1. Introduction
Interoperable multilayer networks are pivotal in transforming public health by enhancing disease control strategies and diagnostic systems (Loza et al., 2012). By employing computational algorithms to replicate realistic social models of educational institutions, these multilayer networks assist in identifying vulnerable populations and optimizing control measure distribution during disease outbreaks. Moreover, diagnostic systems based on neural networks contribute significantly to detecting health risks such as hypertension, achieving a high level of effectiveness.
These networks enable the integration of varied health intelligence data, enhancing disease detection, alerting, response, and prediction capabilities during public health crises. Additionally, implementing data sharing standards and interoperability, coupled with innovative methodological approaches, workforce structures, and data governance, guarantees the security and reliability of public health data systems.
Within this framework, digital health concerns use digital technologies for health. This process involves incorporating different technological tools into healthcare, such as eHealth (Hallberg & Salimi, 2020), mobile health (mHealth), telemedicine (Groom et al., 2021), and utilizing computer science concepts like big data and artificial intelligence (Hyder & Razzak, 2020).
This study shows the link between digital health, which is increasingly used in public healthcare, and multilayer networks. These networks consist of advanced structures where multiple layers interact through connecting copula nodes (represented by IT devices, m-Apps, EHRs, etc.).
The multilayer network architecture, characterized by its intricate system of interconnected layers, each serving a specific function, offers a high degree of adaptability, expansiveness, robust security measures, and unwavering dependability essential for accommodating the intricate and demanding specifications inherent in digital health. By enabling efficient data management and communication between various healthcare stakeholders, multilayer networks play a crucial role in expanding access to healthcare services, improving patient outcomes, and making healthcare systems more resilient and cost-effective. This multilayer design structure is vital in digital health for diverse services support: Digital health requires transmitting various data types, including voice, video, and significant medical files. Multilayer networks can efficiently handle this diversity by segregating services based on bandwidth and latency requirements and coordinating devices (smartphones, tablets, etc.).
Scalability—the ability of an information system to maintain its equilibrium State with increased storage volume—is another core issue that adds flexibility to healthcare ecosystems (Satamraju, 2020) that can face severe and unforeseen stress (as in the case of pandemics). The demand for digital health services can fluctuate significantly, driven by factors such as pandemics or changes in healthcare policies. Multilayer networks can scale up or down based on demand, ensuring that the network infrastructure can always meet the needs of healthcare providers and patients.
Preserving patient data privacy and security holds utmost importance within the healthcare sector. Multilayer networks can implement advanced security protocols and encryption at various levels (Fareed & Yassin, 2023), offering robust protection against unauthorized access and data breaches. This protection is especially important for sensitive medical data transmitted during digital health consultations.
Healthcare services need reliable networks to guarantee uninterrupted digital health consultations and data transfers. Multilayer networks can provide backup solutions, allowing seamless service even if one path or layer experiences issues.
Multilayer networks also prioritize Quality of Service management, which is crucial for digital health services. This process ensures that high-priority services such as live video consultations always have capacity and speed, even during network congestion.
Consistent with this introductory framework, the paper is structured as follows: digital health and its public health implications will be briefly introduced before a fundamental multilayer network analysis. The two topics will then be jointly examined, analyzing their public implications, even in cost/benefit analysis and scalable digital health ecosystems. A brief discussion anticipates the conclusion.
2. Literature Review
Interoperable multilayer networks play a pivotal role in revolutionizing public digital health by enhancing healthcare service delivery, improving public health outcomes, and contributing to substantial cost savings for public healthcare systems (Channi et al., 2022; Osipov & Skryl, 2021).
These networks facilitate seamless data exchange and integration across healthcare systems and providers, increasing accessibility, efficiency, and data-driven decision-making through blockchains (Geng et al., 2024).
By reducing redundancies, optimizing resource allocation, and minimizing unnecessary procedures, these networks pave the way for a more efficient and effective healthcare system, ensuring financial sustainability while improving care access and patient engagement for universal health coverage (Bloom et al., 2023).
Innovative multilayer network analysis is crucial in improving interoperability, reducing spatial and temporal constraints, and streamlining processes within healthcare systems, ultimately enabling high-quality care delivery at a lower cost and transforming patient care paradigms (van der Weert et al., 2022).
By integrating the multilayer network model into healthcare architectures, players can comprehensively represent the healthcare system, fostering trust among medical entities and enhancing treatment outcomes (Rahimi et al., 2023).
This study represents an advance in the current literature (see, for instance, Moro Visconti, 2021; Pathinarupothi et al., 2016), as it innovatively links digital health studies with multilayer network theory analysis.
3. Digital Health and Public Healthcare
Digital health has transformed public healthcare by significantly enhancing the accessibility of services, particularly benefiting individuals residing in rural or underserved areas with limited medical facilities. Utilizing remote consultations in digital health diminishes the necessity for travel, ensuring prompt care delivery. In times of public health emergencies such as pandemics, digital health services become indispensable for delivering care while minimizing the risks of disease transmission, underscoring their crucial role in emergency scenarios. Additionally, digital health plays a role in addressing healthcare workforce shortages in underserved regions by enabling remote service provision and expanding the reach of specialists beyond conventional boundaries, thereby enhancing the optimization of healthcare delivery.
The impact of digital health on public healthcare has been profound and multifaceted, with significant benefits observed in several key areas and some concerns (Jandoo, 2020). Digital health dramatically enhances access to healthcare services, especially for people living in rural or underserved areas where medical facilities are scarce or hard to reach. By providing remote consultations, digital health reduces the need for travel and helps patients receive timely care. Digital health supports public health by facilitating distance health monitoring, disease management, and health education. During public health crises, for instance, pandemics (Leite et al., 2020), using digital healthcare services becomes imperative to deliver efficient care while reducing the potential for disease spread. By enabling healthcare providers to offer services remotely, digital health can help address the shortage of healthcare professionals in underserved areas, optimizing the workforce. It allows specialists to extend their reach beyond traditional geographic boundaries.
