Introduction
Anterior segment optical coherence tomography (AS-OCT) uses low coherence interferometry than can visualize the corneal structures with an ultra-high axial resolution of 3.6 μm in tissue [
1]. AS-OCT has been successfully used to depict the corneal features in infectious keratitis of various etiologies: corneal alterations have been described for bacterial keratitis, including hyper-reflective lesions (infiltrates), epithelial defect, stromal oedema, stromal thinning, hyper-reflective material on the corneal anterior or endothelial surface [
2,
3,
4,
5].
Modern keratorefractive surgery is characterized by the use of the femtosecond laser, which creates a surgical interface both in laser in situ keratomileusis (LASIK), where a flap is created prior to excimer laser ablation, and in keratorefractive lenticule extraction (KLEx), where an intrastromal lenticule is delineated and removed through a small incision [
6]. The OCT features of an infection developing after LASIK and KLEx may considerably differ from the classical presentation, as it usually originates in the surgical interface and not through an epithelial disruption [
7,
8,
9].
The involvement of the surgical interface at AS-OCT in infectious keratitis after keratorefractive surgery has not been evaluated by previous studies. We therefore reviewed the OCT features of 4 cases of infectious keratitis occurring after LASIK and KLEx.
Case Reports
Patient Selection
The clinical records of patients developing an infection after LASIK and KLEx where reviewed. The diagnosis of corneal infection was based upon previously validated criteria [
10]. Our refractive surgery center keeps a record of all proved or suspected infective complications occurred within the first post-operative 12 months. The diagnosis was based on slitlamp examination (corneal infiltrates compatible with infection, hyperemia, oedema), subjective symptoms (pain, blurred vision), culture. Such records were reevaluated by the authors and classified as culture-proven infectious keratitis, probable culture-negative infectious keratitis, non-infectious keratitis. AS-OCT had been performed only in the most recent cases: 4 cases of infectious keratitis undergone OCT examination were retrieved (2 after LASIK and 2 after KLEx). All cases were culture-negative.
Infectious Keratitis Post-Femtosecond LASIK
Patient #1
This 36-year-old woman developed an infiltrate in OD 3 days after bilateral femtosecond LASIK for myopia.
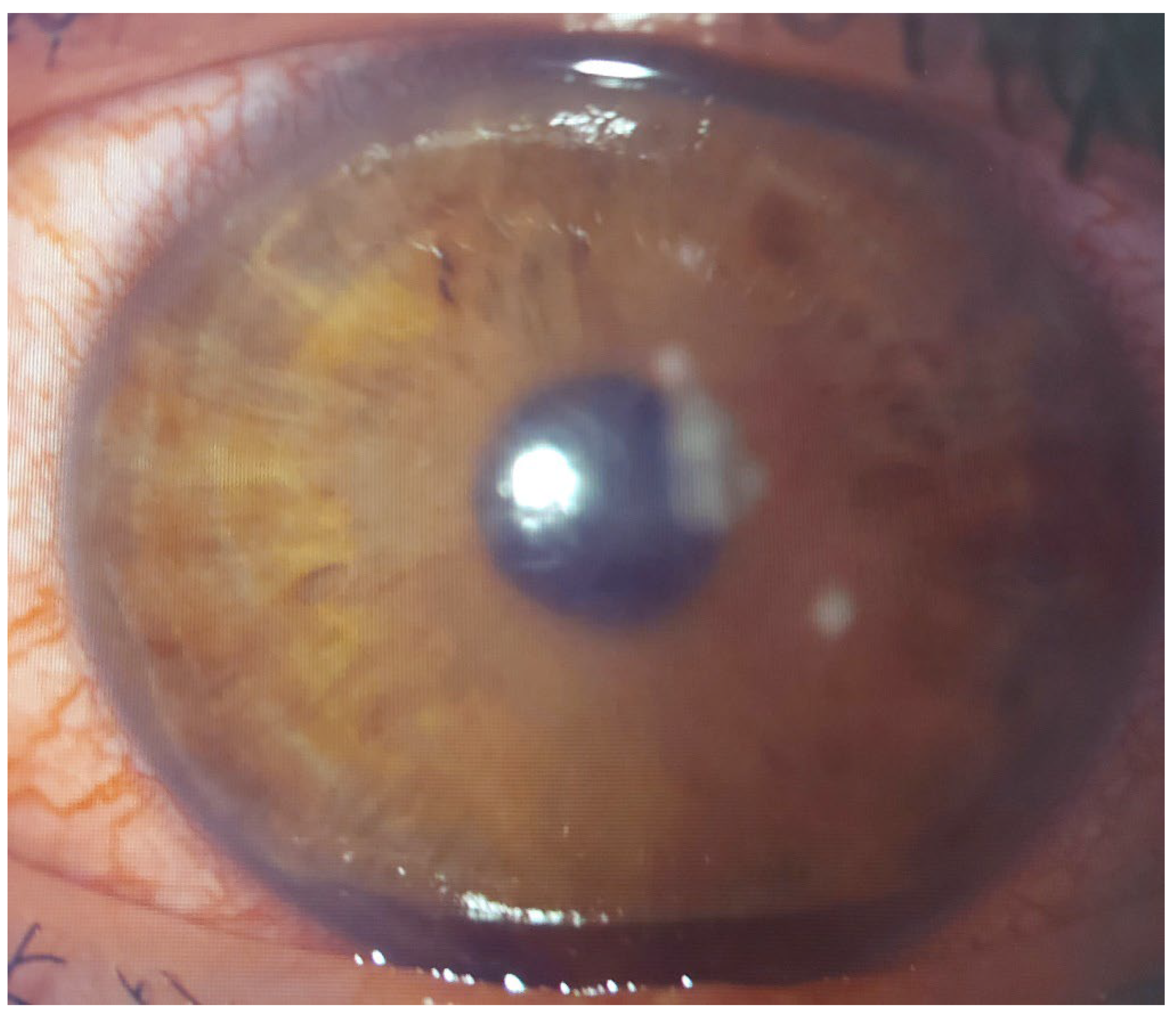
At presentation, a round paracentral infiltrate was evident at slitlamp (
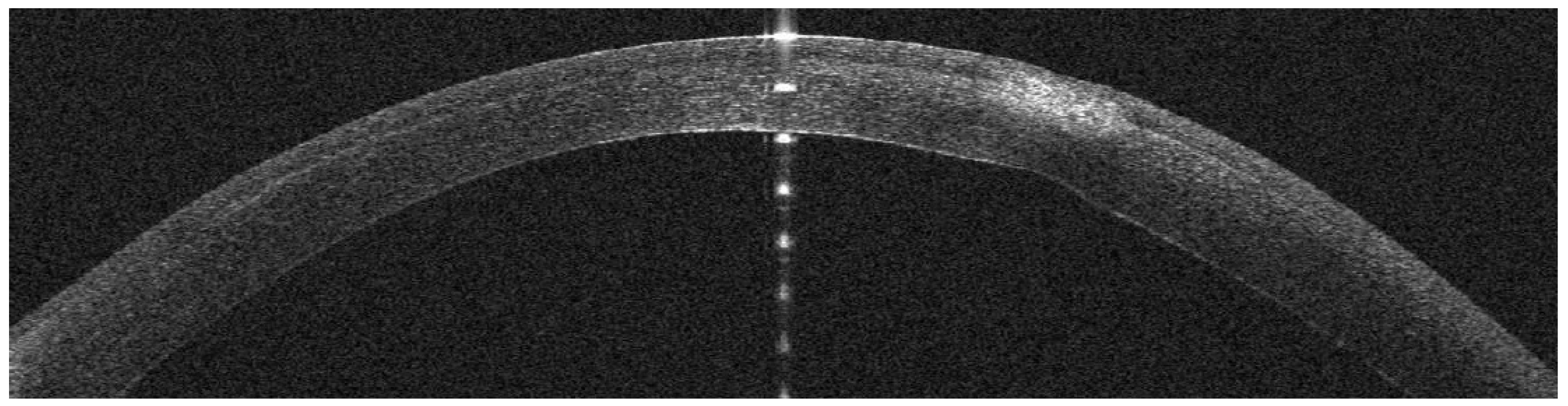
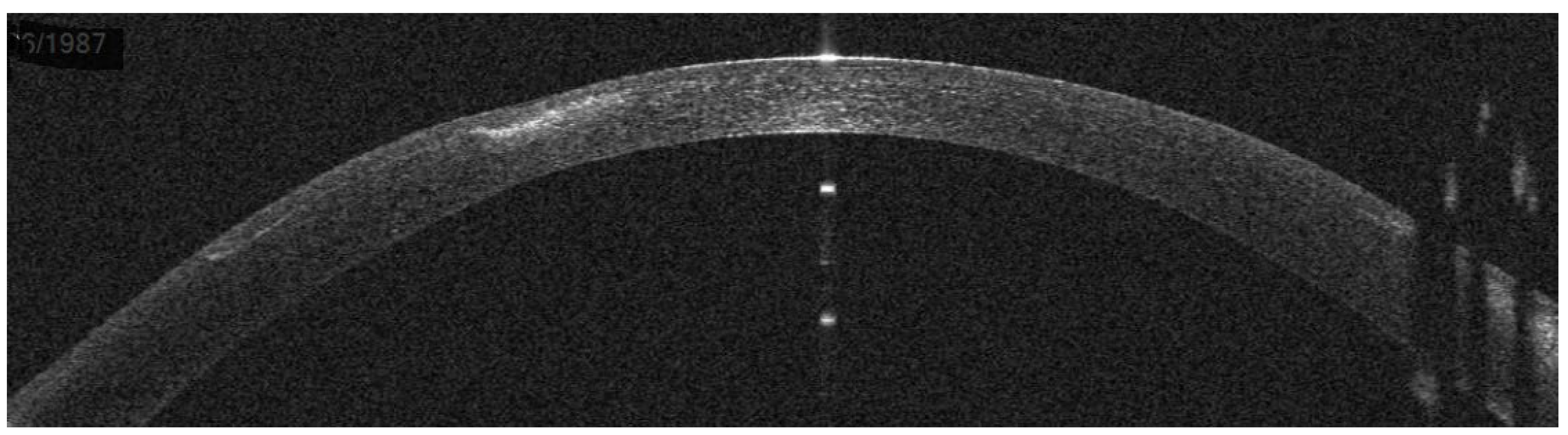
Figure 1); the AS-OCT revealed a hyper-reflective area in the surgical interface, causing posterior shadowing; the overlying flap and epithelium were not damaged (
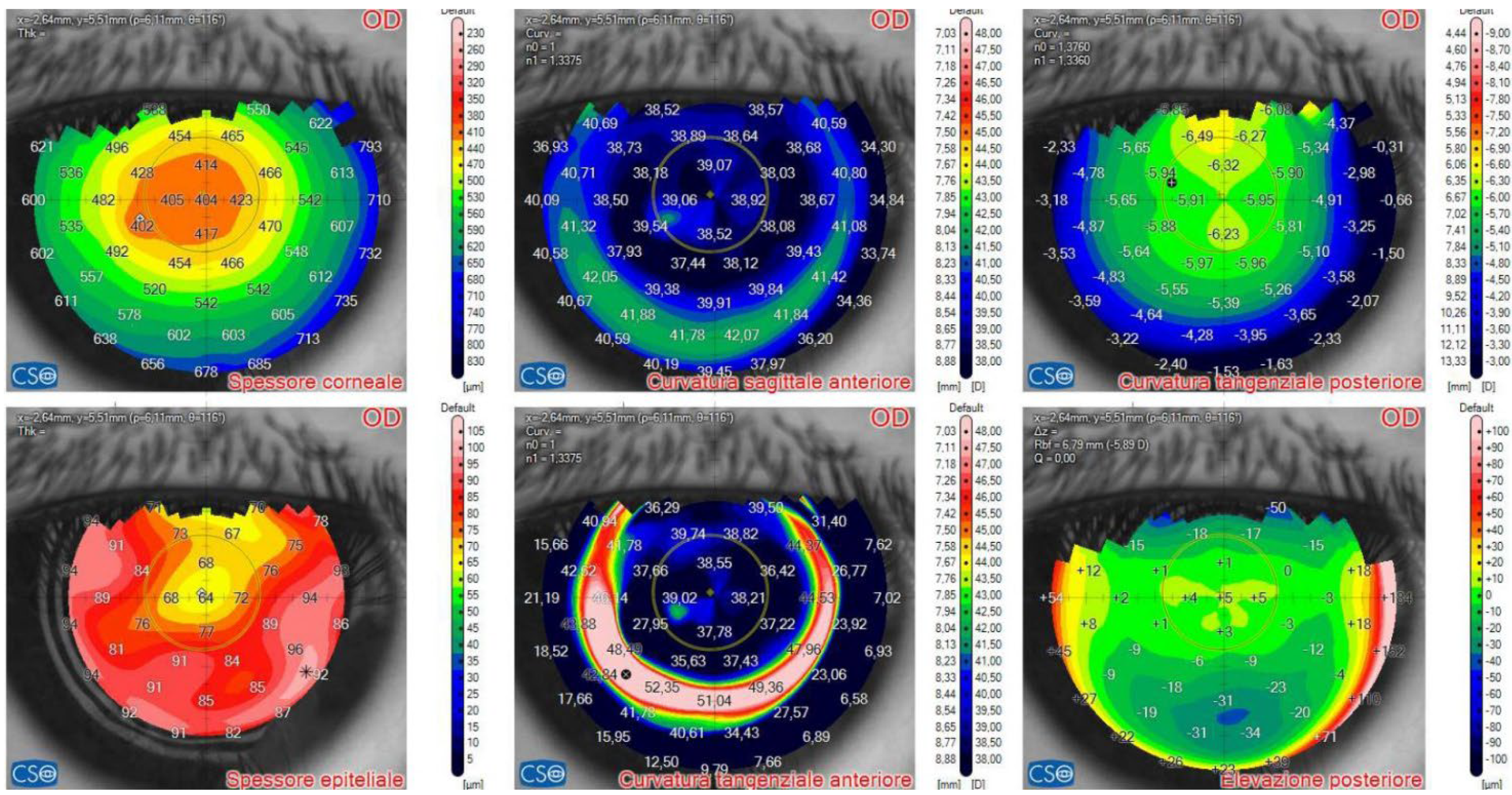
Figure 2). On OCT tomography, the anterior tangential map showed an area of increased curvature corresponding to the infiltrate and the epithelial map revealed moderate thickening peripherally to the infiltrate (
Figure 3). Topical treatment with fortified tobramycin, moxifloxacin and 0.6% iodopovidone was started.
