1. Introduction
Pulmonary Hypertension affects 1% of the population and up to 10% of people over the age of 65. It is an independent mortality factor, with patients suffering from severe pulmonary hypertension having an annual mortality rate exceeding 30%, and a five-year mortality rate over 60% [
1]. Unfortunately, the current definition of PH is hemodynamic, characterized by a mean pulmonary arterial pressure (PAP) of over 20 mmHg at rest, measured via right heart catheterization. This test is often not feasible in everyday practice, and European guidelines recommend an initial evaluation using echocardiography to estimate the Probability of Pulmonary Hypertension (PHP) [
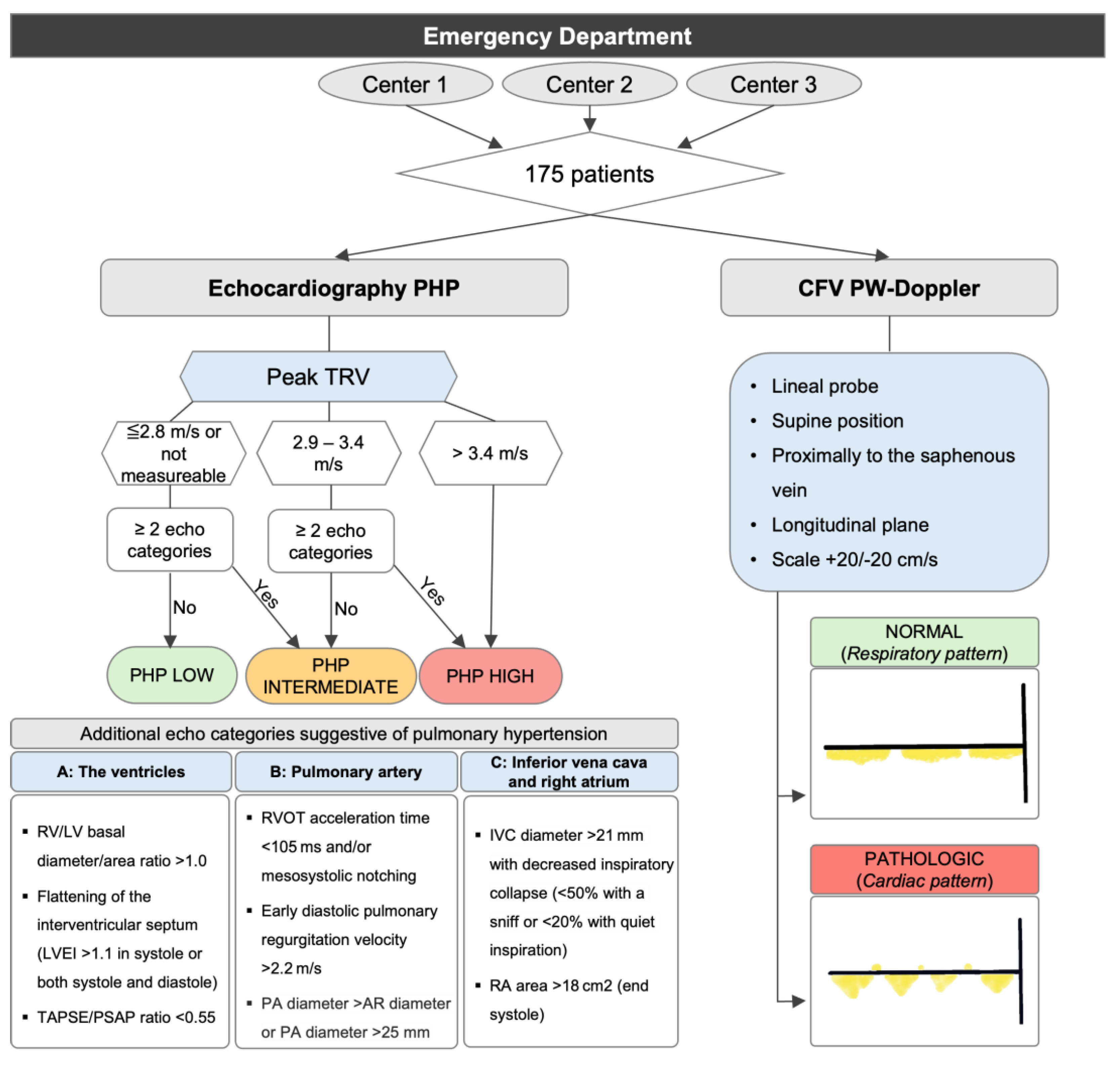
2]. This algorithm classifies PHP as high, intermediate, or low, based on tricuspid regurgitation velocity and using three categories, which incorporate eight echocardiographic parameters: the right-to-left ventricular basal diameter ratio greater than 1, septal flattening (left ventricular eccentricity index greater than 1.1 in systole and/or diastole), right ventricular outflow acceleration time of less than 105 ms and/or mesosystolic notching, pulmonary artery diameter greater than the aortic root diameter or over 25 mm, early pulmonary regurgitation maximum velocity greater than 2.2 m/s, TAPSE/PASP less than 0.55, IVC diameter over 21 mm with decreased inspiratory collapse, and right atrial area over 18 cm
2.
