1. Introduction
According to the World Health Organization (2020), genetics is defined as the study of heredity [
1]. On the other hand, genomics is a scientific field that examines the relationships between all genes in an individual’s genome, their functions, and their combined effects on growth and development [
1]. Through the use of genomics, healthcare professionals have improved diagnostic times, identification of at-risk individuals, and informed precision therapies that could improve health outcomes [
2]. Therefore, genomics is an essential component of healthcare, contributing to diagnosis, risk assessment, prevention, treatment, management, and thus overall prognosis [
3]. However, and despite the value of genomics in healthcare practice, studies have suggested that not all healthcare professionals are adequately prepared to integrate genomics into their practice [
4,
5,
6,
7,
8].
As healthcare professionals, nurses are responsible for continually educating themselves and thus have adequate knowledge of genomics. This will enable them to better inform patients, family members, and caregivers regarding the risks of being diagnosed with various genetic disorders and the available treatments [
9,
10,
11]. Moreover, it is crucial for nurses to possess genomic literacy to effectively communicate with other healthcare professionals and enhance the quality of care provided to their communities [
12]. However, findings from studies across multiple countries consistently demonstrate that nurses have insufficient knowledge of genomics, underscoring the necessity for improving genetic/genomic literacy [
2,
4,
5,
13,
14,
15]. Hence, one possible approach to enhance nurses’ understanding of genomics could involve healthcare managers and nurse educators using reliable tools like the Genomic Nursing Concept Inventory (GNCI) [
16] to evaluate and improve nurses’ knowledge of genomics.
The GNCI is the first English inventory in nursing designed to measure the understanding of fundamental genomic concepts that are crucial to nursing practice [
16,
17]. It offers an accessible and evidence-based way to assess genomic knowledge, since it can be administered in 30-minutes either on paper or online forms [
18]. GNCI allows for a holistic evaluation of nurses’ genomic knowledge since it examines their understanding of genomics and in cases of misconceptions, where the gap in their knowledge exists [
16,
17,
18]. Consequently, the results provide valuable information that enables educators to focus on poorly understood concepts and address misconceptions directly [
16,
17,
18]. This underlines the value of GNCI in educational settings because it could enable educators and managers to more efficiently and effectively assess and improve nurses' genomic knowledge [
16,
17,
18,
19]. Nevertheless, despite the growing importance of genomics in nursing and the value of GNCI, it has not been translated and validated in multiple languages, including Greek. Therefore, this study aimed to translate and validate the GNCI in Greek, evaluate the genomic knowledge of nurses in Crete, Greece, and explore potential variables that might influence it.
2. Materials and Methods
2.1. Participants
This cross-sectional study was conducted in public hospitals and health units in Crete (Greece). For the collection of the data, the sampling method of convenience was used. Data collection for the questionnaire took place between July and December 2022, and 324 clinical nurses were recruited in total. Participants were handed a self-reported questionnaire that assessed their demographic characteristics (gender, age, educational level, and workplace), and the Genomic Nursing Concept Inventory.
2.2. The Genomic Nursing Concept Inventory
The tool used in this study was the Genomic Nursing Concept Inventory (GNCI) developed and weighted by Ward, Haberman, & Barbosa-Leiker [
16]. The GNCI is made up of 31 multiple-choice items (each with one right answer) that correspond to 18 concepts divided into four thematic groups (genome basics, mutations, inheritance patterns, and genomic healthcare applications). The mean score takes values from 0 to 1. The results back up the 1-factor model, demonstrating scale one-dimensionality. The GNCI takes 30 minutes to administer and has been tested with nursing students, nursing professors, and a limited number of working nurses, yielding good psychometric results.
2.3. Translation
The process included the independent translation of the original English Forward Translation by two different people. After this phase, the two translations were compared by a third person who was able to decide between any different translation versions in order to obtain an agreed translation (1st reconciliation version). The agreed version was then translated into the language of the original questionnaire (back-ward translation) by a bilingual person (whose mother tongue was English) who was a professional translator, but did not know the standard form of the questionnaire. The version of the questionnaire that resulted from the translation process was completed by 10 clinical nurses from the target population to assess the apparent validity (Face Validity), confirming that the scale consists of questions that are consistent with the attribute to be measured and does not result in an incomplete response to the questions or misleading answers [
20].
