Submitted:
31 May 2024
Posted:
04 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patient Selection
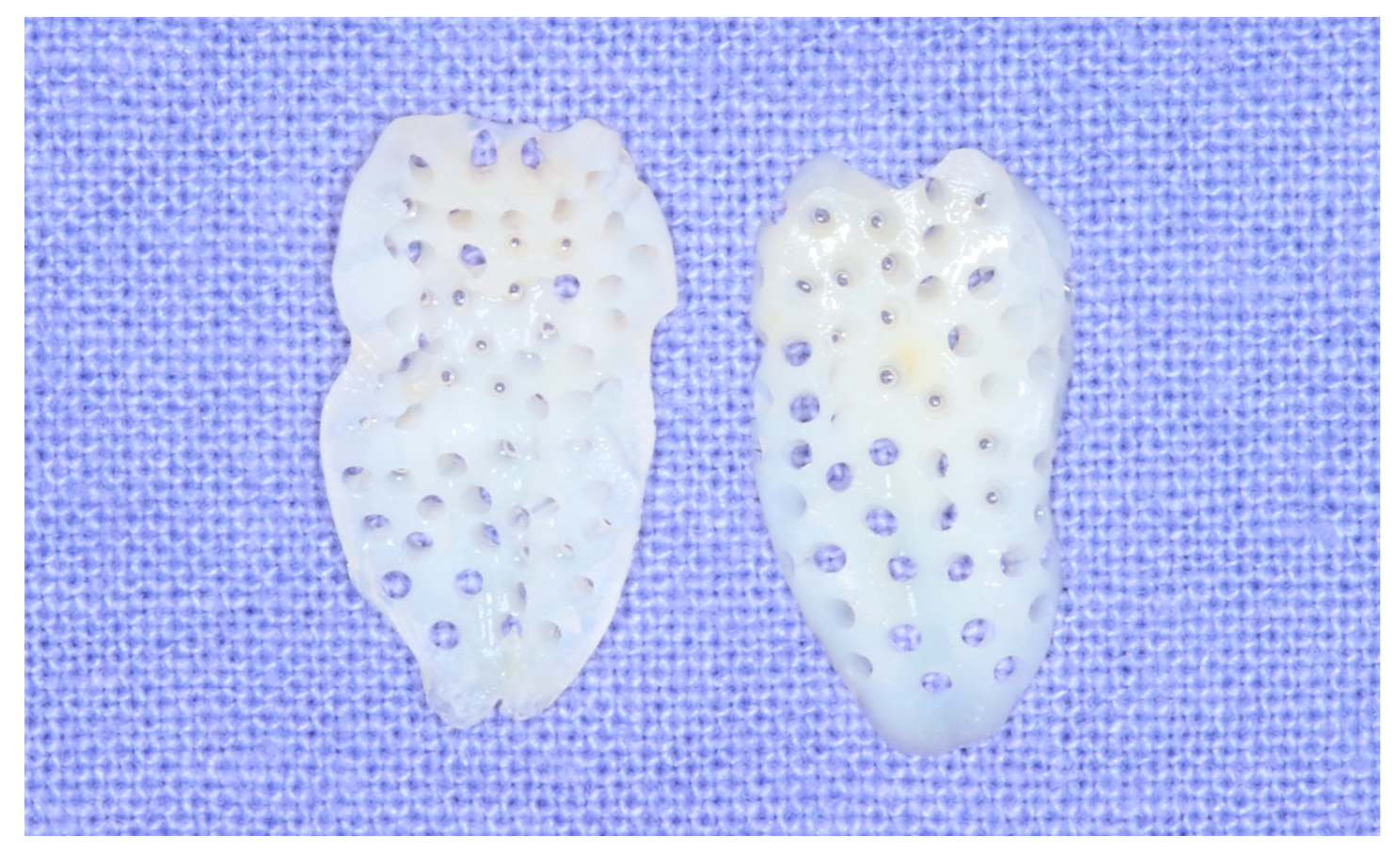
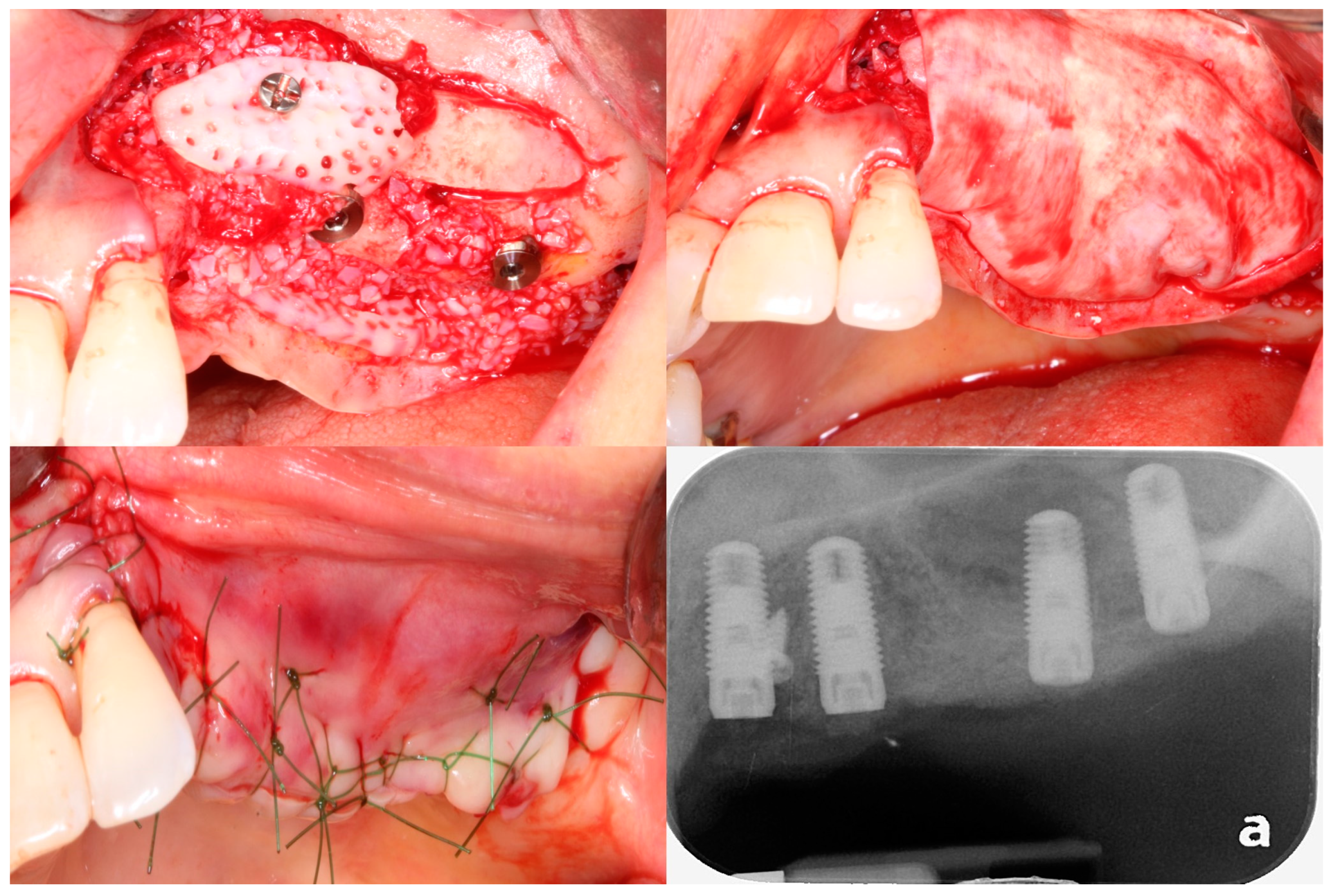
2.2. Preparation of Osteoinductive Tooth Block Bone
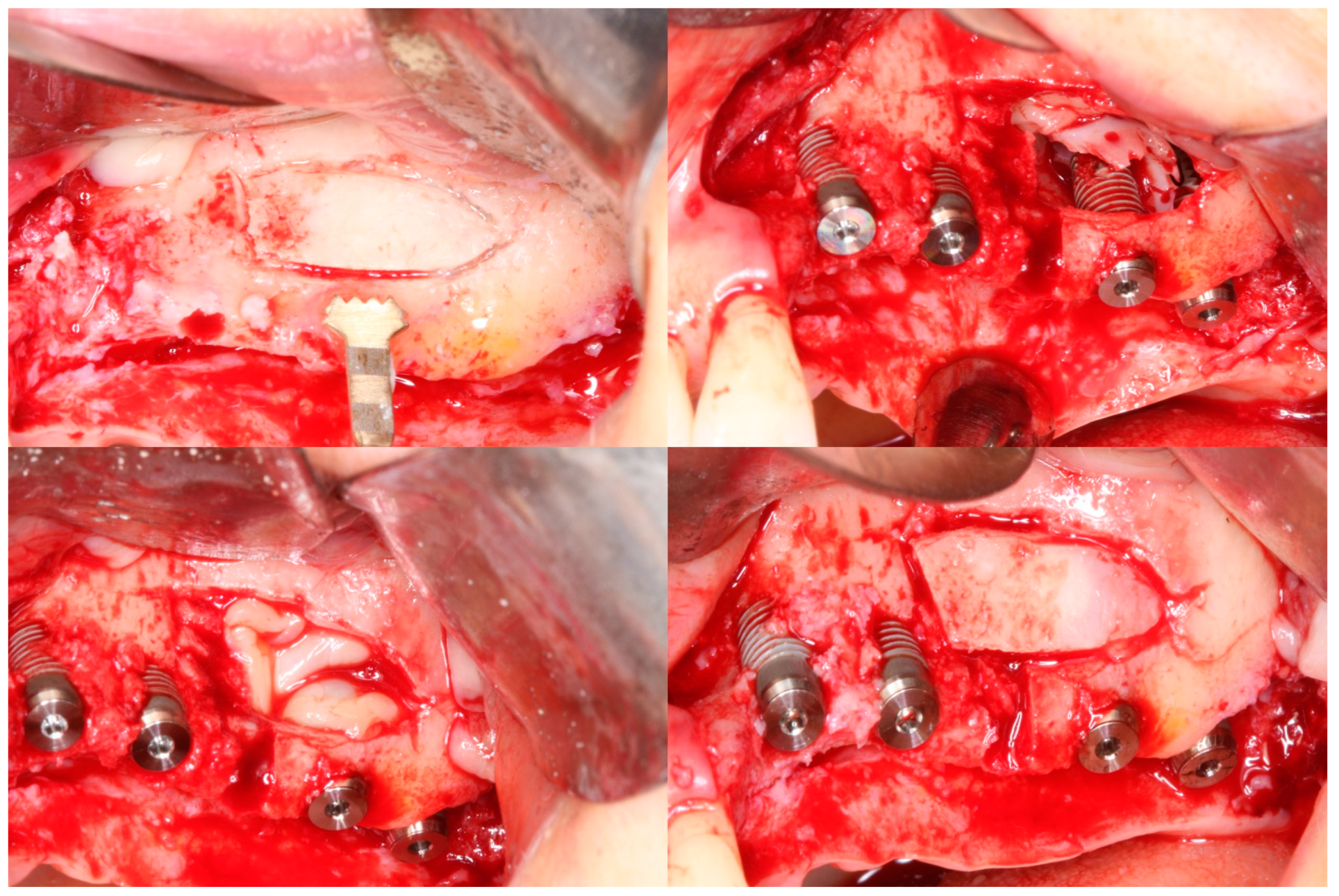
2.3. Surgical Protocol
3. Results
3.1. Clinical Results
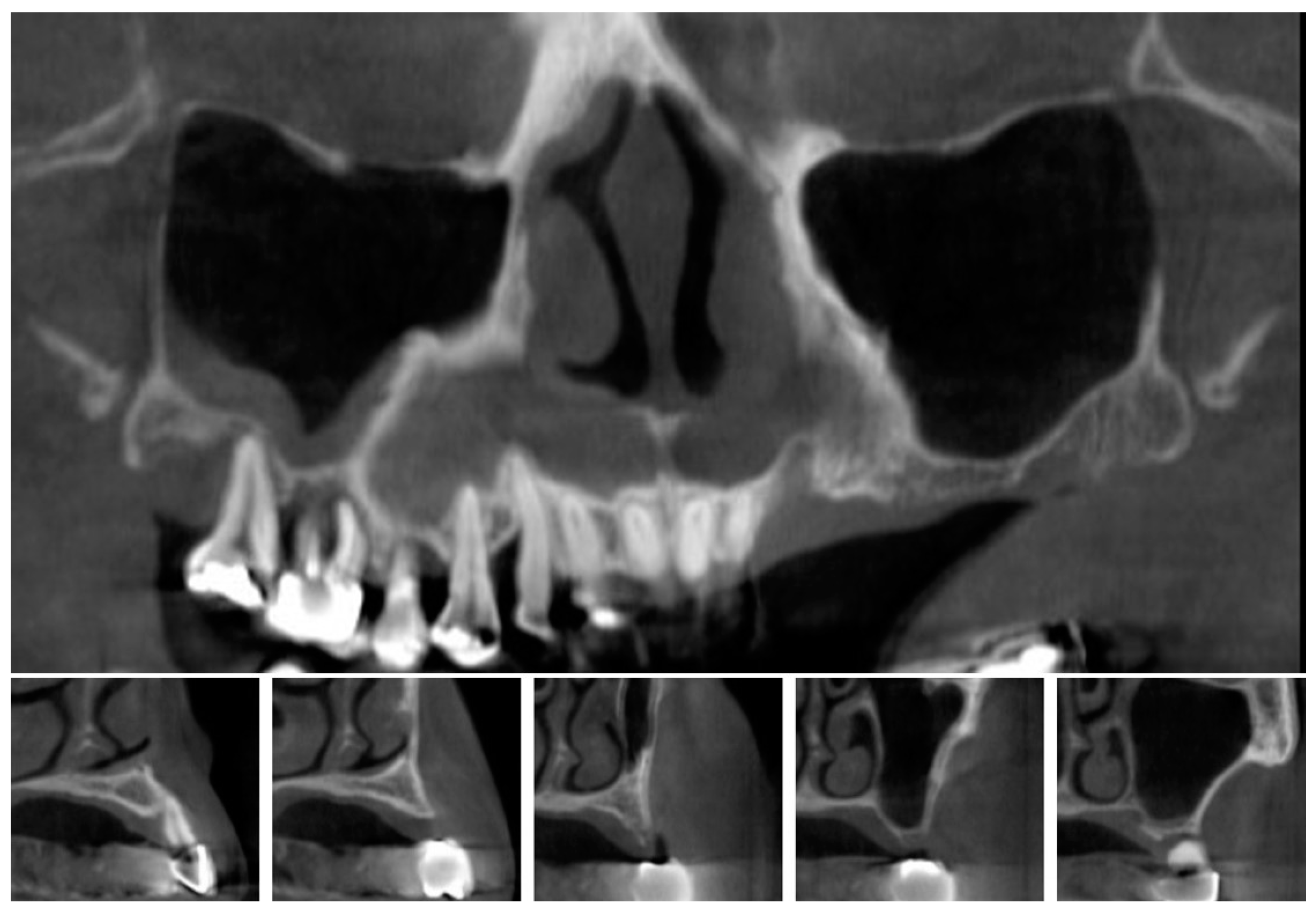
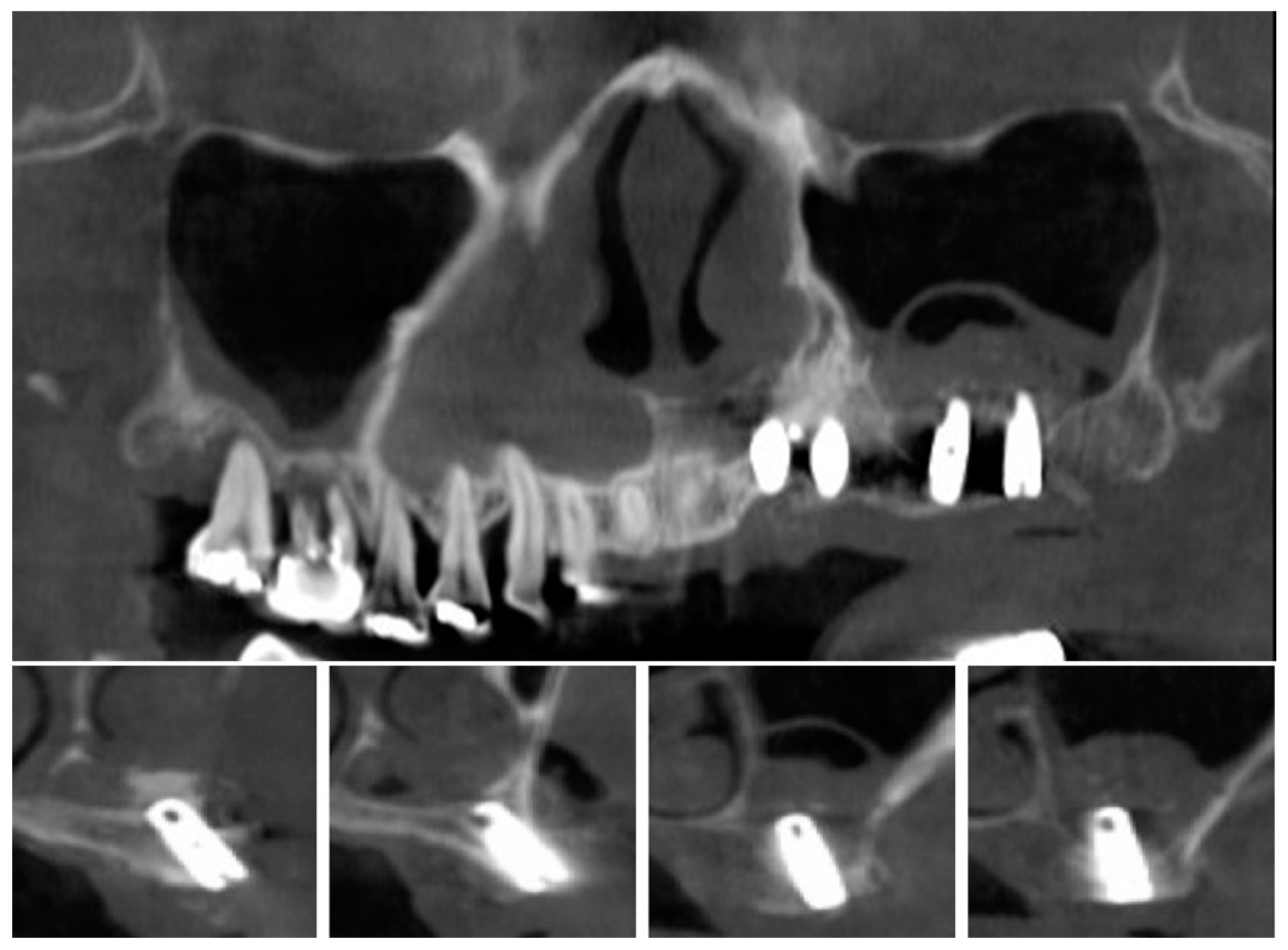
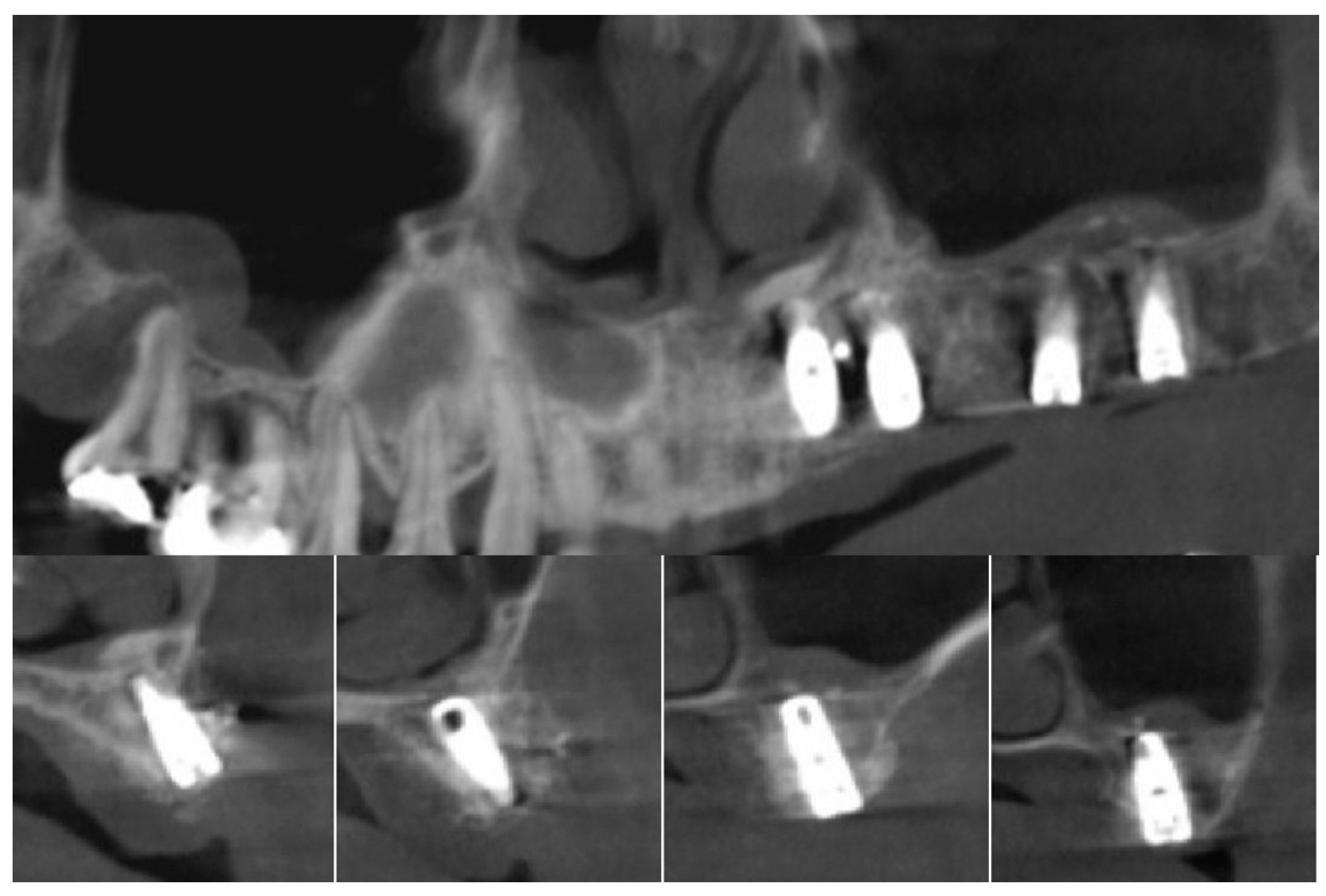
3.2. Radiographic Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Le Guéhennec L, Soueidan A, Layrolle P, Amouriq Y. Surface treatments of titanium dental implants for rapid osseointegration. Dent Mater J. 2007;23:844-854.
