1. Introduction
Body composition assessment and research emerged together with obesity and related chronic diseases increase in the mid-1970s, as well as with the identification of sarcopenia as a relevant health concern in the late 1980s [
1]. Since then, a wide range of techniques have been developed trying to accurately assess body composition (i.e. body fat and muscle mass) in children/teenagers, adults, and elders. Of note, valid and accurate body composition assessment is essential for diagnostic and clinical purposes in health and disease [
2].
There are some powerful and accurate reference methods to distinguish body mass components, such as underwater weighing, air replacement plethysmography, neutron activation analysis, computed tomography, and dual energy x-ray densitometry (DXA) [
3]. Among these, DXA is widely used as a gold standard reference method to assess accuracy and agreement of other methods [
4,
5,
6,
7,
8].
In clinical settings, such as nutritional evaluation, ambulatory visits, as well as in sports, fitness or wellness contexts, a wide range of indirect methods have been used to assess body fat percentage due to their low cost, they are less time-consuming, transportable, and have no side effects [
3]. The most used indirect methos include calculation by analytical formulas from simple anthropometric traits, and caliper testing. Of note, bioelectrical impedance (BIA) and ultrasound (US) scanning have gained attention in clinical and research studies [
3,
6].
BIA devices are generally simple to use, inexpensive, and avoid radiation exposure. This method is based on the electrical properties of the body and determines the resistance resulting from an electrical current passing through the body. The subject’s weight, height, and age are considered to estimate total body water. Then, it applies specific equations to determine the body fat percentage (BF%) [
4]. US techniques have also become common in the last decade. These devices identify adipose tissue using ultrasound waves that travel into body tissues. This method is non-invasive and non-traumatizing to the subject [
9]. Thus, BIA and US have been proposed as a possible alternative to assess and monitor BF% in the general population.
However, both BIA and US are not free from potential bias. Once they are indirect methods, several factors may influence the result. Height, sex, age, ethnicity, total body water, body sites of US measure (protocol), nutritional status, and physical activity are among possible confounding variables to the measurements [
3,
9]. Furthermore, several equipment models are available which makes it difficult to establish standard protocols. In this sense, validation, and agreement of these equipment with gold standard methods are still required.
The present study aimed to assess agreement of measurement of BF% obtained by a tetrapolar bioimpedance analyzer and an A-mode US scanner using a three-site protocol compared to DXA in a group of male college students.
2. Materials and Methods
2.1. Participants and Study Design
This is a cross-sectional study. A convenience sample of healthy male college students were recruited to participate. Inclusion criteria was to be enrolled in any undergrad or graduate course at the university. Data collection occurred in the Image Laboratory of the Faculty of Physical Education. All men who volunteered to participate and gave informed consent were included in the study. Twenty-three subjects completed all the analysis.
2.2. BF% Assessment
All subjects underwent BF% assessment at morning time, between 9h and 11h, in the following order: BIA, US, and DXA. Volunteers were dressed in light clothes and were instructed to remove all jewelry and metals prior to examinations. A tetrapolar BIA device was used in this study (OMROM HBF 514-C®) to assess body weight and BF%. Height of the participants was also evaluated using a wall stadiometer, and body mass index (BMI) was derived from Quetelet’s formula (Weight/Heigth2).
An A-mode, 2.5 MHz, portable US device (BodyMetrix BX2000
® system, Intela Metrix, Concord, CA, USA) was used. The US emits high-frequency sound waves to penetrate body tissues. Differentiation of body tissue interfaces is determined based on thickness of tissue and the length of time it takes for the ultrasonic waves to pass through and reflect back into the transducer [
6]. Measure was performed according to manufacturing instructions. A thin layer of US gel was applied to the probe and then placed perpendicular to the point of skin contact at each site. The Bodyview
® software (IntelaMetrix, Concord, CA, USA) was used to analyze images and to measure thickness of adipose tissue at each site. BF% was derived using the adapted Jackson–Pollock three-site protocol (chest, abdomen, and thigh).
DXA derived BF% was measured using a Lunar densitometry, model DPX (General Eletric-GE, Rommelsdorf, Germany). The equipment was daily calibrated according to manufacturer instructions. Participants were instructed to lie quietly in a supine position with their arms at their sides on the scanning bed. Scanning of the entire body was performed.