The CFV is an accessible vein that can be assessed with ultrasound, with a short learning curve. There are between zero and two valves between the right atrium and the CFV, thus the pressure in the right atrium can be transmitted and assessed through the CFV. Ultrasound evaluation of patients in the Emergency Department can be challenging, and sometimes there is not enough experience in echocardiography, proper imaging windows, or even equipment for an adequate evaluation of the PHP. However, we face conditions such as heart failure or pulmonary thromboembolism where detecting significant pulmonary hypertension can be crucial and change clinical practice. This article evaluates the presence of a cardiac pattern in the CFV for detecting a high PHP in patients presenting to the emergency department for various reasons.
2. Materials and Methods
A total of 175 patients who attended the Emergency Department for any reason and were over 18 years old were recruited. The only exclusion criterion was refusal to participate in the study. The study was approved by the local ethics committee and adhered to the principles established in the Helsinki Declaration.
This was a prospective, multicenter observational study conducted in three hospitals. Due to the limited existing evidence regarding the assessment of CFV by PW-Doppler, the study was considered a pilot study, and a calculation of the necessary number of patients was not performed as such. A complete echocardiography was performed, which included all the parameters mentioned for calculating PHP (
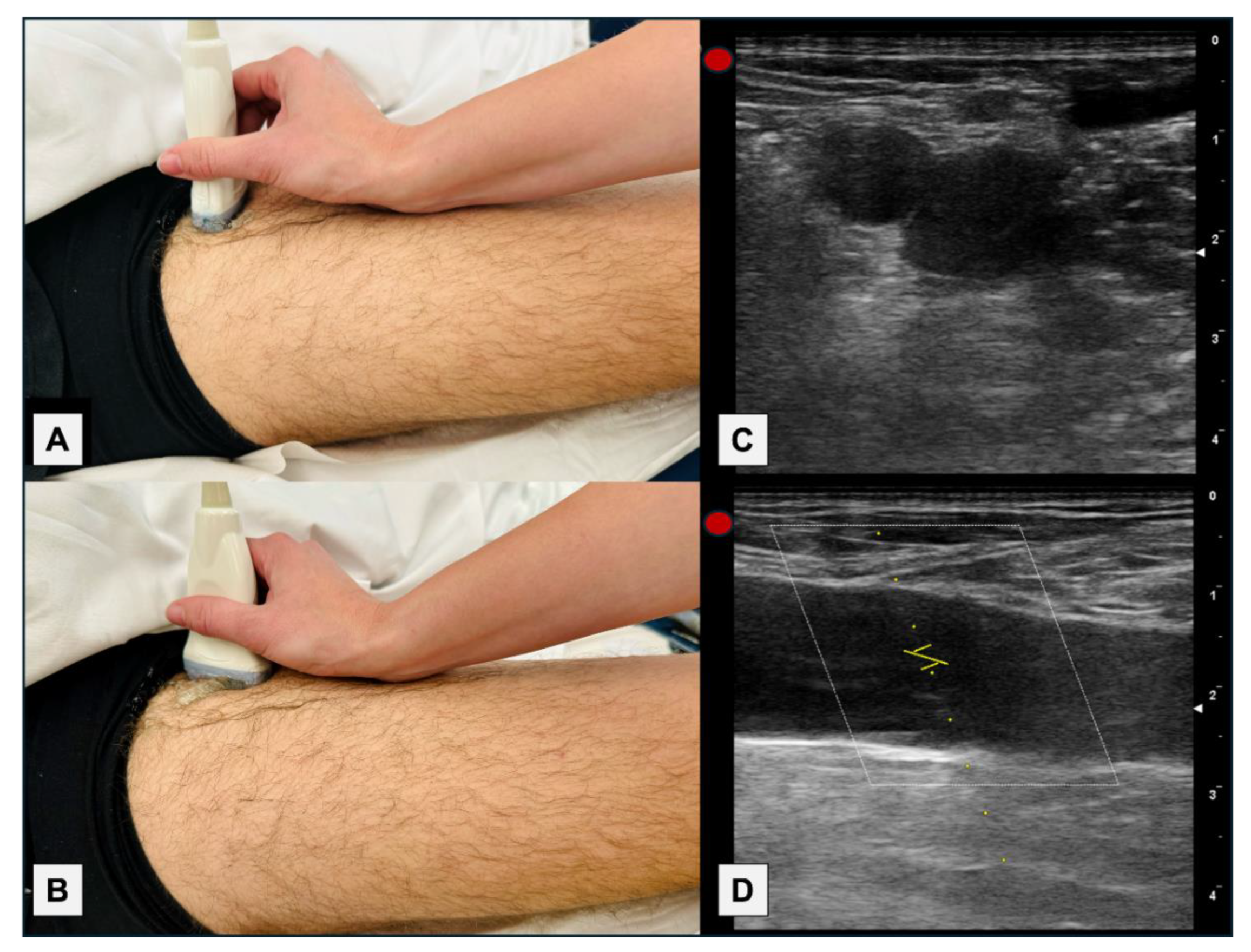
Figure 1). The morphology of the PW-Doppler of the CFV was assessed using a linear probe, in a supine position, proximally to the saphenous vein, after confirming the absence of deep vein thrombosis, in a longitudinal plane, and adjusting the scale to +20/-20 cm/s (
Figure 1 and
Figure 2).
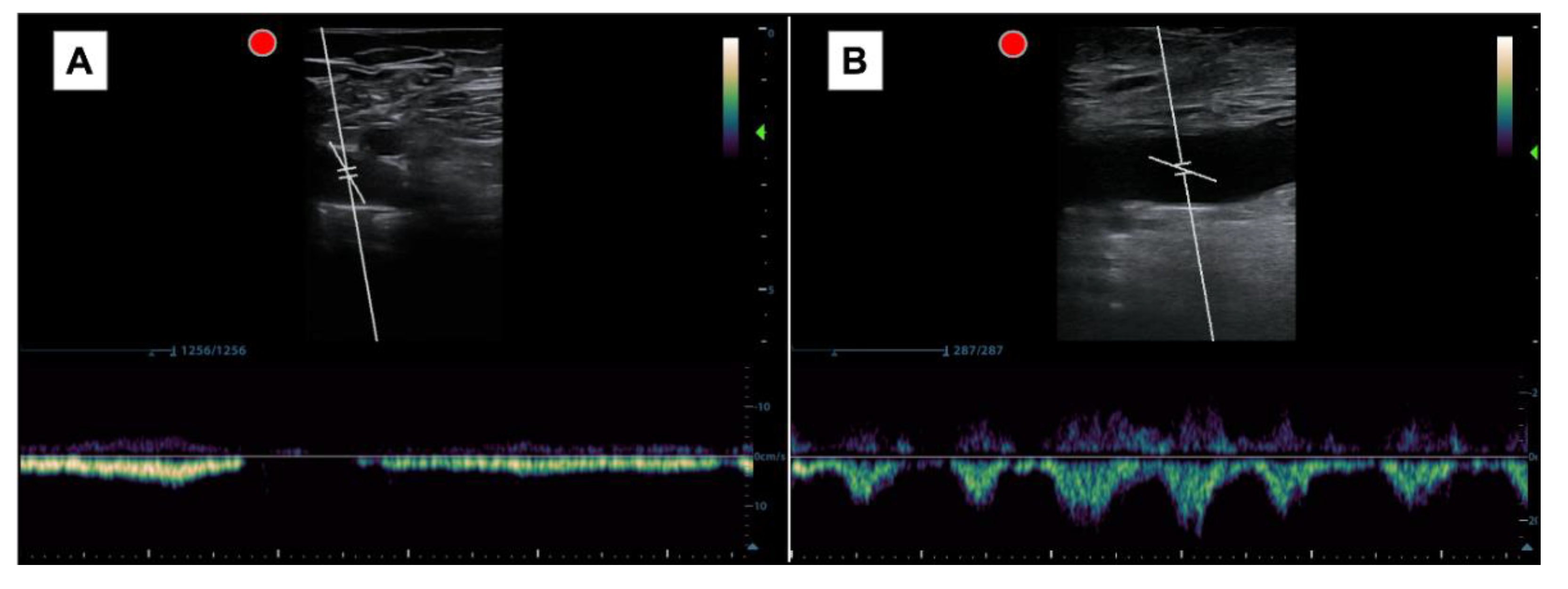
The pattern obtained was interpreted as either a respiratory (normal) or cardiac (pathological) pattern. The cardiac pattern is recognized when the systolic and diastolic waves are clearly identified, regardless of whether there is retrograde flow or no flow during spontaneous inspiration. The respiratory pattern, on the other hand, is defined when the systolic and diastolic waves are not adequately distinguished and disappear with inspiration (
Figure 3).
