1. Introduction
Interaction and collaboration between humans and robots in healthcare offers a promising solution to today's challenges in this field. Robots can help medical teams save time and effort while increasing efficiency and availability for patients, especially in repetitive tasks where they excel. Furthermore, human-robot collaboration is effective in improving the safety and quality of healthcare. The possibilities for using robotic systems to improve human-machine collaboration are endless. In fact, pilot projects around the world suggest that healthcare, among other sectors, will not be immune to the robot revolution [
1,
2]. Robot manufacturing has become a significant contributor to the field of healthcare technology, offering a diverse range of devices with applications in various areas of healthcare. Currently, around 40 percent of all robots used in healthcare are designed for rehabilitation and mobility [
3].
These robots assist patients physically or assess their condition to help them achieve their therapeutic goals. Additionally, surgical robots are becoming increasingly prevalent, providing instruments that can be controlled by surgeons via a console, allowing for less evasive and more precise surgical procedures [
3,
4].In the context of interventions on complex cancers, robotic systems guarantee highly precise and efficient operations, resulting in less discomfort for patients and a reduced risk of postoperative complications. Furthermore, robot-assisted surgery is demonstrating its ability to lighten the workload of healthcare teams, saving time and resources while improving efficiency and availability for patient care [
4]. As healthcare gets better, robots are getting smarter [
3]. They can now do things like help people using artificial intelligence and look more human. In addition to the use of AI in these robots, there are other key ideas to improve healthcare, including AI-enabled services, cutting-edge AI systems, blockchain technology, digital well-being services, and pandemic-specific healthcare management systems [
5]. The adoption of such ideas raises questions such as how much it will cost to implement these systems, how they will affect healthcare professionals, and how to ensure they remain safe and private [
1].
Another very important issue that has been overlooked is ensuring that AI systems are aligned with ethical principles and human values. This helps avoid negative consequences like violence, discrimination, and harmful decisions that could affect humans and the environment. If not implemented correctly, AI could perpetuate social injustices, amplify inequalities, and operate in ways that are contrary to fundamental human interests. It's therefore essential to develop and implement accurate and robust ethical guidelines for AI, ensuring that it serves the well-being of societies as a whole [
6].
This article is organized as follows: Section II explains how we surveyed the literature and reviewed academic studies on using robots in hospitals. It also looks at future uses for robots in healthcare, recent research, and how it will affect the future of robot integration in hospitals and beyond. Section III explains how robots are used in healthcare. It also looks at the different areas of healthcare where robots are used, the benefits of integrating robots into hospitals, and the logistics needed for robots to operate in each hospital. In Section IV, we look at how robots are used in hospitals. We look at the main types of robots and give examples of how they are used. We also look at the technical details and the pros and cons of these robots. Section V looks at how robots will affect hospitals in the future. Section VI looks at the problems, challenges, and implications of robotic systems and the associated emerging technologies. Finally, Section VII concludes the discussion of this article.
2. Methodology for Literature Review
In this review article, we have used the following methodology for our research:
Initial search: An extensive search of prominent databases was conducted, including IEEE Xplore, ACM Digital Library, ScienceDirect, ResearchGate, Google Scholar, Web of Science, and Scopus. Keywords related to "robotics", "artificial intelligence", "healthcare", and "hospital" were used.
Inclusion criteria: The research papers selected were those deemed most relevant to the central themes of this article, namely the application of robotics in the hospital domain, future prospects for the use of robotic systems in healthcare, and emerging and relevant technologies in the context of improving healthcare quality.
To ensure that the information was up-to-date, articles published from 2015 onwards were prioritized. However, some seminal works and fundamental studies were also included, regardless of the date of publication. This approach allows for greater coverage of the subject matter, as some publications remain highly relevant despite the date of publication. The following papers were excluded from the review on the grounds of meeting the exclusion criteria:
Papers that did not address the application of robotics in the hospital domain;
Papers that were not related to future prospects for the use of robotic systems in healthcare and emerging and relevant technologies in the context;
Papers that had not been peer-reviewed.
Given the inherent limitations of the healthcare domain, we endeavored to assess the quality of each potential source by evaluating the depth of the analysis, the methodological rigor, and the contribution to the field. To ensure that only impactful and high-quality studies were included in our review, we employed a rigorous process of study selection.
Cross-referencing was employed to ensure the inclusion of only the most relevant studies. To expand the scope of our literature review, we also examined the references of the articles analyzed, as well as those of the selected articles, to identify any additional relevant contributions that could enhance the value of our work.
The articles included ensure a balanced mix of theoretical research, practical case studies, and academic analyses, providing a comprehensive perspective on the topic.
3. Robotics in Healthcare: An Overview
3.1. The Impact of Robotics in Healthcare
According to Yang et al. 2020, the COVID-19 pandemic has accelerated the need for technological innovation in several areas in recent years. This underlines the urgency of finding effective solutions to global challenges. In particular, the acceleration of robotics has ushered in a new era of possibilities. During the pandemic, robotics was instrumental in minimising human contact and reducing the spread of the virus, with applications ranging from disinfection robots to automated hospital assistants [
7].
In Shishehgar et al. 2018 study, the rapid adoption of robotics in response to the global pandemic of COVID-19 has highlighted the potential of this technology to reshape many sectors. The advent of robotic technology, encompassing automated vehicles and factory assistants, is transforming a multitude of industries.
It's estimated that around 20% of the global population is affected by health problems. Robotics could be a great way to help bridge the gap in healthcare [
8]. And it's not just surgery and rehab that robotics is transforming. Automation and robotics are also changing the way we do things in emerging industries like telemedicine and remote monitoring [
9], as well as helping with personal care tasks [
10], and even areas not directly related to clinical practice, like transporting medications and medical supplies. These autonomous robots can navigate aisles and deliver critical items like medications, biological samples, and medical equipment quickly and accurately [
11].
The integration of robots into healthcare teams addresses two significant challenges: the need to care for an ageing population and the shortage of qualified healthcare professionals. Furthermore, it offers personalized care for diverse needs. The integration of research and industry is a crucial aspect of healthcare. The development and implementation of robotic technologies have the potential to significantly transform the delivery of care, improving both the efficiency and quality of care [
12].
3.2. Applications across Medical Fields
Robotic systems alleviate pressure in various industries, particularly in the healthcare sector by streamlining tasks, from virtual consultations to equipment delivery [
13]. Hospitals can implement various types of robotic systems; these systems can improve efficiency and reduce the risk of human error [
4]. Robotics has a multitude of applications in the medical field:
Robotic surgery: is a surgical procedure in which a robot is used to assist the surgeon. Surgical robots are used in complex surgical procedures, offering enhanced precision and control, such as laparoscopic surgery, cardiac surgery, and neurosurgery [
14].
Robotic Rehabilitation: a variety of robotic devices are employed in the rehabilitation of patients with neurological or musculoskeletal injuries. These devices facilitate movement and promote recovery [
15];
Telemedicine and Remote Monitoring: robots can be employed to facilitate remote medical consultations, patient monitoring, and remote assistance in cases of remote accessibility or emergencies [
9];
Transportation: robotic systems are used for the autonomous delivery of medicines, biological samples, and medical supplies inside hospitals, a process that optimizes logistics and reduces human error [
11];
Diagnosis and Imaging: robotics and AI technology can be used in diagnostic imaging equipment, such as computerized tomography (CT) and magnetic resonance imaging (MRI), to automate processes and enhance diagnostic accuracy [
16];
Surgeon Assistance: in addition to robotic surgery, robots are employed to assist surgeons during complex procedures, such as holding instruments or providing enhanced vision assistance [
14].
The examples presented are illustrative of the current applications of robotics in medicine within the hospital context. As technology evolves, it is anticipated that innovative applications will emerge to enhance the efficiency and quality of healthcare [
17].
Despite the significant investment in the development of surgical and rehabilitation robots, there remains a great need for further research and innovation in emerging areas such as cleaning and disinfection in medical environments [
1], medical diagnosis and imaging, assisting in the operating room, etc. It is also necessary to improve the adaptability of robots operating in these environments, enabling them to seamlessly integrate with diverse medical settings and respond effectively to changing circumstances. Furthermore, enhancing HRI through the development of dynamic algorithms is crucial, as it can facilitate smarter actions and significantly improve the overall efficiency of healthcare delivery. Research in healthcare robotics is advancing rapidly and is exploring new technological frontiers. This development highlights the need for innovative and robust solutions that can support different medical contexts [
1,
18,
19,
20].
3.3. Revolutionising Hospital Logistics
Looking ahead, robotics will continue to play an important role in digital transformation, particularly in healthcare, and it's also clear that the integration of robots in healthcare will become more profound [
21]. Robots will need to collaborate by working together on several tasks ranging from surgical procedures to disinfection and patient care [
22,
23,
24]. Robots are becoming increasingly sophisticated and adaptable, providing innovative solutions to meet new challenges in healthcare [
21,
25]. Multidisciplinary collaboration, however, will be the key to a promising future for medical robotics [
24].
The adoption of new technologies, such as the integration of artificial intelligence systems into robotics is resulting in safer surgical procedures and shorter hospital stays [
26]. Furthermore, autonomous robotic systems are playing a pivotal role in the logistics and transport of materials within hospitals, revolutionizing the way supplies are managed and delivered. By denying access to certain areas and delivering supplies autonomously, these systems are not only improving operational efficiency but also enhancing patient safety and reducing the risk of contamination [
27]. The TUG autonomous mobile robot developed by Aethon is a good example of mobile robots in healthcare. TUG helps healthcare professionals in hospitals and other medical facilities. It is a small, self-driving robot that can move around hospitals and do different tasks, like carrying things like medicine, samples, supplies, and bedding [
28], these systems enhance efficiency and reduce the likelihood of errors [
27]. Another example is the portable UVC disinfection system, Tru-D. It uses UV light to disinfect surfaces better than chemical/mechanical methods, especially in places where chemical disinfectants don't work. It can disinfect a room, including shadowed areas. Sensor360 technology ensures the UVC dose is accurate, even in shaded areas, increasing the effectiveness of disinfection [
29]. Telepresence robots enable specialists to conduct remote consultations, expanding access to quality healthcare [
27]. Additionally, therapeutic robots such as the social assistive robot (SAR), like PARO can offer emotional support to patients, particularly those with dementia, revolutionizing care delivery in hospitals and communities and improving patient well-being [
30]. In summary, robotic systems are revolutionizing healthcare delivery, offering tailored assistance, improving efficiency, and enhancing patient outcomes across various medical fields [
27,
30].
4. Types of Robotic Systems in Hospitals
4.1. Transportation and Logistics
In the hospital environment, the problem of transport and logistics, in general, relates to the efficient movement of goods and resources such as medical supplies, equipment, laboratory samples, non-medical materials, and patients. This challenge is critical in the sense that any delay or error in the delivery of these items can have serious consequences for the treatment and, consequently, the recovery of patients [
31,
32]. In addition to the above, there are the following challenges associated with logistics in the hospital sector:
Inventory Management: Hospitals can improve efficiency, reduce costs, and increase quality by involving external organizations in the provision of internal services. This can include outsourcing logistics to specialized companies to guarantee the availability of supplies [
33].
Tracking and tracing: RFID technology can be used to track and trace assets and inventory in hospitals. It can also be used to plan routes and optimize storage and distribution processes [
34].
Transport coordination: Health information systems can facilitate the efficient movement of supplies between different areas of the hospital. This ensures the timely and accurate delivery of supplies, thus enhancing the overall efficiency of the hospital [
35].
Waste and chemical products logistics: The implementation of a specific inventory model for pharmaceutical products and derivatives can assist in the effective management of medical waste and chemical products utilized, thereby ensuring compliance with environmental and safety regulations [
36].
Patient transport: The use of advanced internal transport management and control systems in hospitals can help ensure that patients are transported safely and efficiently between units, thus minimizing waiting times and the risks associated with transport [
37].
To overcome these challenges, we must improve how different departments work together and make sure the logistics processes is as efficient as possible considering the implications of security and privacy [
38,
39].
The integration of Autonomous Mobile Robots (AMRs) into hospital environments is becoming more common, but there are many challenges associated with the implementation of these systems [
40]:
Vehicle routing problem (VRP): Problem in optimize AMR routes to serve locations efficiently. Then a solution is creating a pathfinder algorithm that adapt to changes in the hospital layout [
40].
Stochastic problems: Dealing with things like how long the trip will take is difficult because the weather can affect it. One way to deal with this is to use models that consider how things like the weather can change [
40].
Pathfinding: Problem finding the shortest route between two locations in a hospital. One solution is to develop algorithms that adapt to changes in the hospital layout [
41].
Conflict Resolution: Problem in minimizing collisions or delays based on routing solutions to ensure safe and efficient operation of AMRs. So, one solution is to use real-time collision avoidance algorithms and coordination of multiple robots [
42].
Fleet Management: It is difficult to decide how many vehicles a hospital needs, to link AMRs with existing hospital systems and to know how much material to transport. AMRs must not stop medical procedures or patient movement, while keeping hygiene and safety in areas where infection is a risk [
43].
Hygiene and Safety: The problem is that we can't guarantee critical medical procedures and the movement of patients, while maintaining hygiene and safety in environments where there is a risk of infection. The solution is to develop strict hygiene protocols and routes that don't disrupt hospital flow [
44].
Uncertainty and Variability: The hospital is facing challenges with patient arrivals and medical tasks. The solution is to use predictive machine learning to adjust operations to meet demand [
45].
Robust Optimization: It is difficult to develop data-driven approaches to deal with uncertainty in data. The solution uses robust optimization and data analysis to create solutions that can cope with changes [
45].
Real-time Recalculation: Problem with real-time route calculations due to temporary obstructions or changes in the environment. The solution is to use adaptive navigation systems that can recalculate routes instantly [
46].
Integration with Existing Systems: AMRs need to be integrated with existing hospital management systems to avoid impeding critical medical procedures and patient movement. The solution is to develop APIs and interfaces that allow AMRs to be integrated with existing hospital systems [
47].
Furthermore, the necessity to guarantee that AMRs do not impede critical medical procedures and the movement of patients introduces an additional layer of complexity to logistics planning [
43]. In addition, the development and popularity of supplies using intelligent express boxes and the use of methods such as the Open Vehicle Routing Problem (OVRP) in relation to the classic VRP problem, means that vehicles do not have to return to the depot, which allows a significant reduction in delivery times but also guarantees the safety of distribution in the event of a risk of infection [
48]. However, several methodologies have been proposed, such as Open-Loop Distribution, Open-Loop and Closed-Loop Distribution, and Multi-objective Solutions. Among these, Open-Loop it is considered the best approach for the distribution problem and carbon emission cost. There are still aspects to be improved in logistic distribution optimization, as well as solving problems of uncertainty such as customer returns and exchanges [
49].
4.1.1. Main Robotic Transport Systems
Robotic transport systems using wheeled robots are highly efficient and cost-effective in certain environments, such as hospitals, where they can increase operational efficiency by performing routine transport tasks. However, their inability to climb stairs and negotiate significant height changes limits their use to areas with consistent levels and floors. By integrating lift systems and considering hybrid robot designs, these limitations can be mitigated, extending the potential applications of wheeled robots [
50]. For example, some hospitals, such as St. Olav's Hospital in Trondheim, Norway, use AGVs to efficiently transport goods around the hospital campus, optimizing logistics operations and reducing labor costs [
51]. The use of transport and logistics robots in hospitals, particularly for tasks such as the autonomous movement of goods, has shown significant success. These robots, known as AGVs, not only increase operational efficiency, but also open new possibilities for human-robot interaction thanks to their design to promote autonomy and accessibility [
51].
The features of hospital robots include load capacity, operational autonomy, precision in navigating hospital corridors and integration with hospital systems for managing materials and supplies. The ability to operate in complex, high-demand environments such as hospitals is an important differentiator for these robots. Among the advantages of these robots are the ability to operate continuously, without the need for breaks, the precision and consistency of delivery of sensitive materials, and the reduced risk of contamination and cross-infection since they minimize human contact. They can also free operators from repetitive tasks so that they can focus solely on direct patient care [
52,
53]. However, there are advantages and disadvantages to be considered, such as the high initial cost of implementation, the need for specialized training, and the adaptation of hospital infrastructures to accommodate the new technology.
