Submitted:
14 June 2024
Posted:
18 June 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Overview of CAR-NK Cell Therapy
| 1st Author | Year | Cell Type | Generation | Intracellular Signaling Domains |
|---|---|---|---|---|
| P Kvacskay [14] | 2024 | CAR-T | First | CD3ζ |
| Y Wang [15] | 2024 | CAR-T | Second | CD28, 4-1BB with CD3ζ |
| Ritmeester-Loy [16] | 2024 | CAR-T | Third | CD28, 4-1BB, and CD3ζ |
| R Basar [13] | 2020 | CAR-NK | First | CD3ζ or NK cell activating domains (e.g., 2B4) |
| L Herrera [17]. | 2021 | CAR-NK | Second | DAP12, 2B4, CD3ζ, or NK cell-specific costimulatory molecules (e.g., CD137, NKG2D) |
| A Page [18]. | 2024 | CAR-NK | Third | Combinations of NK cell-specific signaling domains (e.g., DAP12, 2B4, NKG2D, CD137) |
3. The Comparison of CAR-NK Cells to CAR-T Cells Therapies
3.1. Intracellular Signaling Domains
3.2. Cell Sources for Both CAR-T and CAR-NK Cells
3.3. CAR-T and CAR-NK Cells In Vitro Expansion
3.4. Pre-Expansion Prior to Transduction in CAR-T and CAR-NK Cells
3.5. Cell Killing Mechanism
3.6. Cytokine Release Syndrome and Neurotoxicity
3.7. CAR-T and CAR-NK Therapies in Hematological Malignancies and Solid Tumors
3.8. Cost-Effectiveness
- (1)
- Off-the-shelf availability: Unlike CAR-T cells, which are patient-specific and require a lengthy and costly manufacturing process, CAR-NK cells can be derived from healthy donors and stored for immediate use [48]. This eliminates the need for individualized cell production and reduces waiting time for patients.
- (2)
- Safety: CAR-NK cells have been associated with fewer severe side effects such as cytokine release syndrome (CRS), neurotoxicity, and graft-versus-host disease (GVHD) [49]. This could potentially lead to lower healthcare costs related to the management of these side effects.
- (3)
- Natural cytotoxicity: CAR-NK cells preserve the natural cytotoxicity of NK cells even if the expression of targeted tumor antigens is downregulated [48]. This could potentially lead to more effective treatment outcomes and, therefore, cost savings in the long run.
- (4)
- Manufacturing costs: While the exact cost of manufacturing CAR-NK cells is not specified, the cost of manufacturing CAR-T cells has been estimated to be between $48,000 and $106,000 per dose [50]. The ability to produce CAR-NK cells from healthy donors and in larger batches could potentially reduce these costs.
