1. Introduction
Mallet finger refers to a condition in which the tip of the finger displays a deformity, characterized by the inability of the affected distal interphalangeal (DIP) joint to extend the distal phalanx actively, resulting in a flexed position. (
Figure 1) [
1]. This injury type can be classified as a simple tendinous disruption or one secondary to a bony avulsion. The classification of the injury can also be based on whether the skin covering the area is damaged or intact, categorized as either an open or closed mallet injury. Frequent causes involve sports activities resulting in a direct impact on the finger, from becoming trapped in a door, or from minor energy-related injuries during routine tasks like pulling up socks. Open injuries can be the result of traumatic lacerations or high-impact crush injuries [
2]. It is frequently encountered in the management of hand trauma, comprising approximately 5.6% of all tendon injuries in the hand and wrist and 2% of all sporting injuries [
3,
4]. Mallet finger injuries are predominantly observed in male patients in their youth and middle age [
5]. Because pediatric bone generally possesses lower tensile strength in comparison to ligaments, bony avulsion injuries tend to occur more frequently than in adults [
3,
6,
7]. Overall, the dominant hand is more commonly affected, with the ulnar three digits accounting for the majority of mallet finger injuries [
8].
Patients commonly arrive with an inability to extend the DIP joint to a neutral position after a traumatic injury. During examination, the finger exhibits flexion at the DIP joint, often accompanied by swelling, contusion, and tenderness over the dorsal part of the DIP joint, while rarely one may observe the presence of a swan-neck deformity [
3]. To identify bony mallet finger injuries, a standard anteroposterior (AP) and lateral radiographic view of the finger, focused on the DIP joint, are captured. Sometimes additional stress views may be obtained to help assess the reducibility of the fragment or correction of palmar subluxation [
3]. There are multiple known systems used to classify acute mallet finger injuries based on radiological findings (Doyle, Wehbe and Schneider, Niechajev)[
3]. The classification developed by Wehbe and Schneider emphasizes bony mallet injuries, taking into account factors such as the size of the articular fragment and the presence of palmar subluxation (
Table 1) [
1].
Initially, nonoperative management is the recommended choice for treating nearly all mallet finger injuries. At present, the prevailing recommendation is to solely splint the DIP joint[
3]. There's a suggestion from some quarters, however, that immobilizing both the DIP joint and the proximal interphalangeal (PIP) joint could aid in relaxing the extensor hood and intrinsic muscles, facilitating the healing process [
9]. On the other hand, during a cadaver study done by Katzman et al., it was indicated that the gapping of the extensor tendon happens due to the movement of the distal tendon stump when the DIP joint flexes, and not due to the retraction of the proximal tendon edge during PIP joint extension, questioning the need to splint the PIP joint [
10]. Different splinting variations have been described in the literature. Among the nonsurgical treatment options frequently used for mallet fingers, Stack splints, custom thermoplastic splints, and foam-padded aluminum splints are commonly considered. Currently, there’s no conclusive evidence of a specific splint design or splint placement resulting in a superior clinical outcome [
11,
12,
13].
The suggested duration of immobilization involves wearing the splint full-time for a period of six weeks, followed by an additional 2–6 weeks of night splinting. Should the DIP joint flex at any time within the initial six weeks, the patient should be advised to restart the splinting regimen [
3,
5,
14]. Non-surgical treatment could still carry the potential risk of complications. These include minor skin issues, persistent pain, hyperpigmentation, skin necrosis, and flexion deformity of the DIP joint. Similarly, it's typical to observe five to ten degrees of extension lag following conservative treatment with splints, which generally does not lead to functional impairment [
9,
14,
15].