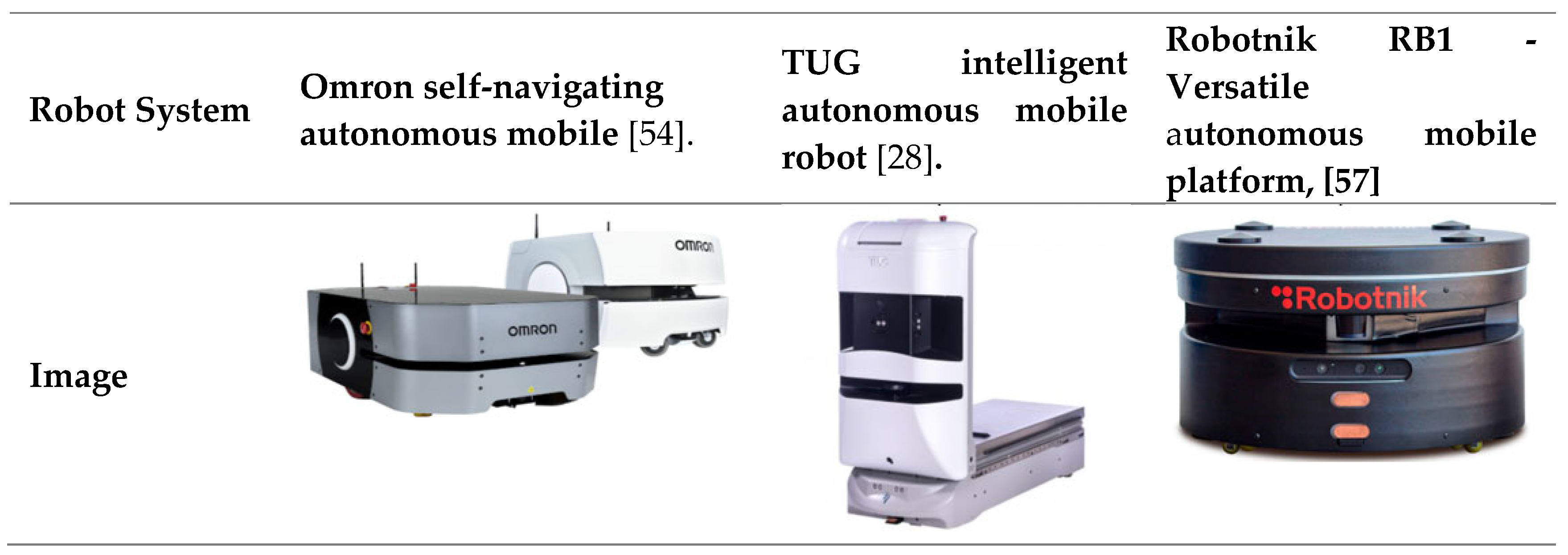
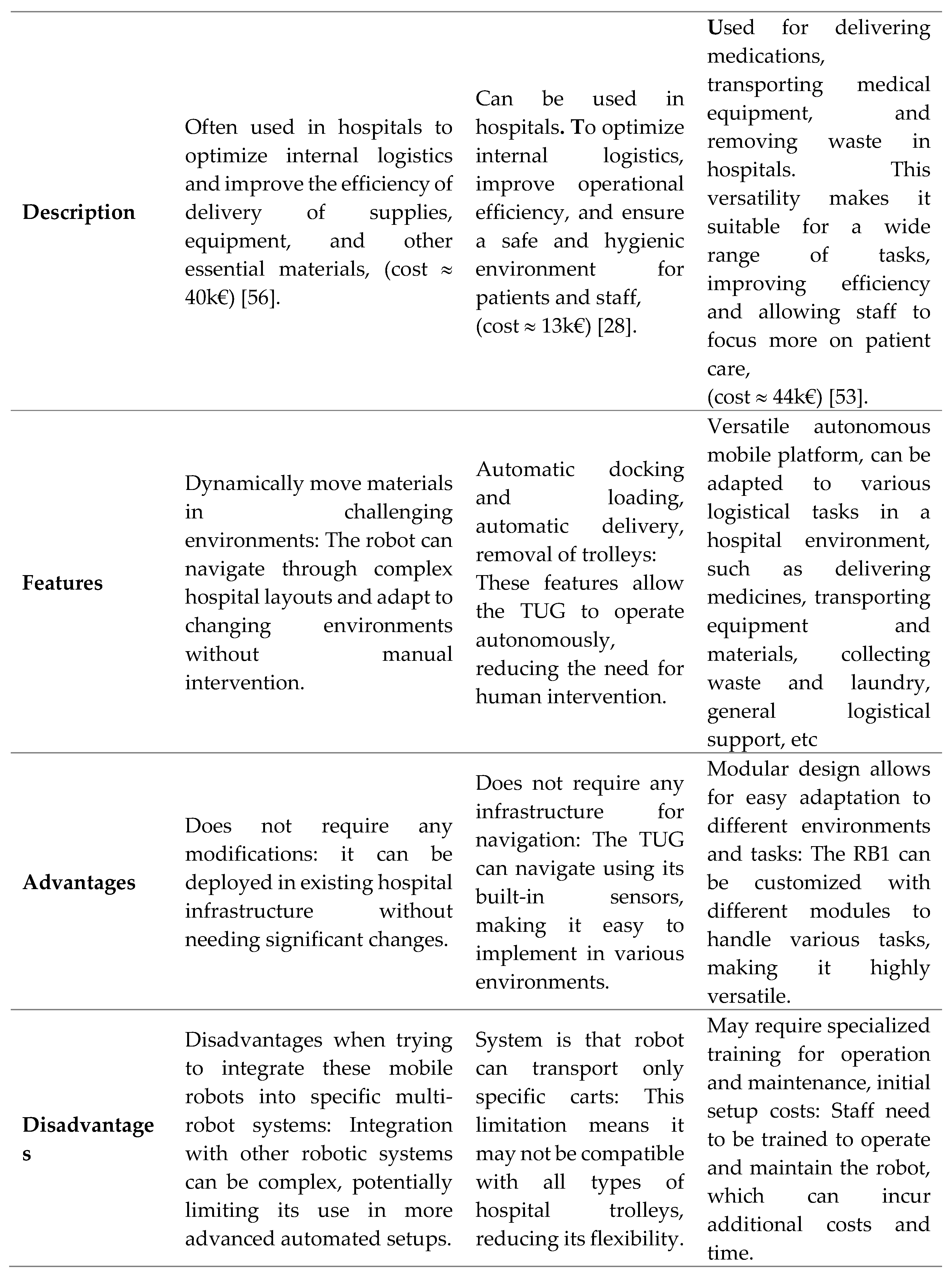
Table 1 provides a comprehensive overview of the robots employed in logistics and transport systems [
54,
55].
4.1.2. Quadruped Robots
Initially developed for military purposes, quadruped robots have since emerged as a multifaceted solution in hospital environments. From telepresence to surveillance in hazardous areas to inspection of sensitive products, these robots have been employed in a variety of vital ways in hospitals [
60]. One noteworthy example is the Boston Dynamics Spot Quadruped, which has been designed to navigate complex terrain in a timely and secure manner, thus enabling the reliable automation of critical inspection and data collection tasks [
61]. Furthermore, companies such as DEEP Robotics, responsible for the X30, are investigating new applications, including potential uses in emergency rescue and fire detection, including in hospital environments [
62]. These initiatives significantly expand the scope of robotic intervention, providing critical safety and emergency solutions within hospitals. Despite the advantages of quadruped robots, there are challenges associated with them, including energy efficiency [
39]. Nevertheless, their principal advantage lies in their capacity to operate in environments devoid of lifts, rendering them invaluable in emergency situations, such as power cuts, where they can ascend stairs and transport objects and patients with ease, thereby providing vital support at critical times within the hospital environment. It should be noted that this quadruped robots system places greater emphasis on the applications and benefits of quadruped robots in hospitals, with particular focus on their importance in security scenarios [
63].
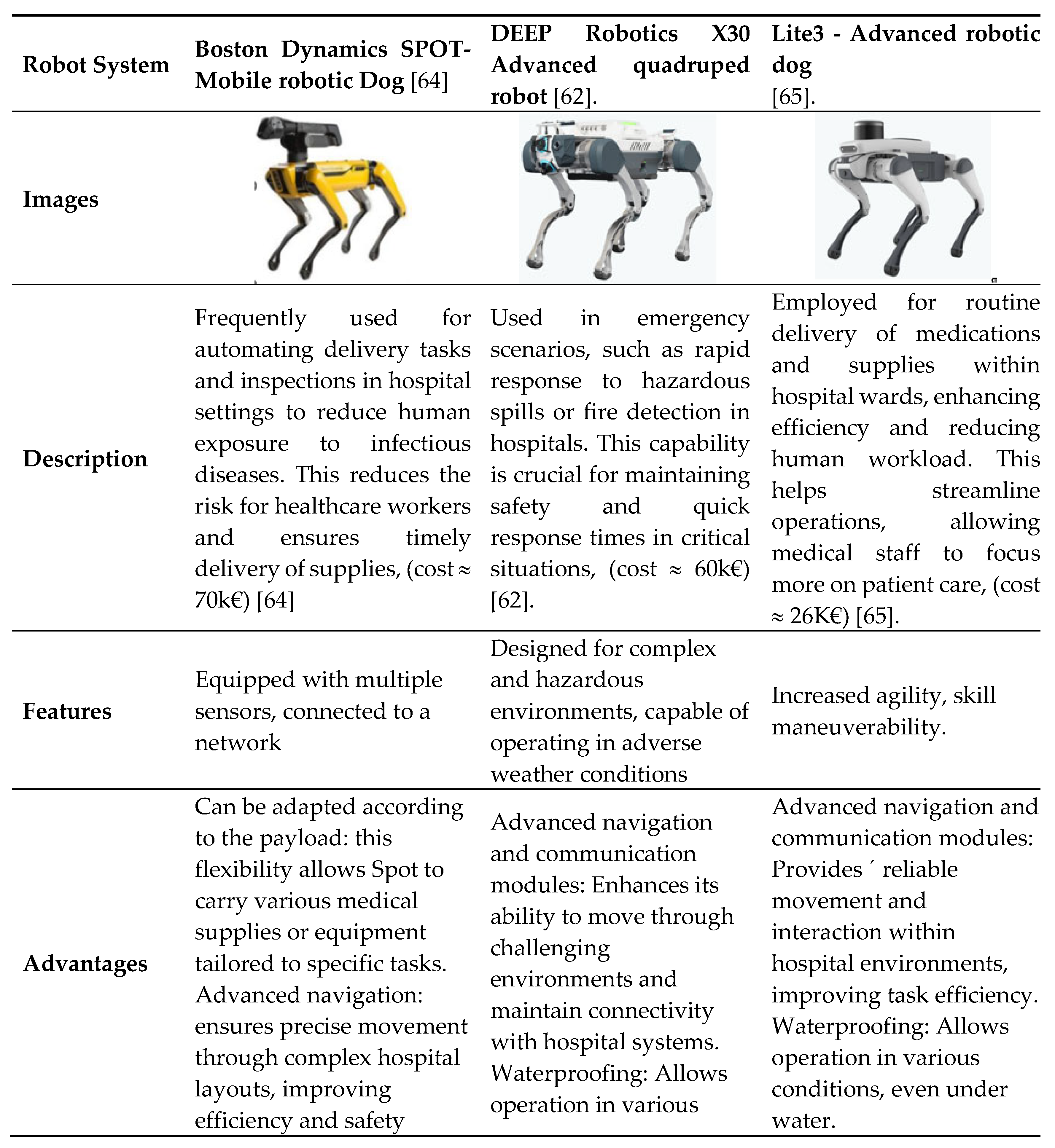
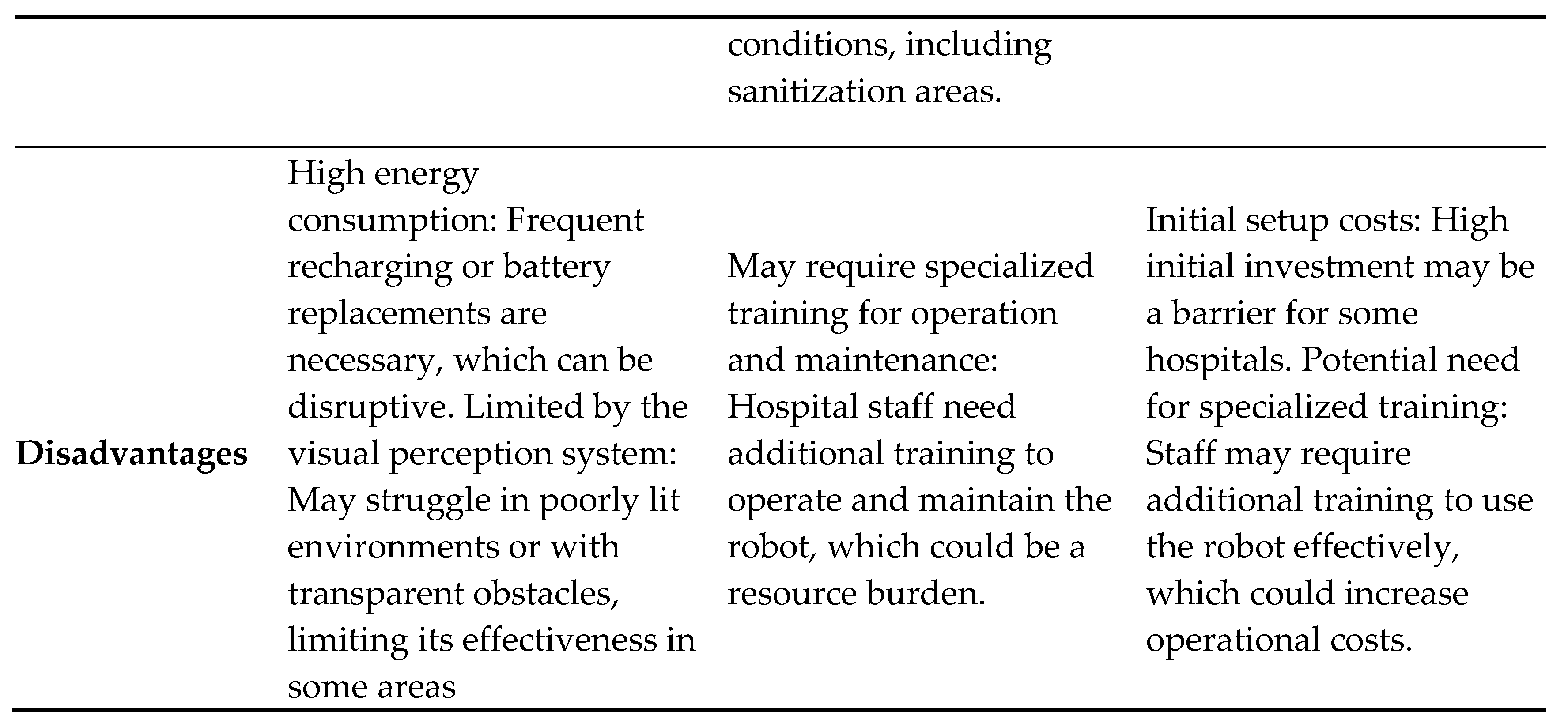
Table 2 presents a comprehensive analysis of the distinctive characteristics, advantages, and disadvantages of various quadruped robots. Each quadruped robot is designed with its own unique specifications, rendering them suitable for a variety of applications in hospital environments and beyond [
64,
65].
4.2. Cleaning and Disinfection
Cleaning and disinfection in hospital environments is a critical and complex challenge that directly impacts patient safety and the operational efficiency of healthcare institutions. Hospitals are places where infection prevention is of paramount importance, as the presence of pathogens can lead to nosocomial infections (hospital-acquired infections), which represent a significant risk to patient health. However, there are several challenges associated with this problem, which can be described as follow [
66,
67,
68,
69]:
High microbial load: Hospitals are environments where the concentration of pathogens is high due to the presence of patients with various infectious diseases. Surfaces, medical equipment and even the air can become a breeding ground for pathogens [
67].
Variety of Pathogens: Hospitals are home to a wide variety of micro-organisms, including bacteria, viruses, fungi and protozoa. In addition, some can be multi-drug resistant, making them even more difficult to control [
67].
Complex environments: In hospitals, there are different areas with specific cleaning and disinfection requirements, such as operating theatres, intensive care units (ICU), patient rooms and common areas, which require customized cleaning and disinfection procedures [
68].
Cleaning and disinfecting procedures: Effective cleaning and disinfection involves rigorous, standardized procedures, including mechanical cleaning, chemical disinfection, and sterilization [
66,
68].
Suitable Products and Technologies: The choice of cleaning and disinfection products is critical. Products must be effective against pathogens, safe for occupants and not damage surfaces and equipment. New technologies such as ultraviolet (UV) light and hydrogen peroxide fogging systems are also being used to complement traditional methods [
67,
68].
Training and awareness: The effectiveness of cleaning and disinfection depends on the proper training of healthcare professionals and cleaning teams. They need to be aware of the protocols, the correct use of chemical products and the importance of hand hygiene to prevent the spread of infections [
66,
67,
68].
Continuous monitoring and assessment: Quality control of cleaning and disinfection requires constant monitoring and periodic evaluation. The use of appropriate tools such as microbiological analysis of surfaces and regular audits help to ensure that hygiene standards are maintained [
66,
68].
The problem of cleaning and disinfection in hospital environments is complex and multifaceted, requiring an integrated approach that combines strict protocols and ongoing training [
66,
67,
68].
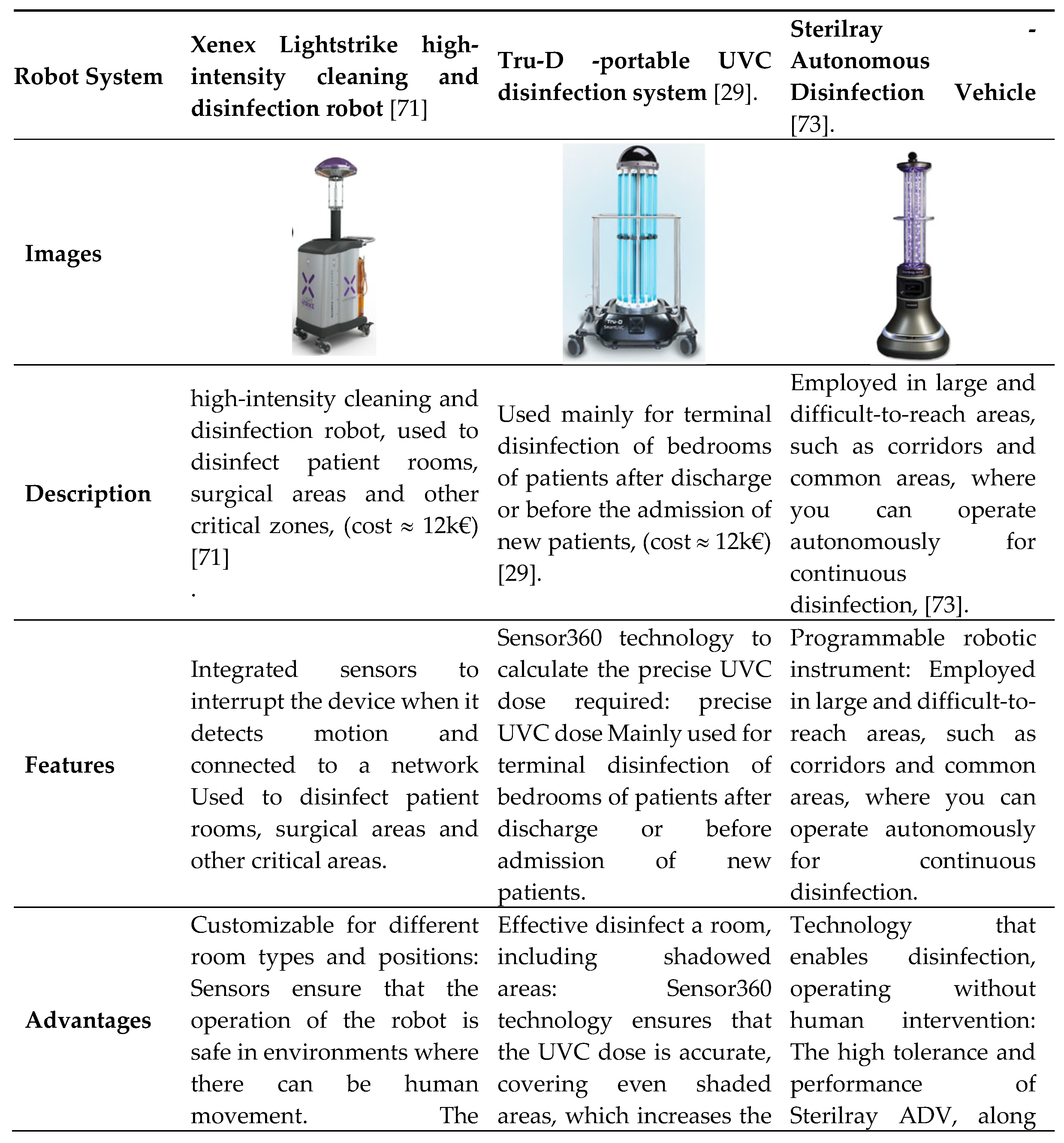
4.2.1. Cleaning and disinfection robot systems
Many ultraviolet (UV) germicidal systems are available, incorporating specific technological advances. However, the effectiveness and operational status of traditional UV germicidal irradiation (UVGI) systems and robots require continuous improvement [
70].