2.4. Data Analysis
Internal consistency was assessed by the Cronbach’s alpha. A Cronbach α coefficient >0.6 indicates acceptable reliability for research purposes and suggests that items are interdependent and homogeneous in terms of the construct they measure. The McNemar test is used to analyze pretest-posttest study designs. The sample size for McNemar's test is calculated using the asymptotic approximation due to Miettinnen [
21]. For 80% power and error type I equal 5%, the minimum sample size is 74. Confirmatory Factor Analysis (CFA) was conducted to determine the model’s fit with a population of 324 clinical nurses. Adequate or good fit was indicated by a Standardized Root Mean Squared Residual (SRMR) less than or equal to 0.08, Coefficient of determination (CD) greater than or equal to 0.90, Comparative Fit Index (CFI) greater than or equal to 0.90. Continuous variables were expressed as mean ± standard deviation (SD) and categorical variables as numbers (percentages). Multiple linear regression analysis was used to examine the adjusted associations between demographic variables and the GNCI total score. Assumptions for linear regression were checked and fulfilled. The statistical analyses were conducted using STATA (version 12) for the CFA and IBM SPSS (version 26) for the remainder. The threshold for statistical significance was set at an alpha level of 0.05.
3. Results
The sample was comprised of 324 participants, 262 (80.9 %) females and 62 (19.1 %) males, aged between 23 and 59 years (
Table 1). The participants were recruited from five public hospitals and eleven healthcare units in Crete, Greece.
CVR results showed that 100% of items (n = 31) were acceptable. Cronbach's alphas for the 31 items were 0.622. The contribution of each item to the scale can be examined in