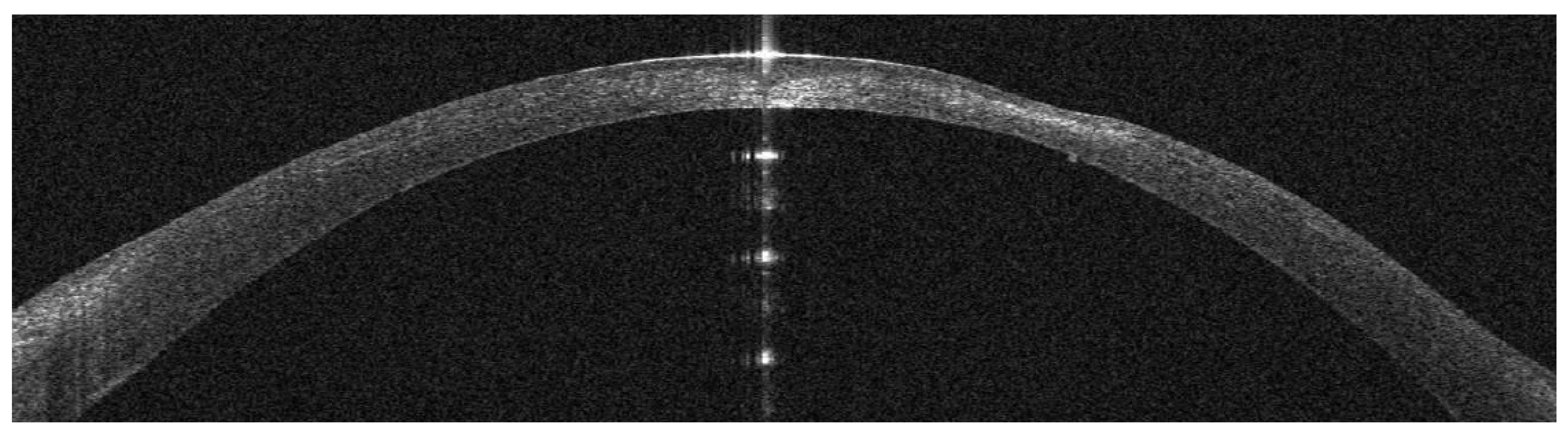
Two days after presentation, the patient complained of blurred vision; at the slitlamp, the infiltrate appeared denser and a surrounded by a ring (
Figure 4). On AS-OCT, the infiltrate was thicker, localized stromal oedema was present, and the temporal interface was separated by a layer of fluid, causing the ring effect at the slitlamp (
Figure 5).
Nine days after presentation, symptoms had resolved and the infiltrate had a cicatricial aspect, with neat margins and no surrounding oedema (
Figure 6). At AS-OCT, an hyperdense area was still present, with an overlying stromal thinning (
