1. Introduction
American Indian/Alaska Native/Native American (AI/AN) populations have long experienced disparities in healthcare access and outcomes, rooted in a history of colonization, forced relocation, and systemic marginalization [
1,
2,
3,
4]. These historical traumas have contributed to persistent health inequities, making AI/AN particularly vulnerable to the devastating effects of the COVID-19 virus [
5,
6,
7,
8,
9,
10,
11]. The COVID-19 pandemic has presented challenges throughout the world. Among the various sectors and populations the pandemic has affected, AI/AN communities have faced unique and disproportionate burdens stemming from historical, socioeconomic, and health-related disparities. The COVID-19 pandemic has disproportionately affected the AI/AN population across the country. AI/AN populations endured (i) COVID-19 infection rates over 3.5 times higher than those in non-Hispanic Whites, (ii) hospitalization rates four times higher compared to non-Hispanic Whites, and (iii) higher rates of mortality at younger ages than non-Hispanic Whites [
12,
13]. Additionally, a number of studies have demonstrated greater COVID-19 vaccine hesitancy amongst minority groups compared to Whites in the United States [
14,
15]. These disparities highlight the urgent need for targeted interventions within these communities.
Vaccination against COVID-19 represents a critical tool in mitigating the spread of the virus and protecting vulnerable populations [
16]. At the end of 2021, the vaccination rate of American Indians in Michigan was 52%, below the ideal 70% vaccination rate that was necessary to protect the community from disease [
17]. However, disparities in vaccination uptake have emerged, raising concerns about equitable access and vaccine acceptance among AI/AN.
Educational interventions play a pivotal role in addressing these challenges, offering opportunities to dispel myths and educate communities to make informed decisions about vaccination. By examining attitudes and beliefs among AI/AN in the context of the COVID-19 pandemic, this study aims to contribute to the understanding of vaccine hesitancy and the effectiveness of educational interventions in promoting vaccination acceptance within this marginalized population.
2. Materials and Methods
2.1. Study Design
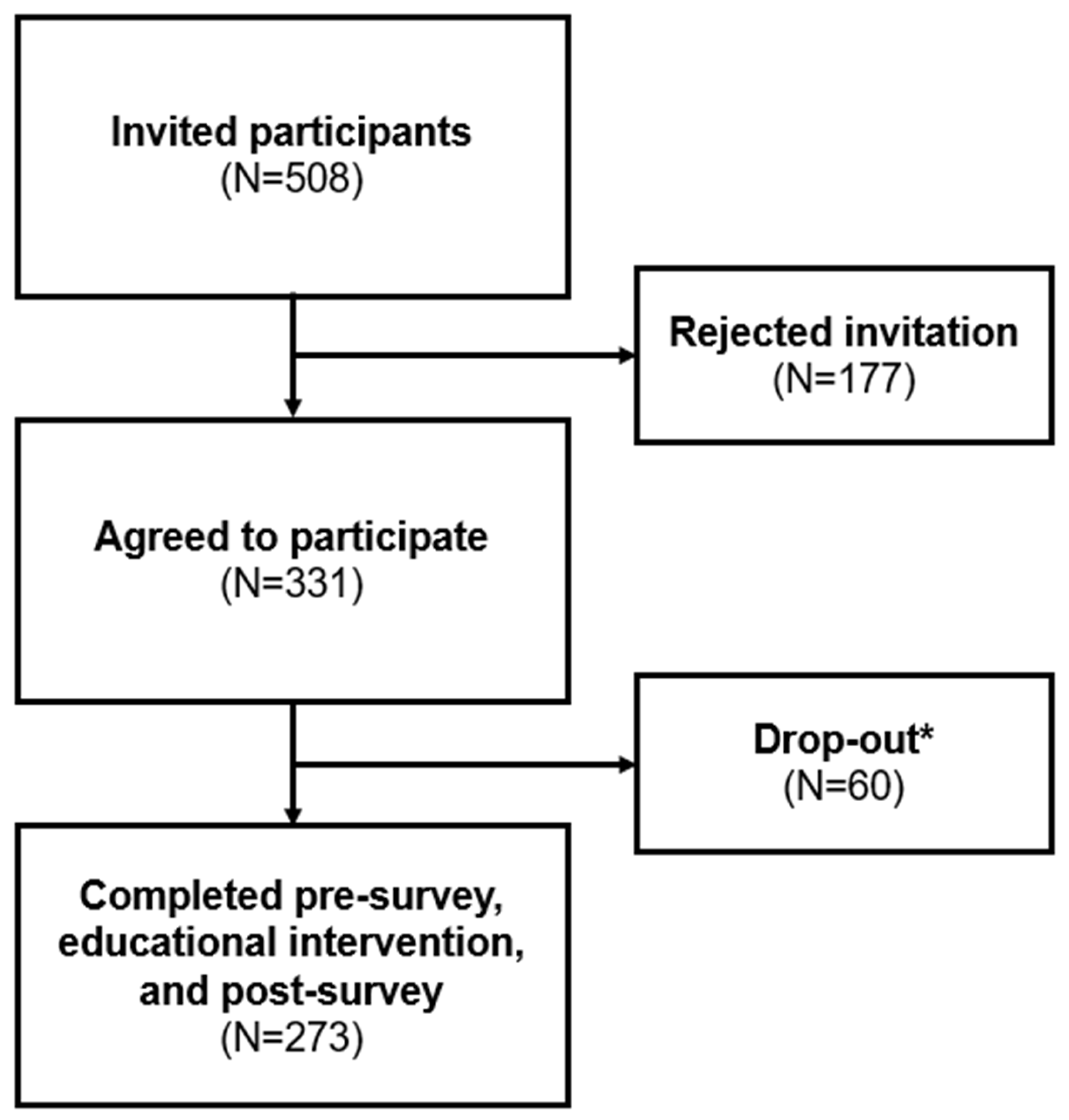
A pre/post prospective study design was used to collect data using questionnaires at a single outpatient, Indian Health Service (IHS) clinic in central Michigan. This study was conducted from February 22, 2022 to January 4, 2024. Research assistants recruited patients in the waiting room of the selected clinic to complete the questionnaire. The study protocol included a pre-survey, a randomized educational intervention in either a video or infographic format, and a post-survey (
Figure 1). After informed consent was obtained, participants completed the questionnaire using a pre-loaded survey on a project-issued iPad or on their personal Smartphone device via a QR code. Then, participants’ attitudes and knowledge regarding COVID-19 and the COVID vaccines were analyzed to draw conclusions about the effectiveness of the interventions. Data recorded from this study remained anonymous and the separate secure document with participants’ email addresses was the only patient-identifying information gathered during this study. Questionnaires and educational interventions were distributed by CITI-trained Central Michigan University (CMU) College of Medicine students. The CMU College of Medicine Research Institutional Review Board (IRB) and the Saginaw Chippewa Indian Tribe provided approval and oversite to maintain ethical standards and participant anonymity.
