1. Introduction
The significance of AI-driven decision-making stems from its capability to transform multiple industries, especially healthcare, finance, and production, by leveraging strong algorithms to analyze huge datasets and extract substantial insights [
1,
2]. AI systems can identify patterns, predict and automate complex activities, boosting the productivity, accuracy, and speed of decision-making processes [
3,
4]. In healthcare, to name but a few, AI-driven decision-making could facilitate disease diagnosis, treatment mechanism personalization, and resource allocation. As well, in business, AI can aid with strategic planning, risk management, and consumer engagement [
5,
6]. AI’s capacity to handle a great deal of data and provide intelligent recommendations not only develop decision results, but also aids businesses to remain competitive, innovate, and navigate the complexities of a progressively data-driven world [
7,
8].
Information systems are involved of hardware, software, data, and human resources to collect, preserve, evaluate, and distribute information within an organization [
9,
10]. These technologies make it simpler to manage, retrieve, and utilize data to assist in decision-making and operations [
11,
12]. HIS usually include EHRs, databases, and software applications that streamline the flow of patient data, allow for greater interaction between healthcare practitioners, and enhance general healthcare service [
13,
14]. Information systems play a significant role in ensuring the accessibility, security, and integrity of information, which leads to better healthcare results, effective management, and medical research advancement [
15,
16].
HIS are critical elements of modern medical systems owing to the fact that they present a systematic and digitized path to manage patient data, health records, and management tasks [
17,
18]. These technologies make medical operations simpler by developing the efficiency of data collection, storage, and retrieval. The incorporation of electronic health records (EHRs) facilitates automated contact between clinicians, making dependable and up-to-date patient information simply available, propelling to more informed and coordinated care [
19,
20]. HIS also help to increase patient security by lowering the possibility of errors associated with physical record-keeping. In addition, they play a functional role in data analytics, guiding healthcare businesses in achieving new insights, optimizing resource allocation, and boosting entire patient care [
21]. As the healthcare environment alters, effective arrangement as well as use of information systems is essential for presenting treatment, optimizing patient results, and advancing clinical studies and development [
22].
AI-driven decision-making in HIS is essential because it provides healthcare providers with tools for evaluating complicated patient data, resulting in more accurate and timely clinical decisions [
23]. Utilizing ML algorithms and predictive analytics, AI could help in early disease detection, treatment modification, and resource allocation. The capability to manage huge volumes of diverse healthcare data enables the rapid discovery of patterns and correlations that would not be apparent using standard approaches, thereby boosting patient outcomes [
24]. AI-powered decision-making enhances operational efficiency by automating regular duties, freeing up healthcare practitioners to focus on more intricate and essential elements of patient care [
25]. Furthermore, it contributes substantially to medical research, healthcare development, and healthcare policy planning, thus developing and improving the whole healthcare ecosystem [
26].
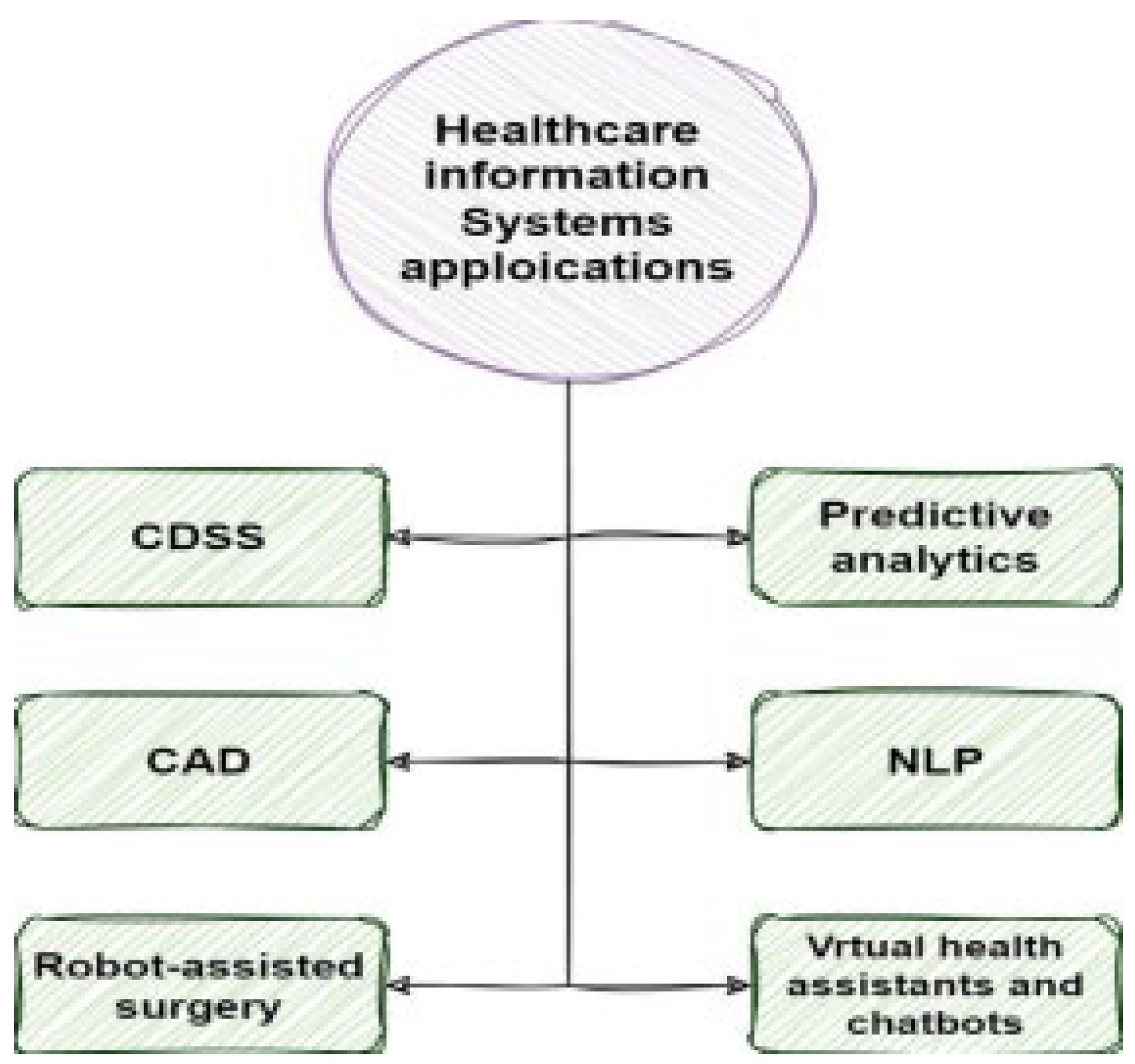
To the best of our knowledge, no previous examination has been undertaken of numerous AI-driven methodologies employed in decision-making inside HIS. However, we studies an in-depth Systematic Literature Review (SLR) to accurately evaluate the different AI-driven methodologies used in decision-making processes inside HIS. Our paper concentrates on using AI-powered approaches as the basis for decision-making in HIS. Our study is remarkable for thoroughly investigating a wide range of successful AI-driven decision-making procedures used in HIS. Our work uses an SLR to analyze, integrate, and assess solutions provided in linked studies. In addition, we divided HIS into six categories: CDSS, predictive analytics, NLP, CAD, virtual health assistants (VHAs), and chatbots. Every group has been extensively investigated, with an emphasis on advantages, limitations, simulation environment, dataset, and the AI-powered technique used in applications. Our research focuses on the methodologies and applications of AI-driven decision-making in HIS, as well as prospective approaches for usage in medical and health prediction systems. Furthermore, we explored potential tasks that might demand attention in future research. Therefore, this paper’s contributions are:
Describing the current challenges with AI-driven decision-making in HIS.
Undertaking studies regarding AI-powered decision-making in HIS.
Evaluating specific AI-driven methodologies for advantages, drawbacks, datasets, and simulations.
Highlighting important features of particular methodologies for subsequent research.
Investigating research approaches based on AI.
The partitioning below forms the study’s foundation. The following section goes deeply into the survey articles that are relevant to AI-powered techniques employed in healthcare information system decision making. The third section discusses the process of research and the article selection procedure. Part 4 discusses the publications chosen for investigation and evaluation. Section 5 expands on the comparison and rationale of several cutting-edge studies. Finally, in Part 6, the rest of the open issues are addressed, and the implications are explained in the last part.
2. Related Works
After understanding the essential ideas of AI-driven decision-making in HIS, we will examine multiple examples related to past studies and compare them to our study. In this regard, Wang, Zhang [
27] systematically reviewed the human-centered design and analysis aspects of AI-empowered CDSS. This research, which concentrated on the convergence of AI and healthcare, looked at the techniques, systems, and results of studies on the development and evaluation of CDSS that highlight human elements. It looked at how these systems are designed to meet user demands, integrate workflows, and provide a total user experience in healthcare contexts. By integrating existing literature, the paper oriented to present a comprehensive overview of standards, issues, and opportunities for developing AI-driven clinical decision support. Also, Moazemi, Vahdati [
28] conducted a systematic review emphasizing on the application of AI in clinical decision support for monitoring patients within cardiovascular Intensive Care Units (ICUs). The study’s purpose was to undertake a thorough review of the current literature on AI-powered systems aimed at improving decision-making in cardiology intensive care units. Their holistic study explored the methods, technologies, and results of AI applications, proposing a vision on how these techniques aid in the tracking and controling patients with cardiovascular illnesses. Moreover, Loftus, Shickel [
29] explored the application of AI-enabled decision support in the domain of nephrology. Their paper, which structurred to develop medical decision-making via the application of recent technology, looked at existing study, techniques, and results for AI usages in nephrology. This study presnted vision on how AI algorithms and decision support systems can enable the recognition, control, and treatment of kidney-related illness. Additionally, Xu, Xie [
30] conducted a comprehensive research of the interpretability of CDSS based on AI, examining both technological and medical perspectives. Their paper explored the present literature to holistically study the methodologies, tools, and frameworks used to develop the interpretability of AI-driven CDSS in the field of healthcare. By gathering data from several studies, the paper enabled to address challenges and developed transparency, explainability, and comprehension of AI-based decision support systems. Furthermore, Lau, Nandy [
31] conducted an SLR to investigate the prospect of AI-driven technologies for speeding the accomplishment of the United Nations Sustainable Development Goals (SDGs), especially in the field of women’s healthcare. The analysis looked at a number of scholarly publications, research papers, and related material to see if AI may help solve women’s medical concerns while also advancing the UN SDG goals. As well, Marino, Putignano [
32] offered a survey of the innovative state of research and developments in the application of AI technologies to investigate and understand factors influencing human longevity. It investigated how AI-driven techniques may help identify biomarkers, forecast health directions, and design tailored therapies to promote lifespan. By combining findings from current literature and studies, the publication presented a basic knowledge of the role AI serves in promoting lifetime research, which is beneficial for scientists, healthcare practitioners, and scientists in the area.
Table 1 shows specification of these related works.
3. Methodology of Research
We examined major works that investigated AI-driven decision-making in HIS. This section examines AI-driven decision-making through the prism of SLR methodology. The SLR process entails a thorough examination of all research performed on a certain issue. This part closes with an in-depth look into AI-driven decision-making methodologies in the HIS setting. Likewise, the reliability of the research selection procedures is investigated. The next subsections include thorough information about the research methodology, including selection criteria and study questions.
3.1. Formalization of Question
The main goals of our study are to find, analyze, and compare significant articles in the subject of managing AI-driven decision-making. To accomplish these objectives, a SLR will be applied to comprehensively investigate the components and characteristics of the methodologies employed in this context. Furthermore, an SLR aids in acquiring a thorough awareness of the primary issues and limitations involved with this field. The next paragraph presents some research questions:
Research Question 1: How can AI-driven decision-making processes in the field of HIS be classified? The answer to this question is in Part 5.
Research Question 2: What approaches do scholars use to do their research? Parts 5.1 through 5.7 answer this question.
Research Question 3: What parameters received the greatest attention in the papers? What is the most common AI-driven decision-making methodologies used in HIS? The answer to this question is found in section 6.
Research Question 4: What untapped opportunities exist in this area? section 7 provides the answer to this question.