Table 2. A McNemar's test determined that the difference in the proportion of correct answers pre- and post-test wasn’t statistically significant, for all 31 items (p > 0.05).
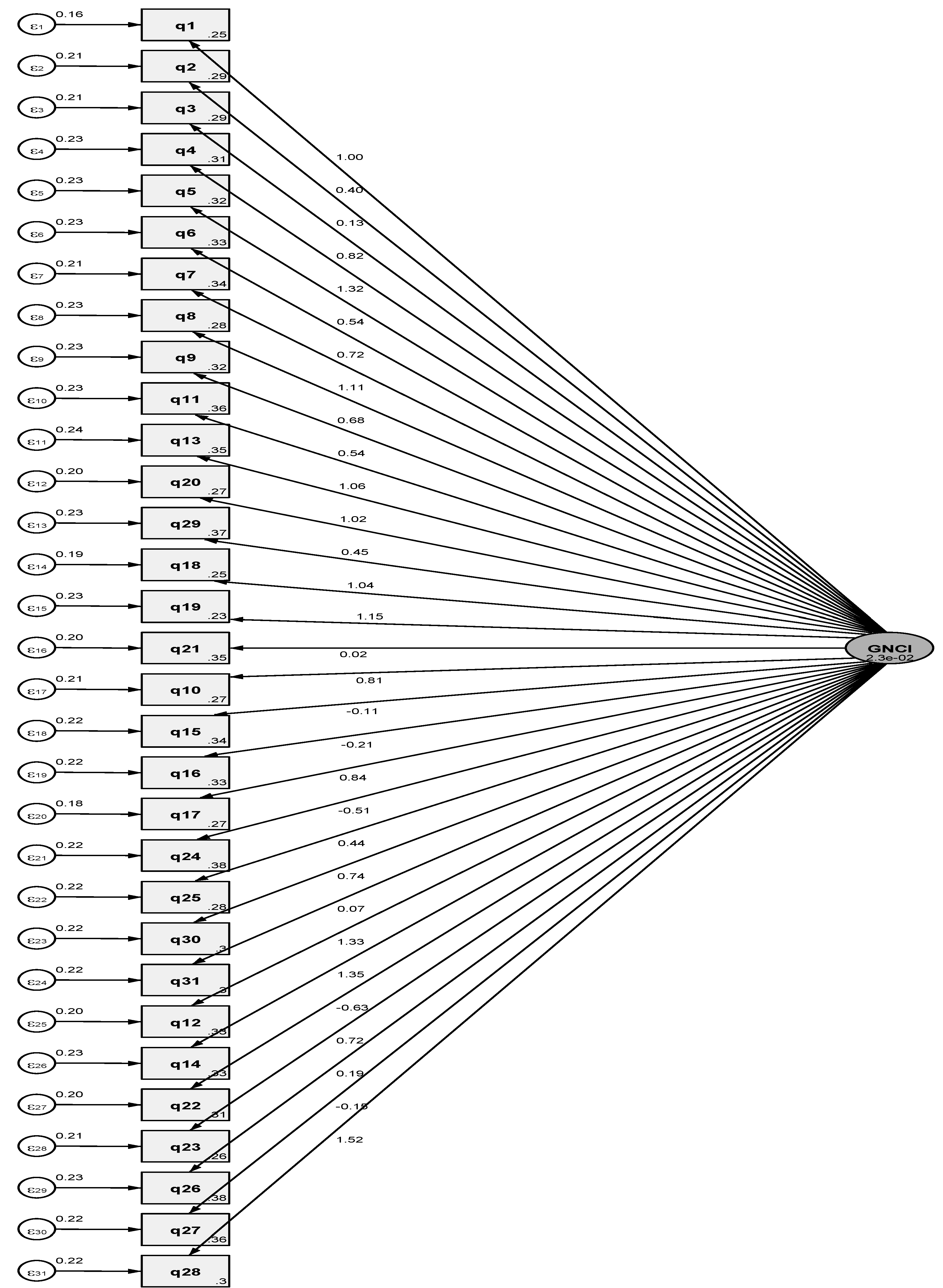
A one-factor model was conducted by CFA (
Figure 1), giving acceptable global fit indices. The resulting global fit indices (SRMR = 0.076, CD = 0.677, CFI = 0.744) showed that the 31 items in the one-factor solution proposed by the primary researchers should be accepted for the Greek GNCI.
The mean GNCI score was 0.35±0.14 indicating that the participants had moderate genomic knowledge (
Table 3). Furthermore, all subscales of GNCI had moderate scores. More specifically, the mean Genome Basic subscale was 0.36±0.17, the mean Mutation subscale score was 0.35±0.30, the mean Inheritance subscale score was 0.33±0.19, and the mean Genomic healthcare score was 0.34±0.21 (
Table 3).
Moreover, the result of the Multiple Linear Regression analysis (
Table 4) showed that of the studied variables (age, biological sex, educational level, workplace) only biological sex statistically significantly affects the average score of the GNCI scale, with female nurses having a higher score than male nurses (p <0.001).
4. Discussion
The main objective of this study was to translate and validate the Genomic Nursing Concept Inventory (GNCI) in Greek. Additionally, the study aimed to evaluate the genomic knowledge of Greek nurses and identify potential factors that could influence their genomic knowledge. The internal consistency of the Greek version of the GNCI was found to be acceptable, with a Cronbach’s alpha of 0.622. Moreover, our findings suggest that Greek nurses have a moderate level of genomic knowledge, and gender is the only demographic factor that could influence their understanding of genomics.
