1. Introduction
The first years after the birth of a child can come with a number of stressors for the parents. This can lead to impairments in mental health not only in parents themselves, but also in their children. Children of psychosocially stressed mothers and fathers are at high risk of social, emotional and cognitive problems [
1] because the development of a positive mother-child relationship is considered an essential resilience factor for child development. Maternal sensitivity in dealing with the infant is considered a key variable in mother-child interaction and child attachment development [
2,
3,
4]. A good parent-child relationship and a secure infant attachment have been identified as moderators of a child's healthy psychological and physical development [
4].
Common factors for a strained parent-child relationship are stress, psychological burden and mental disorders. Such factors limit the parental ability to sensitively perceive, correctly interpret and appropriately respond to the child's signals [
2,
5]. Furthermore, these stress factors influence the parents' reflexive ability to empathize with their child's feelings and needs and to differentiate these from their own inner states [
6], thus establishing negative interaction cycles that have a considerable impact on the development of regulatory disorders, insecure attachment patterns, child behavioural problems and psychopathologies [
7,
8,
9]. Affected parents and children should not be considered separately. For example, up to 18% of infants and young children also show psychological and/or psychosomatic symptoms in the form of early childhood regulatory disorders [
10]. Also, the additional burden of illness and social isolation, which has affected many families during the coronavirus pandemic, has already had an impact on mother-child bonding and the frequency and severity of regulatory disorders in infants [
11].
The occurrence of mental health, especially postnatal depression and anxiety disorders in mothers has been intensively studied worldwide. Studies on the prevalence of mental health disorders in mothers are showing large variations, with global prevalence estimates of 18% for postnatal depression, 15% and 19% for postnatal anxiety symptoms and anxiety disorders [
12,
13,
14]. Children of mothers with postnatal mental illness seem to have an increased risk of developing their own psychological problems. Martini and colleagues showed that in infants, regulatory disorders like sleeping or feeding problems or excessive crying were associated with maternal mental health problems [
15]. Population-based studies from Denmark and Australia revealed prevalence rates of regulatory problems of up to 21% in the first two years of life of the children [
16,
17]. Postnatal mental health in fathers has not been a focus of research for a long time, but in the last two decades there has been an increase in studies devoted to this disorder. A meta-analysis by Cameron and colleagues assessed a prevalence rate of 8.4% for paternal prenatal and postpartum depression [
18]. In Germany, prevalence data on mental health problems in parents and their infants in the first years of life are mostly derived from hospital- or outpatient-based studies, often including only mothers and not fathers [
15,
19].
There are several well-known determinants for maternal mental health problems in the postpartum period and beyond, for example an unplanned pregnancy or a lack of social support [
20,
21,
22]. In a German study assessing psychosocial stressors in families with infants and toddlers, 20% of the parents reported lack of family and social support and 21% an unplanned pregnancy [
23]. Given the high percentages and the well-established associations between parental stressors and mental health in parents and their children in their first years of life, data from population-based studies assessing mental health problems in parents and children are needed. Population-based data could provide an overall picture of the mental health status of parents and their young children and identify potential gaps in the healthcare and social system in Germany.
The SKKIPPI cohort study was established to assess the occurrence and determinants of psychosocial stress and mental health disorders in parents and their offspring in early childhood [
24]. The study is part of a multi-component project with randomised intervention as well as qualitative studies [
25,
26,
27], funded by the German health care innovation fund to improve integrated and innovative care in Germany [
28].
The objective of this analysis was to describe the cohort study population regarding psychosocial stress, mental health problems and possible determinants that may play a role in the development of these problems and to provide a screening instrument for potentially affected parents.
2. Materials and Methods
2.1. Study Design and Setting
The SKKIPPI cohort study was a prospective observational population-based study. The study was conducted in three urban regions of northern and eastern Germany (Berlin, Flensburg and Leipzig). After inclusion in the study, we screened for parents with an elevated mental health risk and collected relevant characteristics using a screening online questionnaire (
Supplementary Material 1). Participants with an elevated mental health risk were invited for further assessments, details on these further assessments and the entire study were described previously [
24]. The analysis presented in this paper contains only data collected with the above named screening online questionnaire. This article is reported in accordance with ‘Strengthening the reporting of observational studies in epidemiology’ (STROBE) Statement – Checklist: cohort, case-control, and cross-sectional studies (combined) [
29].
2.2. Study Population
A random sample of 30,000 addresses of families with children aged up to 12 months (at the time the sample was drawn), was provided by the residents' registration offices in Berlin, Leipzig, and Flensburg. The children’s parents received at least one invitation letter to participate in this study. Invitation letters were sent to the registered mother but included two access codes, so both parents were able to participate in the first step of the study. Mothers who gave birth to more than one child within the 12 month sampling period (i. e. multiple births or two children in one year) received only one invitation letter. If no mother was registered, the person entitled to custody received the invitation letter. Other caregivers were able to complete the screening online questionnaire indicating their caregiver status, but only data from biological or adoptive parents were included for analysis. Inclusion criteria comprised that parents were at least 18 years of age and able to complete the screening online questionnaire in German, English, Turkish, or Arabic language. Written or online informed consent was obtained from all participants prior to the study inclusion.