3.2. The Procedure of Paper Exploration
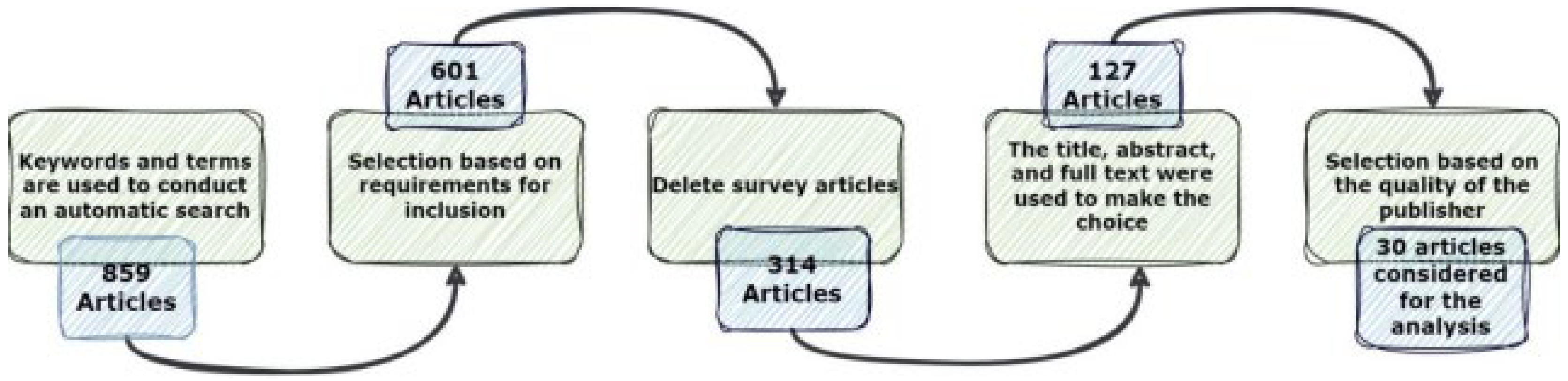
The present examination’s search and selection approaches are separated into four distinct phases, as shown in
Figure 1. At first, a thorough list of keywords and phrases was utilized to search many sources, as shown in
Table 2. Informative resources were acquired from electronic databases, including chapters, journals, technical studies, conference papers, notes, and special issues, totaling 859 articles, as illustrated in
Figure 2. These papers were then rigorously reviewed using a predefined set of criteria, and only those that met the standards were chosen for further investigation. The distribution of publications during these phases is shown below, with 601 articles left after the first stage.
The titles and abstracts of the selected publications were then painstakingly scrutinized, with an emphasis on their discussion, methodology, analysis, and conclusions to guarantee conformity with the study’s aims. This filtering lowered the number of publications to 314. The objective was to discover works that fit the study’s established criteria. After careful assessment, 127 papers were chosen for more research.
Figure 3 depicts the last stage, which included reducing the number of articles to 30 for the study’s final phase.
4. AI-Driven Decision-Making Techniques in HIS
AI-driven decision-making techniques in HIS apply advanced algorithms, ML, and AI to enhance the clinical decision support process. These technologies have an extensive variety of applications, involving predictive analytics, NLP, and ML models that evaluate massive datasets to find patterns, predict results for patients, and assist physicians in making informed decisions. AI-driven decision-making improves diagnostic accuracy, treatment planning, and individualized patient care. These strategies are also important in automating regular processes, increasing productivity, and promoting evidence-based treatment in medical facilities. Organizations that incorporate AI into HIS expect to apply data-driven insights to enhance results for patients, speed up workflows, and, ultimately, enhance general treatment quality.
Figure 4 displays our taxonomy of several HIS that make AI-based decisions. In the subsequent parts we dwell deep in each group comprehensively.
4.1. CDSS
In the context of AI-driven decision-making within HIS, CDSS play a pivotal role in enhancing the quality of healthcare delivery. Considering that, Comito, Falcone [
33] proposed an approach to improve disease diagnosis through AI-driven CDSS. The main emphasis of this paper is on using patient similarities to improve diagnosis accuracy. The authors demonstrated a method that employs AI to identify patterns and similarities across patients, allowing healthcare personnel to make more informed and precise diagnoses. Also, Vasey, Nagendran [
34] introduced the DECIDE-AI reporting guideline, designed for the early-stage clinical evaluation of DSS powered by AI. The recommendation sought to establish a consistent structure for investigators and developers to publicly report on the early phases of AI-driven DSS development and assessment. DECIDE-AI stressed the need of thorough and detailed reporting by addressing essential variables such system characteristics, training data, algorithm specifications, and outcomes indicators. In addition, Choudhury [
35] created the DECIDE-AI reporting standard, which is sought to the early-stage clinical assessment of DSS powered by AI. This article presented a uniform methodology for academics to openly report on the early phases of AI-driven DSS improvement and evaluation. DECIDE-AI reflected the demand of holistic and succinct reporting, emphasizing on system features, training data, algorithm specifications, and efficiency standards. As well, Liu, Barreto [
36] delve in the discrepancy among doctors’ beliefs and actual adoption of CDSS utilizing AI for vancomycin dose. It examined the items that propel to the difference among physicians’ intrinsic perception of CDSS and their purpose to apply AI-powered device for definite tasks, like dose selection. Their study concentrated on facets like safety, application, conceived relevance to clinical treatment, and the efficiency of the installed AI system. And, Amann, Blasimme [
37] proposed a comprehensive exploration of the challenge of explainability in AI usability for healthcare. Their research underscored the need of making AI systems understandable and interpretable to multiple stakeholders, consisting healthcare provider, patients, and lawmakers. It solved the challenges of gaining explainability in complicated AI models and proposed interdisciplinary techniaues that consisted expertise from computer science, healthcare, ethics, and regulations.
Table 3 indicates specifications of studies investigated CDSS making AI-driven decisions.
4.2. Predictive Analytics
Predictive analytics is significance in AI-driven decision making in HIS owing to the fact that it evaluates large amounts of healthcare information applying complicated algorithms and ML methods. By the similar token, Elvas, Nunes [
38] studied the application of AI-driven decision support for early detection of cardiac events, with a specific stress on disclosing patterns and predicting myocardial ischemia. It resolved the issues of gaining explainability in complicated AI models and proposed interdisciplinary strategies that consisted profession from computer science, healthcare, ethics, and regulations. Additionally, Rehman, Farrakh [
39] emphasizing on developing CDSS by incorporating Explainable AI (XAI) for better disease forecasting in healthcare. Their paper applied XAI to enhance transparency and interpretability in the decision-making procedure of AI models, making anticipations more understandable to healthcare experts. This mechanism is pivotal for instilling safety and boosting the adoption of AI-powered disease detection systems in healthcare infrastructure. Beside, Chen, Lim [
40] presented an AI-based human-centered decision support system with a specific utilization to predictive maintenance in asset management during pandemics. Their method used developed AI methodologies to enhance human decision-making in investment management, with a considerable highlights on the challenges and concerns increased by the challengable consitions of a pandemic. Their study ivestigated how AI increased predictive maintenance techniques, enabling for proactive and effective asset management whilest regarding human-centric decision-making. Also, Wang, Zhao [
41] offered a management decision support system based on an integrated structure of AI and big data analytics. The application of AI in maintenance anticipating improved asset performance and reliability by presenting a total method to decision support that considers the altering issues provided by the epidemic. Their techniques highlighted the incorporation of AI algorithms and complex analytics mechanisms for deriving related patterns and trends from large datasets. Moreover, Hasan, Dhawan [
42] used a data analytics and knowledge management strategy for COVID-19 prediction and control. It needed the use of advanced data analytics tools to evaluate numerous datasets related to the COVID-19 pandemic. The objective of this paper is to develop prediction models that can estimate the virus’s spread, examine its impacts, and assist in implementing effective control measures. Furthermore, their report stressed the use of knowledge management systems to organize, exchange, and communicate crucial information on the epidemic.
Table 4 demonstrates specifications of studies investigated predictive analytics applying AI-driven decision-making.
4.3. NLP
Based on a comprehensive analysis, NLP is critical in AI-driven decision-making in HIS. NLP, a subfdomain of AI, studies the interaction among computers and human language. This capacity is crucial for making sense of the huge volume of textual data proposed in medical facilities. So, Afshar, Adelaine [
43] outlined the implementation of a real-time NLP and deep learning (DL) CDSS within the EHR environment. The research, which focused on an opioid abuse screener for hospitalized individuals, described the creation and implementation of a full pipeline. This included combining NLP approaches for extracting and analyzing relevant medical data in real time with DL technologies to establish a doable opioid abuse screening device. Besides, Elkin, Mullin [
44] studied the stilization of AI and NLP to integrate structured and free-text data from EHRs for the identiication of nonvalvular atrial fibrillation (NVAF), to decreasing strokes and mortality. An analysis and case-control evaluation were used in the inquiry to define the success of an AI-driven method. This offered technique developed NVAF detection by incorporating structured and unstructured data in EHRs, presenting a more holistic image of patient health. And, Stewart, Chaturvedi [
45] explored the value of NLP in terms of patient results and real-world evidence. It concentrated on how NLP, a branch of AI, is employed to derive valuable insights from unstructured text data in healthcare settings like clinical notes, reports, and patient charts. Their research underlined the significance of natural language processing (NLP) in transforming unstructured data into structured data, enabling extensive evaluation and interpretation. In addition, Joyce, Markossian [
46] presented a process of analyzing a clinical decision support device that utilizes NLP to analyze hospitalized patients for challenging drug application. Their research introduced a quasi-experimental method to specifying the tool’s application in identifying and screening persons with drug use issues while hospitalized. The NLP-based tool evaluated unstructured clinical text data, like EHRs, to automatically diagnose and recognize cases of dangerous drug use. Barrera, Torres [
47] introduced a recommender system designed for occupational hygiene services, employing NLP techniques. The system used NLP to evaluate and comprehend textual data relating to occupational hygiene, allowing it to offer appropriate services. The recommender system used textual information to improve its reliability and effectiveness of proposing occupational hygiene treatments based on particular demands.
Table 3 shows specifications of studies investigated NLP applications that use AI-driven decision-making.
4.4. CAD
CAD is critical in AI-driven decision-making HIS because it uses advanced algorithms and ML approaches to help medical personnel comprehend and analyze health information. Considering that, Creswell, Vo [
48] investigated the initial user perspectives regarding the application of CAD software for the interpretation of chest X-ray images, with the overarching objective of improving access to and the quality of care for individuals with a focus on tuberculosis. This research investigated the early experiences and views of users who used the CAD system for chest X-ray interpretation, with the goal of determining its potential for improving diagnostic accuracy and optimizing healthcare delivery for TB patients. Moreover, Tran, Sadeghi-Naini [
49] explored the application of AI in computational radiology for breast cancer screening and diagnosis. This work emphasized the application of AI algorithms and investigates the feasibility of computational techniques to enhance the reliability and effectiveness of breast cancer detection using radiological imaging. Their paper employed powerful ML and image analysis methods to enhance radiologists’ diagnostic capabilities and accelerate the screening procedure. As well, Ibrahim, Kibarer [
50] concentrated on the CAD of tuberculosis using a incorporation of microbiological and radiographic images. This research examined the integration of computational methods for TB identification, applyig both microbiological and radiographic imaging data. Their research investigated the probability of CAD techniques to develop the accuracy and effectiveness of TB recognition. Their research applied modern image processing technologies to enable early TB recognition, which is specially significant for optimal disease therapy. Furthermore, Shukla, Zakariah [
51] proposed an AI-driven method for liver cancer screening and prediction, using a Cascaded Fully Convolutional Neural Network (C-FCNN). This paper emphasize on employing complicated DL algorithms to enhance the reliability and efficiency of liver cancer diagnosis. Their propsoed mechanism, which used a cascaded design, developed forecasting sensitivity and specificity by hierarchically analyzing medical imaging data linked to liver cancer. And, Khanna, Agarwal [
52] developed two strong automated CAD prediction models for the early identification of COVID-19 infection from chest X-ray images, with the goal of matching the performance of professional radiologists. These systems, designed for early detection, employed strong computational algorithms to assess chest X-ray images and predict the probability of COVID-19 infection. Their work focused on developing and validating these automated systems with the objective of offering an effective and reliable technique for early diagnosis, which is crucial for timely intervention and management of COVID-19 patients.
Table 6 represents specifications of studies investigated CAD applications applying AI-driven decision-making.
4.5. Robot-Assisted Surgery
Robot-assisted surgery mixed with AI-driven decision-making is a novel strategy for HIS. This integration entails using robotic devices to help surgeons in executing surgeries and using AI algorithms to improve decision-making procedures. In this consideration, Zeineldin, Junger [
53] developed an AI-driven system for neurosurgery, emphasizing a pace onwards minimum invasive robotics. Their endeavor involved creating and deploying an AI system to enhance neurosurgical procedures. The inclusion of AI aimed to provide minimally intrusive robotics technologies, perhaps increasing precision while lowering patient impact. The report discussed the system’s development, operation, and clinical use. Additionally, Parry, Markowitz [
54] investigated patient perspectives on the incorporation of AI in healthcare decision-making through a multi-center comparative study. Their study concentrated on gaining insights directly from patients and investigated attitudes, concerns, and preferences surrounding the usage of AI technology in healthcare. This multi-center strategy included a broad patient group, allowing for a thorough study of differences in attitudes across healthcare environments. Furthermore, Kotha, Viswanath [
55] introduced a healthcare system that leverages AI to enhance the efficiency of emergency medical triage. They used AI-powered robotic technology and developed data processing skills to quickly examine and classify patients depending on the complexity of their medical issues. The solution not only helped healthcare personnel prioritize patients in urgent circumstances, but it also combined with an information system, providing critical medical information for more accurate and rapid decision-making. In addition, Kolbinger, Bodenstedt [
56] explored the integration of AI into robot-assisted oncological surgeries to provide context-aware guidance. In this viability research, the scientists examined the ability of AI algorithms to improve surgical decision-making by examining difficult surgical situations. The system’s goal is to increase the accuracy and productivity of oncological operations by incorporating real-time contextual information. The research used AI to evaluate the possibility of dynamically adjusting surgical assistance during robotic operations, particularly in cancer, where processes can be complex and contain important decision points. As well, Ai, Pan [
57] addressed the development and design of the control system for an innovative minimally invasive surgical robot. The objective of this research was to develop an efficient and reliable control system that would allow the robot to perform surgical tasks successfully and with minimal invasiveness. The paper’s authors highlighted the use of sophisticated control algorithms, sensor systems, and human-machine interfaces to assure the robot’s responsiveness and precision during operations.