- Misch CE. Maxillary sinus augmentation for endosteal implants: organized alternative treatment plans. Int J Oral Implantol. 1987;4:49–58.
- Smiler DG, Johnson PW, Lozada JL, Misch C, Rosenlicht JL, Tatum OH, Wagner JR. Sinus lift grafts and endosseous implants: Treatment of the atrophic posterior maxilla. Dent Clin North Am. 1992;36:151–186.
- Chanavaz M. Maxillary sinus: anatomy, physiology, surgery, and bone grafting related to implantology--eleven years of surgical experience (1979-1990). J Oral Implantol. 1990;16:199–209.
- Thomason JM, Heydecke G, Feine JS, et al. How do patients perceive the benefit of reconstructive dentistry with regard to oral health-related quality of life and patient satisfaction? A systemic review. Clin Oral Implants Res. 2007; 18: 168-188.
- Sohn DS, Heo JU, Kwak DH, Kim DE, Kim JM, Moon JW, Lee JH, Park IS. Bone regeneration in the maxillary sinus using an autologous fibrin-rich block with concentrated growth factors alone. Implant Dent. 2011;20:389–395.
- Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991;62:2–4.
- Boyne PJ. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613–616.
- Tatum Jr H. Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986;30:207–229.
- Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007;22 Suppl:49-70.