2.3. Data Collection
In the screening online questionnaire, the following data were collected, covering the four common domains of stress factors: parent, family, parent-child interaction, and child [
30]. Sociodemographic characteristics, perinatal stressors and characteristics (e.g. pregnancy planned, multiple pregnancy, complications during pregnancy), individual parental stressors (e.g. partnership/professional/financial problems, possible parental childhood trauma) and mental health problems in the parent and the child. Possible parental childhood trauma was assessed with the following single question “Have there been any severe, negative experiences in your childhood that you have not overcome to date?”. Data on mental health problems included questions on lifetime mental health disorders and current mental health problems. Current mental health problems were assessed using questions from the Patient Health Questionnaire (PHQ) 4 [
31], questions on obsessive-compulsive thoughts/acts from the Zohar-Fineberg Obsessive Compulsive Screen [
32], as well as questions regarding alcohol/drug abuse [
33] and current regulatory problems of the child [
34]. The PHQ 4 is subdivided into two parts: the PHQ 2 (2-item depression scale) and the Generalized Anxiety Disorder (GAD) 2 (2-item anxiety scale) [
31].
The screening online questionnaire (
Supplementary Material 1) was newly developed by the study team, discussed with various experts, and piloted. We developed a scoring system with points ranging from 0-5 for each of the 40 question and a cut-off of 5 points indicating an elevated mental health risk. The cut-off of the screening questionnaire was adjusted early in the study to 10 points because it was found that too many mothers without evidence of a mental health disorder in the further assessments of the study were identified as positive by the screening online questionnaire. Data from the questionnaire were screened for plausibility and completeness. Answers in the questionnaire were validated at entry. User input that did not match a given data type or range was dismissed and the user was prompted to answer the question again. It was not mandatory to answer questions, but when a question was skipped the user was asked once for confirmation.
2.4. Statistical Analysis
The data of the screening online questionnaire were analysed descriptively. Results are presented in the form of means and standard deviations for continuous data, and frequencies and percentages for categorical data. For each analysis, all respective available data were used, missing data were not replaced. All statistical analyses were performed using SPSS Version IBM SPSS Statistics 26.
3. Results
3.1. Participants
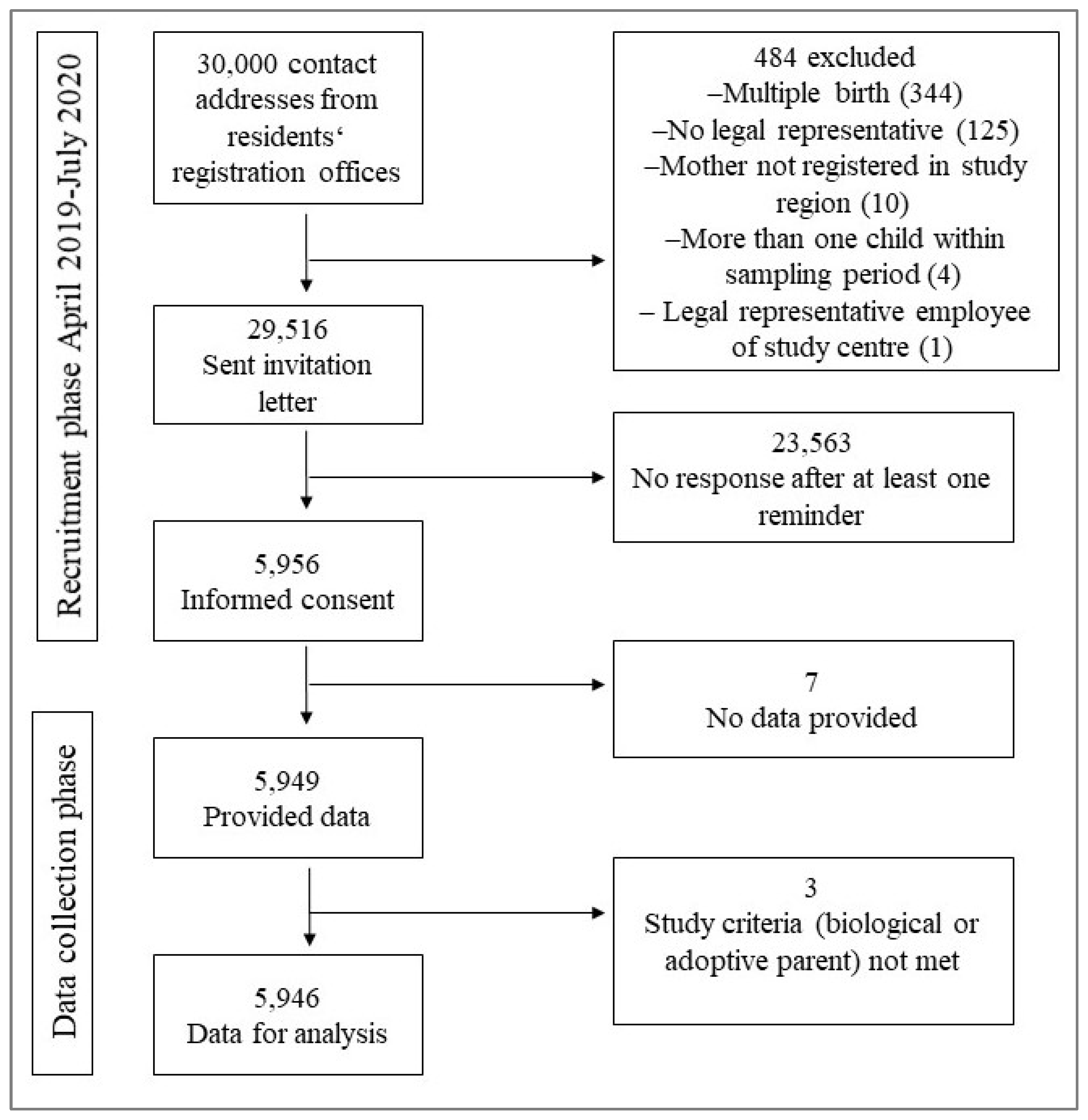
Until the end of the recruitment period (March 2019 - July 2020) 29,516 invitation letters were sent out and at least one additional reminder letter if the first letter was unanswered. 484 received no letter, the specific reasons for exclusion can be found in
Figure 1. Nearly 99% of all parents filled out the screening online questionnaire completely. However, we also included data from questionnaires that were not completely filled out. Of all participants, 4,981 (83.8%) indicated to be biological mothers, three to be adoptive mothers (0.1%) and 962 (16.2%) assumed to be biological fathers. No adoptive father participated in the study. In total, either the mother, the father or both parents of 5,151 children participated in the study (17.5%). Over 95% of the study parents participated prior to 16th of March 2020, the date when lockdowns and other measures related to the SARS-CoV-2 pandemic started in Germany.