Surgical recommendations are often based on fractures that encompass over 30% of the articular surface or the occurrence of palmar subluxation in the distal phalanx [
3,
12]. Biomechanical research indicates that fractures encompassing over 30% of the articular surface have a heightened risk of subluxation [
16]. Surgery is also the preferred choice of treatment for open injuries or if non-surgical management proves ineffective [
12]. Numerous types of techniques have been described for the fixation of mallet finger fractures. They can be broadly categorized as closed reduction involving percutaneously inserted Kirschner wires (K-wires) or open reduction with fixation. Ishiguro first described extension block pinning in 1988 for the treatment of mallet finger fractures, which has been the most widely accepted surgical technique [
17]. Other authors achieved closed reduction with techniques utilizing direct pining of the avulsed fragment, presenting favorable results [
18,
19]. In addition, some new novel methods recently described include umbrella handle K-wiring and the Delta wiring technique [
9]. Complications associated with the use of K-wires are well known: pin migration, infection, dermal necrosis, nail bed deformities, and rarely osteomyelitis [
3,
20,
21]. The occurrence of such adverse events may negatively affect the functional outcome. Likewise, open reduction and fixation have been described, incorporating techniques like hook plate [
22], tension band wiring [
23], screws [
24], and interosseous wires [
25].
Our clinical routine for the operative treatment of mallet finger injuries mainly involves the usage of Ishiguro’s technique. The aim of this paper is to evaluate the effectiveness of the extension block pinning technique described by Ishiguro et al. in the adolescent population.
2. Materials and Methods
2.1. Study Design
The Authors reviewed 36 patients from the Database of the Pediatric Surgery Department in a single-arm, retrospective cohort study to evaluate the capabilities of the Ishiguro pinning method. This evaluation was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. Inclusion criteria were
(1) adolescent patients who were
(2) operated on due to mallet finger injuries
(3) between February 2014 and December 2022
(4) by a minimally invasive extension block pinning technique described by Ishiguro et al [
17,
26]. Surgical indications encompassed cases with
(5) a displaced large fragment comprising over one-third of the articular surface or
(6) fractures coupled with palmar subluxation of the distal phalanx [
20]. Additionally, twelve patients in total were initially excluded from our study,
(1) two who had injuries older than three weeks,
(2) another two who were above the age of 18,