- Adell R, Lekholm U, Gröndahl K, Brånemark P-I, Lindström J, Jacobsson M. Reconstruction of severely resorbed edentulous maxillae using osseointegrated fixtures in immediate autogenous bone grafts. Int J Oral Maxillofac Implants. 1990;5.
- Klijn RJ, Meijer GJ, Bronkhorst EM, Jansen JA. A meta-analysis of histomorphometric results and graft healing time of various biomaterials compared to autologous bone used as sinus floor augmentation material in humans. Tissue Eng Part B Rev. 2010;16:493–507.
- Schlegel KA, Fichtner G, Schultze-Mosgau S, Wiltfang J. Histologic findings in sinus augmentation with autogenous bone chips versus a bovine bone substitute. Int J Oral Maxillofac Implants. 2003;18.
- Lee EY, Kim KW. A double layers technique for maxillary sinus augmentation with demineralized and mineralized bone graft materials. Maxillofac Plast Reconstr Surg. 2009;31:46–52.
- Hatano N, Shimizu Y, Ooya K. A clinical long-term radiographic evaluation of graft height changes after maxillary sinus floor augmentation with a 2: 1 autogenous bone/xenograft mixture and simultaneous placement of dental implants. Clin Oral Implants Res. 2004;15:339–345.
- Kim YK, Lee J, Yun JY, Yun PY, Um IW. Comparison of autogenous tooth bone graft and synthetic bone graft materials used for bone resorption around implants after crestal approach sinus lifting: a retrospective study. J Periodontal Implant Sci. 2014;44:216–221.