Table 7 illustrates specifications of studies investigated robot-assisted surgery applications applying AI-driven decision-making.
4.6. VHAs and Chatbots
Leveraging VHAs and chatbots for AI-driven decision-making in HIS is a game-changing strategy to improving patient care and increasing operational efficiency. In this regard, Wang, Gupta [
58] presented an instrumental case study on SnehAI, an AI chatbot designed to address the sexual and reproductive health needs of young people in India. Their research looked at SnehAI’s creation, deployment, and effect, offering insight on how the AI chatbot works as an important tool for delivering information, guidance, and support to young people dealing with sexual and reproductive health concerns. Besides, Fan, Chao [
59] proposed an empirical investigation into the practical application and effectiveness of self-diagnosis health chatbots in real-world scenarios. The case study delve deep into the use of patterns, user interactions, and results of persons applying health chatbots for self-diagnosis. The authors studied the advantages and limitations of these chatbots in solving users’ health concerns, concentrating on items like accuracy, user happiness, and adherence to offer. And, Chakraborty, Paul [
60] proposed an AI medical chatbot meant to predict infectious diseases. Their paper improved and deployed the chatbot structure, which delve deep in how AI technology can be applied to anticipate the emerge of infectious illnesses. Their method applies ML algorithms and real-time data to establish anticipation, probably presenting a new fashion for early recognition and proactive control of infectious diseases. As well, Esmaeilzadeh, Mirzaei [
61] emphasized on data from an experimental research on how patients perceive interactions among humans and AI in medical area. Their investigation studied patients’ perspective, preferences, and sentiments around the adoption of AI into their healthcare experience. It evaluated several standards, involving reliability, communication function, and total satisfaction with AI-powered connection in healthcare. Additionally, Chow, Wong [
62] argued the analayze and arrangement of an AI-assisted teaching chatbot for radiotherapy. Their study, which applied the IBM Watson Assistant Platform, modeled the chatbot’s framework, operation, and capabilities, underscoring its performance in proposing instructional support for radiotherapy. Their paper explored the utilization of AI technology to develop the chatbot’s capacity to present individualized information, answer questions, and help users comprehend difficult radiation concepts. Using the IBM Watson Assistant Platform, their research described the chatbot’s architecture, operation, and capabilities, stressing its role in providing instructional assistance for radiotherapy.
Table 8 displays specifications of studies investigated virtual health assistant and chatbots applications applying AI-driven decision-making.
5. Results and Comparison
AI in HIS has a remarkable impact on the procedure of decision-making, transforming the business by proposing developed analytical tools and insights. AI applications in clinical decision-making, like ML and predictive analytics, facilitate improving diagnostic accuracy, personalized treatment regimens, and patient management efficiency. These systems can analyze massive information, detect patterns, and present real-time recommendations, aiding healthcare crew to make more informed and timely decisions. AI eases decision-making processes by optimizing resource allocation, boosting efficiencies of workflows, and the system’s general efficiency. Ethical issues are significant, with a stress on patient privacy, data security, and transparency in AI-powered decision-making. While AI has notable potential to significantly influence decision-making in HIS, it needs careful consideration of ethical, regulatory, and social impacts due to take its advantages legally and ethically.
Quantifying the influence of AI in HIS on decision-making entails measuring concrete results and performance measures. In clinical decision-making, studies frequently assess advances in diagnostic accuracy, error reduction, and effectiveness realized with AI applications. Sensitivity, specificity, and predictive values are standard metrics for assessing the quantitative influence on clinical decision quality. Functionally, the adoption of AI in healthcare systems should be quantified through gains in resource usage, processing time decrease, and workflow optimization, each of which contribute to increased decision-making efficiency. Another quantitative component is cost-effectiveness, which is quantified using financial measures to assess the economic benefits of AI adoption. Ethical concerns and regulatory compliance should be measured using quantitative measures such as data security, privacy breaches, and compliance to recognized ethical principles. Overall, a quantitative evaluation of AI in healthcare decision-making requires strong data analysis and quantifiable results to assess the actual advantages and performance improvements gained by introducing AI into information systems.
Qualitatively analyzing the use of AI in HIS for decision-making involves considering non-quantifiable factors that contribute to the efficacy and impact of AI technology. In clinical decision-making, qualitative evaluation concentrates on the considered boost to diagnostic precision, the ability to manage challenging and uncommon circumstances, and healthcare personnel’ overall trust in AI-generated recommendations. Basically, qualitative analyzes can document the user experience by exploring the simplicity of combination, user satisfaction, and the extent to which AI increses decision-making workflow. Ethical concerns consisting transparency, interpretability of AI decisions, and adherence to established ethical norms are frequently assessed qualitatively. Besides, the societal influence of AI on decision-making must be qualitatively evaluated by studying its part in mitigating healthcare inequality, boosting practice availability, and developing patient results. An in-detail qualitative analysis presents crucial vision into the complex facets of AI’s application in healthcare decision-making that go beyond quantitative indicators. Owing to the results, Python is the most significance programming language for replicating proposed techniques in AI-driven decision-making for HIS. Python’s user-friendly library ecosystem, which includes TensorFlow, PyTorch, and scikit-learn, makes it perfect for enhancing sophisticated artificial intelligence systems. Its open-source nature encourages collaboration and code sharing, which promotes rapid growth and innovative thinking. Python’s rich set of data manipulation and analysis capabilities makes it easier to work with a wide range of healthcare datasets, ensuring interoperability with the intricacies of medical information. Additionally, Python’s adaptability to emerging AI methodologies is aided by active community support and regular updates, making it a must-have tool for researchers and practitioners seeking to simulate and deploy advanced AI-driven decision-making applications in HIS.
Figure 5 shows the prevalence of programming languages and libraries used for modeling suggested approaches in this field.
We categorized studied papers into six different groups in terms of applications of HIS which apply AI-driven decision making. In the following subsection we look into these methods holistically.
Figure 6 designates this classification appropriately.
I. CDSS
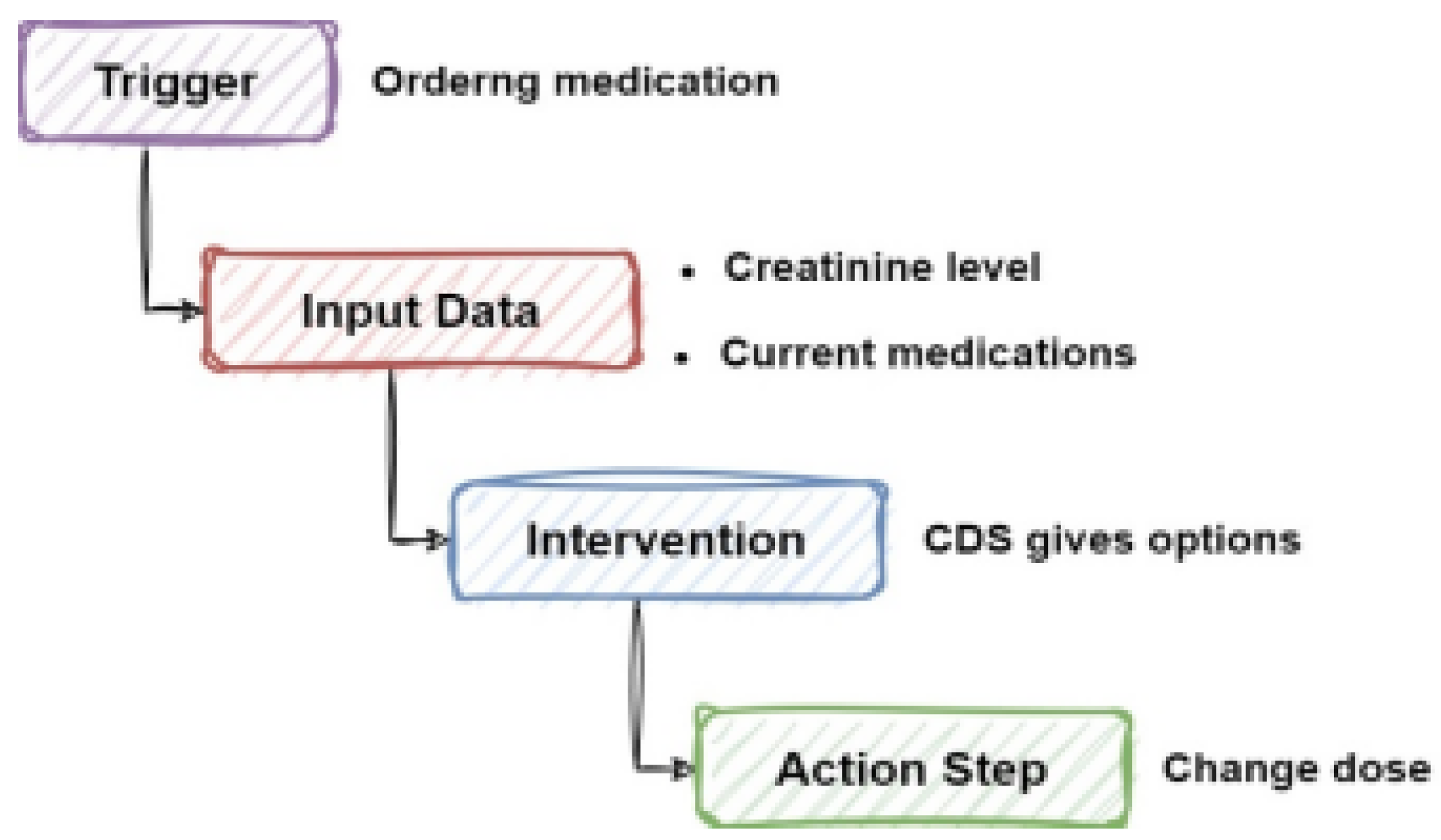
CDSS are fundamental elements of AI-driven decision-making in HIS. They apply strong algorithms and ML strategies to assess large datasets, medical literature, and patient data, presenting real-time insights and support through clinical decision-making procedure. CDSS improves diagnosis accuracy, treatment planning, and patient management by giving evidence-based ideas, warnings, and pertinent information. It also helps physicians navigate complicated medical settings and ensure alignment with recent medical knowledge. Regardless of their benefits to enhancing clinical decision-making accuracy, CDSS in AI-driven decision-making face challenges such as the risk of over-reliance on algorithmic recommendations, issues interpreting contextual nuances throughout medical data, integration issues with existing medical procedures, and ethical concerns about transparency, patient privacy, and bias reduction. Effectively tackling these problems is critical to fulfilling CDSS’s full potential in AI-driven decision-making and allowing its smooth incorporation into HIS, resulting in improved patient care and perform efficiency. CDSS often collects pertinent input data prompted by clinical activities, such as prescription orders, and then provides suggestions suited to specific patient profiles, assisting healthcare workers in making informed decisions and maximizing patient care.
Figure 7 displays the CDSS sequence with AI-driven decision-making.
