Submitted:
27 June 2024
Posted:
01 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Endometrial Cancer
3. Genetic Correlation
| Program | Ref | Description | Data Input1 | Examples2 |
|---|---|---|---|---|
| Genetic correlation | ||||
| BOLT-REML | [20] | A Monte Carlo algorithm for variance component analysis to estimate genetic correlations and partition SNP heritability among multiple phenotypes. Computationally fast. | Individual | 37340002 30929738 |
| GenomicSEM | [21] | Synthesizes genetic correlations of multiple traits with unknown amounts of sample overlap | Summary | 32606422 35513722 |
| GCTA | [22] | Provides highly accurate estimates of genetic correlations between phenotypes while accounting for different genetic architectures. | Individual | 24944428 |
| PCGC-s | [23] | Estimates genetic correlation and partitioned heritability large datasets while accounting for case-control sampling and covariates. | Summary | 31488892 |
| LD Score Regression | [24] | Estimates genetic correlations across multiple phenotypes while accounting for cryptic relatedness and population stratification. | Summary | 30093612 29608257 26414676 |
| HDL | [25] | Highly powered and accurate estimates of genetic correlations fully account for whole genome LD and reduce the variance of genetic correlation estimates. | Summary | 35492879 34997191 |
| MTG2 | [26] | Combines the average information algorithm used by REML with an eigen-decomposition of the genomic relationship matrix to estimate genetic variance. | Individual | 29977057 35729236 |
| GNOVA | [27] | Provides powerful statistical inference through annotation-stratified genetic covariance analysis that is robust to LD and sample overlap. | Summary | 37034223 34634379 |
| ρ-HESS | [28] | Localized and precise quantification of genetic correlation between pairs of traits due to small-region genetic variation. Accounts for LD and sample overlap while making no distributional assumptions on the causal effect size under a fixed effects model. | Summary | 34355204 34561436 |
| LAVA | [29] | Tests local genetic correlation between two phenotypes. Can also analyze local heritability and conditional genetic relationships between several phenotypes. | Summary | 36471075 38637617 |
| Colocalization | ||||
| COLOC | [30] | Bayesian statistical test to enable the computation of probabilities that two traits share a common genetic causal variant from single variant association p-values and MAFs. Locus-specific analysis. | Summary | 34268601 34355204 |
| GWAS-PW | [31] | Bayesian statistical test to enable the computation of probabilities that two traits share a common genetic causal variant from single variant association p-values and MAFs. Locus-specific analysis. | Summary | 33144283 35178771 35851147 |
| Cross-Trait Locus Identification | ||||
| MTAG | [32] | Joint analysis of multiple traits to increase statistical power and account for sample overlap. | Summary | 34268601 31488892 29292387 |
| CPASSOC | [33] | Assess cross-phenotype associations for both continuous or binary traits. | Summary | 37636041 31669095 |
| MV-PLINK | [34] | Computationally fast implementation of canonical correlation analysis, including multiple phenotypes and uses | Individual | 35278618 |
| MultiPhen | [35] | Employs ordinal regression for joint multivariate modelling of multiple phenotypes, with increased statistical power and an appropriate type 1 error rate. | Individual | 35701404 35680855 |
| conjFDR | [36] | A model-free strategy for analysis that leverages genetic overlap between two phenotypes which boosts statistical power and identifies shared genomic association regardless of the cross-trait correlations. | Summary | 37752828 31792363 |
| bGWAS | [37] | A Bayesian method that leverages published studies for related risk factors to construct priors. Increase power to identify susceptibility variants and allows for assessment of posterior and direct effects. | Summary | 37168552 35653391 |
| RE2C | [38] | A generalized likelihood model that accounts for correlations of statistics and achieves optimal power under the condition of heterogeneity | Summary | 35492870 3734002 35753705 |
| MetABF | [39] | Employs a Bayesian framework using both an independent and fixed effect model to meta-analysis GWAS statistics. An efficient tool that allows the expected relationships between studies or traits to be encoded in the analysis. | Summary | 36653479 35492870 |
