Submitted:
21 June 2024
Posted:
24 June 2024
You are already at the latest version
Abstract
Keywords:
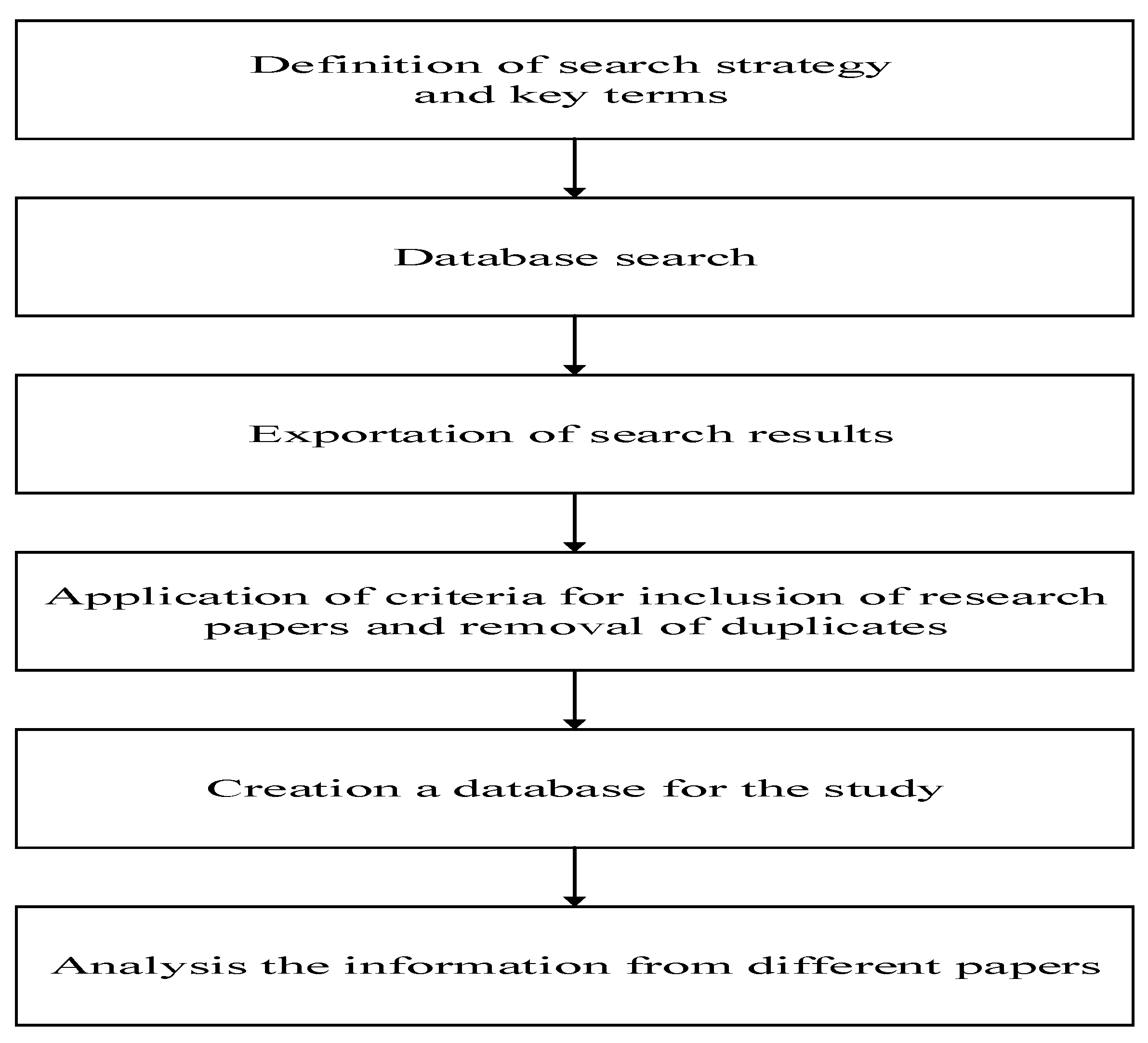
Introduction
Literature Review
Results and Discussion
Results and Discussion
Conclusions
Acknowledgments
References
- Adler-Milstein, J., Embi, P. J., Middleton, B., Sarkar, I. N., & Smith, J. (2017). Crossing the health IT chasm: considerations and policy recommendations to overcome current challenges and enable value-based care. Journal of the American Medical Informatics Association, 24(5), 1036-1043.