II. Predictive Analytics
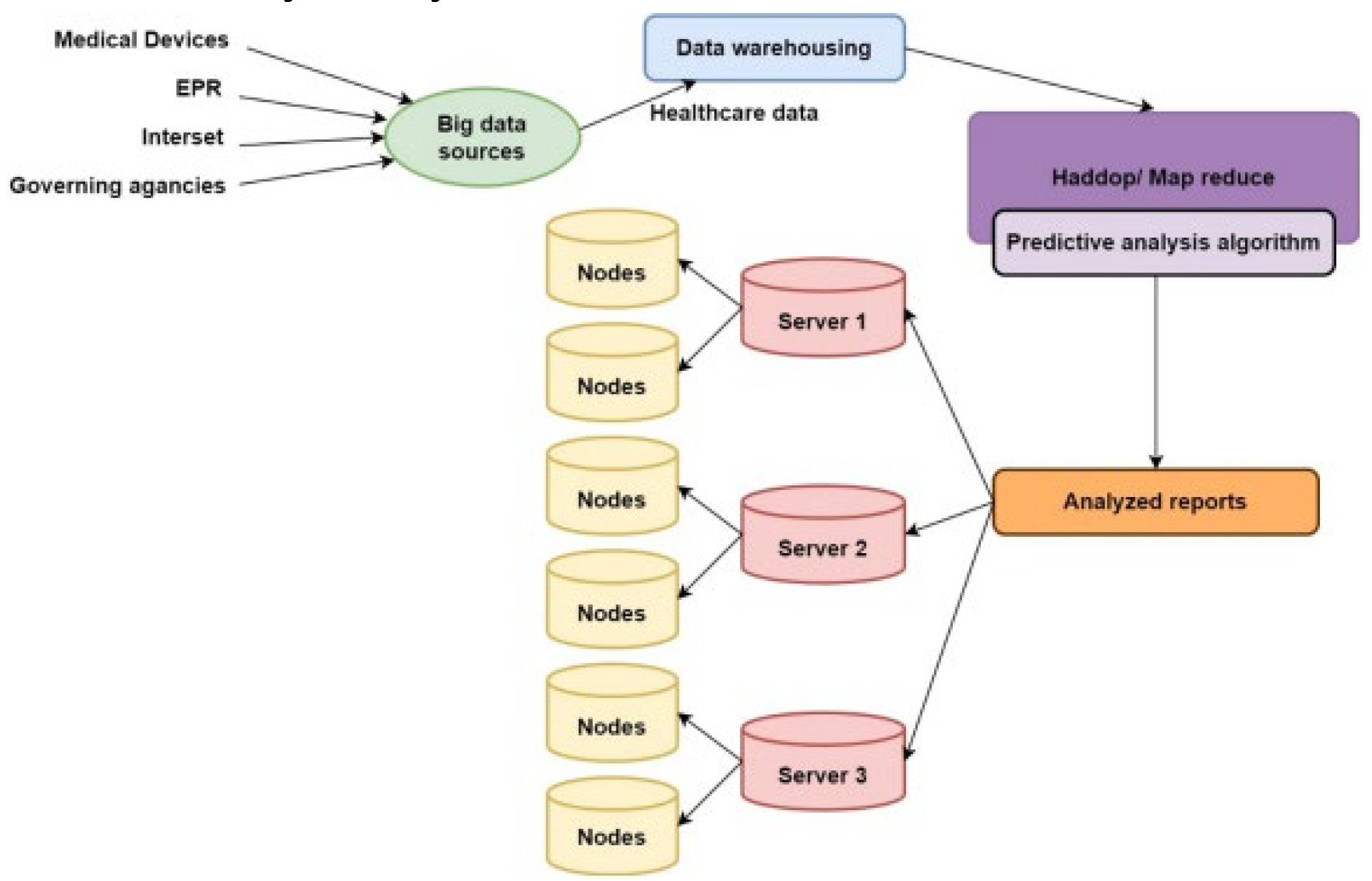
Predictive analytics in AI-driven decision-making for HIS uses complicated algorithms to evaluate large datasets and estimate future health results, allowing for preventive interventions, customized treatment strategies, and resource management. Predictive analytics uses ML and statistical analysis to identify trends and possible dangers in patient data, allowing physicians to make more informed decisions and boost results for patients whereas improving resource allocation within the healthcare system. Notwithstanding its advantages, such as early diagnosis of health problems, improved resource allocation, and cost savings via focused treatments and preventative activities, predictive analytics has drawbacks. These involve reliance on previous data, data privacy and security issues, difficulties comprehending sophisticated algorithms, potential biases in historical data, and the risk of undermining clinical experience and human beings in decision-making procedures. Resolving these difficulties is critical to unlocking predictive analytics’ full promise for improving healthcare outcomes in an ethical and fair manner. A predictive analytics system in healthcare is designed in several steps, starting with the integration of data from different sources to generate big data, followed by evaluation employing predictive analytic algorithms and distributed architecture that guarantee scalability, fault tolerance, and improved performance.
Figure 8 depicts the architecture of predictive analytics systems that use AI-driven decision-making.
III. NLP
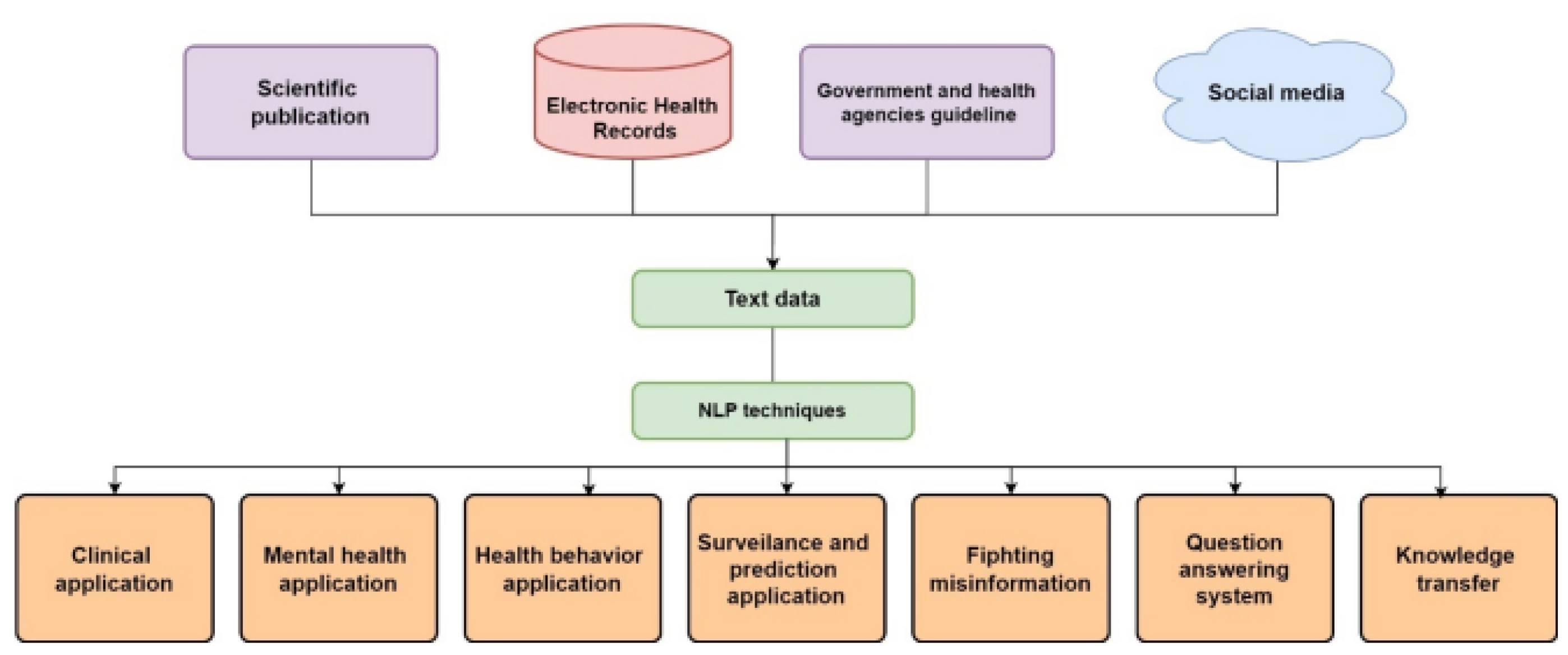
NLP serves an important role in AI-driven decision-making in HIS by making it easier to extract, understand, and apply meaningful insights from unstructured textual data. NLP systems turn free-text input into structured data, allowing for a full examination of patient histories and symptoms. This feature enables healthcare professionals to make well-informed judgments based on a comprehensive understanding of a patient’s health situation, which improves information retrieval efficacy, aids CDSS, and allows for tailored therapy. In spite of its advantages in extracting critical information, improving CDSS, and developing information retrieval processes, NLP integration faces obstacles like medical language complication. Making sure privacy and security compliance, problems with interoperability, dealing with evolving clinical terminology, and mitigating biases in NLP approaches. Managing these issues is critical for the effective implementation of NLP in HIS, which starts with analyzing different textual data sources employing NLP methods and directing transformed data to various healthcare applications, eventually resulting to more informed decision-making, better patient care, and improved health results.
Figure 9 indicates the framework of an NLP application with AI-powered decision-making.
IV. CAD
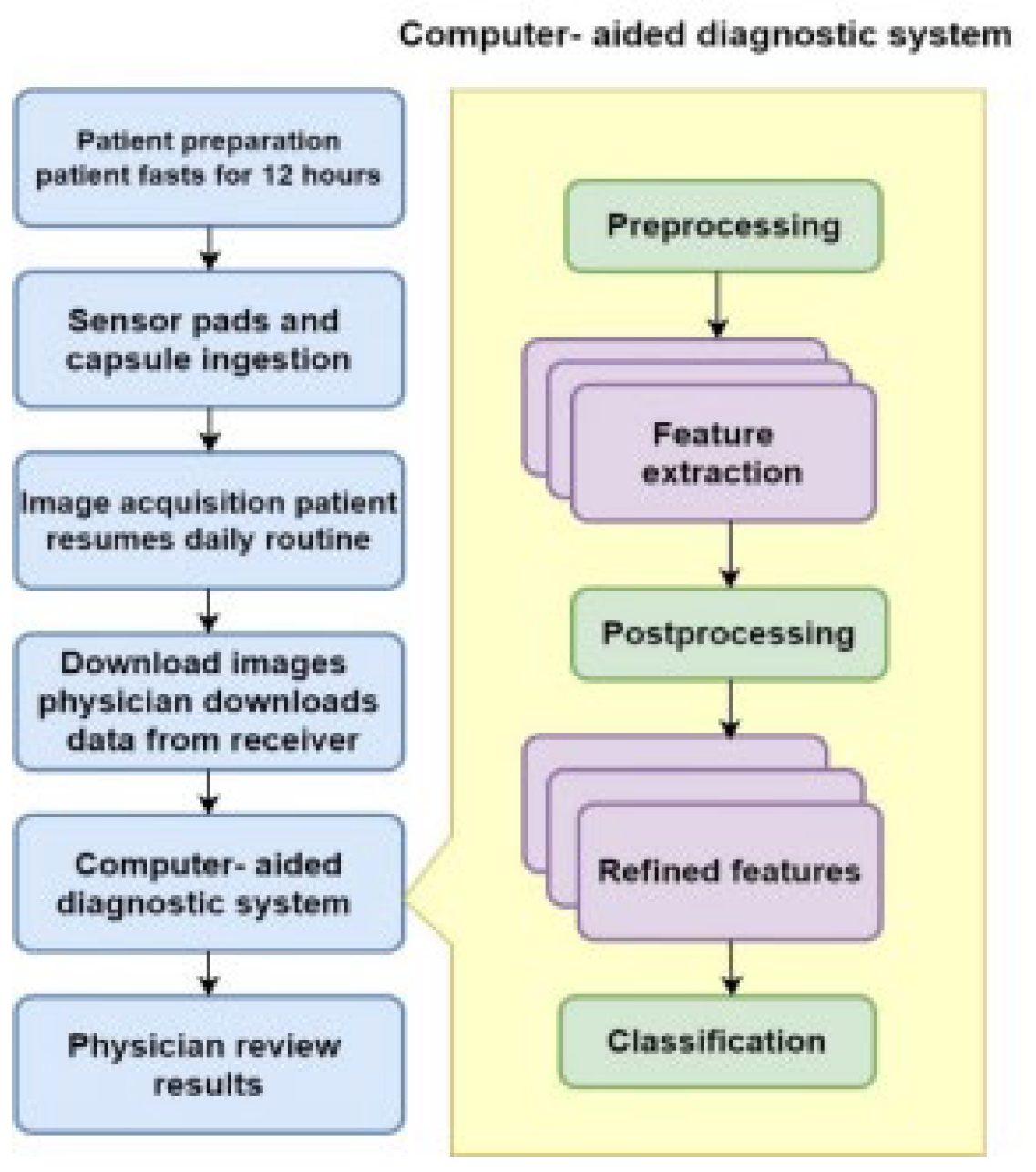
CAD is an fundamental section of AI-driven decision-making in HIS, applying complex algorithms and ML techniques to help clinicians in analyzing medical imaging and diagnostic information. CAD systems develop diagnostic accuracy by automatically recognizing paradigms, abnormalities, and possible concerns in sophisticated medical images like X-rays, MRIs, and CT scans, enabling radiologists and physicians in detecting small anomalies that may otherwise be ignored during physical analysis. This technology fasten the diagnostic process, enables for early disease diagnosis, and lastly gains patient results, motivating an integrated techniques to diagnostic decision-making in healthcare treatments. CAD integration confronting challenges such as mitigating false positives and false negatives, issuing biases in training data, interpreting nuanced medical images, integrating into recent healthcare processes, and enabling data privacy and regulatory compliance. Resolving these challenges is pivotal to setect CAD’s full potential in AI-driven decision-making for better diagnostic accuracy and patient care. The CAD process involves of patient organization, image collection with sensor pads and capsules, transmission of information to CAD systems, analyze with effective algorithms, and medical assessment of CAD-produces data, all of which propel to develope diagnostic strengths and more informed healthcare decisions.