2.2. Participants
Participants were recruited from a single Indian Health Services outpatient clinic in rural Michigan which serves 4,123 active patients between 2018 and 2021. The inclusion criteria were defined as patients from this clinic who were above the age of 18 and able to understand English. The exclusion criteria were defined as individuals who were not patients of this clinic or those who were not above the age of 18 or were unable to understand English.
2.3. Questionnaires and Educational Interventions
The study protocol questionnaire included a validated 56-item pre-survey, a randomized educational intervention, and a 38-item post-survey (
Figure 1), which were collected via Qualtrics Online Survey Platform between February 22, 2022, to January 4, 2024. These three components were intended to be completed during a single session, though participants had the flexibility to pause and resume as needed, such as when waiting for their appointment. The pre-survey obtained information on the following domains: demographics, COVID-19 and vaccine knowledge, COVID-19 vaccination status, and vaccine beliefs and concerns. Questions regarding demographics, virus and vaccine knowledge, and vaccination status consisted of multiple-choice answers. Demographic data was optional to complete. 29 of these items utilized a three-point Likert scale which included 2 = agree, 1 = unsure, or 0 = disagree to assess attitude regarding COVID-19 and its vaccine. There were seven multiple choice questions aimed at assessing COVID-19 and vaccine knowledge. Next, using the Qualtrics randomization function, participants received either a seven-minute COVID-19 or vaccine educational video or received a COVID-19 and vaccine educational infographic (
Supplementary material S1 and S2). If participants received the infographic, they were required to spend at least four-minutes reading it before moving on to the next step. Both materials were produced using information from the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO). Immediately following the educational intervention, participants received the same COVID-19 knowledge and attitude questions they had answered in the pre-intervention questionnaire. The questions regarding demographics from the pre-intervention survey were not included in the post-intervention survey. After completion of the post-intervention questionnaire, participants received a
$10 gift card for their completion of these three components.
Knowledge levels were assessed through inquiries covering various aspects, such as measures to protect against COVID-19 transmission, modes of COVID-19 spread, vaccine effects, COVID-19 vaccine efficacy, post-vaccine behavior, COVID-19 virus side effects, and COVID-19 vaccine development. Attitudes were evaluated across multiple dimensions, including trust in COVID-19 vaccine effectiveness and safety, personal belief in the benefits of COVID-19 vaccination, confidence in COVID-19 vaccine testing and results, perception of rapid COVID-19 vaccine development, concerns about COVID-19 vaccine side effects, concerns about long-term effects of COVID-19 vaccines, challenges in discerning trustworthy vaccine information, influence of trusted sources on vaccination, concerns about missing work due to vaccine side effects, etc.
2.4. Study Sample and Statistical Analysis
This Indian Health Service clinic served 4,123 active patients between 2018 and 2021, prior to the start of this study. The sample was randomly selected from individuals in the clinic’s waiting room during the study period. The sample size was determined based on a desire to detect a medium intervention effect size (half a standard deviation difference between means) with a power of 95% and an alpha value of 0.05, resulting in an estimated sample size of 210.
Changes in attitudes and knowledge were assessed using paired t-tests to compare pre-intervention and post-intervention survey item responses. Selected pre/post analyses were also computed using non-parametric statistics (Wilcoxon matched-pairs signed-ranks test) with comparable results. Additionally, independent t-tests were used to compare changes in attitudes and knowledge items between participants exposed to infographic versus videographic interventions. The influence of demographic factors on changes in attitudes and knowledge was explored through independent t-tests and one-way ANOVAs. The assumption of homogeneity of variance was assessed for both t-tests and ANOVAs. Due to the large number of tests computed for item change, the Benjamini-Hochberg procedure was applied to adjust for multiple hypothesis testing. Results are reported for each individual item test as computed and then compared with an adjusted p-value for comparison.
3. Results
The 273 participants represent 54% of invited participants. Participants, residing across 27 counties throughout Michigan, completed the pre-survey, educational intervention, and post-survey (
Figure 2). The demographic profile of these participants is detailed in
Table 1. Notably, the cohort comprised predominantly females (67%), with the most common age brackets being 25-34 years (22%) and 35-44 years (21%). The majority identified as non-Hispanic (91%), and a significant portion resided in micropolitan areas (79%), as classified by Core Based Statistical Areas. Regarding political affiliations, most participants identified as democratic (30%) or with alternative affiliations (31%). In terms of COVID-19 impacts, more than half of the participants (55%) reported pandemic-related disruptions to their employment status. Additionally, 51% of participants or someone in their household identified as essential workers during the pandemic. The majority (88%) self-tested for COVID-19, with 90% of participants reporting a history of positive test results. Over half (58%) the participants knew someone hospitalized or deceased due to COVID-19. Regarding co-morbidities, 47% reported having at least one at-risk medical condition, while 33% reported having two or more. Concerning household members, 40% indicated one household member with an at-risk condition, and 36% indicated two or more. Participants were also queried about adherence to a list of CDC guidelines, such as mask-wearing, social distancing, and hand hygiene, with a majority (74%) reporting compliance with four or more precautions. Regarding seasonal vaccinations, 58% received the influenza vaccine last year, and 52% either received or planned to receive it this year. Lastly, 59% of this study cohort were already partially or completely vaccinated.