2.3. Statistical Analysis
Normality of data was assessed using the Shapiro Wilk test. All BF% measures presented parametric distribution. Correlations between BMI, BIA, US, and DXA derived BF% were analyzed with the Pearson coefficient, and the Concordance correlation coefficient (simple agreement analysis). One sample T-test was used to compare the mean differences between BF% derived from DXA and the other methods (DXA – BIA, and DXA – US). The Bland-Altman plots were used to analyze agreement between DXA and BIA, as well as between DXA and US. Limits of agreement were set at a confidence and agreement level of 95%. A linear regression analysis was used to investigate proportion bias related to BIA and US when compared to DXA. All analysis was done using the software Jamovi for windows, version 2.3.28.
3. Results
Descriptive characteristics of the subjects, as well as the measured BF% from DXA, BIA, and US are presented in
Table 1. Mean BMI showed that the sample was slightly overweight.
BF% derived by BIA and US were highly correlated with DXA (
Table 2). BMI was also highly correlated with all BF% methods (r = 0.85; 0.93; and 0.84 for DXA, BIA and US, respectively. All p < .001).
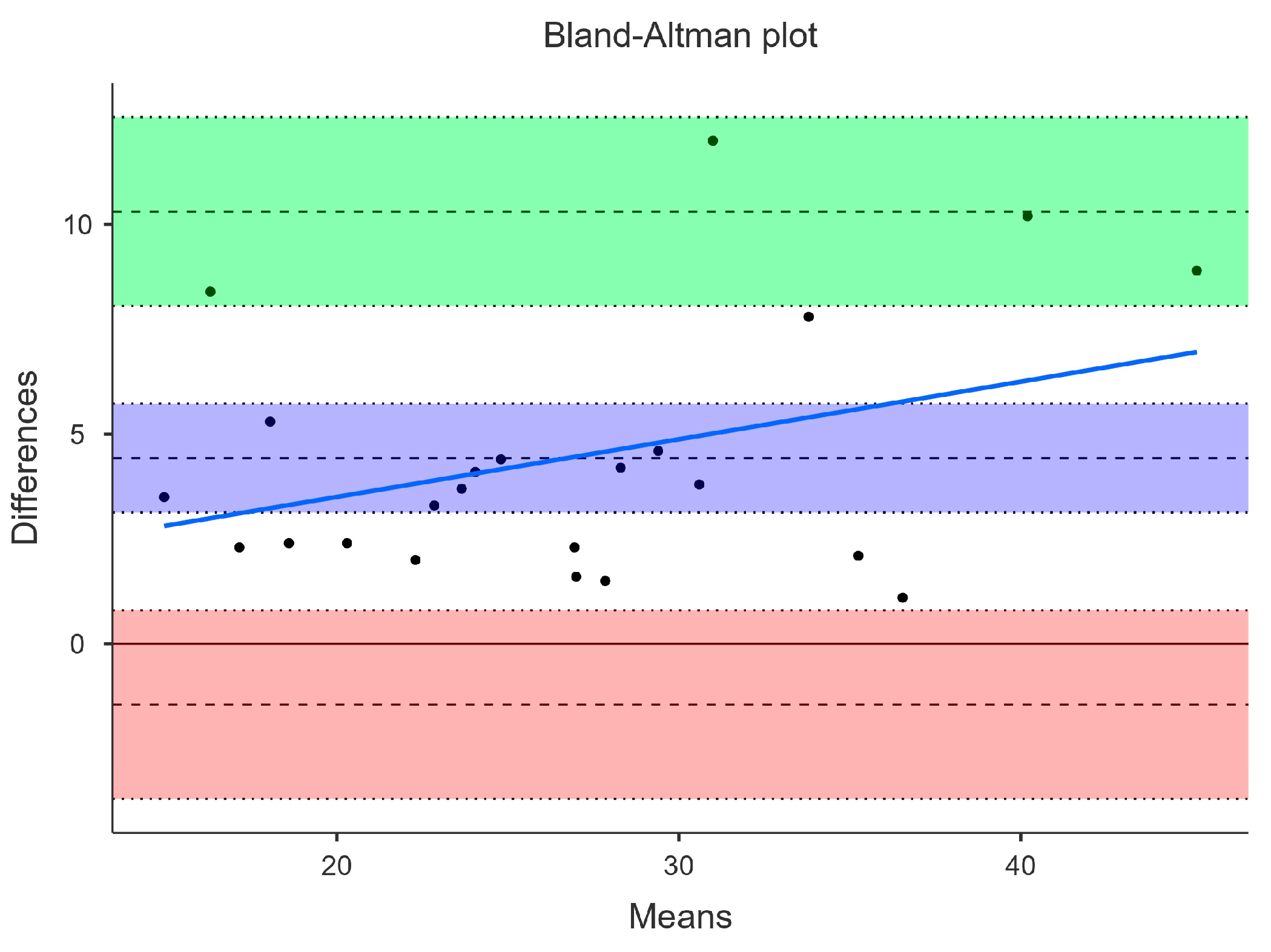
3.1. Agreement between DXA and BIA
Concordance correlation coefficient was high for BIA (0.80). Yet, BF% measured by BIA (24.5 ± 7.5) was on average 4.4% lower than DXA (29.0 ± 8.5). This mean difference was statistically significant (p < .001). Bland-Altman plot showed very large limits of agreement between DXA and BIA. Lower and upper agreement limits were -1.45 (95% CI -3.70 – 0.80) and 10.31 (95% CI 8.06 – 12.56). There was a tendency of BIA to underestimate BF%, especially among those with higher BF%, as shown by the blue proportional bias line in
Figure 1. Linear regression confirmed this tendency of proportional bias of both BIA (p = .09) to underestimate BF% when compared to DXA.
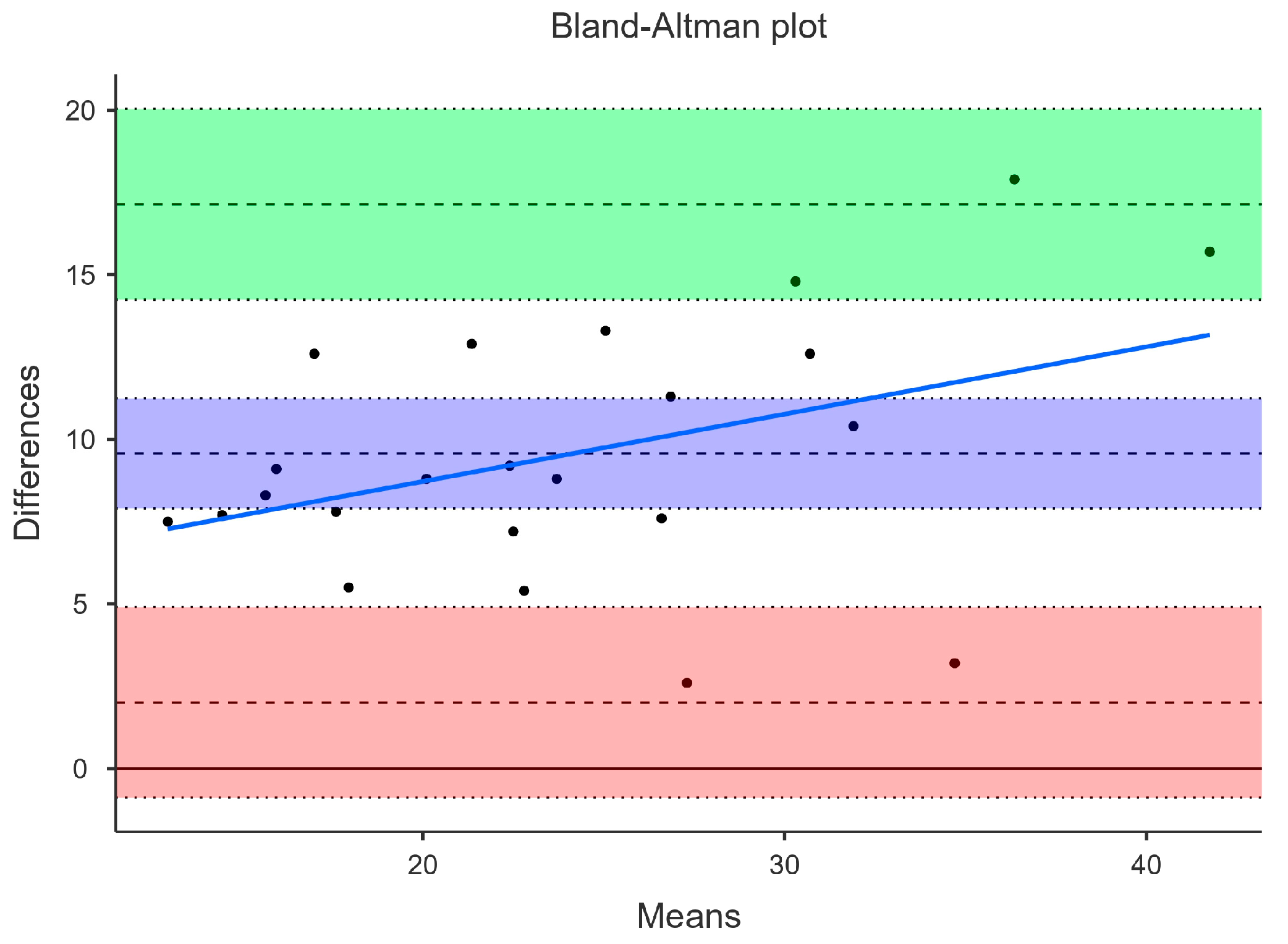
3.1. Agreement between DXA and US