(3) and eight children who were lost to follow-up.
2.2. Surgical Technique and Postoperative Care
All patients received prophylactic oral antibiotic treatment in the form of Augmentin 500/125 mg (amoxicillin/clavulanic acid), local digital Oberst anesthesia (bupivacaine), and additionally, some adolescents received general anesthesia.
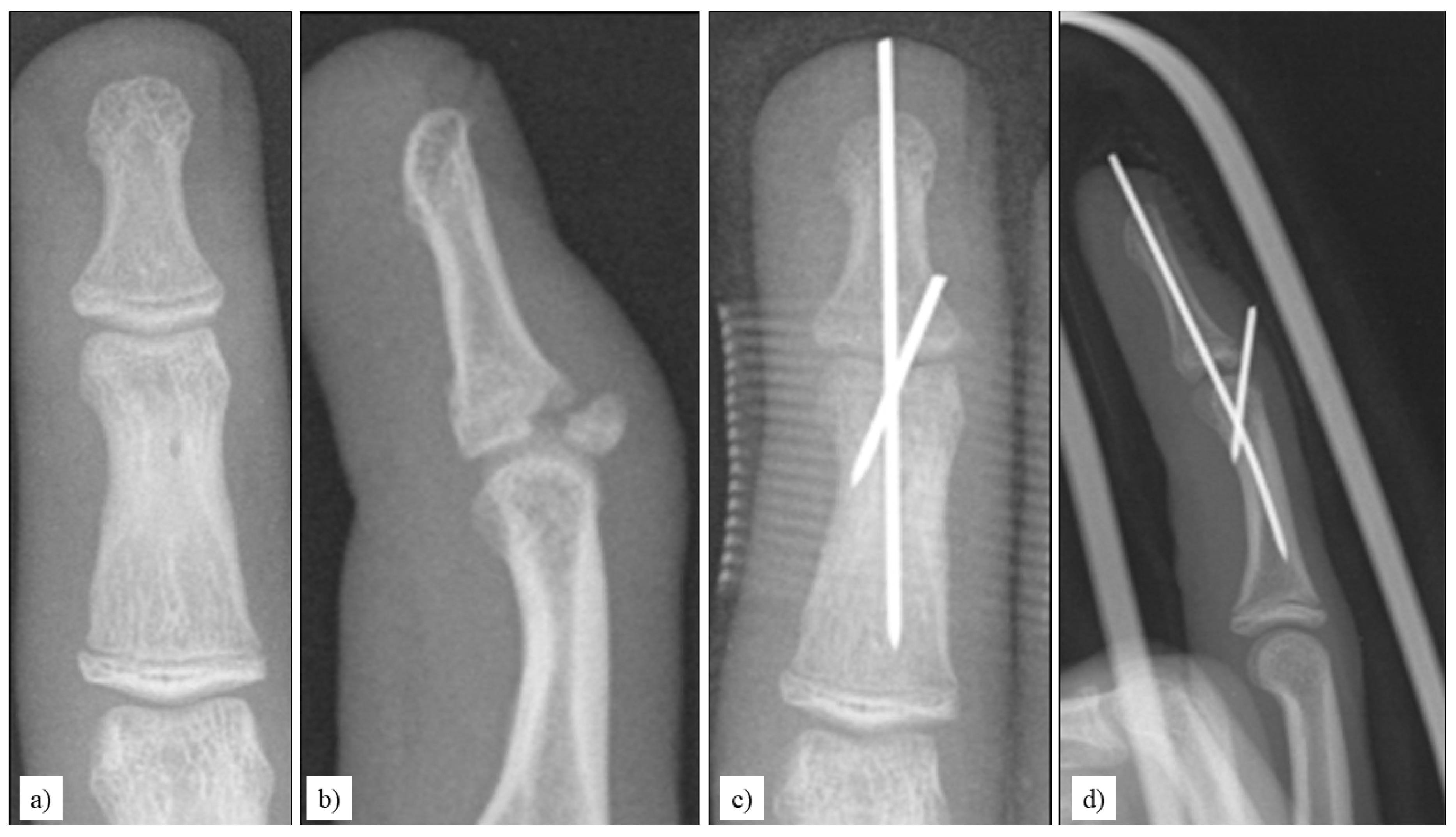
Through fluoroscopic imaging, a 1-1.2 millimeter (mm) K-wire was percutaneously inserted into the middle phalanx, positioned 1–2 mm dorsal and proximal to the fracture fragment, all while maintaining the DIP in maximum flexion. Subsequently, the distal phalanx was pulled distally and extended in order to achieve the reduction of the fracture. Following that, the DIP joint was immobilized by a second percutaneous K-wire, running palmar to the fracture (
Figure 2) [
17,
26].
Post-surgery, an aluminum splint was utilized to stabilize the DIP and PIP joints, with an emphasis on promoting active motion of the metacarpophalangeal joint. Once a week, the pin site underwent disinfection. At the six-week mark post-surgery, the K-wires were removed, and both passive and active exercises for the DIP joint were promoted. Functional status was assessed after hardware removal during the final follow-up, two months postoperatively. In some select cases, we examined videos sent by patients who were previously lost to follow-up, to determine the postoperative range of motion (ROM) of the DIP joint. To classify functional results, we used Crawford’s (1984) evaluation criteria (
Table 2) [
13].
2.3. Evaluated Endpoints
Demographic outcomes included sex, age, side, and etiology of the injury. The primary endpoint of this study was the functional outcome of adolescent mallet finger injuries treated with the extension block pinning technique. Functional outcomes were assessed using Crawford's evaluation criteria, which classify results as excellent, good, fair, or poor based on the degree of extension deficit, flexion capacity, and presence of pain (
Table 2) [
13]. Furthermore, we followed Wehbé and Schneider’s (1984) classification [
1], which considers the extent of subluxation of the distal phalanx and the size and displacement of the fracture fragment. Secondary endpoints included the time to surgery from injury, narcosis technique, rate of bone union, the occurrence and nature of complications, and the overall duration of postoperative recovery. Fracture union was characterized by the presence of bridging trabeculae on plain radiographs and a pain-free DIP joint. The level of anatomical reduction and the congruity of the articular surface were verified through plain radiographs obtained postoperatively and during the final follow-up.