When looking at COVID-19 virus and vaccine knowledge before and after the educational intervention, our data revealed that out of the seven knowledge-based questions, knowledge regarding COVID-19 and vaccine topics increased in five of these variables (
Table 2). After receiving the intervention, participants showed increasing knowledge in protection and reduction of COVID-19 transmission (
p < 0.001), how vaccines work (
p = 0.008), how the COVID-19 vaccines work (
p < 0.001), COVID-19 vaccine side effects (
p = 0.013), and COVID-19 vaccine development (
p < 0.001). Topics regarding how COVID-19 spreads (
p = 0.94) and being cautious in the public (
p = 0.138) did not show significant change. Of the knowledge items that showed overall statistical significance, when stratifying the participants into various demographic groups (
Table 3), those who identified as female improved their knowledge regarding post-vaccine behaviors compared to those who identified as male (
p = 0.014); those who identified as a different political affiliation other than republican, democratic, or independent improved their knowledge regarding COVID-19 vaccine development (
p = 0.016). Belief in COVID-19 vaccine efficacy (
p = 0.029) was most improved in those identified as republican compared to other political affiliations; and individuals whose employment status was affected by the pandemic also improved their knowledge of COVID-19 vaccine efficacy (
p = 0.043) compared to those whose employment status was not affected by the pandemic. No other demographic associations were seen among other knowledge items (Table A1).
Our data demonstrated that, overall, seven out of 29 attitude items showed statistically significant changes, and two out of 29-items showed meaningful trends. Results demonstrated that participants increased their trust in the vaccine (
p <0.001), increased their belief that the COVID-19 vaccine would benefit their body (
p = 0.012) (
Table 4). More had confidence that the COVID-19 vaccine underwent adequate testing (
p = 0.012), and more cited a source that they trust told them to receive a COVID-19 vaccine (
p =0.006). The results also showed significant reduction in negative misconceptions, such as less individuals believing that the vaccine was developed too quickly (
p = 0.016), reduced concerns about side effects of the vaccine (
p = 0.01) and the long-term effects of the vaccine (
p <0.001). Trends were observed in decreased concerns over knowing who to trust for COVID-19 information (
p = 0.057) and being worried about missing work to receive the vaccine (
p = 0.052). There was no statistical significance or meaningful trends in the other 21 attitude topics, such as concern about contracting the virus, belief in CDC recommendations, etc. (Table A2). Of the attitude items that showed overall statistical significance, when stratifying the participants into various demographic groups, those who identified as male (
p = 0.021) and individuals who reside in metropolitan areas (
p = 0.014) showed a greater decrease in concerns about the COVID-19 vaccine side effect (
Table 5). Also, those who identified as male (
p = 0.021), individuals who had never tested themselves for COVID-19 (
p = 0.038), and individuals with two more co-morbidities (
p = 0.002) showed a greater decrease in concerns about the long-term effects of the COVID-19 vaccines. Individuals with no co-morbidities increased their belief in the benefits of the COVID-19 vaccine (
p = 0.04); fewer individuals with two or more co-morbidities believed that the COVID-19 vaccine was developed too quickly (
p = 0.01); and, the more CDC precautions the individual followed, the more they were concerned about missing work due to the COVID-19 side effects (
p = 0.02). No other demographic associations were seen among other attitude items (Table A3).
The significant knowledge and attitude item changes by the participants’ vaccination status shows that individuals who were unvaccinated and hesitant regarding the COVID-19 vaccinations increased their knowledge the most in topics regarding vaccine effects (
p = 0.004) and COVID-19 vaccine efficacy (
p<0.001) (
Table 6). In addition, both unvaccinated groups increased their beliefs in the benefits of the COVID-19 vaccination after the intervention (
p = 0.011). No other demographic associations were seen among other knowledge and attitude items (Table A4).
However, those who received an infographic educational intervention were less concerned about the COVID-19 vaccine (p = 0.036) and the more CDC precautions an individual followed, the more likely they were to receive the COVID-19 vaccine (p = 0.03) (Table A5).
4. Discussion
4.1. The Impact and Role of Educational Interventions in Addressing Public Health Issues among Populations with Disproportionate Outcomes
Overall, the educational interventions have demonstrated positive outcomes, enhancing COVID-19 knowledge and attitudes while reducing misconceptions about vaccinations. A minor difference was observed between the video and infographic regarding concerns over the COVID-19 vaccine. This discrepancy may highlight the importance of cultural relevance in educational materials. For instance, the inclusion of a non-AI/AN infectious disease physician in the video may not have resonated strongly with AI/AN communities as culturally representative personnel would. Integrating cultural components into educational interventions can foster greater trust and engagement, ultimately enhancing their impact within AI/AN communities.
At the onset of the pandemic, AI/AN communities faced notably low vaccination rates. However, by April 2021, they had become the most vaccinated minority group, reflecting successful efforts by Tribal leadership to tailor vaccine distribution strategies to their community’s needs and leveraging existing trusted resources [
19,
20,
21]. Initiatives, such as the IHS’s COVID-19 Vaccine Task Force (VTF) and the involvement of native language speakers from the Cherokee and Navajo Nations played pivotal roles in educating community members about COVID-19 vaccine safety and efficacy [
22,
23]. Despite these achievements, vaccine hesitancy persists, influenced in part by historical experiences of infectious diseases like smallpox, tuberculosis, measles, and diphtheria since European contact in the 15th century, which have contributed to ongoing health disparities and mistrust within AI/AN communities [
11]. Various strategies are available in promoting uptake and decreasing vaccine hesitancy, with educational interventions, like the ones utilized in this study, serving as an additional tool in the toolbox alongside other resources such as native language speakers and community health educators. Initiatives such as the Diné (Navajo) Teachings and Public Health Students Informing Peers and Relatives about Vaccine Education (RAVE) intervention aim to address this hesitancy by serving as trusted messengers, delivering culturally relevant vaccine education [
24]. Leveraging the ethnic concordance of providers and patients, along with community health educators and Traditional Knowledge Holders utilizing the Hózhó Resilience Model, further enhances trust and empathy in healthcare interactions [
25,
26,
27].
