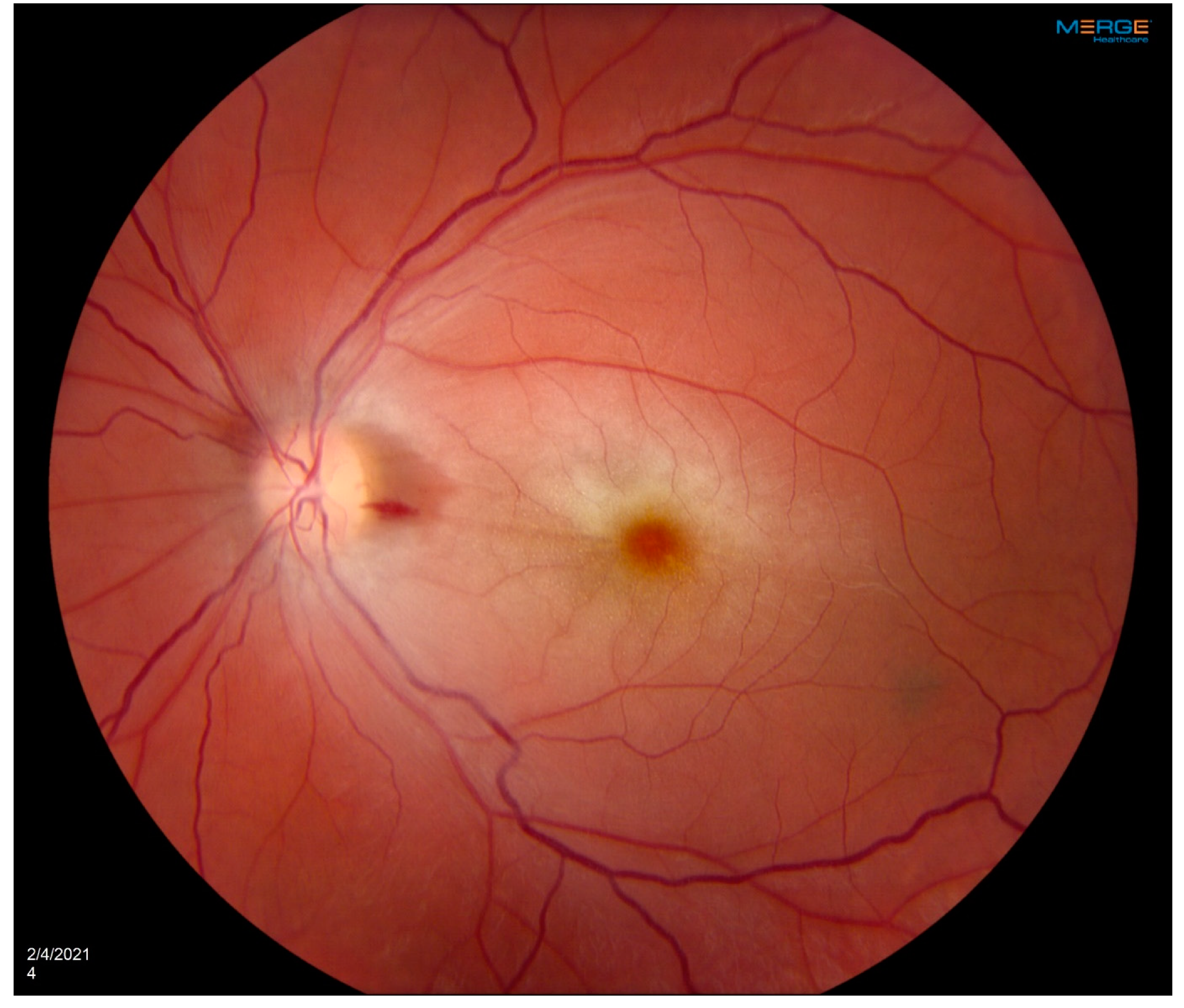
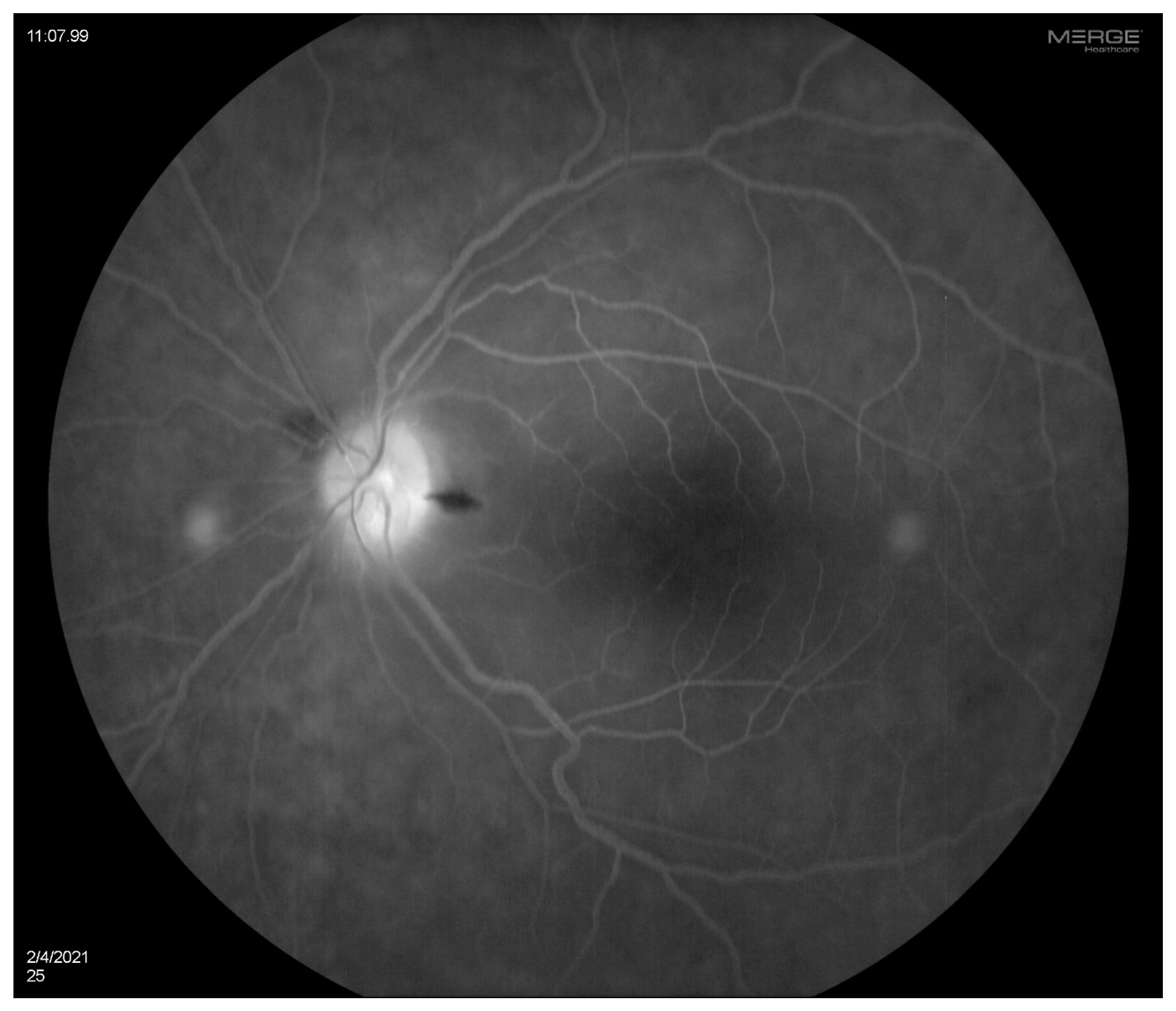
A 35-year-old woman with a prior history of left central retinal artery occlusion and bilateral sensorineural hearing loss concerning initially for neurosarcoidosis (never histologically proven) presented for clinic follow-up. She had a complicated disease course dating back many years involving different specialists including fluctuating hearing loss partially responsive to corticosteroids necessitating cochlear implants and developed central retinal occlusion of the left eye (
Figure 1 and
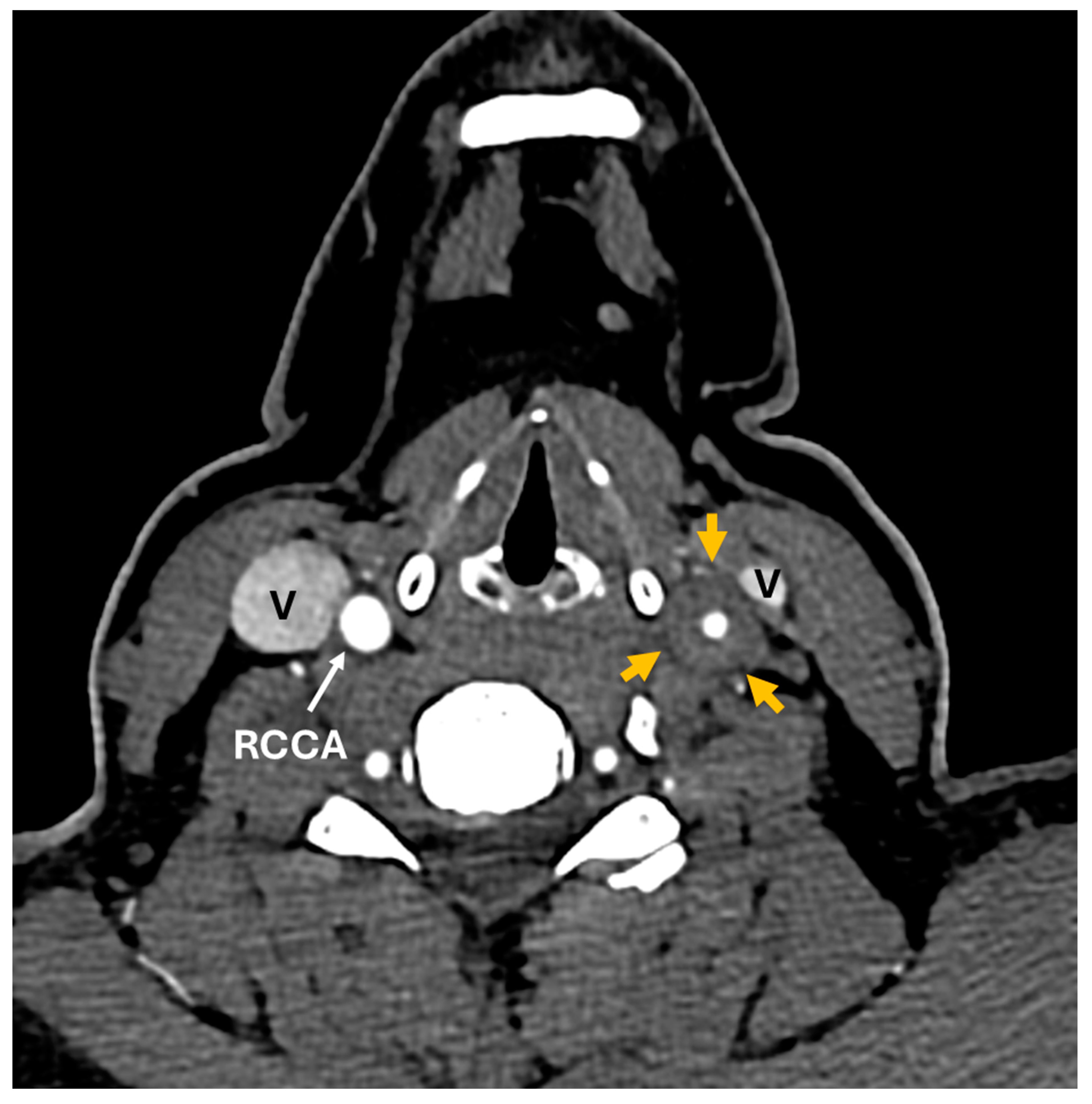
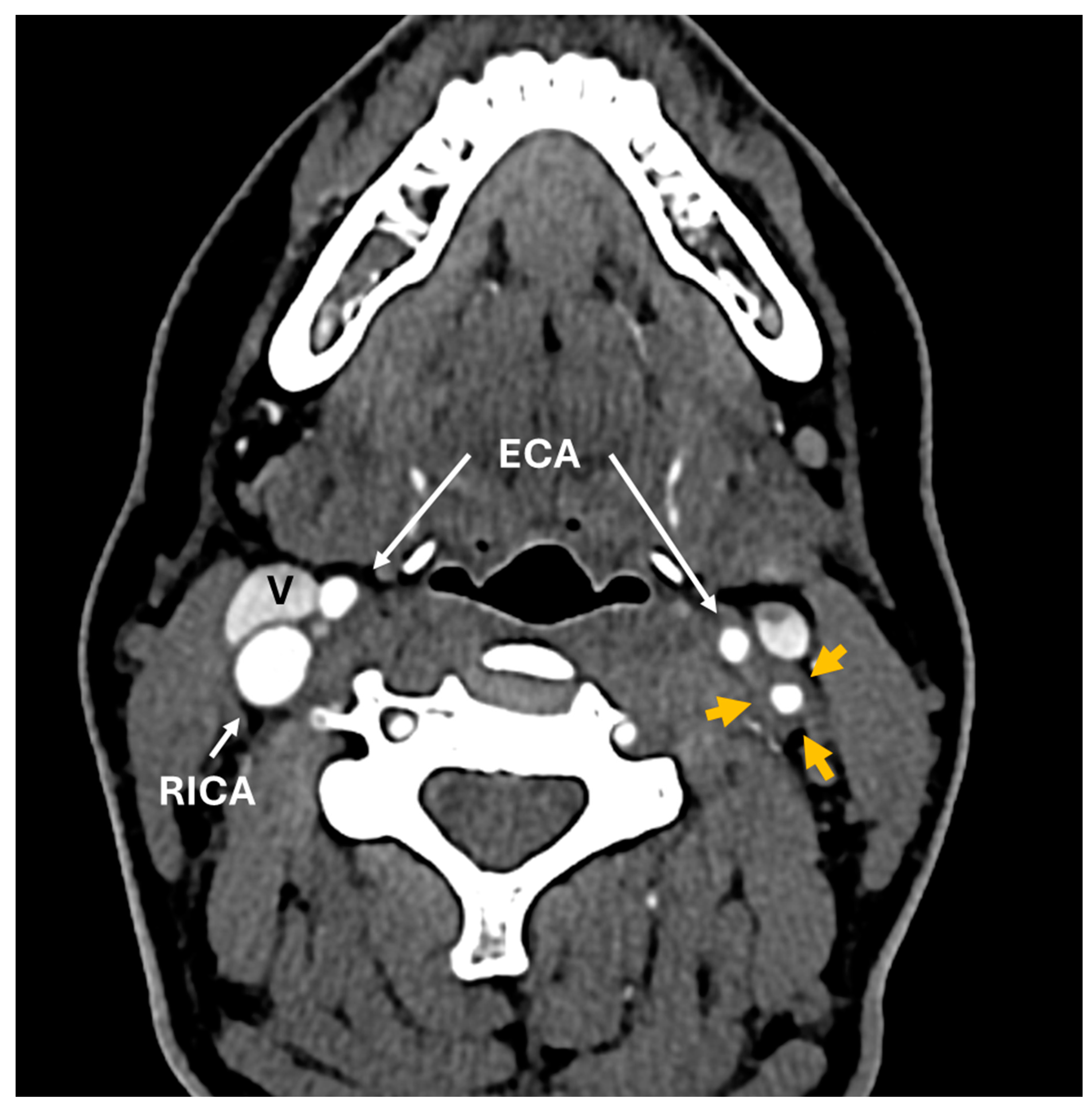