3.2. Sociodemographic Characteristics
Most parents (mothers 74%, fathers 67%) were between 30 and 39 years of age (
Table 1). Around 80% of them were born in Germany. Nearly 85% had a high educational level according to the International Standard Classification of Education (ISCED) categorisation. Children ranged in age from 6 to 29 months (m=14.6 months ±3.0).
3.3. Perinatal Stressors and Characteristics
Approximately three quarters of both mothers and fathers indicated that the pregnancy was planned, and the timing was suitable, in contrast to 5% of mothers and 3% of fathers who stated that the pregnancy was not planned and the timing not suitable (
Supplementary Material 2). Three percent of the mothers delivered twins and 7% premature babies. Nearly one quarter of the babies were delivered by Caesarean birth.
3.4. Individual Parental Stressors
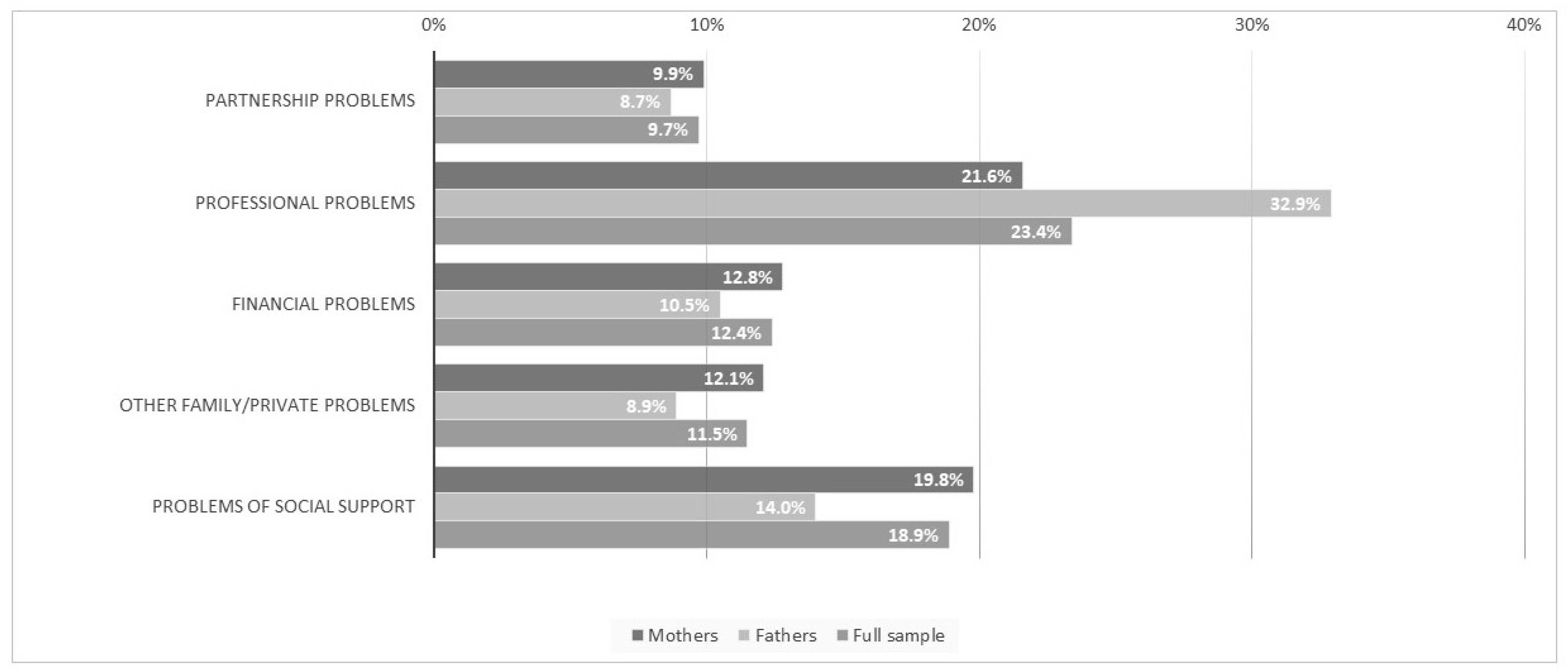
One third of the fathers and 22% of the mothers reported to have rather more or strong/very strong professional problems (
Figure 2). Severe, negative experiences in childhood that have not yet been overcome were disclosed in 22% of the mothers and 16% of the fathers (
Table 2). In terms of digital media use, 16% of both parents indicated feeling stressed when their child seeks attention while using their smartphone/tablet.