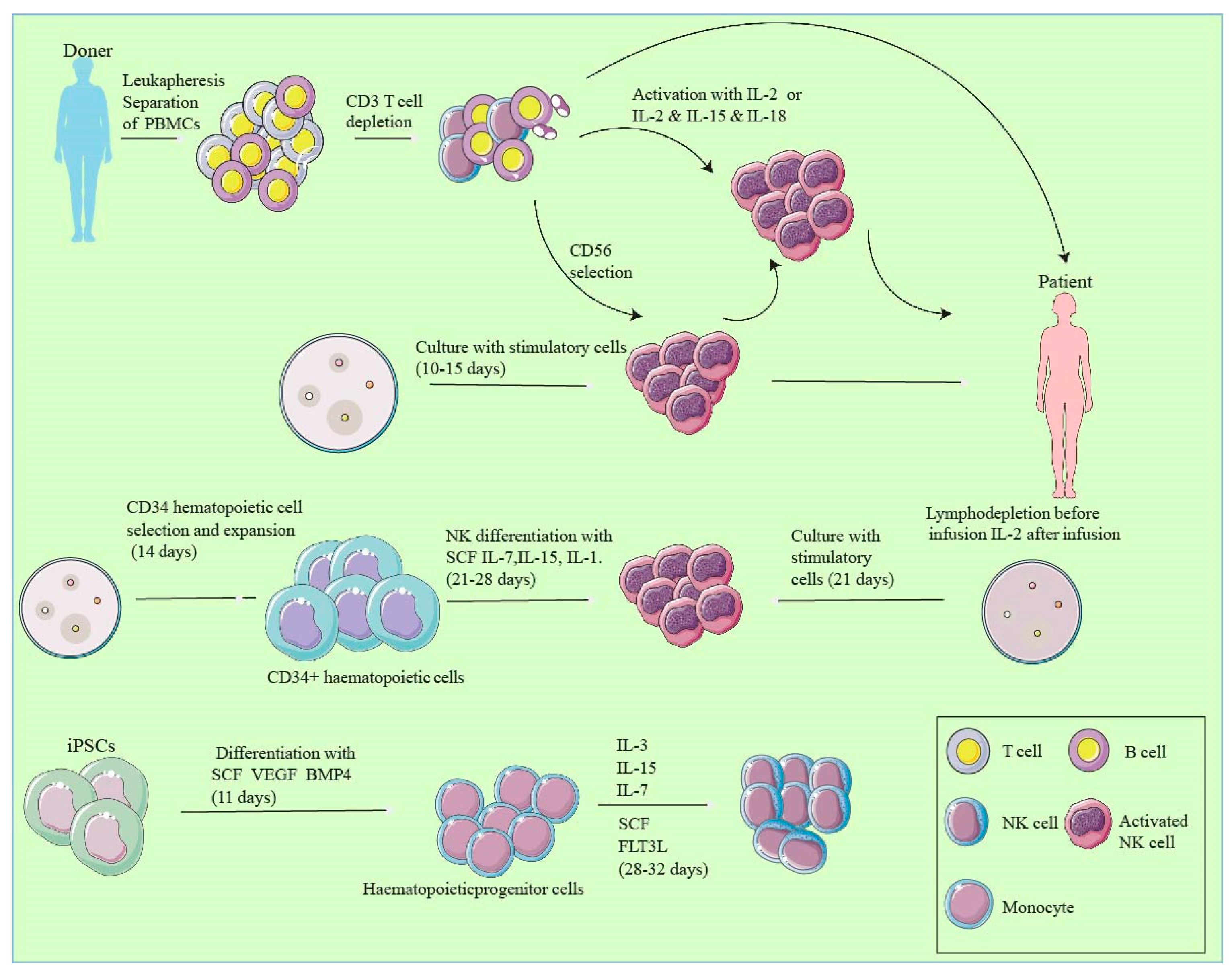
4. Development of CAR-NK Cells
4.1. CAR-NK Cell Preparation Process
4.2. Technological Advances and Innovations
- (1)
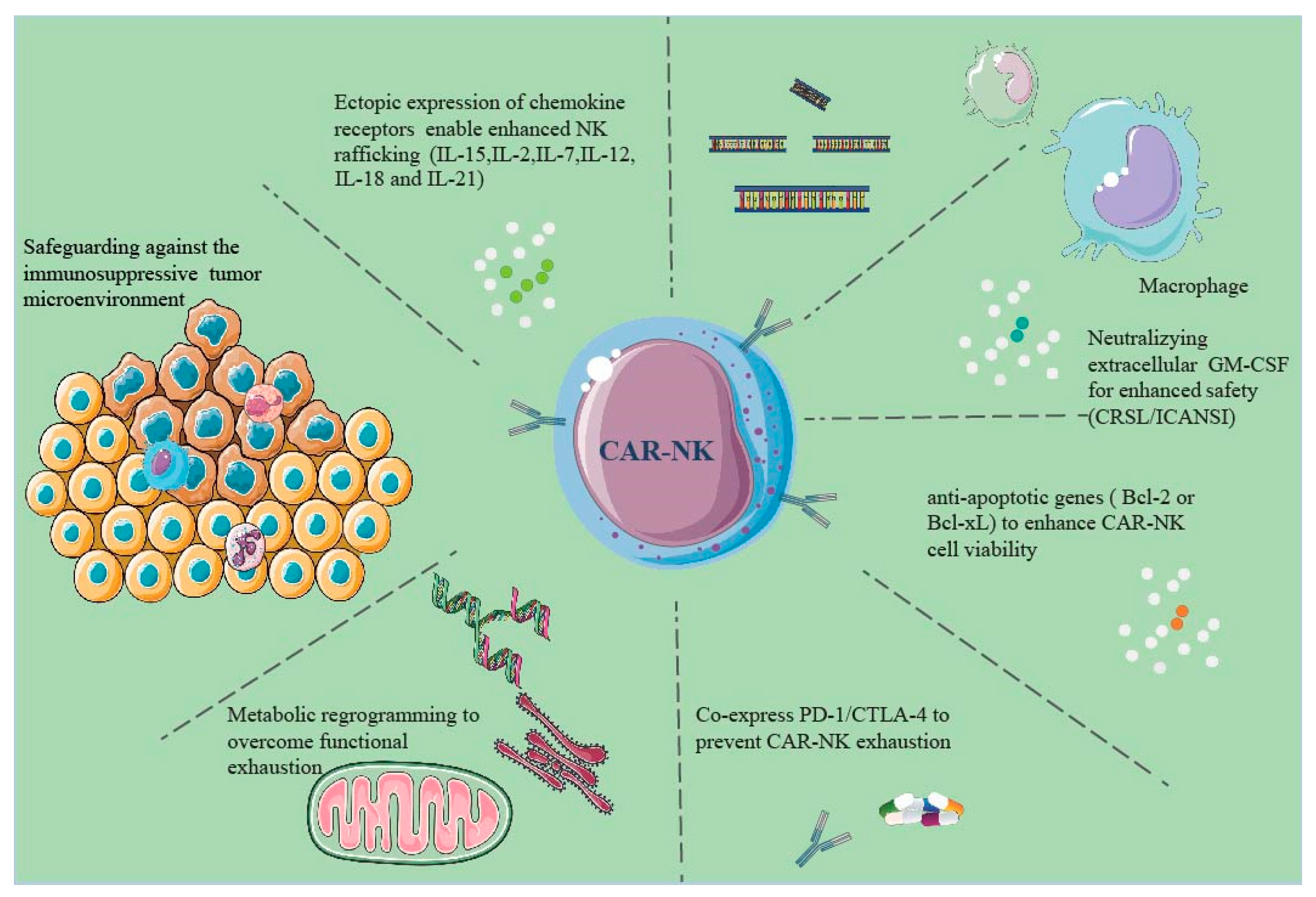
- Enhanced CAR Designs: The initial generation of CARs featured a single-chain variable fragment (scFv) from an antibody targeting a tumor antigen, linked to a CD3ζ signaling domain for NK cell activation [61]. However, limitations in efficacy and persistence arose, with CAR-NK cells becoming exhausted or anergic after repeated activations. Addressing these drawbacks, subsequent generations of CARs now incorporate additional co-stimulatory domains, like CD28, 4-1BB, or OX40 [62]. These modifications significantly bolster the survival, proliferation, and functionality of CAR-NK cells [63]. Further, innovations have led to exploring diverse antigen recognition formats, such as NKG2D receptors, bispecific antibodies, or nanobodies, enhancing the specificity and adaptability of CAR-NK cells [64].
- (2)
- Identification of Novel Therapeutic Targets: The efficacy and safety of CAR-NK cell therapy heavily depend on the chosen tumor antigens. Ideal targets are those predominantly expressed on tumor cells, minimizing off-target effects on healthy tissues [65]. However, this is challenging since many tumor antigens also appear on normal cells at lower levels. To circumvent this, researchers have discovered more tumor-specific targets. Some target antigens are uniquely expressed in tumor-specific conditions, like HIF1α in hypoxic environments [12], while others, like CD38 or CD19, exhibit distinct glycosylation patterns in tumor cells compared to their normal counterparts [19].
- (3)
- Synergistic Combination Therapies: The integration of CAR-NK cells with other treatment modalities – such as chemotherapy, radiotherapy, checkpoint inhibitors, or cytokines – offers a promising strategy to elevate their effectiveness and safety [66]. These combinations can synergistically augment tumor infiltration, activation, persistence, and anti-tumor activity of CAR-NK cells [67]. For instance, combining CAR-NK cells with IL-15 or IL-21 can significantly enhance NK cell survival and functionality [68]. Additionally, pairing CAR-NK cells with PD-1 or PD-L1 inhibitors can disrupt the immune checkpoints that typically inhibit NK cell activity [69].