- Alhamzah, F., Abbas., Naveed, Akhtar, Qureshi., Nohman, Khan., Rabia, Chandio., Javed, Ali. (2022). The Blockchain Technologies in Healthcare: Prospects, Obstacles, and Future Recommendations; Lessons Learned from Digitalization. International Journal of Online Engineering, 18(09):144-159. [CrossRef]
- Amitava, Banerjee., Lydia, N., Drumright., Andrew, R, J, Mitchell. (2018). Can the NHS be a learning healthcare system in the age of digital technology. [CrossRef]
- Aslan, A., Mold, F., Van Marwijk, H., & Armes, J. (2024). What are the determinants of older people adopting communicative e-health services: a meta-ethnography. BMC Health Services Research, 24(1), 60.
- Brenda, Miao., Douglas, Arneson., Michelle, Wang., Atul, J., Butte. (2022). Open challenges in developing digital therapeutics in the United States. PLOS digital health, 1(1):e0000008-e0000008. [CrossRef]
- Chen, Z. S., & Ruan, J. Q. (2024). Metaverse healthcare supply chain: Conceptual framework and barrier identification. Engineering Applications of Artificial Intelligence, 133, 108113.
- Dimitrova, M., Dimitrov, R., Ahchiyska, K., Nikolaeva, M., Ganova, M., & Petrova, G. (2023). Digital health in Bulgaria: Imagination or possible reality?. Pharmacia, 70(3), 649-655.
- Gleiss, A., & Lewandowski, S. (2022). Removing barriers for digital health through organizing ambidexterity in hospitals. Journal of Public Health, 1-15. [CrossRef]
- Gopal, G., Suter-Crazzolara, C., Toldo, L., & Eberhardt, W. (2019). Digital transformation in healthcare–architectures of present and future information technologies. Clinical Chemistry and Laboratory Medicine (CCLM), 57(3), 328-335. [CrossRef]
- Grigorieva, N. S., Demkina, A. E., & Korobeynikova, A. N. (2024). Digitalization in the Russian healthcare: barriers to digital maturity. Population and Economics, 8(1), 1-14. [CrossRef]
- Grigorieva, N. S., Demkina, A. E., & Korobeynikova, A. N. (2024). Digitalization in the Russian healthcare: barriers to digital maturity. Population and Economics, 8(1), 1-14.
- Guido, Lerzynski. (2021). Ethical Implications of Digitalization in Healthcare. [CrossRef]
- I.A., Shaderkin. (2022). Telemedicine barriers and ways to overcome them.. Рoссийский журнал телемедицины и электрoннoгo здравooхранения, 8(2):59-76. [CrossRef]
- Inampudi, S., Rajkumar, E., Gopi, A. et al. (2024). Barriers to implementation of digital transformation in the Indian health sector: a systematic review. Humanit Soc Sci Commun 11, 632. [CrossRef]
- Joshi, S., & Sharma, M. (2023). Assessment of implementation barriers of blockchain technology in public healthcare: evidences from developing countries. Health Systems, 12(2), 223–242. [CrossRef]
- K., Ramar., G., V., Hariharan, Shanmugasundaram., Bhanu, Prasad, Andraju., Sandhiya, Baskar. (2022). Digital Healthcare using Blockchain. [CrossRef]
- Kajüter, Patricia; Arlinghaus, Tim; Kus, Kevin; and Teuteberg, Frank, “Analysis of Barriers to Digital Linking among Healthcare Stakeholders” (2022). Wirtschaftsinformatik 2022 Proceedings. 7.
- Kalman, J. L., Burkhardt, G., Samochowiec, J., Gebhard, C., Dom, G., John, M.,... & Falkai, P. (2024). Digitalising mental health care: Practical recommendations from the European Psychiatric Association. European Psychiatry, 67(1), e4. [CrossRef]
- Krefting, D., Arzt, M., Maurer, J. T., Penzel, T., Prasser, F., Sedlmayr, M., & Schöbel, C. (2023). Sleep apnea healthcare management in dynamically changing times: Unlocking the potential of digitalization for better care of obstructive sleep apnea—in Germany and beyond. Somnologie, 27(4), 248-254.
- Krefting, D., Bavendiek, U., Fischer, J., Marx, G., Molinnus, D., Panholzer, T.,... & Sedlmayr, M. (2024). Die digitalen Fortschrittshubs Gesundheit–Gemeinsame Datennutzung über die Universitätsmedizin hinaus. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz, 1-9.
- Lapão, L. V. (2019). The future of healthcare: the impact of digitalization on healthcare services performance. The internet and health in Brazil: Challenges and trends, 435-449.