Figure 7). At OCT tomography, a diffuse epithelial oedema was observed (
Figure 8).
At 1 month, the infiltrate had regressed to a small nubecola (
Figure 9), the stromal thickness had recovered (
Figure 10), the tangential anterior map was regular and epithelial oedema had resolved (
Figure 11). Unaided visual acuity was 20/16.
Patient #2
This 35-year-old woman developed an infiltrate in OD 18 days after bilateral femtosecond LASIK for myopia.
At presentation, a small round superior infiltrate surrounded by mild oedema was evident at slitlamp (
Figure 12); the AS-OCT revealed a thin hyper-reflective area in the surgical interface; the overlying flap and epithelium were not damaged, and the interface was slightly hyperdense (
Figure 13). Topical treatment was administered as in patient #1.
Three days after presentation, the infiltrate had resolved; only slight interface inflammation was evident (
Figure 14). Unaided visual acuity was 20/20.
Infectious Keratitis Post-KLEx
Patient #3
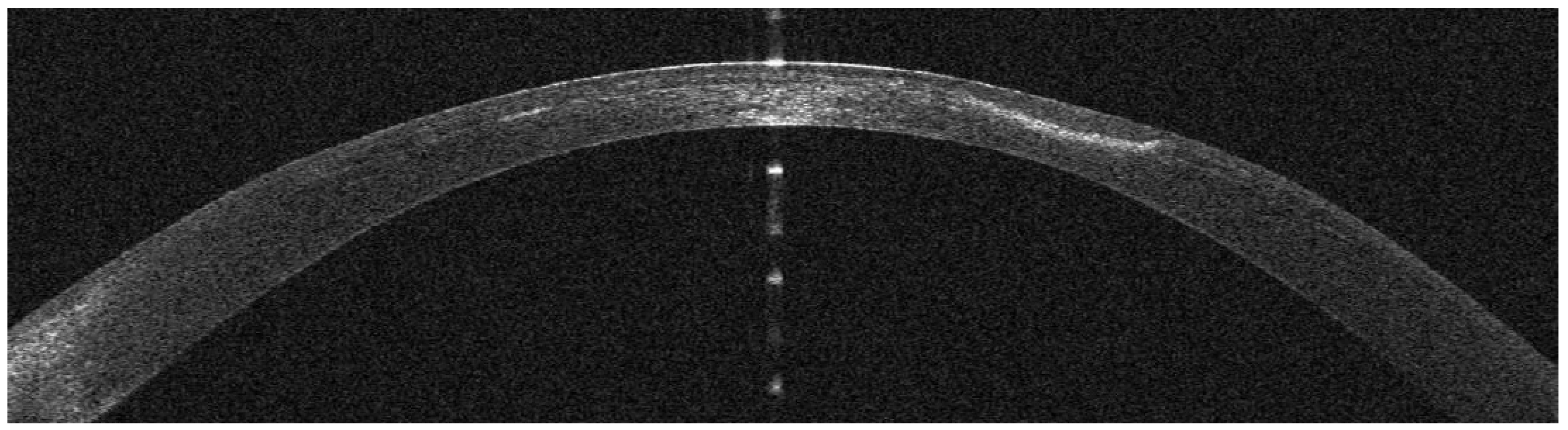
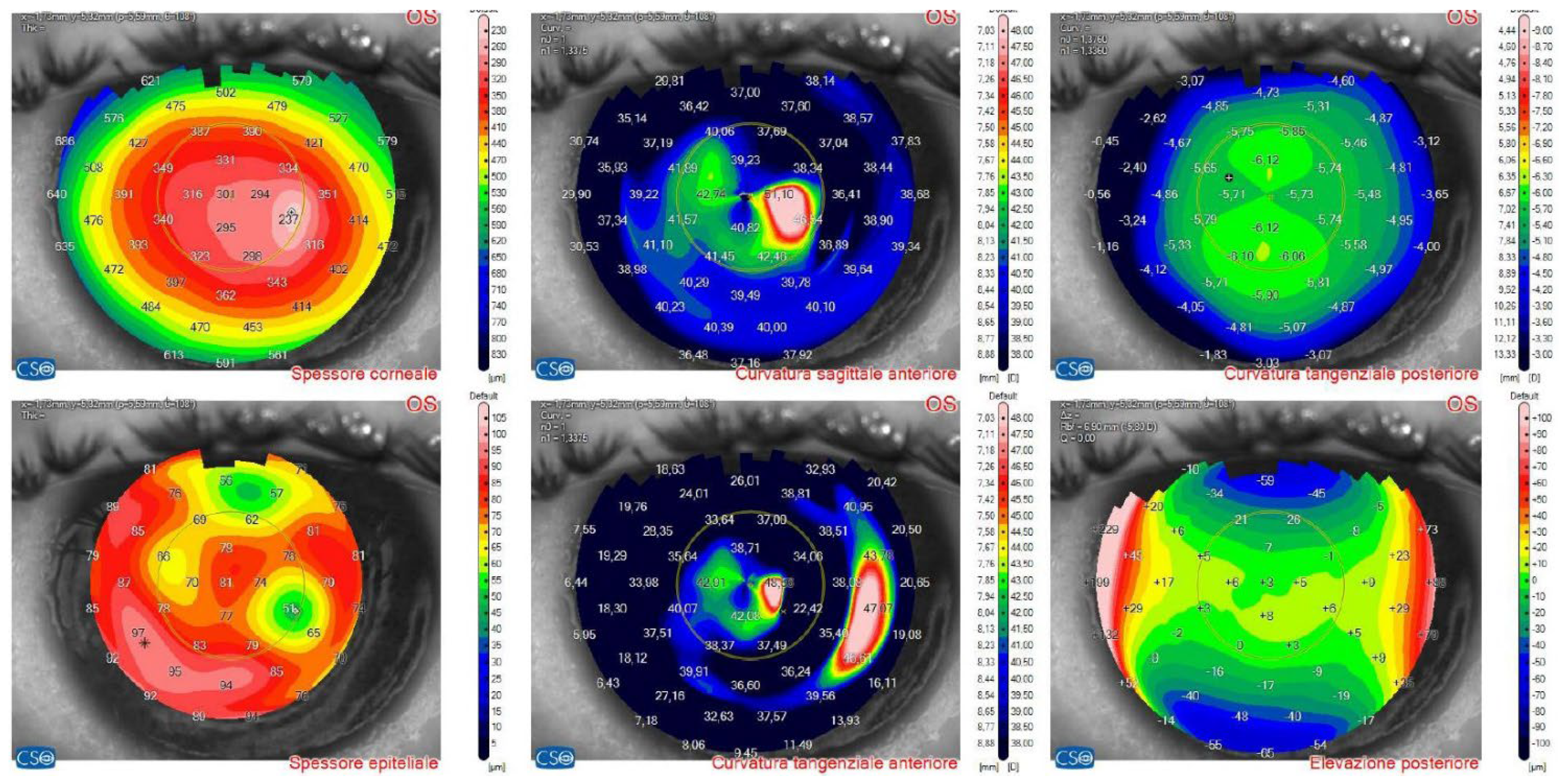
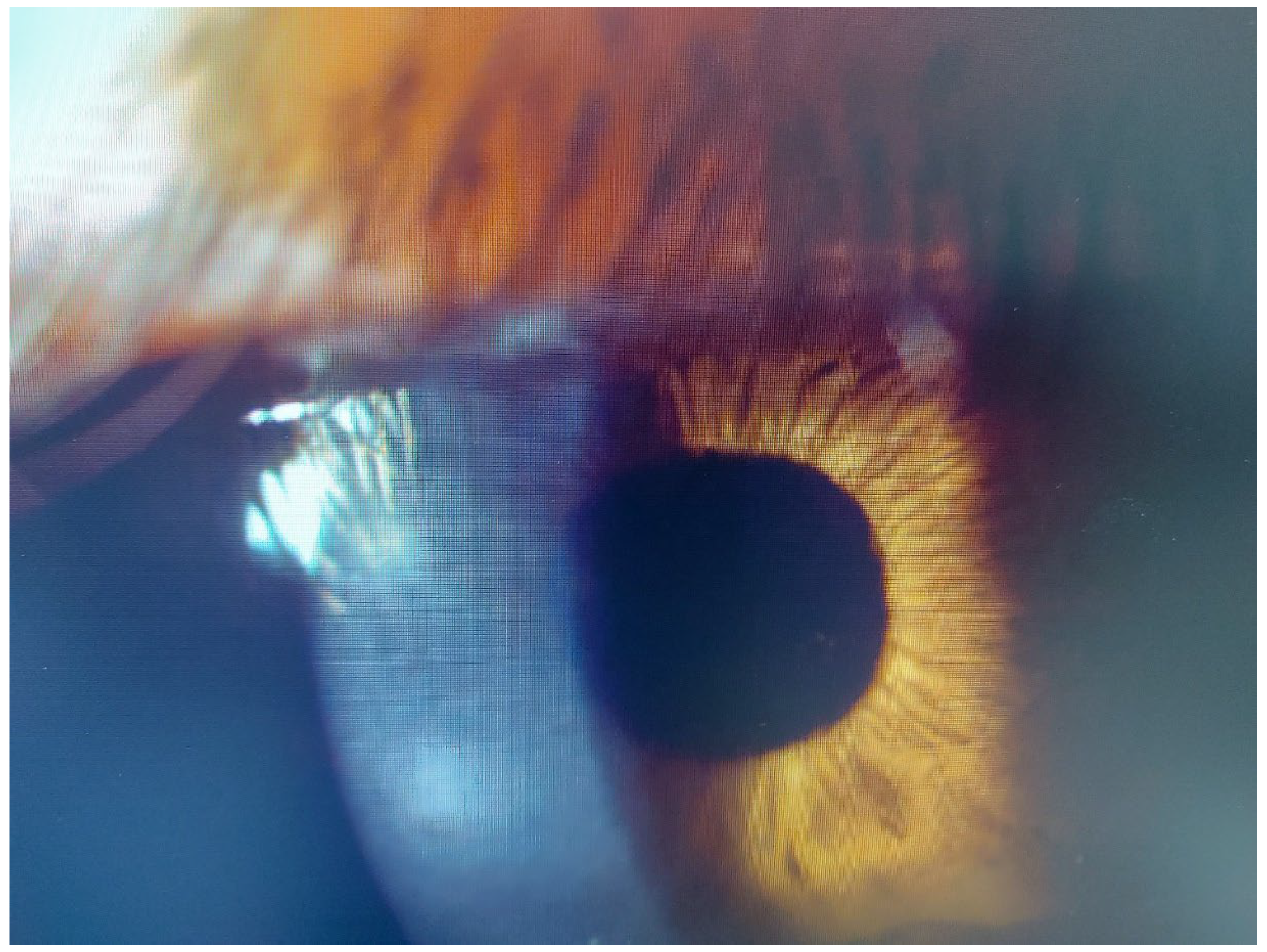
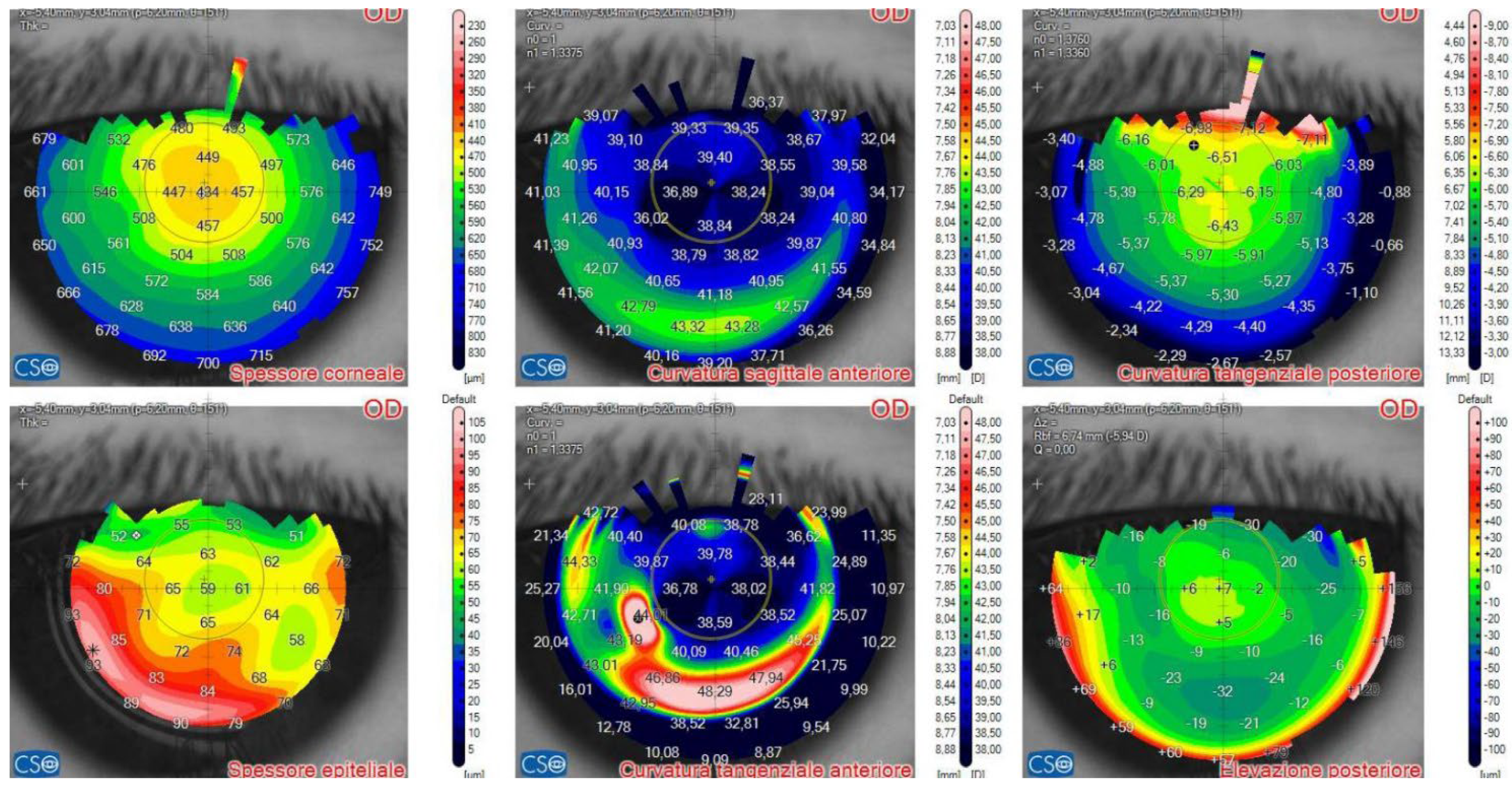
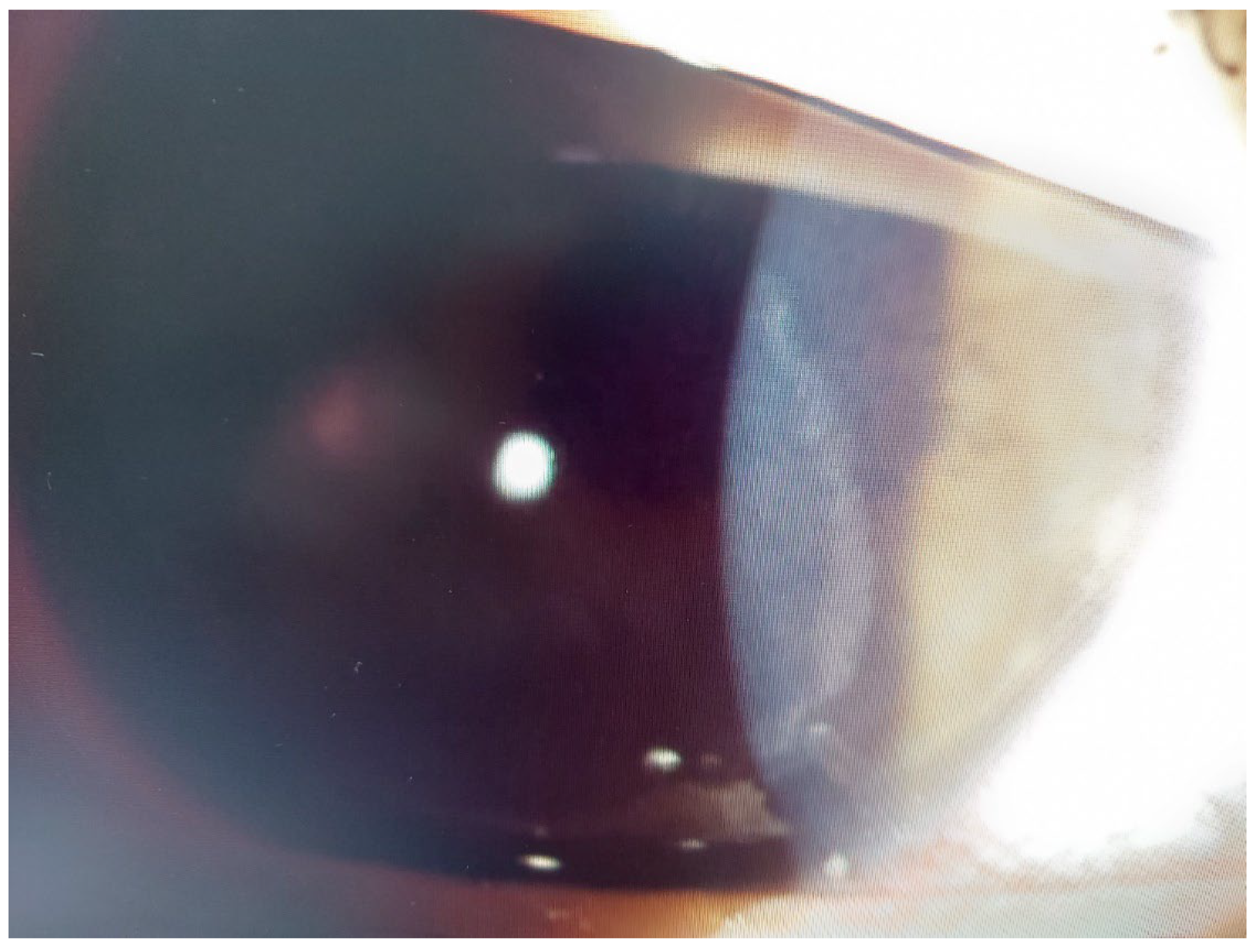
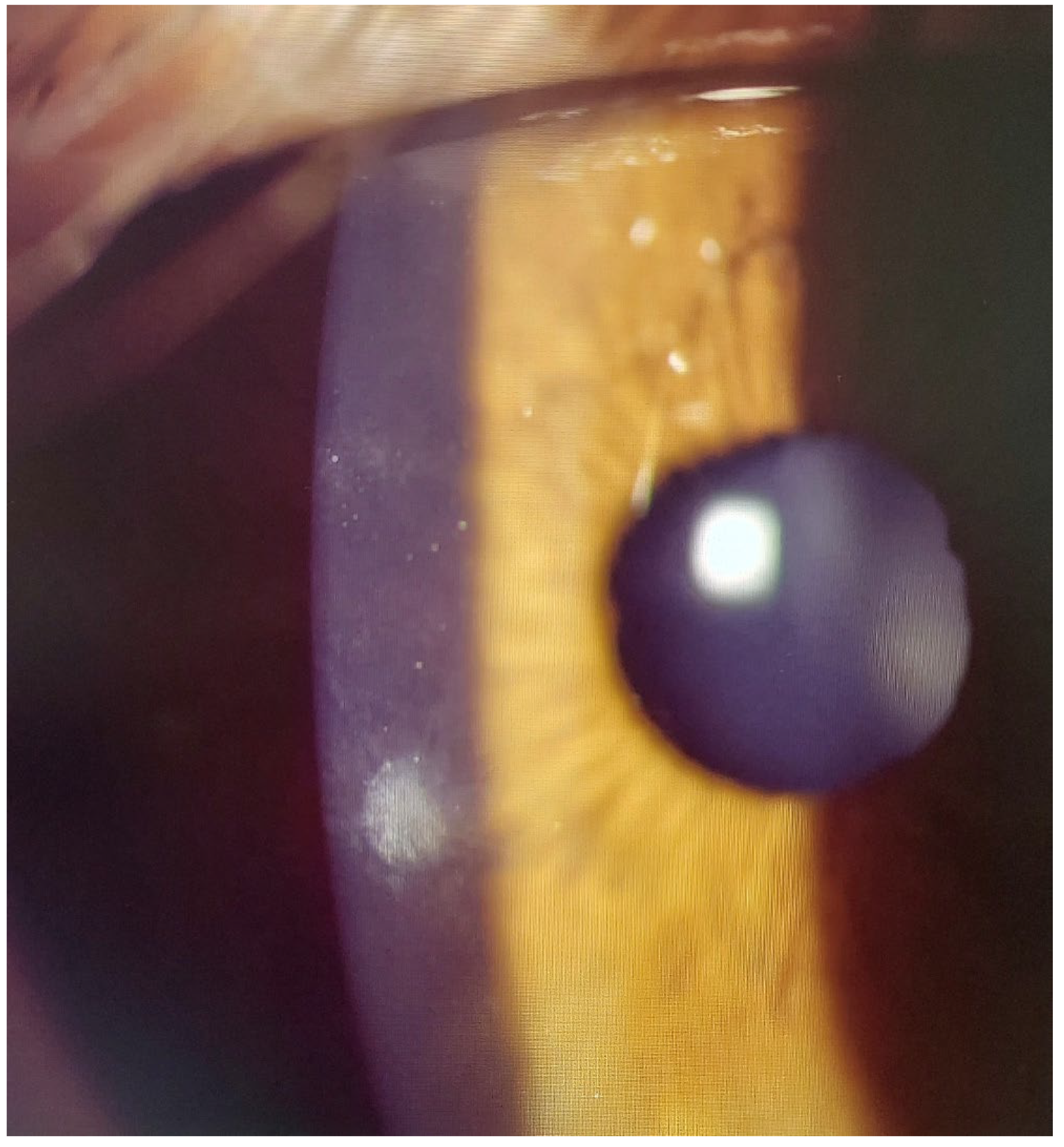
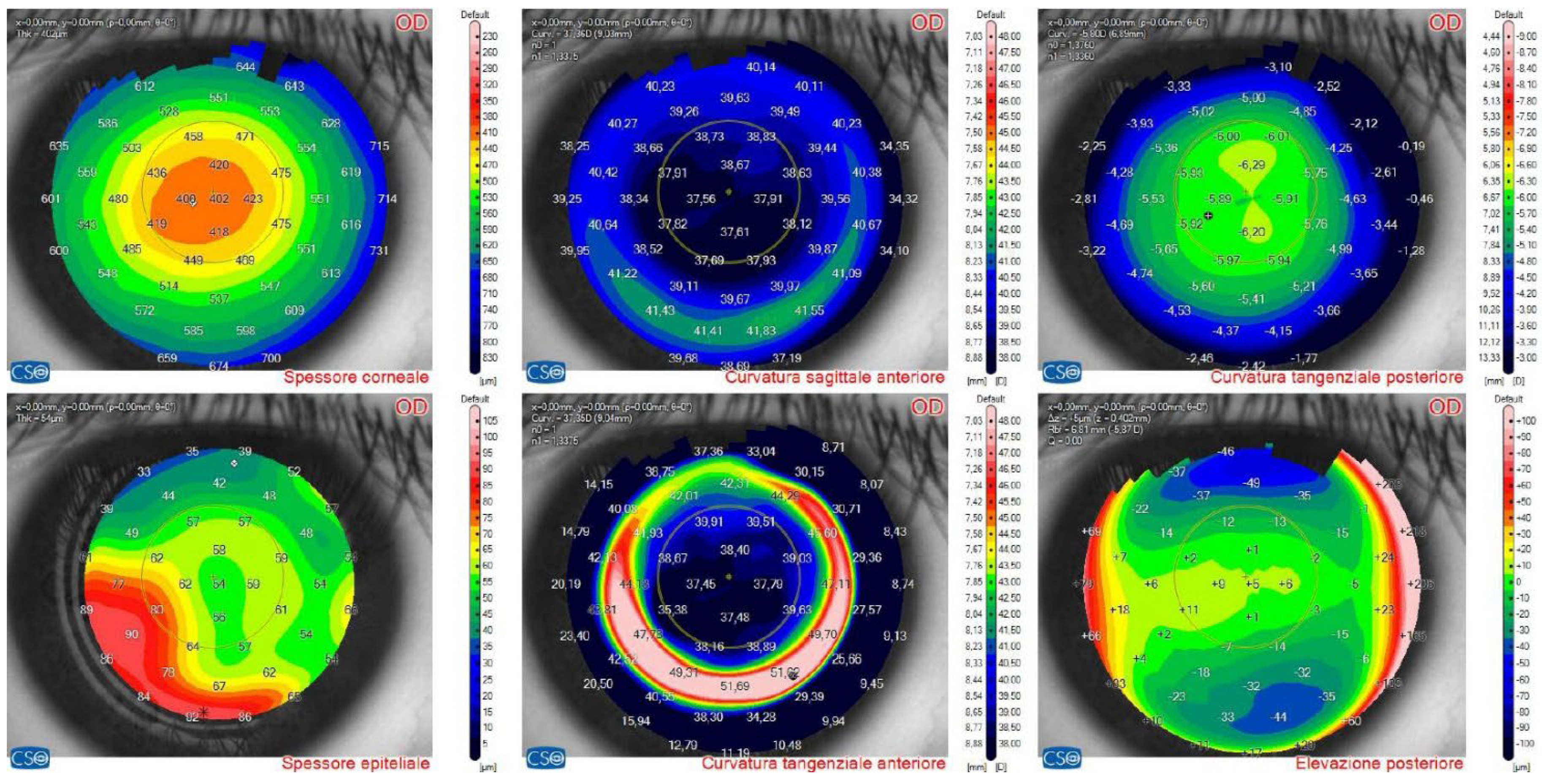
