1. Introduction
The elderly population of the world is rapidly expanding [
1]. According to WHO, one in six individuals on the planet will be 60 years of age or older by 2030 [
2]. At this point, there will be 1.4 billion people over the age of 60, up from 1 billion in 2020. The number of individuals in the world who are 60 or older is expected to double (to 2.1 billion) by 2050. It is anticipated that between 2020 and 2050, the number of people 80 years of age or older will triple, reaching 426 million [
2]. Furthermore, the development of multimorbidity is significantly influenced by ageing, with a frequency in older adults ranging from 55 to 98% [
3]. Multimorbidity is known as the existence of two or more chronic diseases in one person. Because of its negative effects on health and society, multimorbidity is becoming a major healthcare concern [
4,
5]. Approximately, 45% of Americans, or 133 million people, have at least one chronic illness, and the percentage is rising [
6]. Hospitalization, long-term impairment, lower quality of life, and even mortality can result from chronic diseases, which include cancer, diabetes, hypertension, stroke, heart disease, respiratory disorders, obesity, arthritis, and oral diseases [
7].
Tooth loss is a significant global public health issue [
8]. Based on the CDC, one in six persons aged 65 years and older in the USA are edentulous [
9]. Moreover, in the United States, half of all individuals between the ages of 20 and 64 have experienced at least one permanent tooth loss [
10]. Furthermore, the National Health and Nutrition Examination Survey (NHANES) data from 2009 to 2014 revealed that 6.2 million Americans aged 50 and older, 17.6% of adults aged 65 and older, and 22.5% of those aged 75 and older in the US were affected by edentulism [
11].
The dental and medical fields have mostly acknowledged the oral-systemic relationship in recent years. New research has been conducted and continues to demonstrate the relationship between dental and systemic health. For instance, the primary cause of tooth loss, periodontal disease was linked, via the inflammatory process, to several systemic disorders [12-14].
Furthermore, in terms of individual chronic conditions, tooth loss was associated with certain chronic conditions such as diabetes [
15] and cardiovascular diseases [
16]. While in terms of multimorbidity, Felton [
17], found a significant association between tooth loss and multimorbidity.
Besides multimorbidity, tooth loss negatively affects people's dietary intake. Being edentate was significantly associated with lower consumption of dietary fibre, vitamin C, and other nutrients [
18,
19]. Moreover, two studies found associations between tooth loss, obesity, and malnutrition [
20,
21]. On the other hand, inadequate nutrition is an important determinant of multimorbidity [
22,
23].
People who has lost all of their teeth may experience low self-esteem and social isolation as a result of their inability to communicate and engage with others in daily life [
24]. Common risk factors, such as dietary deficiencies, alcoholism, and smoking, which are all connected to low socioeconomic status, may have an impact on the association between tooth loss and multimorbidity [
25,
26].
The current study aims to examine the relationship among edentulism, nutritional intake, and the progress of multimorbidity among older Americans.
Methods
2. Study Design
Longitudinal data from the Health and Retirement Study (HRS) were used in this study. With response rates consistently above 80%, data were collected every two years since 1992. Participants received study materials prior to each interview. Oral consent was obtained right before each interview, and participants were given a confidentiality statement. Since 2006, half of the panel respondents have additionally participated in an upgraded face-to-face interview. The current work did not require ethical approval because the HRS data are publicly accessible and do not contain personal information.
2.1. Study Sample
Adult Americans 50 years of age and older made up the study sample [
27]. Since the introduction of the oral health question started in 2006, data from that year were included in the current analysis. Those over 50 who responded to the oral health question, took part in the 2013 nutritional module were among the inclusion requirements. Individuals who lacked complete data for any of the characteristics covered in each wave were not included in the analysis.
2.2. Study Variables
The predictor variables for this study were divided into three main categories: demographic factors, health-related behaviours, and socioeconomic factors. The demographic variables were gender (Male, Female) and age. Whereas socioeconomic position (SEP) was indicated by total wealth and its measures were reported in nominal dollars and calculated as the sum of the appropriate wealth components less debt. In this analysis we used wealth in 2006 and categorised it into quartiles (highest, second highest, second lowest, and lowest).
