributions
Conceptualization, O.N. and F.S.; methodology, O.N., F.S.; validation, O.N and F.S..; formal analysis, O.N., F.S., M.O., and G.S.; investigation, O.N. and F.S.; resources, O.N and F.S.; writing—original draft preparation, F.S.; writing—review and editing, O.N. and G.S.; writing—final draft, O.N., F.S. and G.S.; supervision, O.N., E.M, M.O.; project administration, F.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Ethics Approval and Constent to Participate
The study was approved by the Regional and Institutional Committee of Science and Research Ethics and the Hungarian Office of Health Authorization and Administrative Procedures, and was conducted in accordance with the Declaration of Helsinki. (No.: ETT-TUKEB IV/9854-1/2021/EKU) All patients provided written informed consent prior to participation.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets generated and analyzed in this study are not publicly available due to the impossibility of obtaining data anonymously. Patient anonymity cannot be preserved at the appropriate measurement investigator, but data can be obtained from the corresponding author upon reasonable request.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
List of Abbreviations
| MMP-8 |
matrix-metalloproteinase-8 |
| BOB |
Bleeding on Brushing |
| FMPS |
Full-mouth plaque score |
| FMBS |
Full-mouth bleeding score |
| PMN-leukocytes |
Polymorphonuclear-leukocytes |
| ELISA |
enzyme-linked immunosorbent assay |
| PPD |
Probing pocket depth |
| ATS |
ANOVA-type statistic |
| DMFT-index |
Decayed, Missing, Filled teeth - index |
References
- Loe H, Theilade E, Jensen SB. Experimental Gingivitis in Man. J Periodontol (1930). 1965;36(3):177-87. [CrossRef]
- Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent RL, Jr. Microbial complexes in subgingival plaque. J Clin Periodontol. 1998;25(2):134-44. [CrossRef]
- Slots, J. Periodontology: past, present, perspectives. Periodontol 2000. 2013;62(1):7-19. [CrossRef]
- Loe H, Anerud A, Boysen H, Morrison E. Natural history of periodontal disease in man. Rapid, moderate and no loss of attachment in Sri Lankan laborers 14 to 46 years of age. J Clin Periodontol. 1986;13(5):431-45. [CrossRef]
- Bartold PM, Van Dyke TE. Periodontitis: a host-mediated disruption of microbial homeostasis. Unlearning learned concepts. Periodontol 2000. 2013;62(1):203-17. [CrossRef]
- Salazar MG, Jehmlich N, Murr A, Dhople VM, Holtfreter B, Hammer E, et al. Identification of periodontitis associated changes in the proteome of whole human saliva by mass spectrometric analysis. J Clin Periodontol. 2013;40(9):825-32. [CrossRef]
- Leppilahti JM, Ahonen MM, Hernandez M, Munjal S, Netuschil L, Uitto VJ, et al. Oral rinse MMP-8 point-of-care immuno test identifies patients with strong periodontal inflammatory burden. Oral Dis. 2011;17(1):115-22. [CrossRef]
- Sorsa T, Suomalainen K, Uitto VJ. The role of gingival crevicular fluid and salivary interstitial collagenases in human periodontal diseases. Arch Oral Biol. 1990;35 Suppl:193S-6S. [CrossRef]
- Krause PJ, Ingardia CJ, Pontius LT, Malech HL, LoBello TM, Maderazo EG. Host defense during pregnancy: neutrophil chemotaxis and adherence. Am J Obstet Gynecol. 1987;157(2):274-80. [CrossRef]
- Sorsa T, Tjaderhane L, Salo T. Matrix metalloproteinases (MMPs) in oral diseases. Oral Dis. 2004;10(6):311-8. [CrossRef]
- Chen HY, Cox SW, Eley BM, Mantyla P, Ronka H, Sorsa T. Matrix metalloproteinase-8 levels and elastase activities in gingival crevicular fluid from chronic adult periodontitis patients. J Clin Periodontol. 2000;27(5):366-9. [CrossRef]
- Sorsa T, Hernandez M, Leppilahti J, Munjal S, Netuschil L, Mantyla P. Detection of gingival crevicular fluid MMP-8 levels with different laboratory and chair-side methods. Oral Dis. 2010;16(1):39-45. [CrossRef]
- Sorsa T, Mantyla P, Ronka H, Kallio P, Kallis GB, Lundqvist C, et al. Scientific basis of a matrix metalloproteinase-8 specific chair-side test for monitoring periodontal and peri-implant health and disease. Ann N Y Acad Sci. 1999;878(1):130-40. [CrossRef]
- Sorsa T, Gursoy UK, Nwhator S, Hernandez M, Tervahartiala T, Leppilahti J, et al. Analysis of matrix metalloproteinases, especially MMP-8, in gingival creviclular fluid, mouthrinse and saliva for monitoring periodontal diseases. Periodontol 2000. 2016;70(1):142-63. [CrossRef]
- Rathnayake N, Gieselmann DR, Heikkinen AM, Tervahartiala T, Sorsa T. Salivary Diagnostics-Point-of-Care diagnostics of MMP-8 in dentistry and medicine. Diagnostics (Basel). 2017;7(1):7. [CrossRef]
- Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Clin Periodontol. 2018;45 Suppl 20(S20):S149-S61. [CrossRef]
- Al-Majid A, Alassiri S, Rathnayake N, Tervahartiala T, Gieselmann DR, Sorsa T. Matrix Metalloproteinase-8 as an Inflammatory and Prevention Biomarker in Periodontal and Peri-Implant Diseases. Int J Dent. 2018;2018:7891323. [CrossRef]
- Petersen PE, Baez RJ, World Health Organization. Oral health surveys: basic methods. 5th ed. [E-book]. Geneva: World Health Organization; 2013. Available online: https://iris.who.int/handle/10665/97035.