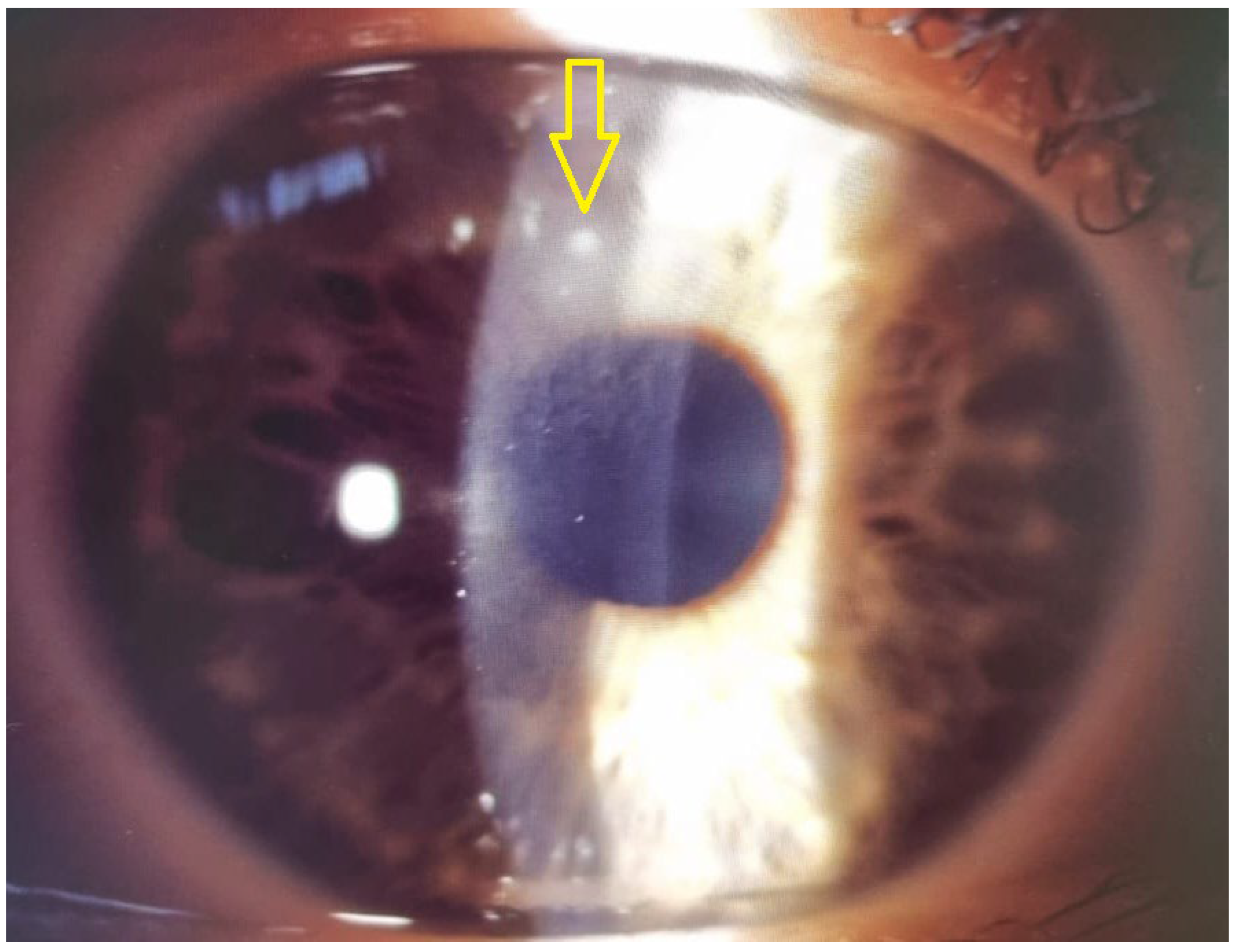
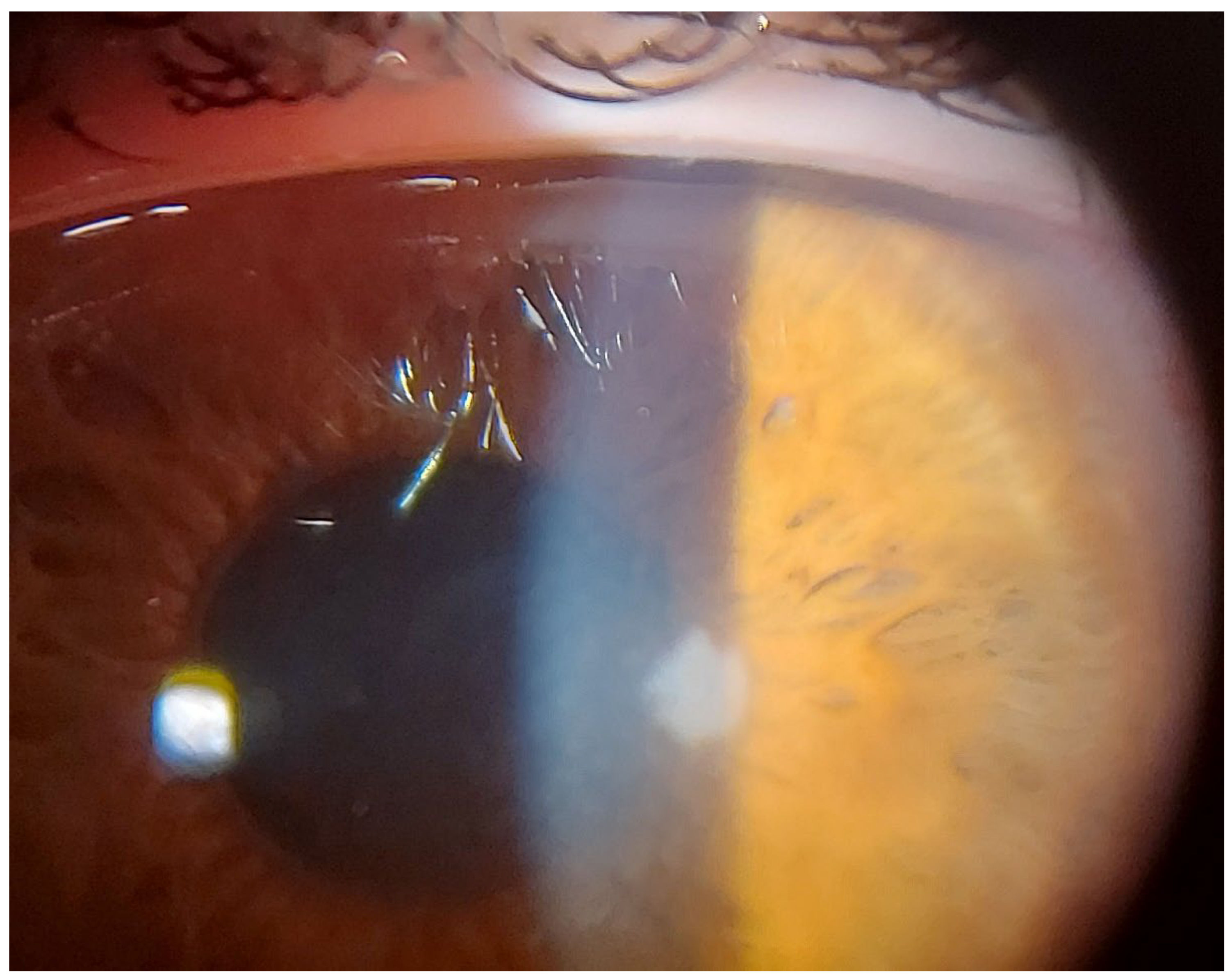
This 34-year-old woman developed an infiltrate in OS 24 days after bilateral KLEx for myopia. At slitlamp, a paracentral, well-defined infiltrate was visible (
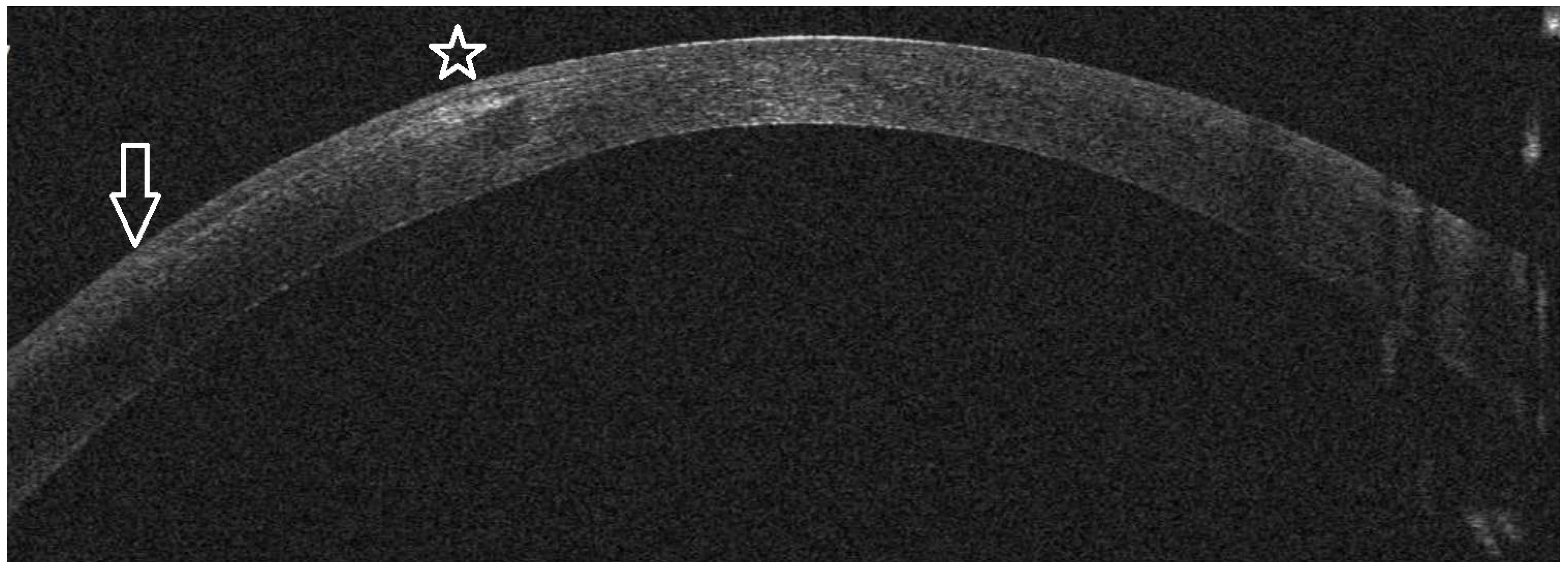
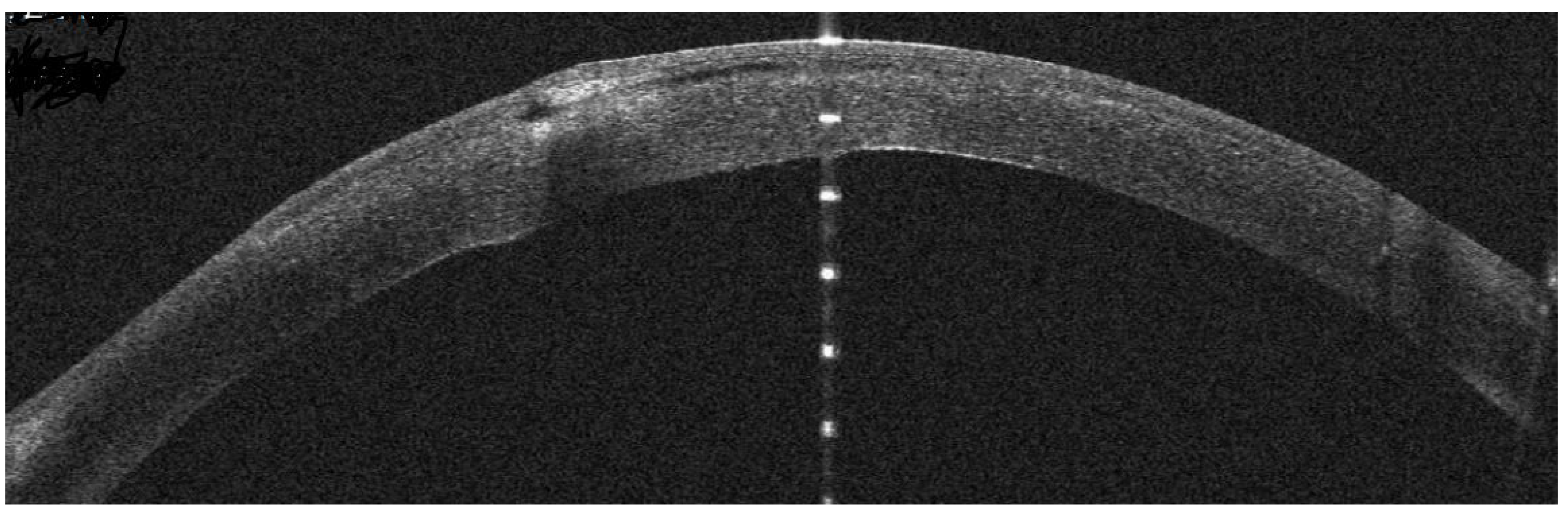
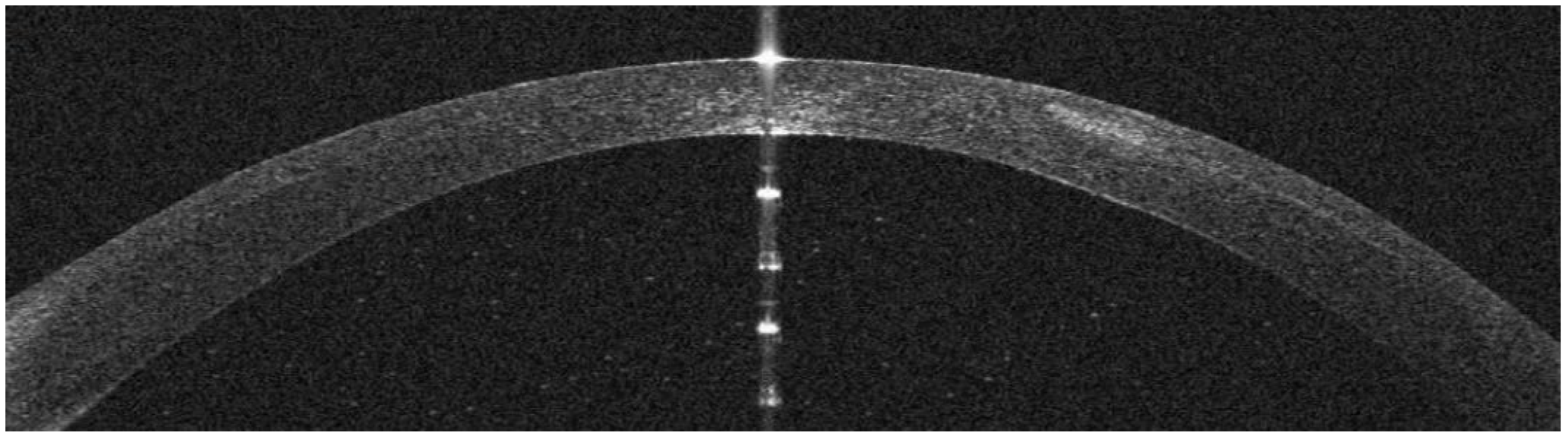
Figure 15), corresponding on AS-OCT to a localized hyper-reflective area in the interface (
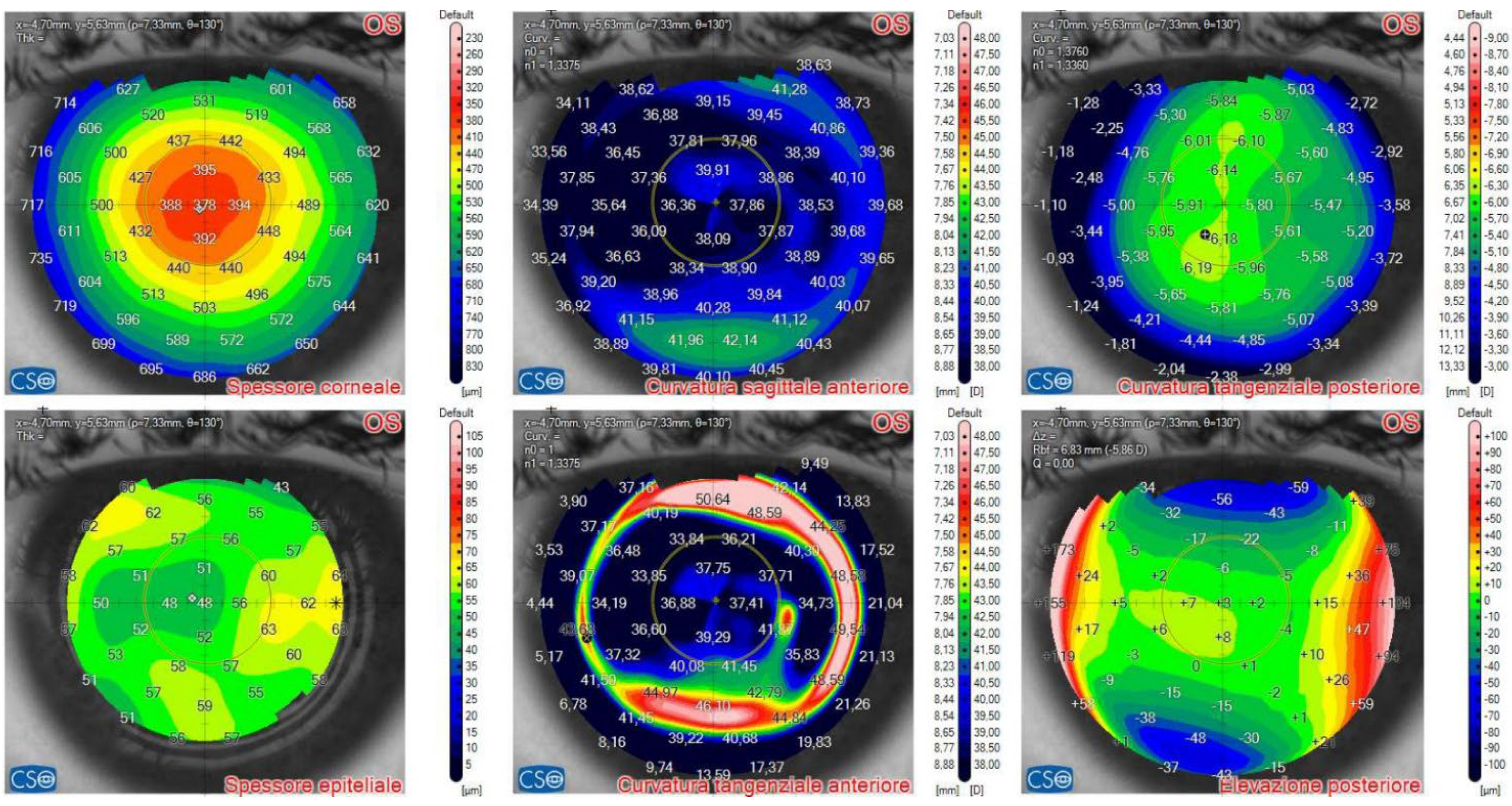
Figure 16) and causing a slight irregularity on anterior tangential tomography (
Figure 17). Topical treatment was started as in patient #1.