Concordance correlation coefficient was moderate for US (0.49). BF% measured by US (19.4 ± 7.0) was on average 9.6% lower than DXA (29.0 + 8.5%). This mean difference was statistically significant (p < .001). Bland-Altman plot showed very large limits of agreement between DXA and US. Lower and upper agreement limits were 2.01 (95% CI -0.89 – 4.90) and 17.14 (95% CI 14.25 – 20.04). The tendency to underestimate BF%, especially among those with higher BF%, was more pronounced in US, as shown by the proportional bias line (blue) in
Figure 2. Linear regression confirmed this proportional bias tendency of US (p = .057) to underestimate BF% when compared to DXA.
4. Discussion
This study aimed to investigate agreement of measurement of BF% obtained by BIA and US compared to DXA in a group of healthy male college students. The main result was that, although the methods showed a high correlation, both BIA and US significantly underestimated BF% compared to the gold standard reference (DXA). This underestimation was more pronounced among those with high BF%.
BIA has been widely used in research settings to assess body composition of adults [
2], older adults [
10], people with chronic disease [
5], and male and female college students [
11]. There are several BIA devices that are commercially available, and some were tested for their validity and agreement with gold standard methods.
Although we did not find a single study testing the BIA model that was used in the present study, Pribyl, Smith and Grimes [
11] analyzed accuracy of a very similar model (Omrom HBF-500) within a sample of male and female college students (±25.8 years). They found that BIA significantly overestimated BF% in males by approximately 1.5% with tighter agreement limits, while the present study found an underestimation of BF% by BIA with large agreement limits. Yet, they compared BIA with air displacement plethysmograpy (BOD POD) as criterion, while this study used DXA as the reference. So, further comparison is limited. Furthermore, another study with young men compared BIA devices with BOD POD as reference and found no significant differences regarding BF% [