Smoking in 2006 was selected as a behavioural factor, and it was categorized as a dichotomous variable (never/former smoker and current smoker).
Complete tooth loss (edentulism) in 2006 was indicated by answering “yes” to the question “Have you lost all your upper and lower natural permanent teeth?”.
Health and Retirement Study included one file where individual nutritional intake was calculated in 2013. This wave is called Health Care and Nutrition Study (HCNS) 2013. Individual intake was calculated according to the values of Nutrients Recommendations: Dietary Reference Intake (DRI). According to the available nutrients in HRS, only 10 out of 13 nutrients of US Food and Drug Administration were chosen, Protein, Vitamin C, Vitamin D, Vitamin B12, Vitamin E, Calcium, Zinc, Polyunsaturated fatty acids, Folate and ß- carotene. These nutrients were calculated based on DRI [
28] as the following:
Protein (men <56 g/day; women <46 g/day), Vitamin C (men 90 mg/day; women 75 mg/day),
Vitamin D, HRS calculated vitamin D, in International Unit which contradict with the US Food and drug administration as they calculated in microgram MCG, and there are two measures for vitamin D according to age, (both 50–70 years, 15µg/day; both >70 years, 20µg/day). Based on this, a convertor was used to accurately measure the values, yielding 15 IU= 600 and 20 IU= 800.Vitamin B12 (<2.4µg/day). Vitamin E (15 mg/day). Zinc (men <11 mg/day; women <8 mg/day). Polyunsaturated fatty acids (men 160 mg, women 90 mg). Folate (<400µg/day), and ß- carotene (3 mg).
Each of these nutrients was coded as 0= inadequate intake or 1= adequate intake and were summed up in one variable, total nutrients, ranging from 0 to 10.
Multimorbidity was indicated by self-reported diagnoses of 5 chronic conditions: diabetes, heart conditions, lung diseases, cancer, and stroke. These conditions were selected because they are highly prevalent among older adults and are classified as major causes of disability and death in USA [
9]. In this analysis, multimorbidity in 2018 was used as a dichotomous variable: 1 or less condition versus 2 or more conditions. Participants with more than 1 chronic condition at baseline (2006) were excluded from the analysis.
The final analysis included data on multimorbidity, tooth loss, nutritional intake, wealth, smoking age and gender. These data were from Health and Retirement Survey, specifically from RAND HRS Longitudinal File 2018 (V1).
This study is human observational and followed properly the STROBE guidelines.