| Causal Inference | ||||
| LCVA | [40] | Distinguishes causal relationships among genetically correlated phenotypes such that a positive result is more likely to be the true causal effect. | Summary | 36653534 36151087 31669095 |
| MiXer | [41] | Applies a bivariate causal model to quantify and visualize polygenic overlap by estimating the total number of shared and trait-specific causal variants. | Summary | 37752828 34761251 |
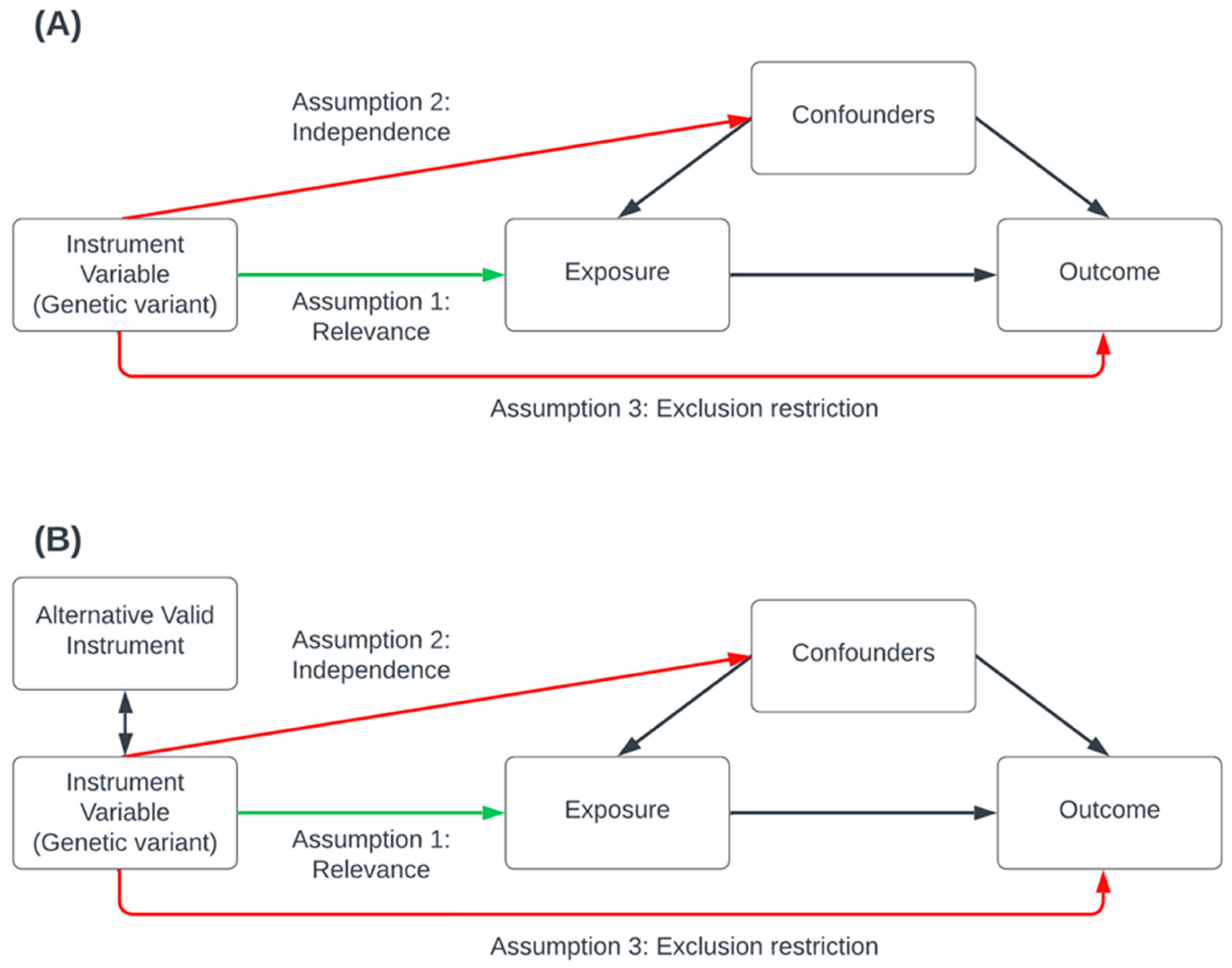
| Mendelian randomization | [42] | Uses instrument variables in statistical models to identify causal relationships between an exposure and outcome. Various programs and techniques have been developed (see Table 2) | Both | 34268601 |
4. Colocalization
5. Cross-Trait Locus Identification
6. Causal Inference Analysis
| Methods | Ref | Description |
|---|---|---|
| Packages | ||
| MR-Base | [66] | A web platform housing GWAS summary statistics that can perform two-sample MR analyses |
| MendelianRandomization | [67] | R software package that implements several methods for MR analyses based on summary statistics including multivariable MR |
| CAUSE | [68] | R software package for MR analysis accounting for both uncorrelated and correlated horizontal pleiotropy effects |
| TwoSampleMR | [69] | R software package to perform a range of two-sample MR analyses using GWAS summary data from two independent exposure and outcome cohorts. |
| OneSampleMR | [70] | R software package to perform a range of one-sample MR analyses using GWAS data from a single cohort (individual-level data) |
| Consistency Assumption: Instrument Strength Independent of Direct Effect | ||
| MR-Egger | [71] | A sensitivity analysis tool used to test for bias from pleiotropy caused by some genetic variants having multiple proximal phenotypic correlations, making them invalid instrumental variables. Egger’s test provides a valid causal effect estimate when some or all the genetic variants are invalid instrumental variables. |
| Consistency Assumption: Majority Valid | ||
| Weight-median | [72] | A sensitivity analysis tool that uses GWAS summary data for MR with multiple genetic variants. Provides a consistent causal effect estimate even when up to 50% of the information comes from invalid instrumental variables. |
| Consistency Assumption: Plurality Valid | ||
| Weighted-MBE | [73] | A sensitivity analysis tool using summary data that is robust to horizontal pleiotropy. Provides a consistent causal estimate when the largest number of similar individual-instrument causal effect estimates comes from valid instruments, even if the majority of instruments are invalid. |
| Consistency Assumption: Horizontal pleiotropy around 0 | ||
| MR-LDP | [74] | An efficient variational Bayesian expectation-maximization algorithm using GWAS summary statistics to estimate the causal effects of complex traits that have multiple instrumental variants within LD. The random component eliminates the impact of horizontal pleiotropy. |
| MR-RAPS | [75] | Uses GWAS summary data under a random-effect model to estimate the causal effects of genetic variants while accounting[68] for pleiotropy. It is robust to outliers but sensitive to the assumption that pleiotropy is normally distributed around 0. |
| Consistency Assumption: Outlier-robust | ||
| GSMR + HEIDI | [76] | Uses summary GWAS data to perform MR analysis by accounting for LD between the variants, thereby improving statistical power. Detects and accounts for outliers that could violate MR assumptions. |
| MR-GRAPPLE | [77] | Uses GWAS summary statistics to identify multiple pleiotropic pathways and determine the causal effect, under a likelihood model pervasive pleiotropy accounted for as long as the InSIDE assumption holds for all genetic instruments. |
| MR-Lasso | [65] | Extension of the IVW-MR framework by adding an intercept term for each genetic variant and a lasso penalty term for identification. Aim removes a potential source of bias (outliers) that could violate the analysis's assumptions. |
| MR-Robust | [65] | IVW method is performed by regression resulting in MM-estimation (robust against influential points) and Tukey's loss function (robust against outliers). Aims to downweigh outliers which could cause a violation of the assumptions underlying the analysis. |