Digital health has the potential to significantly decrease healthcare expenditure by mitigating the necessity for face-to-face consultations, a process known to incur substantial costs and consume a considerable amount of time. Furthermore, it can diminish the financial burden on patients related to transportation expenses, thereby enhancing accessibility to healthcare. The ability for patients to access healthcare services remotely enhances the likelihood of their participation in regular health monitoring and post-treatment care, transitioning from being in-patient or out-patient to home-based patients whenever feasible.
Integrating digital health into the healthcare system optimizes the delivery process, enhancing its effectiveness. It expedites the diagnosis and treatment, diminishes appointment waiting times, and enables more efficient appointment schedule management.
The delivery of healthcare through digital platforms has demonstrated comparable effectiveness to in-person visits, especially within specific medical fields like psychiatry (Smith et al., 2020) and dermatology (Dhaduk et al., 2021). Furthermore, digital health technologies facilitate consistent healthcare delivery, which is critical for managing chronic conditions and ensuring patients’ overall health.
The adoption of digital health solutions in remote areas has notably enhanced healthcare accessibility by negating the necessity for patients to undertake lengthy journeys for medical appointments. This adoption, in turn, guarantees prompt healthcare provision and alleviates the healthcare burden on individuals in underserved locales.
This provision highlights the importance of incorporating digital health solutions in emergency response strategies to ensure the continuity of healthcare services. By enabling remote service provision and extending the reach of healthcare specialists beyond traditional boundaries, digital health helps mitigate healthcare workforce shortages in underserved areas. This innovative approach optimizes healthcare delivery and ensures patients in remote regions can access quality care.
The infusion of digital health technologies into the healthcare sector accelerates diagnosing and treating patients, minimizing waiting times for appointments and refining the management of appointment schedules. This fine-tuning elevates the efficacy of healthcare provision, ensuring that individuals receive prompt and effective care irrespective of their geographical proximity. By streamlining diverse procedures and frameworks, this advancement markedly amplifies the overall efficiency and influence of healthcare delivery, thereby ensuring that patients, regardless of their location, are promptly and effectively catered to with a superior standard of care.
4. Multilayer Networks
The interconnected layers provide insights into relationships, enabling personalized treatment strategies. Real-time data integration enhances decision-making and enables customized care delivery. The interdisciplinary approach ensures comprehensive patient care, especially for complex cases. Machine learning models analyze vast data to provide decision support for proactive patient management. The integration of data sources like genomics and EHRs enables personalized treatment strategies. By incorporating real-time health data, multilayer networks support proactive patient management.
The link between digital health and multilayer networks involves how digital health relies on advanced and interconnected network infrastructures to deliver healthcare services remotely.
Network Science (Barabási, 2016) is a prolific field coming from several disciplines, which is compatible with the increasing use of Big Data (Bianconi, 2018), even in healthcare (Palanisamy & Thirunavukarasu, 2019). In the beginning, single networks can be classified as undirected or directed.
Multilayer networks are complex and advanced systems distinguished by many interconnected networks, where each stratum represents a unique classification of interaction, association, or linkage. This system starkly contrasts conventional network models, which typically concentrate on singular connections between nodes; in contrast, multilayer networks encompass multiple strata, with each layer symbolizing a unique form of relationship or interaction between entities. This approach provides a more nuanced and comprehensive understanding of complex systems by examining the intricate interrelations among various layers.
Multilayer networks present a formidable instrument for encapsulating the intricacy of real-world systems, offering perspectives that may not be readily discernible when employing more basic, single-layer network frameworks.
Multilayer networks, also known as multiplex networks according to Bianconi (2018), are intricate mathematical constructs utilized by researchers and professionals to gain insights into, make predictions about, and exert control over the complicated dynamics of complex systems spanning a diverse array of fields, such as the realm of public healthcare.
The mathematical formulation of multilayer networks involves a meticulous examination of the inter-layer connections between nodes across different layers, contributing to the model’s overall complexity and richness.
To define copula nodes that connect different layers, we introduce additional nodes, called copula nodes, which serve as bridges between layers. A copula node can be connected to nodes in different layers, facilitating the interaction or information flow between them. The connectivity pattern of copula nodes is typically defined based on the specific application and desired network structure.
One way to represent inter-layer connections in a multilayer network is through inter-layer coupling matrices C, where ′Cll′ denotes the strength of the connection between layer l and layer ′l′. These coupling matrices can model how information or influence propagates across layers. Multilayer networks are dynamic, showing a temporal evolution (incorporating machine learning) and allowing for a combination of synergistic networks linked by connecting copula (replica) nodes.
Multilayer networks’ complexity and ability to represent multiple types of interactions, relationships, and connectivity make them particularly suited for digital health applications. They offer a flexible, scalable, resilient framework for integrating diverse data sources and facilitating comprehensive, patient-centered healthcare delivery.
In healthcare and digital health, these layers can represent various data and communication channels, such as EHRs, telehealth video conferencing systems, wearable health devices, and more.
Critical characteristics of multilayer networks impacting digital health are reported in
Table 1.
Some typical applications of multilayer networks in digital health (Balram et al., 2016) include Patient Interaction Networks between patients based on relationships such as social interactions, co-occurrence in healthcare facilities, or shared medical conditions.
Other applications refer to understanding the disease spread (through transportation networks, social interactions, and genetic similarities) across different populations or geographical regions. Networks catalyze the integration of heterogeneous data sources such as genomics, EHRs, and lifestyle information to develop personalized treatment strategies and predict patient outcomes, optimizing the allocation of healthcare resources such as hospital beds, medical personnel, and medical supplies by modeling the interconnectedness of healthcare facilities and patient flows.
In the ever-evolving landscape of digital health, unlocking the power of interconnected networks is crucial for optimizing the impact and efficiency of digital healthcare innovations. Interoperable multilayer networks facilitate the integration of disparate healthcare data sources. By enabling seamless data exchange and accessibility across different platforms and systems (e.g., hospital systems, out-patient services, home health care), they support comprehensive patient-centered care (Moro Visconti & Martiniello, 2019). This integration supports more informed decision-making by healthcare providers and personalized care plans for patients.