3. Statistical analysis
The incidence of multimorbidity among older Americans aged 50 years and over was included in 2018. Prevalence of edentulism in 2006 and mean of total nutrition (2013) were also included. The analysis was limited to people with complete data, the variable with greatest missing cases was nutrition since it was obtained from one off survey of a subsample of HRS.
First, we assessed the distribution of multimorbidity (2018), tooth loss (2006), total nutrition (2013).
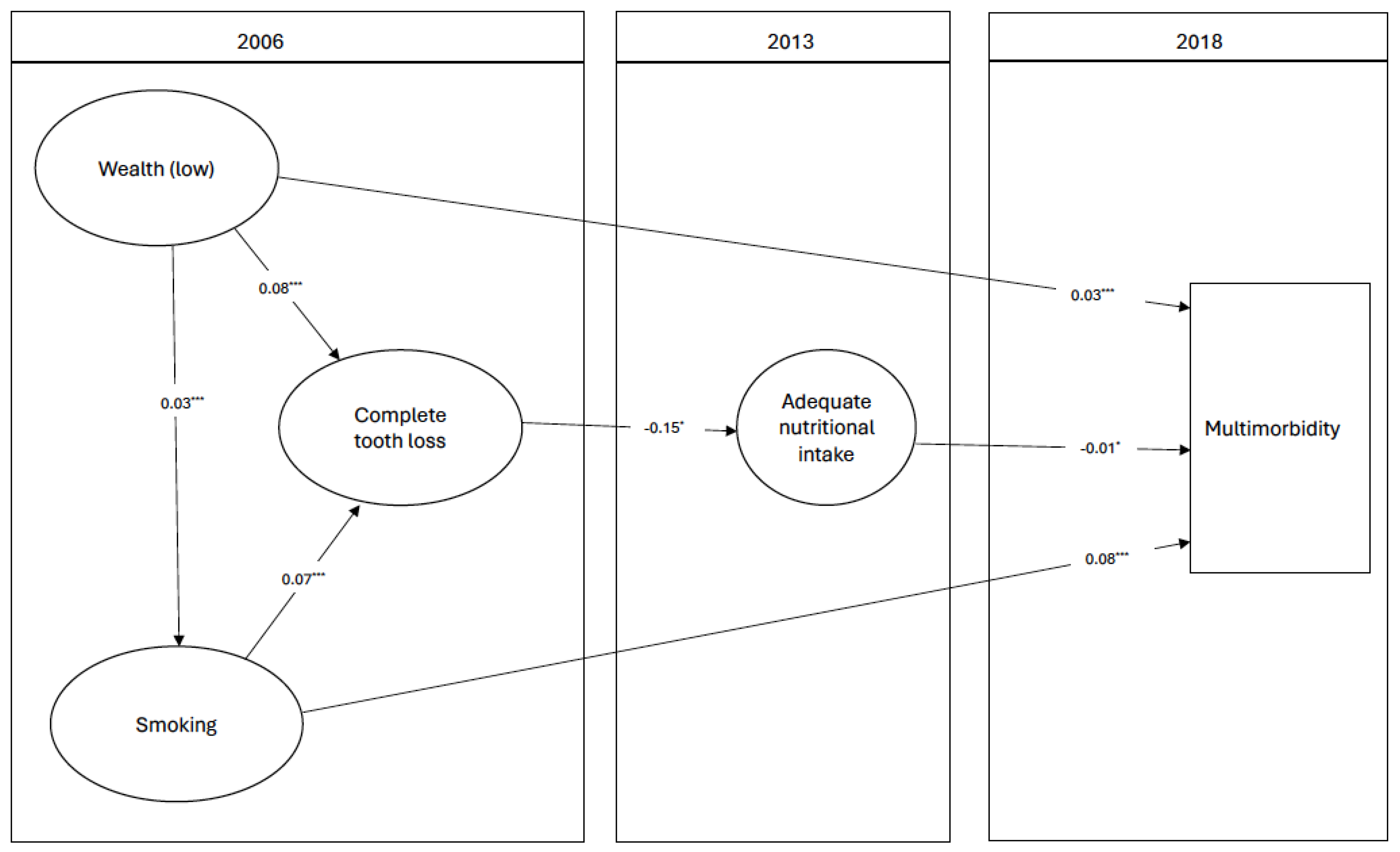
To test the relationship between total tooth loss and multimorbidity through nutritional intake, Structure Equation Modelling (SEM) was constructed. One path analysis diagram was created with multiple adjustments. The following associations were tested: (1) associations of wealth and smoking with tooth loss adjusting for age and gender; (2) association between tooth loss and total nutrition adjusting for age and gender; (3) association between total nutrition and multimorbidity adjusting for smoking, wealth and age. All analyses were conducted using Stata 14.2
4. Results
The analysis included 3,463 participants. Incidence of multimorbidity in 2018 was 24.07%. Percentage of participants with complete tooth loss in 2006 was 10.11%. The mean of total nutrition in 2013 was 4.50 (95%CI:4.43, 4.55) (
Table 1).
Figure 1 demonstrates the direction of association between tooth loss in 2006, total nutrition in 2013 and multimorbidity in 2018. Those who lost all their teeth in 2006 had a significantly lower score of adequate nutrition in 2013 {estimate -0.15(95% CI: -0.30, - 0.01)}. A negative association was observed between adequate nutrition in 2013 and multimorbidity {estimate -0.008 (95%CI: -0.01, -0.002)} after accounting for smoking and wealth. (
Table 2).
5. Discussion
In this study, we examined the relationship between edentulism and progress of multimorbidity among older adults in the United States using longitudinal data from the HRS and examined the role of Nutritional intake in this relation. The analysis using SEM demonstrated that nutritional intake is in the pathway between edentulism and multimorbidity. Tooth loss in 2006 was negatively associated with adequate total nutritional in 2013 which in turn was negatively associated with incidence of multimorbidity in 2018. These results were consistent with previous studies that reported that tooth loss was associated with declines in fruits, vegetable, and fibres consumption which in turn influenced the risk of chronic conditions [
29,
30].