These robots are widely used in hospital environments for disinfection according to standard procedures and play a crucial role in reducing nosocomial infections [
70]. Due to the risks associated with exposure to UV light, it is essential to optimize these robots to ensure safety in areas occupied by patients and healthcare professionals. Although safe operation in the presence of humans requires further research, the use of UVGIs is expected to increase significantly in the post-pandemic era. This growth will require more advanced designs for effective and safe disinfection, making hospital environments healthier and more resistant to pathogens [
70].
Cleaning and disinfection robots have become essential tools for maintaining safe and sanitized hospital environments, especially in the post-pandemic era, where efficient disinfection is vital for preventing nosocomial infections [
71,
72].
Table 3 provides a comprehensive overview of the robots used in cleaning and disinfection systems, comparing them in terms of characteristics, advantages and disadvantages.
In comparison to traditional manual disinfection methods, robotic cleaning and disinfection systems present a promising alternative for the disinfection of critical areas, including hospital waiting rooms [
4]. Nevertheless, it is of paramount importance to enhance research on pathogen inactivation, particularly in hospital settings, where environmental resistance can present a significant obstacle. For instance, the efficacy of ultraviolet C (UV-C) irradiation cycles for standard disinfection may be diminished in instances of elevated microbial load or resilient pathogens, such as Candida auris. This underscores the necessity for the development of more resilient strategies to ensure patient safety [
75].
4.3. Socially and Assistive
There are a number of challenges that affect both patients and healthcare professionals when providing care in a hospital environment. These challenges can be grouped into the following main categories [
76,
77,
78]:
Work Overload and Staff Shortages: A significant proportion of hospitals are confronted with a high demand for patients, coupled with a shortage of healthcare professionals, which results in an underload of work. This can result in significant fatigue and burnout among operators [
79].
Resource management: The management of resources, including medical equipment, hospital beds and consumables, can present significant challenges. The unavailability of resources or the misallocation of resources can result in delays in the delivery of essential treatments and procedures [
80].
Patient safety: The management of patients is a constant concern, with the potential for hospital-acquired infections, medical errors and falls [
81].
Infrastructure and technology: A significant proportion of hospitals continue to operate with infrastructures and technologies that are no longer fit for purpose [
82].
Patient Satisfaction and Experience: It is of the utmost importance to enhance the patient experience, yet this can prove challenging when attempting to reconcile it with operational efficiency. Long waiting times, a lack of privacy and communication all contribute to patient dissatisfaction [
83,
84].
Regulation and compliance: Hospitals are required to adhere to a multitude of regulations and compliance standards, which can be intricate and disagreeable. Ensuring compliance while maintaining quality is a persistent challenge [
85].
Costs and Financing: The effective financial management of hospitals is of paramount importance, particularly in the context of rising costs and budgetary constraints [
86].
To address these issues, it is often necessary to adopt a multifaceted approach that incorporates technological innovation, enhanced management practices, ongoing training of healthcare professionals, and the implementation of effective policies and quality standards [
87,
88].
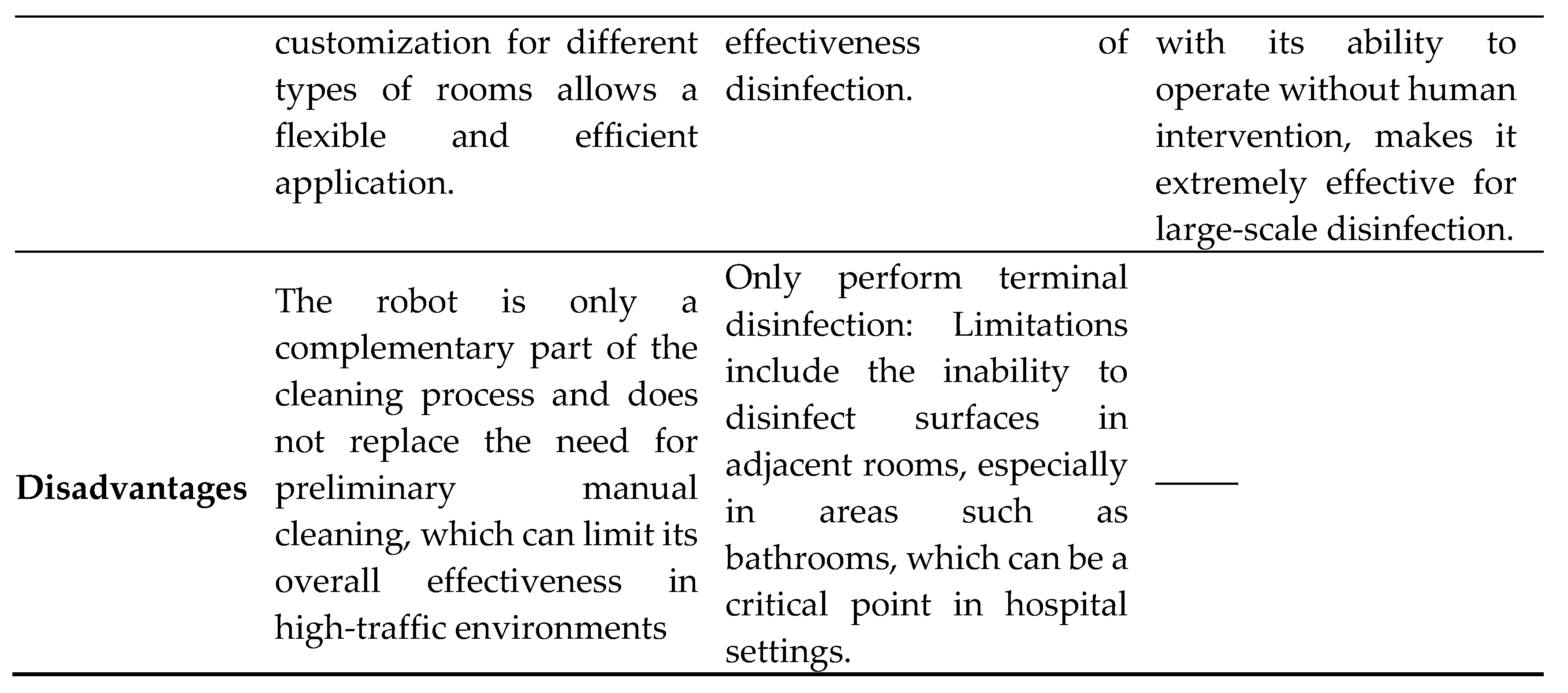
4.3.1. Socially Assistive Robot Systems
Socially Assistive Robots (SARs) can take various forms, such as humanoids or animals, and aid in areas traditionally performed by humans, such as companionship and service provision [
4]. In the healthcare context, for SAR-mediated treatment to be effective, it is essential that the patient trusts both the operator and the robotic system [
10].
A good example of trust in a SAR system is the PARO robot, which is used significantly more often in affective therapy sessions than other systems in the same category, such as NAO. While PARO is used in 9 affective therapy sessions, NAO and AIBO are used in only 1 and 0 sessions respectively [
89]. This trust is a significant predictor of treatment adherence, satisfaction with treatment, and continuity of care. Trust in the patient-therapist relationship is positively correlated with rehabilitation and treatment outcomes, including pain reduction, improvement in disability, physical and mental health, and satisfaction with treatment. It is therefore crucial to prioritize building trust in the therapeutic relationship, particularly as new technologies such as social assistive robotics (SARs) are integrated into standard care [
10].
Table 4 provides a comprehensive overview of the assistive robots used in hospital settings, comparing them in terms of characteristics, advantages, and disadvantages. This comparison includes various robots like PARO, NAO, and AIBO, highlighting their unique features and their impact on patient care [
89,
90]. These robots are shown in Figure 4.
4.4. Telemedicine and Telepresence
Telemedicine and telepresence are technological innovations that have the potential to transform healthcare delivery in remote hospital environments. This includes remote consultations, patient monitoring, health education and even therapeutic interventions delivered via electronic devices and virtual communication. However, there are challenges to the implementation and integration of these technologies, such as [
96,
97,
98]:
Privacy and Data Security: As in other areas, data protection is a crucial requirement, and telemedicine is no exception. This involves the transmission of sensitive information about patients' medical data. The challenge lies in ensuring that this data is protected against unauthorized access [
96,
98].
Care quality: The quality of care is related to the diagnosis (accurate diagnosis), which must be precise because the accuracy of the diagnosis can be affected by the variable quality of the images and videos transmitted. Remote assessment can lead to inaccurate diagnostic results. Conversely, telepresence can result in a sense of distance between the patient and the doctor, which may negatively impact the quality of the doctor-patient interaction, which is a crucial aspect of effective care [
97].
Health standardization and policy: The absence of standardization in the services associated with telemedicine can result in inconsistencies in the quality of healthcare [
96,
99].
Both telemedicine and telepresence have the potential to revolutionize care in the hospital setting, providing access to quality care in an efficient manner. However, in order to achieve this potential, it is necessary to address comprehensively the challenges related to privacy, quality of care, and regulation, in addition to the other challenges already mentioned. By addressing these challenges, healthcare systems can leverage the advantages of these cutting-edge technologies [
96,
97,
98,
99].
4.4.1. Telemedicine
The utilization of telemedicine has expanded in tandem with technological advancement, driven not only by technological advancements themselves, but also by the growing necessity to expand access to healthcare.
Telemedicine encompasses a diverse range of clinical activities, including motor and cognitive assessments, as well as medical consultations. It is particularly beneficial in remote areas and for patients with reduced mobility [
97,
100]. Several models and procedures have been developed to guide the use of telemedicine, offering an up-to-date framework for its implementation. These models have the potential to enhance public health outcomes and can be adapted for scientific studies or future health emergencies. Furthermore, the advent of electronic and mobile technology has rendered telemedicine accessible and useful in a multitude of medical contexts [
97,
100].
To further maximize the benefits of telemedicine, the integration of AI is a promising solution. The implementation of AI-based telemedicine requires dynamic protocols and the use of innovative AI algorithms based on data modelling. These algorithms can apply machine learning to large datasets of disease populations, providing effective and personalized solutions to complex healthcare problems [
101]. AI models allow direct learning from data, avoiding the need for prior statistical modelling. This approach produces more objective results, with a focus on generalizing predictions for diagnostic purposes across different populations [
102]. Data derived from computational approaches can be used to test synergistic combinations of variables and eliminate redundant resources, facilitating more effective diagnosis. It is crucial to recognize that data entry methods are extremely important, as speech recognition and interpretation is a significant challenge in the use of AI [
101]. On the other hand, robotic telemedicine is a promising cutting-edge tool in telemedicine, with the potential to transform physical examination and clinical care, and to facilitate remote patient monitoring [
103]. The resilience of health systems has enabled more efficient use of health technologies, including the use of robotic systems and Internet of Things (IoT) devices. These technologies have been fundamental to the delivery of medical services, such as the creation of smart hospitals that minimize exposure risks and improve the quality of care [
101].
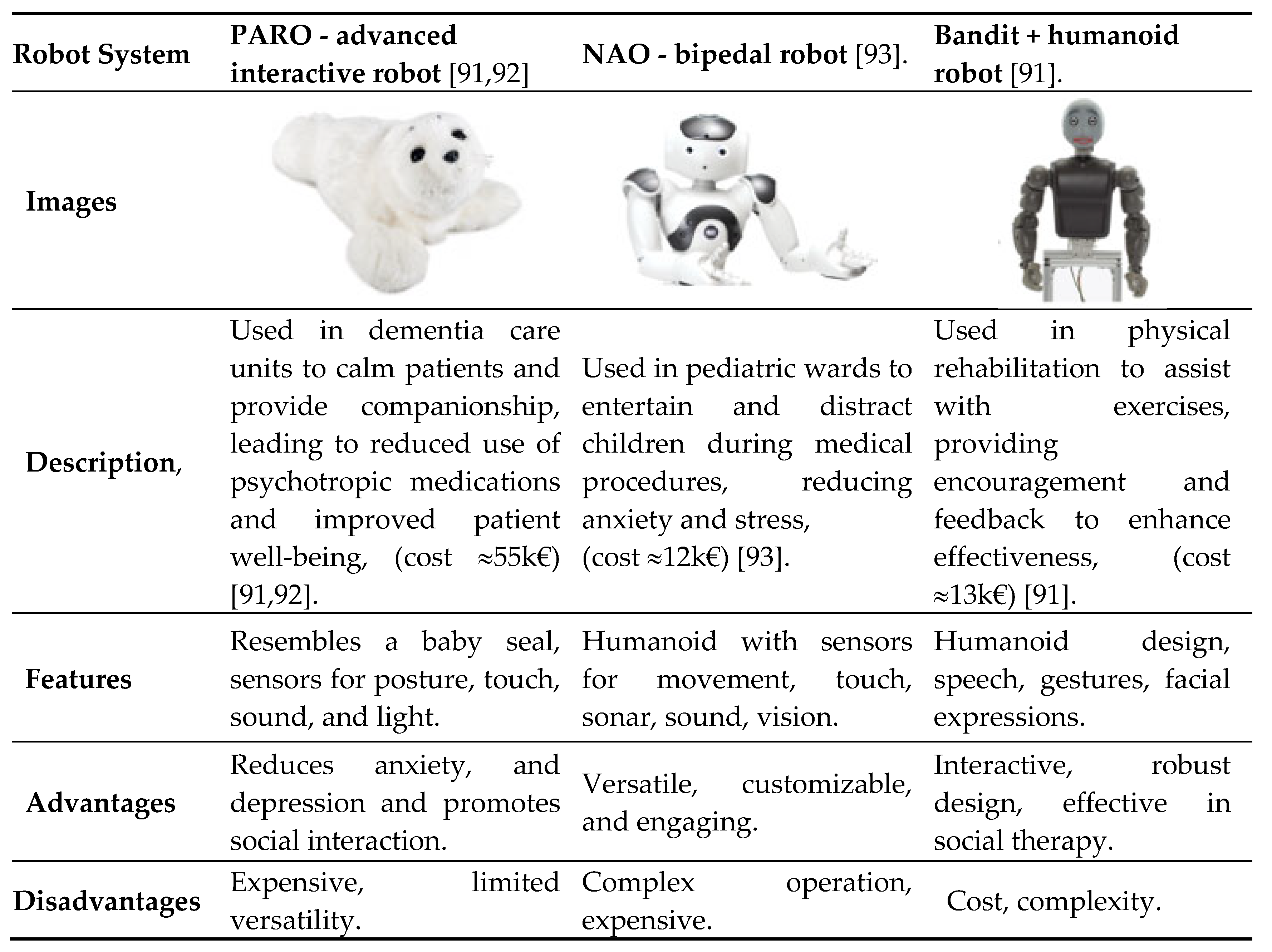
4.4.2. Telepresence
The advent of telepresence systems has brought to the fore several challenges currently being faced by healthcare systems and medical personnel across the globe.
In this context, robotic-assisted tele diagnosis has emerged as a potential solution, allowing specialist doctors to examine patients remotely. The World Health Organization (WHO) has predicted that the global population of people aged 60 and over will increase from 605 million to 2 million between 2000 and 2025. This will result in a doubling of the percentage from approximately 11% to 22%. This suggests that telepresence may be a viable alternative to address the increased demand for healthcare in the elderly population [
100,
104].
Table 6 Gives a more comprehensive overview of telepresence robots, including examples of practical use, advantages and disadvantages associated with each telepresence robot system. This can help readers to better understand the clinical and practical implications of these robotic systems in healthcare [
105] - [
106].
Telepresence robots may be a viable solution, as some systems can perform simple tasks such as taking patients' vital signs, which could ease the workload of healthcare professionals and carers. There are already several telepresence robotic systems on the market today, including commercial products such as Double Robot, GoBe, and Giraff (
Table 6.), based on social robotic telepresence functionality [
108].
4.4.3. Smarter Telepresence
The future of telepresence technology is likely to be characterized by the convergence of three-dimensional telepresence technology, virtual and augmented reality techniques, and robotics. This will result in the creation of fully interactive and immersive experiences, in which the distinction between the real and the virtual will become almost imperceptible.
There is a need to improve existing methods and algorithms for 3D face generation, in particular audio-based 3D speaker algorithms, as well as the possibility of their implementation in Virtual Reality, Augmented Reality (AR) and Mixed Reality (MR) systems [
109]. The implementation of the speaking face will be an essential component in future telepresence conferencing systems [
110].
4.5. Surgery and Rehabilitation
Surgery and rehabilitation are complex processes that affect the human body in different ways. In terms of surgery, these surgical challenges manifest themselves in the following ways:
Invasive procedure: Surgery involves making an incision in the body to correct a medical problem. This can cause pain, trauma and bleeding [
111,
112];
Risks and complications: All surgery carries risks such as infection, excessive bleeding and reaction to anesthesia. In some cases, these can lead to serious complications that can cause permanent disability or even death [
113].