The interconnected nature of multilayer networks is a holistic perspective that plays a vital role in facilitating more accurate diagnosis, meticulous treatment planning, and the maintenance of seamless care continuity, all of which are fundamental components of patient-centric healthcare provision.
Utilizing multilayer networks makes incorporating real-time health data from wearable devices and home monitoring systems into patient records feasible, rendering this information readily available to healthcare providers. Integrating data from wearable devices and other health monitoring instruments with digital health platforms enriches remote patient monitoring capabilities.
Integrating artificial intelligence and machine learning models into multilayer networks can analyze vast amounts of data from various layers to provide decision support, predict health outcomes, and identify at-risk patients (Noorbakhsh-Sabet et al., 2019). This integration facilitates proactive management of patient health and personalized care delivery. Artificial neural networks (Rashida, 2023) emulate the functioning of the human brain by simulating interconnected nodes (neurons) that communicate with each other.
Interconnected layered networks foster synergy between diverse healthcare fields by offering a cohesive foundation for exchanging data and facilitating communication. This interdisciplinary approach is essential for comprehensive patient care, especially for complex cases requiring multiple specialties.
The multilayered structure of digital health solutions allows for scalability and flexibility, accommodating evolving healthcare needs, technologies, and regulations. This level of flexibility is paramount in ensuring patient-centered care continuity, as Poitras et al. (2018) highlighted in the rapidly evolving digital health domain.
Interoperable systems play a pivotal role in diminishing redundancies and inefficiencies within the healthcare sector by facilitating the seamless exchange of patient information among various healthcare entities and environments. Consequently, this integration can reduce healthcare expenditure due to the decreased necessity for repetitive tests and the optimization of care coordination processes.
Patient-centric digital health solutions that leverage interoperable multilayered networks empower individuals to actively participate in managing their healthcare journey. This increased involvement through access to their health records can enhance satisfaction levels and foster greater adherence to prescribed treatment regimens.
5. Multilayer Networks and Public-Driven Digital Health
The structured framework of multilayer networks enhances relationships across technological infrastructure, service provision, and accessibility. These networks offer a comprehensive method to grasp complexities in digital health systems, empowering stakeholders to address challenges effectively. These networks encompass patient-generated data, social support, healthcare providers, public health initiatives, and technological frameworks, fostering comprehensive and participatory healthcare frameworks.
The underlying technological frameworks ensure secure data storage, processing, and accessibility for authorized users, enhancing health outcomes and healthcare services.
The complex nature of healthcare systems requires a thorough comprehension of the interconnections in digital health, where multilayer networks play a crucial role in optimizing operations and services. These networks offer a structured framework to improve relationships across levels, from technological infrastructure to service provision, ensuring accessibility, effectiveness, and resilience in challenging circumstances.
The correlation between multilayer networks and digital health traces back to the intricate and interconnected nature of healthcare systems, where digital health functions as a pivotal element essential for the system’s operations. Multilayer networks present a structured framework to comprehend and enhance the connections and relationships between various network layers (or types) within a given system. These networks facilitate a deeper insight into the intricate systems supporting digital health and aid in optimizing such systems, ranging from technological infrastructure to delivering services.
Utilizing multilayer networks offers a holistic and all-encompassing method for grasping the complexities inherent in the systems that uphold digital health. These systems encompass everything from the technological backbone to providing services and more. They empower various stakeholders to tackle the multifaceted hurdles present in contemporary healthcare, ensuring that digital health services remain accessible, efficient, and robust in the face of challenges.
This multidimensional discussion sheds light on how these networks impact the digital health landscape and patient-centric care delivery. Public-driven multilayer networks in digital health refer to complex, interconnected systems significantly influenced, shaped, or utilized by the general public or patient communities. These networks embody multiple layers of interaction and data exchange, encompassing various stakeholders, technologies, and communication channels in the healthcare ecosystem. The “public-driven” aspect emphasizes the role of patients, their families, and the broader community in contributing to, accessing, and using these networks, often focusing on enhancing patient care, improving health outcomes, and facilitating public engagement in health-related matters. Interactions include:
- a)
Patient-Centric Data Layers: One layer might include patient-generated health data from wearable devices, mobile health apps, or patient-reported outcomes. This layer empowers patients to actively contribute their health data, making them integral participants in their healthcare management.
- b)
Community and Social Support Layers: These layers can represent online patient communities, social media platforms, and support groups where patients and caregivers share experiences, advice, and support. Such interactions provide emotional and social support and facilitate the exchange of valuable health-related information and resources.
- c)
Healthcare Provider Layers: Traditional healthcare provider networks, including hospitals, clinics, and private practices, form another layer. These institutions may engage with patients via digital health platforms, offering virtual consultations, remote monitoring, and digital health assessments.
- d)
Public Health and Research Layers: Public health initiatives and research projects that engage with the public for data collection, health surveillance, and participatory research studies constitute another crucial layer. These efforts can lead to better-informed public health strategies and more targeted healthcare interventions.
- e)
Technology and Infrastructure Layers: The backbone of these networks is the underlying technological frameworks that support digital health services, such as cloud computing (Mishra et al., 2019), data analytics platforms, and cybersecurity measures. These frameworks ensure data is securely stored, processed, and accessible to authorized users.
Public-driven multilayer networks in digital health signify a notable transition towards embracing more comprehensive and participatory healthcare frameworks that harness the synergistic potential of technology, data analytics, and community involvement to enhance health results and provide healthcare services. These networks within the domain of digital health present a holistic and all-encompassing approach to managing processes related to homecare assistance, amalgamating cutting-edge technological advancements with data-centric decision-making strategies to efficiently allocate resources, enhance patient care quality, and endorse the de-hospitalization campaign (Massaro et al., 2018).
6. Cost/Benefit Analysis
Integrating electronic health records brings various benefits, such as cost reductions, improved data legibility, and enhanced decision-making processes. These benefits highlight the economic, clinical, and informational advantages of digital advancements in healthcare systems.
Multilayer networks amplify healthcare services’ effectiveness, availability, and excellence. They present a promising avenue for further enhancement in healthcare systems, as demonstrated in
Table 2.