3.5. Mental Health Problems of the Parents and the Child
The lifetime occurrence of depression was 15% for mothers and around 7% for fathers, and anxiety disorders around 6% for mothers and circa 3% for fathers (
Table 3). Nearly one tenth of the mothers and fathers scored 3 or higher in the PHQ 2 Questionnaire (depressive symptoms within the PHQ 4), 11%, and 7%, respectively in the GAD-2 Questionnaire (anxiety symptoms within the PHQ 4). Twenty-one percent and 15%, respectively reported obsessive-compulsive thoughts and 20% and 12% respectively reported mood swings and difficulties in controlling feelings. Between two and five percent of the parents reported that their child exhibited symptoms of one of the indicated regulatory problems at the time of survey (
Table 4).
4. Discussion
4.1. Main Findings
Results from the screening online questionnaire of the SKKIPPI cohort study showed that parents of children in the first years after birth were facing a variety of considerable psychosocial stressors. Obsessive-compulsive thoughts, mood swings and difficulties in controlling feelings and depressive and anxiety symptoms were the most frequently reported mental health problems by both parents. Al least one regulatory problem of the child was reported by around 5% of the parents. The use of the screening online questionnaire turned out to be feasible.
4.2. Comparison with Other Studies
Parents of nearly 18% of the children drawn from the residents' registration offices in Berlin, Leipzig, and Flensburg participated in the first step of the study. During preparation of the study a response rate of 20% was estimated [
24] and the response rate achieved (17.5%) was only slightly below and corresponds to response rates from other epidemiological studies in Germany in previous years [
35,
36]. Nearly 99% of the consented participants also finished the questionnaire, so completeness of the data is very high. Given the fact that the invitation letter was primarily addressing the mother, the high number of mothers in the study sample (85%) is not surprising. To get a broader insight into the specific problems that fathers have in the early childhood period, future studies should address the fathers more comprehensively. As the majority of parents completed the online questionnaire before the restrictions and lockdowns due to the SARS-CoV-2 pandemic were implemented in Germany (95%), we assume that the results of this part of the study were not significantly influenced by the pandemic.
Our age range of 30-39 years for most participants corresponds to the average age for first time parents in Germany. In 2020, mothers were on average 30 years old and fathers 33 years old at the time of birth of their first child [
37]. It is striking that the number of single parents in our sample was relatively low (5% for both parents). In 2019, the proportion of single mothers or fathers among all families in Germany was 18.6% [
38]. One reason for this difference could be the fact that our sample included only parents with very small children. It is likely that many parents separate a little later and not so soon after birth. The above-mentioned prevalence for Germany was assessed for all families with minor children and not only very small children. Another possible reason could be that single parents with small children have less time to participate in this kind of study.
Concerning adverse perinatal stressors, an unwanted/unplanned pregnancy is a known risk factor for postpartum depression [
20]. In our questionnaire, we asked not only if the pregnancy was planned, but also if it was a suitable time. More than one fifth of the parents in our study reported that the pregnancy was not planned, a prevalence that has also been assessed by Lorenz et al. in another German sample [
23]. Unfortunately, we do not know whether parents having ambivalent or adverse feelings about being pregnant had a higher or lower participation rate in this study. While more than 93% of the parents indicated that their child is or was breastfed at least to some extent, we did not ask how long they were breastfeeding for. There may be a certain amount of mothers who only breastfed for a short period. Unfortunately, we did not ask specific questions to ascertain whether breastfeeding was seen more as a stressful or positive experience for the parents. The same is true for other perinatal characteristics like childbirth setting, delivery procedure or being a parent for the first time.
Parents in our study reported to be confronted with a variety of individual stressors. We found the highest percentages for both mothers and fathers in the categories of professional problems and problems concerning lack of social support. The latter stressor is a well-known risk factor that has been investigated in various studies on postnatal depression [
20,
22]. Work-related or professional stress as determinant for mental health problems has been assessed in various studies in men and women in the general population [
39,
40], but seems to be less often considered in the postnatal setting and should be further investigated. Severe, negative experiences during childhood has been shown to be a risk factor for pre- and postnatal depression [
41,
42]. Comparing our study with another study on psychosocial stress, parents in our study reported more often severe, negative experiences during childhood [
23]. As this stressor was only assessed with one single question in our study, this result should be interpreted with caution. Within the further assessments of the SKKIPPI cohort study, participants get a more detailed questionnaire on this topic, so we may get a better insight into this particular stressor. A recent review on research related to parent distraction with phones and mobile devices suggests its adverse impact on parenting sensitivity and behaviours [
43], but most evidence comes from self-reporting and observations and more longitudinal data is needed in this area of research. In our study, around 16% of mothers and fathers feel stressed if their child seeks their attention while they are using their smart phone/tablet. As mobile phones have become an indispensable part of parents' daily lives, this influence should be investigated more specifically in future studies.