| MR-PRESSO | [78] | Uses summary-level data to test and correct for horizontal pleiotropic outliers using a regression framework to “leave-one-out” approach which detects and removes outliers from the analysis to determine which SNP is driving the difference in computed residual sum of squares. |
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Uffelmann, E.; Huang, Q.Q.; Munung, N.S.; de Vries, J.; Okada, Y.; Martin, A.R.; Martin, H.C.; Lappalainen, T. Genome-Wide Association Studies. Nature Reviews Methods Primers 2021, 1, 1–21. [Google Scholar] [CrossRef]
- Gu, B.; Shang, X.; Yan, M.; Li, X.; Wang, W.; Wang, Q.; Zhang, C. Variations in Incidence and Mortality Rates of Endometrial Cancer at the Global, Regional, and National Levels, 1990–2019. Gynecol. Oncol. 2021, 161, 573–580. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Crosbie, E.J.; Kitson, S.J.; McAlpine, J.N.; Mukhopadhyay, A.; Powell, M.E.; Singh, N. Endometrial Cancer. Lancet 2022, 399, 1412–1428. [Google Scholar] [CrossRef] [PubMed]
- Kitson, S.J.; Crosbie, E.J. Endometrial Cancer and Obesity. Obstet. Gynaecol. 2019, 21, 237–245. [Google Scholar] [CrossRef]
- Setiawan, V.W.; Yang, H.P.; Pike, M.C.; McCann, S.E.; Yu, H.; Xiang, Y.-B.; Wolk, A.; Wentzensen, N.; Weiss, N.S.; Webb, P.M.; et al. Type I and II Endometrial Cancers: Have They Different Risk Factors? J. Clin. Oncol. 2013, 31, 2607–2618. [Google Scholar] [CrossRef] [PubMed]
- Raglan, O.; Kalliala, I.; Markozannes, G.; Cividini, S.; Gunter, M.J.; Nautiyal, J.; Gabra, H.; Paraskevaidis, E.; Martin-Hirsch, P.; Tsilidis, K.K.; et al. Risk Factors for Endometrial Cancer: An Umbrella Review of the Literature. Int. J. Cancer 2019, 145, 1719–1730. [Google Scholar] [CrossRef] [PubMed]
- Kaaks, R.; Lukanova, A.; Kurzer, M.S. Obesity, Endogenous Hormones, and Endometrial Cancer Risk: A Synthetic Review. Cancer Epidemiol. Biomarkers Prev. 2002, 11, 1531–1543. [Google Scholar] [PubMed]
- Mucci, L.A.; Hjelmborg, J.B.; Harris, J.R.; Czene, K.; Havelick, D.J.; Scheike, T.; Graff, R.E.; Holst, K.; Möller, S.; Unger, R.H.; et al. Familial Risk and Heritability of Cancer Among Twins in Nordic Countries. JAMA 2016, 315, 68–76. [Google Scholar] [CrossRef]
- Lu, Y.; Ek, W.E.; Whiteman, D.; Vaughan, T.L.; Spurdle, A.B.; Easton, D.F.; Pharoah, P.D.; Thompson, D.J.; Dunning, A.M.; Hayward, N.K.; et al. Most Common “sporadic” Cancers Have a Significant Germline Genetic Component. Hum. Mol. Genet. 2014, 23, 6112–6118. [Google Scholar] [CrossRef]
- Johnatty, S.E.; Tan, Y.Y.; Buchanan, D.D.; Bowman, M.; Walters, R.J.; Obermair, A.; Quinn, M.A.; Blomfield, P.B.; Brand, A.; Leung, Y.; et al. Family History of Cancer Predicts Endometrial Cancer Risk Independently of Lynch Syndrome: Implications for Genetic Counselling. Gynecol. Oncol. 2017, 147, 381–387. [Google Scholar] [CrossRef]
- Lichtenstein Paul; Holm Niels V.; Verkasalo Pia K.; Iliadou Anastasia; Kaprio Jaakko; Koskenvuo Markku; Pukkala Eero; Skytthe Axel; Hemminki Kari Environmental and Heritable Factors in the Causation of Cancer — Analyses of Cohorts of Twins from Sweden, Denmark, and Finland. N. Engl. J. Med. 343, 78–85. [CrossRef]
- Spurdle, A.B.; Bowman, M.A.; Shamsani, J.; Kirk, J. Endometrial Cancer Gene Panels: Clinical Diagnostic vs Research Germline DNA Testing. Mod. Pathol. 2017, 30, 1048–1068. [Google Scholar] [CrossRef] [PubMed]
- Dörk, T.; Hillemanns, P.; Tempfer, C.; Breu, J.; Fleisch, M.C. Genetic Susceptibility to Endometrial Cancer: Risk Factors and Clinical Management. Cancers 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Ryan, N.A.J.; Glaire, M.A.; Blake, D.; Cabrera-Dandy, M.; Evans, D.G.; Crosbie, E.J. The Proportion of Endometrial Cancers Associated with Lynch Syndrome: A Systematic Review of the Literature and Meta-Analysis. Genet. Med. 2019, 21, 2167–2180. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, D.D.; Tan, Y.Y.; Walsh, M.D.; Clendenning, M.; Metcalf, A.M.; Ferguson, K.; Arnold, S.T.; Thompson, B.A.; Lose, F.A.; Parsons, M.T.; et al. Tumor Mismatch Repair Immunohistochemistry and DNA MLH1 Methylation Testing of Patients with Endometrial Cancer Diagnosed at Age Younger than 60 Years Optimizes Triage for Population-Level Germline Mismatch Repair Gene Mutation Testing. J. Clin. Oncol. 2014, 32, 90–100. [Google Scholar] [CrossRef]