As aforementioned, a major outcome of this study was that the Greek version of the GNCI was successfully translated and validated, thus establishing a valuable tool for assessing and improving the genomic knowledge of Greek nurses. Although the internal consistency was acceptable (Cronbach’s alpha = 0.622), this value is slightly below the commonly accepted threshold of 0.70 [
22]. For example, the developer of GNCI reported a Cronbach's alpha of 0.77 [
16]. In addition, another study found that the Cronbach's alpha of GNCI was 0.78 [
18]. Nevertheless, a Cronbach’s alpha higher than 0.6 is considered adequate for exploratory research and initial validation studies [
23]. Especially for the Greek GNCI, since CFA (SRMR = 0.076, CD = 0.677, CFI = 0.744) further supported its reliability and validity. Previous research has also yielded comparable CFA results [
19,
24,
25,
26,
27,
28], which suggests that the items on the Greek GNCI are interconnected, and collectively represent a unified construct for genomic knowledge in nurses [
19,
29,
30]. Furthermore, the CFA results indicate that the Greek translation of the GNCI preserves the structural integrity of the original instrument, thereby confirming its suitability for use in the Greek context [
19,
29,
30]. Consequently, our study provides a means for improving genomic knowledge among nurses in Greece. Since, GNCI could help educators and healthcare managers in pinpointing areas of deficiency and designing tailored educational initiatives to improve genomic knowledge among nurses and nursing students.
Another major finding of the present study was that the nurses who participated in the study had a moderate level of genomic knowledge. Unfortunately, other studies in various contexts also confirm this finding [
5,
14,
25,
31,
32,
33], with some studies even indicating that nurses have low levels of genomic knowledge [
12,
26,
34]. These moderate to low scores suggest that nurses may not yet possess the holistic and comprehensive genomic knowledge necessary to effectively integrate genomics into their practice. Therefore, these findings highlight the urgent need to increase nurses’ genomic knowledge, and thus improve healthcare outcomes of their patients. A possible solution to this could be the incorporation of genomics into both undergraduate nursing curricula and continuing professional development programs for nurses and nurse educators [
35,
36,
37]. This could enable nurses to better apply genomic information in clinical settings, ultimately improving patient care and outcomes [
3,
6,
38,
39,
40].
We also found that only gender was associated with GNCI scores, with female nurses attaining higher GNCI scores than male nurses. This finding is interesting since other studies also suggested that female nurses score higher on the GNCI than their male counterparts [
3,
37]. However, different studies have indicated that male nurses have higher scores than female nurses [
12,
41]. This underscores the need for further research to understand the underlying factors contributing to this disparity. For example, a potential explanation could be the different attitudes toward genomics between male and female nurses in various contexts [
3,
12,
37,
41]. Additionally, the gender disparity in genomic knowledge among nurses may reflect differences in nursing education and practice, globally [
13,
24,
42].
Other demographic variables such as age, educational level, and workplace did not show any significant associations with GNCI scores. However, another study suggested that both age and experience were positively associated with genomic knowledge [
12]. Moreover, it has been suggested that nurses' knowledge of genomics increases with experience [
43]. Consequently, these findings underscore the importance of developing educational strategies that target all nurses, regardless of age, educational level, and workplace settings.
Limitations
The present study, despite its merits, has a few limitations worth mentioning. First, the cross-sectional design used in the research limits our ability to make causal inferences. Additionally, the sample size was limited to nurses in Crete, which may not accurately represent nurses from all regions of Greece. Therefore, future research could include a more diverse sample and utilize longitudinal designs to track changes in genomic knowledge over time. Another limitation is the moderate internal consistency of the GNCI, as shown by Cronbach’s alpha. Although, as stated, it is acceptable for research purposes, future studies should aim to improve the instrument’s reliability by refining individual items or considering additional items that better capture the construct of genomic nursing knowledge.
5. Conclusions
In conclusion, the present study has successfully translated and validated the GNCI in Greek. The results indicated that nurses had a moderate level of genomic knowledge, with gender influencing this knowledge. Specifically, female nurses tend to have higher genomic knowledge levels. These findings highlight the importance of implementing targeted educational strategies to enhance genomic competencies, especially in addressing the gender disparity in knowledge levels. Moreover, using the GNCI can help nurse educators and healthcare managers better prepare nurses to integrate genomics into their practice, ultimately improving patient care outcomes.