Figure 10 depicts CAD with AI-based decision-making.
V. Robot-Assisted Surgery
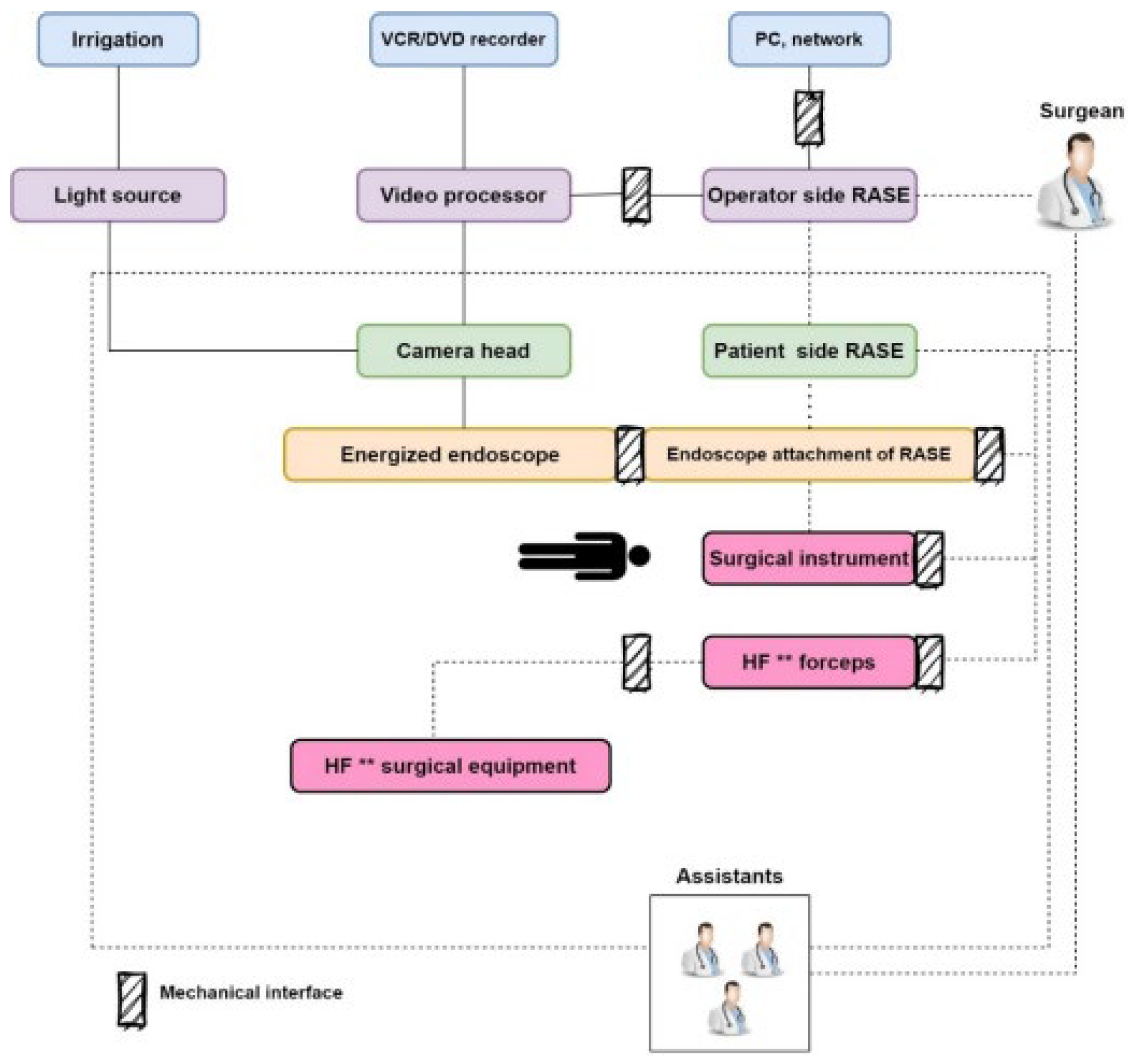
Robot-assisted surgery is an important progress in AI-powered decision-making in HIS, incorporating contemporary robotic technology with surgical strategies to allow surgeons to do less invasive operations with more precision and management. AI technologies develop surgical decision-making by conducting real-time data analysis and feedback, allowing surgeons to explore complicated patient data, adapt to evolving surgical circumstances, and make smart decisions throughout the procedures. This integration not only enhance surgical productivity and security, but also enables for the seamless integration of data-driven visions, leading to better patient results and a more customized technique for surgical practices. In spite of its positive facets in terms of accuracy, patient trauma elimination, and real-time decision-making, HIS robot-assisted surgery faces challenges such as high costs, integration into existing workflows, surgeon training, data security issues, potential biases in AI algorithms, regulatory compliance, and ethical considerations. Solving these issues is critical to the broad adoption and proper deployment of robot-assisted surgery in AI-powered healthcare systems. The architecture of robot-assisted surgery includes a variety of elements, such as irrigation, light transmission, video processing, robotic techniques, and surgical tools, all of which serve to enhance surgical accuracy by enabling surgeons with better vision, control, and accuracy during processes.
Figure 11 displays the architecture of robot-assisted surgery using AI-driven decision-making.
VI. VHAs and Chatbots
VHAs and Chatbots are critical parts of AI-driven decision-making in HIS, utilizing NLP and ML methods to engage with users, give information, help, and support clinical decision-making. These intelligent systems improve availability and effectiveness by responding in real time to questions regarding signs, prescriptions, and general health recommendations, along with helping with appointment scheduling, reminders for medications, and chronic disease treatment. VHAs and Chatbots use AI to speed healthcare delivery, improve interaction among patients and doctors, and assist improved decision-making with individualized health recommendations. Their incorporation with HIS transform’s patient involvement and assistance in the digital era. Considering their benefits in improving availability of healthcare information and services, VHAs and Chatbots face issues such as facilitating the accuracy and integrity of health information, solving regulatory concerns about data privacy and security, developing confidence in users, reducing algorithmic bias, incorporating perfectly into present healthcare workflows, and preserving interoperability with different systems. Resolving these issues is critical for maximizing the potential of VHAs and Chatbots in AI-driven decision-making while maintaining patient care and security requirements. A Virtual Assistant Intelligent Module’s architecture consists of interrelated parts such as the user interface, interpreter, knowledge base module, area traversal technique, and expert knowledge, which allow for dynamic communication, accurate interpretation of user queries, efficient data retrieval, and continuous development to enhance interactions between users.
Figure 12 displays the architecture of VHAs.
5.1. Prevalent Criteria
Prevalent criteria in AI-driven decision-making techniques within HIS encompass several key aspects [
63]. In this part we discuss some significant criteria which are considered the most in evaluation of investigated papers in AI-based decision-making in HIS.
Accuracy: Accuracy is an important criterion for ensuring that AI systems provide dependable and precise predictions or suggestions. In healthcare, erroneous forecasts would have a substantial influence on patient findings and treatment strategies. To verify the reliability of AI models, thorough validation and testing are required, which frequently include comparisons to gold-standard approaches and real-world validation studies [
64]. As Eq.1, true negative to true positive rate in the confusion matrix leverages (correctly recognized) and (total patterns).
Precision: According to Eq.2, the specified number of accurate predictions has been denoted by P, as well as the ratio of true positive forecasts to all positively predicted events [
65]. Additionally, STP specifies the whole number of true positives, and AFP indicates the total number of false positives.
Recall: Recall, as has specifies in Eq.3, a measure of how many true positive observations there are, is shown by how accurately it can forecast [
66]. Additionally, AFN details all false negatives in Eq.
F1-score: According to Eq.4, the F1 score also indicates the Harmonic attained by precision and recall, as well as the complete functioning criteria assessment of recall and precision [
67].
Furthermore, as Eq. 5, a confusion matrix with true negatives, true positives, false positives, and false negatives quantifies the performance metrics, reflecting projected and actual outcomes. Correct predictions encompass positive and negative outcomes, while incorrect predictions encompass False Positives and False Negatives [
68].
True positives predict a true positive class. False forecasts as true negatives are classified as such. MCC, a comprehensive metric, exceeds the F1 score in classification situations, yielding informative findings. It receives good marks while every area of the confusion matrix advantage from prediction results.
Interpretability: Interpretability is crucial for understanding the reasoning behind AI-driven decisions, especially in healthcare, wherein certain algorithms’ “black box” nature can prove hazardous. Clinicians must believe and comprehend the reasons behind the recommendations to make informed decisions. Transparent and interpretable systems enable the acceptance and application of AI in healthcare [
69].
Scalability: Scalability is essential for AI models to associate with the enhancing volume, diversity, and velocity of medical information. Medical datasets are large and complex, ranging from EHRs to medical imaging. Scalable AI systems could simply manage and evaluate these datasets, enabling them to function successfully in a broad range of medical contexts while incorporating the broadening complication of data [
70].
Considering these criteria together helps to the appropriate and successful adoption of AI-driven decision-making procedures in HIS, resulting in improved patient care, clinical results, and advancement of healthcare procedures.
Figure 13 shows frequency of various parameters considered for evaluating HIS applying AI-driven decision-making.
5.2. Challenges of the AI Applications in Decision-Making in HIS
Deploying AI-driven decision-making processes in this area various challenges. Handling the hurdles of AI-driven decision-making in HIS demands addressing many critical elements [
71]. Data quality and availability are critical because inconsistent or biased data might jeopardize the dependability of AI models, underlining the necessity of assuring data quality and accuracy, particularly among varied patient populations. Interpretability and explainability are critical for developing confidence in AI suggestions, demanding the creation of accurate and interpretable frameworks. Ethical and legal issues of patient privacy, approval, and algorithmic bias need to be carefully managed in order to strike a balance between advancements in healthcare and individual rights, as well as compliance with HIPAA. Integrating AI into healthcare operations presents considerable hurdles owing to potential resistance and interruptions, emphasizing the significance of user-friendly interfaces and seamless integration. Validation and generalization of AI algorithms throughout demographics and healthcare environments are critical to assuring their efficacy and usability in a variety of circumstances. Resource and financial restrictions could limit the availability of progressed AI systems, resulting in uneven adoption and delivery of healthcare solutions. AI models must be continuously learned and updated in order to stay up with increasing healthcare knowledge and findings. Collaboration among physicians, data scientists, policymakers, and technology developers are critical for overcoming these problems and developing strong, ethical, and successful AI-driven decision-making solutions for HIS [
72].
5.3. Datasets Commonly Used in ML Implementation for Decision-Making in HIS
Datasets are necessary for the productive utilization of ML for decision-making in HIS. These datasets, which contain a broad domain of healthcare information, enable the basis for training, validating, and testing ML systems [
73]. The application of well-maintained databases facilitates the improvement of predictive algorithms for disease diagnosis, therapy designing, and patient care. The relation rooted from the capacity of ML systems to emphasize notable patterns and insights from tremendous volumes of medical data, leading to better clinical decision support. These databases involve patient information, medical imaging, genetic data, and other pertinent data to increase individualized and evidence-based healthcare treatments. Moreover, the ethical and responsible application of datasets supports the dependability of ML-driven evaluation, stressing the importance of accurate, representative, and securely maintained healthcare datasets in developing decision-making within HIS. Widespread datasets used in ML implementation for decision-making in HIS consist a broad domain of healthcare data, which allows to provide and increase prediction models [
74]. The datasets consist:
EHRs: Patient data produced in EHRs operate as the main dataset, involving data like medical records, diagnoses, treatments, prescriptions, and test outcomes [
75].
Medical Imaging Datasets: Radiological images, consisting X-rays, MRIs, and CT scans, are pivotal for ML-based diagnostic decision-making. These datasets enable developing the algorithms for image recognition, lesion detection, and disease categorization [
76].
Genomic and Molecular Datasets: Genomic data may generate significant data regarding general variations and disease risk. ML models apply genomic dat to increase the precision of medicine, adjust drugs, and predict sickness risks emloying genetic profiles [
77].
Clinical Trials and Research Databases: Datasets from clinical research and research give a wealth of data regarding treatment results, experimental drugs, and patient responses. ML models can apply this data to make evidence-based decisions and detect trends in efficiency of treatments [
78].
Patient Outcome Databases: Datasets tracking patient findings, readmission rates, and post-therapy follow-ups might predict outcome of treatment and aid in decision-making for optimal treatment for patients [
79].
Health Monitoring Devices: Wearable technology and health monitoring devices generate real-time data on the patient’s health activity levels, and physiological metrics, which could be analyzed by ML systems to allow continual health monitoring and early detection of abnormalities [
80].
NLP Datasets: Unstructured data, like clinical notes, research articles, and medical literature, is evaluated applying NLP methods to extract useful information for decision support. These datasets aid to understand contextual subtleties in medical data [
81].