- O’Mara, T.A.; Glubb, D.M.; Kho, P.F.; Thompson, D.J.; Spurdle, A.B. Genome-Wide Association Studies of Endometrial Cancer: Latest Developments and Future Directions. Cancer Epidemiol. Biomarkers Prev. 2019, 28, 1095–1102. [Google Scholar] [CrossRef]
- Wang, X.; Glubb, D.M.; O’Mara, T.A. 10 Years of GWAS Discovery in Endometrial Cancer: Aetiology, Function and Translation. EBioMedicine 2022, 77, 103895. [Google Scholar] [CrossRef]
- O’Mara, T.A.; Glubb, D.M.; Amant, F.; Annibali, D.; Ashton, K.; Attia, J.; Auer, P.L.; Beckmann, M.W.; Black, A.; Bolla, M.K.; et al. Identification of Nine New Susceptibility Loci for Endometrial Cancer. Nat. Commun. 2018, 9, 3166. [Google Scholar] [CrossRef] [PubMed]
- Loh, P.-R.; Bhatia, G.; Gusev, A.; Finucane, H.K.; Bulik-Sullivan, B.K.; Pollack, S.J.; Schizophrenia Working Group of Psychiatric Genomics Consortium; de Candia, T.R.; Lee, S.H.; Wray, N.R.; et al. Contrasting Genetic Architectures of Schizophrenia and Other Complex Diseases Using Fast Variance-Components Analysis. Nat. Genet. 2015, 47, 1385–1392. [CrossRef]
- Grotzinger, A.D.; Rhemtulla, M.; de Vlaming, R.; Ritchie, S.J.; Mallard, T.T.; Hill, W.D.; Ip, H.F.; Marioni, R.E.; McIntosh, A.M.; Deary, I.J.; et al. Genomic Structural Equation Modelling Provides Insights into the Multivariate Genetic Architecture of Complex Traits. Nat. Hum. Behav. 2019, 3, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Lee, S.H.; Goddard, M.E.; Visscher, P.M. GCTA: A Tool for Genome-Wide Complex Trait Analysis. Am. J. Hum. Genet. 2011, 88, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Weissbrod, O.; Flint, J.; Rosset, S. Estimating SNP-Based Heritability and Genetic Correlation in Case-Control Studies Directly and with Summary Statistics. Am. J. Hum. Genet. 2018, 103, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Bulik-Sullivan, B.; Finucane, H.K.; Anttila, V.; Gusev, A.; Day, F.R.; Loh, P.-R.; ReproGen Consortium; Psychiatric Genomics Consortium; Genetic Consortium for Anorexia Nervosa of the Wellcome Trust Case Control Consortium 3; Duncan, L.; et al. An Atlas of Genetic Correlations across Human Diseases and Traits. Nat. Genet. 2015, 47, 1236–1241. [CrossRef]
- Ning, Z.; Pawitan, Y.; Shen, X. High-Definition Likelihood Inference of Genetic Correlations across Human Complex Traits. Nat. Genet. 2020, 52, 859–864. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; van der Werf, J.H.J. MTG2: An Efficient Algorithm for Multivariate Linear Mixed Model Analysis Based on Genomic Information. Bioinformatics 2016, 32, 1420–1422. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Li, B.; Ou, D.; Erlendsdottir, M.; Powles, R.L.; Jiang, T.; Hu, Y.; Chang, D.; Jin, C.; Dai, W.; et al. A Powerful Approach to Estimating Annotation-Stratified Genetic Covariance via GWAS Summary Statistics. Am. J. Hum. Genet. 2017, 101, 939–964. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Mancuso, N.; Spendlove, S.; Pasaniuc, B. Local Genetic Correlation Gives Insights into the Shared Genetic Architecture of Complex Traits. Am. J. Hum. Genet. 2017, 101, 737–751. [Google Scholar] [CrossRef] [PubMed]
- Werme, J.; van der Sluis, S.; Posthuma, D.; de Leeuw, C.A. An Integrated Framework for Local Genetic Correlation Analysis. Nat. Genet. 2022, 54, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Giambartolomei, C.; Vukcevic, D.; Schadt, E.E.; Franke, L.; Hingorani, A.D.; Wallace, C.; Plagnol, V. Bayesian Test for Colocalisation between Pairs of Genetic Association Studies Using Summary Statistics. PLoS Genet. 2014, 10, e1004383. [Google Scholar] [CrossRef]
- Pickrell, J.K.; Berisa, T.; Liu, J.Z.; Ségurel, L.; Tung, J.Y.; Hinds, D.A. Detection and Interpretation of Shared Genetic Influences on 42 Human Traits. Nat. Genet. 2016, 48, 709–717. [Google Scholar] [CrossRef] [PubMed]
- Turley, P.; Walters, R.K.; Maghzian, O.; Okbay, A.; Lee, J.J.; Fontana, M.A.; Nguyen-Viet, T.A.; Wedow, R.; Zacher, M.; Furlotte, N.A.; et al. Multi-Trait Analysis of Genome-Wide Association Summary Statistics Using MTAG. Nat. Genet. 2018, 50, 229–237. [Google Scholar] [CrossRef]