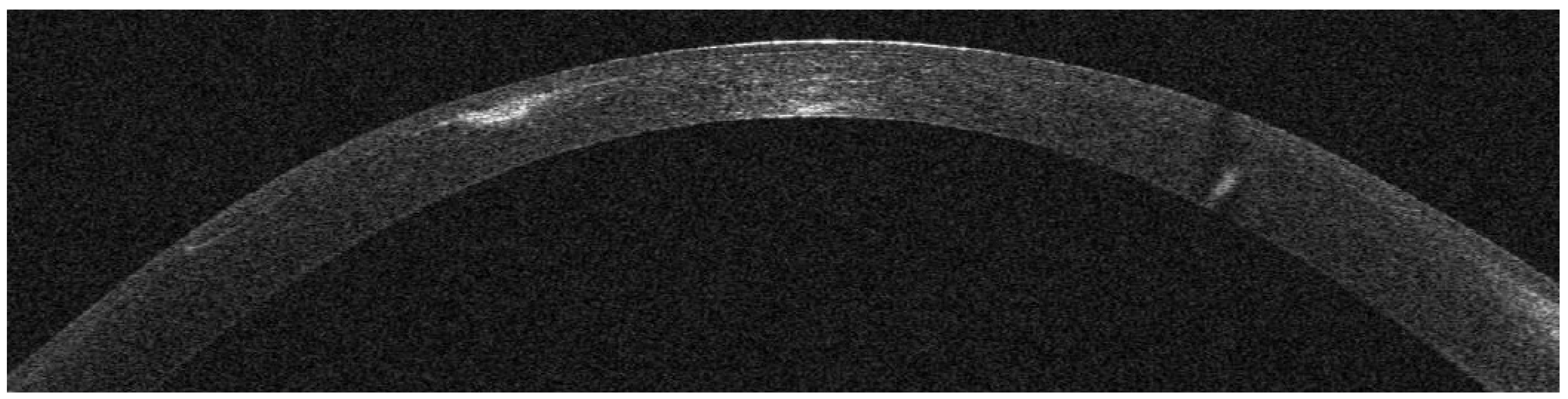
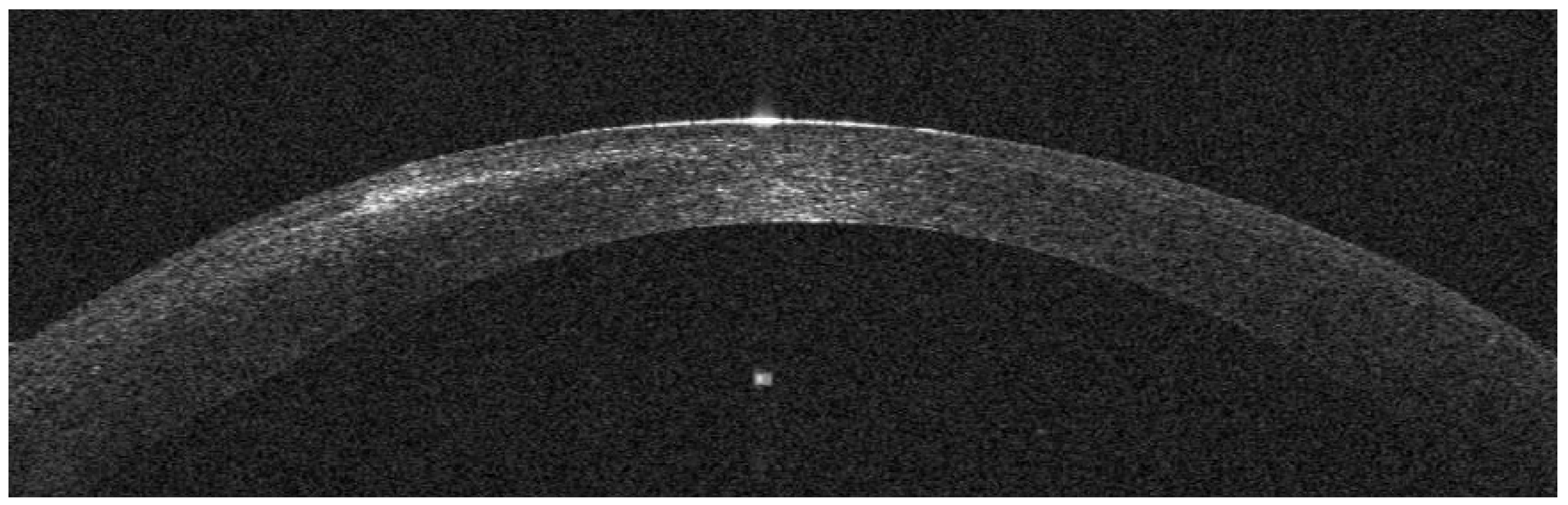
Seven days after presentation, the infiltrate was less defined, and was associated to interface inflammation and oedema (
Figure 18). On AS-OCT sections and tomography, a generalized corneal thinning was evident, more pronounced in the lesion area, locally thick only 237µm, with a global epithelial oedema sparing the lesion area (
Figure 19 and
Figure 20).
Figure 18.
(patient #3). Left eye, corneal infiltrate 31 days after KLEx, evolving to interface oedema and inflammation.
Figure 18.
(patient #3). Left eye, corneal infiltrate 31 days after KLEx, evolving to interface oedema and inflammation.
Figure 19.
(patient #3). Left eye, corneal infiltrate 31 days after KLEx. At AS-OCT, the infiltrate has expanded and the overlying stroma has considerably thinned.
Figure 19.
(patient #3). Left eye, corneal infiltrate 31 days after KLEx. At AS-OCT, the infiltrate has expanded and the overlying stroma has considerably thinned.
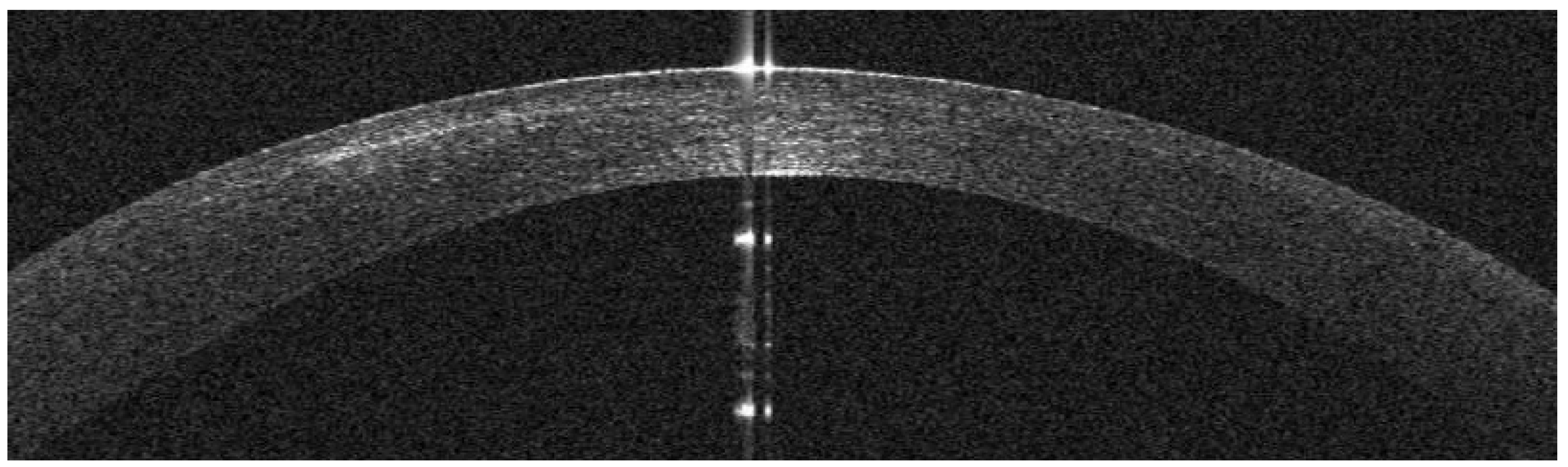
Figure 19.
(patient #3). Left eye, corneal infection 3 months after KLEx. At AS-OCT, the infiltrate has been replaced by a thinner scar (hyper-reflective), over which stroma and epithelium (with medium reflectivity) have filled the tissue loss.
Figure 19.
(patient #3). Left eye, corneal infection 3 months after KLEx. At AS-OCT, the infiltrate has been replaced by a thinner scar (hyper-reflective), over which stroma and epithelium (with medium reflectivity) have filled the tissue loss.
Figure 20.
(patient #3). Left eye, corneal infiltrate 31 days after KLEx. At AS-OCT tomography, an overall corneal thinning is present (above, left), the infiltrate is causing more irregular curvature on axial (above, center) and tangential curvature (bottom, center). The epithelium has thickened, except in the area overlying the infiltrate (bottom, left).
Figure 20.
(patient #3). Left eye, corneal infiltrate 31 days after KLEx. At AS-OCT tomography, an overall corneal thinning is present (above, left), the infiltrate is causing more irregular curvature on axial (above, center) and tangential curvature (bottom, center). The epithelium has thickened, except in the area overlying the infiltrate (bottom, left).
Figure 20.
(patient #3). Left eye, corneal infection 3 months after KLEx. At AS-OCT tomography, the corneal thinning is reduced (above, left), the profile on axial (above, center) and tangential curvature (bottom, center) is more regular, the epithelium has returned to normal thickness (bottom, left).
Figure 20.
(patient #3). Left eye, corneal infection 3 months after KLEx. At AS-OCT tomography, the corneal thinning is reduced (above, left), the profile on axial (above, center) and tangential curvature (bottom, center) is more regular, the epithelium has returned to normal thickness (bottom, left).
Two months later the infectious process had resolved and the cornea had recovered the post-operative thickness, with a compensatory reformation of stroma and epithelium (
Figure 21 and
Figure 22). Visual acuity was 20/25 with +3 x 83°.