- Iezzi G, Degidi M, Piattelli A, Mangano C, Scarano A, Shibli JA, Perrotti V. Comparative histological results of different biomaterials used in sinus augmentation procedures: a human study at 6 months. Clin Oral Implants Res. 2012;23:1369–1376.
- Chen TW, Chang HS, Leung KW, Lai YL, Kao SY. Implant placement immediately after the lateral approach of the trap door window procedure to create a maxillary sinus lift without bone grafting: a 2-year retrospective evaluation of 47 implants in 33 patients. J Oral Maxillofac Surg. 2007;65:2324–2328.
- Mazor Z, Peleg M, Garg AK, Luboshitz J. Platelet-rich plasma for bone graft enhancement in sinus floor augmentation with simultaneous implant placement: patient series study. Implant Dent. 2004;13:65–72.
- Moon JW, Shin HI, Jung JK. New bone formation in the maxillary sinus using peripheral venous blood alone. J Oral Maxillofac Surg. 2011;69:2357–2367.
- Urist MR, Huo YK, Brownell AG, Hohl WM, Buyske J, Lietze A, Tempst P, Hunkapiller M, DeLange RJ. Purification of bovine bone morphogenetic protein by hydroxyapatite chromatography. Proc Natl Acad Sci U S A. 1984;81:371–375.
- Yeomans JD, Urist MR. Bone induction by decalcified dentine implanted into oral, osseous and muscle tissues. Arch Oral Biol. 1967;12:999-1008.
- Kim ES, Kang JY, Kim JJ, Kim KW, Lee EY. Space maintenance in autogenous fresh demineralized tooth blocks with platelet-rich plasma for maxillary sinus bone formation: a prospective study. Springerplus. 2016;5:274.
- Peleg M, Garg AK, Misch CM, Mazor Z. Maxillary sinus and ridge augmentations using a surface-derived autogenous bone graft. J Oral Maxillofac Surg. 2004;62:1535–1544.
- Pinchasov G, Juodzbalys G. Graft-free sinus augmentation procedure: a literature review. J Oral Maxillofac Res. 2014;5.
- Xu H, Shimizu Y, Ooya K. Histomorphometric study of the stability of newly formed bone after elevation of the floor of the maxillary sinus. Br J Oral Maxillofac Surg. 2005;43:493–499.
- Schlegel AK, Donath K. BIO-OSS--a resorbable bone substitute? J Long Term Eff Med Implants. 1998;8:201–209.
- Hallman M, Cederlund A, Lindskog S, Lundgren S, Sennerby L. A clinical histologic study of bovine hydroxyapatite in combination with autogenous bone and fibrin glue for maxillary sinus floor augmentation: results after 6 to 8 months of healing. Clin Oral Implants Res. 2001;12:135–143.
- Kim YK, Lee J, Um IW, Kim KW, Murata M, Akazawa T, et al. Tooth-derived bone graft material. J Korean Assoc Oral Maxillofac Surg. 2013;39(3):103-111.
- Lee KH, Kim YK, Cho WJ, Um IW, Murata M, Mitsugi M. Autogenous tooth bone graft block for sinus augmentation with simultaneous implant installation: a technical note. J Korean Assoc Oral Maxillofac Surg. 2015;41(5):284-289.
- Schwarz F, Golubovic V, Becker K, Mihatovic I. Extracted tooth roots used for lateral alveolar ridge augmentation: a proof-of-concept study. J Clin Periodontol. 2016;43(4):345–353.
- Becker K, Drescher D, Hönscheid R, Golubovic V, Mihatovic I, Schwarz F. Biomechanical, micro-computed tomographic and immunohistochemical analysis of early osseous integration at titanium implants placed following lateral ridge augmentation using extracted tooth roots. Clin Oral Implants Res. 2017; 28(3):334-340.
- Asfour A, Farzad P, Andersson L, Joseph B, Dahlin C. Host tissue reactions of non-demineralized autogenic and xenogenic dentin blocks implanted in a non-osteogenic environment. An experimental study in rabbits. Dent Traumatol. 2014;30(3):198-203.
- Park SM, Kim DH, Pang EK. Bone formation of demineralized human dentin block graft with different demineralization time: In vitro and in vivo study. J Craniomaxillofac Surg. 2017;45(6):903-912.
- Urist MR. Bone histogenesis and morphogenesis in implants of demineralized enamel and dentin. J Oral Surg.1971;29:88-102.
- Bang G. Induction of heterotopic bone formation by demineralized dentin in guinea pigs: antigenicity of the dentin matrix. J Oral Pathol.1972;1:172-185.
- Bang G. Induction of heterotopic bone formation by demineralized dentin: an experimental model in guinea pigs. Scand J Dent Res.1973;81:240-250.