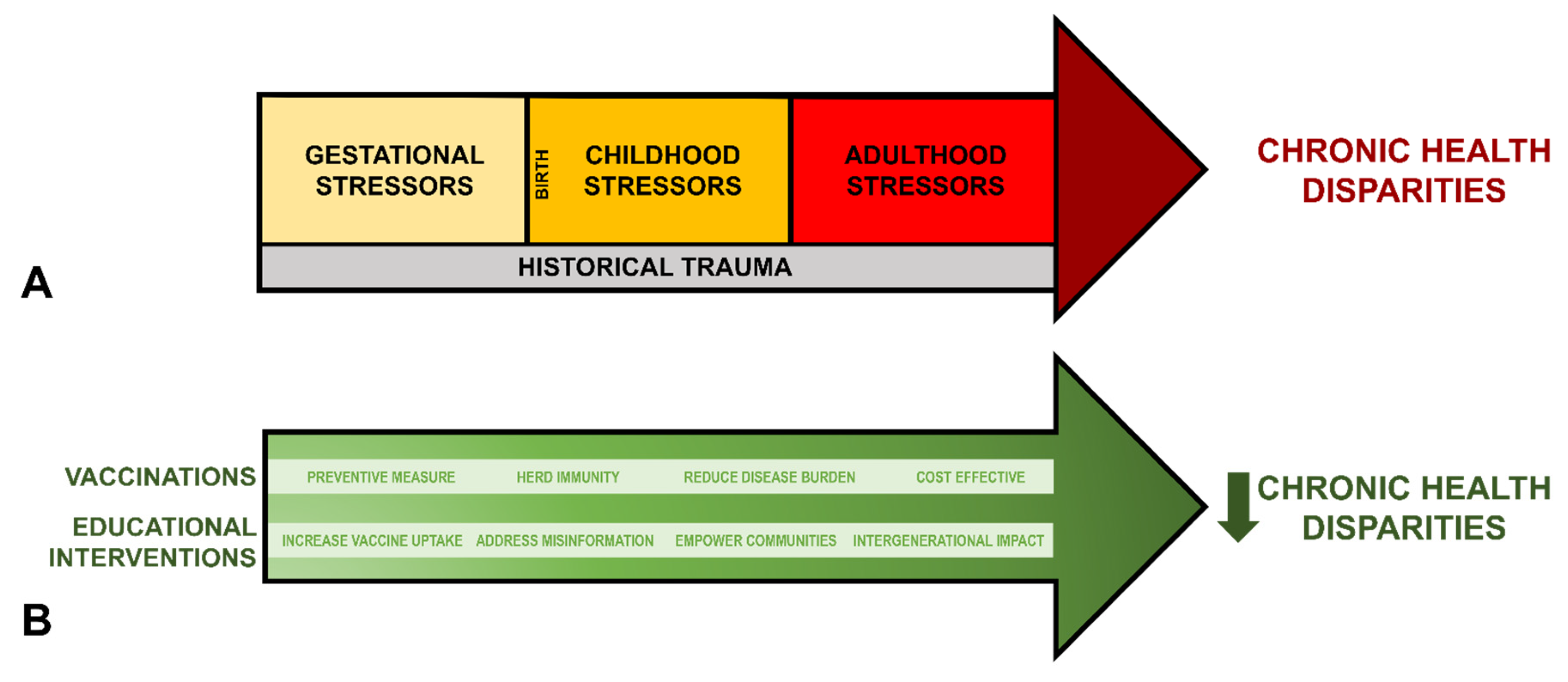
Derived from Warne and Lajimodiere,
Figure 3A summarizes the cumulative effects of historical trauma alongside gestational, childhood, and adulthood stressors on chronic disease disparities amongst the AI/AN populations [
28].
Figure 3B illustrates how vaccination and educational interventions counteract and reduce these disparities. Educational interventions represent a valuable tool in addressing public health challenges, providing targeted strategies to enhance health literacy, promote preventive healthcare behaviors, and address concerns surrounding factors contributing to chronic disease disparities. These interventions are often guided by theoretical frameworks, such as the Health Belief Model. This model emphasizes individual perceptions of susceptibility, severity, benefits, and barriers to health actions, helping tailor interventions to the specific needs and beliefs of AI/AN communities [
29]. By offering culturally sensitive and appropriate health education, these interventions empower individuals to make informed decisions about their health, advocate for their healthcare needs, and engage in preventative health measures, such as vaccination [
30,
31,
32,
33]. For example, previous culturally tailored interventions in smoking cessation have shown to be impactful among AI/AN populations [
34,
35]. Furthermore, educational initiatives have the potential to foster trust and collaboration between healthcare providers and AI/AN communities, facilitating more effective healthcare delivery and improving outcomes [
36,
37]. Through comprehensive educational efforts tailored to the historical and cultural contexts of AI/AN populations, these initiatives can contribute to reducing chronic disease disparities and promoting holistic well-being across generations.
4.2. Factors Influencing COVID-19 Attitudes and Knowledge: Gender, Political Affiliation, Place of Residence, Number of CDC Precautions Followed, and Number of Co-Morbidities
4.2.1. Gender
This study identified females as having greater concerns about challenges in accessing vaccination sites and arranging care for dependents to receive the vaccine, as well as showing a greater improvement in knowledge of post-vaccine behaviors after the educational intervention. However, there was no significant change in vaccination status compared to males. Although previous studies have found that females and parents were more likely to avoid the COVID-19 vaccine, this study showed no statistically significant differences in vaccination status when stratifying by gender [
38,
39]. The studies which demonstrate females having lower COVID-19 vaccination rates are correlated with potential side effects of the vaccination. Many studies have demonstrated that biological females have a more robust immune response to vaccination and, subsequently, stronger side effects compared to biological males [
40,
41,
42]. In turn, these side effects may compromise the parents’ ability to care for their dependents [
38,
43]. The differences in concern of the vaccine side effects can also be contributed to societal factors, such as historical medical mistrust and lack of female representation in the healthcare system [
43,
44]. The rates of medical mistrust and vaccination hesitancy have only increased following the COVID-19 pandemic [
45,
46]. While this study did not show statistically significant differences amongst vaccination status, addressing these biological and societal concerns regarding vaccination side effects during educational interventions can help build trust amongst female patients.
4.2.2. Political Affiliation
According to the American Research Collaborative, Native Americans predominantly voted for the democratic party over the republican party [
47]. Our study found that those who identified as republican improved their knowledge regarding COVID-19 vaccine efficacy the most compared to other political affiliations after the educational intervention. In contrast, those who identified with a political affiliation other than republican, democratic, or independent demonstrated significant improvement in their knowledge regarding COVID-19 vaccine development. The politicization of the COVID-19 pandemic played a substantial role in shaping public perception regarding vaccination. While our study did not reveal any differences in attitudes or vaccination status amongst political affiliations, several studies have shown that those identifying with republican ideologies are less likely to be vaccinated against COVID-19, have higher rates of vaccine hesitancy, and be less amenable to other public health efforts, such as masking, compared to other political affiliations [
15,
48,
49,
50]. In addition, a study in France found that those who voted for far left or far right political candidates, or those who did not vote at all, were significantly more likely to refuse the vaccine [
51]. The relationship between political affiliations, public health behaviors, and vaccine acceptance is complex and highlights the need for targeted interventions and inclusive messages to ensure widespread vaccine uptake and mitigate the impact of political polarization in public health initiatives.