- Zhu, X.; Feng, T.; Tayo, B.O.; Liang, J.; Young, J.H.; Franceschini, N.; Smith, J.A.; Yanek, L.R.; Sun, Y.V.; Edwards, T.L.; et al. Meta-Analysis of Correlated Traits via Summary Statistics from GWASs with an Application in Hypertension. Am. J. Hum. Genet. 2015, 96, 21–36. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, M.A.R.; Purcell, S.M. A Multivariate Test of Association. Bioinformatics 2009, 25, 132–133. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, P.F.; Hoggart, C.J.; Pomyen, Y.; Calboli, F.C.F.; Elliott, P.; Jarvelin, M.-R.; Coin, L.J.M. MultiPhen: Joint Model of Multiple Phenotypes Can Increase Discovery in GWAS. PLoS One 2012, 7, e34861. [Google Scholar] [CrossRef] [PubMed]
- Smeland, O.B.; Frei, O.; Shadrin, A.; O’Connell, K.; Fan, C.-C.; Bahrami, S.; Holland, D.; Djurovic, S.; Thompson, W.K.; Dale, A.M.; et al. Discovery of Shared Genomic Loci Using the Conditional False Discovery Rate Approach. Hum. Genet. 2020, 139, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Mounier, N.; Kutalik, Z. BGWAS: An R Package to Perform Bayesian Genome Wide Association Studies. Bioinformatics 2020, 36, 4374–4376. [Google Scholar] [CrossRef]
- Lee, C.H.; Eskin, E.; Han, B. Increasing the Power of Meta-Analysis of Genome-Wide Association Studies to Detect Heterogeneous Effects. Bioinformatics 2017, 33, i379–i388. [Google Scholar] [CrossRef] [PubMed]
- Trochet, H.; Pirinen, M.; Band, G.; Jostins, L.; McVean, G.; Spencer, C.C.A. Bayesian Meta-Analysis across Genome-Wide Association Studies of Diverse Phenotypes. Genet. Epidemiol. 2019, 43, 532–547. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, L.J.; Price, A.L. Distinguishing Genetic Correlation from Causation across 52 Diseases and Complex Traits. Nat. Genet. 2018, 50, 1728–1734. [Google Scholar] [CrossRef] [PubMed]
- Frei, O.; Holland, D.; Smeland, O.B.; Shadrin, A.A.; Fan, C.C.; Maeland, S.; O’Connell, K.S.; Wang, Y.; Djurovic, S.; Thompson, W.K.; et al. Bivariate Causal Mixture Model Quantifies Polygenic Overlap between Complex Traits beyond Genetic Correlation. Nat. Commun. 2019, 10, 2417. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, E.; Glymour, M.M.; Holmes, M.V.; Kang, H.; Morrison, J.; Munafò, M.R.; Palmer, T.; Schooling, C.M.; Wallace, C.; Zhao, Q.; et al. Mendelian Randomization. Nat Rev Methods Primers 2022, 2. [Google Scholar] [CrossRef]
- Rødevand, L.; Rahman, Z.; Hindley, G.F.L.; Smeland, O.B.; Frei, O.; Tekin, T.F.; Kutrolli, G.; Bahrami, S.; Hoseth, E.Z.; Shadrin, A.; et al. Characterizing the Shared Genetic Underpinnings of Schizophrenia and Cardiovascular Disease Risk Factors. Am. J. Psychiatry 2023, appiajp20220660. [Google Scholar] [CrossRef] [PubMed]
- Ohi, K.; Sumiyoshi, C.; Fujino, H.; Yasuda, Y.; Yamamori, H.; Fujimoto, M.; Shiino, T.; Sumiyoshi, T.; Hashimoto, R. Genetic Overlap between General Cognitive Function and Schizophrenia: A Review of Cognitive GWASs. Int. J. Mol. Sci. 2018, 19. [Google Scholar] [CrossRef] [PubMed]
- Romero, C.; Werme, J.; Jansen, P.R.; Gelernter, J.; Stein, M.B.; Levey, D.; Polimanti, R.; de Leeuw, C.; Posthuma, D.; Nagel, M.; et al. Exploring the Genetic Overlap between Twelve Psychiatric Disorders. Nat. Genet. 2022, 54, 1795–1802. [Google Scholar] [CrossRef] [PubMed]
- Duncan, L.E.; Shen, H.; Ballon, J.S.; Hardy, K.V.; Noordsy, D.L.; Levinson, D.F. Genetic Correlation Profile of Schizophrenia Mirrors Epidemiological Results and Suggests Link Between Polygenic and Rare Variant (22q11.2) Cases of Schizophrenia. Schizophr. Bull. 2018, 44, 1350–1361. [Google Scholar] [CrossRef] [PubMed]
- Catalá-López, F.; Suárez-Pinilla, M.; Suárez-Pinilla, P.; Valderas, J.M.; Gómez-Beneyto, M.; Martinez, S.; Balanzá-Martínez, V.; Climent, J.; Valencia, A.; McGrath, J.; et al. Inverse and Direct Cancer Comorbidity in People with Central Nervous System Disorders: A Meta-Analysis of Cancer Incidence in 577,013 Participants of 50 Observational Studies. Psychother. Psychosom. 2014, 83, 89–105. [Google Scholar] [CrossRef] [PubMed]
- Tran, E.; Rouillon, F.; Loze, J.-Y.; Casadebaig, F.; Philippe, A.; Vitry, F.; Limosin, F. Cancer Mortality in Patients with Schizophrenia: An 11-Year Prospective Cohort Study. Cancer 2009, 115, 3555–3562. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; Song, J.; Lu, Y.; Fall, K.; Chen, X.; Fang, F.; Landén, M.; Hultman, C.M.; Czene, K.; Sullivan, P.; et al. A Shared Genetic Contribution to Breast Cancer and Schizophrenia. Nat. Commun. 2020, 11, 4637. [Google Scholar] [CrossRef] [PubMed]