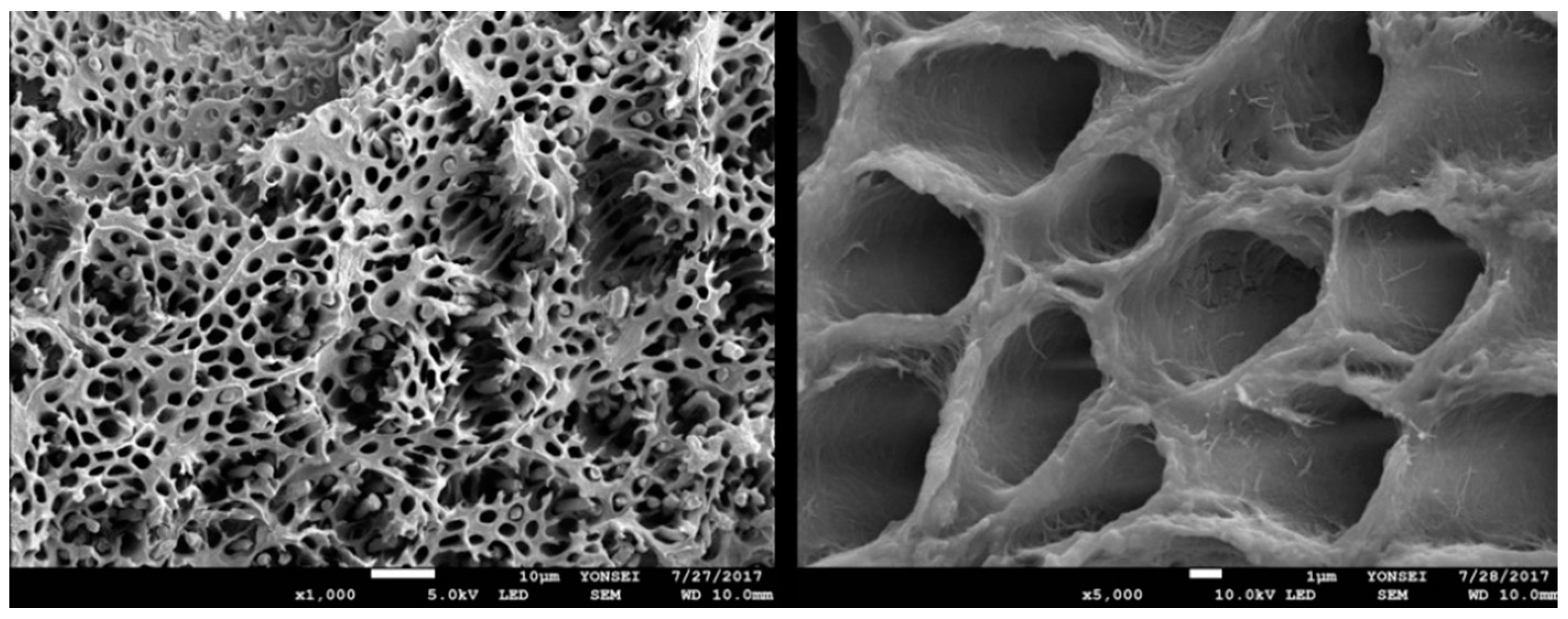
- Kabir MA, Murata M, Akazawa T, Kusano K, Yamada K, Ito M. Evaluation of perforated demineralized dentin scaffold on bone regeneration in critical-size sheep iliac defects. Clin Oral Implants Res. 2017;28(11):e227-e235.
- Moon YS, Sohn DS, Kim G, Park IS. Comparative histomorphometric evaluation of bone regeneration with different preparations of xenogeneic tooth block bone. Int J Oral Maxillofac Implants. 2019;34(6):1413-1422.
- Kim YK, Pang KM, Yun PY, Leem DH, Um IW. Long-term follow-up of autogenous tooth bone graft blocks with dental implants. Clin Case Rep. 2017;8;5(2):108-118.
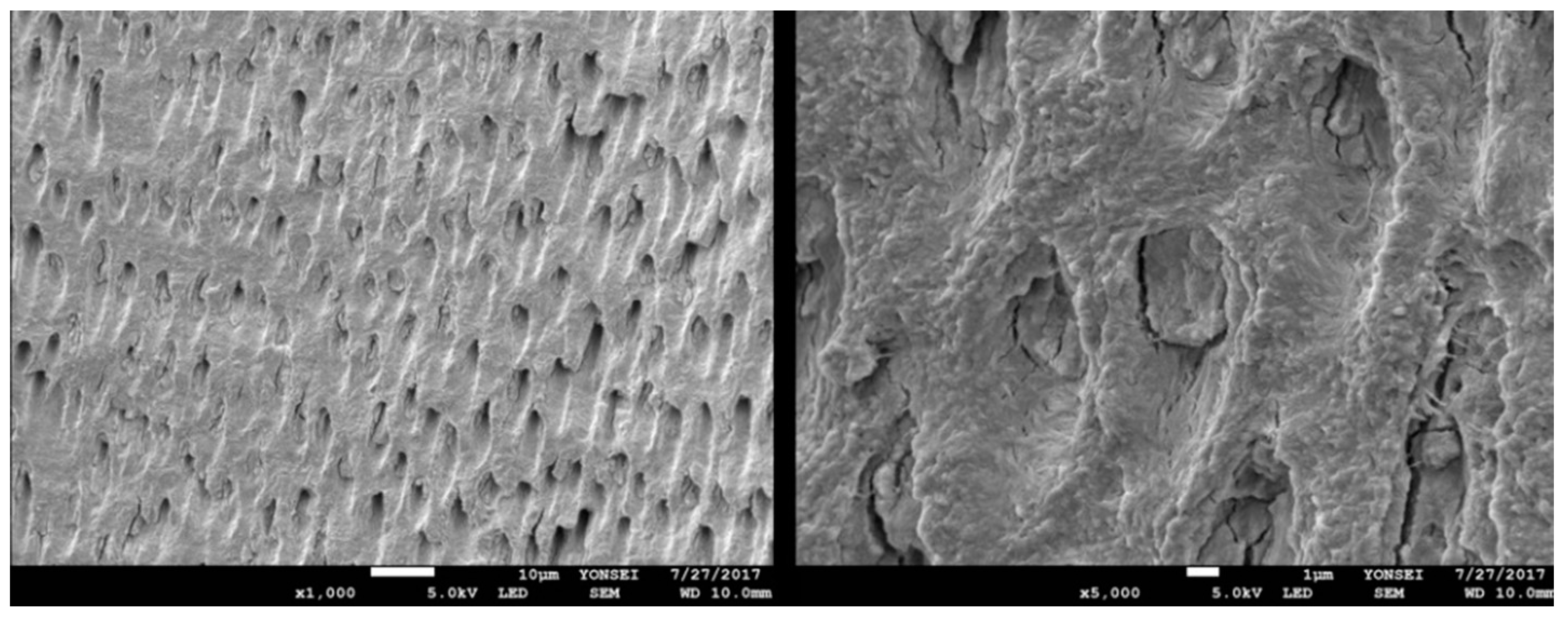
- Lee EY, Kim ES, Kim KW. Scanning electron microscopy and energy dispersive X-ray spectroscopy studies on processed tooth graft material by vacuum-ultrasonic acceleration. Maxillofac Plast Reconstr Surg. 2014;36:103.
- Gomes MF, Abreu PP de, Morosolli ARC, Araújo MM, Goulart M das GV. Densitometric analysis of the autogenous demineralized dentin matrix on the dental socket wound healing process in humans. Braz Oral Res. 2006;20:324–330.
| Subject | Sex/Age | Region | Failed site | Sinus membrane perforation | Months to second stage surgery | Months in function | ||
| 1 | M/50 | #16 | - | No | 4 | 58 | ||
| 2 | M/46 | #26 | - | No | 6 | 42 | ||
| 3 | F/50 | #27 | - | Yes | 4.5 | 60 | ||
| 4 | M/46 | #14,15,16,17 | - | No | 7 | 51 | ||
| 5 | M/59 | #26,27 | - | No | 5 | 50 | ||
| 6 | F/57 | #26 | - | No | 5 | 48 | ||
| 7 | F/52 | #17 | - | Yes | 10 | 50 | ||