4.2.3. Place of Residence
Population density affects access to healthcare resources, which in turn impacts vaccination status. Studies have demonstrated disparities in vaccination among the AI/AN communities, with individuals residing in rural areas facing additional accessibility challenges [
12,
52]. Although our study did not show differences among vaccination status in micropolitan versus metropolitan areas, this study did find that individuals who resided in metropolitan areas were less concerned about the COVID-19 vaccine side effects. Studies have shown that metropolitan areas are associated with higher vaccination rates compared to micropolitan areas due to variables, such as better healthcare infrastructure, accessibility to vaccination sites, and differences in socioeconomic status and education levels [
53,
54]. Recognizing these unique challenges is critical in implementing effective interventions in rural and micropolitan areas.
4.2.4. Number of CDC Precautions Followed
Throughout the pandemic, the CDC released various precautions to help the public limit the spread of the virus, such as social distancing and hand washing. Prior studies have shown that those who had never smoked before compared to former smokers were significantly less adherent to masking [
55]. Native Americans are at a 32% higher of smoking or being exposed to smoke compared to other ethnic groups, suggesting a potential association between smoking habits and adherence to preventive measures [
56]. The CDC also endorsed handwashing as a preventative measure, which has also been shown to be a common precaution practiced by adults across the United States [
57]. Our study also revealed that handwashing was the most reported precaution amongst our participants. In addition, our study revealed that individuals who followed more precautions were more likely to be worried about missing work due to vaccine side effects and were more likely to get vaccinated. Their commitment to preventive measures may suggest a proactive approach to health protection to both them and others. In addition, individuals may perceive potential vaccination side effects as a hindrance to their daily responsibilities, such as missing work. One study demonstrated the risk of staff shortages due to inability to work after COVID-19 vaccine boosters [
58]. This correlation of adherence to more precautions and missing work may reflect broader on the balance of personal well-being, general public health, and professional commitments—additional factors to consider when implementing public health initiatives.
4.2.5. Number of Co-Morbidities
While our study revealed only one significant change in knowledge amongst number of co-morbidities, individuals without co-morbidities acknowledged more benefits of the vaccination compared to those with co-morbidities. Furthermore, individuals with two or more co-morbidities exhibited decreased negative perceptions of COVID-19 compared to those with one or no co-morbidities. Given that AI/AN exhibit lower life expectancy than most other ethnic groups, partly due to an increased likelihood of obesity and diabetes, addressing misconceptions and promoting positive attitudes towards COVID-19 vaccination becomes imperative [
33,
59,
60]. According to the Great Lakes Inter-Tribal Epidemiology Center 2021 report of AI/AN in Michigan, Minnesota, and Wisconsin, AI/AN individuals reported having higher prevalence of hypertension at 35.7% and diabetes at 16% compared to their White counterparts in this three-state area [
61]. During the peak of the pandemic, pre-existing co-morbidities, such as obesity and diabetes, were reported as factors that led to more severe COVID-19 outcomes [
62,
63]. Therefore, targeted interventions that address concerns and promote vaccination uptake, especially among individuals with co-morbidities, can play a pivotal role in reducing the disproportionate impact of COVID-19 on AI/AN communities.
4.3. Limitations
The logistical challenges encountered during the study led to a prolonged data collection timeline. Throughout this period, various pandemic-related factors, such as the emergence of new COVID-19 strain variants, fluctuations in COVID-19 cases, the introduction of booster shot recommendations, and changes in recommendations by public health leaders, potentially impacted the participants’ opinions over time. Although efforts were made to ensure demographic diversity, the study population consisted primarily of patients from a single IHS center, potentially introducing selection bias and limiting generalizability.
The surveys were distributed at the clinic, which excludes individuals facing significant transportation barriers and those who may not be eligible for IHS services. Additionally, the surveys required individuals to be literate in English and were administered on either an iPad or Smartphone device, further limiting the study’s inclusivity by excluding non-English speaking individuals and those with limited proficiency in technology.
Furthermore, while the educational intervention was approved by the tribal council, it did not incorporate any cultural components, potentially limiting its effectiveness within AI/AN communities. It’s also worth noting that the clinic conducted extensive COVID-19 vaccination efforts, including setting up clinics at multiple locations, working with the local health department, and conducting targeted outreach and publicity campaigns. These comprehensive efforts to promote vaccination, including walk-in clinics and public relations activities, may have influenced the study population’s attitudes and behaviors regarding COVID-19 vaccination independently of our educational intervention. Despite these limitations, the study addresses several gaps in previous research, including the longitudinal assessment of intervention effects and the comparison of different educational modalities.
5. Conclusions
This study conducted at a single IHS clinic in central Michigan illustrates the critical role of educational interventions in addressing vaccine hesitancy among AI/AN populations, especially amidst the challenges posed by the COVID-19 pandemic.
One key finding of the study is the comparable effectiveness of both the video and infographic interventions in increasing COVID-19 knowledge among participants. This suggests that investments in either modality could yield positive outcomes. However, it’s crucial to consider potential barriers for individuals associated with each intervention, such as hearing or vision impairments for videos and reading impairments for infographics. Addressing these barriers through accessible formats or alternative modalities can enhance inclusivity and effectiveness of educational interventions.
Furthermore, the historical underfunding of IHS underscores the urgent need for increased financial support and allocation of resources towards interventions tailored to AI/AN populations [
64,
65]. Investing in educational initiatives, community educators, native language speakers, and Traditional Knowledge Holders can address healthcare disparities and promote health equity within these communities. By bolstering funding from culturally sensitive interventions, policymakers and healthcare leaders can take proactive steps towards improving healthcare access and outcomes for AI/AN populations.
While this study provides valuable insights into the effectiveness of educational interventions, it also highlights the importance of addressing barriers, integrating cultural components, and advocating for increased funding to ensure equitable healthcare outcomes.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on
Preprints.org. Video S1: Video educational intervention; Infographic S1: Infographic educational intervention.