4.3. Strategies to Enhance CAR-NK Cells
4.4. Synthetic Biology Applications in CAR-NK Cells:
5. Clinical Applications and Future Outlook
5.1. Clinical Trials of CAR-NK Cells:
5.2. Future Research Directions and Challenges
- (1)
- Optimizing CAR Design and Engineering:
- (2)
- Developing Novel Sources and Production Methods:
- (3)
- Overcoming Tumor Microenvironment Barriers:
- (4)
- Addressing Off-Target Effects and Adverse Events:
- (5)
- Enhancing Surgical Oncology Outcomes through CAR-NK Cell Therapy Integration
- (6)
- Ethical Considerations in CAR-NK Cell Therapy:
6. Summary
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Mitra, A.; Barua, A.; Huang, L.; Ganguly, S.; Feng, Q.; He, B. From bench to bedside: the history and progress of CAR T cell therapy. Front Immunol 2023, 14, 1188049. [Google Scholar] [CrossRef] [PubMed]
- Maus, M.V. A decade of CAR T cell evolution. Nat Cancer 2022, 3, 270–271. [Google Scholar] [CrossRef] [PubMed]
- Pan, K.; Farrukh, H.; Chittepu, V.; Xu, H.; Pan, C.X.; Zhu, Z. CAR race to cancer immunotherapy: from CAR T, CAR NK to CAR macrophage therapy. J Exp Clin Cancer Res 2022, 41, 119. [Google Scholar] [CrossRef] [PubMed]
- Huang, R.; Wen, Q.; Zhang, X. CAR-NK cell therapy for hematological malignancies: recent updates from ASH 2022. J Hematol Oncol 2023, 16, 35. [Google Scholar] [CrossRef] [PubMed]
- Ghazvinian, Z.; Abdolahi, S.; Tokhanbigli, S.; Tarzemani, S.; Piccin, A.; Reza Zali, M.; Verdi, J.; Baghaei, K. Contribution of natural killer cells in innate immunity against colorectal cancer. Front Oncol 2022, 12, 1077053. [Google Scholar] [CrossRef]
- Liu, E.; Marin, D.; Banerjee, P.; Macapinlac, H.A.; Thompson, P.; Basar, R.; Nassif Kerbauy, L.; Overman, B.; Thall, P.; Kaplan, M.; et al. Use of CAR-Transduced Natural Killer Cells in CD19-Positive Lymphoid Tumors. N Engl J Med 2020, 382, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Rezvani, K.; Rouce, R.; Liu, E.; Shpall, E. Engineering Natural Killer Cells for Cancer Immunotherapy. Mol Ther 2017, 25, 1769–1781. [Google Scholar] [CrossRef]
- Zhang, C.; Wang, Z.; Yang, Z.; Wang, M.; Li, S.; Li, Y.; Zhang, R.; Xiong, Z.; Wei, Z.; Shen, J.; et al. Phase I Escalating-Dose Trial of CAR-T Therapy Targeting CEA(+) Metastatic Colorectal Cancers. Mol Ther 2017, 25, 1248–1258. [Google Scholar] [CrossRef]
- Glienke, W.; Esser, R.; Priesner, C.; Suerth, J.D.; Schambach, A.; Wels, W.S.; Grez, M.; Kloess, S.; Arseniev, L.; Koehl, U. Advantages and applications of CAR-expressing natural killer cells. Front Pharmacol 2015, 6, 21. [Google Scholar] [CrossRef]
- Klingemann, H. The NK-92 cell line-30 years later: its impact on natural killer cell research and treatment of cancer. Cytotherapy 2023, 25, 451–457. [Google Scholar] [CrossRef]
- Li, T.; Niu, M.; Zhang, W.; Qin, S.; Zhou, J.; Yi, M. CAR-NK cells for cancer immunotherapy: recent advances and future directions. Front Immunol 2024, 15, 1361194. [Google Scholar] [CrossRef] [PubMed]
- Xie, G.; Dong, H.; Liang, Y.; Ham, J.D.; Rizwan, R.; Chen, J. CAR-NK cells: A promising cellular immunotherapy for cancer. EBioMedicine 2020, 59, 102975. [Google Scholar] [CrossRef] [PubMed]
- Basar, R.; Daher, M.; Rezvani, K. Next-generation cell therapies: the emerging role of CAR-NK cells. Hematology Am Soc Hematol Educ Program 2020, 2020, 570–578. [Google Scholar] [CrossRef]
- Kvacskay, P.; Merkt, W. CD19.CAR T cells versus obinutuzumab—who will win the race for use in deep B cell depletion therapy in systemic autoimmunity? Rheumatology 2024. [CrossRef]
- Wang, Y.; Rousset, X.; Prunier, C.; Dosda, E.; Gutierrez-Guerrero, A.; Abrial, P.; Menkova, I.; Viallet, J. Abstract 4018: An innovative in vivo model for CAR-T cell therapy development: Tolerability and efficacy evaluation of CD19-targeting CAR-T cells on human lymphoma using the chicken CAM assay. Cancer Research 2024, 84, 4018–4018. [Google Scholar] [CrossRef]
- Ritmeester-Loy, S.A.; Draper, I.H.; Bueter, E.C.; Lautz, J.D.; Zhang-Wong, Y.; Gustafson, J.A.; Wilson, A.L.; Lin, C.; Gafken, P.R.; Jensen, M.C.; et al. Differential protein-protein interactions underlie signaling mediated by the TCR and a 4-1BB domain–containing CAR. 2024, 17, eadd4671. [Google Scholar] [CrossRef] [PubMed]
- Herrera, L.; Santos, S.; Vesga, M.A.; Carrascosa, T.; Garcia-Ruiz, J.C.; Perez-Martinez, A.; Juan, M.; Eguizabal, C. The Race of CAR Therapies: CAR-NK Cells for Fighting B-Cell Hematological Cancers. Cancers (Basel) 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Page, A.; Chuvin, N.; Valladeau-Guilemond, J.; Depil, S. Development of NK cell-based cancer immunotherapies through receptor engineering. Cellular & Molecular Immunology 2024, 21, 315–331. [Google Scholar] [CrossRef]
- Zhang, L.; Meng, Y.; Feng, X.; Han, Z. CAR-NK cells for cancer immunotherapy: from bench to bedside. Biomarker research 2022, 10, 12. [Google Scholar] [CrossRef]
- Flemming, A. CD3ε tunes CAR T cell anticancer activity. Nature Reviews Immunology 2020, 20, 520–521. [Google Scholar] [CrossRef]
- Singh, R.; Kim, Y.H.; Lee, S.J.; Eom, H.S.; Choi, B.K. 4-1BB immunotherapy: advances and hurdles. Exp Mol Med 2024, 56, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Cappell, K.M.; Kochenderfer, J.N. A comparison of chimeric antigen receptors containing CD28 versus 4-1BB costimulatory domains. Nat Rev Clin Oncol 2021, 18, 715–727. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Zhang, R.; Nie, X.; Yang, Y.; Hua, Y.; Lu, P. 4-1BB Targeting Immunotherapy: Mechanism, Antibodies, and Chimeric Antigen Receptor T. Cancer Biother Radiopharm 2023, 38, 431–444. [Google Scholar] [CrossRef] [PubMed]
- Depil, S.; Duchateau, P.; Grupp, S.A.; Mufti, G.; Poirot, L. 'Off-the-shelf' allogeneic CAR T cells: development and challenges. Nat Rev Drug Discov 19, 185-199. [CrossRef]