- Rosenauer T, Wagenschwanz C, Kuhn M, Kensche A, Stiehl S, Hannig C. The Bleeding on Brushing Index: a novel index in preventive dentistry. Int Dent J. 2017;67(5):299-307. [CrossRef]
- Raisanen IT, Sorsa T, van der Schoor GJ, Tervahartiala T, van der Schoor P, Gieselmann DR, et al. Active Matrix Metalloproteinase-8 Point-of-Care (PoC)/Chairside Mouthrinse Test vs. Bleeding on Probing in Diagnosing Subclinical Periodontitis in Adolescents. Diagnostics (Basel). 2019;9(1):34. [CrossRef]
- Hernandez M, Baeza M, Raisanen IT, Contreras J, Tervahartiala T, Chaparro A, et al. Active MMP-8 Quantitative Test as an Adjunctive Tool for Early Diagnosis of Periodontitis. Diagnostics (Basel). 2021;11(8):1503. [CrossRef]
- Newman MG, Takei HH, Klokkevold PR, Carranza FA, Elangovan S. Newman and Carranza’s clinical periodontology. 13th ed. Philadelphia, PA: Elsevier; 2018.
- Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. Lancet. 2005;366(9499):1809-20. [CrossRef]
- Zuur AF, Ieno EN, Walker N, Saveliev AA, Smith GM. Mixed effects models and extensions in ecology with R: Springer New York; 2009.
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing [dataset]. Vienna, Austria: The R Foundation; 2024 [cited 2024 March 8]. Available online: https://www.R-project.org/.
- Brooks ME, Kristensen K, van Benthem KJ, Magnusson A, Berg CW, Nielsen A, et al. glmmTMB Balances Speed and Flexibility Among Packages for Zero-inflated Generalized Linear Mixed Modeling. R J. 2017;9(2):378-400. [CrossRef]
- Faraway, J.J. Extending the Linear Model with R. 2nd ed. New York: Chapman and Hall/CRC; 2016 2016/03/23.
- Hartig F. _DHARMa: Residual Diagnostics for Hierarchical (Multi-Level / Mixd) Regression Models_. R package version 0.4.6 [dataset]. Free Software Foundation, Inc.; 2022 [updated 2022 Sept 8; cited 2024 March 8]. Available online: https://CRAN.R-project.org/package=DHARMa.
- Smith C, Warren M. GLMs in R for Ecology. 2nd ed. [s. l.]: [s. n.]; 2023.
- Lenth RV. _emmeans: Estimated Marginal Means, aka Least-Squares Means_. R package version 1.10.0 [dataset]. Free Software Foundation, Inc.; 2024 [cited 2024 March 8]. Available online: https://CRAN.R-project.org/package=emmeans.
- Lang NP, Cumming BR, Loe H. Toothbrushing frequency as it relates to plaque development and gingival health. J Periodontol. 1973;44(7):396-405. [CrossRef]
- Armitage, G.C. The complete periodontal examination. Periodontol 2000. 2004;34(1):22-33. [CrossRef]
- Mombelli A, Gusberti FA, van Oosten MA, Lang NP. Gingival health and gingivitis development during puberty. A 4-year longitudinal study. J Clin Periodontol. 1989;16(7):451-6. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).