A Mindray M9 (Mindray Medical Spain, Madrid, Spain) and GE VENUE (GE Healthcare, Madrid, Spain) ultrasound equipments were used. Image acquisition was performed by leading physicians in point-of-care ultrasound units with extensive experience. PHP calculation was carried out using Excel formulas to avoid errors.
Statistical analysis was performed using SPSS 26.0 (IBM, Chicago, IL, USA). It was verified that the variables that did not follow a normal distribution using the Kolmogorov-Smirnov test. Qualitative results are expressed as percentages. Quantitative variables are expressed as Mean (M) and Standard Deviation (SD). A comparison of the proportions of ultrasound variables was made using Bonferroni adjustment and a significance level (p) of 0.05. Correlation studies were conducted using the Chi-square test, and subsequently, the performance of the variables for the diagnosis of PHP was studied using the ROC curve. Sensitivity (Sn), specificity (Sp), positive predictive value (PPV), and negative predictive value (NPV) of the eight variables of the PHP algorithm and the presence of the cardiac pattern at the level of the CFV were analyzed, as well as the Odds Ratios (OR) with their 95% confidence intervals (CI95%) and relative risks (RR).
3. Results
The average age was 61 years (SD 20.5) and 46.3% were women. Forty-eight percent had acute heart failure, and the rest had other pathologies (
Figure 4). A total of 33.1% had prior heart disease, 6% had sleep apnea-hypopnea syndrome, 12% had lung disease, and another 12% were obese. Notably, 23% had high Pulmonary Hypertension Probability (PHP), 34.5% intermediate, and 61% low. The mean pulmonary artery systolic pressure (PASP) in patients with high PHP was 52.3 (SD 9.7) and in the intermediate-low group was 25.1 (SD 7.3). The distribution of ultrasound parameters according to the presence of high PHP is shown in
Table 1. A Bonferroni adjustment confirmed differences in the distribution of the nine ultrasound variables in patients with and without high PHP, with a significance level below 0.05.