Recovery time: Recovery from surgery can be long and arduous. The patient may need to stay in the hospital for several days or weeks, and even then, full recovery may take months. During this time, the patient may experience pain, weakness and tiredness [
114].
As regards rehabilitation, these challenges manifest themselves as follows ways:
Long and challenging process: Rehabilitation aims to help patients regain function and strength after surgery or injury. This may involve physiotherapy, occupational therapy, speech therapy and other interventions. The process can be long and challenging and requires increased effort from the patient [
115].
Pain and discomfort: Rehabilitation can cause pain and discomfort as patients work on their muscle strength and range of motion [
116].
Motivation and support: It is important for the patient to be motivated and to have the support of family, friends, and health care professionals during the rehabilitation process [
116].
It's important to stress that both surgery and rehabilitation are important parts of the treatment of many medical conditions. However, it is important to be aware of the challenges that these processes can present. Preparing for surgery and rehabilitation, and getting support from healthcare professionals and family members, can increase the chances of a successful recovery [
117,
118].
4.5.1. Surgical Robots
Robotic surgery is a significant application of robotics in the field of medicine [
16], robotic systems are used to assist in surgical procedures, including minimally invasive surgery. These systems have been developed to overcome the limitations of traditional surgical methods [
119]. Robotic-assisted surgery (RAS) technologies, such as the da Vinci Surgical System, have rapidly evolved in recent years. They aim to improve surgical precision, dexterity, and access to minimally invasive procedures. Additionally, augmented reality (AR) provides an advanced interface to enhance user perception [
119].
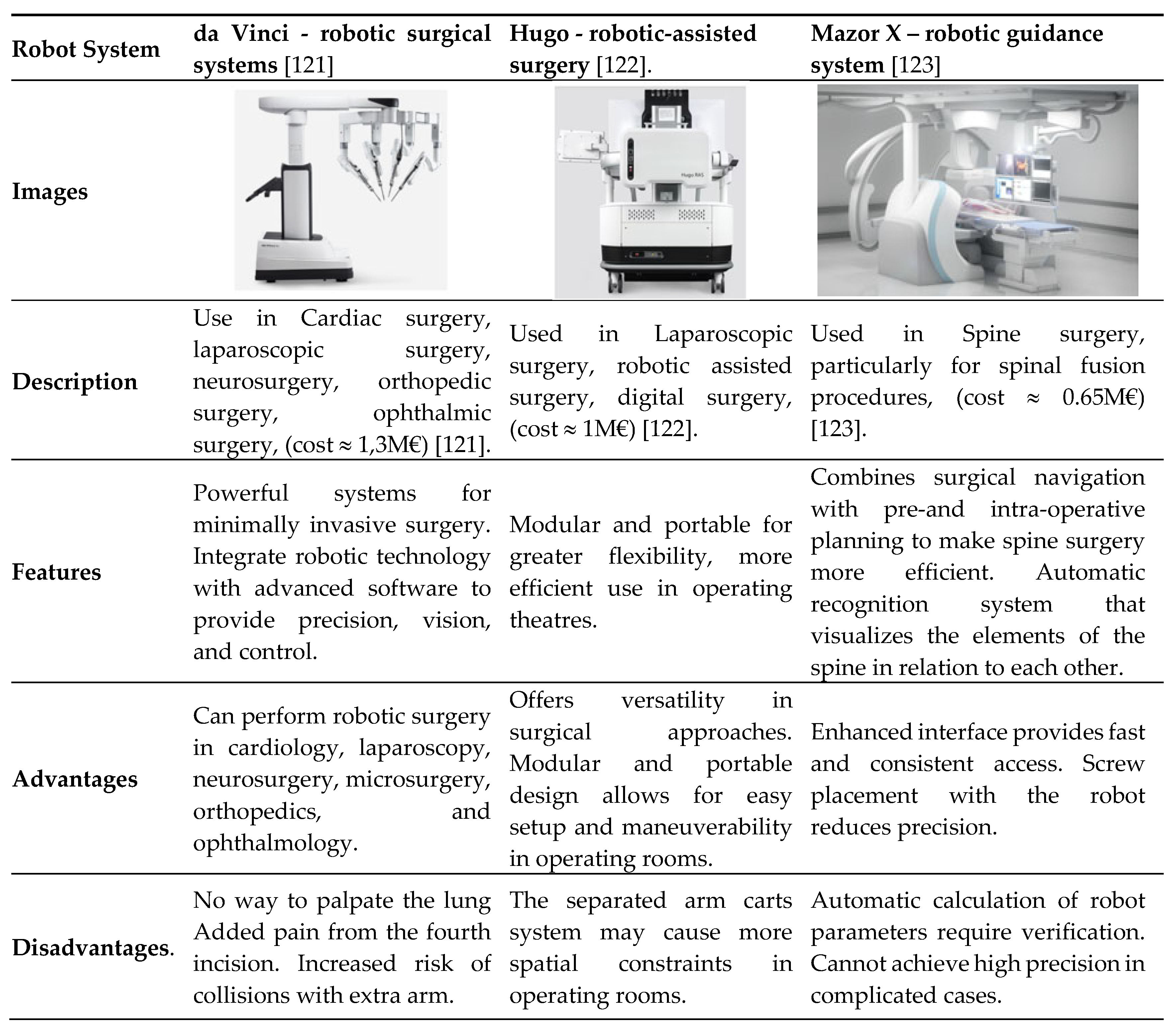
Today, different robotic surgical systems have been developed, Cepolina et al. 2022, as well as a comparative analysis of these systems, considering their space requirements in the operating theatre, accessibility to the patient, efficiency and intuitiveness of the presentation of the surgical scenario, modularity and reconfigurability of the system, miniaturization of the surgical instrument, haptic or force feedback, certification status and availability for purchase [
120]. Some robotic systems, such as da Vinci, Hugo, and Mazor X, stood out from the rest for their effectiveness in providing the surgeon with an intuitive representation of the surgical scenario, receiving a very good (VG) rating [
120].
Table 7 summarizes the main surgical robotic systems in the hospital environment, as well as use cases, technical characteristics, advantages and disadvantages, to provide a more comprehensive overview of surgical robotic systems in the hospital environment.
The da Vinci surgical system developed by Intuitive Surgical integrates state-of-the-art robotic technology with cutting-edge software to provide precision, improved vision, and control during surgical procedures [
124]. With more than 5,500 units installed worldwide by 2020 and more than seven million surgeries performed, da Vinci systems have been instrumental in numerous specialties, including cardiology, laparoscopy, neurosurgery, microsurgery, orthopedics’ and ophthalmology [
120].This technology has revolutionized modern surgical practice and has become indispensable in advanced medical centers around the world.
4.5.2. Autonomous Robotic Surgery
Despite the advances in robotic surgery over the last two decades, the control of the robotic system is currently still under the command of a human surgeon. There is a need to promote greater autonomy in these robotic systems - from assisted robotic surgery to autonomous robotic surgery [
127]. The prospects for autonomous robotic surgery are many and can bring benefits to robotic surgery, for example, standardization of techniques will lead to less variation in clinical outcomes. Automated processing of sensory information can lead to greater precision and fewer errors associated with stress and fatigue [
127]. In addition, the use of new techniques such as machine learning models can analyze pre- and intra-operative information to predict and ensure that the robot does not damage sensitive tissues and nerves when operating autonomously [
128].
However, there are also challenges associated with autonomous surgery, including ethical, legal, patient safety and privacy issues, as well as additional costs associated with the use of autonomous robotic surgery (ARS). It is difficult to introduce ARS as a new standard for surgical procedures without solid evidence of significant cost effectiveness and improved outcomes compared to standard surgical techniques, due to the high costs associated with current healthcare systems [
128].
Although there are currently some concerns about autonomy in medical robotics, the future is still promising, and more and more research is progressing towards total autonomy [
128]. Furthermore, liability issues can be addressed by extending the current regulatory framework, and much research and development is underway to provide more precise guidelines [
127,
128]. Still about liability, and self-operating mechanisms in the event of an emergency or system failure, these systems can be crucial in avoiding complications in interventions or even the death of the patient; a good example of this is the Smart Tissue Autonomous Robot (STAR) [
129]. The advanced autonomous approach allows the operator to choose from a variety of autonomously generated surgical plans, and the robot performs a wide range of tasks independently. The results of the study's simulated model show that the autonomous system outperformed the manual techniques of experienced surgeons and RAS techniques in terms of consistency and precision [
129].
In addition, ref. O'Sullivan et al. 2019 pointed out that AI systems could be crucial in medical robotics. For example, a ‘flight recorder’ could be implemented to record all data and assist in failure analysis, allowing surgeons to better understand and reconstruct the causes of the robot's failure behaviour. These improvements would increase confidence in the system [
130]. However, the increasing independence of robots is inevitable, making medical processes more autonomous and the role of the human being more focused on supervision.
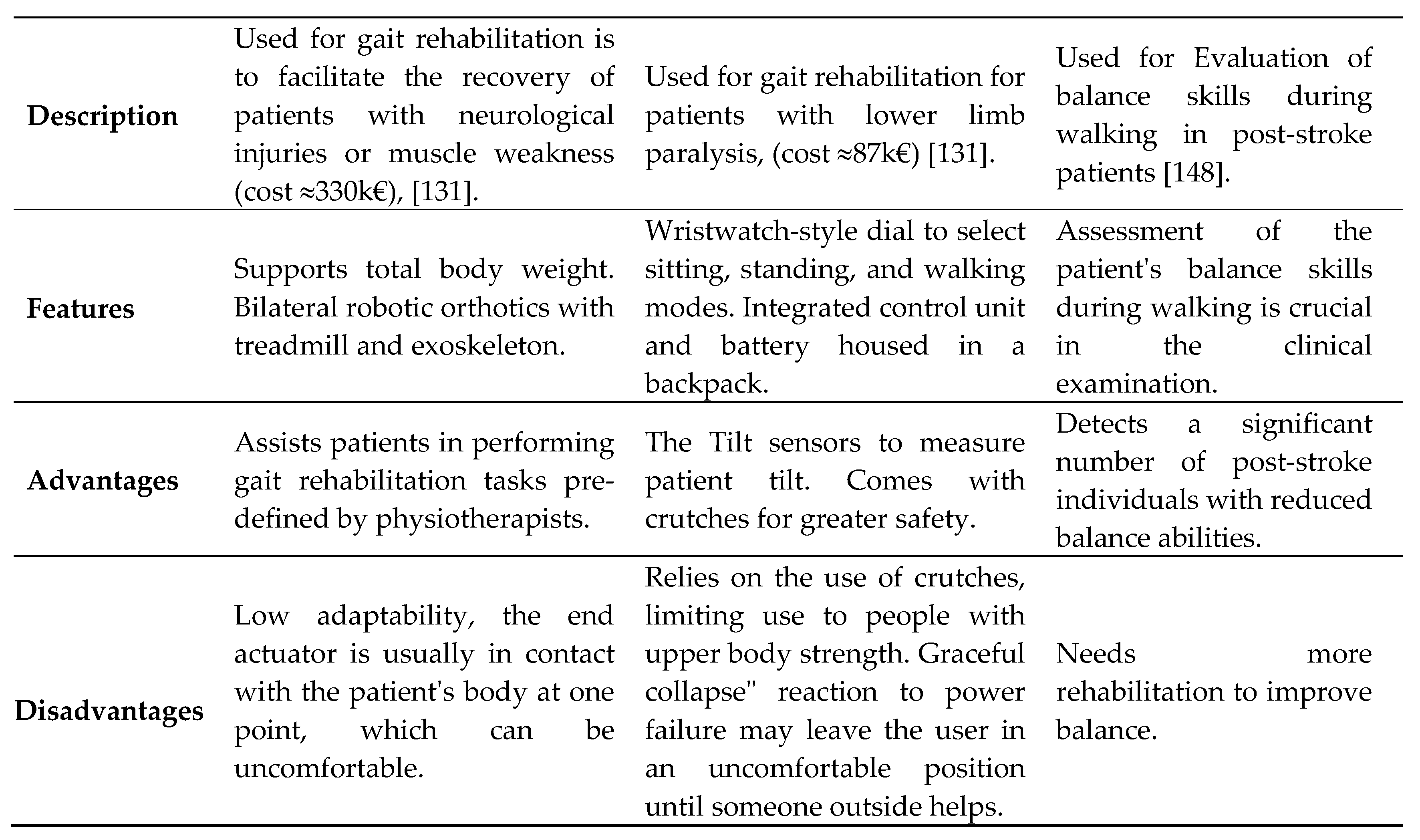
4.5.3. Rehabilitation Robots
Rehabilitation robots are specially designed machines that help people with physical disabilities during their recovery process. These robots are particularly beneficial for individuals dealing with conditions like stroke, multiple sclerosis (MS), traumatic brain injury (TBI), spinal cord injuries (SCI), and Spina bifida (SB) [
131,
132,
133].
In the case of spinal cord injuries, where individuals may face challenges with upper and lower body movements, rehabilitation robots address specific needs. Lower limb rehabilitation robots target leg movements, helping with walking and balance, while upper limb robots focus on arm and hand rehabilitation, helping with tasks such as reaching and grasping objects [
134]. Overall, rehabilitation robots play a crucial role in individualizing recovery programs designed by physiotherapists. By targeting specific areas of impairment, thus these robots can play an important role in aiding patients in regaining their natural motor skills and promoting overall well-being [
135].
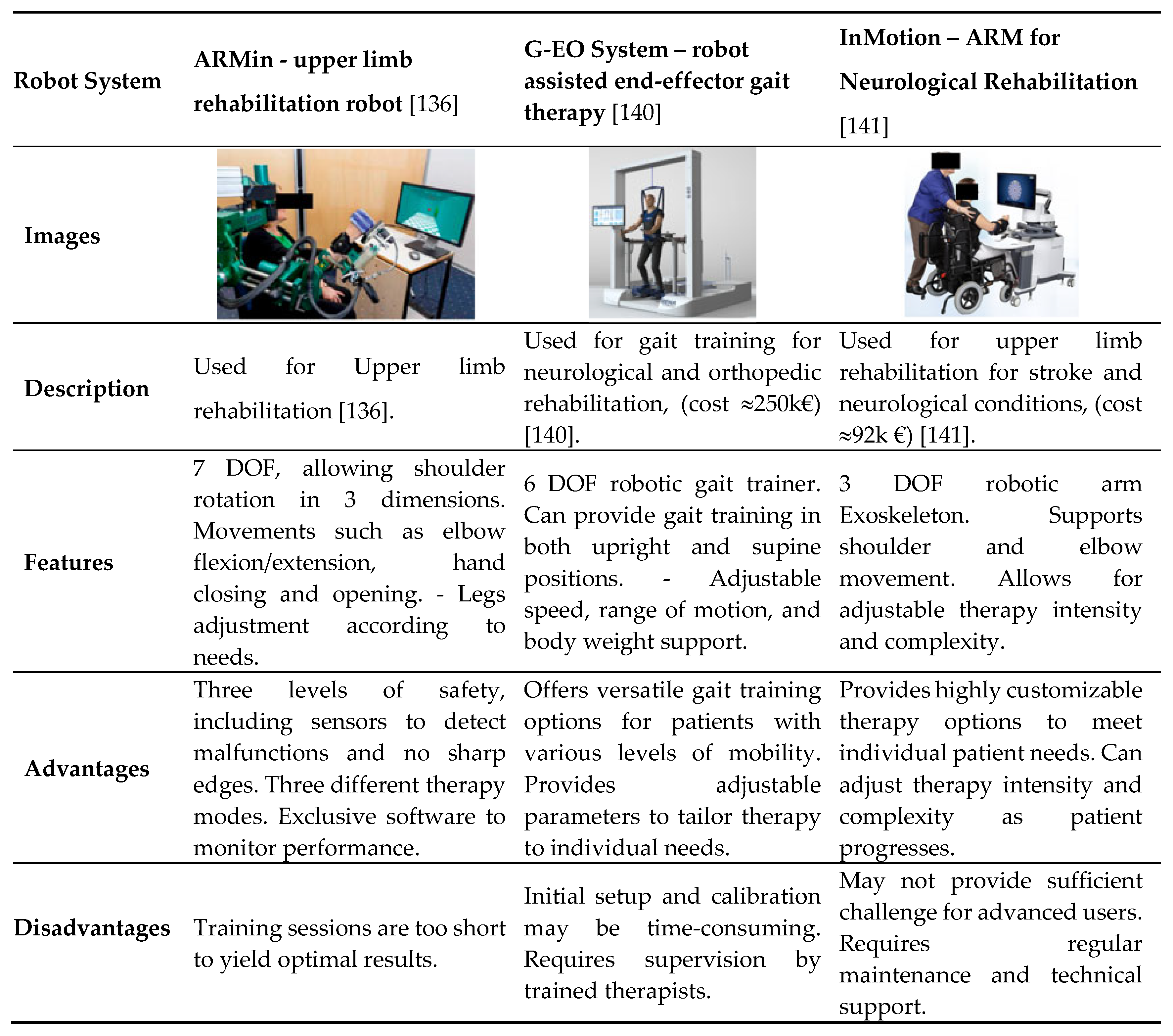
Upper limb rehabilitation
Upper limb rehabilitation involves the use of robotic systems to target specific joints and movements of the shoulder, arm, forearm, hand, and fingers to aid in recovery and regain functionality. Examples of the upper limb rehabilitation robotic system, like ARMin [
136], G-EO System [
137], and InMotion [
138].
Table 8 It shows a summary of the main systems for upper limb rehabilitation in the hospital environment, from which we can get a more comprehensive view through practical cases where each of these systems is used, comparing their technical characteristics, advantages and disadvantages of each of these systems [
136,
137,
138,
139].