Author Contributions
Conceptualization, M.A.T. and N.R.; methodology, M.A.T. and N.R.; formal analysis; M.A.T. and S.Z., investigation, M.A.T., S.T.R., J.H.K., M.K., S.S., C.M., A.S.K., A.C., C.B., B.K.; data curation, M.A.T. and S.Z.; writing—original draft preparation, M.A.T., S.T.R., C.M., A.S.C., A.C..; writing—review and editing, M.A.T., S.Z., N.R.; visualization, M.A.T.; supervision, M.A.T. and N.R.; project administration, M.A.T. and N.R.; funding acquisition, M.A.T. and N.R.. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported in part by the Michigan State Medical Society Foundation, grant number P64840, and Blue Cross Blue Shield of Michigan, grant number 2022010089.SAP.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Central Michigan University (Protocol 2021-1028 on December 2, 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Acknowledgments
The authors express their profound gratitude to the following individuals: Lisa Mun and Katharine Keener for their data collection efforts; Michael Huber, MD for securing clinic approval for data collection; Nicholas Haddad, MD for his expertise in infectious diseases and contribution to the educational interventions; and, Donald Blubaugh for creating and refining the videographic informational intervention. We also extend our sincere thanks to the anonymous Indian Health Service clinic for their cooperation.
Conflicts of Interest
The authors declare no conflicts of interest.
| 1 |
Mean values that show a value closer to 0 indicate an incorrect response, 1 indicates a partially correct response, and 2 indicates a completely correct response. |
| 2 |
Mean values that show a value closer to 0 indicate “disagree” and 2 indicates “agree”. |
| 3 |
The “Unvaccinated, hesitated” individuals include those who selected “Definitely will not,” “Very unlikely,” and “Somewhat unlikely” to the question, “If given the opportunity to take a COVID-19 vaccine, how likely is it that you would get the vaccine/shot?” |
| 4 |
The “Unvaccinated, not hesitant” individuals include those who selected “Somewhat likely,” “Very likely,” and, “Definitely will”; the “vaccinated” individuals include those who received one or more COVID-19 vaccinations. |
References
- C. Grills et al., “Applying culturalist methodologies to discern COVID-19’s impact on communities of color,” (in eng), J Community Psychol, vol. 51, no. 6, pp. 2331-2354, Jul 2023. [CrossRef]
- M. Y. Brave Heart et al., “Psychiatric disorders and mental health treatment in American Indians and Alaska Natives: results of the National Epidemiologic Survey on Alcohol and Related Conditions,” (in eng), Soc Psychiatry Psychiatr Epidemiol, vol. 51, no. 7, pp. 1033-46, Jul 2016. [CrossRef]
- M. L. Castor, M. S. Smyser, M. M. Taualii, A. N. Park, S. A. Lawson, and R. A. Forquera, “A nationwide population-based study identifying health disparities between American Indians/Alaska Natives and the general populations living in select urban counties,” (in eng), Am J Public Health, vol. 96, no. 8, pp. 1478-84, Aug 2006. [CrossRef]
- S. M. Manson, J. Beals, S. A. Klein, C. D. Croy, and A.-S. Team, “Social epidemiology of trauma among 2 American Indian reservation populations,” (in eng), Am J Public Health, vol. 95, no. 5, pp. 851-9, May 2005. [CrossRef]
- C. A. Wong et al., “American Indian and Alaska Native infant and pediatric mortality, United States, 1999-2009,” (in eng), Am J Public Health, vol. 104 Suppl 3, no. Suppl 3, pp. S320-8, Jun 2014. [CrossRef]
- M. A. Herne, M. L. Bartholomew, and R. L. Weahkee, “Suicide mortality among American Indians and Alaska Natives, 1999-2009,” (in eng), Am J Public Health, vol. 104 Suppl 3, no. Suppl 3, pp. S336-42, Jun 2014. [CrossRef]
- M. Landen, J. Roeber, T. Naimi, L. Nielsen, and M. Sewell, “Alcohol-attributable mortality among American Indians and Alaska Natives in the United States, 1999-2009,” (in eng), Am J Public Health, vol. 104 Suppl 3, no. Suppl 3, pp. S343-9, Jun 2014. [CrossRef]
- M. Veazie, C. Ayala, L. Schieb, S. Dai, J. A. Henderson, and P. Cho, “Trends and disparities in heart disease mortality among American Indians/Alaska Natives, 1990-2009,” (in eng), Am J Public Health, vol. 104 Suppl 3, no. Suppl 3, pp. S359-67, Jun 2014. [CrossRef]
- T. Murphy, P. Pokhrel, A. Worthington, H. Billie, M. Sewell, and N. Bill, “Unintentional injury mortality among American Indians and Alaska Natives in the United States, 1990-2009,” (in eng), Am J Public Health, vol. 104 Suppl 3, no. Suppl 3, pp. S470-80, Jun 2014. [CrossRef]
- D. K. Espey et al., “Leading causes of death and all-cause mortality in American Indians and Alaska Natives,” (in eng), Am J Public Health, vol. 104 Suppl 3, no. Suppl 3, pp. S303-11, Jun 2014. [CrossRef]
- D. A. Henderson et al., “Smallpox as a biological weapon: medical and public health management. Working Group on Civilian Biodefense,” (in eng), JAMA, vol. 281, no. 22, pp. 2127-37, Jun 09 1999. [CrossRef]
- S. M. Hatcher et al., “COVID-19 Among American Indian and Alaska Native Persons—23 States, January 31-July 3, 2020,” (in eng), MMWR Morb Mortal Wkly Rep, vol. 69, no. 34, pp. 1166-1169, Aug 28 2020. [CrossRef]
- J. Arrazola et al., “COVID-19 Mortality Among American Indian and Alaska Native Persons—14 States, January-June 2020,” (in eng), MMWR Morb Mortal Wkly Rep, vol. 69, no. 49, pp. 1853-1856, Dec 11 2020. [CrossRef]
- D. Allington, B. Duffy, S. Wessely, N. Dhavan, and J. Rubin, “Health-protective behaviour, social media usage and conspiracy belief during the COVID-19 public health emergency,” (in eng), Psychol Med, vol. 51, no. 10, pp. 1763-1769, Jul 2021. [CrossRef]
- J. Khubchandani, S. Sharma, J. H. Price, M. J. Wiblishauser, M. Sharma, and F. J. Webb, “COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment,” (in eng), J Community Health, vol. 46, no. 2, pp. 270-277, 04 2021. [CrossRef]
- M. Clinic, “Herd immunity and COVID-19.
- (coronavirus): What you need to know,” ed, 2021.
- “Michigan Department of Health & Human Services.” https://www.michigan.gov/documents/coronavirus/MI_COVID-19_Vaccination_Prioritization_Guidance_710349_7.pdf. (accessed.