Incorporating digital health technologies within the healthcare industry has exhibited notable benefits. The utilization of digital health data is pivotal in ensuring cost-effective and efficient healthcare choices, underscoring the significance of unbiased information for all involved parties. Additionally, digital radiography systems provide substantial advantages compared to traditional systems, with reduced expenses and faster amortization periods, signifying their cost-effectiveness and efficacy within healthcare environments.
The inclusion of information technology in healthcare institutions has been demonstrated to enhance service quality, albeit with substantial expenses that necessitate thorough investment validation. Integrating electronic health records produces diverse benefits, including cost reductions, enhanced data legibility, and improved decision-making processes, spotlighting the economic, clinical, and informational benefits of digital advancements in healthcare systems.
The advantages of using digital health technologies (Woods et al., 2023) are increasingly becoming apparent within the healthcare sector. Multilayer networks play a crucial role in amplifying healthcare provisions’ effectiveness, availability, and excellence, presenting a promising avenue for further enhancement in this realm, as shown in
Table 2.
While the initial setup and ongoing maintenance of multilayer networks in public digital health require significant investment, the potential benefits of improved healthcare access, efficiency, and patient outcomes can outweigh these costs over time. Additionally, multilayer networks can contribute to long-term savings by reducing unnecessary procedures and hospital readmissions and enabling more effective public health interventions.
The economic advantages derived from using digital health technologies like e-health, m-Health, and telemedicine have been the subject of thorough examination, with numerous crucial statistical data and research projects that illustrate these benefits’ significance. Numerous empirical research endeavors have elucidated the transformative impact of digital health technologies on healthcare delivery, shedding light on their propensity to engender substantial cost reductions.
For instance, in their recent study, Evers and colleagues (2022) estimated the potential cost-saving implications of telemedicine services as opposed to traditional in-person medical consultations.
Furthermore, a report published by Deloitte in 2015 highlighted the efficacy of remote patient monitoring initiatives in mitigating hospital readmissions by as much as 30% while concurrently generating potential cost reductions amounting to an impressive $10 billion annually, specifically within the healthcare landscape of the United States. Beyond mere cost savings, incorporating digital health technologies can create novel revenue streams for healthcare providers and other relevant stakeholders.
For instance, McKinsey (2021) estimated that the global telemedicine market could generate $250 billion in revenue annually by 2025. This forecast underscores the significant economic implications and opportunities the telemedicine industry holds for stakeholders, highlighting the immense potential for financial gains and market expansion within this sector. This growth derives from the rising acceptance and integration of virtual healthcare solutions, such as mobile health applications and wearable gadgets that offer subscription services and in-application purchases.
Digital health technologies have the potential to enhance the operational efficiency present within healthcare systems, thereby leading to significant cost savings and the generation of revenue. For example, Upadhyay (2023) discovered that implementing Electronic Health Records (EHRs) generates cost savings in the US healthcare system, amounting to $81 billion annually. This financial benefit depends on the notable reduction in administrative expenditures and enhanced operational efficiency facilitated by EHR systems. This considerable financial benefit stems from the noteworthy reduction in administrative expenses and the enhancement of operational efficiency through streamlining workflow processes. Haleem et al., 2021 demonstrated that Telemedicine consultations potentially decrease patient wait times and enhance the volume of patients attended to daily. Consequently, this heightened productivity can lead to a notable increase in the overall revenue generated by healthcare providers.
Telehealth services have been associated with improved healthcare outcomes while remaining a cost-effective mode of healthcare delivery (Mahtta et al., 2021).
Digital health technologies improve patient outcomes, which can result in long-term cost savings and revenue generation through better population health management and reduced healthcare utilization. For instance, Kruse et al. (2017) found that telemedicine interventions have been linked with enhanced clinical results and increased patient contentment within various medical fields. Peyroteo et al., 2021 have shown that the application of remote digital health platforms in monitoring chronic conditions can enhance the efficacy of disease management protocols and lower the rate of hospital admissions. Consequently, there is a notable decrease in the overall healthcare expenditures linked to managing chronic illnesses as the emphasis transitions towards preventive healthcare and refined treatment approaches.
Several studies have evaluated digital health investments’ Return on Investment (ROI) and found positive returns for healthcare organizations and payers. For example, Snoswell et al. (2020) estimated that every $1 spent on telehealth could result in $6 in healthcare cost savings.
7. Scalable Digital Health Ecosystems
Integrating multilayer networks fosters collaborative interactions among stakeholders, leading to innovative healthcare solutions. Overcoming obstacles such as data diversity and multidimensionality requires knowledge-driven frameworks for efficient management of healthcare Big Data. Effective sharing of inter-organizational digital transformation knowledge is essential for successful implementation and expansion within scalable digital health ecosystems. Synergies like economies of scale and experience, value co-creation patterns, and real options positively impact public healthcare ecosystems, leading to cost savings and improved performance.
Scalable digital health ecosystems entail amalgamating multilayer networks to augment healthcare innovation and resilience. These ecosystems utilize digital platforms to facilitate interactions among diverse stakeholders, establish a web of value exchange, and create inventive healthcare solutions.