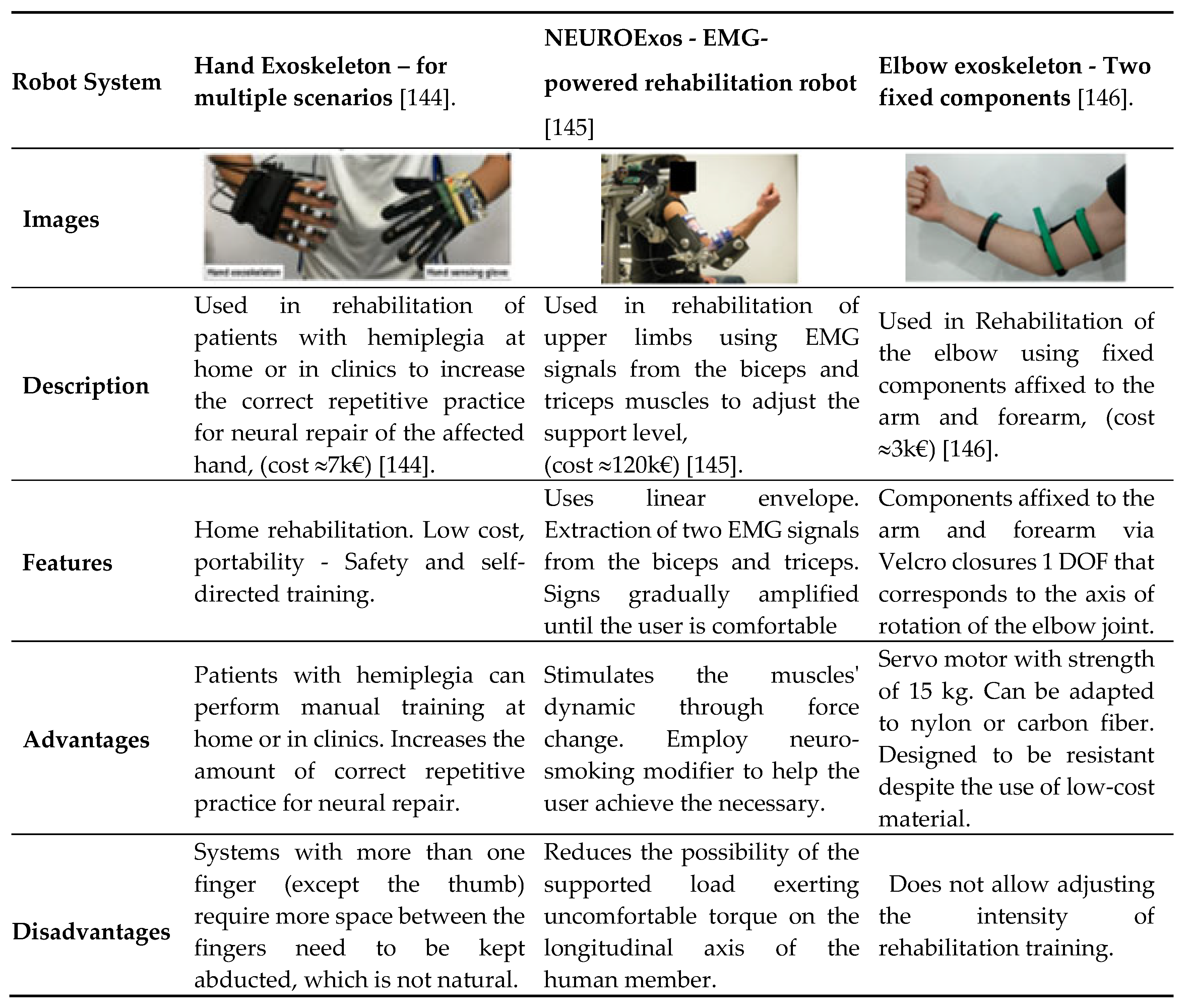
EMG-Driven Exoskeleton Robots
For the purposes of robotic rehabilitation, it is essential that the extraction of an electromyographic (EMG) signal is both efficient and accurate. Two methods of obtaining the EMG signal are available: invasive, which involves an intramuscular electromyograph (iEMG) injection, and non-invasive, which involves the use of a surface electromyograph (sEMG). It is crucial to acknowledge that the utilization of invasive techniques necessitates the administration of an intramuscular injection [
136].
In the invasive technique, the electrodes are placed on the motor units of the muscle, while in the non-invasive technique the non-invasive technique, the electrodes are placed in the abdominal region of the muscle where the maximum contraction [
136,
142]. Although iEMGs provide accurate EMG signals, sEMGs are often used because they are more acceptable to the patient and do not require an invasive procedure [
136,
143]. The following examples illustrate the use of EMG-driven upper limb robots and the associated control methods. These are based on the input signal, the resources used and the controller mechanism [
136].
Table 9 provides a summary of the principal systems for EMG-driven exoskeleton robots in the hospital environment. It offers a more comprehensive view of these systems through practical cases in which each system is used, comparing their technical characteristics, advantages and disadvantages.
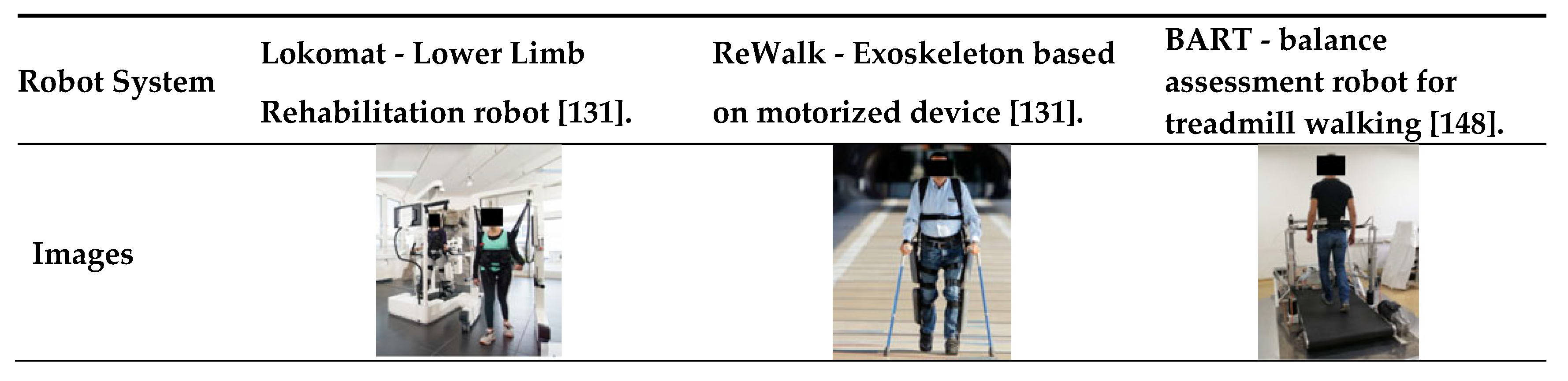
Lower Limb rehabilitation
It is important to note that Lower Limb Rehabilitation (LLR) exoskeletons are just one type of LLR. LLRs, such as exoskeletons, have been developed over the years to aid in the recovery of lower limb function. A review of various LLR robots from 1999 to 2017 was conducted by Hobbs et al. 2020, in a recent study [
131,
147]. Several systems with a high degree of maturity have been proposed and are already available on the market, such as, Lokomat, ReWalk, and BART. These systems incorporate technological advances in developing LLR systems, bases, and exoskeletons. It is important to note that this information is based on recent studies [
131].
Table 10 provides a summary of the principal systems for Lower Limb rehabilitation robots in the hospital environment. It offers a more comprehensive view of these systems through practical cases in which each system is used, comparing their technical characteristics, advantages and disadvantages [
131,
132,
133,
134,
135,
136,
137,
138,
139,
140,
141,
142,
143,
144,
145,
146,
147,
148]
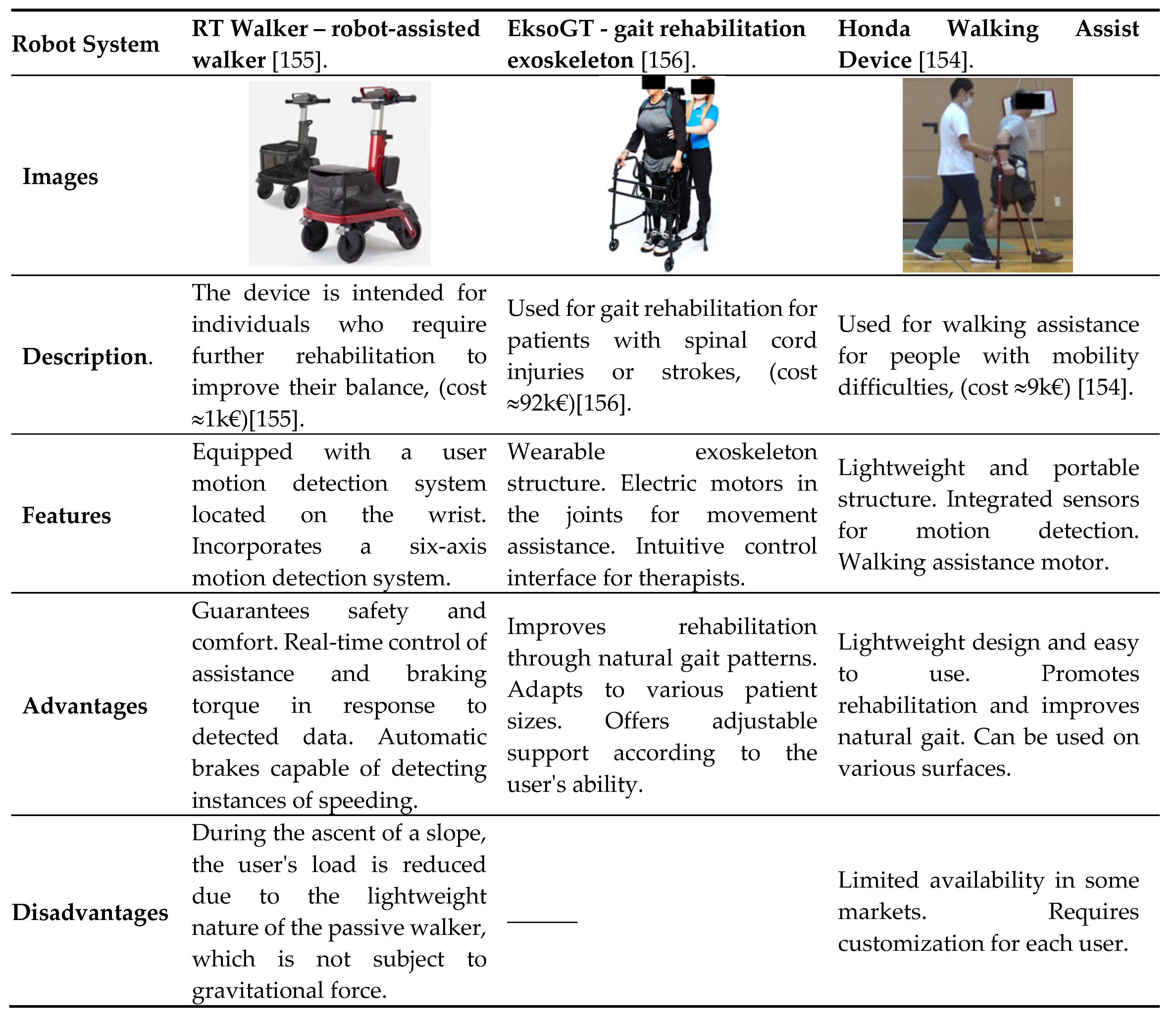
Walking Assisting Robots
The utilization of different types of walking assistants is contingent upon the level of disability. For instance, individuals with total paralysis resulting from spinal cord or traumatic brain injuries may benefit from utilizing a smart wheelchair [
150]. Although there are various types of walking assistants available, a new category has been introduced for intelligent walking assistants. These robots are designed to assist individuals with moderate upper and lower body strength, as well as patients in hospitals who require support for daily ambulation and walking exercises [
151].
Standard the Intelligent walking assistants (IWA) functionalities include obstacle avoidance and guidance, user intent prediction, user gait estimation, user speed estimation, and fall detection and prevention. Cane Walking Assistants (CWA) are like a walking stick and their relatively small size makes them easy to use both indoors and outdoors. Although small, the CWA provides the necessary stability for people who are confident enough in their gait to require little or no assistance [
152].
The authors, Di et al. 2016, propose an intelligent cane robot that includes an omnidirectional base, a universal joint that connects the cane to the base, a laser rangefinder (LRF) sensor, a force-torque (FT) sensor, and a touch panel. They also propose a fall detection and prevention system that uses a load sensor in the insole that users wear inside their shoes. The combination of load sensor data, LRF and FT sensor data, acoustic sensors, Charge Coupled Device (CCD), localization cameras and RGB depth cameras can enable the robot to perform these activities and provide an impedance-based fall prevention controller [
131,
152].
A multitude of methodologies and techniques have been proposed for the purpose of assisting individuals with walking difficulties. These include approaches for regulating the user's gait to control the robot's movement. Additionally, there are proposals for the incorporation of safety features, such as fall detection and prevention, as well as obstacle avoidance [
152].
Table 11 provides a summary of the principal systems for Walking Assisting Robots in the hospital environment. It offers a more comprehensive view of these systems through practical cases in which each system is used, comparing their technical characteristics, advantages and disadvantages [
153,
154].
One of the key advantages of intelligent walking robot rehabilitation systems, such as the cane robot, is that they can actively assist users in maintaining balance. In the case of the elderly, although they may still be able to use a conventional cane, in the event of a fall, they will be unable to move the cane in time to prevent the fall. The cane robot is capable of being controlled to move to an optimal position to help the user maintain balance using fall detection and prevention algorithms [
152,
157]. However, the fall detection procedure utilizing a vision-based method required 500 ms, whereas the time taken for fall detection by monitoring the movement of the center of gravity (COG) was 400 ms [
158].
New methods can detect the risk of falling much faster, thus preventing accidents. For example, the A center of pressure (COP)-based fall detection (COP-FD) method can be used to prevent slipped, tripped, or crossed legs. In addition, the Leg-Motion-Based Fall Detection (LM-FD) method can be employed to accentuate leg movement, thereby reducing the detection time by approximately 80% (to within 50 ms) [
152].
5. Future Directions and Emerging Technologies
The future of healthcare remains unclear, although there are indications of potential future developments. One emerging trend is the growing importance of digital healthcare, driven by the need for digital solutions in this domain. In this context, several ambitious proposals have been put forward, including the concept of a Metaverse for healthcare, which is also related to the Internet of Medical Things (IoMT) [
151,
152].
The Metaverse approach to healthcare makes use of the most advanced technologies that can be employed in the context of digital health, including AI, robotics, quantum computing, IoT, and muti-robot systems. These systems, when integrated with advanced automation and decision-making tools, can transform the way medical services are delivered [
4,
124]. In terms of characteristics, Metaverse for healthcare should be a highly secure, efficient and professional ecosystem of medical and healthcare services, based on the Metaverse, with attributes of knowledge, socialization, digitalization and intelligent perspectives [
151,
152]. In addition, visualization and teleoperation can enable complex medical procedures to be carried out remotely, improving access to and the quality of healthcare. However, for these technologies to be effective, it is necessary to develop new, robust, reliable and secure solutions that can be used in cybernetic design [
4]. Furthermore, these solutions must be sustainable and easy to implement [
152]. The collaboration of all interested parties, including industry, regulators, professionals, users, legislators and governments, is essential for creating the necessary infrastructures that will allow these approaches to be implemented in our society [
4]. Examples of sectors where this collaboration is already in place include the automotive, aviation and special exploitation sectors, where many of the technologies mentioned above are already integrated into procedures and structures, forming part.
For example, in the automotive sector, the use of AI, advanced systems and robotics are already part of the ecosystem in this field, such as AI-empowered industrial robots (InRos), based on a model that takes advantage of technology, organizational structure and environment, this paper examines the adoption of InRos in Auto Component Manufacturing Companies (ACMCs) in the context of an emerging economy [
162]. Another illustration of the integration of AI and advanced robotic systems into the domain of space exploration is the elucidation of the mental processes of individuals on board and the facilitation of human-robot collaboration [
163]. Space robotics, in conjunction with AI, is currently employed in space programs to construct, repair and maintain satellites and space structures in orbit [
164].
In the aviation industry, there is a plethora of applications in aviation management that assist airlines in enhancing efficiency, reducing costs and improving customer satisfaction. These applications employ technologies associated with AI, ML and DL, as well as advanced robotic systems [
165]. Nevertheless, as robotics and AI have already been integrated into other domains and numerous applications are already functioning autonomously, it is similarly necessary for this technology to be incorporated into healthcare [
4].
In healthcare, automation can improve the accuracy and efficiency of medical procedures, while multi-robot systems can collaborate in hospital environments to carry out complex tasks. AI-assisted decision-making can support doctors in choosing the best treatments, and virtualization and teleoperation can enable the remote execution of surgeries and other critical procedures. Integrating these emerging technologies into hospitals will not only improve the quality of care but will also increase patient safety and reduce operating costs. To achieve this, it is essential to develop robust, reliable, and secure solutions by promoting collaboration between industry, regulators, professionals, users, legislators and governments. This collaborative approach can create the necessary conditions for the implementation of these technologies, transforming healthcare in a similar way to what is already happening in the automotive, aviation and space exploration sectors [
4,
151,
152,
157].
6. Discussion
Why have a robot in the team?
There has been considerable debate surrounding the integration of AI and robots in healthcare. However, there are numerous aspects of this debate, with one key area being the specific tasks that robots should perform in healthcare teams. Nurses tend to favor AI and robots for repetitive tasks, such as monitoring patients, recording and reviewing information in the electronic medical record system [
44].
In the view of medical professionals, the deployment of AI and robots in the field of medicine and public health is a matter of great importance. However, many of these technologies are not yet capable of performing the tasks that are currently required of them, either because they lack the necessary capabilities or because the health systems in which they are used are not yet equipped to cope with the demands placed upon them. Examples of such tasks include the carrying out of scientific research, the implementation of measures to promote and raise awareness, the improvement of healthcare (preventive medicine), and the organization of campaigns to dissuade risky behavior [
166].
What risks or challenges will I face?