The correlation study using the Chi-square test showed that all parameters of the PHP algorithm were significant (
Table 2), with the presence of a cardiac pattern in the CFV having the highest contingency coefficient (0.59, p < 0.001).
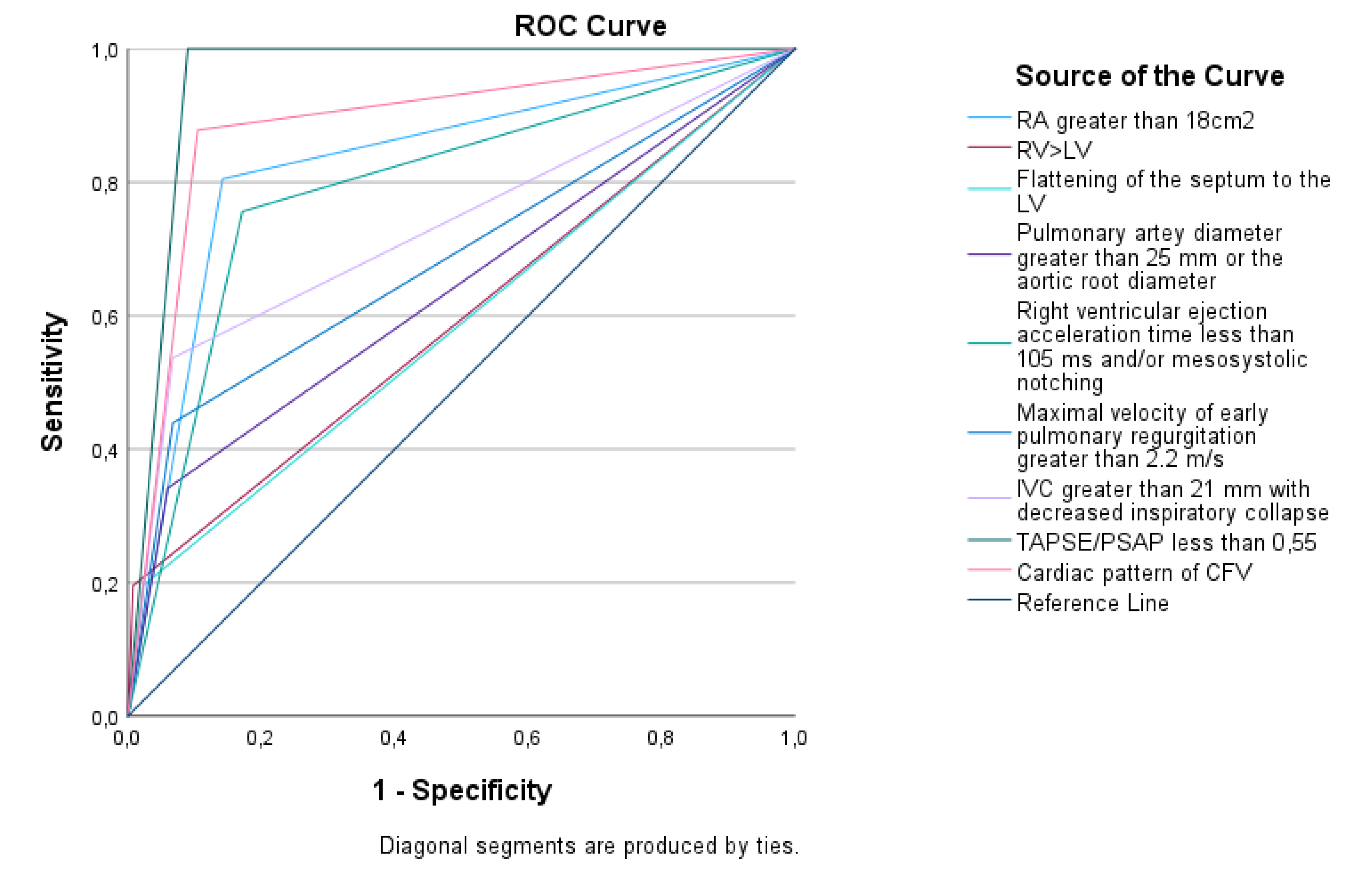
The ROC curve (
Figure 5,
Table 3) indicates that the parameters with the highest area under the curve (AUC) are dilated right atrium (RA), the cardiac pattern of the CFV, and TAPSE/PASP < 0.55 (AUCs of 0.83, 0.89, and 0.96, respectively).
Sensitivity, specificity, positive predictive value, negative predictive value, odds ratios with 95% confidence intervals, and relative risks are detailed in Table 5. The presence of a femoral cardiac pattern has an RR of 18 and increases the probability of having high PHP by 61 times (CI95% 21-183). Additionally, it has a high specificity (96%), therefore making it less likely for the patient to have high PHP (≤ 4%). This parameter correctly detects 72% of patients with high PHP and has a PPV of 88% and an NPV of 90%, indicating that its absence strongly suggests the absence of high PHP.
4. Discussion
The assessment of PHP is complex and may not be feasible for a physician who is not an expert in echocardiography. However, the CFV is an accessible vein, easy to scan, and holds promising potential.
It’s important to understand that between the RA and the CFV, there are no connivent valves in 21% of people, one in 71%, two in 7%, and three in 1% [
3]. Thus, whatever occurs in the RA will directly transmit to the CFV. Under normal conditions, during inspiration, the diaphragm moves downward, decreasing intrathoracic pressure, which generates negative pressure in the right cavities and a suction effect from the venous system. At the end of this suction effect, we even stop seeing flow in the PW-Doppler of the CFV. However, if the pressure in the right atrium increases, the suction effect disappears, and the transmission of systolic and diastolic waves to the CFV occurs.