- Caimi, P.F.; Melenhorst, J.J. Allogeneic CAR T Cells: Complex Cellular Therapy Designs Test the Limits of Our Preclinical Models. Cancer Immunology Research 2024, 12, 385–386. [Google Scholar] [CrossRef] [PubMed]
- Heipertz, E.L.; Zynda, E.R.; Stav-Noraas, T.E.; Hungler, A.D.; Boucher, S.E.; Kaur, N.; Vemuri, M.C. Current Perspectives on "Off-The-Shelf" Allogeneic NK and CAR-NK Cell Therapies. Front Immunol 2021, 12, 732135. [Google Scholar] [CrossRef]
- Barnes, S.A.; Trew, I.; de Jong, E.; Foley, B. Making a Killer: Selecting the Optimal Natural Killer Cells for Improved Immunotherapies. Front Immunol 2021, 12, 765705. [Google Scholar] [CrossRef] [PubMed]
- Khawar, M.B.; Sun, H. CAR-NK Cells: From Natural Basis to Design for Kill. Front Immunol 2021, 12, 707542. [Google Scholar] [CrossRef] [PubMed]
- Si, X.; Xiao, L.; Brown, C.E.; Wang, D. Preclinical Evaluation of CAR T Cell Function: In Vitro and In Vivo Models. Int J Mol Sci 2022, 23. [Google Scholar] [CrossRef]
- Hwu, P.; Rosenberg, S.A. The genetic modification of T cells for cancer therapy: an overview of laboratory and clinical trials. Cancer Detect Prev 1994, 18, 43–50. [Google Scholar]
- Rosenberg, S.A.; Restifo, N.P. Adoptive cell transfer as personalized immunotherapy for human cancer. 2015, 348, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Roddie, C.; O'Reilly, M.; Dias Alves Pinto, J.; Vispute, K.; Lowdell, M. Manufacturing chimeric antigen receptor T cells: issues and challenges. Cytotherapy 2019, 21, 327–340. [Google Scholar] [CrossRef] [PubMed]
- Rezvani, K.; Rouce, R.H. The Application of Natural Killer Cell Immunotherapy for the Treatment of Cancer. Front Immunol 2015, 6, 578. [Google Scholar] [CrossRef] [PubMed]
- Ghassemi, S.; Durgin, J.S.; Nunez-Cruz, S.; Patel, J.; Leferovich, J.; Pinzone, M.; Shen, F.; Cummins, K.D.; Plesa, G.; Cantu, V.A.; et al. Rapid manufacturing of non-activated potent CAR T cells. Nat Biomed Eng 2022, 6, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Wrona, E.; Borowiec, M.; Potemski, P. CAR-NK Cells in the Treatment of Solid Tumors. Int J Mol Sci 2021, 22. [Google Scholar] [CrossRef] [PubMed]
- Portillo, A.L.; Hogg, R.; Ashkar, A.A. Production of human CAR-NK cells with lentiviral vectors and functional assessment in vitro. STAR Protoc 2021, 2, 100956. [Google Scholar] [CrossRef] [PubMed]
- Naeimi Kararoudi, M.; Likhite, S.; Elmas, E.; Yamamoto, K.; Schwartz, M.; Sorathia, K.; de Souza Fernandes Pereira, M.; Sezgin, Y.; Devine, R.D.; Lyberger, J.M.; et al. Optimization and validation of CAR transduction into human primary NK cells using CRISPR and AAV. Cell reports methods 2022, 2, 100236. [Google Scholar] [CrossRef] [PubMed]
- Tomasik, J.; Jasinski, M.; Basak, G.W. Next generations of CAR-T cells - new therapeutic opportunities in hematology? Front Immunol 2022, 13, 1034707. [Google Scholar] [CrossRef] [PubMed]
- Sadelain, M.; Rivière, I.; Riddell, S. Therapeutic T cell engineering. Nature 2017, 545, 423–431. [Google Scholar] [CrossRef]
- Schaible, P.; Bethge, W.; Lengerke, C.; Haraszti, R.A. RNA Therapeutics for Improving CAR T-cell Safety and Efficacy. Cancer Res 2023, 83, 354–362. [Google Scholar] [CrossRef]
- Shin, E.; Bak, S.H.; Park, T.; Kim, J.W.; Yoon, S.R.; Jung, H.; Noh, J.Y. Understanding NK cell biology for harnessing NK cell therapies: targeting cancer and beyond. Front Immunol 2023, 14, 1192907. [Google Scholar] [CrossRef] [PubMed]
- Neelapu, S.S.; Tummala, S.; Kebriaei, P.; Wierda, W.; Gutierrez, C.; Locke, F.L.; Komanduri, K.V.; Lin, Y.; Jain, N.; Daver, N.; et al. Chimeric antigen receptor T-cell therapy - assessment and management of toxicities. Nat Rev Clin Oncol 2018, 15, 47–62. [Google Scholar] [CrossRef] [PubMed]
- Brudno, J.N.; Kochenderfer, J.N. Toxicities of chimeric antigen receptor T cells: recognition and management. Blood 2016, 127, 3321–3330. [Google Scholar] [CrossRef] [PubMed]
- Roschewski, M.; Longo, D.L.; Wilson, W.H. CAR T-Cell Therapy for Large B-Cell Lymphoma — Who, When, and How? 2022, 386, 692-696. [CrossRef]
- Fang, F.; Xiao, W.; Tian, Z. NK cell-based immunotherapy for cancer. Seminars in immunology 2017, 31, 37–54. [Google Scholar] [CrossRef] [PubMed]
- Yan, T.; Zhu, L.; Chen, J. Current advances and challenges in CAR T-Cell therapy for solid tumors: tumor-associated antigens and the tumor microenvironment. Exp Hematol Oncol 2023, 12, 14. [Google Scholar] [CrossRef]
- Lee, M.Y.; Robbins, Y.; Sievers, C.; Friedman, J.; Abdul Sater, H.; Clavijo, P.E.; Judd, N.; Tsong, E.; Silvin, C.; Soon-Shiong, P.; et al. Chimeric antigen receptor engineered NK cellular immunotherapy overcomes the selection of T-cell escape variant cancer cells. J Immunother Cancer 2021, 9. [Google Scholar] [CrossRef]
- Lu, H.; Zhao, X.; Li, Z.; Hu, Y.; Wang, H. From CAR-T Cells to CAR-NK Cells: A Developing Immunotherapy Method for Hematological Malignancies. 2021, 11. [CrossRef]
- Zhang, X.W.; Wu, Y.S.; Xu, T.M.; Cui, M.H. CAR-T Cells in the Treatment of Ovarian Cancer: A Promising Cell Therapy. Biomolecules 2023, 13. [Google Scholar] [CrossRef]
- Katy Spink; Steinsapir, A. The long road to affordability: a cost of goods analysis for an autologous CAR-T process. Cell Gene Therapy Insights 2018, 4, 1105–1116. [CrossRef]
- Fang, F.; Xie, S.; Chen, M.; Li, Y.; Yue, J.; Ma, J.; Shu, X.; He, Y.; Xiao, W.; Tian, Z. Advances in NK cell production. Cell Mol Immunol 2022, 19, 460–481. [Google Scholar] [CrossRef] [PubMed]
- Elahi, R.; Heidary, A.H.; Hadiloo, K.; Esmaeilzadeh, A. Chimeric Antigen Receptor-Engineered Natural Killer (CAR NK) Cells in Cancer Treatment; Recent Advances and Future Prospects. Stem Cell Rev Rep 2021, 17, 2081–2106. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Meng, Y.; Zhang, L.; Han, Z.; Feng, X. High-efficient generation of natural killer cells from peripheral blood with preferable cell vitality and enhanced cytotoxicity by combination of IL-2, IL-15 and IL-18. Biochem Biophys Res Commun 2021, 534, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Rafei, H.; Daher, M.; Rezvani, K. Chimeric antigen receptor (CAR) natural killer (NK)-cell therapy: leveraging the power of innate immunity. Br J Haematol 2021, 193, 216–230. [Google Scholar] [CrossRef] [PubMed]