Figure 2). This was concerning for possible underlying inflammatory condition such as neurosarcoidosis or Susac syndrome (MRI atypical sans corpus lesion) and she received IV immunoglobulin treatment. When she returned for follow-up, she had complaints of episodes of confusion, but quiescent symptoms without visual change, status post adalimumab and methotrexate addition. She sought emergency care for new transient arm numbness and confusion and CTA neck revealed carotid bulb circumferential thickening suggestive of vasculitis (
Figure 3,
Figure 4 and
Figure 5). The patient was initiated on Infliximab with IV methylprednisolone and close follow-up with neurology and vascular medicine for management of Takayasu arteritis.
A 56-year-old woman was diagnosed with Takayasu arteritis in 1991, initially treated with glucocorticoids for several years. Initial symptoms included constitutional symptoms and left-sided carotidynia. She had markedly elevated inflammatory markers and anemia at disease onset and later developed erythema nodosum. Imaging studies in the early phase of her illness revealed moderate stenosis of the right subclavian artery and marked thickening of the left common carotid. She was subsequently treated with methotrexate and cyclosporine, and eventually her disease went into remission. In 2014, MR angiogram of the chest showed radiographic evidence of vessel wall edema in the aorta, and at that time, the patient was started on mycophenolate mofetil. In November 2017 patient developed blurry vision and there was leakage on her fluorescein angiogram, felt to be nonspecific. She was taken off mycophenolate due to no evidence of active vasculitis on clinical or laboratory findings. She was in remission however required ascending aorta hemiarch repair, and aortic valve replacement (subsequently on warfarin) for dilated aortic root of 61 mm with histopathology showing healed arteritis. Two years later she developed a paracentral scotoma in the left eye and was diagnosed by outside Ophthalmology as branch retinal artery occlusion by retinal imaging, suspicious for embolic disease, in the context of subtherapeutic anticoagulation.