2.4. Statistical Analysis
Statistical analyses were performed using SPSS software (version 26.0; IBM, Armonk, NY, USA). Descriptive statistics were used to summarize patient demographics, injury characteristics, and treatment outcomes. Continuous variables such as age and follow-up duration were reported as mean values with ranges, while categorical variables such as injury type and outcome classification were presented as frequencies and percentages.
3. Results
We treated 25 boys and 11 girls with an average age of 14.5 (range: 11-17). Right and left hands were affected in the same number of cases (13-13). Involved digits were; the middle finger in 21 cases, the ring finger in six, the little finger in five, the index finger in three, and the thumb in one case. Out of 35 cases, the initial injury occurred during participation in sporting activities, while in one instance, it happened due to bumping up against a wall.
Compound fractures or open fractures were not observed. The average extent of articular surface involvement was 44% (range: 33-63%). Subluxation of the distal phalanx was detected in two out of the 36 fractures (5.5% of all cases). Following Wehbé and Schneider’s (1984) classification [
1], there were 34 fractures classified as type IB and two as type IIB.
Average duration from injury to surgery was 3.5 days (range: 0-16 days) with the majority of the procedures (28) being performed under digital nerve block, while eight patients underwent general anesthesia. Mean follow-up time was 8.6 months (range: 2-42 months). We noticed the subluxation of the distal phalanx postoperatively in one finger, which required the repositioning of the K-wire immobilizing the DIP joint. Bone union was attained in all cases, with a mean postoperative day of 42 (range: 30-92 days). Following Crawford's evaluation criteria [
13], we achieved 27 excellent, five good, four fair, and no poor results (
Figure 3,
Table 2).
Three children experienced superficial infection at the pin site during the fourth and fifth postoperative weeks, while in one scenario we noticed dermal necrosis, which was resolved with pin removal and appropriate dressing. In a single instance, signs of osteomyelitis were observed, and resolution was achieved through immobilization and the administration of oral antibiotics. No other complications, such as non-union, fractures of bone fragments, or nail-plate deformities, were observed.
4. Discussion
The literature provides an extensive selection of approaches for managing adolescent mallet finger fractures. In the majority of cases, the use of either an aluminum splint or a Brooks splint proves to be an effective treatment option [
13]. Several authors advocate for conservative treatment for nearly all mallet finger injuries, with comparative studies showing no clinically significant functional difference, between those treated with splinting, and those treated with K-wire fixation [
3,
12,
27]. Yet prolonged discomfort from splinting may present challenges with compliance, underscoring the importance of patients adhering well to ensure the success of the conservative treatment plan. The above might be particularly important amongst the pediatric population. In addition, some patients with large fracture fragments treated with splinting may reportedly present with secondary subluxation [
28]. A new non-operative treatment method, using low-intensity pulsed ultrasound (LIPUS) has recently been described in the literature as an alternative to splinting. It does not limit the active ROM, which seems to be the biggest hurdle and compliance difficulty when using splints. In a preliminary study with a limited number of cases, they observed similar functional outcomes between LIPUS treatment and Ishiguro’s method for mallet fractures involving a large fragment [
29].
Largely displaced fractures (more than 30 % of the articular surface) and the presence of palmar subluxation are the most frequently described indications for surgery, which align with our clinical practice. Other factors, including cosmetic appearance and the need for patients to maintain fine manual dexterity, should also be considered [
3,
12].
Ishiguro initially described extension block pinning in 1988 for the treatment of mallet finger fractures [
17]. It introduced a relatively easy, quick method, allowing the closed reduction of the fracture, which reduces the possibility of the fragment becoming comminuted. A notable drawback however is its inability to provide sufficient stability without the use of splinting [
3,
20,
21].