In terms of the potential risks associated with the adoption of AI and robotic systems in healthcare, many healthcare professionals express concern about the dehumanization of healthcare. In other words, the dehumanization of medicine is a significant concern for healthcare professionals, healthcare regulators and patients. One of the most significant challenges associated with the adoption of AI/carebots is the potential for the dehumanization of healthcare. The integration of new technologies into healthcare must be carefully considered to ensure that the benefits of human-centered care are not lost. This includes the prescription of medication, which is a crucial aspect of healthcare that must be preserved [
167].
Interoperability is important in healthcare. There are some good approaches, like the Internet of Medical Things (IoMT), but this technology needs a new, secure solution that can be used in cyber design. We need to find sustainable and energy-efficient IoMT-enabled healthcare system solutions, such as future healthcare devices, and study lightweight and efficient intrusion detection systems to protect IoMT-enabled devices [
159]. The IoMT concept takes a Metaverse approach to healthcare, where these technologies are already integrated into the healthcare ecosystem and related areas [
160,
161].
In the multiverse approach, concerns such as the security and privacy of user data are addressed; to increase trust, it is imperative to ensure user privacy and protect user data from any form of cyber-attack and information leakage to unauthorized users [
159,
168].
Another question is, there ethical and legal considerations, most studies are unable to provide guarantees on how to ensure that AI and robots will work in line with ethical issues. In most studies pertaining to the challenges of implementing robotic solutions. For healthcare professionals in general and for patients, there is an urgent need to resolve ethical issues such as shared moral or hybrid responsibility between AI and humans. The extent to which these systems can be held morally responsible, as well as the factors influencing their decision-making, is a key area of concern. It is also important to consider how AI robots can deal with the choice between two or more ethically debatable options.
One of the big questions is whether we can really say that these systems are morally responsible, and what factors influence their decision-making. It's also worth thinking about how AI robots handle the choice between two or more options that are open to debate from an ethical point of view. For instance, it's important to figure out whether a surgical robot should prioritize saving one patient's life over another during an unexpected critical situation.
These are questions that haven't been answered yet in a practical way. Most of these approaches are still in the early stages of development, which contrasts with the rapid technological advances that have been made recently [
169].
It is imperative that legal issues such as liability in the event of medical negligence, the legal status of AI and autonomous robots be reviewed in society at large, including the healthcare sector. In consideration of the concerns, it is sufficient to establish a robust and up-to-date legal framework that can serve as a foundation for new regulations pertaining to healthcare professions and institutions, as well as a link to other areas and contexts where autonomous technologies are used for healthcare [
170].
How can we resolve the issue of aligning AI values?
In addition to the other issues, there is a need to address the alignment of AI values. This raises the discussion of how to ensure that AI systems reflect ethical principles and human values. Proper alignment is crucial to avoid negative consequences such as violence, discrimination and harmful decisions. Without such alignment, there is a risk that AI will cause social injustice, inequality and damage to human beings and the environment. Therefore, the central question is how to develop and apply ethical guidelines that ensure that AI serves society well [
6].
In addition to the issues already discussed, there are still numerous challenges in using robot-assisted clinical practice. This includes a range of technological, safety, clinical, insurance financial, psychological, social, ethical and legal issues. The discussion revolves around how to address these challenges effectively. How can we ensure that robotic technology meets clinical safety standards? What are the financial and insurance implications of implementing these systems?
Also, how can we address the psychological and social impacts of integrating robots into medical practice? And finally, what are the ethical and legal considerations that must be resolved to ensure responsible and equitable implementation? These are fundamental questions that need clear and practical answers so that robotics can really benefit clinical practice.
7. Conclusions
The demand for digital healthcare is increasingly evident, with the lack of human resources and the growing pressure on healthcare services. With current developments in Artificial intelligence (AI), machine learning (ML) and deep learning (DL) in advanced robotic systems, there is a need to make healthcare systems more resilient, efficient and competitive,
In this article, we study robotic systems, which can be adapted to a healthcare context. Therefore, with the support of the most recent literature on the subject, the challenges in how to integrate these systems, considering security and privacy issues, the risk of dehumanization of healthcare, ethical and legal issues associated with it, have been investigated. In addition, our extended research project explores the challenges associated with deploying more intelligent and autonomous robotic systems in healthcare systems such as STAR, BART, PARO.
Due to the limitations of technological maturity, these present their own challenges. Furthermore, our research encompassed a comprehensive examination of recent advancements in the field of robotic systems, AI, and their applications in the context of contemporary healthcare, with a view to facilitating more efficient, secure, and dependable integration.
This entailed a comprehensive review of the following areas: AI, ML, DL, robotics systems, healthcare, medical technologies, the Internet of Medical Things (IoMT), and the metaverse in healthcare. Furthermore, we considered the potential of robotic systems to enhance the efficiency of treatment, processes, and operations (e.g., PARO, Spot, DaVinci).
This entailed research studies investigating the potential for robotic and AI systems to collaborate with humans in order to save lives. The comprehensive study of these topics not only contributed to a thorough understanding of the potential of AI and robotic systems, but also provided valuable insights into the practical implementation and optimization of these systems in the context of healthcare.
Considering the challenges of robot-assisted clinical practice and following the future directions and emerging technologies in the hospital context, considering aspects such as automation, muti-robotic systems, intelligent decision-making, virtualization and teleoperation. However, despite these technological advances, there are numerous challenges to be overcome in robot-assisted clinical practice, including technological issues such as the need to develop more intuitive and secure interfaces; financial and insurance challenges related to the high cost of acquisition and maintenance, liability in the event of robot error, privacy of patient data, psychological, social, ethical, and legal issues.
Author Contributions
Conceptualization, E.C. and S.O.; methodology, E.C. and A.C; software, E.C., S.O. and A.C; validation, E. C., S.O, and A.C.; formal analysis, E.C. and S.O.; investigation, E.C.; resources, E.C.; data curation, E.C., S.O. and A.C.; writing—original draft preparation, E.C., S.O. and A.C.; writing—review and editing, E.C., S.O. and A.C; visualization, E.C., S.O. and A.C; supervision, E.C., S.O. and A.C; project administration, E.C., S.O. and A.C; funding acquisition, A.C.. All authors have read and agreed to the published version of the manuscript.
Funding
This work was partially supported by Instituto de Telecomunicacoes, Lisboa, Portugal and FCT/MCTES through national funds and when applicable co-funded EU funds under the project UIDB/50008/2020.
Acknowledgments
We would like to thank ISCTE–Instituto Universitario de Lisboa and IT–Instituto de Telecomunicacoes for providing the required resources to perform this research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Christoforou, E.G.; Avgousti, S.; Ramdani, N.; Novales, C.; Panayides, A.S. The Upcoming Role for Nursing and Assistive Robotics: Opportunities and Challenges Ahead. Front Digit Health 2020, 2. [Google Scholar] [CrossRef] [PubMed]
- Ohneberg, C.; Stöbich, N.; Warmbein, A.; Rathgeber, I.; Mehler-Klamt, A.C.; Fischer, U.; Eberl, I. Assistive Robotic Systems in Nursing Care: A Scoping Review. BMC Nurs 2023, 22. [Google Scholar] [CrossRef] [PubMed]
- Locsin, R.C.; Ito, H. Can Humanoid Nurse Robots Replace Human Nurses? Journal of Nursing 2018, 5, 1. [Google Scholar] [CrossRef]
- Morgan, A.A.; Abdi, J.; Syed, M.A.Q.; Kohen, G. El; Barlow, P.; Vizcaychipi, M.P. Robots in Healthcare: A Scoping Review. Current Robotics Reports 2022, 3, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Vyas, S.; Gupta, S.; Shukla, V.K. Towards Edge AI and Varied Approaches of Digital Wellness in Healthcare Administration: A Study. In Proceedings of the Proceedings of 3rd IEEE International Conference on Computational Intelligence and Knowledge Economy, ICCIKE 2023; Institute of Electrical and Electronics Engineers Inc., 2023; pp. 186–190.
- Floridi, L.; Cowls, J.; Beltrametti, M.; Chatila, R.; Chazerand, P.; Dignum, V.; Luetge, C.; Madelin, R.; Pagallo, U.; Rossi, F.; et al. AI4People—An Ethical Framework for a Good AI Society: Opportunities, Risks, Principles, and Recommendations. Minds Mach (Dordr) 2018, 28. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.Z.; Nelson, B.J.; Murphy, R.R.; Choset, H.; Christensen, H.; Collins, S.H.; Dario, P.; Goldberg, K.; Ikuta, K.; Jacobstein, N.; et al. Combating COVID-19-The Role of Robotics in Managing Public Health and Infectious Diseases. Sci Robot 2020, 5. [Google Scholar] [CrossRef] [PubMed]
- Shishehgar, M.; Kerr, D.; Blake, J. A Systematic Review of Research into How Robotic Technology Can Help Older People. Smart Health 2018, 7–8. [Google Scholar] [CrossRef]
- Waller, M.; Stotler, C. Telemedicine: A Primer. Curr Allergy Asthma Rep 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Langer, A.; Feingold-Polak, R.; Mueller, O.; Kellmeyer, P.; Levy-Tzedek, S. Trust in Socially Assistive Robots: Considerations for Use in Rehabilitation. Neurosci Biobehav Rev 2019, 104. [Google Scholar] [CrossRef]
- Huang, R.; Li, H.; Suomi, R.; Li, C.; Peltoniemi, T. Intelligent Physical Robots in Health Care: Systematic Literature Review. J Med Internet Res 2023, 25. [Google Scholar] [CrossRef]
- Jeelani, S.; Dany, A.; Anand, B.; Vandana, S.; Maheswaran, T.; Rajkumar, E. Robotics and Medicine: A Scientific Rainbow in Hospital. J Pharm Bioallied Sci 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Abdi, J.; Al-Hindawi, A.; Ng, T.; Vizcaychipi, M.P. Scoping Review on the Use of Socially Assistive Robot Technology in Elderly Care. BMJ Open 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Lanfranco, A.R.; Castellanos, A.E.; Desai, J.P.; Meyers, W.C. Robotic Surgery: A Current Perspective. Ann Surg 2004, 239, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Xie, S.Q.; Das, R.; Zhu, G.L. Control Strategies for Effective Robot Assisted Gait Rehabilitation: The State of Art and Future Prospects. Med Eng Phys 2014, 36. [Google Scholar] [CrossRef] [PubMed]
- Halder Roy, A.; Ghosh, S.; Gupta, B. Robotics in Medical Domain: The Future of Surgery, Healthcare and Imaging. Wirel Pers Commun 2023, 132, 2885–2903. [Google Scholar] [CrossRef]
- Yang, G.Z.; Cambias, J.; Cleary, K.; Daimler, E.; Drake, J.; Dupont, P.E.; Hata, N.; Kazanzides, P.; Martel, S.; Patel, R.V.; et al. Medical Robotics-Regulatory, Ethical, and Legal Considerations for Increasing Levels of Autonomy. Sci Robot 2017, 2. [Google Scholar] [CrossRef] [PubMed]
- Bergeles, C.; Gosline, A.H.; Vasilyev, N.V.; Codd, P.J.; Del Nido, P.J.; Dupont, P.E. Concentric Tube Robot Design and Optimization Based on Task and Anatomical Constraints. IEEE Transactions on Robotics 2015, 31. [Google Scholar] [CrossRef] [PubMed]
- Varlamov, O. “Brains” for Robots: Application of the Mivar Expert Systems for Implementation of Autonomous Intelligent Robots. Big Data Research 2021, 25. [Google Scholar] [CrossRef]
- Schillinger, P.; Kohlbrecher, S.; Von Stryk, O. Human-Robot Collaborative High-Level Control with Application to Rescue Robotics. In Proceedings of the Proceedings - IEEE International Conference on Robotics and Automation; 2016; Vol. 2016-June.
- Cresswell, K.; Cunningham-Burley, S.; Sheikh, A. Health Care Robotics: Qualitative Exploration of Key Challenges and Future Directions. J Med Internet Res 2018, 20. [Google Scholar] [CrossRef]
- Wilk-Jakubowski, G.; Harabin, R.; Ivanov, S. Robotics in Crisis Management: A Review. Technol Soc 2022, 68. [Google Scholar] [CrossRef]
- Piaggio, D.; Zarro, M.; Pagliara, S.; Andellini, M.; Almuhini, A.; Maccaro, A.; Pecchia, L. The Use of Smart Environments and Robots for Infection Prevention Control: A Systematic Literature Review. Am J Infect Control 2023, 51, 1175–1181. [Google Scholar] [CrossRef]
- Vigo, F.; Egg, R.; Schoetzau, A.; Montavon, C.; Brezak, M.; Heinzelmann-Schwarz, V.; Kavvadias, T. An Interdisciplinary Team-Training Protocol for Robotic Gynecologic Surgery Improves Operating Time and Costs: Analysis of a 4-Year Experience in a University Hospital Setting. J Robot Surg 2022, 16, 89–96. [Google Scholar] [CrossRef]
- Piaggio, D.; Zarro, M.; Pagliara, S.; Andellini, M.; Almuhini, A.; Maccaro, A.; Pecchia, L. The Use of Smart Environments and Robots for Infection Prevention Control: A Systematic Literature Review. Am J Infect Control 2023, 51, 1175–1181. [Google Scholar] [CrossRef]
- Moawad, G.N.; Rahman, S.; Martino, M.A.; Klebanoff, J.S. Robotic Surgery during the COVID Pandemic: Why Now and Why for the Future. J Robot Surg 2020, 14, 917–920. [Google Scholar] [CrossRef]
- Tornbjerg, K.; Kanstrup, A.M.; Skov, M.B.; Rehm, M. Investigating Human-Robot Cooperation in a Hospital Environment: Scrutinising Visions and Actual Realisation of Mobile Robots in Service Work. In Proceedings of the DIS 2021 - Proceedings of the 2021 ACM Designing Interactive Systems Conference: Nowhere and Everywhere; Association for Computing Machinery, Inc, June 28 2021; pp. 381–391.
- Sharma, N.; Pandey, J.K.; Mondal, S. A Review of Mobile Robots: Applications and Future Prospect. International Journal of Precision Engineering and Manufacturing 2023, 24. [Google Scholar] [CrossRef]
- Nottingham, M.; Peterson, G.; Doern, C.; Doll, M.; Masroor, N.; Sanogo, K.; Stevens, M.; Bearman, G. Ultraviolet-C Light as a Means of Disinfecting Anesthesia Workstations. Am J Infect Control 2017, 45. [Google Scholar] [CrossRef]
- Carranza, K.A.R.; Day, N.J.B.; Lin, L.M.S.; Ponce, A.R.; Reyes, W.R.O.; Abad, A.C.; Baldovino, R.G. Akibot: A Telepresence Robot for Medical Teleconsultation. In Proceedings of the 2018 IEEE 10th International Conference on Humanoid, Nanotechnology, Information Technology, Communication and Control, Environment and Management, HNICEM 2018; 2018.
- Volland, J.; Fügener, A.; Schoenfelder, J.; Brunner, J.O. Material Logistics in Hospitals: A Literature Review. Omega (United Kingdom).
- Moons, K.; Waeyenbergh, G.; Pintelon, L. Measuring the Logistics Performance of Internal Hospital Supply Chains – A Literature Study. Omega (United Kingdom).
- Wang, H. Research on the Application of Logistics Management in Integrated Supply Chain Management System.; 2017.
- Patil, R.; Nema, S.; Kadam, S. Radio Frequency Identification System for Asset Tracking and Inventory Management in Hospitals. In Proceedings of the 2017 4th International Conference on Signal Processing and Integrated Networks, SPIN 2017; 2017.
- Ker, J.I.; Wang, Y.; Hajli, N. Examining the Impact of Health Information Systems on Healthcare Service Improvement: The Case of Reducing in Patient-Flow Delays in a U.S. Hospital. Technol Forecast Soc Change 2018, 127. [Google Scholar] [CrossRef]
- Puspitasari, R.; Arvianto, A.; Rinawati, D.I.; Laksono, P.W. Q Inventory Model with Product Expiry and Product Return on Pharmaceutical Products at Hospital Kardinah. In Proceedings of the 2016 2nd International Conference of Industrial, Mechanical, Electrical, and Chemical Engineering, ICIMECE 2016; 2017.
- Lv, Y.; Guo, D. Advance on Control and Management of Internal Transport System for Large-Scale General Hospital Buildings. In Proceedings of the Proceedings of 2013 IEEE International Conference on Service Operations and Logistics, and Informatics, SOLI 2013; 2013.
- Ahmadi-Javid, A.; Jalali, Z.; Klassen, K.J. Outpatient Appointment Systems in Healthcare: A Review of Optimization Studies. Eur J Oper Res 2017, 258. [Google Scholar] [CrossRef]
- Noma, A.M.; Ibrahim Musa, K.; Mamman, H.; Mato, A.D.; Abdulwadud Yusuf, A.; Sambo, M.A. Design of Intelligent and Secure Hospital Appointment Scheduling System. In Proceedings of the Proceedings of the 2022 IEEE Nigeria 4th International Conference on Disruptive Technologies for Sustainable Development, NIGERCON 2022; 2022.
- Cheng, L.; Zhao, N.; Yuan, M.; Wu, K. Stochastic Scheduling of Autonomous Mobile Robots at Hospitals. PLoS One 2023, 18. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Choi, M.; Kim, K.K.; Kim, Y. Bin Low-Power Counters Using Pathfinding Technique. In Proceedings of the Proceedings - International SoC Design Conference 2023, ISOCC 2023; 2023.
- Wang, C.; Savkin, A.V.; Clout, R.; Nguyen, H.T. A Method for Collision Free Navigation of a Robotic Hospital Bed among Steady and Moving Obstacles. In Proceedings of the 2014 IEEE Conference on Control Applications, CCA. Part of 2014 IEEE Multi-conference on Systems and Control, MSC 2014; 2014.