Clinical characteristics of patients with ocular manifestations and Takayasu’s arteritis have been reported to be similar to patients without ocular manifestations with a mean age in the 3rd decade of life and majority of Asian origin. Ocular manifestations of Takayasu arteritis can be seen in a wide range of 8.1-68% of the patients (1). Apart from two case based systematic reviews, current literature is lacking in describing extent of ocular involvement in Takayasu arteritis (1,3). Current classification of Takayasu arteritis does not include visual changes and consequently no ophthalmological examination is recommended even after diagnosis and ocular manifestations can go unnoticed.
A study by Pasko et al noted ocular manifestations presenting prior to diagnosis of Takayasu arteritis in 74.6% of the cases (3). This may be explained by cases where the initial manifestations include constitutional symptoms and are non-specific. Limitation of flow in the carotid artery results in chronic ischemia and hypoperfusion retinopathy and ocular ischemic syndrome may be of consequence (4). It remains imperative to distinguish and categorize the ocular disorder and pursue retinal angiogram.
A study from 1994 pointed at presence of Takayasu’s retinopathy as a statistically significant poor prognostic factor (5). Mirouse et al associated Takayasu retinopathy independently with mortality and complication free survival (6). Although medical management is the recommended initial management for Takayasu arteritis, patients who have vascular complications may require surgical interventions and endovascular procedures (7). Although information on ocular ischemia surgical management for Takayasu arteritis patients is limited, case series and case reports have demonstrated favorable results of balloon angioplasty and endovascular stenting in Takayasu retinopathy patients (1). Adopting routine fundus fluorescein angiography for surveillance in patients with Takayasu arteritis may be beneficial. Newer diagnostic techniques especially optical coherence tomography (OCT) angiography (OCTA) and novel diagnostics to assess retina perfusion must be investigated (1).
In young patients with visual loss and deficits it is imperative to recall Takayasu arteritis as a potential suspect even though such cases are few and far between because it can translate into meaningful difference in outcomes with proper management. Raising ophthalmological awareness and increasing education for pursuing comprehensive diagnostic testing is crucial.
Author Contributions
Conceptualization, SM, CW, AA; investigation, CW, SM.; writing—original draft preparation, SM. CW; writing—review and editing, SM, CW visualization, SM, CW, AA.; supervision, AA, FB; project administration, AA, FB. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study deemed exempt by the IRB at Mayo Clinic 1/31/24. IRB number 24-000157.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Zeng, Y.; Duan, J.; Ge, G.; Zhang, M. Therapeutic Management of Ocular Ischemia in Takayasu’s Arteritis: A Case-Based Systematic Review. Front. Immunol. 2022, 12, 791278. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Alvarez, C.; Crowson, C.S.; Koster, M.J.; Warrington, K.J. Prevalence of Takayasu Arteritis: A Population-based Study. J. Rheumatol. 2021, 48, 952–952. [Google Scholar] [CrossRef] [PubMed]
- Szydełko-Paśko, U.; Przeździecka-Dołyk, J.; Nowak, Ł.; Małyszczak, A.; Misiuk-Hojło, M. Ocular Manifestations of Takayasu’s Arteritis—A Case-Based Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 3745. [Google Scholar] [CrossRef] [PubMed]
- Guclu, H.; Gurlu, V.P.; Ozal, S.A.; Guclu, O. Central Retinal Artery Occlusion in Takayasu’s Arteritis as the First Presentation of the Disease. Case Rep. Ophthalmol. Med. 2016, 2016, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, K.; Maetani, S. Long-term outcome for 120 Japanese patients with Takayasu's disease. Clinical and statistical analyses of related prognostic factors. Circulation 1994, 90, 1855–1860. [Google Scholar] [CrossRef] [PubMed]
- Mirouse, A.; Biard, L.; Comarmond, C.; Lambert, M.; Mekinian, A.; Ferfar, Y.; Kahn, J.-E.; Benhamou, Y.; Chiche, L.; Koskas, F.; et al. Overall survival and mortality risk factors in Takayasu's arteritis: A multicenter study of 318 patients. J. Autoimmun. 2019, 96, 35–39. [Google Scholar] [CrossRef]
- Maz, M.; Chung, S.A.; Abril, A.; Langford, C.A.; Gorelik, M.; Guyatt, G.; Archer, A.M.; Conn, D.L.; Full, K.A.; Grayson, P.C.; et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Giant Cell Arteritis and Takayasu Arteritis. Arthritis Rheumatol. 2021, 73, 1349–1365. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).