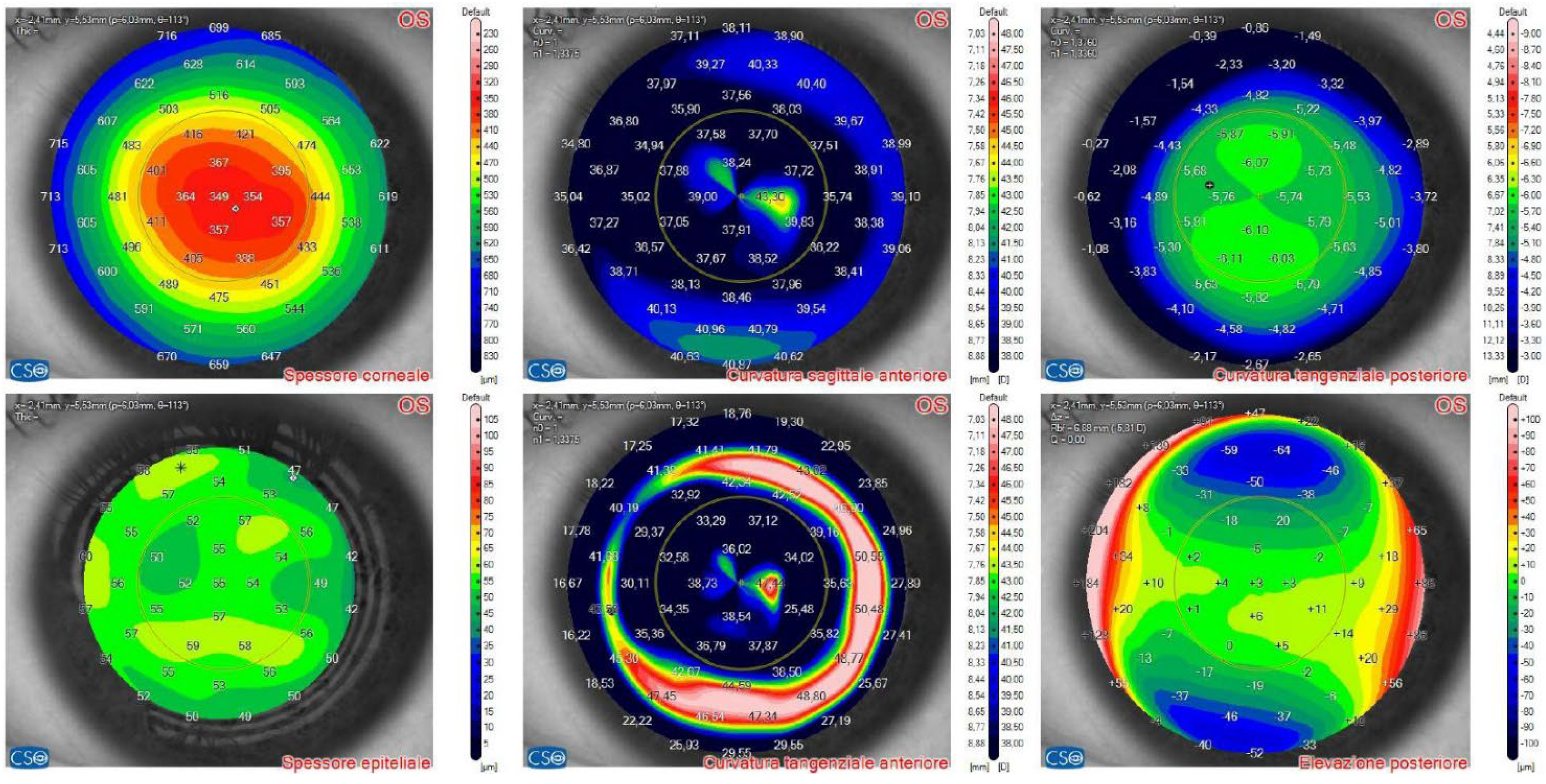
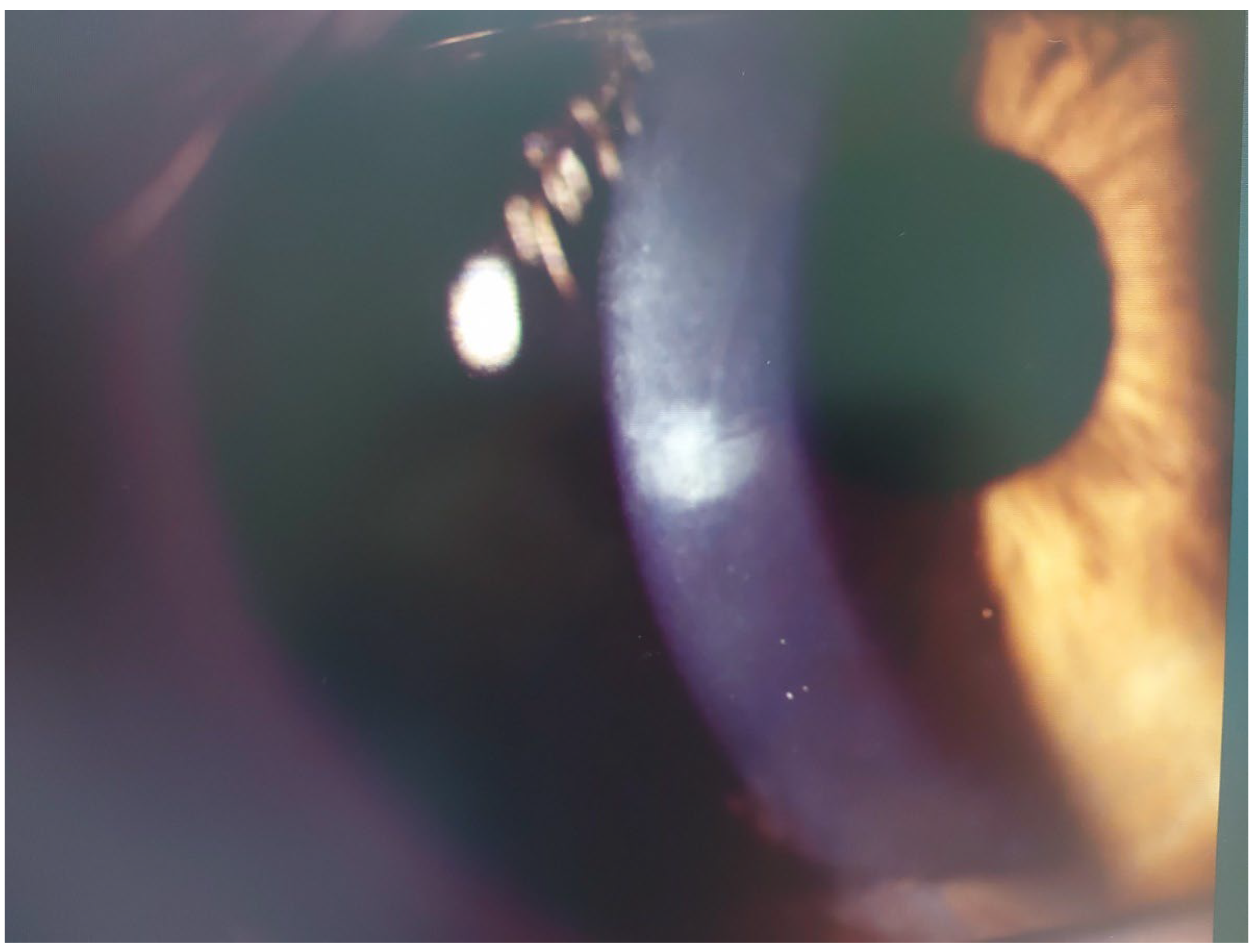
Figure 21.
(patient #4). Left eye, multiple corneal infiltrates 2 days after KLEx.
Figure 21.
(patient #4). Left eye, multiple corneal infiltrates 2 days after KLEx.
Figure 21.
(patient #4). Left eye, multiple corneal infiltrates 2 days after KLEx. On AS-OCT, one of the infiltrates is centered in the surgical interface, expanding externally, with a thin hyper-reflective line corresponding to the inflamed interface.
Figure 21.
(patient #4). Left eye, multiple corneal infiltrates 2 days after KLEx. On AS-OCT, one of the infiltrates is centered in the surgical interface, expanding externally, with a thin hyper-reflective line corresponding to the inflamed interface.
Patient #4
Two days after bilateral KLEx for myopia, this 31-year-old man developed multiple infiltrates in the surgical interface, causing interface inflammation (
Figure 23 and
Figure 24). Prompt topical treatment resolved the picture and a final 20/20 unaided visual acuity was obtained.
AS-OCT Features
In all 4 cases, a hyper-reflective infiltrate in the surgical interface was the presenting feature. An epithelial damage was only found in patient #3 at a later stage. Interface inflammation was revealed by its hyper-reflectivity, assuming in case #3 the characteristic of a diffuse lamellar keratitis (DLK), causing considerable thinning due to stromal reabsorption. In case 1, where the ring pseudo-infiltrate posed a differential diagnosis with an acanthamoeba keratitis, a fluid layer was well demonstrated by OCT, thus excluding the acanthamoeba etiology.
Discussion
In the present series of post-refractive infections, AS-OCT was successfully used to picture all the inflammatory phases, evidencing interface inflammation, stromal oedema, fluid accumulation, changes in stromal and epithelial thickness.
AS-OCT during primary infectious keratitis can differentiate scars from infiltrates, both hyper-reflective, the latter presenting with an overlying epithelial defect or “opaque” epithelium, and with rounder and less defined margins [
4]. In our cases, where the infection started at the surgical interface, the epithelium was not interrupted at presentation, developing oedema in more advanced phases, and only in 1 case presenting a late defect. Post-infectious scars were in our series thinner and covered by thickened epithelium. AS-OCT has been also used to quantify post-infectious scars and irregularities [
11].
Peculiar features of
acanthamoeba keratitis (often clinically showing a ring infiltrate) at AS-OCT have been described, consisting in superficial hyper-reflective infiltrates, with stromal oedema, hyper-reflective stromal bands (due to radial keratoneuritis) and microcysts [
12,
13]. In our case #1, a ring pseudo-infiltrate was evident at slitlamp, but at AS-OCT its origin was readily identified as being the edge of the fluid collection in the surgical interface, in the absence of all the other amoebic characteristics.
The use of AS-OCT in infectious keratitis after refractive surgery has been the subject of few articles, reporting interface infiltrates, flap perforation, opaque epithelium [
7,
8,
9]; in more severe cases, pronounced oedema and endothelial plaques [
8]. Around the infiltrate, the surgical interface appeared denser in one case of presumed bacterial keratitis in KLEx [
7]. In case of mycobacterial keratitis after LASIK, the OCT could differentiate epithelial from stromal opacity [
9]. After healing, a hyper-reflective interface was observed, corresponding to clinical haze [
14].
DLK is an uncommon complication of LASIK [
15] and KLEx [
16]. It is caused by an immune reaction to chemical and biological substances introduced in the interface (including products of sterilization, glove powder, ink) [
17] and to excess energy in the femtosecond laser energy [
18]. In more severe cases, it can lead to stromal reabsorption, first compensated by epithelial thickening, then by stromal reformation [
15]. In our patient #3, a similar pattern was observed during the healing phase; stromal reabsorption was not limited to the area of the infiltrate, but involved the whole surgical interface. Similarly to the case reported by Reinstein et al. [
16], our case lacked the cellular infiltration at slitlamp, typical of post-LASIK DLK [
15]. Such circumstances may suggest the prudent use of topical steroids associated to the antibiotic treatment.
The limitations of this study are the small sample, which is justified by the rarity of the condition, and the absence of a positive culture, which is equally rare, given the intrastromal nature of all lesions.
Conclusion
In 4 cases of infectious keratitis post-keratorefractive surgery with femtosecond lasers, AS-OCT provided an excellent picture of the infiltrate and the associated abnormalities, such as stromal oedema, interface inflammation, stromal reabsorption and reformation, epithelial changes, and fluid layers, providing a precise mean to follow the evolution of the lesions and to confirm the efficacy of the treatment.