- Wen, W.; Chen, X.; Shen, X.-Y.; Li, H.-Y.; Zhang, F.; Fang, F.-Q.; Zhang, X.-B. Enhancing cord blood stem cell-derived NK cell growth and differentiation through hyperosmosis. Stem Cell Research & Therapy 2023, 14, 295. [Google Scholar] [CrossRef]
- Bozhilov, Y.K.; Hsu, I.; Brown, E.J.; Wilkinson, A.C. In Vitro Human Haematopoietic Stem Cell Expansion and Differentiation. Cells 2023, 12. [Google Scholar] [CrossRef]
- Hsu, L.J.; Liu, C.L.; Kuo, M.L.; Shen, C.N.; Shen, C.R. An Alternative Cell Therapy for Cancers: Induced Pluripotent Stem Cell (iPSC)-Derived Natural Killer Cells. Biomedicines 2021, 9. [Google Scholar] [CrossRef]
- Montazersaheb, S.; Fathi, E.; Farahzadi, R. Cytokines and signaling pathways involved in differentiation potential of hematopoietic stem cells towards natural killer cells. Tissue Cell 2021, 70, 101501. [Google Scholar] [CrossRef] [PubMed]
- Moseman, J.E.; Foltz, J.A.; Sorathia, K.; Heipertz, E.L.; Lee, D.A. Evaluation of serum-free media formulations in feeder cell–stimulated expansion of natural killer cells. Cytotherapy 2020, 22, 322–328. [Google Scholar] [CrossRef]
- Klingemann, H.; Boissel, L.; Toneguzzo, F. Natural Killer Cells for Immunotherapy - Advantages of the NK-92 Cell Line over Blood NK Cells. Front Immunol 2016, 7, 91. [Google Scholar] [CrossRef]
- Zhang, C.; Oberoi, P.; Oelsner, S.; Waldmann, A.; Lindner, A.; Tonn, T.; Wels, W.S. Chimeric Antigen Receptor-Engineered NK-92 Cells: An Off-the-Shelf Cellular Therapeutic for Targeted Elimination of Cancer Cells and Induction of Protective Antitumor Immunity. Front Immunol 2017, 8, 533. [Google Scholar] [CrossRef] [PubMed]
- Chu, J.; Deng, Y.; Benson, D.M.; He, S.; Hughes, T.; Zhang, J.; Peng, Y.; Mao, H.; Yi, L.; Ghoshal, K.; et al. CS1-specific chimeric antigen receptor (CAR)-engineered natural killer cells enhance in vitro and in vivo antitumor activity against human multiple myeloma. Leukemia 2014, 28, 917–927. [Google Scholar] [CrossRef] [PubMed]
- Imai, C.; Iwamoto, S.; Campana, D. Genetic modification of primary natural killer cells overcomes inhibitory signals and induces specific killing of leukemic cells. Blood 2005, 106, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Schonfeld, K.; Sahm, C.; Zhang, C.; Naundorf, S.; Brendel, C.; Odendahl, M.; Nowakowska, P.; Bonig, H.; Kohl, U.; Kloess, S.; et al. Selective inhibition of tumor growth by clonal NK cells expressing an ErbB2/HER2-specific chimeric antigen receptor. Mol Ther 2015, 23, 330–338. [Google Scholar] [CrossRef] [PubMed]
- St-Pierre, F.; Bhatia, S.; Chandra, S. Harnessing Natural Killer Cells in Cancer Immunotherapy: A Review of Mechanisms and Novel Therapies. Cancers (Basel) 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Yan, Y.; Zhang, J.; Wei, Z.; Li, H.; Xing, L. Synergistic treatment strategy: combining CAR-NK cell therapy and radiotherapy to combat solid tumors. Front Immunol 2023, 14, 1298683. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Hu, Y.; Shi, C. Targeting Natural Killer Cells for Tumor Immunotherapy. Front Immunol 2020, 11, 60. [Google Scholar] [CrossRef] [PubMed]
- Romee, R.; Rosario, M.; Berrien-Elliott, M.M.; Wagner, J.A.; Jewell, B.A.; Schappe, T.; Leong, J.W.; Abdel-Latif, S.; Schneider, S.E.; Willey, S.; et al. Cytokine-induced memory-like natural killer cells exhibit enhanced responses against myeloid leukemia. Sci Transl Med 2016, 8, 357ra123. [Google Scholar] [CrossRef] [PubMed]
- Jia, L.; Zhang, Q.; Zhang, R. PD-1/PD-L1 pathway blockade works as an effective and practical therapy for cancer immunotherapy. Cancer biology & medicine 2018, 15, 116–123. [Google Scholar] [CrossRef]
- Valeri, A.; Garcia-Ortiz, A.; Castellano, E.; Cordoba, L.; Maroto-Martin, E.; Encinas, J.; Leivas, A.; Rio, P.; Martinez-Lopez, J. Overcoming tumor resistance mechanisms in CAR-NK cell therapy. Front Immunol 2022, 13, 953849. [Google Scholar] [CrossRef]
- Li, H.; Zhao, Y. Increasing the safety and efficacy of chimeric antigen receptor T cell therapy. Protein Cell 2017, 8, 573–589. [Google Scholar] [CrossRef]
- Lanier, L.L. Up on the tightrope: natural killer cell activation and inhibition. Nat Immunol 2008, 9, 495–502. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhou, W.; Yang, J.; Yang, J.; Wang, W. Chimeric antigen receptor engineered natural killer cells for cancer therapy. Exp Hematol Oncol 2023, 12, 70. [Google Scholar] [CrossRef]
- Liu, G.; Rui, W.; Zheng, H.; Huang, D.; Yu, F.; Zhang, Y.; Dong, J.; Zhao, X.; Lin, X. CXCR2-modified CAR-T cells have enhanced trafficking ability that improves treatment of hepatocellular carcinoma. European journal of immunology 2020, 50, 712–724. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Wang, Y.; Miao, L.; Liu, Q.; Musetti, S.; Li, J.; Huang, L. Combination Immunotherapy of MUC1 mRNA Nano-vaccine and CTLA-4 Blockade Effectively Inhibits Growth of Triple Negative Breast Cancer. Mol Ther 2018, 26, 45–55. [Google Scholar] [CrossRef]
- Doedens, A.L.; Phan, A.T.; Stradner, M.H.; Fujimoto, J.K.; Nguyen, J.V.; Yang, E.; Johnson, R.S.; Goldrath, A.W. Hypoxia-inducible factors enhance the effector responses of CD8(+) T cells to persistent antigen. Nat Immunol 2013, 14, 1173–1182. [Google Scholar] [CrossRef] [PubMed]
- Kilgour, M.K.; Bastin, D.J.; Lee, S.-H.; Ardolino, M.; McComb, S.; Visram, A. Advancements in CAR-NK therapy: lessons to be learned from CAR-T therapy. 2023, 14. [CrossRef]