- Glubb, D.M.; Thompson, D.J.; Aben, K.K.H.; Alsulimani, A.; Amant, F.; Annibali, D.; Attia, J.; Barricarte, A.; Beckmann, M.W.; Berchuck, A.; et al. Cross-Cancer Genome-Wide Association Study of Endometrial Cancer and Epithelial Ovarian Cancer Identifies Genetic Risk Regions Associated with Risk of Both Cancers. Cancer Epidemiol. Biomarkers Prev. 2021, 30, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Lindström, S.; Wang, L.; Feng, H.; Majumdar, A.; Huo, S.; Macdonald, J.; Harrison, T.; Turman, C.; Chen, H.; Mancuso, N.; et al. Genome-Wide Analyses Characterize Shared Heritability among Cancers and Identify Novel Cancer Susceptibility Regions. J. Natl. Cancer Inst. 2023, 115, 712–732. [Google Scholar] [CrossRef] [PubMed]
- Masuda, T.; Low, S.-K.; Akiyama, M.; Hirata, M.; Ueda, Y.; Matsuda, K.; Kimura, T.; Murakami, Y.; Kubo, M.; Kamatani, Y.; et al. GWAS of Five Gynecologic Diseases and Cross-Trait Analysis in Japanese. Eur. J. Hum. Genet. 2020, 28, 95–107. [Google Scholar] [CrossRef] [PubMed]
- Painter, J.N.; O’Mara, T.A.; Morris, A.P.; Cheng, T.H.T.; Gorman, M.; Martin, L.; Hodson, S.; Jones, A.; Martin, N.G.; Gordon, S.; et al. Genetic Overlap between Endometriosis and Endometrial Cancer: Evidence from Cross-Disease Genetic Correlation and GWAS Meta-Analyses. Cancer Med. 2018, 7, 1978–1987. [Google Scholar] [CrossRef]
- Kho, P.F.; Mortlock, S.; Amant, F.; Annibali, D.; Ashton, K.; Attia, J.; Auer, P.L.; Beckmann, M.W.; Black, A.; Brinton, L.; et al. Genetic Analyses of Gynecological Disease Identify Genetic Relationships between Uterine Fibroids and Endometrial Cancer, and a Novel Endometrial Cancer Genetic Risk Region at the WNT4 1p36.12 Locus. Hum. Genet. 2021, 140, 1353–1365. [Google Scholar] [CrossRef] [PubMed]
- Kraft, P.; Chen, H.; Lindström, S. The Use Of Genetic Correlation And Mendelian Randomization Studies To Increase Our Understanding of Relationships Between Complex Traits. Curr Epidemiol Rep 2020, 7, 104–112. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Majumdar, A.; Wang, L.; Kar, S.; Brown, K.M.; Feng, H.; Turman, C.; Dennis, J.; Easton, D.; Michailidou, K.; et al. Large-Scale Cross-Cancer Fine-Mapping of the 5p15.33 Region Reveals Multiple Independent Signals. HGG Adv 2021, 2, 100041. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Fortune, M.D.; Burren, O.S.; Schofield, E.; Todd, J.A.; Wallace, C. Integration of Disease Association and EQTL Data Using a Bayesian Colocalisation Approach Highlights Six Candidate Causal Genes in Immune-Mediated Diseases. Hum. Mol. Genet. 2015, 24, 3305–3313. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, A.E.; Gao, Y.; Deep-Soboslay, A.; Tao, R.; Hyde, T.M.; Weinberger, D.R.; Kleinman, J.E. Mapping DNA Methylation across Development, Genotype and Schizophrenia in the Human Frontal Cortex. Nat. Neurosci. 2016, 19, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wu, X.; Xiao, J.; Zhang, L.; Hao, Y.; Xiao, C.; Zhang, B.; Li, J.; Jiang, X. A Large-Scale Genome-Wide Cross-Trait Analysis for the Effect of COVID-19 on Female-Specific Cancers. iScience 2023, 26, 107497. [Google Scholar] [CrossRef] [PubMed]
- Kho, P.F.; Wang, X.; Cuéllar-Partida, G.; Dörk, T.; Goode, E.L.; Lambrechts, D.; Scott, R.J.; Spurdle, A.B.; O’Mara, T.A.; Glubb, D.M. Multi-Tissue Transcriptome-Wide Association Study Identifies Eight Candidate Genes and Tissue-Specific Gene Expression Underlying Endometrial Cancer Susceptibility. Commun Biol 2021, 4, 1211. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Kho, P.F.; Ramachandran, D.; Bafligil, C.; Amant, F.; Goode, E.L.; Scott, R.J.; Tomlinson, I.; Evans, D.G.; Crosbie, E.J.; et al. Multi-Trait Genome-Wide Association Study Identifies a Novel Endometrial Cancer Risk Locus That Associates with Testosterone Levels. iScience 2023, 26, 106590. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Zhou, X.; Sun, J.; Wang, L.; Zhao, J.; Chen, J.; Yuan, S.; He, Y.; Timofeeva, M.; Spiliopoulou, A.; et al. Exploring the Cross-Cancer Effect of Smoking and Its Fingerprints in Blood DNA Methylation on Multiple Cancers: A Mendelian Randomization Study. Int. J. Cancer 2023, 153, 1477–1486. [Google Scholar] [CrossRef] [PubMed]
- Kar, S.P.; Lindström, S.; Hung, R.J.; Lawrenson, K.; Schmidt, M.K.; O’Mara, T.A.; Glubb, D.M.; Tyrer, J.P.; Schildkraut, J.M.; Chang-Claude, J.; et al. Combining Genome-Wide Studies of Breast, Prostate, Ovarian and Endometrial Cancers Maps Cross-Cancer Susceptibility Loci and Identifies New Genetic Associations. bioRxiv 2020, 2020.06.16.146803.