Tooth loss affects chewing ability and limits selection of food items which impacts adequate intake of essential nutrients [
18,
19]. For example, older adults with fewer teeth or no teeth will have difficulties eating fresh fruits and vegetables and could consume other unhealthy food [
18,
31]. While this relationship was always clear when tooth loss was indicated by number of teeth or functional dentition, it was less clear when complete edentulism was used, however, this was mainly attributed to the lack of longitudinal studies [
21]. The current analysis found a longitudinal association between complete tooth loss and inadequate nutritional intake. On the other hand, there are evidence of a consistent relationship between inadequate nutrition and higher incidence of multimorbidity and comorbidity [
22,
23]. The impact of nutrition on the onset and management of chronic illnesses has been widely acknowledged [
23], which led to recommendations for food consumption based on daily reference intakes for particular macro- and micronutrients [
22]. The findings of the current analysis highlight the role of adequate nutritional intake in the progress of multimorbidity even after accounting for other behavioural and socioeconomic factors.
In this study we did not test the direct relationship between tooth loss in 2006 and incidence multimorbidity in 2018 as the focus of the research question was on demonstrating the indirect relation through inadequate nutritional intake. However, there are several studies that demonstrated association between tooth loss and multimorbidity [
32], and between tooth loss and individual chronic conditions [
16,
20,
33,
34].
While the nutritional pathway between tooth loss and multimorbidity was tested in this study, there are other pathways for this relationship, including a psychological pathway due to the impact of tooth loss on talking and socialising with others that could lead to social isolation [
35] that impacts multimorbidity. Adverse socioeconomic factors and associated risk behaviours could also have a common impact on tooth loss and multimorbidity [
11,
36].
The strength of this study is in using longitudinal data of older American adults to assess the relationship between tooth loss, nutritional intake and multimorbidity, and in using Structural Equation Modelling to demonstrate the nutritional pathway. The nutritional intake variable was based on recommendation for essential nutrients intake which affect chronic conditions. The focus on progress of multimorbidity and tooth loss, both common public health problems in the ageing population is another strength of this analysis. There are few limitations worth mentioning. First, we used self-reported doctor diagnoses of chronic conditions, which could be subjected to recall bias. However, including clinical assessments is very difficult and expensive in longitudinal studies of this size. Oral health was limited to self-reported complete tooth loss, which is also subjected to recall bias. A better indicator could have been number of teeth or functional dentition.
The findings of this study on the impact of tooth loss on nutritional intake and progress of multimorbidity, highlight the importance of identifying health promotion interventions to improve oral health and nutritional intake to halt the progress of multimorbidity among older adults. Future research should include intervention study design to examine the relationship[ demonstrated in this study.
This study demonstrated a longitudinal association between tooth loss and inadequate nutritional intake and between nutritional intake and progress of multimorbidity, using national longitudinal survey of American older adults. The study highlights the importance of both oral health and nutritional intake in the progress of multimorbidity among older American adults.
Author Contributions
R.M. Conception of the idea, data management, data analysis, interpretation of results and writing manuscript draft, W.S. conception of the idea, data analysis, writing final manuscript, T.N. conception of the idea, writing final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research did not receive any fund.
Conflicts of Interest
All authors declare no conflict of interest.
References
- Sanderson, W.C.; Scherbov, S. Measuring the speed of aging across population subgroups. PLoS One 2014, 9, e96289. [Google Scholar]
- WHO. Ageing and health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 28 November 2023).
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: a systematic review of the literature. Ageing research reviews 2011, 10, 430–439. [Google Scholar] [CrossRef]
- Le Reste, J.Y.; Nabbe, P.; Manceau, B.; Lygidakis, C.; Doerr, C.; Lingner, H.; Czachowski, S.; Munoz, M.; Argyriadou, S.; Claveria, A. The European General Practice Research Network presents a comprehensive definition of multimorbidity in family medicine and long term care, following a systematic review of relevant literature. Journal of the American Medical Directors Association 2013, 14, 319–325. [Google Scholar] [CrossRef]
- Sevostyanova, E.; YuA, N.; VYа, P. The problem of multimorbidity in a modern therapeutic clinic. Bulletin Of Siberian Medicine 2022, 21, 162–170. [Google Scholar] [CrossRef]
- Tinker, A. How to improve patient outcomes for chronic diseases and comorbidities. Health Catalyst 2017. [Google Scholar]
- Comlossy, M. Chronic disease prevention and management. Proceedings of National Conference of State Legislatures; pp. 1–16.