- Larisa, Pătru, (Grigorie)., C., Patru. (2023). Etichal Issues of Digitalization in Healthcare Organizations. Lumen Proceedings. [CrossRef]
- Lea, Meier., Kevin, Tippenhauer., Murat, Sariyar. (2021). Decentralized Digital Health Services Caught Between the Pressure for Innovation and the Burden of Regulations.. 281:1046-1050. [CrossRef]
- Lerzynski, G. (2021). Ethical implications of digitalization in healthcare. Digitalization in Healthcare: Implementing Innovation and Artificial Intelligence, 163-170.
- Lu, W. C., Tsai, I. C., Wang, K. C., Tang, T. A., Li, K. C., Ke, Y. C., & Chen, P. T. (2021). Innovation resistance and resource allocation strategy of medical information digitalization. Sustainability, 13(14), 7888. [CrossRef]
- Mahajan, N., Garg, S., Pandita, S., & Sehgal, G. (2022). Smart Healthcare and Digitalization: Technological and Cybersecurity Challenges. In Cross-Industry Applications of Cyber Security Frameworks (pp. 124-147). IGI Global.
- Moetlhoa, B., Nxele, S.R., Maluleke, K. et al. (2024). Barriers and enablers for implementation of digital-linked diagnostics models at point-of-care in South Africa: stakeholder engagement. BMC Health Serv Res 24. [CrossRef]
- Nikitenko, V., Voronkova, V., Kozar, Y., Oleksenko, R., Yanchevskyi, O., & Korobko, I. (2023). Digital Healthcare in the Context of Challenges and Opportunities of Technological Progress in the Countries of the European Union. Revista de la universidad del ZULIA, 14(40), 315-333.
- Numair, T., Harrell, D. T., Huy, N. T., Nishimoto, F., Muthiani, Y., Nzou, S. M.,... & Kaneko, S. (2021). Barriers to the digitization of health information: a qualitative and quantitative study in Kenya and Lao PDR using a cloud-based maternal and child registration system. International Journal of Environmental Research and Public Health, 18(12), 6196.
- Radwan, H. A., Alsharif, A. T., Alsharif, M. T., Aloufi, M. R., & Alshammari, B. S. (2023). Digital technologies in dentistry in Saudi Arabia: Perceptions, practices and challenges. Digital Health, 9, 20552076231197095.
- Rahul, Lamba. (2019). A Solution to the Digitization of Healthcare Institutions in Developing Countries. Journal of Health and Medical Informatics, 10(4):1-3.
- Rau, E., Tischendorf, T., & Mitzscherlich, B. (2024). Implementation of the electronic health record in the German healthcare system: an assessment of the current status and future development perspectives considering the potentials of health data utilisation by representatives of different stakeholder groups. Frontiers in Health Services, 4, 1370759.
- Rudwan, Masoud. (2022). Digital transformation in healthcare. International journal of scientific and research publications, 12(7):379-382. [CrossRef]
- Sánchez-Bayón, A. (2021). Balance de la economía digital ante la singularidad tecnológica: cambios en el bienestar laboral y la cultura empresarial. Sociología y Tecnociencia, 11(2). 53-80.
- Sánchez-Bayón, A. (2023). Digital transition and readjustmen on EU tourism industry. Studies in Business and Economics, 18(1): 275-297. [CrossRef]
- Sánchez-Bayón A, González-Arnedo E, Andreu-Escario Á (2022) Spanish Healthcare Sector Management in the COVID-19 Crisis Under the Perspective of Austrian Economics and New-Institutional Economics. Frontiers in Public Health 10:801525 (1-15). [CrossRef]
- Sánchez-Bayón, A., Sastre, F.J. & Sánchez, L.I. (2024). Public management of digitalization into the Spanish tourism services: a heterodox analysis. Review of Manageral Science, 18(4): 1-19. [CrossRef]
- Saxena, S. G., & Godfrey, T. (2022). Advancing digital technologies in healthcare. In Digital Innovation for Healthcare in COVID-19 Pandemic (pp. 75-93). Academic Press.
- Sushanta, Kumar, Tarai. (2023). Digital Innovation in Healthcare. Advances in healthcare information systems and administration book series, 1-19. [CrossRef]
- van Drumpt, S., Timan, T., Talie, S., Veugen, T., & van de Burgwal, L. (2024). Digital transitions in healthcare: the need for transdisciplinary research to overcome barriers of privacy enhancing technologies uptake. Health and Technology, 1-15.