12].
Rockamann et al. [
8] compared four different BIA devices with DXA in a sample of college men (±19.8 years) and women. All devices were hand-held. In the present study, a tetrapolar hand-held and feet device was analyzed, limiting comparison. Despite that, they found that two of the four devices underestimate BF% by -3.6 and -5.8% even with a moderate correlation coefficient (around 0.64), which is similar to the result of the present study (we found a mean difference of -4.5% with a high correlation).
Just like BIA, US has been used in research and clinical settings for its low cost, ease of use and transportation [
7]. Some previous studies investigated the validity of the device that we used in the present study. Johnson and colleagues [
9] found that the BodyMetrix B2000 (BMB2000) failed to agree with DXA when measuring BF% of college men (±23.0 years) with a significant underestimation of -4.4%, even though with a strong correlation (r=0.84). This result is similar to what was found in the present study, but the underestimation here was even higher, reaching -9.6%, with a moderate concordance correlation of 0.49. Differences could be related to the fact that the present study used a three-site protocol, whereas Johnson et al. used a seven-site protocol.
Indeed, agreement of different BMB2000 protocols may vary. Baranauskas and colleagues [
6] observed significant differences in BF% of male and female college students (±22.8 years) between seven-site and three-site Jackson and Pollock protocols, showing that the three-site BF% was significantly lower than the seven-site. In addition, both three-site (-5.1%) and seven-site (-3.9%) protocols significantly underestimated BF% when compared to DXA. Similar to the Baranauskas study, Elsey and colleagues [
13] also found the three-site protocol to underestimate BF% compared to seven-site in a sample of female athletes.