These datasets are necessary owing to the fact that they are able to be utilized to train ML models that will detect trends, predict findings, and develop clinical decision-making. Making sure the quality, accuracy, and ethical application of these datasets is critical for the efficient implementation of ML in HIS, which propel to better patient care and outcomes.
6. Open Issues
Various unsolved difficulties remain in the area of AI-driven decision-making in HIS, posing both challenges and opportunities for future research and development. Let’s have a look at the open issues of AI-driven decision-making in HIS. The unresolved problems about AI-driven decision-making in HIS involve a number of important fields that must be considered and handled. Interoperability and standards remain a challenge due to the lack of a uniform framework, which hampers data transfer and AI integration across many healthcare systems [
82]. Ethical and legal frameworks are crucial for safeguarding patient privacy, openness, and integrity in algorithmic decision-making, and they require ongoing stakeholder interaction to generate robust recommendation [
83]. Explainability and interpretability systems are crucial for instilling trust and responsibility in AI-generated proposals, needing more research and rules to ensure cohesive interaction between complex algorithmic outputs. Data quality and bias foundations are crucial for improving the accuracy and integrity of AI systems, needing comprehensive approaches to difficulties like as data correctness, consistency, and bias detection [
84]. Human-AI interaction frameworks must allow for efficient interaction and well defined duties among AI systems and healthcare practitioners to allow to utilize AI’s computational capacities while maintaining human expertise and sensitivity. Security and privacy regulations are crucial for preserving sensitive patient data and maintaining trust in AI-powered decision-making, requiring powerful encryption technology and ethical AI deployment protocols [
85]. Validation and generalization frameworks are crucial for assessing the effectiveness and practicality of AI models across diverse patient populations and healthcare environments, needing consistent ways to complete evaluation. Resource allocation and cost-effectiveness frameworks are critical for maximising AI installation while ensuring long-term resource utilization and economic feasibility [
86]. The long-term influence on the workforce poses issues in transforming old roles and duties to the integration of AI technology, necessitating deliberate workforce management frameworks to ensure a smooth transition [
87]. Lastly, real-world implementation investigations are critical for turning AI discoveries into actual advancements in patient care and clinical processes, underlining the importance of robust studies to assess AI’s true influence in healthcare environments and encourage evidence-based practices. Resolving these outstanding challenges will help to ensure the ethical, useful, and fair integration of AI-powered decision-making in HIS, thereby improving patient outcomes and healthcare services [
88].
Future research into AI-driven decision-making in HIS is vital for plenty of reasons [
89]. First of all, the continuously developing nature of both technology and healthcare need continuous research and development in order to keep up with growing issues and possibilities [
90]. Anticipating and resolving possible ethical, regulatory, and technological challenges ensures that AI applications be implemented responsibly, hence maintaining patient confidence and security [
91]. In addition, continual advancements in explainability, data quality, and bias reduction contribute to the reliability and equality of AI-driven decisions, hence boosting acceptability among healthcare professionals. More study will also concentrate on enhancing interoperability, optimizing human-AI collaboration, and conducting real-world implementation studies, all of which are substantial for the successful integration and scaling of AI solutions in a range of healthcare contexts [
92]. Healthcare systems that are proactive in research and development may fully achieve the potential of AI-driven decision-making, enhancing patient outcomes, simplifying procedures, and ensuring the long-term sustainability and usefulness of these technologies in healthcare delivery [
93].
Later studies in AI-driven decision-making in HIS will focus on specific important fields to address current difficulties and spur innovation [
94]. To begin with, explainability and interpretability research will be critical in enahncing transparency and reliability in AI algorithms, enabling their simple integration into healthcare decision-making procedures, and ensuring ethical compliance. Data quality and bias decreasing initiatives will prioritize increasing AI models’ transparency and equality by addressing issues like data accuracy, validation, and bias recognition, with the goal of supporting fairness and equity in healthcare results. Besides, ethical and regulatory improvement will be critical for providing strong ethical roles and legal structures to regulate the ethical application of AI in healthcare, enabling stakeholder confidence, and ensuring secure AI adoption. Human-AI interconnected frameworks will prioritize infuence interoperability methods that allow for seamless data stream across healthcare systems, making it simpler to incorporate and scale AI applications, and finally prepolling to more accurate and tailored healthcare results. Real-world implementation research will give critical visions into the scalability, efficiency, and cost-effectiveness of AI-driven decision-making systems in healthcare settings, supporting evidence-based practices and motivating AI technology uptake. Continuous validation and progressie attempts will ensure that AI models are reliable, generalizable, and ethical in evolving clinical contexts, while security and privacy development will emphasize on establishing strong security structures and privacy-enhancing technologies to preserve sensitive patient data and maintain reliability in AI-powered decision-making. These next paces will lead breakthroughs in AI-driven decision-making in HIS, eventually enhancing patient results and care service.
7. Conclusion and Limitation
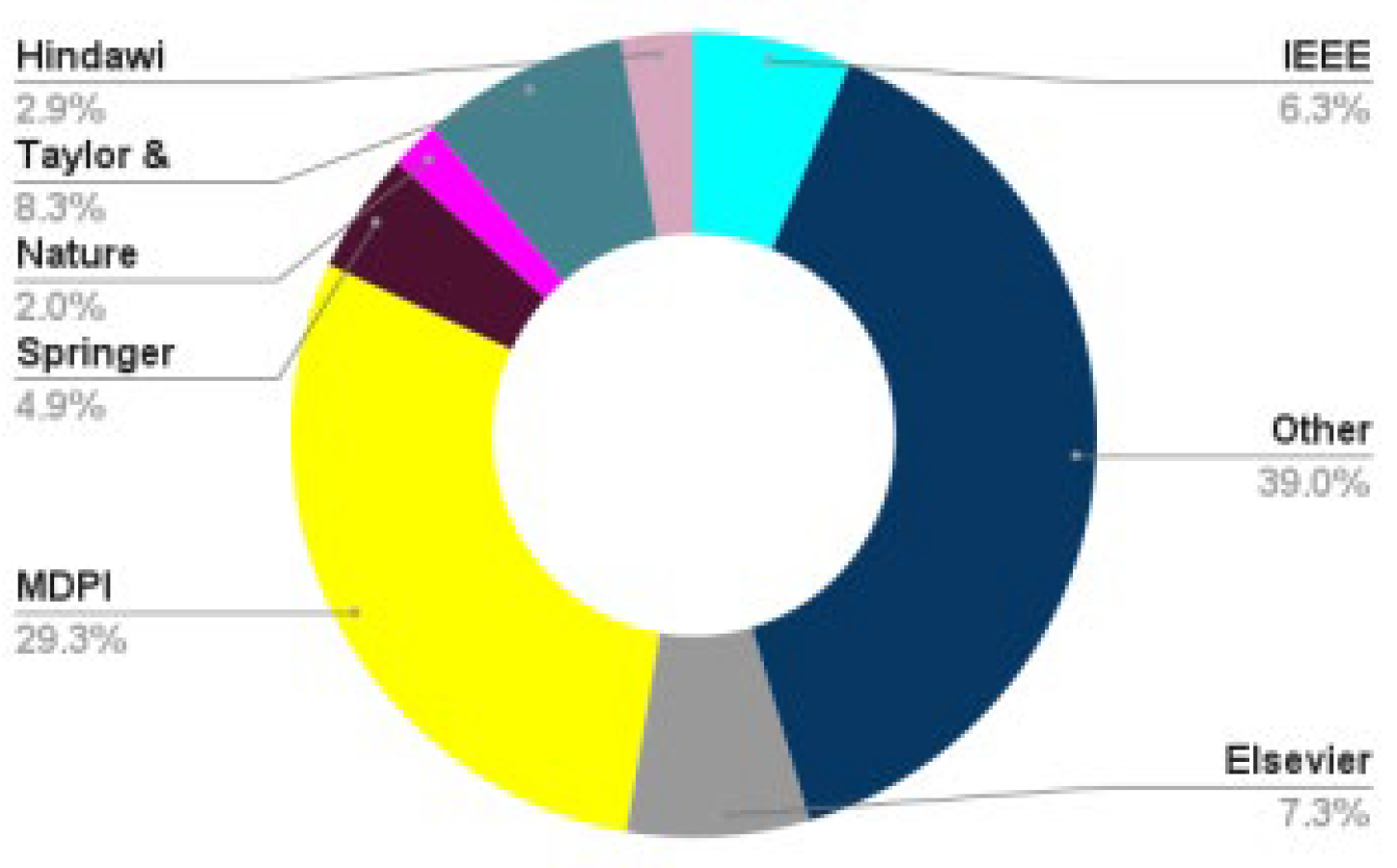
We conducted a thorough investigation of AI-driven decision-making in HIS, establishing a new taxonomy for classifying applications in this sector. The suggested taxonomy divides AI-driven decision-making applications into six separate categories, offering a formal framework for assessing their unique benefits, drawbacks, simulation settings, and dataset properties. The appraisal of significant works in this field emphasizes the importance of our results, with the majority of publications published in 2023 and 2022, mostly by Springer. Python and MATLAB emerged as the most popular programming languages, accounting for 48% and 20% of suggested technique simulations, respectively. Interpretability, accuracy, and privacy were noted as critical issues in the research, stressing their importance in furthering the area of AI-driven decision-making in HIS.
Numerous important gaps highlight the need for more study on AI-driven decision-making in HIS. To begin, obtaining interpretability in complicated AI models remains a hurdle, preventing their smooth incorporation into medical processes and undermining confidence between healthcare practitioners. Addressing biases in AI models is critical to ensuring equitable and impartial decision-making, especially among varied patient groups. The standardization of assessment measures is critical for assessing the performance of various AI-driven systems and comparing results among research. Privacy problems, particularly in the management of sensitive healthcare data, necessitate complete solutions to retain patient confidence and regulatory compliance. Furthermore, the real-world use of AI-driven decision-making tools involves addressing integration problems, guaranteeing usability, and assessing the long-term influence on patient outcomes. Future research should concentrate on improving interpretability methods, implementing bias mitigation techniques, determining standardized assessment frameworks, improving privacy-preserving approaches, and carrying out robust real-world validations to close these gaps and drive the ethical and efficient deployment of AI-driven decision-making in HIS.
Author Contributions
Conceptualization, Maryam Bagher and Mohsen Bagheritabar; methodology, Maryam Bagher and Y.L.; software, Maryam Bagher and Mohsen Bagheritabar; validation, Maryam Bagher, Mohsen Bagheritabar, S.A., M.S.P., P.M., and Y.L.; formal analysis, Maryam Bagher; investigation, Maryam Bagher, Mohsen Bagheritabar, S.A., M.S.P., and P.M.; resources, Y.L.; data curation, Maryam Bagher, Mohsen Bagheritabar, S.A., M.S.P., and P.M.; writing—original draft preparation, Maryam Bagher; writing—review and editing, Maryam Bagher and Y.L..; visualization, Maryam Bagher; supervision, Y.L.; project administration, Maryam Bagher, Mohsen Bagheritabar, S.A., M.S.P., P.M., and Y.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ramírez, J.G.C., AI in Healthcare: Revolutionizing Patient Care with Predictive Analytics and Decision Support Systems. Journal of Artificial Intelligence General science (JAIGS) ISSN: 3006-4023, 2024. 1(1): p. 31-37. [CrossRef]
- Bertl, M., P. Ross, and D. Draheim, Systematic AI support for decision-making in the healthcare sector: Obstacles and success factors. Health Policy and Technology, 2023. 12(3): p. 100748. [CrossRef]
- Patil, S. and H. Shankar, Transforming healthcare: harnessing the power of AI in the modern era. International Journal of Multidisciplinary Sciences and Arts, 2023. 2(1): p. 60-70.
- Heilig, T. and I. Scheer, Decision Intelligence: Transform Your Team and Organization with AI-Driven Decision-Making. 2023: John Wiley & Sons.
- Kasula, B.Y. and P. Whig, AI-Driven Machine Learning Solutions for Sustainable Development in Healthcare—Pioneering Efficient, Equitable, and Innovative Health Service. International Journal of Sustainable Development Through AI, ML and IoT, 2023. 2(2): p. 1-7.
- Sylolypavan, A., et al., The impact of inconsistent human annotations on AI driven clinical decision making. NPJ Digital Medicine, 2023. 6(1): p. 26. [CrossRef]
- Harry, A., The future of medicine: harnessing the power of AI for revolutionizing healthcare. International Journal of Multidisciplinary Sciences and Arts, 2023. 2(1): p. 36-47. [CrossRef]
- Sarella, P.N.K. and V.T. Mangam, AI-Driven Natural Language Processing in Healthcare: Transforming Patient-Provider Communication. Indian Journal of Pharmacy Practice, 2024. 17(1). [CrossRef]
- Kazi, K., AI-Driven IoT (AIIoT) in Healthcare Monitoring, in Using Traditional Design Methods to Enhance AI-Driven Decision Making. 2024, IGI Global. p. 77-101.