- Pattingre, S.; Tassa, A.; Qu, X.; Garuti, R.; Liang, X.H.; Mizushima, N.; Packer, M.; Schneider, M.D.; Levine, B. Bcl-2 antiapoptotic proteins inhibit Beclin 1-dependent autophagy. Cell 2005, 122, 927–939. [Google Scholar] [CrossRef] [PubMed]
- Cherkassky, L.; Morello, A.; Villena-Vargas, J.; Feng, Y.; Dimitrov, D.S.; Jones, D.R.; Sadelain, M.; Adusumilli, P.S. Human CAR T cells with cell-intrinsic PD-1 checkpoint blockade resist tumor-mediated inhibition. J Clin Invest 2016, 126, 3130–3144. [Google Scholar] [CrossRef]
- Dillon, L.M.; Rebelo, A.P.; Moraes, C.T. The role of PGC-1 coactivators in aging skeletal muscle and heart. IUBMB Life 2012, 64, 231–241. [Google Scholar] [CrossRef]
- Denman, C.J.; Senyukov, V.V.; Somanchi, S.S.; Phatarpekar, P.V.; Kopp, L.M.; Johnson, J.L.; Singh, H.; Hurton, L.; Maiti, S.N.; Huls, M.H.; et al. Membrane-bound IL-21 promotes sustained ex vivo proliferation of human natural killer cells. PLoS One 2012, 7, e30264. [Google Scholar] [CrossRef]
- Delconte, R.B.; Kolesnik, T.B.; Dagley, L.F.; Rautela, J.; Shi, W.; Putz, E.M.; Stannard, K.; Zhang, J.G.; Teh, C.; Firth, M.; et al. CIS is a potent checkpoint in NK cell-mediated tumor immunity. Nat Immunol 2016, 17, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Chen, S. Releasing the brake in CAR natural killer cells. Blood 2021, 137, 579–581. [Google Scholar] [CrossRef] [PubMed]
- Imamura, M.; Shook, D.; Kamiya, T.; Shimasaki, N.; Chai, S.M.; Coustan-Smith, E.; Imai, C.; Campana, D. Autonomous growth and increased cytotoxicity of natural killer cells expressing membrane-bound interleukin-15. Blood 2014, 124, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, R.; Baker, J.; Beilhack, A.; Zeiser, R.; Olson, J.A.; Sega, E.I.; Karimi, M.; Negrin, R.S. In vivo trafficking and survival of cytokine-induced killer cells resulting in minimal GVHD with retention of antitumor activity. Blood 2008, 112, 2563–2574. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Yang, Y.; Wang, G.; Liu, M. Current landscape and future directions of bispecific antibodies in cancer immunotherapy. Front Immunol 2022, 13, 1035276. [Google Scholar] [CrossRef] [PubMed]
- Basar, R.; Daher, M.; Rezvani, K. Next-generation cell therapies: the emerging role of CAR-NK cells. Blood Adv 2020, 4, 5868–5876. [Google Scholar] [CrossRef] [PubMed]
- Clubb, J.D.; Gao, T.A.; Chen, Y.Y. Synthetic Biology in the Engineering of CAR-T and CAR-NK Cell Therapies: Facts and Hopes. Clin Cancer Res 2023, 29, 1390–1402. [Google Scholar] [CrossRef]
- Zhang, C.; Hu, Y.; Xiao, W.; Tian, Z. Chimeric antigen receptor- and natural killer cell receptor-engineered innate killer cells in cancer immunotherapy. Cell Mol Immunol 2021, 18, 2083–2100. [Google Scholar] [CrossRef]
- Cienfuegos-Jimenez, O.; Vazquez-Garza, E.; Rojas-Martinez, A. CAR-NK Cells for Cancer Therapy: Molecular Redesign of the Innate Antineoplastic Response. Curr Gene Ther 2022, 22, 303–318. [Google Scholar] [CrossRef]
- Jiang, H.; Zhang, W.; Shang, P.; Zhang, H.; Fu, W.; Ye, F.; Zeng, T.; Huang, H.; Zhang, X.; Sun, W.; et al. Transfection of chimeric anti-CD138 gene enhances natural killer cell activation and killing of multiple myeloma cells. Mol Oncol 2014, 8, 297–310. [Google Scholar] [CrossRef]
- Yang, L.; Shen, M.; Xu, L.J.; Yang, X.; Tsai, Y.; Keng, P.C.; Chen, Y.; Lee, S.O. Enhancing NK cell-mediated cytotoxicity to cisplatin-resistant lung cancer cells via MEK/Erk signaling inhibition. Sci Rep 2017, 7, 7958. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Chen, C.; Guo, Y.; Hu, S.; Sun, Z. Effect of CRISPR/Cas9-Edited PD-1/PD-L1 on Tumor Immunity and Immunotherapy. Front Immunol 2022, 13, 848327. [Google Scholar] [CrossRef] [PubMed]
- Dai, H.; Wu, Z.; Jia, H.; Tong, C.; Guo, Y.; Ti, D.; Han, X.; Liu, Y.; Zhang, W.; Wang, C.; et al. Bispecific CAR-T cells targeting both CD19 and CD22 for therapy of adults with relapsed or refractory B cell acute lymphoblastic leukemia. J Hematol Oncol 2020, 13, 30. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, K.; Nishikawa, H. Engineering strategies for broad application of TCR-T- and CAR-T-cell therapies. Int Immunol 2021, 33, 551–562. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Chen, R.; Huang, Y.; Meng, X.; Chen, J.; Liao, C.; Tang, Y.; Zhou, C.; Gao, X.; Sun, J. Tuning the ignition of CAR: optimizing the affinity of scFv to improve CAR-T therapy. Cell Mol Life Sci 2021, 79, 14. [Google Scholar] [CrossRef] [PubMed]
- Brudno, J.N.; Lam, N.; Vanasse, D.; Shen, Y.W.; Rose, J.J.; Rossi, J.; Xue, A.; Bot, A.; Scholler, N.; Mikkilineni, L.; et al. Safety and feasibility of anti-CD19 CAR T cells with fully human binding domains in patients with B-cell lymphoma. Nature medicine 2020, 26, 270–280. [Google Scholar] [CrossRef] [PubMed]
- Themeli, M.; Kloss, C.C.; Ciriello, G.; Fedorov, V.D.; Perna, F.; Gonen, M.; Sadelain, M. Generation of tumor-targeted human T lymphocytes from induced pluripotent stem cells for cancer therapy. Nat Biotechnol 2013, 31, 928–933. [Google Scholar] [CrossRef] [PubMed]
- Knorr, D.A.; Ni, Z.; Hermanson, D.; Hexum, M.K.; Bendzick, L.; Cooper, L.J.; Lee, D.A.; Kaufman, D.S. Clinical-scale derivation of natural killer cells from human pluripotent stem cells for cancer therapy. Stem Cells Transl Med 2013, 2, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Melaiu, O.; Lucarini, V.; Cifaldi, L.; Fruci, D. Influence of the Tumor Microenvironment on NK Cell Function in Solid Tumors. Front Immunol 2019, 10, 3038. [Google Scholar] [CrossRef]
- Vitale, M.; Cantoni, C.; Pietra, G.; Mingari, M.C.; Moretta, L. Effect of tumor cells and tumor microenvironment on NK-cell function. European journal of immunology 2014, 44, 1582–1592. [Google Scholar] [CrossRef]
- Murugan, D.; Murugesan, V.; Panchapakesan, B.; Rangasamy, L. Nanoparticle Enhancement of Natural Killer (NK) Cell-Based Immunotherapy. 2022, 14, 5438.