One study performed a thorough investigation about various BMB2000 protocols in college men (±20.0 years) and compared the results to DXA [
14]. The authors observed that the three-site protocol, as used in the present study, showed a strong Pearson correlation with DXA (r=0.87). In the present study, Pearson correlation was very similar (r=0.89), but the concordance correlation coefficient, which is more adequate to test agreement between methods, was moderate in the present findings (0.49). Moreover, Kang et al. [
14] observed an underestimation of about -7.0% compared to DXA measured BF%, and this was the worst of all 9 protocols they evaluated.
Strengths and limitations are recognized in the present study. Firstly, we assessed a small convenience sample and may be statistically underpowered. However, a gold standard method that is time consuming and difficult to access was used as reference. Secondly, only one US protocol was analyzed. However, we choose the three-site protocol due to its alleged facility and suitability to clinical settings. Thirdly, only college adult men were included, which makes it impossible to generalize the results to other groups. Noteworthy, this study analyzed a BIA device that was not analyzed before (to the best of our knowledge).
5. Conclusions
In summary, BIA and US have been considered effective alternatives to the expense and technicality of DXA [
9]. However, these methods also require practical device operation skills and proper training before the examination, especially US, because of details like proper probe positioning, and image analysis [
15]. In the present study, both devices showed to be inaccurate to estimate BF% compared to DXA, even though presenting moderate to high correlation. This inaccuracy was higher as higher the DXA measured BF%. Underestimation and proportional bias were more pronounced in the US method.
These results are consistent with previous literature. Therefore, the risk of (mis)interpretation and bias is clear and may potentially impact nutritional and physical activity planning in clinical settings [
16]. BF% underestimation may supposedly lead to accommodation and lack of engagement in nutritional and physical activity programs among healthy, overweight, and obese people. So, it is possible that simple, and inexpensive methods of BF% assessment may negatively interfere in BF monitoring [
8].
Future studies should continue to investigate validity and agreement between new body composition devices and reference methods with diverse and larger samples as body composition monitoring is essential in health and many disease contexts.
Author Contributions
Conceptualization, M.O. and M.D.; methodology and data collection, M.O.; V.C.L.; M.A.D.; G.R.; formal analysis, M.D.; data curation, M.O. and M.D; writing—original draft preparation, M.D.; writing—review and editing, M.O.; V.C.L.; M.A.D.; G.R.; supervision, M.D..; funding acquisition, M.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Research Support Foundation of the Federal District, Brazil (FAPDF) and The APC was funded by the Research Support Foundation of the Federal District, Brazil (FAPDF).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethical Committee of the Brasilia Higher Education Center (IESB) under the protocol nº 6.812.917, of 09 May 2024, for studies involving humans.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data is contained within this article.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Heymsfield, S.B. Advances in Body Composition: A 100-Year Journey. Int J Obes 2024. [Google Scholar] [CrossRef] [PubMed]
- Cimmino, F.; Petrella, L.; Cavaliere, G.; Ambrosio, K.; Trinchese, G.; Monda, V.; D’Angelo, M.; Di Giacomo, C.; Sacconi, A.; Messina, G.; et al. A Bioelectrical Impedance Analysis in Adult Subjects: The Relationship between Phase Angle and Body Cell Mass. J Funct Morphol Kinesiol 2023, 8. [Google Scholar] [CrossRef] [PubMed]