- Wysocki, O., et al., Assessing the communication gap between AI models and healthcare professionals: Explainability, utility and trust in AI-driven clinical decision-making. Artificial Intelligence, 2023. 316: p. 103839. [CrossRef]
- Vyas, B., Java-Powered AI: Implementing Intelligent Systems with Code. Journal of Science & Technology, 2023. 4(6): p. 1-12.
- Suha, S.A. and T.F. Sanam, Exploring dominant factors for ensuring the sustainability of utilizing artificial intelligence in healthcare decision making: An emerging country context. International Journal of Information Management Data Insights, 2023. 3(1): p. 100170.
- Saxena, P.D., et al., Impact of Artificial Intelligence on Healthcare Informatics: Opportunities and Challenges. Journal of Informatics Education and Research, 2023. 3(2). [CrossRef]
- Gudigantala, N., S. Madhavaram, and P. Bicen, An AI decision-making framework for business value maximization. AI Magazine, 2023. 44(1): p. 67-84. [CrossRef]
- Ray, P.P. and P. Majumder, The potential of ChatGPT to transform healthcare and address ethical challenges in artificial intelligence-driven medicine. Journal of Clinical Neurology (Seoul, Korea), 2023. 19(5): p. 509. [CrossRef]
- Božić, V., “Artificial Intelligence–powered” Expert Systems in Hospitals.
- Van Berkel, N., et al., Measurements, algorithms, and presentations of reality: Framing interactions with AI-enabled decision support. ACM Transactions on Computer-Human Interaction, 2023. 30(2): p. 1-33.
- Durga, K., Intelligent Support for Cardiovascular Diagnosis: The AI-CDSS Approach, in Using Traditional Design Methods to Enhance AI-Driven Decision Making. 2024, IGI Global. p. 64-76.
- Chen, C. and Y. Zheng, When consumers need more interpretability of artificial intelligence (AI) recommendations? The effect of decision-making domains. Behaviour & Information Technology, 2023: p. 1-9. [CrossRef]
- Jeyaraman, M., et al., Unraveling the ethical enigma: artificial intelligence in healthcare. Cureus, 2023. 15(8). [CrossRef]
- Kaul, R., et al., The role of AI for developing digital twins in healthcare: The case of cancer care. Wiley Interdisciplinary Reviews: Data Mining and Knowledge Discovery, 2023. 13(1): p. e1480.
- Dogheim, G.M. and A. Hussain, Patient care through AI-driven remote monitoring: Analyzing the role of predictive models and intelligent alerts in preventive medicine. Journal of Contemporary Healthcare Analytics, 2023. 7(1): p. 94-110.
- Babarinde, A.O., et al., Review of AI applications in Healthcare: Comparative insights from the USA and Africa. International Medical Science Research Journal, 2023. 3(3): p. 92-107. [CrossRef]
- Bao, Y., W. Gong, and K. Yang, A Literature Review of Human–AI Synergy in Decision Making: From the Perspective of Affordance Actualization Theory. Systems, 2023. 11(9): p. 442. [CrossRef]
- Mahdi, S.S., et al., How does artificial intelligence impact digital healthcare initiatives? A review of AI applications in dental healthcare. International Journal of Information Management Data Insights, 2023. 3(1): p. 100144. [CrossRef]
- Nawrat, Z., Introduction to AI-driven surgical robots. Artif Intell Surg, 2023. 3(2): p. 90-7. [CrossRef]
- Wang, L., et al., Human-centered design and evaluation of AI-empowered clinical decision support systems: a systematic review. Frontiers in Computer Science, 2023. 5: p. 1187299. [CrossRef]
- Moazemi, S., et al., Artificial intelligence for clinical decision support for monitoring patients in cardiovascular ICUs: A systematic review. Frontiers in Medicine, 2023. 10: p. 1109411. [CrossRef]
- Loftus, T.J., et al., Artificial intelligence-enabled decision support in nephrology. Nature Reviews Nephrology, 2022. 18(7): p. 452-465. [CrossRef]
- Xu, Q., et al., Interpretability of Clinical Decision Support Systems Based on Artificial Intelligence from Technological and Medical Perspective: A Systematic Review. Journal of Healthcare Engineering, 2023. 2023. [CrossRef]
- Lau, P.L., M. Nandy, and S. Chakraborty. Accelerating UN sustainable development goals with ai-driven technologies: A systematic literature review of women’s healthcare. in Healthcare. 2023. MDPI. [CrossRef]
- Marino, N., et al., Towards AI-driven longevity research: An overview. Frontiers in Aging, 2023. 4: p. 1057204. [CrossRef]
- Comito, C., D. Falcone, and A. Forestiero, AI-Driven Clinical Decision Support: Enhancing Disease Diagnosis Exploiting Patients Similarity. IEEE Access, 2022. 10: p. 6878-6888. [CrossRef]
- Vasey, B., et al., Reporting guideline for the early-stage clinical evaluation of decision support systems driven by artificial intelligence: DECIDE-AI. Nature medicine, 2022. 28(5): p. 924-933.
- Choudhury, A., Factors influencing clinicians’ willingness to use an AI-based clinical decision support system. Frontiers in Digital Health, 2022. 4: p. 920662. [CrossRef]
- Liu, X., et al., Discrepancy between perceptions and acceptance of clinical decision support Systems: implementation of artificial intelligence for vancomycin dosing. BMC Medical Informatics and Decision Making, 2023. 23(1): p. 157. [CrossRef]
- Amann, J., et al., Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC medical informatics and decision making, 2020. 20: p. 1-9. [CrossRef]
- Elvas, L.B., et al., AI-Driven Decision Support for Early Detection of Cardiac Events: Unveiling Patterns and Predicting Myocardial Ischemia. Journal of Personalized Medicine, 2023. 13(9): p. 1421. [CrossRef]
- Rehman, A., A. Farrakh, and U.F. Mushtaq, Improving Clinical Decision Support Systems: Explainable AI for Enhanced Disease Prediction in Healthcare. International Journal of Computational and Innovative Sciences, 2023. 2(2): p. 9-23.
- Chen, J., et al., Artificial intelligence-based human-centric decision support framework: an application to predictive maintenance in asset management under pandemic environments. Annals of Operations Research, 2021: p. 1-24. [CrossRef]
- Wang, J., et al., Managerial decision support system using an integrated model of AI and big data analytics. Annals of Operations Research, 2022: p. 1-18. [CrossRef]
- Hasan, I., et al., Data analytics and knowledge management approach for COVID-19 prediction and control. International Journal of Information Technology, 2023. 15(2): p. 937-954. [CrossRef]
- Afshar, M., et al., Deployment of Real-time Natural Language Processing and Deep Learning Clinical Decision Support in the Electronic Health Record: Pipeline Implementation for an Opioid Misuse Screener in Hospitalized Adults. JMIR Medical Informatics, 2023. 11: p. e44977. [CrossRef]
- Elkin, P.L., et al., Using artificial intelligence with natural language processing to combine electronic health record’s structured and free text data to identify nonvalvular atrial fibrillation to decrease strokes and death: Evaluation and case-control study. Journal of medical Internet research, 2021. 23(11): p. e28946. [CrossRef]
- Stewart, R., J. Chaturvedi, and A. Roberts, Natural language processing–relevance to patient outcomes and real-world evidence. 2023, Taylor & Francis. p. 1-5. [CrossRef]
- Joyce, C., et al., The evaluation of a clinical decision support tool using natural language processing to screen hospitalized adults for unhealthy substance use: protocol for a quasi-experimental design. JMIR Research Protocols, 2022. 11(12): p. e42971. [CrossRef]
- Barrera, N., et al., A recommender system for occupational hygiene services using natural language processing. Healthcare Analytics, 2023. 3: p. 100148. [CrossRef]
- Creswell, J., et al., Early user perspectives on using computer-aided detection software for interpreting chest X-ray images to enhance access and quality of care for persons with tuberculosis. BMC Global and Public Health, 2023. 1(1): p. 30. [CrossRef]
- Tran, W.T., et al., Computational radiology in breast cancer screening and diagnosis using artificial intelligence. Canadian Association of Radiologists Journal, 2021. 72(1): p. 98-108. [CrossRef]
- Ibrahim, A.U., A.G. Kibarer, and F. Al-Turjman, Computer-aided Detection of Tuberculosis from Microbiological and Radiographic Images. Data Intelligence, 2023: p. 1-26. [CrossRef]
- Shukla, P.K., et al., AI-DRIVEN novel approach for liver cancer screening and prediction using cascaded fully convolutional neural network. Journal of Healthcare Engineering, 2022. 2022. [CrossRef]
- Khanna, M., et al., Radiologist-level two novel and robust automated computer-aided prediction models for early detection of COVID-19 infection from chest X-ray images. Arabian Journal for Science and Engineering, 2023. 48(8): p. 11051-11083. [CrossRef]
- Zeineldin, R.A., et al., Development of an AI-driven system for neurosurgery with a usability study: a step towards minimal invasive robotics. at-Automatisierungstechnik, 2023. 71(7): p. 537-546. [CrossRef]
- Parry, M.W., et al., Patient Perspectives on Artificial Intelligence in Healthcare Decision Making: A Multi-Center Comparative Study. Indian Journal of Orthopaedics, 2023. 57(5): p. 653-665. [CrossRef]
- Kotha, S., et al., ARTEMIS: AI-driven Robotic Triage Labeling and Emergency Medical Information System. arXiv preprint arXiv:2309.08865, 2023.
- Kolbinger, F.R., et al., Artificial Intelligence for context-aware surgical guidance in complex robot-assisted oncological procedures: An exploratory feasibility study. European Journal of Surgical Oncology, 2023: p. 106996. [CrossRef]
- Ai, Y., et al., Control system design for a novel minimally invasive surgical robot. Computer Assisted Surgery, 2016. 21(sup1): p. 45-53. [CrossRef]
- Wang, H., et al., An artificial intelligence chatbot for young people’s sexual and reproductive health in india (snehai): Instrumental case study. Journal of Medical Internet Research, 2022. 24(1): p. e29969. [CrossRef]
- Fan, X., et al., Utilization of self-diagnosis health chatbots in real-world settings: case study. Journal of medical Internet research, 2021. 23(1): p. e19928. [CrossRef]
- Chakraborty, S., et al., An AI-Based Medical Chatbot Model for Infectious Disease Prediction. Ieee Access, 2022. 10: p. 128469-128483. [CrossRef]
- Esmaeilzadeh, P., T. Mirzaei, and S. Dharanikota, Patients’ perceptions toward human–artificial intelligence interaction in health care: experimental study. Journal of medical Internet research, 2021. 23(11): p. e25856.
- Chow, J.C., et al. Developing an AI-Assisted Educational Chatbot for Radiotherapy Using the IBM Watson Assistant Platform. in Healthcare. 2023. MDPI. [CrossRef]
- Shamszare, H. and A. Choudhury. Clinicians’ Perceptions of Artificial Intelligence: Focus on Workload, Risk, Trust, Clinical Decision Making, and Clinical Integration. in Healthcare. 2023. MDPI.
- Bayyapu, S., R.R. Turpu, and R.R. Vangala, ADVANCING HEALTHCARE DECISION-MAKING: THE FUSION OF MACHINE LEARNING, PREDICTIVE ANALYTICS, AND CLOUD TECHNOLOGY.
- Zhang, P. and M.N. Kamel Boulos, Generative AI in medicine and healthcare: Promises, opportunities and challenges. Future Internet, 2023. 15(9): p. 286. [CrossRef]
- Mardiani, E., L. Judijanto, and A.Y. Rukmana, Improving Trust and Accountability in AI Systems through Technological Era Advancement for Decision Support in Indonesian Manufacturing Companies. West Science Interdisciplinary Studies, 2023. 1(10): p. 1019-1027. [CrossRef]
- Bhavaraju, S.R., Artificial intelligence in healthcare: doctor as a stakeholder. 2023.
- Ayo-Farai, O., et al., Engineering innovations in healthcare: a review of developments in the USA. Engineering Science & Technology Journal, 2023. 4(6): p. 381-400. [CrossRef]
- Batra, P. and D.M. Dave, Revolutionizing Healthcare Platforms: The Impact of AI on Patient Engagement and Treatment Efficacy. International Journal of Science and Research (IJSR), 2024. 13(10.21275): p. 613-624.
- Yelne, S., et al., Harnessing the power of AI: a comprehensive review of its impact and challenges in nursing science and healthcare. Cureus, 2023. 15(11). [CrossRef]
- Pradhan, B., et al., An AI-Assisted Smart Healthcare System Using 5G Communication. IEEE Access, 2023. [CrossRef]
- Amin, A., et al. An explainable ai framework for artificial intelligence of medical things. in 2023 IEEE Globecom Workshops (GC Wkshps). 2023. IEEE.