- Davies, N.M.; Holmes, M.V.; Davey Smith, G. Reading Mendelian Randomisation Studies: A Guide, Glossary, and Checklist for Clinicians. BMJ 2018, 362, k601. [Google Scholar] [CrossRef] [PubMed]
- Slob, E.A.W.; Burgess, S. A Comparison of Robust Mendelian Randomization Methods Using Summary Data. Genet. Epidemiol. 2020, 44, 313–329. [Google Scholar] [CrossRef] [PubMed]
- Hemani, G.; Zheng, J.; Elsworth, B.; Wade, K.H.; Haberland, V.; Baird, D.; Laurin, C.; Burgess, S.; Bowden, J.; Langdon, R.; et al. The MR-Base Platform Supports Systematic Causal Inference across the Human Phenome. Elife 2018, 7. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Ye, T.; Xue, H.; Lin, Z.; Xu, S.; Woolf, B.; Mason, A.M.; Burgess, S. MendelianRandomization v0.9.0: Updates to an R Package for Performing Mendelian Randomization Analyses Using Summarized Data. Wellcome Open Res. 2023, 8, 449. [Google Scholar] [CrossRef] [PubMed]
- Morrison, J.; Knoblauch, N.; Marcus, J.H.; Stephens, M.; He, X. Mendelian Randomization Accounting for Correlated and Uncorrelated Pleiotropic Effects Using Genome-Wide Summary Statistics. Nat. Genet. 2020, 52, 740–747. [Google Scholar] [CrossRef] [PubMed]
- TwoSampleMR: R Package for Performing 2-Sample MR Using MR-Base Database; Github;
- Palmer, T. OneSampleMR: R Package of Useful Functions for One-Sample Mendelian Randomization and Instrumental Variable Analyses; Github;
- Bowden, J.; Davey Smith, G.; Burgess, S. Mendelian Randomization with Invalid Instruments: Effect Estimation and Bias Detection through Egger Regression. Int. J. Epidemiol. 2015, 44, 512–525. [Google Scholar] [CrossRef]
- Bowden, J.; Davey Smith, G.; Haycock, P.C.; Burgess, S. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet. Epidemiol. 2016, 40, 304–314. [Google Scholar] [CrossRef] [PubMed]
- Hartwig, F.P.; Davey Smith, G.; Bowden, J. Robust Inference in Summary Data Mendelian Randomization via the Zero Modal Pleiotropy Assumption. Int. J. Epidemiol. 2017, 46, 1985–1998. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Q.; Yang, Y.; Shi, X.; Yeung, K.-F.; Yang, C.; Peng, H.; Liu, J. MR-LDP: A Two-Sample Mendelian Randomization for GWAS Summary Statistics Accounting for Linkage Disequilibrium and Horizontal Pleiotropy. NAR Genom. Bioinform. 2020, 2, lqaa028. [Google Scholar] [CrossRef]
- Zhao, Q.; Chen, Y.; Wang, J.; Small, D.S. Powerful Three-Sample Genome-Wide Design and Robust Statistical Inference in Summary-Data Mendelian Randomization. Int. J. Epidemiol. 2019, 48, 1478–1492. [Google Scholar] [CrossRef]
- Zhu, Z.; Zheng, Z.; Zhang, F.; Wu, Y.; Trzaskowski, M.; Maier, R.; Robinson, M.R.; McGrath, J.J.; Visscher, P.M.; Wray, N.R.; et al. Causal Associations between Risk Factors and Common Diseases Inferred from GWAS Summary Data. Nat. Commun. 2018, 9, 224. [Google Scholar] [CrossRef]
- Wang, J.; Zhao, Q.; Bowden, J.; Hemani, G.; Davey Smith, G.; Small, D.S.; Zhang, N.R. Causal Inference for Heritable Phenotypic Risk Factors Using Heterogeneous Genetic Instruments. PLoS Genet. 2021, 17, e1009575. [Google Scholar] [CrossRef] [PubMed]
- Burgess, S.; Foley, C.N.; Allara, E.; Staley, J.R.; Howson, J.M.M. A Robust and Efficient Method for Mendelian Randomization with Hundreds of Genetic Variants. Nat. Commun. 2020, 11, 376. [Google Scholar] [CrossRef]
- Dimou, N.; Omiyale, W.; Biessy, C.; Viallon, V.; Kaaks, R.; O’Mara, T.A.; Aglago, E.K.; Ardanaz, E.; Bergmann, M.M.; Bondonno, N.P.; et al. Cigarette Smoking and Endometrial Cancer Risk: Observational and Mendelian Randomization Analyses. Cancer Epidemiol. Biomarkers Prev. 2022, 31, 1839–1848. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Glubb, D.M.; O’Mara, T.A. Dietary Factors and Endometrial Cancer Risk: A Mendelian Randomization Study. Nutrients 2023, 15. [Google Scholar] [CrossRef]
- Niu, D.; Li, C.; Qu, H.; Zheng, Y. Does Cannabis Elevate Cancer Risk? : Evidence from Mendelian Randomization. Wien. Klin. Wochenschr. 2023. [Google Scholar] [CrossRef] [PubMed]
- Wei, Z.; Yang, B.; Tang, T.; Xiao, Z.; Ye, F.; Li, X.; Wu, S.; Huang, J.-G.; Jiang, S. Gut Microbiota and Risk of Five Common Cancers: A Univariable and Multivariable Mendelian Randomization Study. Cancer Med. 2023, 12, 10393–10405. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Tang, L.; Zhou, Y.; Zhao, S.; Zhu, H. Causal Relationship between Gut Microbiota and Cancers: A Two-Sample Mendelian Randomisation Study. BMC Med. 2023, 21, 66. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Liu, C.; Wu, J.; Kong, F. Association of Coffee and Caffeine Consumption with Risk and Prognosis of Endometrial Cancer and Its Subgroups: A Mendelian Randomization. Front Nutr 2023, 10, 1291355. [Google Scholar] [CrossRef]