- M. A. Takagi et al., “The impact of educational interventions on COVID-19 and vaccination attitudes among patients in Michigan: A prospective study,” (in eng), Front Public Health, vol. 11, p. 1144659, 2023. [CrossRef]
- C. f. D. C. a. Prevention. US Department of Health and Human Services, CDC. ttps://covid.cdc.gov/covid-data-tracker (accessed April 5, 2021).
- G. Sears et al., “Building Trust and Awareness to Increase AZ Native Nation Participation in COVID-19 Vaccines,” (in eng), Int J Environ Res Public Health, vol. 20, no. 1, Dec 20 2022. [CrossRef]
- R. Treisman. “https://www.npr.org/sections/coronavirus-live-updates/2021/04/26/990884991/outpacing-the-u-s-hard-hit-navajo-nation-has-vaccinated-more-than-half-of-adults.” NPR. https://www.npr.org/sections/coronavirus-live-updates/2021/04/26/990884991/outpacing-the-u-s-hard-hit-navajo-nation-has-vaccinated-more-than-half-of-adults (accessed April 26, 2021).
- U. S. D. o. H. a. H. Services, “Indian Health Service: COVID-19 Pandemic Vaccine Plan November 2020,” ed, 2020.
- H. Kaur. “Tribal health providers have figured out the key to Covid-19 vaccine success. Here’s their secret.” https://www.cnn.com/2021/02/09/us/tribal-health-providers-covid-vaccine-trnd/index.html (accessed February 26, 2021, 2021).
- M. Tutt et al., “Diné teachings and public health students informing peers and relatives about vaccine education: Providing Diné (Navajo)-centered COVID-19 education materials using student health messengers,” (in eng), Front Public Health, vol. 10, p. 1046634, 2022. [CrossRef]
- J. Takeshita et al., “Association of Racial/Ethnic and Gender Concordance Between Patients and Physicians With Patient Experience Ratings,” (in eng), JAMA Netw Open, vol. 3, no. 11, p. e2024583, Nov 02 2020. [CrossRef]
- M. Kahn-John, “The path to development of the Hózhó Resilience Model for nursing research and practice,” (in eng), Appl Nurs Res, vol. 29, pp. 144-7, Feb 2016. [CrossRef]
- M. V. Geana, K. A. Greiner, A. Cully, M. Talawyma, and C. M. Daley, “Improving health promotion to American Indians in the midwest United States: preferred sources of health information and its use for the medical encounter,” (in eng), J Community Health, vol. 37, no. 6, pp. 1253-63, Dec 2012. [CrossRef]
- D. Warne and D. Lajimodiere, “American Indian health disparities: psychosocial influences,” Social and Personality Psychology Compass, vol. 9/10, pp. 567–579, 2015. [CrossRef]
- C. L. Jones, J. D. Jensen, C. L. Scherr, N. R. Brown, K. Christy, and J. Weaver, “The Health Belief Model as an explanatory framework in communication research: exploring parallel, serial, and moderated mediation,” (in eng), Health Commun, vol. 30, no. 6, pp. 566-76, 2015. [CrossRef]
- T. D. Noe, C. E. Kaufman, L. J. Kaufmann, E. Brooks, and J. H. Shore, “Providing culturally competent services for American Indian and Alaska Native veterans to reduce health care disparities,” (in eng), Am J Public Health, vol. 104 Suppl 4, no. Suppl 4, pp. S548-54, Sep 2014. [CrossRef]
- S. M. Manson and D. S. Buchwald, “Aging and Health of American Indians and Alaska Natives: Contributions from the Native Investigator Development Program,” (in eng), J Aging Health, vol. 33, no. 7-8_suppl, pp. 3S-9S, 2021. [CrossRef]
- W. F. Denetclaw et al., “Diné Navajo Resilience to the COVID-19 pandemic,” (in eng), PLoS One, vol. 17, no. 8, p. e0272089, 2022. [CrossRef]
- “StatPearls,” 2024.
- M. Santiago-Torres et al., “Efficacy and Utilization of Smartphone Applications for Smoking Cessation Among American Indians and Alaska Natives: Results From the iCanQuit Trial,” (in eng), Nicotine Tob Res, vol. 24, no. 4, pp. 544-554, Mar 01 2022. [CrossRef]
- W. S. Choi et al., “All Nations Breath of Life: A Randomized Trial of Smoking Cessation for American Indians,” (in eng), Am J Prev Med, vol. 51, no. 5, pp. 743-751, Nov 2016. [CrossRef]
- L. R. Thomas, D. M. Donovan, R. L. Sigo, L. Austin, G. A. Marlatt, and S. Tribe, “The Community Pulling Together: A Tribal Community–University Partnership Project to Reduce Substance Abuse and Promote Good Health in a Reservation Tribal Community,” (in eng), J Ethn Subst Abuse, vol. 8, no. 3, pp. 283-300, 2009. [CrossRef]
- R. Idoate et al., “Urban American Indian Community Health Beliefs Associated with Addressing Cancer in the Northern Plains Region,” (in eng), J Cancer Educ, vol. 36, no. 5, pp. 996-1004, Oct 2021. [CrossRef]
- A. Dror et al., “Vaccine hesitancy: the next challenge in the fight against COVID-19,” (in eng), Eur J Epidemiol, vol. 35, no. 8, pp. 775-779, Aug 2020. [CrossRef]
- S. Zintel, C. S. Zintel, C. Flock, A. L. Arbogast, A. Forster, C. von Wagner, and M. Sieverding, “Gender differences in the intention to get vaccinated against COVID-19: a systematic review and meta-analysis,” (in eng), Z Gesundh Wiss, pp. 1-25, Jan 07 2022. [CrossRef]
- S. L. Klein and A. Pekosz, “Sex-based biology and the rational design of influenza vaccination strategies,” (in eng), J Infect Dis, vol. 209 Suppl 3, no. Suppl 3, pp. S114-9, Jul 15 2014. [CrossRef]
- T. Galbadage et al., “Systematic Review and Meta-Analysis of Sex-Specific COVID-19 Clinical Outcomes,” (in eng), Front Med (Lausanne), vol. 7, p. 348, 2020. [CrossRef]
- C. Vitale, M. Fini, I. Spoletini, M. Lainscak, P. Seferovic, and G. M. Rosano, “Under-representation of elderly and women in clinical trials,” (in eng), Int J Cardiol, vol. 232, pp. 216-221, Apr 01 2017. [CrossRef]
- E. Conis, “A mother’s responsibility: women, medicine, and the rise of contemporary vaccine skepticism in the United States,” (in eng), Bull Hist Med, vol. 87, no. 3, pp. 407-35, 2013. [CrossRef]
- T. A.-P. G. i. H. A. W. Group, “GENDER AND COVID-19 VACCINES Listening to women-focused organizations in Asia and the Pacific,” a. V. Gender-Based Violence Area of Responsibility, Ed., ed. UN Women, 2021, p. 16.