Obsessive-compulsive symptoms are less well studied during the postnatal period as compared to depressive or anxiety problems, but various studies showed that the postpartum period is a high-risk time for this kind of mental health problem in mothers and fathers [
44,
45]. In our sample, a large number of parents reported obsessive-compulsive thoughts, but not as much obsessive-compulsive acts. Obviously, we cannot deduce from these results that all parents indicating obsessive-compulsive thoughts had an obsessive-compulsive disorder as these kinds of thoughts can also be part of a depressive symptomatology. However, the high number should draw more attention to this kind of symptom. Within the further assessments of the SKKIPPI cohort study, participants will get a comprehensive psychiatric diagnostic interview, so we will get more precise numbers for obsessive-compulsive disorders in our sample. As for the occurrence of actual depressive symptoms, former studies from Germany reported lower numbers for depression in mothers in the first months after birth, ranging from 3% to 6% [
19,
46], however samples were not population- but hospital-based. Data from a recent, large population-based study in Germany (based on PHQ 8), showed similar rates to our study, however they included both women and men with and without children and not only parents (women 10.8% versus men 7.6%, n=254,510, age >=15 years) [
47]. Interestingly, the age range of 15-29 years in the above-mentioned study showed the highest prevalence rates (11.5% for both men and women together). For anxiety problems, previous data from Germany showed similar frequencies for mothers in the first months after birth (circa 11%) [
19], but the sample was hospital-, not population-based.
Occurrences of regulatory problems in the children of our sample were lower than in other German studies [
15,
17]. Some of our participants indicated in the questionnaire that their children have had regulatory problems in the very first months after birth, but not anymore at the time of the assessment. Another reason for this difference could be that we did not implement a specific questionnaire for this kind of problem in the online questionnaire but asked only for the parental perception of the child’s current behaviour. Within the further assessments of the SKKIPPI cohort study, the presence of problems concerning crying, feeding, and sleeping are investigated in more detail using the specific questionnaire developed by Groß and colleagues [
34].
4.3. Strengths and Limitations
One of the strengths of our study is the large, population-based sample, while previous studies are often based on hospital or other routine healthcare related data. We developed a short questionnaire in simple language assessing all kinds of parental stressors and translated it into several languages. We assessed not only typical maternal, but also paternal and child-related stressors. However, several limitations have to be discussed. Firstly, even if we recruited a population-based sample, it is not representative of Germany, since we recruited participants in only three regions of Germany, which are mostly urban. There is a need to get more data for rural regions where stressors can also be distinct from psychosocial and other stressors in urban regions. The reason for choosing these specific regions was the location of the respective partner institutions of the overall SKKIPPI study project. Secondly, we could not assess specific data on the non-responders of the study, so potential differences in the characteristics between responders and non-responders are unknown. The educational level of the participants was very high (85% belonged to the highest group). This is a common finding in epidemiological studies and reflects a general underrepresentation of people with middle and low education levels [
48,
49]. Therefore, our goal to reach more people with lower education levels by keeping the questionnaire short and in simple language was not sufficient. Future studies should therefore try to implement specific adapted strategies to recruit more people with lower educational levels, e.g. through more targeted sampling. Thirdly, we cannot exclude that social expectations may have played a role in answering some of the more personal questions. For example, in answering the questions if the pregnancy was planned, if the child was breastfed or how close the relationship to the child is. However, we tried to reduce the social desirability bias by collecting data via online questionnaire and not by face-to-face interview. Fourthly, we collected data on the lifetime occurrence but not on the beginning of the mental health problems, thus were not able to assess their presence during pregnancy. The reason for this was based on considerations that such prenatal information may not be validly assessed retrospectively, and answers may be biased.
5. Conclusions
Our data analyses from a large German population-based cohort study indicated that a substantial proportion of parents were burdened by psychosocial problems and showed indications of mental health problems during this period. Based on these data, the availability of early preventive and low-threshold support measures in the health and social care system should be adapted to the needs of new parents. Future research efforts should include follow-up analyses of this cohort and further attempts to include more fathers, parents with lower socioeconomic status and families with migration backgrounds in population-based studies. The newly developed questionnaire can be used in these and other studies with the aim of screening potentially affects parents.
Supplementary Materials
The following supporting information can be downloaded at: Preprints.org, Supplementary material 1_Screening tool.pdf; Supplementary material 2_Stressors.pdf.
Author Contributions
Conceptualization, J.F., L.K., C.L.-K., T.R., A.B., S.R. and T.K.; methodology, J.F., L.K., C.L.-K., T.R., A.B., S.R., K.I. and T.K.; validation, S.R., J.F. and M.B.; formal analysis, S.R., J.F., K.I. and M.B.; investigation, J.F., M.B. and N.L.; resources, J.F., K.I. and N.L.; data curation, K.I.; writing—original draft preparation, J.F.; writing—review and editing, M.B., L.K., C.L.-K., T.R., A.B., S.R., F.S.-S. and T.K..; visualization, J.F., and A.B.; supervision, T.K., L.K., and A.B.; project administration, T.K., L.K., N.L. and A.B.; funding acquisition, T.K., L.K., A.B. and S.R.. All authors have read and agreed to the published version of the manuscript.
Funding
The SKKIPPI project is supported by a grant from the German Health Care Innovation Fund (No 01 VSF17027).
Institutional Review Board Statement
Ethical approval for this study was obtained from the ethics committee of the Charité - Universitätsmedizin Berlin (reference number: EA2/201/18). The study has been registered in the German Clinical Trial Registry on February 8th 2019 (DRKS-ID: DRKS00016653).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data will be available from the authors upon reasonable request with restrictions regarding scientific purpose and data protection.