- Goktas, P., A. Kucukkaya, and P. Karacay, Leveraging the efficiency and transparency of artificial intelligence-driven visual Chatbot through smart prompt learning concept. Skin Research and Technology, 2023. 29(11). [CrossRef]
- Husnain, A., et al., AI’S healing touch: examining machine learning’s transformative effects on healthcare. Journal of World Science, 2023. 2(10): p. 1681-1695. [CrossRef]
- Ogbuke, N., et al., Data-driven technologies for global healthcare practices and COVID-19: opportunities and challenges. Annals of Operations Research, 2023: p. 1-36. [CrossRef]
- Abbas, A., AI in Healthcare: Applications, Challenges, and Future Prospects.
- Singh, A., et al., Revolutionizing Breast Healthcare: Harnessing the Role of Artificial Intelligence. Cureus, 2023. 15(12). [CrossRef]
- Alam, M.N., M. Kaur, and M.S. Kabir, Explainable AI in Healthcare: Enhancing transparency and trust upon legal and ethical consideration. Int Res J Eng Technol, 2023. 10(6): p. 1-9.
- Mergen, M., et al., Immersive training of clinical decision making with AI driven virtual patients–a new VR platform called medical tr. AI. ning. GMS Journal for Medical Education, 2023. 40(2).
- Gupta, B.B., et al., Analysis of cutting-edge technologies for enterprise information system and management. Enterprise Information Systems, 2023. 17(11): p. 2197406. [CrossRef]
- Raut, R., et al. Intelligent Information System for Detection of COVID-19 Based on AI. in Proceedings of 3rd International Conference on Recent Trends in Machine Learning, IoT, Smart Cities and Applications: ICMISC 2022. 2023. Springer.
- Fawaz, A., A. Ferraresi, and C. Isidoro, Systems Biology in Cancer Diagnosis Integrating Omics Technologies and Artificial Intelligence to Support Physician Decision Making. Journal of Personalized Medicine, 2023. 13(11): p. 1590. [CrossRef]
- Khan, A., Harnessing the Power of AI: A Review of Advancements in Healthcare. BULLET: Jurnal Multidisiplin Ilmu, 2023. 2(3): p. 546-556.
- Ghanvatkar, S. and V. Rajan, Evaluating Explanations from AI Algorithms for Clinical Decision-Making: A Social Science-based Approach. medRxiv, 2024: p. 2024.02. 26.24303365. [CrossRef]
- Olabanji, S.O., et al., AI-Driven cloud security: Examining the impact of user behavior analysis on threat detection. Asian Journal of Research in Computer Science, 2024. 17(3): p. 57-74. [CrossRef]
- Mykhalko, Y., et al., FROM TEXT TO DIAGNOSE: CHATGPT’S EFFICACY IN MEDICAL DECISION-MAKING. INDEXED IN PUBMED/MEDLINE, SCOPUS, EMBASE, EBSCO, INDEX COPERNICUS, POLISH MINISTRY OF EDUCATION AND SCIENCE, POLISH MEDICAL BIBLIOGRAPHY, 2023. 76(11): p. 2345-2350. [CrossRef]
- Chintala, S., AI-Driven Personalised Treatment Plans: The Future of Precision Medicine. Machine Intelligence Research, 2023. 17(02): p. 9718-9728.
- Cipriano, L.E., Evaluating the impact and potential impact of machine learning on medical decision making. 2023, SAGE Publications Sage CA: Los Angeles, CA. p. 147-149. [CrossRef]
- Sarker, M., Assessing the Integration of AI Technologies in Enhancing Patient Care Delivery in US Hospitals. Journal of Knowledge Learning and Science Technology ISSN: 2959-6386 (online), 2023. 2(2): p. 338-351. [CrossRef]
- Martins, A., et al., PharmiTech: Addressing Polypharmacy Challenges Through AI-Driven Solutions. Available at SSRN 4668688.
- Wahab, N.A.B.A. and R.B.M. Nor, Challenges and Strategies in Data Management and Governance for AI-Based Healthcare Models: Balancing Innovation and Ethical Responsibilities. AI, IoT and the Fourth Industrial Revolution Review, 2023. 13(12): p. 24-32.
- Parsa, A.D., et al., Artificial Intelligence for Global Healthcare, in Artificial Intelligence in Medical Virology. 2023, Springer. p. 1-21.
- Andolina, S. and J.A. Konstan, Introduction to the special issue on AI, decision-making, and the impact on humans. 2023, Taylor & Francis. p. 1367-1370. [CrossRef]
- Sharma, R., AI Fusion: Unleashing Synergies in M&A, IT Supply Chain, and IoT-Driven Medical Device Sales with SAP Integration. 2024, EasyChair.
Figure 1.
Process of selecting papers.
Figure 1.
Process of selecting papers.
Figure 2.
First step of selecting papers.
Figure 2.
First step of selecting papers.
Figure 3.
Last step of selecting papers.
Figure 3.
Last step of selecting papers.
Figure 4.
Taxonomy of various HIS make AI-driven decisions.
Figure 4.
Taxonomy of various HIS make AI-driven decisions.
Figure 5.
Frequency of programming languages and libraries applied for simulating proposed methods in this area.
Figure 5.
Frequency of programming languages and libraries applied for simulating proposed methods in this area.
Figure 6.
Applications of HIS apply AI-driven decision making.
Figure 6.
Applications of HIS apply AI-driven decision making.
Figure 7.
The sequence of CDSS applying AI-driven decision-making.
Figure 7.
The sequence of CDSS applying AI-driven decision-making.
Figure 8.
The architecture of predictive analytics systems applies AI-driven decision making.
Figure 8.
The architecture of predictive analytics systems applies AI-driven decision making.
Figure 9.
Architecture of NLP application employing AI-driven decision-making.
Figure 9.
Architecture of NLP application employing AI-driven decision-making.
Figure 10.
CAD with AI-based decision-making.
Figure 10.
CAD with AI-based decision-making.
Figure 11.
Architecture of robot-assisted surgery applying AI-driven decision making.
Figure 11.
Architecture of robot-assisted surgery applying AI-driven decision making.
Figure 12.
Architecture of VHAs applying AI-driven decision making.
Figure 12.
Architecture of VHAs applying AI-driven decision making.
Figure 13.
Frequency of various parameters considered for evaluating HIS applying AI-driven decision-making.
Figure 13.
Frequency of various parameters considered for evaluating HIS applying AI-driven decision-making.
Table 1.
Related works.
| Authors |
Main Idea
|
Advantages
|
Disadvantages
|
| Wang, Zhang [27] |
|
|
Resistance to change Limited expertise |
| Moazemi, Vahdati [28] |
|
|
|
| Loftus, Shickel [29] |
|
|
|
| Xu, Xie [30] |
|
|
|
| Lau, Nandy [31] |
|
|
|
| Marino, Putignano [32] |
|
|
|
| Ours |
|
Comprehensive SLR Identification of trends Addressing existed gaps |
|
Table 2.
Keywords and phrase used to search papers.
Table 2.
Keywords and phrase used to search papers.
| S# |
Keywords and search criteria |
S# |
Keywords and search criteria |
| S1 |
“AI” and “Information Systems” |
S6 |
“Healthcare” and “Information Systems” |
| S2 |
“Decision-making” and “AI” |
S7 |
“Clinical Decision Support Systems” and “AI-driven Decision-making” |
| S3 |
“Predictive Analytics” and “AI” |
S8 |
“NLP” and “AI” |
| S4 |
“Computer-aided diagnostics” and “AI” |
S9 |
“Robot-assisted Surgery” and “AI” |
| S10 |
“Virtual Health Assistants and Chatbots” and “AI” |
S11 |
“AI-driven Decision-making” and “Healthcare Information Systems” |
Table 3.
Specification of CDSS making AI-driven decisions.
Table 3.
Specification of CDSS making AI-driven decisions.
| Author |
Main Idea
|
Advantage
|
Disadvantage
|
Simulation Environment
|
Dataset
|
| Comito, Falcone [33] |
|
|
Poor explainability Poor interpretability Overfitting Poor data availability |
Cyhon |
38,597 samples |
| Vasey, Nagendran [34] |
|
High transparency High reproducibility |
High complexity Poor adaptability Poor flexibility |
Python |
43,986 samples |
| Choudhury [35] |
|
High reliability High flexibility |
Poor privacy Poor integrity |
- |
273 samples |
| Liu, Barreto [36] |
|
|
Poor integrity Poor privacy |
Python |
215 samples |
| Amann, Blasimme [37] |
|
|
High complexity Poor interpretability Poor generalizability |
Python |
400 samples |
Table 4.
Specifications of predictive analytics applying AI-driven decision-making.
Table 4.
Specifications of predictive analytics applying AI-driven decision-making.
| Author |
Main Idea
|
Advantage
|
Disadvantage
|
Simulation Environment
|
Dataset
|
| Elvas, Nunes [38] |
|
High accuracy High interpretability High adaptability |
High complexity Bias Poor interpretability |
Python |
512,724 samples |
| Rehman, Farrakh [39] |
|
High transparency High interpretability Poor bias |
|
Python |
PIMA |
| Chen, Lim [40] |
|
High adaptability High scalability High flexibility |
Poor privacy Poor security Poor generalizability |
- |
15 samples |
| Wang, Zhao [41] |
|
High accuracy High scalability |
Poor integrity Poor privacy Poor complexity |
- |
130 samples |
| Hasan, Dhawan [42] |
|
|
|
Python |
14,000 samples |
Table 5.
Specifications of NLP applications applying AI-driven decision-making.
Table 5.
Specifications of NLP applications applying AI-driven decision-making.
| Author |
Main Idea
|
Advantage
|
Disadvantage
|
Simulation Environment
|
Dataset
|
| Afshar, Adelaine [43] |
|
High integrity High accuracy High scalability |
Poor interpretability Bias Poor generalizability |
Tensorflow |
12,500 samples |
| Elkin, Mullin [44] |
|
High accuracy High integrity High generalizability |
Poor interpretability Bias High complexity |
Keras |
2722 samples |
| Stewart, Chaturvedi [45] |
|
|
Poor interpretability Bias Poor generalizability poor complexity |
MATLAB |
60 samples |
| Joyce, Markossian [46] |
|
High accuracy High integrity High scalability |
High interpretability High complexity |
MATLAB |
2400 samples |
| Barrera, Torres [47] |
|
High accuracy High adaptability |
|
Python |
200,000 samples |
Table 6.
Specifications of CAD applications applying AI-driven decision-making.
Table 6.
Specifications of CAD applications applying AI-driven decision-making.
| Author |
Main Idea
|
Advantage
|
Disadvantage
|
Simulation Environment
|
Dataset
|
| Creswell, Vo [48] |
|
|
Poor explainability Poor interpretability Poor integrity Poor security |
Python |
281,550 samples |
| Tran, Sadeghi-Naini [49] |
|
|
Poor integrity Poor explainability |
Python |
25,856 samples |
| Ibrahim, Kibarer [50] |
|
High accuracy High integrity |
Poor integrity Poor generalizability Poor interpretability |
MATLAB |
600 samples |
| Shukla, Zakariah [51] |
|
High specificity High sensitivity High integrity |
Overfitting Poor interpretability |
Tensoorflow |
2012 samples |
| Khanna, Agarwal [52] |
|
High scalability High robustness |
High complexity Poor generalizability Poor interpretability |
Python |
16 samples |
Table 7.
Specifications of robot-assisted surgery applications applying AI-driven decision-making.
Table 7.
Specifications of robot-assisted surgery applications applying AI-driven decision-making.
| Author |
Main Idea
|
Advantage
|
Disadvantage
|
Simulation Environment
|
Dataset
|
| Zeineldin, Junger [53] |
|
High integrity High visualization High precision |
Poor interpretability Poor generalizability High complexity |
Keras |
1251 samples |
| Parry, Markowitz [54] |
|
High adaptability High precision |
Poor generalizability Bias |
MATLAB |
1684 samples |
| Kotha, Viswanath [55] |
|
|
Poor privacy Poor security |
Raspberry Pi |
425,087 samples |
| Kolbinger, Bodenstedt [56] |
|
High precision High accuracy High visualization High adaptability |
Poor generalizability Poor privacy |
Pytorch |
3000 samples |
| Ai, Pan [57] |
|
High accuracy High precision High robustness High stability |
Poor complexity Poor adaptability |
- |
100 samples |
Table 8.
Specifications of virtual health assistant and chatbots applications applying AI-driven decision-making.
Table 8.
Specifications of virtual health assistant and chatbots applications applying AI-driven decision-making.
| Author |
Main Idea
|
Advantage
|
Disadvantage
|
Simulation Environment
|
Dataset
|
| Wang, Gupta [58] |
|
High accessibility High scalability |
|
Python |
135,263 samples |
| Fan, Chao [59] |
|
High accessibility Poor latency High availability High privacy |
|
- |
16,519 samples |
| Chakraborty, Paul [60] |
|
|
|
Python |
20 samples |
| Esmaeilzadeh, Mirzaei [61] |
|
|
Poor generalizability Bias |
Tensorflow |
105 samples |
| Chow, Wong [62] |
|
High availability High scalability |
Poor adaptability Poor privacy |
MATLAB |
20 samples |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).