- El-Mayta, R.; Zhang, Z.; Hamilton, A.G.; Mitchell, M.J. Delivery technologies to engineer natural killer cells for cancer immunotherapy. Cancer Gene Ther 2021, 28, 947–959. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Song, W.; Li, Z.; Zhang, M. Preclinical and clinical studies of CAR-NK-cell therapies for malignancies. Front Immunol 2022, 13, 992232. [Google Scholar] [CrossRef]
- Santomasso, B.D.; Nastoupil, L.J.; Adkins, S.; Lacchetti, C.; Schneider, B.J.; Anadkat, M.; Atkins, M.B.; Brassil, K.J.; Caterino, J.M.; Chau, I.; et al. Management of Immune-Related Adverse Events in Patients Treated With Chimeric Antigen Receptor T-Cell Therapy: ASCO Guideline. J Clin Oncol 2021, 39, 3978–3992. [Google Scholar] [CrossRef]
- Gong, Y.; Klein Wolterink, R.G.J.; Wang, J.; Bos, G.M.J.; Germeraad, W.T.V. Chimeric antigen receptor natural killer (CAR-NK) cell design and engineering for cancer therapy. Journal of Hematology & Oncology 2021, 14, 73. [Google Scholar] [CrossRef]
- He, J.; Yan, Y.; Zhang, J.; Wei, Z.; Li, H.; Xing, L. Synergistic treatment strategy: combining CAR-NK cell therapy and radiotherapy to combat solid tumors. 2023, 14. [CrossRef]
- Zhu, C.; Wu, Q.; Sheng, T.; Shi, J.; Shen, X.; Yu, J.; Du, Y.; Sun, J.; Liang, T.; He, K.; et al. Rationally designed approaches to augment CAR-T therapy for solid tumor treatment. Bioact Mater 2024, 33, 377–395. [Google Scholar] [CrossRef]
- Wang, W.; Liu, Y.; He, Z.; Li, L.; Liu, S.; Jiang, M.; Zhao, B.; Deng, M.; Wang, W.; Mi, X.; et al. Breakthrough of solid tumor treatment: CAR-NK immunotherapy. Cell death discovery 2024, 10, 40. [Google Scholar] [CrossRef]