- Monferdini, L., Pini, B., Bigliardi, B., & Bottani, E. (2024). Challenges and opportunities of digitalization in the healthcare supply chain: A literature review. Procedia Computer Science, 232, 2220-2229. [CrossRef]
- Pukinskytė, S. (2022). Challenges in healthcare sector while applying digitalization tools: the case of E. Sveikata (Doctoral dissertation, Kauno technologijos universitetas.).
- Tranfield, D., Denyer, D., & Smart, P. (2003). Towards a methodology for developing evidence-informed management knowledge by means of systematic review. British journal of management, 14(3), 207-222. [CrossRef]
| Obstacles & barriers for healthcare digitalization | References |
| workload motivation to maintain high performance |
Nuamir et al. (2021) |
| Complexity of technology tools. Data used by digital healthcare tools is still insufficient. Telemedicine as a tool has limitations in terms of observation and accurate diagnosis. Provision Medical education is lacking digital literacy fundamentals. Undeveloped legal base. Not sequential digital healthcare strategy. Digital healthcare is still in the early stage of development. Insufficient patient privacy and data security. The use of digital tools may reduce healthcare specialist’s skills. Infrastructural barriers. Lack of funding. Cultural and country-specific barriers. Religious barriers limit implementation opportunities. Poor tool functionality. Data inaccessibility. Lack of training. Lack of support. Connectivity Issues. Unawareness of risk management plans. Poor organizational system management. Special skills needed. User ignorance for the Digitalization. Lack of understanding of the tool. |
Pukinskytė, S. (2022). |
| Limited connectivity. Restricted offline functionality. Challenges related to load shedding or rolling electricity blackouts. |
Moetlhoa et al. (2024) |
| Lack of network coverage and information technology (IT) infrastructure. High installation and operating cost. Lack of medical records and experts. Lack of physical examination. Data accuracy and misdiagnosis. Data privacy and confidentiality. Language and communication barriers. User barriers, and ethical, legal, and accountability concerns. |
Inampuid et al. (2024) |
| common basic rules have not been developed. each region independently followed its own way to digitize, resulting a huge variety of software products used even within one region, which makes electronic document flow between medical institutions difficult and practically impossible between regions. Low basic digital skills in medical workers. low level of digital knowledge and trust among patients creates a low demand for digital technologies among the population. Citizens are concerned about safety of their personal data on digital media. fear of medical errors in society associated with the use of telemedicine technologies. |
Grigorieva, Demkina, & Korobeynikova (2024) |
| Lack of interoperability between systems Significant risks in digital transformation implementation Lack of awareness, evidence, and funding for e-health initiatives. Legal hurdles and shortage of qualified human resources in healthcare. |
Sushanta, Kumar, Tarai. (2023) |
| Structural and spatial disparities in medical facilities and practitioners. Exodus of general practitioners and specialists in rural regions. |
Rudwan, Masoud. (2022) |
| Poor standardization of information exchange protocols between sources (devices) | I.A., Shaderkin. (2022). |
| Regulatory requirements and legal uncertainties | Lea, Meier., Kevin, Tippenhauer., Murat, Sariyar. (2021). |
| sociological, economical, and infrastructure obstacles | Joshi, S., & Sharma, M. (2023). |
| Ethical Issues of Digitalization in Healthcare Organizations. | Larisa, Pătru, (Grigorie)., C., Patru. (2023). |
| Doctors claim that EHR distracts them from their regular clinical effectiveness. They believe that their time spent on EHR could have been better used on patients. |
Rahul, Lamba. (2019). |
| Data transparency, traceability, immutability, audit, data provenance, flexible access, trust, privacy, and security. | Alhamzah, et al. (2022). |
| rigger fears and insecurities in patients | Guido, Lerzynski. (2021). |
| Regulatory, commercial, and technical barriers hinder healthcare digitalization adoption. Potential obstacles include digital divide, cybersecurity risks, and biased algorithms Educate patient about healthcare digitalization. |
Brenda, et al. (2022) |
| Data breaches, malware, viruses, legacy systems, and network security risks. | Ramar et al. (2022). |
| Poor quality and validation of clinical data. Lack of understanding and underdevelopment of analytic tools. |
Amitava, et al. (2018). |
| Cost management | Monferdini et al. (2024) |
| IT Infrastructure of a country. functionality problems of the service Low compatibility (not all healthcare facilities can provide the required network access). A lack of data often leads to poor data integrity and quality. barriers resulting from workflow deficiency. lack of integration in the clinical work. issues around physicians include that they simply have no time for non-patient related concerns. Hierarchical deficiency includes missing top-management support, low change management, and scattered key players that operate independently within the organization causing unclear roles and responsibilities |