Author Contributions
Conceptualization, K.G., A.C., E.P., A.L., E.PA., A.P.; methodology, K.G., A.C., E.P., A.L., A.T., E.PA., A.P.; formal analysis, K.G., A.C., A.T., A.L., E.PA., A.P.; validation, K.G., A.C., E.P., A.L., E.PA., A.P.; investigation, K.G., A.C., E.P., A.L., A.P.; resources, K.G., A.C., E.P., A.L., A.T., E.PA., A.P.; writing— original draft preparation, K.G., A.C., E.PA., & A.P.; writing—review and editing, K.G., A.C., E.P., A.L., A.T., E.PA., & A.P.; supervision, K.G., E.PA., & A.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted under the Declaration of Helsinki, the new General Data Protection Regulation (GDPR) [EU 2016/679] 25.5.2018 on sensitive personal data, and approved by the relevant Research Ethics Committee of the Hellenic Mediterranean University (protocol code 81 approved 03 June 2022).
Informed Consent Statement
The data collected were anonymous, their use was made solely for the purposes of the survey, and access to them by the lead researcher. The participants consented in writing, having been fully informed that the procedure was anonymous, their personal data and answers would be used exclusively for research purposes, and at any time and at any time they would be able to leave. Therefore, informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
We would like to thank all participants for their voluntary participation.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Genomics. Available online: https://www.who.int/health-topics/genomics#tab=tab_1 (accessed on 3 May 2024).
- Thomas, J.; Keels, J.; Calzone, K.A.; Badzek, L.; Dewell, S.; Patch, C.; Tonkin, E.T.; Dwyer, A.A. Current State of Genomics in Nursing: A Scoping Review of Healthcare Provider Oriented (Clinical and Educational) Outcomes (2012-2022). Genes (Basel) 2023, 14. [Google Scholar] [CrossRef] [PubMed]
- Dagan, E.; Amit, Y.; Sokolov, L.; Litvak, P.; Barnoy, S. Integrating Genomic Professional Skills Into Nursing Practice: Results From a Large Cohort of Israeli Nurses. Journal of Nursing Scholarship 2021, 53, 753–761. [Google Scholar] [CrossRef]
- Ielapi, N.; Andreucci, M.; Licastro, N.; Faga, T.; Grande, R.; Buffone, G.; Mellace, S.; Sapienza, P.; Serra, R. Precision Medicine and Precision Nursing: The Era of Biomarkers and Precision Health. Int J Gen Med 2020, 13, 1705–1711. [Google Scholar] [CrossRef] [PubMed]
- Wright, H.; Zhao, L.; Birks, M.; Mills, J. Nurses' competence in genetics: An integrative review. Nurs Health Sci 2018, 20, 142–153. [Google Scholar] [CrossRef]
- Calzone, K.A.; Kirk, M.; Tonkin, E.; Badzek, L.; Benjamin, C.; Middleton, A. The Global Landscape of Nursing and Genomics. J Nurs Scholarsh 2018, 50, 249–256. [Google Scholar] [CrossRef]
- Kaphingst, K.A. Future Forecasting for Research and Practice in Genetic Literacy. Public Health Genomics 2023, 26, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Daack-Hirsch, S.; Driessnack, M.; Perkhounkova, Y.; Furukawa, R.; Ramirez, A. A Practical First Step to Integrating Genetics Into the Curriculum. Journal of Nursing Education 2012, 51, 294–298. [Google Scholar] [CrossRef]
- Calzone, K.A.; Jenkins, J.; Yates, J.; Cusack, G.; Wallen, G.R.; Liewehr, D.J.; Steinberg, S.M.; McBride, C. Survey of Nursing Integration of Genomics Into Nursing Practice. Journal of Nursing Scholarship 2012, 44, 428–436. [Google Scholar] [CrossRef]
- Calzone, K.A.; Jenkins, J.; Bakos, A.D.; Cashion, A.K.; Donaldson, N.; Feero, W.G.; Feetham, S.; Grady, P.A.; Hinshaw, A.S.; Knebel, A.R.; et al. A blueprint for genomic nursing science. J Nurs Scholarsh 2013, 45, 96–104. [Google Scholar] [CrossRef]
- Aiello, L.B. Assessment of Understanding of Foundational Genomic Concepts Among RN-to-BSN Nursing Students. 2018.