- Sadeghi, S.; Chen, P.-C.; Jewett, A.; Kaur, K. Chapter 14 - Combination of NK cell immunotherapy with chemotherapy and radiation enhances NK cell therapy and provides improved prognosis in cancer patients and in humanized BLT mouse model system. In NK Cells in Cancer Immunotherapy: Successes and Challenges, Jewett, A., Fong, Y., Eds.; Academic Press: 2023; pp. 301-320.
- Fares, J.; Davis, Z.B.; Rechberger, J.S.; Toll, S.A.; Schwartz, J.D.; Daniels, D.J.; Miller, J.S.; Khatua, S. Advances in NK cell therapy for brain tumors. npj Precision Oncology 2023, 7, 17. [Google Scholar] [CrossRef]
- Kennedy, P.R.; Felices, M.; Miller, J.S. Challenges to the broad application of allogeneic natural killer cell immunotherapy of cancer. Stem Cell Res Ther 2022, 13, 165. [Google Scholar] [CrossRef]
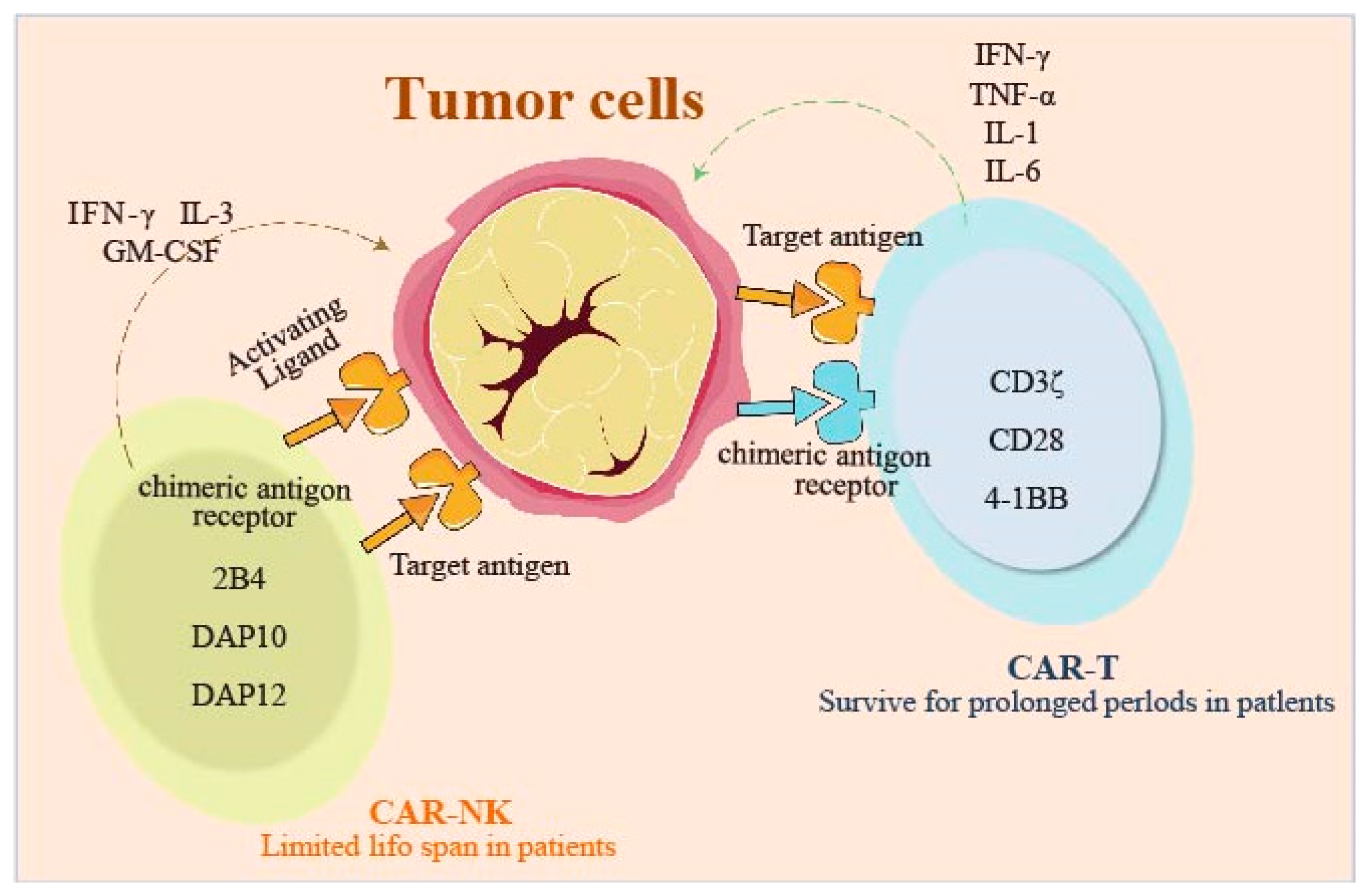
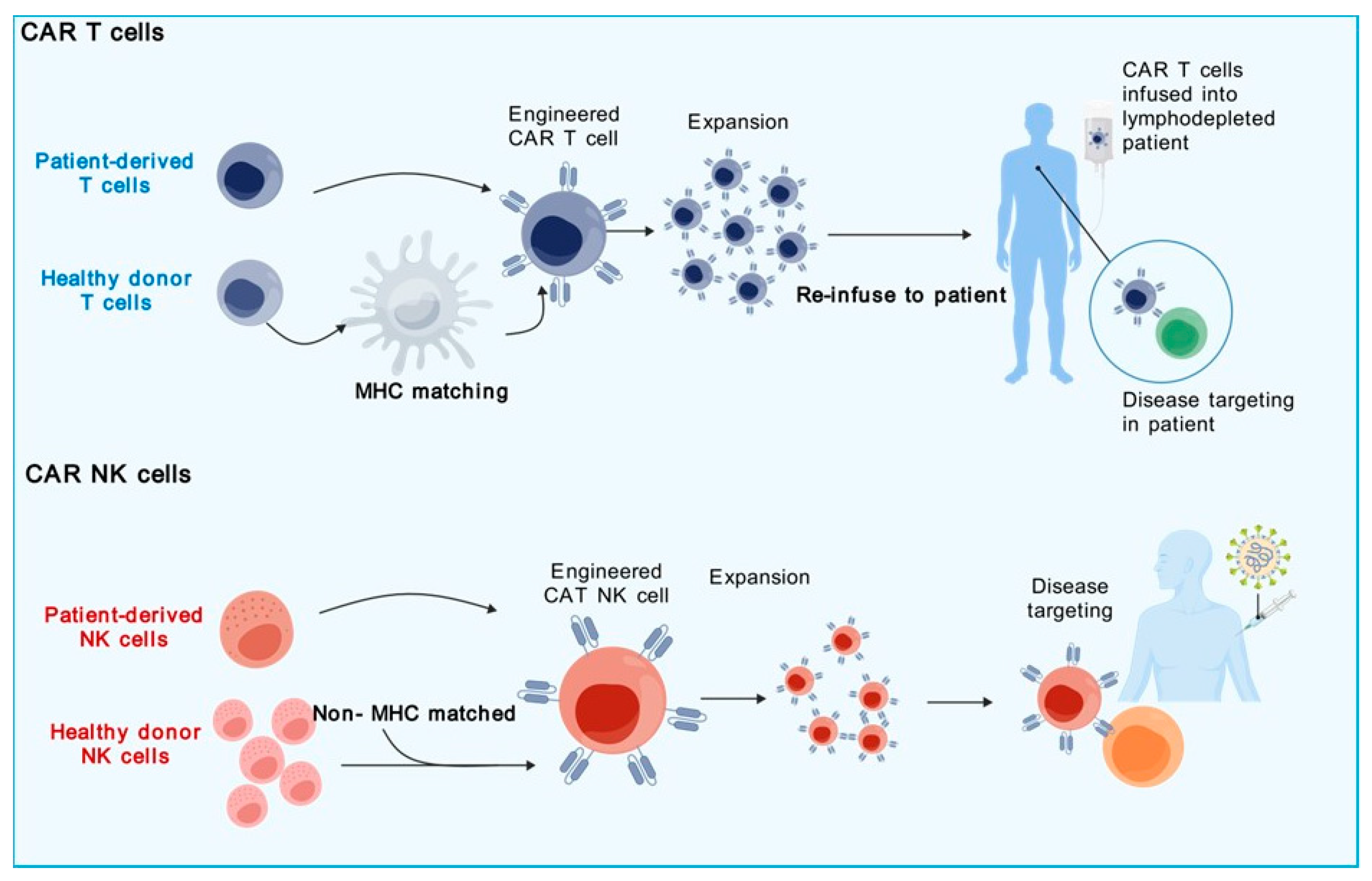
| Parameter | CAR-T Cells | CAR-NK Cells |
|---|---|---|
| Intracellular Signaling Domains | CD3ζ with co-stimulatory domains such as CD28 and 4-1BB | Like CAR-T structure but can utilize NK-specific signaling domains like 2B4, DAP10, DAP12. |
| Cell Source | Autologous or MHC-matched allogeneic | Autologous, non-MHC matched allogeneic cell lines, or NK cell lines |
| Off-the-shelf Ready-to-use CAR Product | Typically, autologous, or MHC-matched allogeneic CAR-T cells | NK cell lines. Allogeneic NK cells possible, but with poor recovery rate post-cryopreservation |
| In Vitro Expansion Capability | Yes | Yes Pre-Expansion Prior to Transduction |
| Cell Killing Mechanism | CAR-dependent cellular cytotoxicity | Both CAR-dependent and CAR-independent NK cell-mediated cytotoxicity |
| Cytokine Release Syndrome and Neurotoxicity | Common and usually severe | Less common |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