Gleiss, & Lewandowski (2022) |
| Cultural barriers which evolve around the issue of differences in adopting and accessing digital resources. Barriers occur on an individual, like attitude toward technology or devoid intrinsic motivation and knowledge. Low perceived usefulness and confidence in technology in general. Mistrust toward their technologies. fear of more transparency about the medical processes, which results in a loss of control and strengthens the patient’s position. Fear and doubts also arise from missing social contact when switching to digital solutions such as online consultations. lack of business education of healthcare professionals often leads to ignorance toward anticipated healthcare benefits. Monetary problems concerning digital innovations range from verification issues to missing public funds. market-entry barrier for startups. Costs are a barrier, because high implementation costs often represent a deterrent, and the amount of lifecycle costs is sometimes difficult to estimate. general lack of (external) financial incentives for the introduction and use of digital innovations in healthcare. Data security and privacy issues are relevant for both users and providers. differences in legislation at federal and state levels even increase the legal complexity structural barriers. issues of standardization, certification, approval, and cooperation. high costs lack of interoperability of technology frequent software Updates privacy concerns technological disruption network coverage issues |
Saxena & Godfrey (2022) |
| ethical challenges related to patient privacy and data security algorithm understanding |
Lerzynski (2021) |
| Challenges in methodology, implementation, and evaluation Lack of digitally qualified workforce |
Lapão (2019). |
| Technological cyber security challenges | Mahajan et al. (2022) |
| digitalized analysis and process medical data sharing infrastructure resources regulation and constraints operational issue The dearth of expertise in digitalization shortcomings of inadequate experience limitations of traditional realization and storage of relational data regulation and responsibilities |
Lu et al. (2021) |
| Health barriers support networks application interface/design digital literacy lack of awareness online security access to digital devices and the internet relationship with healthcare provider in-person preference |
Aslan, Mold,Marwijk and Jo Armes (2024) |
| trust in technology financial Barriers |
Van Drumpt et al. (2024) |
| Rules Data collection challenges |
Krefting et al. (2023) |
| Lack of practitioners’ awareness’ lack of education. lack of clinical evidence. |
Radwan et al. (2023) |
| low level of digital literacy among health care providers. low level of motivation to make changes in organizational processes. significant gaps in basic digital skills among health professionals. low level of digital knowledge and patients’ |
Grigorieva et al. (2024) |
| Standardization and interoperability among various healthcare systems, devices, and platforms. Data Governance and Security. Infrastructure and Technical Requirements. Governance and Stakeholder Engagement. Adoption and Implementation Support. Regulatory barriers. Lack of infrastructure. Funding and investment. Data privacy and security Concerns. Cultural and organizational factors. Organizational barriers. Lack of digital literacy among healthcare specialists. deficiency in legal regulations. |
Dimitrova et al. (2023) |
| structural problems. timing of the introduction. insufficient information and communication measures. |
Rau, Tischendor & Mitzscherlich (2024) |
| human, technical, ethical–legal, and economic barriers | Kalman et al. (2024) |
| management technologies, data security, organizational structure, and societal acceptance | Chen & Raun (2024) |
| 1 | Obstacles related to high cost of digitalization |
| 2 | Obstacles related to the fear of healthcare industry employees of reducing accuracy and productivity with the use of technology |
| 3 | Obstacles related to quantity and quality of data |
| 4 | Obstacles related to security and privacy of patients data |
| 5 | Obstacles related to complexity of using technology |
| 6 | Obstacles related to limitations of digital tools |
| 7 | Obstacles related to lack of education, skills and knowledge about digitalization |
| 8 | Obstacles related to inappropriate rules |
| 9 | Obstacles related to lack of strategy |
| 10 | Obstacles related to Infrastructure |
| 11 | Obstacles related to country culture and organizational culture |
| 12 | Obstacles related to lack of support |
| 13 | Obstacles related to lack of integrity and connectivity between technological tools |
| 14 | Obstacles related to healthcare management |
| 15 | Obstacles related to rolling electricity blackouts and internet weakness |
| 16 | Obstacles related to ethical concerns |
| 17 | Obstacles related to organizational structure |
| 18 | Obstacles related to workload and time limitation |
| 19 | Obstacles related to motivation of healthcare employees |
| 20 | Obstacles related to supply chain of technologies providers and healthcare organizations |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