- Pan, B.; Zhang, Z.; Lim, A. A Hybrid Algorithm for Time-Dependent Vehicle Routing Problem with Time Windows. Comput Oper Res 2021, 128. [Google Scholar] [CrossRef]
- Holland, J.; Kingston, L.; McCarthy, C.; Armstrong, E.; O’dwyer, P.; Merz, F.; McConnell, M. Service Robots in the Healthcare Sector. Robotics 2021, 10. [Google Scholar] [CrossRef]
- Mohajerin Esfahani, P.; Kuhn, D. Data-Driven Distributionally Robust Optimization Using the Wasserstein Metric: Performance Guarantees and Tractable Reformulations. Math Program 2018, 171. [Google Scholar] [CrossRef]
- Farinelli, A.; Iocchi, L.; Nardi, D. Multirobot Systems: A Classification Focused on Coordination. IEEE Transactions on Systems, Man, and Cybernetics, Part B: Cybernetics 2004, 34. [Google Scholar] [CrossRef]
- Datta, P.; Roy, S.; Kumar Rana, A.; Kumar Sinha, P. Low-Cost Robot for Smart Healthcare Services in Hospital. In Proceedings of the Conference Proceedings - 2023 IEEE Silchar Subsection Conference, SILCON 2023; 2023.
- He, Y.; Qi, M.; Zhou, F.; Su, J. An Effective Metaheuristic for the Last Mile Delivery with Roaming Delivery Locations and Stochastic Travel Times. Comput Ind Eng 2020, 145. [Google Scholar] [CrossRef]
- Li, H.; Xiong, K.; Xie, X. Multiobjective Contactless Delivery on Medical Supplies under Open-Loop Distribution. Math Probl Eng 2021, 2021. [Google Scholar] [CrossRef]
- Borkar, K.K.; Aljrees, T.; Pandey, S.K.; Kumar, A.; Singh, M.K.; Sinha, A.; Singh, K.U.; Sharma, V. Stability Analysis and Navigational Techniques of Wheeled Mobile Robot: A Review. Processes 2023, 11. [Google Scholar] [CrossRef]
- Søraa, R.A.; Fostervold, M.E. Social Domestication of Service Robots: The Secret Lives of Automated Guided Vehicles (AGVs) at a Norwegian Hospital. International Journal of Human Computer Studies 2021, 152. [Google Scholar] [CrossRef]
- Pedan, M.; Gregor, M.; Plinta, D. Implementation of Automated Guided Vehicle System in Healthcare Facility. In Proceedings of the Procedia Engineering; 2017; Vol. 192.
- Ramdani, N.; Panayides, A.; Karamousadakis, M.; Mellado, M.; Lopez, R.; Christophorou, C.; Rebiai, M.; Blouin, M.; Vellidou, E.; Koutsouris, D. A Safe, Efficient and Integrated Indoor Robotic Fleet for Logistic Applications in Healthcare and Commercial Spaces: The Endorse Concept. In Proceedings of the Proceedings - IEEE International Conference on Mobile Data Management; 2019; Vol. 2019-June.
- LD Series Autonomous Mobile Robots | Omron. Available online: https://automation.omron.com/en/mx/products/family/LD (accessed on 15 April 2024).
- Niechwiadowicz, K.; Khan, Z. Robot Based Logistics System for Hospitals-Survey. 2008. [Google Scholar]
- Robotics for Logistics | Omron. Available online: https://automation.omron.com/en/mx/industries/logistics/robotics-logistics (accessed on 20 May 2024).
- RB-1 BASE - Warehouse Logistics Robot | Robotnik®. Available online: https://robotnik.eu/products/mobile-robots/rb-1-base-en/ (accessed on 20 May 2024).
- LD-Series | OMRON, Europe. Available online: https://industrial.omron.eu/en/products/ld-series (accessed on 16 March 2024).
- TUG T3 Autonomous Mobile Robot Product Description. 2016.
- Moses, J.; Ford, G. See Spot Save Lives: Fear, Humanitarianism, and War in the Development of Robot Quadrupeds. Digital War 2021, 2. [Google Scholar] [CrossRef]
- Spot | Boston Dynamics. Available online: https://bostondynamics.com/products/spot/ (accessed on 20 May 2024).
- The X30 Series Power Robot Dogs with Advanced Functions - DEEP Robotics. Available online: https://www.deeprobotics.cn/en/index/product3.html (accessed on 1 April 2024).
- Chaudhari, A.; Thakur, J.; Mhatre, P. PROTOTYPE FOR QUADRUPED ROBOT USING IoT TO DELIVER MEDICINES AND ESSENTIALS TO COVID-19 PATIENT. International Journal of Advanced Research in Engineering and Technology (IJARET) 4Volume 2021, 12, 147–155. [Google Scholar]
- Biswal, P.; Mohanty, P.K. Development of Quadruped Walking Robots: A Review. Ain Shams Engineering Journal 2021, 12. [Google Scholar] [CrossRef]
- The Lite 3 Series Advanced Bionic Robot Dogs - DEEP Robotics. Available online: https://www.deeprobotics.cn/en/index/product1.html (accessed on 1 April 2024).
- Assadian, O.; Harbarth, S.; Vos, M.; Knobloch, J.K.; Asensio, A.; Widmer, A.F. Practical Recommendations for Routine Cleaning and Disinfection Procedures in Healthcare Institutions: A Narrative Review. Journal of Hospital Infection 2021, 113. [Google Scholar] [CrossRef]
- Boyce, J.M. Modern Technologies for Improving Cleaning and Disinfection of Environmental Surfaces in Hospitals. Antimicrob Resist Infect Control 2016, 5. [Google Scholar] [CrossRef]
- Browne, K.; White, N.; Tehan, P.; Russo, P.L.; Amin, M.; Stewardson, A.J.; Cheng, A.C.; Graham, K.; O’Kane, G.; King, J.; et al. A Randomised Controlled Trial Investigating the Effect of Improving the Cleaning and Disinfection of Shared Medical Equipment on Healthcare-Associated Infections: The CLEaning and Enhanced DisiNfection (CLEEN) Study. Trials 2023, 24. [Google Scholar] [CrossRef]
- Casini, B.; Tuvo, B.; Scarpaci, M.; Totaro, M.; Badalucco, F.; Briani, S.; Luchini, G.; Costa, A.L.; Baggiani, A. Implementation of an Environmental Cleaning Protocol in Hospital Critical Areas Using a UV-C Disinfection Robot. Int J Environ Res Public Health 2023, 20. [Google Scholar] [CrossRef]
- Dancer, S.J. Hospital Cleaning: Past, Present, and Future. Antimicrob Resist Infect Control 2023, 12. [Google Scholar] [CrossRef]
- LightStrikeTM+ Robot - Xenex® UV Disinfection. Available online: https://xenex.com/light-strike-plus/ (accessed on 16 April 2024).
- Weber, D.J.; Rutala, W.A.; Anderson, D.J.; Chen, L.F.; Sickbert-Bennett, E.E.; Boyce, J.M. Effectiveness of Ultraviolet Devices and Hydrogen Peroxide Systems for Terminal Room Decontamination: Focus on Clinical Trials. Am J Infect Control 2016, 44. [Google Scholar] [CrossRef]
- Sterilray Autonomous Disinfection Vehicle (ADV) - Sterilray, Inc. Available online: https://sterilray.com/sterilray/products/sterilray-autonomous-disinfection-vehicle-adv/ (accessed on 16 March 2024).
- Classic | Our First Gen Device | | Tru-D SmartUVC. Available online: https://tru-d.com/products/tru-d-classic (accessed on 16 April 2024).
- Astrid, F.; Beata, Z.; Van den Nest Miriam; Julia, E.; Elisabeth, P.; Magda, D.E. The Use of a UV-C Disinfection Robot in the Routine Cleaning Process: A Field Study in an Academic Hospital. Antimicrob Resist Infect Control 2021, 10. [CrossRef]
- Figueroa, C.A.; Harrison, R.; Chauhan, A.; Meyer, L. Priorities and Challenges for Health Leadership and Workforce Management Globally: A Rapid Review. BMC Health Serv Res 2019, 19. [Google Scholar] [CrossRef]
- Dalton, K.R.; Rock, C.; Carroll, K.C.; Davis, M.F. One Health in Hospitals: How Understanding the Dynamics of People, Animals, and the Hospital Built-Environment Can Be Used to Better Inform Interventions for Antimicrobial-Resistant Gram-Positive Infections. Antimicrob Resist Infect Control 2020, 9. [Google Scholar] [CrossRef]
- Zajac, S.; Woods, A.; Tannenbaum, S.; Salas, E.; Holladay, C.L. Overcoming Challenges to Teamwork in Healthcare: A Team Effectiveness Framework and Evidence-Based Guidance. Front Commun (Lausanne) 2021, 6. [Google Scholar] [CrossRef]
- Thungjaroenkul, P.; Cunmings, G.G.; Embleton, A. The Impact of Nurse Staffing on Hospital Costs and Patient Length of Stay: A Systematic Review. Nursing Economics 2007, 25. [Google Scholar]
- Kailay, M.; Paposa, K.K. Sustainable Human Resource Management in the Hospital Sector: A Review of Literature. J Health Manag 2024. [Google Scholar] [CrossRef]
- Bates, D.W.; Singh, H. Two Decades since to Err Is Human: An Assessment of Progress and Emerging Priorities in Patient Safety. Health Aff 2018, 37. [Google Scholar] [CrossRef]
- Agitha, N.; Anjarwani, S.E.; Azizah, M.I.; Yunus, I.R.; Witjaksono, R.W. Implementation of COBIT 4.1 to Define and Maintain Infrastructure of Information Technology at Regional Public Hospital in West Nusa Tenggara. In Proceedings of the 2020 International Conference on Advancement in Data Science, E-Learning and Information Systems, ICADEIS 2020; 2020.
- KARIMBUX, N.; JOHN, M.T.; STERN, A.M.Y.; MAZANEC, M.T.; D’AMOUR, A.; COURTEMANCHE, J.I.M.; RABSON, B. MEASURING PATIENT EXPERIENCE OF ORAL HEALTH CARE: A CALL TO ACTION. Journal of Evidence-Based Dental Practice 2023, 23. [Google Scholar] [CrossRef]
- Oben, P. Understanding the Patient Experience: A Conceptual Framework. J Patient Exp 2020, 7. [Google Scholar] [CrossRef]
- Bodenger, G.; Steiner John, E.J. Developing, Implementing, and Maintaining an Effective Compliance Program. Journal of Health Care Compliance 2017, 19. [Google Scholar]
- Carroll, N.; Lord, J.C. The Growing Importance of Cost Accounting for Hospitals. J Health Care Finance 2016, 43. [Google Scholar]
- Hospital Nurse Staffing and Patient Outcomes.
- Griffiths, P.; Ball, J.; Drennan, J.; Dall’Ora, C.; Jones, J.; Maruotti, A.; Pope, C.; Recio Saucedo, A.; Simon, M. Nurse Staffing and Patient Outcomes: Strengths and Limitations of the Evidence to Inform Policy and Practice. A Review and Discussion Paper Based on Evidence Reviewed for the National Institute for Health and Care Excellence Safe Staffing Guideline Development. Int J Nurs Stud 2016, 63. [Google Scholar]
- Abdi, J.; Al-Hindawi, A.; Ng, T.; Vizcaychipi, M.P. Scoping Review on the Use of Socially Assistive Robot Technology in Elderly Care. BMJ Open 2018, 8. [Google Scholar] [CrossRef]
- Seal-Type Robot “PARO” to Be Marketed with Best Healing Effect in the World. Available online: https://www.aist.go.jp/aist_e/list/latest_research/2004/20041208_2/20041208_2.html (accessed on 18 April 2024).
- Valentí Soler, M.; Agüera-Ortiz, L.; Olazarán Rodríguez, J.; Mendoza Rebolledo, C.; Pérez Muñoz, A.; Rodríguez Pérez, I.; Osa Ruiz, E.; Barrios Sánchez, A.; Herrero Cano, V.; Carrasco Chillón, L.; et al. Social Robots in Advanced Dementia. Front Aging Neurosci 2015, 7. [Google Scholar] [CrossRef]
- Hung, L.; Liu, C.; Woldum, E.; Au-Yeung, A.; Berndt, A.; Wallsworth, C.; Horne, N.; Gregorio, M.; Mann, J.; Chaudhury, H. The Benefits of and Barriers to Using a Social Robot PARO in Care Settings: A Scoping Review. BMC Geriatr 2019, 19. [Google Scholar] [CrossRef]
- NAO the Humanoid and Programmable Robot | Aldebaran. Available online: https://www.aldebaran.com/en/nao (accessed on 17 April 2024).
- 2019 American Control Conference (ACC); IEEE, 2019; ISBN 9781538679265.
- Bandit – Robotics and Autonomous Systems Center. Available online: https://rasc.usc.edu/robots/humanoid/bandit/ (accessed on 17 April 2024).
- John, O.; Sarbadhikari, S.N.; Prabhu, T.; Goel, A.; Thomas, A.; Shroff, S.; Allaudin, F.; Weerabaddana, C.; Alhuwail, D.; Koirala, U.; et al. Implementation and Experiences of Telehealth: Balancing Policies With Practice in Countries of South Asia, Kuwait, and the European Union. Interact J Med Res 2022, 11. [Google Scholar] [CrossRef]
- Kruse, C.S.; Krowski, N.; Rodriguez, B.; Tran, L.; Vela, J.; Brooks, M. Telehealth and Patient Satisfaction: A Systematic Review and Narrative Analysis. BMJ Open 2017, 7. [Google Scholar] [CrossRef]
- Ohannessian, R.; Duong, T.A.; Odone, A. Global Telemedicine Implementation and Integration within Health Systems to Fight the COVID-19 Pandemic: A Call to Action. JMIR Public Health Surveill 2020, 6. [Google Scholar] [CrossRef]
- Ohannessian, R. Telemedicine: Potential Applications in Epidemic Situations. European Research in Telemedicine 2015, 4. [Google Scholar] [CrossRef]
- Dorsey, E.R.; Topol, E.J. State of Telehealth. New England Journal of Medicine 2016, 375. [Google Scholar] [CrossRef]
- Bhaskar, S.; Bradley, S.; Sakhamuri, S.; Moguilner, S.; Chattu, V.K.; Pandya, S.; Schroeder, S.; Ray, D.; Banach, M. Designing Futuristic Telemedicine Using Artificial Intelligence and Robotics in the COVID-19 Era. Front Public Health 2020, 8. [Google Scholar] [CrossRef]
- Luo, E.M.; Newman, S.; Amat, M.; Charpignon, M.L.; Duralde, E.R.; Jain, S.; Kaufman, A.R.; Korolev, I.; Lai, Y.; Lam, B.D.; et al. MIT COVID-19 Datathon: Data without Boundaries. BMJ Innov 2021, 7. [Google Scholar] [CrossRef]
- Kadu, A.; Singh, M. Comparative Analysis of E-Health Care Telemedicine System Based on Internet of Medical Things and Artificial Intelligence. In Proceedings of the Proceedings - 2nd International Conference on Smart Electronics and Communication, ICOSEC 2021; 2021.
- Koceski, S.; Koceska, N. Evaluation of an Assistive Telepresence Robot for Elderly Healthcare. J Med Syst 2016, 40. [Google Scholar] [CrossRef]
- Reyes-Cruz, G.; Phypers, I.; Boudouraki, A.; Price, D.; Fischer, J.; Reeves, S.; Galvez Trigo, M.; Maior, H. Augmented Robotic Telepresence (ART): A Prototype for Enhancing Remote Interaction and Participation. In Proceedings of the ACM International Conference Proceeding Series; 2023.
- Takahashi, M.; Ogata, M.; Imai, M.; Nakamura, K.; Nakadai, K. A Case Study of an Automatic Volume Control Interface for a Telepresence System. In Proceedings of the Proceedings - IEEE International Workshop on Robot and Human Interactive Communication; 2015; Vol. 2015-November.
- Asadi, A.; Fischer, K. The Effect of an Empathy-Eliciting Intervention on the Perception of Telepresence Robot Users *. In Proceedings of the Proceedings of IEEE Workshop on Advanced Robotics and its Social Impacts, ARSO; 2023; Vol. 2023-June.
- Zhang, G.; Hansen, J.P. Telepresence Robots for People with Special Needs: A Systematic Review. Int J Hum Comput Interact 2022, 38. [Google Scholar] [CrossRef]
- 109. SIGGRAPH Asia 2014 Autonomous Virtual Humans and Social Robot for Telepresence, SIGGRAPH ASIA 2014. SIGGRAPH Asia 2014 Autonomous Virtual Humans and Social Robot for Telepresence, SA 2014.
- Christoff, N.; Neshov, N.N.; Tonchev, K.; Manolova, A. Application of a 3D Talking Head as Part of Telecommunication AR, VR, MR System: Systematic Review. Electronics (Switzerland) 2023, 12. [Google Scholar] [CrossRef]
- Rotbøll Nielsen, P.; Rudin, Å.; Werner, M.U. Prediction of Postoperative Pain. Curr Anaesth Crit Care 2007, 18, 157–165. [Google Scholar] [CrossRef]
- Edwards, R.R.; Dworkin, R.H.; Sullivan, M.D.; Turk, D.C.; Wasan, A.D. The Role of Psychosocial Processes in the Development and Maintenance of Chronic Pain. Journal of Pain 2016, 17, T70–T92. [Google Scholar] [CrossRef]
- Shakir, A.; Abate, D.; Tebeje, F.; Weledegebreal, F. Magnitude of Surgical Site Infections, Bacterial Etiologies, Associated Factors and Antimicrobial Susceptibility Patterns of Isolates among Post-Operative Patients in Harari Region Public Hospitals, Harar, Eastern Ethiopia. Infect Drug Resist 2021, 14. [Google Scholar] [CrossRef]
- Parks, MS, RN, CNP, L.; Routt, MSN, ANP/GNP-BC, AOCNP, M.; De Villiers, MSN, RN, OCN, ACNS-BC, A. Enhanced Recovery After Surgery. J Adv Pract Oncol 2018, 8. [CrossRef]
- Trulsson Schouenborg, A.; Rivano Fischer, M.; Bondesson, E.; Jöud, A. Physiotherapist-Led Rehabilitation for Patients with Chronic Musculoskeletal Pain: Interventions and Promising Long-Term Outcomes. BMC Musculoskelet Disord 2021, 22. [Google Scholar] [CrossRef]
- Barbari, V.; Storari, L.; Ciuro, A.; Testa, M. Effectiveness of Communicative and Educative Strategies in Chronic Low Back Pain Patients: A Systematic Review. Patient Educ Couns 2020, 103. [Google Scholar] [CrossRef]
- Edwards, P.K.; Mears, S.C.; Lowry Barnes, C. Preoperative Education for Hip and Knee Replacement: Never Stop Learning. Curr Rev Musculoskelet Med 2017, 10. [Google Scholar] [CrossRef]
- Humphrey, R.; Malone, D. Effectiveness of Preoperative Physical Therapy for Elective Cardiac Surgery; 2015; Vol. 95;
- Qian, L.; Wu, J.Y.; Dimaio, S.P.; Navab, N.; Kazanzides, P. A Review of Augmented Reality in Robotic-Assisted Surgery. IEEE Trans Med Robot Bionics 2020, 2, 1–16. [Google Scholar] [CrossRef]
- Cepolina, F.; Razzoli, R.P. An Introductory Review of Robotically Assisted Surgical Systems. International Journal of Medical Robotics and Computer Assisted Surgery 2022, 18. [Google Scholar] [CrossRef]
- Pana, C.F.; Radulescu, V.M.; Voicila, D.D.; Patrascu-Pana, D.M.; Resceanu, I.C. Position Control of Active Arms of Da Vinci Robotic Surgical System. In Proceedings of the Proceedings of the 2023 24th International Carpathian Control Conference, ICCC 2023; 2023.