Author Contributions
Conceptualization, A.L., S.V.F. and G.D.B.; Methodology, A.L. and S.V.F.; Software, C.C.; Validation, G.D.B., M.P. and C.C.; Formal Analysis, A.L. and M.P.; Investigation, A.L.; Resources, M.P.; Data Curation, S.V.F. and C.C.; Writing—Original Draft Preparation, A.L. and M.P.; Writing—Review and Editing, A.L., S.V.F., G.D.B., C.C. and M.P.; Visualization, S.V.F.; Supervision, A.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Siena Eye Laser (protocol code 11/2024, 8 January2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Han, S.B.; Liu, Y.C.; Noriega, K.M.; Mehta, J.S. Applications of anterior segment optical coherence tomography in cornea and ocular surface diseases. J Ophthalmol 2016, 4971572. [Google Scholar] [CrossRef]
- Konstantopoulos, A.; Kuo, J.; Anderson, D.F.; Hossain, P.N. Assessment of the use of anterior segment optical coherence tomography in microbial keratitis. Am J Ophthalmol 2008, 146, 534–542. [Google Scholar] [CrossRef]
- Konstantopoulos, A.; Yadegarfar, G.; Fievez, M.; Anderson, D.F.; Hossain, P. In vivo quantification of bacterial keratitis with optical coherence tomography. Invest Ophthalmol Vis Sci 2011, 52, 1093–1097. [Google Scholar] [CrossRef]
- Soliman, W.; Fathalla, A.M.; El-Sebaity, D.M.; Al-Hussaini, A.K. Spectral domain anterior segment optical coherence tomography in microbial keratitis. Graefes Arch Clin Exp Ophthalmol 2013, 251, 549–553. [Google Scholar] [CrossRef]
- Abdelghany, A.A.; D’Oria, F.; Alio Del Barrio, J.; Alio, J.L. The value of anterior segment optical coherence tomography in different types of corneal infections: An update. J Clin Med 2021, 10, 2841. [Google Scholar] [CrossRef]
- Refr Surg in 2020.
- Li, J.; Ren, S.-W.; Dai, L.-J.; Zhang, B.; Gu, Y.-W.; Pang, C.-J.; Wang, Y. Bacterial keratitis following small incision lenticule extraction. Infection and Drug Resistance 2022, 4585–4593. [Google Scholar] [CrossRef]
- Liu, H.-Y.; Chu, H.-S.; Chen, W.-L.; Hu, F.-R.; Wang, I.-J. Bilateral non-tuberculous mycobacterial keratitis after small incision lenticule extraction. J Refract Surg 2018, 34, 633–636. [Google Scholar] [CrossRef]
- Ko, J.S.; Kim, S.K.; Yong, D.E.; Kim, T.; Kim, E.K. Delayed onset Mycobacterium intracellulare keratitis after laser in situ keratomileusis. A case report and literature review. Medicine 2017, 96, 51–e9356. [Google Scholar] [CrossRef]
- Schallhorn, J.M.; Schallhorn, S.C.; Hettinger, K.; Hannan, S. Infectious keratitis after laser vision correction: Incidence and risk factors. J Cataract Refract Surg 2017, 43, 473–479. [Google Scholar] [CrossRef]
- Ichikawa, K.; Ono, T.; Chen, L.; Kitamoto, K.; Taketatni, Y.; Toyono, T.; et al. Quantitative evaluation of corneal irregularity and scarring after infectious keratitis using anterior segment optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 2024, 262, 133–141. [Google Scholar] [CrossRef]
- Yamazaki, N.; Kobayashi, A.; Yokogawa, H.; Ishibashi, Y.; Oikawa, Y.; Tokoro, M.; Sugiyama, K. In vivo imaging of radial keratoneuritis in patients with acanthamoeba keratitis by anterior-segment optical coherence tomography. Ophthalmology 2014, 121, 2153–2158. [Google Scholar] [CrossRef]
- Oliveira, M.A.; Rosa, A.; Soares, M.; et al. Anterior segment optical coherence anterior tomography in the early management of microbial keratitis: A cross-sectional Study. Acta Med Port 2020, 33, 318–325. [Google Scholar] [CrossRef]
- Ganesh, S.; Brar, S.; Nagesh, B.N. Management of infectious keratitis following uneventful small-incision lenticule extraction using a multimodal approach –A case report. Indian J Ophthalmol 2020, 68, 3064–3066. [Google Scholar]
- Leccisotti, A.; Fields, S.V. Diffuse lamellar keratitis after LASIK with low-energy femtosecond laser. J Cataract Refract Surg 2021, 47, 233–237. [Google Scholar] [CrossRef]
- Stuart, A.; Reinstein, D.Z.; Vida, R.S.; Archer, T.J.; Carp, G. Atypical presentation of diffuse lamellar keratitis after small-incision lenticule extraction: Sterile multifocal inflammatory keratitis. J Cataract Refract Surg 2018, 44, 774–779. [Google Scholar] [CrossRef]
- Chao, C.W.; Azar, D.T. Lamellar keratitis following laser-assisted in situ keratomileusis. Ophthalmol Clin North Am 2002, 15, 35–40. [Google Scholar] [CrossRef]
- Santhiago, M.R.; Wilson, S.E. Cellular effects after laser in situ keratomileusis flap formation with femtosecond lasers: A review. Cornea 2012, 31, 198–205. [Google Scholar] [CrossRef]
Figure 1.
(patient #1). Right eye, corneal infiltrate 3 days after laser in situ keratomileusis (LASIK).
Figure 1.
(patient #1). Right eye, corneal infiltrate 3 days after laser in situ keratomileusis (LASIK).
Figure 2.
(patient #1). Right eye, corneal infiltrate 3 days after LASIK at anterior segment optical coherence tomography section (AS-OCT). The arrow indicates the sidecut of the LASIK flap; the star is above the hyper-reflective interface infiltrate, causing dark shadowing. The epithelium is not damaged.
Figure 2.
(patient #1). Right eye, corneal infiltrate 3 days after LASIK at anterior segment optical coherence tomography section (AS-OCT). The arrow indicates the sidecut of the LASIK flap; the star is above the hyper-reflective interface infiltrate, causing dark shadowing. The epithelium is not damaged.
Figure 3.
(patient #1). Right eye, corneal infiltrate 3 days after LASIK at anterior segment optical coherence tomography (AS-OCT). Upper left: corneal thickness, modified by LASIK treatment. Lower left: epithelial thickness, showing epithelial oedema surrounding the infiltrate. Bottom center: anterior tangential curvature, evidencing a locally increased curvature corresponding to the infiltrate.
Figure 3.
(patient #1). Right eye, corneal infiltrate 3 days after LASIK at anterior segment optical coherence tomography (AS-OCT). Upper left: corneal thickness, modified by LASIK treatment. Lower left: epithelial thickness, showing epithelial oedema surrounding the infiltrate. Bottom center: anterior tangential curvature, evidencing a locally increased curvature corresponding to the infiltrate.
Figure 4.
(patient #1). Right eye, corneal infiltrate 5 days after LASIK. A ring pseudo-infiltrate surrounds an area of corneal oedema.
Figure 4.
(patient #1). Right eye, corneal infiltrate 5 days after LASIK. A ring pseudo-infiltrate surrounds an area of corneal oedema.
Figure 5.
(patient #1). Right eye, corneal infiltrate 5 days after LASIK at anterior segment optical coherence tomography section (AS-OCT). The infiltrate shown in
Figure 2 has grown and is now divided in two by a dark space, corresponding to a fluid layer, which extends to the center of the surgical interface. The whole stroma is thickened by diffuse oedema.
Figure 5.
(patient #1). Right eye, corneal infiltrate 5 days after LASIK at anterior segment optical coherence tomography section (AS-OCT). The infiltrate shown in
Figure 2 has grown and is now divided in two by a dark space, corresponding to a fluid layer, which extends to the center of the surgical interface. The whole stroma is thickened by diffuse oedema.
Figure 6.
(patient #1). Right eye, corneal infiltrate 12 days after LASIK. The infiltrate has healed and evolved into a scar.
Figure 6.
(patient #1). Right eye, corneal infiltrate 12 days after LASIK. The infiltrate has healed and evolved into a scar.
Figure 7.
(patient #1). Right eye, corneal infection 12 days after LASIK at anterior segment optical coherence tomography section (AS-OCT). Oedema has resolved. A thin scar in the interface is associated with overlying thinning.
Figure 7.
(patient #1). Right eye, corneal infection 12 days after LASIK at anterior segment optical coherence tomography section (AS-OCT). Oedema has resolved. A thin scar in the interface is associated with overlying thinning.
Figure 8.
(patient #1). Right eye, corneal infection 12 days after LASIK at AS-OCT tomography. The overall corneal thickness has decreased by 30 µm (above left). The epithelium has instead thickened for a compensatory phenomenon (bottom left). The corneal anterior curvature has returned to almost complete regularity (bottom center).
Figure 8.
(patient #1). Right eye, corneal infection 12 days after LASIK at AS-OCT tomography. The overall corneal thickness has decreased by 30 µm (above left). The epithelium has instead thickened for a compensatory phenomenon (bottom left). The corneal anterior curvature has returned to almost complete regularity (bottom center).
Figure 9.
(patient #1). Right eye, corneal infiltrate 1 month after LASIK. The scar has been partially reabsorbed.
Figure 9.
(patient #1). Right eye, corneal infiltrate 1 month after LASIK. The scar has been partially reabsorbed.
Figure 10.
(patient #1). Right eye, corneal infection 1 month after LASIK at anterior segment optical coherence tomography section (AS-OCT). Stromal reformation and epithelial remodeling have filled the previously thinned area.
Figure 10.
(patient #1). Right eye, corneal infection 1 month after LASIK at anterior segment optical coherence tomography section (AS-OCT). Stromal reformation and epithelial remodeling have filled the previously thinned area.
Figure 11.
(patient #1). Right eye, corneal infection 1 month after LASIK at anterior segment optical coherence tomography (AS-OCT). The overall corneal thickness has returned to the immediate post-operative value (above left). The epithelium has now a normal thickness, except for the area peripheral to the scar (bottom left). The corneal anterior curvature has returned to almost complete regularity (bottom center).
Figure 11.
(patient #1). Right eye, corneal infection 1 month after LASIK at anterior segment optical coherence tomography (AS-OCT). The overall corneal thickness has returned to the immediate post-operative value (above left). The epithelium has now a normal thickness, except for the area peripheral to the scar (bottom left). The corneal anterior curvature has returned to almost complete regularity (bottom center).
Figure 12.
(patient #2). Right eye, corneal infiltrate 18 days after LASIK (arrow), surrounded by interface oedema.
Figure 12.
(patient #2). Right eye, corneal infiltrate 18 days after LASIK (arrow), surrounded by interface oedema.
Figure 13.
(patient #2). Right eye, corneal infiltrate 18 days after LASIK, corresponding on AS-OCT to a thin hyper-reflective area in the surgical interface; the interface is slightly hyper-reflective and surrounded by interface oedema.
Figure 13.
(patient #2). Right eye, corneal infiltrate 18 days after LASIK, corresponding on AS-OCT to a thin hyper-reflective area in the surgical interface; the interface is slightly hyper-reflective and surrounded by interface oedema.
Figure 14.
(patient #2). Right eye, corneal infiltrate 21 days after LASIK and 3 days of antibiotic treatment. At AS-OCT, only slight residual interface inflammation is visible.
Figure 14.
(patient #2). Right eye, corneal infiltrate 21 days after LASIK and 3 days of antibiotic treatment. At AS-OCT, only slight residual interface inflammation is visible.
Figure 15.
(patient #3). Left eye, corneal infiltrate 24 days after keratorefractive lenticule extraction (KLEx).
Figure 15.
(patient #3). Left eye, corneal infiltrate 24 days after keratorefractive lenticule extraction (KLEx).
Figure 16.
(patient #3). Left eye, corneal infiltrate 24 days after keratorefractive lenticule extraction (KLEx), causing a hyper-reflective zone in the surgical interface.
Figure 16.
(patient #3). Left eye, corneal infiltrate 24 days after keratorefractive lenticule extraction (KLEx), causing a hyper-reflective zone in the surgical interface.
Figure 17.
(patient #3). Left eye, corneal infiltrate 24 days after keratorefractive lenticule extraction (KLEx). At AS-OCT tomography, a small, paracentral hypercurve (red) spot is visible on the anterior tangential map (bottom, center). The overlying epithelium is slightly thickened (bottom, left).
Figure 17.
(patient #3). Left eye, corneal infiltrate 24 days after keratorefractive lenticule extraction (KLEx). At AS-OCT tomography, a small, paracentral hypercurve (red) spot is visible on the anterior tangential map (bottom, center). The overlying epithelium is slightly thickened (bottom, left).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).