Acknowledgments
We would like to thank Melanie Liedtke for the data management and data cleaning. Moreover, we thank the student research assistants (Ina Temeschinko, Isabelle-Valentine Springer, Maike Stolz, Maximilian Leschinski, Melisa Celik, Paula Kuper, Sali Al-Rubaiey and Stella Hoffmann) for managing appointments with participants and conducting standardized telephone interviews.).
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Ramchandani, P., A. Stein, J. Evans, T. G. O'Connor, and Alspac study team. "Paternal Depression in the Postnatal Period and Child Development: A Prospective Population Study." Lancet 365, no. 9478 (2005): 2201-5. [CrossRef]
- Ainsworth, M.D.S., S.M. Bell, and D.F. Stayton. "Infant-Mother Attachment and Social Development: Socialization as a Product of Reciprocal Responsiveness to Signals." In The Integration of a Child into a Social World, edited by Richards MPM, 99- 135. New York, NY, US: Cambridge University Press, 1974.
- Carter, A. S., F. E. Garrity-Rokous, R. Chazan-Cohen, C. Little, and M. J. Briggs-Gowan. "Maternal Depression and Comorbidity: Predicting Early Parenting, Attachment Security, and Toddler Social-Emotional Problems and Competencies." J Am Acad Child Adolesc Psychiatry 40, no. 1 (2001): 18-26.
- Grossmann, K. E., and K. Grossmann. "[the Development of Psychological Security in Attachment--Results and Conclusions for Therapy]." Z Psychosom Med Psychother 53, no. 1 (2007): 9-28.
- Papousek, H., and M. Papousek. "Structure and Dynamics of Human Communication at the Beginning of Life." Eur Arch Psychiatry Neurol Sci 236, no. 1 (1986): 21-5.
- Fonagy, P., D. Cottrell, J. Phillips, D. Bevington, D. Glaser, and E. Allison. What Works for Whom?: A Critical Review of Treatments for Children and Adolescents. 2nd ed. London: Guilford Publications, 2014.
- Petzoldt, J., H. U. Wittchen, J. Wittich, F. Einsle, M. Hofler, and J. Martini. "Maternal Anxiety Disorders Predict Excessive Infant Crying: A Prospective Longitudinal Study." Arch Dis Child 99, no. 9 (2014): 800-6. [CrossRef]
- Hemmi, M. H., D. Wolke, and S. Schneider. "Associations between Problems with Crying, Sleeping and/or Feeding in Infancy and Long-Term Behavioural Outcomes in Childhood: A Meta-Analysis." Arch Dis Child 96, no. 7 (2011): 622-9.
- Lyons-Ruth, K. "Contributions of the Mother-Infant Relationship to Dissociative, Borderline, and Conduct Symptoms in Young Adulthood." Infant Ment Health J 29, no. 3 (2008): 203-18.
- Briggs-Gowan, M. J., A. S. Carter, E. M. Skuban, and S. M. Horwitz. "Prevalence of Social-Emotional and Behavioral Problems in a Community Sample of 1-and 2-Year-Old Children." Journal of the American Academy of Child and Adolescent Psychiatry 40, no. 7 (2001): 811-19.
- Sprengeler, M.K., J. Mattheß, M.G. Galeris, M. Eckert, G. Koch, T. Reinhold, A. Berghöfer, J. Fricke, S. Roll, T. Keil, C. Ludwig-Körner, L. Kuchinke, K. von Klitzing, L. O. White, and F. Schlensog-Schuster. "Being an Infant in a Pandemic: Influences of the Covid-19 Pandemic on Infants, Toddlers and Their Mothers in a Clinical Population." Children 10, no. 12 (2023): 1885.
- Arifin, S. R. M., H. Cheyne, and M. Maxwell. "Review of the Prevalence of Postnatal Depression across Cultures." AIMS Public Health 5, no. 3 (2018): 260-95. [CrossRef]
- Dennis, C. L., K. Falah-Hassani, and R. Shiri. "Prevalence of Antenatal and Postnatal Anxiety: Systematic Review and Meta-Analysis." Br J Psychiatry 210, no. 5 (2017): 315-23.
- Hahn-Holbrook, J., T. Cornwell-Hinrichs, and I. Anaya. "Economic and Health Predictors of National Postpartum Depression Prevalence: A Systematic Review, Meta-Analysis, and Meta-Regression of 291 Studies from 56 Countries." Front Psychiatry 8 (2017): 248.
- Martini, J., J. Petzoldt, S. Knappe, S. Garthus-Niegel, E. Asselmann, and H. U. Wittchen. "Infant, Maternal, and Familial Predictors and Correlates of Regulatory Problems in Early Infancy: The Differential Role of Infant Temperament and Maternal Anxiety and Depression." Early Hum Dev 115 (2017): 23-31.
- Skovgaard, A. M., T. Houmann, E. Christiansen, S. Landorph, T. Jorgensen, C. C. C. Study Team, E. M. Olsen, K. Heering, S. Kaas-Nielsen, V. Samberg, and A. Lichtenberg. "The Prevalence of Mental Health Problems in Children 1(1/2) Years of Age - the Copenhagen Child Cohort 2000." J Child Psychol Psychiatry 48, no. 1 (2007): 62-70.