- B. Spires, A. Brewton, J. M. Maples, S. F. Ehrlich, and K. B. Fortner, “Vaccine Hesitancy in Women’s Health,” (in eng), Obstet Gynecol Clin North Am, vol. 50, no. 2, pp. 401-419, Jun 2023. [CrossRef]
- L. A. Kassi, A. K. Lawson, E. C. Feinberg, A. Swanson, S. Shah, and M. Pavone, “Vaccine hesitancy, distress, and medical mistrust in women considering or undergoing fertility treatment during the COVID-19 pandemic,” (in eng), J Assist Reprod Genet, vol. 39, no. 12, pp. 2767-2776, Dec 2022. [CrossRef]
- A. R. Collaborative. “2022 Midterm Voter Election Poll: Native American Voters.” African American Research Collaborative. https://2022electionpoll.us/wp-content/uploads/2022/11/7-Midterm-Survey-NativeAm-National-Crosstab.pdf (accessed.
- J. D. Allen et al., “Medical mistrust, discrimination, and COVID-19 vaccine behaviors among a national sample U.S. adults,” (in eng), SSM Popul Health, vol. 20, p. 101278, Dec 2022. [CrossRef]
- K. F. Foundation. “arge Majorities Now Say they Wear Masks Regularly and can Continue Social Distancing for at least Six Months if Needed, though Republicans Remain Less Likely to Take Such Precautions.” Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/press-release/poll-large-majorities-now-say-they-wear-masks-regularly-and-can-continue-social-distancing-for-at-least-six-months-if-needed-though-republicans-remain-less-likely-to-take-such-precautions/ (accessed 2021).
- S. R. Neely, C. Eldredge, R. Ersing, and C. Remington, “Vaccine Hesitancy and Exposure to Misinformation: a Survey Analysis,” (in eng), J Gen Intern Med, vol. 37, no. 1, pp. 179-187, Jan 2022. [CrossRef]
- C. Group, “A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation,” (in eng), Lancet Infect Dis, vol. 20, no. 7, pp. 769-770, Jul 2020. [CrossRef]
- J. D. Hanson, K. Oziel, A. Harris, M. Sarche, M. O’Leary, and D. Buchwald, “Adaptations of an RCT during COVID: Case Study in one Rural American Indian Community,” (in eng), Collaborations (Coral Gables), vol. 5, no. 1, 2022. [CrossRef]
- H. B. Nguyen et al., “Knowledge, Attitudes, Practices, and Related Factors Towards COVID-19 Prevention Among Patients at University Medical Center Ho Chi Minh City, Vietnam,” (in eng), Risk Manag Healthc Policy, vol. 14, pp. 2119-2132, 2021. [CrossRef]
- E. H. Hassan et al., “Knowledge, attitudes, and practices toward COVID-19 prevention in Yemen: a community-based cross-sectional study,” (in eng), Front Public Health, vol. 11, p. 1178183, 2023. [CrossRef]
- L. Szapary, J. C. Avila, M. A. Monnig, A. W. Sokolovsky, G. DeCost, and J. S. Ahluwalia, “Adherence to COVID-19 Guidelines among Current, Former, and Never Smokers,” (in eng), Am J Health Behav, vol. 46, no. 4, pp. 442-455, Sep 01 2022. [CrossRef]
- J. B. Unger, S. Shakib, T. B. Cruz, B. R. Hoffman, B. H. Pitney, and L. A. Rohrbach, “Smoking behavior among urban and rural Native American adolescents in California,” (in eng), Am J Prev Med, vol. 25, no. 3, pp. 251-4, Oct 2003. [CrossRef]
- L. G. Brown, E. R. Hoover, C. E. Barrett, K. L. Vanden Esschert, S. A. Collier, and A. G. Garcia-Williams, “Handwashing and disinfection precautions taken by U.S. adults to prevent coronavirus disease 2019, Spring 2020,” (in eng), BMC Res Notes, vol. 13, no. 1, p. 550, Dec 04 2020. [CrossRef]
- J. Reusch et al., “Inability to work following COVID-19 vaccination-a relevant aspect for future booster vaccinations,” (in eng), Public Health, vol. 222, pp. 186-195, Sep 2023. [CrossRef]
- E. J. Tomayko et al., “Healthy Children, Strong Families 2: A randomized controlled trial of a healthy lifestyle intervention for American Indian families designed using community-based approaches,” (in eng), Clin Trials, vol. 14, no. 2, pp. 152-161, Apr 2017. [CrossRef]
- S. Sigvardsson, M. Bohman, and C. R. Cloninger, “Replication of the Stockholm Adoption Study of alcoholism. Confirmatory cross-fostering analysis,” (in eng), Arch Gen Psychiatry, vol. 53, no. 8, pp. 681-7, Aug 1996. [CrossRef]
- G. L. I.-T. E. Center, “American Indian/Alaska Native Health in Michigan, Minnesota,and Wisconsin 2021,” ed. Lac du Flambeau, WI: Great Lakes Inter-Tribal Council, Inc., 2021.
- B. M. Popkin et al., “Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships,” (in eng), Obes Rev, vol. 21, no. 11, p. e13128, Nov 2020. [CrossRef]
- J. Xie et al., “Metabolic Syndrome and COVID-19 Mortality Among Adult Black Patients in New Orleans,” (in eng), Diabetes Care, vol. 44, no. 1, pp. 188-93, Aug 25 2020. [CrossRef]
- T. D. Sequist, T. Cullen, K. Bernard, S. Shaykevich, E. J. Orav, and J. Z. Ayanian, “Trends in quality of care and barriers to improvement in the Indian Health Service,” (in eng), J Gen Intern Med, vol. 26, no. 5, pp. 480-6, May 2011. [CrossRef]
- K. J. Cromer, L. Wofford, and D. K. Wyant, “Barriers to Healthcare Access Facing American Indian and Alaska Natives in Rural America,” (in eng), J Community Health Nurs, vol. 36, no. 4, pp. 165-187, 2019. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).