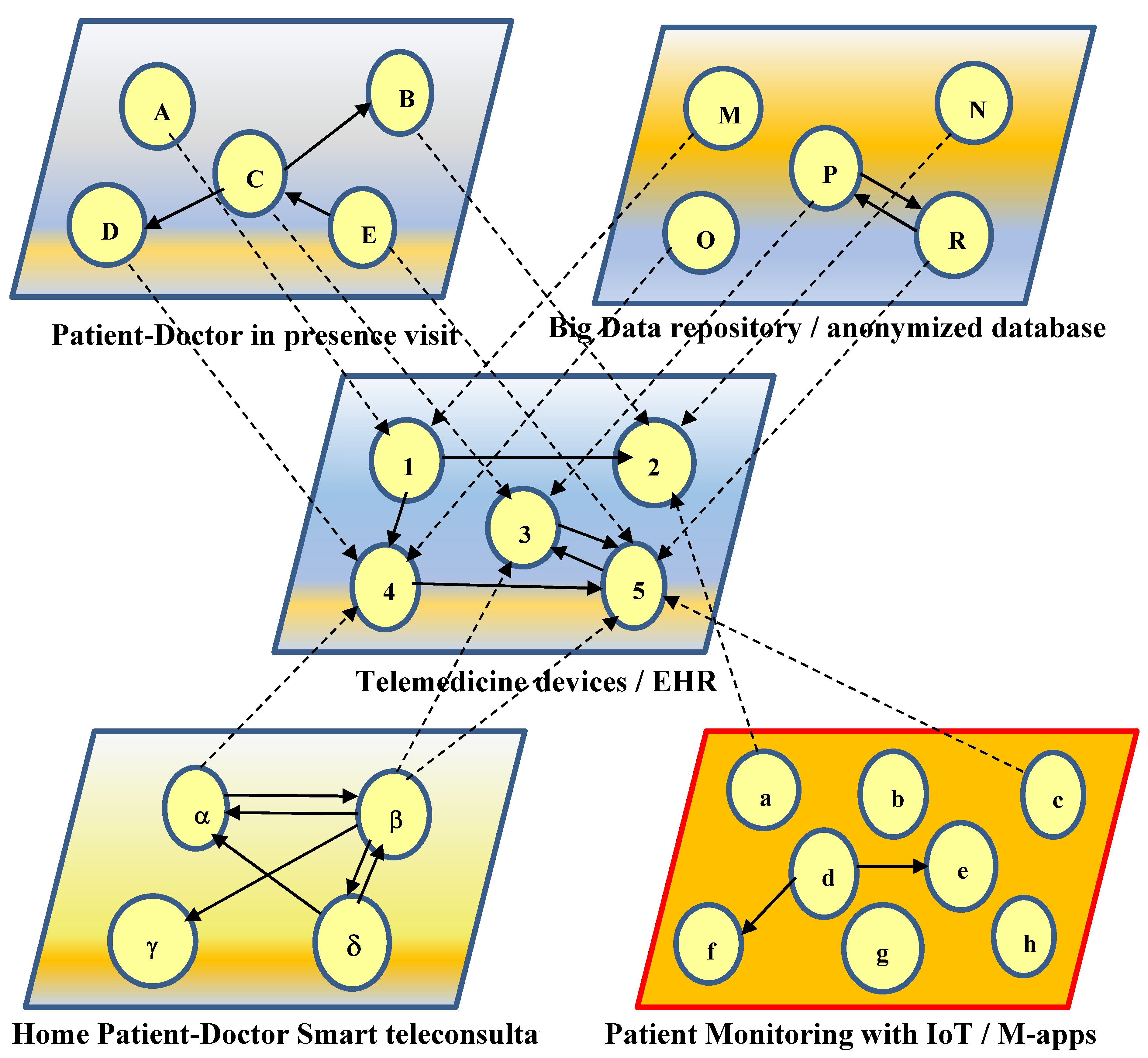
Multilayer networks are connected through copula nodes, which improve the overall scalability of the whole ecosystem (with additional nodes and links connecting adjacent layers).
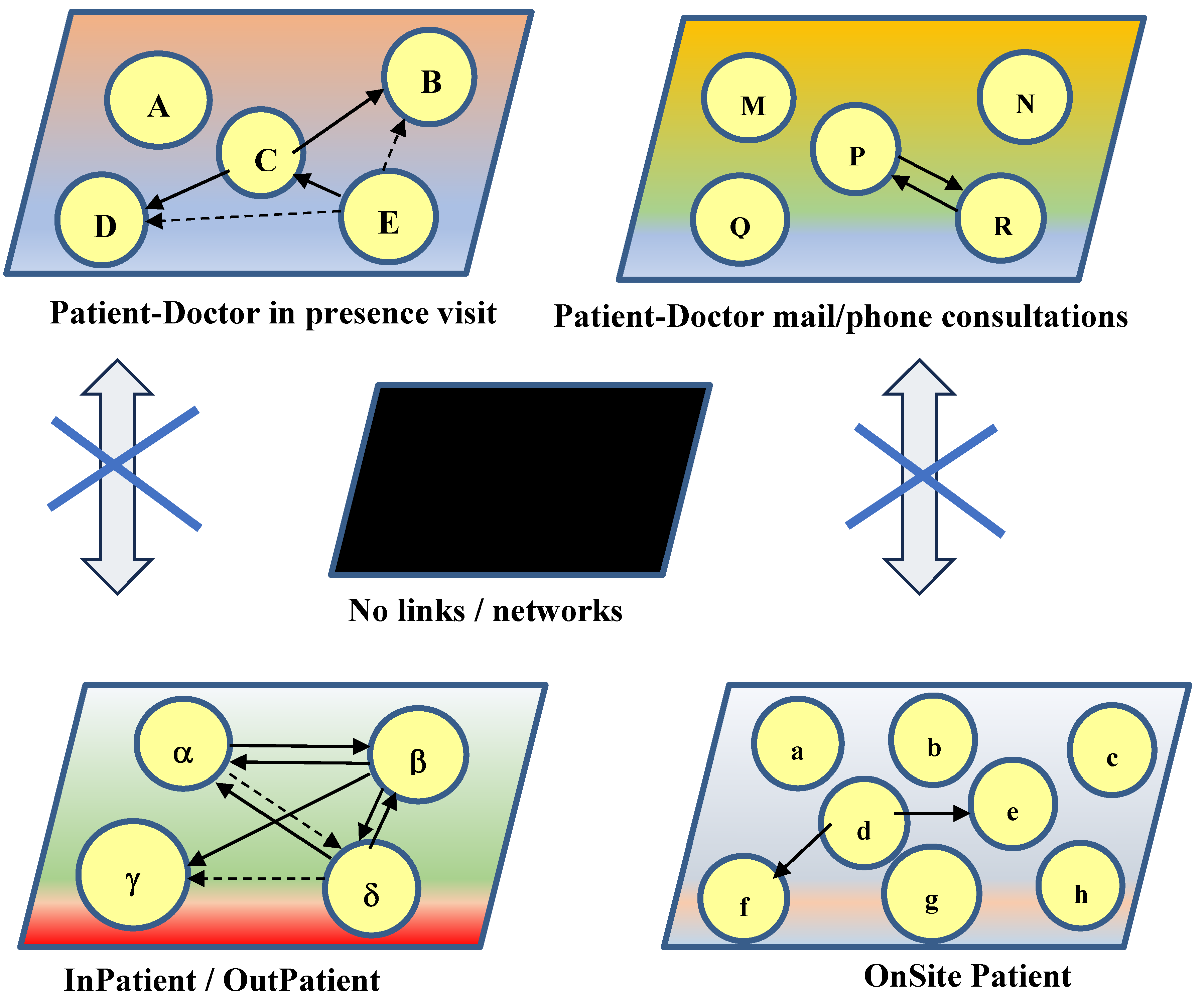
Figure 1 and
Figure 2 explain the value creation process when introducing digital health platforms, linking previously unrelated layers, and modifying the healthcare ecosystem accordingly.