Pegoli et al carried out the most extensive study examining the technique to date, who assessed 65 patients with bony mallet injuries treated with extension block pinning. Their findings revealed that 78% of the patients achieved an excellent to good outcome on Crawford’s scale during follow-up, while 13 patients reported fair outcomes, which they attributed to poor initial reduction. They also reported a total complication rate of 5% [
21]. We got comparable functional results, with 89% of our patients attaining an excellent or good outcome, and only four patients had a fair Crawford result. It is notable however that while Pegoli et al. included six cases in their study, who were treated more than five weeks following the initial injury, we excluded such patients. Comparatively, our overall complication rate was 14%, although these were mainly slight complications. To prevent skin irritation, we cut off the wires outside the skin.
There are some recent variations known to percutaneous K-wire pinning and the extension block technique to treat mallet fractures. Perez-Lopez et al. described the reverse Ishiguro technique, promising an easier and more stable reduction of the fragment [
30], Another variation, using a single K-wire has also been described in the literature, called the Umbrella technique. According to Rocchi et al., this method seems to provide better (although not statistically significant) functional results and lower complication rates compared to Ishiguro’s technique, when treating fractures with a large fragment. However, it presents a greater challenge, with the technique involving intraoperative modification of the K-wire shape and the utilization of a custom-made thermoplastic splint [
31]. Another novel technique that allows early active ROM is called the Delta wire technique, described by Kim et al. in 2013 [
32]. According to a comparative study by Chee WH et al., while it does allow earlier mobilization during the treatment period, it does not lead to clinically better functional results [
3,
33].
Utilizing open reduction and fixation techniques, including interosseus sutures, K-wires, and mini screws could help with achieving more precise anatomical reduction and greater stability, but they are usually associated with higher complication rates [
3,
24,
25]. In 2007, Teoh and Lee detailed the utilization of a hook plate for mallet finger injuries [
22]. The main advantage of the technique is that reduction and stable fixation can be achieved without the placement of a screw through the avulsed fragment. Usage of a hook plate is associated with good functional outcomes when compared to Ishiguro’s technique, with the greatest reported disadvantage being the presence of nail deformities and the undesirable aesthetic appearance of the finger with the plate in place [
3,
34].
This study's exploration into the extension block technique for adolescent mallet finger injuries brings a refreshing perspective to pediatric orthopedics. The high frequency of excellent and good outcomes emphasizes its efficacy, aligning with the literature, and also underscoring a unique application in the pediatric cohort, where treatment nuances differ significantly from adult cases [
21]. Notably, the minimal complications, such as superficial infections, highlight the technique's safety, which is particularly crucial in pediatric care, where balancing efficacy and safety is paramount. The absence of more severe complications in our study is encouraging and supports the technique's suitability for this vulnerable population.
However, the retrospective nature of the study, while providing valuable insights, also imposes limitations. Prospective studies, preferably with larger and more diverse populations and in more varied clinical scenarios, are essential to validate these findings further. Additionally, comparing the extension block technique directly with other treatment modalities could offer a more thorough understanding of its relative effectiveness. Future research directions could explore patient-reported outcomes, such as post-treatment scarring, pain levels, and other functionality. Crafting a randomized and blinded management environment may be able to further generalize the results by reducing bias. Long-term, at least five years of follow-ups, would also be beneficial to assess any delayed complications (for example posttraumatic arthritis) or recurrence, which are critical aspects of pediatric orthopedic interventions.
5. Conclusions
Ishiguro’s extension block technique proves to be a highly effective and reliable method for treating adolescent mallet finger fractures, achieving excellent to good functional outcomes in 89% of cases with minimal complications. All cases achieved bone union within an average of 42 days, and complications were minor, including superficial infections (8%) and a rare instance of osteomyelitis (3%). The technique offers stable fracture fixation, minimizing the risk of comminution and allowing early mobilization, making it particularly suitable for the pediatric population.
While these results are promising, the study's retrospective design and small sample size suggest the need for prospective studies with larger cohorts to confirm these findings. Future research should also investigate long-term outcomes, patient-reported pain and functionality, and comparisons with other treatment modalities. These steps will help establish the technique's comprehensive efficacy and potential to become a standard treatment for adolescent mallet finger injuries.