Previously, the relationship between pulsatility and the pressures of the right atrium had been described by Abu-Yousef [
4] and Krahenbuhl et al. The largest study conducted involved only 46 patients undergoing right catheterization, observing that the appearance of pulsatile flow is an early sign of elevated pressure in the right atrium (sensitivity of 92%) [
5]. Alimoğlu et al. assessed the flow by PW-Doppler in the CFV in 30 patients with right heart failure who underwent right catheterization and observed that patients with increased pressure in the RA had a significantly higher pulsatility index [
6]. Denault et al, based on the description of two cases and emphasizing the direct connection between the RA and the CFV, even proposed an action algorithm in the patient with shock that subsequently has not been validated [
7].
When developing the study protocol, we faced difficulties in choosing how to conduct the examination. The first thing we considered was what we really wanted to assess. We must consider that, being a relatively new window, there was a lot of variability in the variables studied at the level of the PW-Doppler flow in the CFV. According to the authors, they valued: pulsatility, retrograde flow (with different speeds as cutoff points), respiratory phasicity, the pulsatility index, maximum or minimum speeds, or cardiac modulation. To choose the most optimal parameter, we took into account the interesting findings of Taute et al., who assessed the presence of cardiac modulation (which is equivalent to the cardiac pattern or pulsatility without respiratory phasicity) in 47 patients with acute pulmonary embolism, and observed that all patients with a right cardiac score of ≥1.75 had cardiac modulation (Sn 96%, Sp 88%) [
8]; and our own preliminary findings; in which we observed that the pulsatile pattern in the PW-Doppler in the CFV reasonably detected elevated PHP (AUC 0.8, Sn 95%, Sp 64%, PPV 84%, NPV 84%) in 74 patients with heart failure [
9]. In our previous study, we studied the role of pulsatility, retrograde flow (which may be present if the patient has venous insufficiency), and respiratory phasicity to establish which were the best variables. Bringing all this data together, we decided to distinguish only two patterns. The cardiac pattern, as one in which the cardiac waves are easily distinguished and in which breathing does not generate the absence of flow, and the respiratory pattern, in which the waves are not distinguished and with breathing, the flow disappears (
Figure 3).
Another issue we considered was whether to perform measurements in the longitudinal or transverse plane. Although the transverse plane would have been simpler, and we probably would have obtained the same results (considering that the scale should be increased, as the speeds are lower), we chose to evaluate the longitudinal plane of the CFV, because all studies conducted to date used that plane, including ours. A technical issue is that when evaluated in the longitudinal plane and with the flow perpendicular to the PW-Doppler insonation, it is necessary to perform an angle adjustment for a more adequate evaluation (
Figure 3). A specific study comparing the transverse and longitudinal planes would be needed to establish their equivalence and further increase the simplicity and speed of the examination.
Other technical considerations to consider are to rule out the presence of deep venous thrombosis through compression, and the supine position, as it can affect the pattern of the PW-Doppler by compressing the own abdomen compressing the CFV in a seated position, or by increasing the return if the legs are elevated. We must not forget to adjust the scale to +20/-20 cm/s, because if not, we might not distinguish the cardiac waves.
With the previous experience gained and the methodology discussed, we decided to conduct a broader study that would increase the assessment of different pathologies, in a way that closely approximates real-world environments. Although it is a pilot study, all parameters have reached statistical significance, which suggests that the necessary number of patients has been reached. The presence of the cardiac pattern in the CFV consolidates with the results provided as a diagnostic method for elevated PHP, regardless of the reason for consultation. Looking at the results of
Table 3, it is understandable that clinical practice guidelines integrate an algorithm with so many parameters to assign a probability. And it is that all ultrasound variables are acceptable diagnostic tools, but none is perfect. Based on the results obtained, the assessment by PW-Doppler of the CFV could be included in the algorithm for the calculation of the PHP. Certainly, in a challenging environment such as the Emergency Department, or in the hands of those with little experience in echocardiography; with the results of our study, we can say that the absence of a cardiac pattern at the level of the PW-Doppler of the CFV reasonably rules out the presence of significant pulmonary hypertension with a probability of 90%, and if we find a cardiac pattern, there will only be a 4% chance of false positives (Sp 96%) and we will have an 88% chance of significant pulmonary hypertension. Our results align with those previously obtained [
4,
5,
6,
8], but are probably the most relevant to date, as they cover different pathologies and involve a larger number of patients. These results turn this new diagnostic tool into a new parameter to consider in the calculation of PHP. It would be interesting to perform external validation in a different patient cohort in the future.