The obstacles encountered within these ecosystems encompass data diversity, multidimensionality, and the need for knowledge-driven frameworks to handle unstructured healthcare Big Data proficiently. Moreover, mechanisms that underpin the sharing of inter-organizational digital transformation knowledge within these ecosystems are indispensable for effective implementation and expansion, underscoring the significance of formal and informal networking in expediting learning and knowledge dissemination. Through the integration of multilayer networks and the cultivation of collaborative interactions, scalable digital health ecosystems have the potential to propel progress in healthcare delivery and responsiveness to unforeseen crises.
Building up the adjacent (block) matrices corresponding to the above networks shows the increase in edges in the economic system.
A “with-or-without” differential (incremental) approach, consistent with the International Valuation Standard 210 applicable to intangibles, can be used. Compare
Figure 1 (where layers are not connected) with
Figure 2 (where digital health applications leverage scalable interactions among adjacent layers through connecting copula nodes).
Synergies, in the form of economies of scale and experience (horizontal and vertical scalability), value co-creation patterns (where patients interact with doctors and devices, providing information and receiving feedback), and real options (to expand or suspend the investments, according to their outcome) positively influence the public healthcare ecosystem, in terms of cost savings, improved performance, and value for money.
8. Discussion
The use of computational algorithms in multilayer networks aids in identifying vulnerable populations. Neural networks contribute to the high effectiveness of detecting health risks like hypertension. The integration of varied health intelligence data improves disease detection and prediction capabilities. Digital health utilizes various technological tools to improve healthcare services and patient outcomes.
The application of network theory in digital health provides notable benefits; however, implementing interoperable multilayer networks encounters obstacles that require thorough examination. Investments in standardized data formats and protocols are essential to improve data processing capabilities, ensure accessibility, and enhance overall data quality within healthcare institutions. Regulatory frameworks supporting data interoperability while preserving patient confidentiality are critical for advancing patient-focused digital health solutions. Fog computing provides a potential solution by bringing computing services closer to end devices in healthcare settings, addressing challenges such as data security, interoperability, and infrastructure support for IoT devices.
While the potential advantages of utilizing network theory within digital health are undoubtedly substantial and promising, executing interoperable multilayer networks encounters various obstacles that necessitate careful consideration.
These challenges notably involve intricate data privacy and security matters, paramount in safeguarding sensitive information. The challenges also revolve around establishing standardized data formats and protocols to ensure seamless interoperability and exchange among various systems and platforms. Such investments are essential for enhancing data processing capabilities, providing data accessibility, and promoting overall data quality within organizations. Additionally, regulatory frameworks that support data interoperability without compromising patient confidentiality are needed.
Interconnected networks across multiple layers are vital in shaping innovative digital healthcare solutions to prioritize patient needs. They enhance the quality and efficiency of healthcare delivery, improve patient outcomes, and enable more personalized and accessible care. As technology evolves, the importance of interoperability in healthcare will continue to grow, highlighting the need for ongoing efforts to improve data sharing and system integration.
Multilayered networks elevate the fusion of data, empowering bespoke and seamless healthcare while facilitating timely actions. Yet, embracing these advantages demands tackling technical, regulatory, and operational hurdles.
Digital health devices can conveniently use fog computing (Mutlag et al., 2019)—an architectural framework that brings computing, storage, and networking services closer to the end devices or “the edge” of the network. It acts as an intermediary layer between cloud data centers and IoT devices. In healthcare, fog computing can process data locally on smart devices or nearby computing nodes, reducing the reliance on distant cloud servers. This proximity to data sources allows quicker response times, which is crucial in medical emergencies. While fog computing and IoT offer significant benefits for smart healthcare, there are challenges to address, including interoperability between devices, data security concerns, and robust infrastructure to support these technologies. Moreover, ensuring the reliability and accuracy of IoT devices is critical for making life-saving decisions in healthcare.
9. Conclusion
The correlation between digital health and multilayer networks lies in the significant potential of interoperable networks to completely revolutionize public health outcomes and the delivery of healthcare services. Multilayer networks are instrumental in bolstering accessibility, streamlining processes, and promoting data-informed decision-making within public digital health.
These networks facilitate smooth data exchange and seamless integration across various healthcare systems and providers, resulting in considerable cost reductions, eliminating redundancies, optimizing resource distribution, and reducing unnecessary procedures. Through the implementation of cutting-edge multilayer network analysis techniques, public digital health initiatives can secure financial viability, enhance interoperability, and boost operational efficiency, thereby bringing about a fundamental shift in the delivery of patient care and promoting a patient-centered approach.
The seamless integration of telehealth and telecare in digital health transcends boundaries, enabling continuous patient-doctor interactions. Utilizing anonymized healthcare big data, validated by blockchains and analyzed with artificial intelligence, enhances scalability and efficiency in healthcare systems.
Multilayer networks act as a crucial bridge, simplifying the incorporation of digital health technologies and enhancing the delivery of remote healthcare services. Prioritizing network stability, security, and proactive maintenance enhances the reliability and effectiveness of digital health services.
Digital health integrates telehealth and telecare into a unified platform, transforming patient-doctor interactions by surpassing spatial and temporal limitations, expanding connections, and enriching relationships. Utilizing anonymized healthcare big data, verified through blockchains and interpreted using artificial intelligence, produces scalable advantages for the healthcare system.