Author Contributions
Conceptualization, T.M. and G.J.; methodology, H.N., A.G.L., and G.J.; validation, T.M., A.L., A.G.L., H.N. and G.J.; formal analysis, T.M., A.L., A.G.L., H.N. and G.J; investigation, T.M, A.G.L. and G.J.; resources, T.M. and G.J.; data curation, T.M., H.N. and A.G.L.; writing—original draft preparation, T.M.; writing—review and editing T.M., A.L., A.G.L., H.N. and G.J.; visualization, T.M., A.L. and G.J.; supervision, A.L. and G.J.; project administration, A.G.L., A.L. and G.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Ethics Committee of the University of Pécs (Protocol code: PTE/00009-005/2023, Date of approval: 2023.01.05.).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient’s guardians to publish this paper.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wehbé, M.A.; Schneider, L.H. Mallet Fractures. J Bone Joint Surg Am 1984, 66, 658–669.
- Khera, B.H.; Chang, C.; Bhat, W. An Overview of Mallet Finger Injuries. Acta Biomedica 2021, 92.
- Nashi, N.; Sebastin, S.J. A Pragmatic and Evidence-Based Approach to Mallet Finger. J Hand Surg Asian Pac Vol 2021, 26, 319–332. [CrossRef]
- Simpson, D.; McQueen, M.M.; Kumar, P. Mallet Deformity in Sport. Journal of Hand Surgery 2001, 26 B, 32–33. [CrossRef]
- Alla, S.R.; Deal, N.D.; Dempsey, I.J. Current Concepts: Mallet Finger. Hand 2014, 9, 138–144. [CrossRef]
- Carson, S.; Woolridge, D.P.; Colletti, J.; Kilgore, K. Pediatric Upper Extremity Injuries. Pediatr Clin North Am 2006, 53, 41–67.
- Lin, J.S.; Samora, J.B. Outcomes of Splinting in Pediatric Mallet Finger. Journal of Hand Surgery 2018, 43, 1041.e1-1041.e9. [CrossRef]
- Stern, P.J.; Kastrup, J.J. Complications and Prognosis of Treatment of Mallet Finger. Journal of Hand Surgery 1988, 13, 329–334. [CrossRef]
- Nashi, N.; Sebastin, S.J. A Pragmatic and Evidence-Based Approach to Mallet Finger. J Hand Surg Asian Pac Vol 2021, 26, 319–332. [CrossRef]
- Katzman, B.M.; Klein, D.M.; Mesa, J.; Geller, J.; Caliguri, D.A. Immobilization of the Mallet Finger. Journal of Hand Surgery 1999, 24, 80–84. [CrossRef]
- Lamaris, G.A.; Matthew, M.K. The Diagnosis and Management of Mallet Finger Injuries. Hand 2017, 12, 223–228.
- Lin, J.S.; Samora, J.B. Surgical and Nonsurgical Management of Mallet Finger: A Systematic Review. Journal of Hand Surgery 2018, 43, 146-163.e2. [CrossRef]
- Crawford, G.P. The Molded Polythene Splint for Mallet Finger Deformities. J Hand Surg Am 1984, 9, 231–237. [CrossRef]
- Richards, S.D.; Kumar, G.; Booth, S.; Naqui, S.Z.; Murali, S.R. A Model for the Conservative Management of Mallet Finger. Journal of Hand Surgery 2004, 29 B, 61–63. [CrossRef]
- Rayan, G.M.; Taylor Mullins, P. Skin Necrosis Complicating Mallet Finger Splinting and Vascularity of the Distal Interphalangeal Joint Overlying Skin. J Hand Surg Am 1987, 12, 548–552. [CrossRef]
- Husain, S.N.; Dietz, J.F.; Kalainov, D.M.; Lautenschlager, E.P. A Biomechanical Study of Distal Interphalangeal Joint Subluxation After Mallet Fracture Injury. Journal of Hand Surgery 2008, 33, 26–30. [CrossRef]
- Ishiguro, T. A New Method of Closed Reduction for Mallet Fractures. Cent Jpn J Orthop Trauma Surg. 1988, 6, 413–415.