As a limitation, since the ultrasound evaluations were performed by experts in echocardiography, it may be necessary to evaluate its application in laypeople. Additionally, it should be noted that, although not applicable to real life, the gold standard would have been right catheterization; however, this limitation has been overcome by using the calculation of the probability of pulmonary hypertension as the target variable.
5. Conclusions
The cardiac pattern of the CFV is an effective indicator for detecting high PHP, allowing this condition to be ruled out with a high degree of certainty when absent. This finding has the potential to change clinical practice in the diagnosis and management of PH in emergency settings and other areas.
Author Contributions
M.TA designed, recruited, analyzed the database, and wrote the article. P.BR recruited patients. O.LZ and D.L collaborated in writing and designing the article. R.SD, A.RM, A.MM, B.GM, J.HN and JG.SC reviewed and edited the article. L.CD, T.VV, Y.TC and G.GC coordinated and reviewed the study.
Funding
This research did not receive any specific grant from public, commercial or not-for-profit funding agencies.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Hospital Universitario Puerta de Hierro (protocol code MIR/HPDH_2021_02 with date of approval 13/07/2021)
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the person to publish this paper” if applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to national legal standards and laws.
Acknowledgments
To my family, for putting up with me. To my friends, for loving me. To my colleagues, for helping me. To my teachers, for the head slaps.
Conflicts of Interest
The authors declare that they have no competing interests.
References
- Hoeper, M.M.; Humbert, M.; Souza, R.; Idrees, M.; Kawut, S. M.; Sliwa-Hahnle, K.; Jing, Z. C.; Gibbs, J. S. A global view of pulmonary hypertension. Lancet Respir Med. 2016, 4, 306–322. [Google Scholar] [CrossRef] [PubMed]
- Humbert, M.; Kovacs, G.; Hoeper, M. M.; Badagliacca, R.; Berger, R. M. F.; Brida, M.; Carlsen, J.; Coats, A. J. S.; Escribano-Subias, P.; Ferrari, P.; et al. ESC/ERS Scientific Document Group. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur.Heart J. 2022, 43, 3618–3731. [Google Scholar] [CrossRef] [PubMed]
- Basmajian, J.V. The distribution of valves in the femoral, external iliac, and common iliac veins and their relationship to varicose veins. Surg Gynecol Obstet. 1952, 25, 537–542. [Google Scholar]
- Abu-Yousef, M.M.; Kakish, M.E.; Mufid, M. Pulsatile venous Dopplerflow in lower limbs: highly indicative of elevated right atriumpressure. Am J Roentgenol. 1996, 167, 977–80. [Google Scholar] [CrossRef] [PubMed]
- Krahenbuhl, B.; Restellini, A.; Frangos, A. Peripheral venous pulsatility detected by Doppler method for diagnosis of right heartfailure. Cardiology. 1984, 71, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Alimoğlu, E.; Erden, A.; Gürsel, K.; Olçer, T. Correlation of right atrial pressure and blood flow velocities in the common femoral vein obtained by duplex Doppler sonography. J Clin Ultrasound. 2001, 29, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Denault, A.Y.; Aldred, M.P.; Hammoud, A.; Zeng, Y.H.; Beaubien-Souligny, W.; Couture, E.J.; Jarry, S.; Gebhard, C.E.; Langevin, S.; Lamarche, Y.; et al. Doppler Interrogation of the Femoral Vein in the Critically Ill Patient: The Fastest Potential Acoustic Window to Diagnose Right Ventricular Dysfunction? Crit. care explor. 2020, 2, e0209. [Google Scholar] [CrossRef] [PubMed]
- Taute, B.M.; Schmidt, H.; Bach, A.G.; Fischer, R.; Tran, C.L.; Amoury, M.; Melnyk, H. Spectral Doppler Waveform Analysis of Common Femoral Veins for the Detection of Right Ventricular Dysfunction in Acute Pulmonary Embolism. J Cardiovasc Dis Diagn. 2015, 3, 1–5. [Google Scholar] [CrossRef]
- Torres-Arrese, M.; Mata-Martínez, A.; Luordo-Tedesco, D.; Casasola-Sánchez, G.; Montero-Hernández, E.; Cobo-Marcos, M; Tejeda-Jurado, F. ; Berrocal-Espinosa, P.; Martínez-Ballester, J.F.; Tung-Chen, Y. Role of the femoral vein doppler in acute heart failure patients: results from a prospective multicentric study. Rev Clin Esp. 2023, 23, 359–365. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).