This strategy facilitates remote health monitoring, providing accessibility, cost-efficiency, continuous surveillance, early identification, data-informed decision-making, patient empowerment, and expandability. Multilayer networks serve as a link, easing the integration of digital health technologies and improving the provision of remote healthcare services.
This novel approach emphasizes network stability, security, usability, and proactive upkeep, enhancing digital health services’ dependability, efficiency, and efficacy and ultimately elevating healthcare provision and patient outcomes.
Digital health is a powerful catalyzer of patient-doctor interaction, bypassing spatial and temporal limits (anywhere, anytime, 24/7) and increasing the number of nodes (patients, doctors, other stakeholders, devices, etc.) and their edging relationships. Anonymized healthcare big data collected in repository databases can be validated with blockchains and interpreted with artificial intelligence algorithms. This validation produces valuable and scalable effects that benefit the whole healthcare ecosystem.
Remote health monitoring offers numerous benefits, including accessibility, cost-effectiveness, continuous monitoring, early detection, data-driven decision-making, patient empowerment, and scalability (Pramanik et al., 2019).
Integrating telehealth and telecare into a cohesive platform for the healthcare monitoring sector represents a significant advancement in personalized and preventive care, particularly for older people. When effectively combined, these technologies can offer a comprehensive view of an individual’s well-being, encompassing physical, mental, and psychological health (Lamprinakos et al., 2015).
Digital health implementation requires significant adjustments in technology infrastructure and organizational processes (Alami et al., 2019). Through their connecting interlayer copula nodes, multilayer networks represent a bridge that eases adoption, softening technical and operational bottlenecks.
The link between digital health and multilayer networks fosters the successful delivery of remote healthcare services. Multilayer networks provide the necessary infrastructure to support the diverse, scalable, secure, and reliable operation of digital health, enabling healthcare providers to offer superior care to patients remotely.
New research avenues may well investigate the advances made possible by artificial intelligence interpretation, blockchain validation, interoperable data warehousing in the cloud, and other digital asset processes. In terms of improved quality, timeliness, and cost savings, the public utility follows as a natural byproduct of these value co-creating patterns, where complementary stakeholders interact, rotating around a patient-centric approach.
The digital health system driven by multinetwork integration and remote control offers a comprehensive solution to common challenges encountered in traditional digital health setups (Wang et al., 2023). By prioritizing network stability, interconnection, remote management, security, usability, and proactive maintenance, this innovative approach enhances the reliability, efficiency, and effectiveness of digital health services, ultimately improving healthcare delivery and patient outcomes.
References
- Alami, H.; Gagnon, M.P.; Fortin, J.P. Some multidimensional unintended consequences of telehealth utilization: a multi-project evaluation synthesis. International journal of health policy and management 2019, 8, 337. [Google Scholar] [CrossRef] [PubMed]
- Balram, N.; Tošić, I.; Binnamangalam, H. Digital health in the age of The Infinite Network. APSIPA Transactions on Signal and Information Processing 2016, 5, e5. [Google Scholar] [CrossRef]
- Barabási, L. (2016). Network Science. Cambridge University Press.
- Barabási, A.L.; Albert, R. Emergence of scaling in random networks. Science 1999, 286, 509–512. [Google Scholar] [CrossRef]
- Bianconi, G. (2018). Multilayer Networks. Oxford University Press.
- Bloom, G.; Balasubramaniam, P.; Marin, A.; Nelson, E.; Quak, E.; Husain, L.; Barker, T. (2023). Towards digital transformation for universal health coverage. Institute of Development Studies, Brighton.
- Channi, H.K.; Shrivastava, P.; Chowdhary, C.L. (2022). Digital Transformation in Healthcare Industry: A Survey. In Next Generation Healthcare Informatics (pp. 279-293). Singapore: Springer Nature Singapore.
- Dhaduk, K.; Miller, D.; Schliftman, A.; Athar, A.; Al Aseri, Z.A.; Echevarria, A.; Becker, C. Implementing and optimizing in-patient access to dermatology consultations via telemedicine: an experiential study. Telemedicine and e-Health 2021, 27, 68–73. [Google Scholar] [CrossRef]
- Deloitte. (2015). Accelerating the adoption of connected health. https://www2.deloitte.com/content/dam/Deloitte/us/Documents/life-sciences-health-care/us-dchs-connected-health.pdf.
- Evers, E.C.; Fritz, S.A.; Colditz, G.A.; Burnham, J.P. Perceptions of telemedicine and costs incurred by a visit to a general infectious diseases’ clinic: a survey. Open Forum Infectious Diseases 2022, 9, ofab661. [Google Scholar] [CrossRef] [PubMed]
- Fareed, M.; Yassin, A.A. A lightweight and secure multilayer authentication scheme for wireless body area networks in healthcare system. International Journal of Electrical and Computer Engineering 2023, 13, 1782. [Google Scholar] [CrossRef]
- Geng, Q.; Chuai, Z.; Jin, J. (2024). An Integrated Healthcare Service System Based on Blockchain Technologies. IEEE Transactions on Computational Social Systems.