- Wake, M., E. Morton-Allen, Z. Poulakis, H. Hiscock, S. Gallagher, and F. Oberklaid. "Prevalence, Stability, and Outcomes of Cry-Fuss and Sleep Problems in the First 2 Years of Life: Prospective Community-Based Study." Pediatrics 117, no. 3 (2006): 836-42.
- Cameron, E. E., I. D. Sedov, and L. M. Tomfohr-Madsen. "Prevalence of Paternal Depression in Pregnancy and the Postpartum: An Updated Meta-Analysis." J Affect Disord 206 (2016): 189-203.
- Reck, C., K. Struben, M. Backenstrass, U. Stefenelli, K. Reinig, T. Fuchs, C. Sohn, and C. Mundt. "Prevalence, Onset and Comorbidity of Postpartum Anxiety and Depressive Disorders." Acta Psychiatr Scand 118, no. 6 (2008): 459-68. [CrossRef]
- Beck, C. T. "Predictors of Postpartum Depression: An Update. ." Nurs Res 50 (2001): 275-85.
- Clout, D., and R. Brown. "Sociodemographic, Pregnancy, Obstetric, and Postnatal Predictors of Postpartum Stress, Anxiety and Depression in New Mothers." J Affect Disord 188 (2015): 60-7.
- O'Hara, Michael W., and Annette M. Swain. "Rates and Risk of Postpartum Depression—a Meta-Analysis." International Review of Psychiatry 8, no. 1 (2009): 37-54.
- Lorenz, S., S. M. Ulrich, A. Sann, and C. Liel. "Self-Reported Psychosocial Stress in Parents with Small Children—Results from the Kinder in Deutschland–Kid-0–3 Study." Dtsch Arztebl International 117, no. 42 (2020): 709-16.
- Fricke, J., M. Bolster, C. Ludwig-Korner, L. Kuchinke, F. Schlensog-Schuster, P. Vienhues, T. Reinhold, A. Berghofer, S. Roll, and T. Keil. "Occurrence and Determinants of Parental Psychosocial Stress and Mental Health Disorders in Parents and Their Children in Early Childhood: Rationale, Objectives, and Design of the Population-Based Skkippi Cohort Study." Soc Psychiatry Psychiatr Epidemiol 56, no. 6 (2021): 1103-12.
- Eckert, M., J. Mattheß, J. Fricke, K. Richter, M. Sprengeler, G. Koch, S. Roll, M. Bolster, A. Berghöfer, T. Reinhold, P. Vienhues, K. von Klitzing, C. Ludwig-Körner, F. Schlensog-Schuster, T. Keil, and L. Kuchinke. "Evaluation Der Eltern-Säugling-Kleinkind-Psychotherapie Mittels Prävalenz- Und Interventionsstudien (Skkippi)." In DGPPN Kongress 2019, edited by Psychosomatik und Nervenheilkunde Deutsche Gesellschaft für Psychiatrie und Psychotherapie. Berlin: Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde, 2019.
- Mattheß, J., M. Eckert, K. Richter, G. Koch, T. Reinhold, P. Vienhues, A. Berghöfer, S. Roll, T. Keil, F. Schlensog-Schuster, K. von Klitzing, C. Ludwig-Körner, and L. Kuchinke. "Efficacy of Parent-Infant-Psychotherapy with Mothers with Postpartum Mental Disorder: Study Protocol of the Randomized Controlled Trial as Part of the Skkippi Project." Trials 21, no. 1 (2020): 490.
- Sprengeler, M. K., J. Mattheß, M. Eckert, K. Richter, G. Koch, T. Reinhold, P. Vienhues, A. Berghöfer, J. Fricke, S. Roll, T. Keil, C. Ludwig-Körner, L. Kuchinke, K. von Klitzing, and F. Schlensog-Schuster. "Efficacy of Parent-Infant Psychotherapy Compared to Care as Usual in Children with Regulatory Disorders in Clinical and Outpatient Settings: Study Protocol of a Randomised Controlled Trial as Part of the Skkippi Project." BMC Psychiatry 21, no. 1 (2021): 118.
- Berghöfer, A., D. G. Göckler, J. Sydow, C. Auschra, L. Wessel, and M. Gersch. "The German Health Care Innovation Fund - an Incentive for Innovations to Promote the Integration of Health Care." J Health Organ Manag 34, no. 8 (2020): 915-23. [CrossRef]
- von Elm, E., D. G. Altman, M. Egger, S. J. Pocock, P. C. Gotzsche, J. P. Vandenbroucke, and Strobe Initiative. "The Strengthening the Reporting of Observational Studies in Epidemiology (Strobe) Statement: Guidelines for Reporting Observational Studies." J Clin Epidemiol 61, no. 4 (2008): 344-9.
- Stith, S. M., T. Liu, L. C. Davies, E. L. Boykin, M. C. Alder, J. M. Harris, A. Som, M. McPherson, and J. E. M. E. G. Dees. "Risk Factors in Child Maltreatment: A Meta-Analytic Review of the Literature." Aggression and Violent Behavior 14, no. 1 (2009): 13-29.
- Löwe, B., I. Wahl, M. Rose, C. Spitzer, H. Glaesmer, K. Wingenfeld, A. Schneider, and E. Brahler. "A 4-Item Measure of Depression and Anxiety: Validation and Standardization of the Patient Health Questionnaire-4 (Phq-4) in the General Population." J Affect Disord 122, no. 1-2 (2010): 86-95.