- Bernabe, E.; Marcenes, W.; Hernandez, C.R.; Bailey, J.; Abreu, L.G.; Alipour, V.; Amini, S.; Arabloo, J.; Arefi, Z.; Arora, A. , et al. Global, Regional, and National Levels and Trends in Burden of Oral Conditions from 1990 to 2017: A Systematic Analysis for the Global Burden of Disease 2017 Study. J Dent Res 2020, 99, 362–373. [Google Scholar] [CrossRef]
- CDC. About Chronic Diseases. 03 February. Available online: https://www.cdc.gov/chronicdisease/about/index.htm (accessed on 3 February 2024).
- NIH. Tooth Loss in Adults (Age 20 to 64). Available online: https://www.nidcr.nih.gov/research/data-statistics/tooth-loss/adults#:~:text=2.2%25%20of%20adults%2020%20to%2064%20years%20have,are%20more%20likely%20to%20have%20no%20remaining%20teeth (accessed on 29 November 2023).
- Dye, B.A.; Weatherspoon, D.J.; Lopez Mitnik, G. Tooth loss among older adults according to poverty status in the United States from 1999 through 2004 and 2009 through 2014. J Am Dent Assoc 2019, 150, 9–23. [Google Scholar] [CrossRef]
- Genco, R.J.; Sanz, M. Clinical and public health implications of periodontal and systemic diseases: An overview. Periodontology 2000 2020, 83, 7–13. [Google Scholar] [CrossRef]
- Kim, J.; Amar, S. Periodontal disease and systemic conditions: a bidirectional relationship. Odontology 2006, 94, 10–21. [Google Scholar] [CrossRef]
- Linden, G.J.; Lyons, A.; Scannapieco, F.A. Periodontal systemic associations: review of the evidence. Journal of periodontology 2013, 84, S8–S19. [Google Scholar]
- Ahmadinia, A.R.; Rahebi, D.; Mohammadi, M.; Ghelichi-Ghojogh, M.; Jafari, A.; Esmaielzadeh, F.; Rajabi, A. Association between type 2 diabetes (T2D) and tooth loss: a systematic review and meta-analysis. BMC Endocrine Disorders 2022, 22, 100. [Google Scholar] [CrossRef]
- Matsuyama, Y.; Jürges, H.; Listl, S. Causal Effect of Tooth Loss on Cardiovascular Diseases. J Dent Res 2023, 102, 37–44. [Google Scholar] [CrossRef]
- Felton, D.A. Complete Edentulism and Comorbid Diseases: An Update. J Prosthodont 2016, 25, 5–20. [Google Scholar] [CrossRef]
- Nowjack-Raymer, R.E.; Sheiham, A. Numbers of natural teeth, diet, and nutritional status in US adults. J Dent Res 2007, 86, 1171–1175. [Google Scholar] [CrossRef]
- Zhu, Y.; Hollis, J.H. Tooth loss and its association with dietary intake and diet quality in American adults. J Dent 2014, 42, 1428–1435. [Google Scholar] [CrossRef]
- Nascimento, G.G.; Leite, F.R.; Conceição, D.A.; Ferrúa, C.P.; Singh, A.; Demarco, F.F. Is there a relationship between obesity and tooth loss and edentulism? A systematic review and meta-analysis. Obes Rev 2016, 17, 587–598. [Google Scholar] [CrossRef]
- Toniazzo, M.P.; Amorim, P.S.; Muniz, F.; Weidlich, P. Relationship of nutritional status and oral health in elderly: Systematic review with meta-analysis. Clin Nutr 2018, 37, 824–830. [Google Scholar] [CrossRef]
- Koren-Hakim, T.; Weiss, A.; Hershkovitz, A.; Otzrateni, I.; Grosman, B.; Frishman, S.; Salai, M.; Beloosesky, Y. The relationship between nutritional status of hip fracture operated elderly patients and their functioning, comorbidity and outcome. Clinical Nutrition 2012, 31, 917–921. [Google Scholar] [CrossRef]