- Groom, L.L.; McCarthy, M.M.; Stimpfel, A.W.; Brody, A.A. Telemedicine and telehealth in nursing homes: an integrative review. Journal of the American Medical Directors Association 2021, 22, 1784–1801. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sensors international 2021, 2, 100117. [Google Scholar] [CrossRef] [PubMed]
- Hallberg, D.; Salimi, N. Qualitative and Quantitative Analysis of Definitions of e-Health and m-Health. Healthcare informatics research 2020, 26, 119–128. [Google Scholar] [CrossRef]
- Hyder, M.A.; Razzak, J. Telemedicine in the United States: an introduction for students and residents. Journal of medical Internet research 2020, 22, e20839. [Google Scholar] [CrossRef]
- Jandoo, T. WHO guidance for digital health: What it means for researchers. Digital Health 2020, 6. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Krowski, N.; Rodriguez, B.; Tran, L.; Vela, J.; Brooks, M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Lamprinakos, G.C.; Asanin, S.; Broden, T.; Prestileo, A.; Fursse, J.; Papadopoulos, K.A.; Venieris, I.S. An integrated remote monitoring platform towards telehealth and telecare services interoperability. Information Sciences 2015, 308, 23–37. [Google Scholar] [CrossRef]
- Leite, H.; Hodgkinson, I.R.; Gruber, T. New development: ‘Healing at a distance’—telemedicine and COVID-19. Public money & management 2020, 40, 483–485. [Google Scholar]
- Loza, O.; Gomez-Lopez, I.; Mikler, A.R. Multi-coaffiliation networks and public health applications. GSTF Journal of BioSciences 2012, 2. [Google Scholar] [CrossRef]
- Mahtta, D.; Daher, M.; Lee, M.T.; Sayani, S.; Shishehbor, M.; Virani, S.S. Promise and perils of telehealth in the current era. Current cardiology reports 2021, 23, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Massaro, A.; Maritati, V.; Savino, N.; Galiano, A.; Convertini, D.; De Fonte, E.; Di Muro, M. A study of a health resources management platform integrating neural networks and DSS telemedicine for homecare assistance. Information 2018, 9, 176. [Google Scholar] [CrossRef]
- McKinsey. (2021). Telehealth: A quarter-trillion-dollar post-COVID-19 reality? https://www.mckinsey.com/industries/healthcare/our-insights/telehealth-a-quarter-trillion-dollar-post-covid-19-reality.
- Mishra, S.; Bhutia, S.D.; Akhtar, N.; Dhar, S. (2019). Cloud-Based Multilayer Telemedicine Architecture: A Case Study. Advances in Communication, Devices and Networking: Proceedings of ICCDN 2018. Springer Singapore, 553–561).
- Moro-Visconti, R. Connecting patient-centric blockchains with multilayer P2P networks and digital platforms. Blockchain in Digital Healthcare. Chapman and Hall/CRC 2021, 93–112.
- Moro-Visconti, R.; Martiniello, L. Smart hospitals and patient-centered governance. Corporate Ownership & Control 2019, 16.
- Mutlag, A.A.; Abd Ghani, M.K.; Arunkumar, N.A.; Mohammed, M.A.; Mohd, O. Enabling technologies for fog computing in healthcare IoT systems. Future generation computer systems 2019, 90, 62–78. [Google Scholar] [CrossRef]
- Noorbakhsh-Sabet, N.; Zand, R.; Zhang, Y.; Abedi, V. Artificial intelligence transforms the future of health care. The American journal of medicine 2019, 132, 795–801. [Google Scholar] [CrossRef]
- Osipov, V.S.; Skryl, T.V. (2021). Impact of digital technologies on the efficiency of healthcare delivery. In IoT in Healthcare and Ambient Assisted Living (pp. 243-261). Singapore: Springer Singapore.
- Palanisamy, V.; Thirunavukarasu, R. Implications of big data analytics in developing healthcare frameworks–A review. Journal of King Saud University-Computer and Information Sciences 2019, 31, 415–425. [Google Scholar] [CrossRef]
- Pathinarupothi, R.K.; Ramesh, M.V.; Rangan, E. Multilayer architectures for remote health monitoring. 2016 IEEE 18th International Conference on e-Health Networking, Applications and Services (Healthcom) 2016, 1–6.
- Peyroteo, M.; Ferreira, I.A.; Elvas, L.B.; Ferreira, J.C.; Lapão, L.V. Remote monitoring systems for patients with chronic diseases in primary health care: systematic review. JMIR mHealth and uHealth 2021, 9, e28285. [Google Scholar] [CrossRef] [PubMed]
- Poitras, M.E.; Maltais, M.E.; Bestard-Denommé, L.; Stewart, M.; Fortin, M. What are the effective elements in patient-centered and multimorbidity care? A scoping review. BMC health services research 2018, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Pramanik, P.K.D.; Nayyar, A.; Pareek, G. (2019). WBAN: Driving e-healthcare beyond telemedicine to remote health monitoring: Architecture and protocols. In Telemedicine technologies. Academic Press, 89–119.
- Rahimi NI, M.; Yatya, S.M.; Bakar, N.A.A. Enterprise Architecture: Enabling Digital Transformation for Healthcare Organization. Open International Journal of Informatics 2023, 11, 67–73. [Google Scholar] [CrossRef]
- Rashida, M.M. Predicting Determinants of Telemedicine Adoption in Healthcare: An Artificial Neural Network Approach. International Journal of Engineering Research & Technology 2023, 12.
- Satamraju, K.P. Proof of concept of scalable integration of internet of things and blockchain in healthcare. Sensors 2020, 20, 1389. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.; Ostinelli, E.; Macdonald, O.; Cipriani, A. COVID-19 and telepsychiatry: development of evidence-based guidance for clinicians. JMIR mental health 2020, 7, e21108. [Google Scholar] [CrossRef] [PubMed]
- Snoswell, C.L.; Taylor, M.L.; Comans, T.A.; Smith, A.C.; Gray, L.C.; Caffery, L.J. Determining if telehealth can reduce health system costs scoping review. Journal of medical Internet research 2020, 22. [Google Scholar] [CrossRef]
- Upadhyay, S. Implementation levels of electronic health records and their influence on quality and safety. Online Journal of Nursing Informatics 2023, 26. [Google Scholar]
- van der Weert, G.; Burzynska, K.; Knoben, J. An integrative perspective on interorganizational multilevel healthcare networks: a systematic literature review. BMC health services research 2022, 22, 923. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Zhang, J.; He, S.; Guo, H.; Li, T.; Zhong, Q.; He, K. Design and application of a novel telemedicine system jointly driven by multinetwork integration and remote control: Practical experience from PLAGH, China. Healthcare Technology Letters 2023, 10, 113–121. [Google Scholar] [CrossRef]
- Woods, L.; Eden, R.; Canfell, O.J.; Nguyen, K.H.; Comans, T.; Sullivan, C. Show me the money: how do we justify spending health care dollars on digital health? The Medical Journal of Australia 2023, 218, 53. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).