- Chen, J.; Yang, K.; Qiu, Y.; Lai, W.; Qi, S.; Wang, G.; Chen, L.; Li, K.; Zhou, D.; Liu, Q.; et al. Genetic Associations of Leisure Sedentary Behaviors and the Risk of 15 Site-Specific Cancers: A Mendelian Randomization Study. Cancer Med. 2023, 12, 13623–13636. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Lee, W.-H.; Kar, S.; Burgess, S.; Allara, E. Assessing the Role of Cortisol in Cancer: A Wide-Ranged Mendelian Randomisation Study. Br. J. Cancer 2021, 125, 1025–1029. [Google Scholar] [CrossRef] [PubMed]
- Painter, J.N.; O’Mara, T.A.; Marquart, L.; Webb, P.M.; Attia, J.; Medland, S.E.; Cheng, T.; Dennis, J.; Holliday, E.G.; McEvoy, M.; et al. Genetic Risk Score Mendelian Randomization Shows That Obesity Measured as Body Mass Index, but Not Waist:Hip Ratio, Is Causal for Endometrial Cancer. Cancer Epidemiol. Biomarkers Prev. 2016, 25, 1503–1510. [Google Scholar] [CrossRef] [PubMed]
- Prescott, J.; Setiawan, V.W.; Wentzensen, N.; Schumacher, F.; Yu, H.; Delahanty, R.; Bernstein, L.; Chanock, S.J.; Chen, C.; Cook, L.S.; et al. Body Mass Index Genetic Risk Score and Endometrial Cancer Risk. PLoS One 2015, 10, e0143256. [Google Scholar] [CrossRef] [PubMed]
- Nead, K.T.; Sharp, S.J.; Thompson, D.J.; Painter, J.N.; Savage, D.B.; Semple, R.K.; Barker, A.; Australian National Endometrial Cancer Study Group (ANECS); Perry, J.R.B.; Attia, J.; et al. Evidence of a Causal Association Between Insulinemia and Endometrial Cancer: A Mendelian Randomization Analysis. J. Natl. Cancer Inst. 2015, 107. [CrossRef]
- Hazelwood, E.; Sanderson, E.; Tan, V.Y.; Ruth, K.S.; Frayling, T.M.; Dimou, N.; Gunter, M.J.; Dossus, L.; Newton, C.; Ryan, N.; et al. Identifying Molecular Mediators of the Relationship between Body Mass Index and Endometrial Cancer Risk: A Mendelian Randomization Analysis. BMC Med. 2022, 20, 125. [Google Scholar] [CrossRef] [PubMed]
- Masuda, T.; Ogawa, K.; Kamatani, Y.; Murakami, Y.; Kimura, T.; Okada, Y. A Mendelian Randomization Study Identified Obesity as a Causal Risk Factor of Uterine Endometrial Cancer in Japanese. Cancer Sci. 2020, 111, 4646–4651. [Google Scholar] [CrossRef] [PubMed]
- Freuer, D.; Linseisen, J.; O’Mara, T.A.; Leitzmann, M.; Baurecht, H.; Baumeister, S.-E.; Meisinger, C. Body Fat Distribution and Risk of Breast, Endometrial, and Ovarian Cancer: A Two-Sample Mendelian Randomization Study. Cancers 2021, 13. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, O.J.; Bafligil, C.; O’Mara, T.A.; Wang, X.; Evans, D.G.; Kar, S.; Crosbie, E.J. Child and Adult Adiposity and Subtype-Specific Endometrial Cancer Risk: A Multivariable Mendelian Randomisation Study. Int. J. Obes. 2023, 47, 87–90. [Google Scholar] [CrossRef]
- Mariosa, D.; Smith-Byrne, K.; Richardson, T.G.; Ferrari, P.; Gunter, M.J.; Papadimitriou, N.; Murphy, N.; Christakoudi, S.; Tsilidis, K.K.; Riboli, E.; et al. Body Size at Different Ages and Risk of 6 Cancers: A Mendelian Randomization and Prospective Cohort Study. J. Natl. Cancer Inst. 2022, 114, 1296–1300. [Google Scholar] [CrossRef] [PubMed]
- de Leeuw, C.; Savage, J.; Bucur, I.G.; Heskes, T.; Posthuma, D. Understanding the Assumptions Underlying Mendelian Randomization. Eur. J. Hum. Genet. 2022, 30, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Bowden, J.; Del Greco, M.F.; Minelli, C.; Davey Smith, G.; Sheehan, N.; Thompson, J. A Framework for the Investigation of Pleiotropy in Two-Sample Summary Data Mendelian Randomization. Stat. Med. 2017, 36, 1783–1802. [Google Scholar] [CrossRef] [PubMed]
- Verbanck, M.; Chen, C.-Y.; Neale, B.; Do, R. Detection of Widespread Horizontal Pleiotropy in Causal Relationships Inferred from Mendelian Randomization between Complex Traits and Diseases. Nat. Genet. 2018, 50, 693–698. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Baird, D.; Borges, M.-C.; Bowden, J.; Hemani, G.; Haycock, P.; Evans, D.M.; Smith, G.D. Recent Developments in Mendelian Randomization Studies. Curr Epidemiol Rep 2017, 4, 330–345. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.D.; Ebrahim, S. “Mendelian Randomization”: Can Genetic Epidemiology Contribute to Understanding Environmental Determinants of Disease? Int. J. Epidemiol. 2003, 32, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Debat, V.; David, P. Mapping Phenotypes: Canalization, Plasticity and Developmental Stability. Trends Ecol. Evol. 2001, 16, 555–561. [Google Scholar] [CrossRef]
- Hughes, R.A.; Davies, N.M.; Davey Smith, G.; Tilling, K. Selection Bias When Estimating Average Treatment Effects Using One-Sample Instrumental Variable Analysis. Epidemiology 2019, 30, 350–357. [Google Scholar] [CrossRef]
- Griffith, G.J.; Morris, T.T.; Tudball, M.J.; Herbert, A.; Mancano, G.; Pike, L.; Sharp, G.C.; Sterne, J.; Palmer, T.M.; Davey Smith, G.; et al. Collider Bias Undermines Our Understanding of COVID-19 Disease Risk and Severity. Nat. Commun. 2020, 11, 5749. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