- Alloubani, A.; Al-Ruzzieh, M.; Khawaja, N.; Akhu-Zaheya, L. Genomic Literacy among Nurses in Jordan: A Population-based Study. Journal of Cancer Education 2023, 38, 1948–1954. [Google Scholar] [CrossRef]
- Regan, M.; Engler, M.B.; Coleman, B.; Daack-Hirsch, S.; Calzone, K.A. Establishing the Genomic Knowledge Matrix for Nursing Science. J Nurs Scholarsh 2019, 51, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Read, C.Y.; Ward, L.D. Faculty Performance on the Genomic Nursing Concept Inventory. J Nurs Scholarsh 2016, 48, 5–13. [Google Scholar] [CrossRef]
- Seven, M.; Akyüz, A.; Elbüken, B.; Skirton, H.; Öztürk, H. Nurses' knowledge and educational needs regarding genetics. Nurse Education Today 2015, 35, 444–449. [Google Scholar] [CrossRef]
- Ward, L.D.; Haberman, M.; Barbosa-Leiker, C. Development and psychometric evaluation of the genomic nursing concept inventory. J Nurs Educ 2014, 53, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Palomera, G. Assessing Genomic Literacy in Advanced Practice Nursing Students Before and After an Intervention. 2023.
- McCabe, M.; Ward, L.D.; Ricciardi, C. Web-Based Assessment of Genomic Knowledge Among Practicing Nurses: A Validation Study. J Contin Educ Nurs 2016, 47, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.D.; French, B.F.; Barbosa-Leiker, C.; Iverson, A.E. Application of Exploratory Factor Analysis and Item Response Theory to Validate the Genomic Nursing Concept Inventory. J Nurs Educ 2016, 55, 9–17. [Google Scholar] [CrossRef]
- Gignac, G.E. Psychometrics and the measurement of emotional intelligence. Assessing emotional intelligence: Theory, research, and applications 2009, 9-40.
- Miettinen, O.S. The matched pairs design in the case of all-or-none responses. Biometrics 1968, 339–352. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making sense of Cronbach's alpha. Int J Med Educ 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Giannousi, Z.; Manaras, I.; Georgoulias, V.; Samonis, G. Illness perceptions in Greek patients with cancer: a validation of the Revised-Illness Perception Questionnaire. Psychooncology 2010, 19, 85–92. [Google Scholar] [CrossRef]
- Jenkins, J.; Calzone, K.A. Establishing the essential nursing competencies for genetics and genomics. J Nurs Scholarsh 2007, 39, 10–16. [Google Scholar] [CrossRef]
- Zhao, X.; Li, X.; Liu, Y.; Calzone, K.; Xu, J.; Xiao, X.; Wang, H. Genetic and genomic nursing competency among nurses in tertiary general hospitals and cancer hospitals in mainland China: a nationwide survey. BMJ Open 2022, 12, e066296. [Google Scholar] [CrossRef]
- Hines-Dowell, S.; McNamara, E.; Mostafavi, R.; Taylor, L.; Harrison, L.; McGee, R.B.; Blake, A.K.; Lewis, S.; Perrino, M.; Mandrell, B.; Nichols, K.E. Genomes for Nurses: Understanding and Overcoming Barriers to Nurses Utilizing Genomics. J Pediatr Hematol Oncol Nurs 2024, 41, 140–147. [Google Scholar] [CrossRef]
- Kronk, R.; Kalarchian, M.; Lutz, C. Impact of a Professional Development Course for Doctoral Nurses and Students on Genomic Conceptual Knowledge and Competencies. Nurse Educ 2024. [Google Scholar] [CrossRef]