- Badia, A.; Riano, F. A Simple Fixation Method for Unstable Bony Mallet Finger. Journal of Hand Surgery 2004, 29, 1051–1055. [CrossRef]
- Yamanaka, K.; Sasaki, T. Treatment of Mallet Fractures Using Compression Fixation Pins. Journal of Hand Surgery 1999, 24, 358–360. [CrossRef]
- Józsa, G.; Kardos, D.; Oberritter, Z. The Ishiguro Technique for the Treatment of Mallet Finger Fracture in Adolescent. Novel Techniques in Arthritis & Bone Research 2017, 1. [CrossRef]
- Pegoli, L.; Toh, S.; Arai, K.; Fukuda, A.; Nishikawa, S.; Vallejo, I.G. The Ishiguro Extension Block Technique for the Treatment of Mallet Finger Fracture: Indications and Clinical Results. Journal of Hand Surgery 2003, 28 B, 15–17. [CrossRef]
- Teoh, L.C.; Lee, J.Y.L. Mallet Fractures: A Novel Approach to Internal Fixation Using a Hook Plate. Journal of Hand Surgery (European Volume) 2007, 32, 24–30. [CrossRef]
- Damron, T.A.; Engber, W.D. Surgical Treatment of Mallet Finger Fractures by Tension Band Technique. Clin Orthop Relat Res 1994, 133–140.
- Kronlage, S.C.; Faust, D. Open Reduction and Screw Fixation of Mallet Fractures. J Hand Surg Br 2004, 29, 135–138. [CrossRef]
- Bauze, A.; Bain, G.I. Internal Suture for Mallet Finger Fracture. Journal of Hand Surgery 1999, 24, 688–692. [CrossRef]
- Ishiguro, T.; Itoh, Y.; Yabe, Y.; Hashizume, N. Extension Block with Kirschner Wire for Fracture Dislocation of the Distal Interphalangeal Joint. Tech Hand Up Extrem Surg 1997, 1, 95–102. [CrossRef]
- Kalainov, D.M.; Hoepfner, P.E.; Hartigan, B.J.; Carroll IV, C.; Genuario, J. Nonsurgical Treatment of Closed Mallet Finger Fractures. Journal of Hand Surgery 2005, 30, 580–586. [CrossRef]
- Thillemann, J.K.; Thillemann, T.M.; Kristensen, P.K.; Foldager-Jensen, A.D.; Munk, B. Splinting versus Extension-Block Pinning of Bony Mallet Finger: A Randomized Clinical Trial. Journal of Hand Surgery: European Volume 2020, 45, 574–581. [CrossRef]
- Ota, T.; Itoh, S.; Matsuyama, Y. Comparison of Treatment Results for Mallet Finger Fractures in Children Between Low-Intensity Pulsed Ultrasound Stimulation and Ishiguro’s Method. Hand 2018, 13, 80–85. [CrossRef]
- Perez-Lopez, L.M.; Perez-Abad, M.; Merchan, A.S.; Cabrera Ortiz, D.A. Reverse Ishiguro Extension Block Technique as an Alternative for Irreducible Osseous Mallet Finger. Tech Hand Up Extrem Surg. 2023.
- Rocchi, L.; Fulchignoni, C.; De Vitis, R.; Molayem, I.; Caviglia, D. Extension Block Pinning vs Single Kirshner Wiring to Treat Bony Mallet Finger. A Retrospective Study. Acta Biomedica 2021, 92. [CrossRef]
- Kim JH; Kim JH; Lee S; Kim DG Delta Wire Technique for Bony Mallet Finger: Surgical Technique. J Korean Orthop Res Soc. 2013, 16, 13–16.
- Chee, W.H.; Gunasagaran, J.; Ahmad, T.S. A Comparison of Delta Wire Technique versus Extension Block Pinning in the Treatment of Bony Mallet Finger. Handchir Mikrochir Plast Chir 2020, 52, 176–181. [CrossRef]
- Vester, H.; Schul, L.; von Matthey, F.; Beirer, M.; van Griensven, M.; Deiler, S. Patient Satisfaction after Hook Plate Treatment of Bony Avulsion Fracture of the Distal Phalanges. Eur J Med Res 2018, 23, 35. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).