- Ruel, G.; Shi, Z.; Zhen, S.; Zuo, H.; Kröger, E.; Sirois, C.; Lévesque, J.-F.; Taylor, A.W. Association between nutrition and the evolution of multimorbidity: The importance of fruits and vegetables and whole grain products. Clinical Nutrition 2014, 33, 513–520. [Google Scholar] [CrossRef]
- Gerritsen, A.E.; Allen, P.F.; Witter, D.J.; Bronkhorst, E.M.; Creugers, N.H.J. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health and Quality of Life Outcomes 2010, 8, 126. [Google Scholar] [CrossRef]
- Seerig, L.M.; Nascimento, G.G.; Peres, M.A.; Horta, B.L.; Demarco, F.F. Tooth loss in adults and income: Systematic review and meta-analysis. J Dent 2015, 43, 1051–1059. [Google Scholar] [CrossRef]
- Yang, H.; Han, R.; Wang, Z. Socioeconomics, health-related factors, and tooth loss among the population aged over 80 years in China. BMC Public Health 2022, 22, 444. [Google Scholar] [CrossRef]
- Sonnega, A.; Faul, J.D.; Ofstedal, M.B.; Langa, K.M.; Phillips, J.W.; Weir, D.R. Cohort Profile: the Health and Retirement Study (HRS). Int J Epidemiol 2014, 43, 576–585. [Google Scholar] [CrossRef]
- National Institutes of Health. Nutrient Recommendations: Dietary Reference Intakes (DRI). Available online: https://ods.od.nih.gov/HealthInformation/Dietary_Reference_Intakes.aspx (accessed on 13 May 2023).
- Hung, H.C.; Colditz, G.; Joshipura, K.J. The association between tooth loss and the self-reported intake of selected CVD-related nutrients and foods among US women. Community Dent Oral Epidemiol 2005, 33, 167–173. [Google Scholar] [CrossRef]
- Österberg, T.; Dey, D.K.; Sundh, V.; Carlsson, G.E.; Jansson, J.-O.; Mellström, D. Edentulism associated with obesity: a study of four national surveys of 16 416 Swedes aged 55–84 years. Acta Odontologica Scandinavica 2010, 68, 360–367. [Google Scholar] [CrossRef]
- Chari, M.; Sabbah, W. The relationships among consumption of fruits, tooth loss and obesity. Community Dent Health 2018, 35, 148–152. [Google Scholar] [CrossRef]
- Hag Mohamed, S.; Sabbah, W. Is tooth loss associated with multiple chronic conditions? Acta Odontol Scand 2023, 81, 443–448. [Google Scholar] [CrossRef]
- Al-Maweri, S.A.; Ibraheem, W.I.; Al-Ak'hali, M.S.; Shamala, A.; Halboub, E.; Alhajj, M.N. Association of periodontitis and tooth loss with liver cancer: A systematic review. Crit Rev Oncol Hematol 2021, 159, 103221. [Google Scholar] [CrossRef]
- Dioguardi, M.; Gioia, G.D.; Caloro, G.A.; Capocasale, G.; Zhurakivska, K.; Troiano, G.; Russo, L.L.; Muzio, L.L. The Association between Tooth Loss and Alzheimer's Disease: a Systematic Review with Meta-Analysis of Case Control Studies. Dent J (Basel) 2019, 7. [Google Scholar] [CrossRef]
- Kudsi, Z.; Fenlon, M.R.; Johal, A.; Baysan, A. Assessment of Psychological Disturbance in Patients with Tooth Loss: A Systematic Review of Assessment Tools. J Prosthodont 2020, 29, 193–200. [Google Scholar] [CrossRef]
- Mira, R.; Newton, T.; Sabbah, W. Inequalities in the progress of multiple chronic conditions: A systematic review of longitudinal studies. PLoS One 2022, 17, e0263357. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).