- Noelle Marie, D.; Espiritu; Balcita, V.D.G.; Goy, T.P.P.; Perez, E.M.S.; Baldovino, R.G.; Munsayac, F.E.T.; Bugtai, N.T. A 2021 Review on Recent Advancements in Robotic-Assisted Minimally Invasive Surgery: The Philippines Perspective. In Proceedings of the 2021 IEEE 13th International Conference on Humanoid, Nanotechnology, Information Technology, Communication and Control, Environment, and Management, HNICEM 2021; Institute of Electrical and Electronics Engineers Inc., 2021.
- McIntosh, M.K.; Christie, S. Opportunities and Challenges for Robotic-Assisted Spine Surgery: Feasible Indications for the MAZOR<sup>TM</sup> X Stealth Edition. In Proceedings of the Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS; 2023.
- Da Vinci Robotic Surgical Systems | Intuitive. Available online: https://www.intuitive.com/en-us/products-and-services/da-vinci (accessed on 25 April 2024).
- HugoTM RAS System | Medtronic (UK). Available online: https://www.medtronic.com/covidien/en-gb/robotic-assisted-surgery/hugo-ras-system.html?gclid=Cj0KCQjw_qexBhCoARIsAFgBletuys_ZgPNXfAsHlC7BnREhxK9yxOatGGYsh-HU6mu60lCjpWao9X4aAseNEALw_wcB&cmpid=PPC_GOOG_HCP-BD-hugo-RSA_AMEROLM-MS-SurgicalRoboticsHugo-4398090&sfdcid=7014O000001JF3G&cid=PPC:GOOG:%2Bhugo%20%2Brobotic%20%2Bassisted%20%2Bsurgery:ras-hugo&ef_id=Cj0KCQjw_qexBhCoARIsAFgBletuys_ZgPNXfAsHlC7BnREhxK9yxOatGGYsh-HU6mu60lCjpWao9X4aAseNEALw_wcB:G:s&s_kwcid=AL!18272!3!525862272601!b!!g!!%2Bhugo%20%2Brobotic%20%2Bassisted%20%2Bsurgery!12117747053!118230063524 (accessed on 25 April 2024).
- Mazor Robotic Guidance System | Medtronic. Available online: https://www.medtronic.com/us-en/healthcare-professionals/products/spinal-orthopaedic/spine-robotics/mazor-x-stealth-edition.html (accessed on 25 April 2024).
- Connor, M.J.; Dasgupta, P.; Ahmed, H.U.; Raza, A. Autonomous Surgery in the Era of Robotic Urology: Friend or Foe of the Future Surgeon? Nat Rev Urol 2020, 17. [Google Scholar] [CrossRef]
- Han, J.; Davids, J.; Ashrafian, H.; Darzi, A.; Elson, D.S.; Sodergren, M. A Systematic Review of Robotic Surgery: From Supervised Paradigms to Fully Autonomous Robotic Approaches. International Journal of Medical Robotics and Computer Assisted Surgery 2022, 18. [Google Scholar] [CrossRef]
- Peek, G.; Ross, S.B. The Future Implementation of Artificial Intelligence Technology in Esophageal Surgery. Artificial Intelligence Surgery 2023, 3. [Google Scholar] [CrossRef]
- O’Sullivan, S.; Nevejans, N.; Allen, C.; Blyth, A.; Leonard, S.; Pagallo, U.; Holzinger, K.; Holzinger, A.; Sajid, M.I.; Ashrafian, H. Legal, Regulatory, and Ethical Frameworks for Development of Standards in Artificial Intelligence (AI) and Autonomous Robotic Surgery. International Journal of Medical Robotics and Computer Assisted Surgery 2019, 15. [Google Scholar] [CrossRef]
- Kyrarini, M.; Lygerakis, F.; Rajavenkatanarayanan, A.; Sevastopoulos, C.; Nambiappan, H.R.; Chaitanya, K.K.; Babu, A.R.; Mathew, J.; Makedon, F. A Survey of Robots in Healthcare. Technologies (Basel) 2021, 9. [Google Scholar] [CrossRef]
- Rajavenkatanarayanan, A.; Kanal, V.; Tsiakas, K.; Calderon, D.; Papakostas, M.; Abujelala, M.; Galib, M.; Ford, J.C.; Wylie, G.; Makedon, F. A Survey of Assistive Technologies for Assessment and Rehabilitation of Motor Impairments in Multiple Sclerosis. Multimodal Technologies and Interaction 2019, 3. [Google Scholar] [CrossRef]
- Ármannsdóttir, A.L.; Beckerle, P.; Moreno, J.C.; van Asseldonk, E.H.F.; Manrique-Sancho, M.T.; del-Ama, A.J.; Veneman, J.F.; Briem, K. Assessing the Involvement of Users During Development of Lower Limb Wearable Robotic Exoskeletons: A Survey Study. Hum Factors 2020, 62, 351–364. [Google Scholar] [CrossRef]
- Gassert, R.; Dietz, V. Rehabilitation Robots for the Treatment of Sensorimotor Deficits: A Neurophysiological Perspective. J Neuroeng Rehabil 2018, 15. [Google Scholar] [CrossRef]
- Kuroda, Y.; Young, M.; Shoman, H.; Punnoose, A.; Norrish, A.R.; Khanduja, V. Advanced Rehabilitation Technology in Orthopaedics—a Narrative Review. Int Orthop 2021, 45. [Google Scholar] [CrossRef]
- Qassim, H.M.; Wan Hasan, W.Z. A Review on Upper Limb Rehabilitation Robots. Applied Sciences (Switzerland) 2020, 10. [Google Scholar] [CrossRef]
- G-EOS – Reha Technology. Available online: https://www.rehatechnology.com/en/g-eos/ (accessed on 22 May 2024).
- InMotion® ARM | BIONIK. Available online: https://bioniklabs.com/inmotion-arm/ (accessed on 22 May 2024).
- Lopez-Larraz, E.; Antelis, J.M.; Montesano, L.; Gil-Agudo, A.; Minguez, J. Continuous Decoding of Motor Attempt and Motor Imagery from EEG Activity in Spinal Cord Injury Patients. In Proceedings of the Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS; 2012.
- Esquenazi, A. Comment on “Assessing Effectiveness and Costs in Robot-Mediated Lower Limbs Rehabilitation: A Meta-Analysis and State of the Art.” J Healthc Eng 2018, 2018. 2018.
- Cano-de-la-Cuerda, R.; Blázquez-Fernández, A.; Marcos-Antón, S.; Sánchez-Herrera-Baeza, P.; Fernández-González, P.; Collado-Vázquez, S.; Jiménez-Antona, C.; Laguarta-Val, S. Economic Cost of Rehabilitation with Robotic and Virtual Reality Systems in People with Neurological Disorders: A Systematic Review. J Clin Med 2024, 3, 1. [Google Scholar] [CrossRef]
- Ruiz-Olaya, A.F.; Quinayas Burgos, C.A.; Londono, L.T. A Low-Cost Arm Robotic Platform Based on Myoelectric Control for Rehabilitation Engineering. In Proceedings of the 2019 IEEE 10th Annual Ubiquitous Computing, Electronics and Mobile Communication Conference, UEMCON 2019; 2019.
- C. Gopura, R.A.R.; V. Bandara, D.S.; P. Gunasekara, J.M.; S., T. Recent Trends in EMG-Based Control Methods for Assistive Robots. 2013.
- Yang, S.H.; Koh, C.L.; Hsu, C.H.; Chen, P.C.; Chen, J.W.; Lan, Y.H.; Yang, Y.; Lin, Y. De; Wu, C.H.; Liu, H.K.; et al. An Instrumented Glove-Controlled Portable Hand-Exoskeleton for Bilateral Hand Rehabilitation. Biosensors (Basel) 2021, 11. [Google Scholar] [CrossRef]
- Unanyan, N.N.; Belov, A.A. Signal-Based Approach to EMG-Sensor Fault Detection in Upper Limb Prosthetics. In Proceedings of the Proceedings of the 2019 20th International Carpathian Control Conference, ICCC 2019; 2019.
- de la Iglesia, D.H.; Mendes, A.S.; González, G.V.; Jiménez-Bravo, D.M.; de Paz Santana, J.F. Connected Elbow Exoskeleton System for Rehabilitation Training Based on Virtual Reality and Context-Aware. Sensors (Switzerland) 2020, 20. [Google Scholar] [CrossRef]
- Hobbs, B.; Artemiadis, P. A Review of Robot-Assisted Lower-Limb Stroke Therapy: Unexplored Paths and Future Directions in Gait Rehabilitation. Front Neurorobot 2020, 14. [Google Scholar] [CrossRef]
- Matjačić, Z.; Zadravec, M.; Olenšek, A. Feasibility of Robot-Based Perturbed-Balance Training during Treadmill Walking in a High-Functioning Chronic Stroke Subject: A Case-Control Study. J Neuroeng Rehabil 2018, 15. [Google Scholar] [CrossRef]
- Podobnik, J.; Kraljić, D.; Zadravec, M.; Munih, M. Centre of Pressure Estimation during Walking Using Only Inertial-Measurement Units and End-to-End Statistical Modelling. Sensors (Switzerland) 2020, 20. [Google Scholar] [CrossRef]
- Viswanathan, P.; Zambalde, E.P.; Foley, G.; Graham, J.L.; Wang, R.H.; Adhikari, B.; Mackworth, A.K.; Mihailidis, A.; Miller, W.C.; Mitchell, I.M. Intelligent Wheelchair Control Strategies for Older Adults with Cognitive Impairment: User Attitudes, Needs, and Preferences. Auton Robots 2017, 41. [Google Scholar] [CrossRef]
- Yan, Q.; Huang, J.; Tao, C.; Chen, X.; Xu, W. Intelligent Mobile Walking-Aids: Perception, Control and Safety. Advanced Robotics 2020, 34. [Google Scholar] [CrossRef]
- Di, P.; Hasegawa, Y.; Nakagawa, S.; Sekiyama, K.; Fukuda, T.; Huang, J.; Huang, Q. Fall Detection and Prevention Control Using Walking-Aid Cane Robot. IEEE/ASME Transactions on Mechatronics 2016, 21. [Google Scholar] [CrossRef]
- Robot Assist Walker, RT. 2 | Products | RT.WORKS Co., Ltd. Available online: https://www.rtworks.co.jp/eng/product/rt2.html (accessed on 1 May 2024).
- Koseki, K.; Mutsuzaki, H.; Yoshikawa, K.; Endo, Y.; Maezawa, T.; Takano, H.; Yozu, A.; Kohno, Y. Gait Training Using the Honda Walking Assistive Device® in a Patient Who Underwent Total Hip Arthroplasty: A Single-Subject Study. Medicina (Lithuania) 2019, 55. [Google Scholar] [CrossRef]
- Valadão, C.; Caldeira, E.; Bastos-Filho, T.; Frizera-Neto, A.; Carelli, R. A New Controller for a Smart Walker Based on Human-Robot Formation. Sensors (Switzerland) 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- Calafiore, D.; Negrini, F.; Tottoli, N.; Ferraro, F.; Ozyemisci-Taskiran, O.; De Sire, A. Efficacy of Robotic Exoskeleton for Gait Rehabilitation in Patients with Subacute Stroke: A Systematic Review. Eur J Phys Rehabil Med 2022, 58. [Google Scholar] [CrossRef]
- Huang, J.; Di, P.; Wakita, K.; Fukuda, T.; Sekiyama, K. Study of Fall Detection Using Intelligent Cane Based on Sensor Fusion. In Proceedings of the 2008 International Symposium on Micro-NanoMechatronics and Human Science, MHS 2008; 2008.
- WAKITA, K.; HUANG, J.; SEKIYAMA, K.; FUKUDA, T. Real-Time Fall Detection and Prevention Control Using Intelligent Cane for Human Operator. The Abstracts of the international conference on advanced mechatronics : toward evolutionary fusion of IT and mechatronics : ICAM, 2010; 2010, 5. [Google Scholar] [CrossRef]
- Pradyumna, G.R.; Hegde, R.B.; Bommegowda, K.B.; Jan, T.; Naik, G.R. Empowering Healthcare with IoMT: Evolution, Machine Learning Integration, Security, and Interoperability Challenges. IEEE Access 2024, 12. [Google Scholar] [CrossRef]
- Chengoden, R.; Victor, N.; Huynh-The, T.; Yenduri, G.; Jhaveri, R.H.; Alazab, M.; Bhattacharya, S.; Hegde, P.; Maddikunta, P.K.R.; Gadekallu, T.R. Metaverse for Healthcare: A Survey on Potential Applications, Challenges and Future Directions. IEEE Access 2023, 11. [Google Scholar] [CrossRef]
- Chen, D.; Zhang, R. Exploring Research Trends of Emerging Technologies in Health Metaverse: A Bibliometric Analysis. SSRN Electronic Journal 2022. [Google Scholar] [CrossRef]
- Pillai, R.; Sivathanu, B.; Mariani, M.; Rana, N.P.; Yang, B.; Dwivedi, Y.K. Adoption of AI-Empowered Industrial Robots in Auto Component Manufacturing Companies. Production Planning and Control 2022, 33, 1517–1533. [Google Scholar] [CrossRef]
- Venkataramanan, V.; Modi, A.; Mistry, K. AI and Robots Impact on Space Exploration. Advances in Astronautics Science and Technology 2024. [Google Scholar] [CrossRef]
- Doyle, R.; Kubota, T.; Picard, M.; Sommer, B.; Ueno, H.; Visentin, G.; Volpe, R. Recent Research and Development Activities on Space Robotics and AI. Advanced Robotics 2021, 35. [Google Scholar] [CrossRef]
- Soori, M.; Arezoo, B.; Dastres, R. Artificial Intelligence, Machine Learning and Deep Learning in Advanced Robotics, a Review. Cognitive Robotics 2023, 3. [Google Scholar] [CrossRef]
- Sarker, S.; Jamal, L.; Ahmed, S.F.; Irtisam, N. Robotics and Artificial Intelligence in Healthcare during COVID-19 Pandemic: A Systematic Review. Rob Auton Syst 2021, 146. [Google Scholar] [CrossRef]
- Palmer, A.; Schwan, D. Beneficent Dehumanization: Employing Artificial Intelligence and Carebots to Mitigate Shame-Induced Barriers to Medical Care. Bioethics 2022, 36. [Google Scholar] [CrossRef] [PubMed]
- Marchang, J.; Di Nuovo, A. Assistive Multimodal Robotic System (AMRSys): Security and Privacy Issues, Challenges, and Possible Solutions. Applied Sciences (Switzerland) 2022, 12. [Google Scholar] [CrossRef]
- Tóth, Z.; Caruana, R.; Gruber, T.; Loebbecke, C. The Dawn of the AI Robots: Towards a New Framework of AI Robot Accountability. Journal of Business Ethics 2022, 178. [Google Scholar] [CrossRef]
- Eldakak, A.; Alremeithi, A.; Dahiyat, E.; El-Gheriani, M.; Mohamed, H.; Abdulrahim Abdulla, M.I. Civil Liability for the Actions of Autonomous AI in Healthcare: An Invitation to Further Contemplation. Humanit Soc Sci Commun 2024, 11. [Google Scholar] [CrossRef]
Table 1.
Related logistics and transport systems robots.
Table 1.
Related logistics and transport systems robots.
Table 2.
Related quadruped robots’ systems characteristics.
Table 2.
Related quadruped robots’ systems characteristics.
Table 3.
Related Cleaning and disinfection robots’ systems.
Table 3.
Related Cleaning and disinfection robots’ systems.
Table 4.
Summary Table of Key Socially Assistive Robots (SAR) in Hospital Settings.
Table 4.
Summary Table of Key Socially Assistive Robots (SAR) in Hospital Settings.
Table 6.
Summary Table of Key Telepresence robots’ systems in Hospital Settings.
Table 6.
Summary Table of Key Telepresence robots’ systems in Hospital Settings.
Table 7.
Summary Table of Key surgical robots’ systems in Hospital Settings.
Table 7.
Summary Table of Key surgical robots’ systems in Hospital Settings.
Table 8.
Summary Table of Key upper limb rehabilitation systems in Hospital Settings.
Table 8.
Summary Table of Key upper limb rehabilitation systems in Hospital Settings.
Table 9.
Summary Table of Key EMG-Driven Exoskeleton Robots systems in Hospital Settings.
Table 9.
Summary Table of Key EMG-Driven Exoskeleton Robots systems in Hospital Settings.
Table 10.
Summary Table of Key Lower Limb Rehabilitation Robots system.
Table 10.
Summary Table of Key Lower Limb Rehabilitation Robots system.
Table 11.
Summary Table of Key Walking Assisting Robots system.
Table 11.
Summary Table of Key Walking Assisting Robots system.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).