| 8 | F/52 | #27 | - | No | 5.5 | 55 | ||
| 9 | M/65 | #16 | - | Yes | 6.5 | 54 | ||
| 10 | M/50 | #16,26 | - | No | 7.5 | 59 | ||
| 11 | F/58 | #26,27 | - | No | 7.5 | 52 | ||
| 12 | F/47 | #27 | - | No | 4 | 58 | ||
| 13 | M/64 | #16 | - | No | 3 | 50 | ||
| 14 | M/75 | #26 | - | No | 6 | 60 | ||
| 15 | F/54 | #16 | - | No | 10 | 46 | ||
| 16 | M/45 | #17 | - | No | 3.5 | 49 | ||
| 17 | M/52 | #26,27 | - | No | 5 | 53 | ||
| 18 | M/45 | #27 | - | No | 10.5 | 54 | ||
| 19 | F/57 | #26,27 | - | No | 5 | 61 | ||
| Subject | Region |
Preoperative bone height (mm) |
Maxillary sinus width (mm) |
Amount of sinus membrane elevation (mm) |
Bone height at the end of the study (mm) |
Increment of bone height (mm) |
| 1 | #16 | 5 | 12 | 18 | 14 | 9 |
| 2 | #26 | 3 | 18 | 17 | 13 | 10 |
| 3 | #27 | 5 | 16 | 16 | 14 | 9 |
| 4 | #14,15,16,17 | 5,3,5,5 | 22 | 15,18,14,16 | 15,16,14,14 | 10,13,9,8 |
| 5 | #26,27 | 4,4 | 16 | 16,16 | 15,12 | 11,8 |
| 6 | #26 | 6 | 16 | 18 | 20 | 14 |
| 7 | #17 | 2 | 24 | 16 | 15 | 13 |
| 8 | #27 | 2 | 22 | 19 | 18 | 16 |
| 9 | #16 | 2 | 22 | 16 | 14 | 12 |
| 10 | #16,26 | 3,3 | 23 | 23,20 | 20,22 | 17,19 |
| 11 | #26,27 | 3,2 | 24 | 19,18 | 20,16 | 17,14 |
| 12 | #27 | 4 | 22 | 16 | 15 | 11 |
| 13 | #16 | 5 | 12 | 14 | 14 | 9 |
| 14 | #26 | 4 | 16 | 12 | 12 | 8 |
| 15 | #16 | 1 | 20 | 22 | 18 | 17 |
| 16 | #17 | 5 | 13 | 17 | 20 | 15 |
| 17 | #26,27 | 6,6 | 15 | 10,11 | 15,16 | 9,10 |
| 18 | #27 | 3 | 25 | 12 | 14 | 11 |
| 19 | #26,27 | 1,2 | 20 | 21 | 14,14 | 13,12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