- Bondareva, E.A.; Parfenteva, O.I.; Troshina, E.A.; Ershova, E. V.; Mazurina, N. V.; Komshilova, K.A.; Kulemin, N.A.; Ahmetov, I.I. Agreement between Bioimpedance Analysis and Ultrasound Scanning in Body Composition Assessment. American Journal of Human Biology 2024, 36. [Google Scholar] [CrossRef] [PubMed]
- Velázquez-Alva, M.C.; Irigoyen-Camacho, M.E.; Zepeda-Zepeda, M.A.; Rangel-Castillo, I.; Arrieta-Cruz, I.; Mendoza-Garcés, L.; Castaño-Seiquer, A.; Flores-Fraile, J.; Gutiérrez-Juárez, R. Comparison of Body Fat Percentage Assessments by Bioelectrical Impedance Analysis, Anthropometrical Prediction Equations, and Dual-Energy X-Ray Absorptiometry in Older Women. Front Nutr 2022, 9. [Google Scholar] [CrossRef] [PubMed]
- Cruz Rivera, P.N.; Goldstein, R.L.; Polak, M.; Lazzari, A.A.; Moy, M.L.; Wan, E.S. Performance of Bioelectrical Impedance Analysis Compared to Dual X-Ray Absorptiometry (DXA) in Veterans with COPD. Sci Rep 2022, 12. [Google Scholar] [CrossRef]
- Baranauskas, M.N.; Johnson, K.E.; Juvancic-Heltzel, J.A.; Kappler, R.M.; Richardson, L.; Jamieson, S.; Otterstetter, R. Seven-Site versus Three-Site Method of Body Composition Using BodyMetrix Ultrasound Compared to Dual-Energy X-Ray Absorptiometry. Clin Physiol Funct Imaging 2017, 37, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Perez, S.L.; Zhang, Y.; Mourtzakis, M.; Tussing-Humphreys, L.; Ridlon, J.; Gaskins, H.R.; Mutlu, E. Comparison between Handheld Ultrasound and Regional and Whole-Body Dual Energy x-Ray Absorptiometry (DXA) for Body Fat Assessment. Clin Nutr ESPEN 2021, 46, 386–393. [Google Scholar] [CrossRef]
- Rockamann, R.A.; Dalton, E.K.; Arabas, J.L.; Jorn, L.; Mayhew, J.L. Validity of Arm-to-Arm BIA Devices Compared to DXA for Estimating % Fat in College Men and Women. Int J Exerc Sci 2017, 10, 977–988. [Google Scholar] [PubMed]
- Johnson, K.E.; Miller, B.; Juvancic-Heltzel, J.A.; Agnor, S.E.; Kiger, D.L.; Kappler, R.M.; Otterstetter, R. Agreement between Ultrasound and Dual-Energy X-Ray Absorptiometry in Assessing Percentage Body Fat in College-Aged Adults. Clin Physiol Funct Imaging 2014, 34, 493–496. [Google Scholar] [CrossRef]
- Silveira, E.A.; Barbosa, L.S.; Rodrigues, A.P.S.; Noll, M.; De Oliveira, C. Body Fat Percentage Assessment by Skinfold Equation, Bioimpedance and Densitometry in Older Adults. Archives of Public Health 2020, 78. [Google Scholar] [CrossRef]
- Pribyl, M.I.; Smith, J.D.; Grimes, G.R. Accuracy of the Omron HBF-500 Body Composition Monitor in Male and Female College Students. Int J Exerc Sci 2011, 4, 93–101. [Google Scholar]
- Fahs, C.A.; Boring, J.; Levault, L.; Varner, W.; Beck, M. The Accuracy of Commercially Available Upper and Lower Body Bioelectrical Impedance Analyzers in Men and Women. Biomed Phys Eng Express 2020. [Google Scholar] [CrossRef] [PubMed]
- Elsey, A.M.; Lowe, A.K.; Cornell, A.N.; Whitehead, P.N.; Conners, R.T. Comparison of the Three-Site and Seven-Site Measurements in Female Collegiate Athletes Using BodyMetrixTM; 2021; Vol. 14;
- Kang, S.; Park, J.H.; Seo, M.W.; Jung, H.C.; Kim, Y.I.; Lee, J.M. Validity of the Portable Ultrasound BodymetrixTM Bx-2000 for Measuring Body Fat Percentage. Sustainability (Switzerland) 2020, 12, 1–9. [Google Scholar] [CrossRef]
- Lewandowski, Z.; Dychała, E.; Pisula-Lewandowska, A.; Danel, D.P. Comparison of Skinfold Thickness Measured by Caliper and Ultrasound Scanner in Normative Weight Women. Int J Environ Res Public Health 2022, 19. [Google Scholar] [CrossRef] [PubMed]
- Lopes, S.; Fontes, T.; Tavares, R.G.; Rodrigues, L.M.; Ferreira-Pêgo, C. Bioimpedance and Dual-Energy X-Ray Absorptiometry Are Not Equivalent Technologies: Comparing Fat Mass and Fat-Free Mass. Int J Environ Res Public Health 2022, 19. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).