- Fineberg, N., and A. Robert. "Obsessive Compulsive Disorder: A Twentyfirst Century Perspective." In Obsessive Compulsive Disorder: A Practical Guide, edited by N. Fineberg, D. Marazziti and D.J. Stein, 1-13. London: Martin Dunitz, 2001.
- Bundesinitiative Frühe Hilfen. "Kid 0-3: Ein Fragebogen Zur Situation Von Familien Mit Säuglingen Und Kleinkindern in Deutschland." 2013.
- Groß, S, C. Reck, C Thiel-Bonney, and M. Cierpka. "Empirische Grundlagen Des Fragebogens Zum Schreien, Füttern Und Schlafen (Sfs)." Prax. Kinderpsychol. Kinderpsychiat. 62 (2013): 327-47.
- Robert Koch-Institut. "Daten Und Fakten: Ergebnisse Der Studie "Gesundheit in Deutschland Aktuell 2012"." In Beiträge zur Gesundheitsberichterstattung des Bundes , edited by Robert-Koch Institut. Berlin: RKI, 2014.
- Schipf, S., G. Schöne, B. Schmidt, K. Günther, G. Stübs, K. H. Greiser, F. Bamberg, C. Meinke-Franze, H. Becher, K. Berger, H. Brenner, S. Castell, A. Damms-Machado, B. Fischer, C. W. Franzke, J. Fricke, S. Gastell, M. Günther, W. Hoffmann, B. Holleczek, L. Jaeschke, A. Jagodzinski, K. H. Jöckel, R. Kaaks, H. U. Kauczor, Y. Kemmling, A. Kluttig, L. Krist, B. Kurth, O. Kuss, N. Legath, M. Leitzmann, W. Lieb, J. Linseisen, M. Löffler, K. B. Michels, R. Mikolajczyk, I. Pigeot, U. Mueller, A. Peters, S. Rach, T. Schikowski, M. B. Schulze, C. Stallmann, A. Stang, E. Swart, S. Waniek, K. Wirkner, H. Völzke, T. Pischon, and W. Ahrens. "[the Baseline Assessment of the German National Cohort (Nako Gesundheitsstudie): Participation in the Examination Modules, Quality Assurance, and the Use of Secondary Data]." Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 63, no. 3 (2020): 254-66.
- Statistisches Bundesamt (Destatis). "Daten Zum Durchschnittlichen Alter Der Eltern Bei Geburt Nach Der Geburtenfolge Für 1. Kind, 2. Kind, 3. Kind Der Mutter Und Insgesamt 2020." Statistisches Bundesamt. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Geburten/Tabellen/geburten-eltern-biologischesalter.html (accessed July 22, 2021).
- Lenze, A., A. Funcke, and S. Menne. "Factsheet Alleinerziehende in Deutschland." Gütersloh: Bertelsmann Stiftung, 2021.
- Melchior, M., A. Caspi, B. J. Milne, A. Danese, R. Poulton, and T. E. Moffitt. "Work Stress Precipitates Depression and Anxiety in Young, Working Women and Men." Psychol Med 37, no. 8 (2007): 1119-29.
- Wang, J. L., A. Lesage, N. Schmitz, and A. Drapeau. "The Relationship between Work Stress and Mental Disorders in Men and Women: Findings from a Population-Based Study." J Epidemiol Community Health 62, no. 1 (2008): 42-7.
- Leigh, B., and J. Milgrom. "Risk Factors for Antenatal Depression, Postnatal Depression and Parenting Stress." BMC Psychiatry 8 (2008): 24.
- Wosu, A. C., B. Gelaye, and M. A. Williams. "History of Childhood Sexual Abuse and Risk of Prenatal and Postpartum Depression or Depressive Symptoms: An Epidemiologic Review." Arch Womens Ment Health 18, no. 5 (2015): 659-71. [CrossRef]
- McDaniel, B. T. "Parent Distraction with Phones, Reasons for Use, and Impacts on Parenting and Child Outcomes: A Review of the Emerging Research." Human Behavior and Emerging Technologies 1, no. 2 (2019): 72-80.
- Walker, R., M. Blackie, and M. Nedeljkovic. "Fathers' Experience of Perinatal Obsessive-Compulsive Symptoms: A Systematic Literature Review." Clin Child Fam Psychol Rev 24, no. 3 (2021): 529-41.
- Hudepohl, N., J. V. MacLean, and L. M. Osborne. "Perinatal Obsessive-Compulsive Disorder: Epidemiology, Phenomenology, Etiology, and Treatment." Curr Psychiatry Rep 24, no. 4 (2022): 229-37.
- v. Ballestrem, C. L., M. Strauss, and H. Kachele. "Contribution to the Epidemiology of Postnatal Depression in Germany--Implications for the Utilization of Treatment." Arch Womens Ment Health 8, no. 1 (2005): 29-35.
- Robert Koch-Institut. "Depressive Symptoms in a European Comparison – Results from the European Health Interview Survey (Ehis) 2." Journal of Health Monitoring 4, no. 4 (2019): XX--XX.
- Galea, S., and M. Tracy. "Participation Rates in Epidemiologic Studies." Ann Epidemiol 17, no. 9 (2007): 643-53. [CrossRef]
- Jacobsen, T. N., E. A. Nohr, and M. Frydenberg. "Selection by Socioeconomic Factors into the Danish National Birth Cohort." Eur J Epidemiol 25, no. 5 (2010): 349-55.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).