- Ward, L.D.; Barbosa-Leiker, C.; French, B.F. Item and Structure Evaluation of the Genomic Nursing Concept Inventory. J Nurs Meas 2018, 26, 163–175. [Google Scholar] [CrossRef]
- Marsh, H.W.; Guo, J.; Dicke, T.; Parker, P.D.; Craven, R.G. Confirmatory Factor Analysis (CFA), Exploratory Structural Equation Modeling (ESEM), and Set-ESEM: Optimal Balance Between Goodness of Fit and Parsimony. Multivariate Behav Res 2020, 55, 102–119. [Google Scholar] [CrossRef]
- Marsh, H.W.; Morin, A.J.; Parker, P.D.; Kaur, G. Exploratory structural equation modeling: an integration of the best features of exploratory and confirmatory factor analysis. Annu Rev Clin Psychol 2014, 10, 85–110. [Google Scholar] [CrossRef]
- Wright, H.; Birks, M.; Zhao, L.; Mills, J. Genomics in oncology nursing practice in Australia. Collegian 2020, 27, 410–415. [Google Scholar] [CrossRef]
- Chair, S.Y.; Waye, M.M.Y.; Calzone, K.; Chan, C.W.H. Genomics education in nursing in Hong Kong, Taiwan and Mainland China. Int Nurs Rev 2019, 66, 459–466. [Google Scholar] [CrossRef]
- Skirton, H.; O'Connor, A.; Humphreys, A. Nurses' competence in genetics: a mixed method systematic review. J Adv Nurs 2012, 68, 2387–2398. [Google Scholar] [CrossRef]
- Wright, H.; Zhao, L.; Birks, M.; Mills, J. Genomic Literacy of Registered Nurses and Midwives in Australia: A Cross-Sectional Survey. J Nurs Scholarsh 2019, 51, 40–49. [Google Scholar] [CrossRef]
- Sevo, M. Competency of nurse educators in genetics/ genomics knowledge. Journal of Nursing Education and Practice 2013, 3, 123. [Google Scholar]
- Sharoff, L. Comparison of perceived genetic-genomic knowledge of nurse educators and graduate degree nursing students. Journal of Nursing Education and Practice 2017, 7, 67. [Google Scholar] [CrossRef]
- Parviainen, A.; Ward, L.D.; Halkoaho, A.; Laing, B.; Maguire, J.; Palovaara, M.; Mandysova, P.; Bacungan, G.; Mamungay, J.J.; Sund, R. Nursing students’ genomics literacy: Basis for genomics nursing education course development. Teaching and Learning in Nursing 2023, 18, 6–11. [Google Scholar] [CrossRef]
- Majstorovic, D.; Barisic, A.; Stifanic, M.; Dobraca, I.; Vranekovic, J. The Importance of Genomic Literacy and Education in Nursing. Front Genet 2021, 12, 759950. [Google Scholar] [CrossRef]
- Calzone, K.A.; Kirk, M.; Tonkin, E.; Badzek, L.; Benjamin, C.; Middleton, A. Increasing nursing capacity in genomics: Overview of existing global genomics resources. Nurse Educ Today 2018, 69, 53–59. [Google Scholar] [CrossRef]
- Daack-Hirsch, S.; Jackson, B.; Belchez, C.A.; Elder, B.; Hurley, R.; Kerr, P.; Nissen, M.K. Integrating Genetics and Genomics into Nursing Curricula You Can Do It Too! Nursing Clinics of North America 2013, 48, 661. [Google Scholar] [CrossRef]
- Dewell, S.; Benzies, K.; Ginn, C.; Seneviratne, C. Assessing knowledge of genomic concepts among Canadian nursing students and faculty. Int J Nurs Educ Scholarsh 2020, 17. [Google Scholar] [CrossRef]
- Tully, L.A.; Calzone, K.A.; Cashion, A.K. Establishing the Omics Nursing Science & Education Network. J Nurs Scholarsh 2020, 52, 192–200. [Google Scholar] [CrossRef]
- Flowers, E.; Leutwyler, H.; Shim, J.K. Direct-to-consumer genomic testing: Are nurses prepared? Nursing 2020, 50, 48–52. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).