1. Summary
Breast ptosis (BPt), the downward displacement of the nipple-areola complex (NAC), is a common concern in women [
1]. This age-related phenomenon is primarily caused by a decline in collagen production within the breast's soft tissues [
2]. Fibroblast senescence is one of the causes behind this decline. As a result, the skin loses its elasticity, and the supportive structures within the breast gradually weaken. Additionally, the hormonal changes experienced during menopause, particularly the fall in estrogen levels [
3], contribute to a decrease in mammary adipose tissue, accelerating skin ageing [
4]. Notably, other factors such as significant weight fluctuations, large breast size (macromastia), childbirth (parity), and alcohol and tobacco use can worsen the interplay between ageing and genetic predisposition [
5]. These factors collectively alter the breast tissue's architecture, impacting aesthetics and the well-being and quality of life of women affected by BPt [
6].
Mastopexy aims to restore a youthful breast shape [
2]. This procedure addresses excess glandular tissue, thereby enhancing female body aesthetics. It achieves this by repositioning the nipple-areola complex (NAC) to its optimal anatomical location, typically within the range of 19-21 centimetres from the sternal notch. Conversely, for patients with gigantomastia, breast reduction surgery offers a dual benefit. It improves overall aesthetics and significantly enhances quality of life by alleviating many symptoms associated with excessive breast weight. These symptoms can encompass neck, head, shoulder, and back pain [
2].
Matopexy is a widely adopted surgical intervention for correcting breast ptosis and restoring a youthful nipple-areola complex (NAC) position. One of the primary problems of this surgery lies in the unavoidable scarring associated with traditional approaches [
7]. Thus, a common technique, the anchor-shaped incision, employs a periareolar approach for NAC repositioning. While this approach effectively addresses the frequent co-occurrence of breast hypertrophy and ptosis [
8], the resulting scar pattern is aesthetically undesirable. Moreover, traditional techniques carry a higher risk of complications such as fat necrosis, skin loss, infections, seroma formation, hematoma development, suboptimal aesthetic results, compromised nipple sensitivity, and even NAC loss [
9]. These complications underscore the importance of balancing innovative surgical approaches and established techniques, prioritising patient safety and optimal clinical outcomes. In this regard, despite advancements in surgical techniques and the introduction of alternative methods, achieving scar-free breast pexy remains an elusive goal for plastic surgeons. Pursuing this ideal outcome necessitates continuous efforts to minimise scar visibility, improve scar quality, and optimise patient satisfaction. Areas of active research in this field include the development of minimally invasive techniques, meticulously selecting incision sites, and implementing innovative scar improvement strategies [
10].
This study aimed to assess the effectiveness of a novel low-level frequency laser technology in achieving optimal sternal notch-nipple complex (SNNC) positioning in laser-assisted mastopexy. The paucity of structured data with objective outcome measures for procedures like mastopexy highlights the need for robust datasets. This study offers comprehensive data to facilitate comparisons with other mastopexy techniques. Specifically, this information can be used to evaluate outcomes such as the proportion of patients with BPt and SNND pre-operatively and at one, two, and three months post-surgery. This comparative analysis will contribute valuable insights for optimising mastopexy outcomes.
2. Data Description
This data descriptor article describes the patient's clinical information and the associated Dataset from data collected in 39 variables from 231 patients. Several publications based on the collected data are currently being prepared. Other researchers may benefit from the description, methodology, and clinical content, as they can help them develop future studies. In addition, other researchers can use the Dataset for additional analyses.
2.1. Ethical Aspect and Informed Consent
This study was conducted according to Colombian confidentiality and information privacy legal regulations, as outlined in Law 1581 of 2012 and Decree 1377 of 2013 [
11,
12]. All participants received a comprehensive pre-operative briefing. This briefing detailed the surgical intervention's nature, purpose, technical aspects, and a balanced presentation of potential benefits, risks, and complications. The medical team employed clear yet technical language to address any questions or concerns participants may have had regarding the procedure. In this regard, an informed consent was obtained from all participants. This consent form explicitly authorised participation in the research and using anonymised clinical data for research purposes, ensuring the complete confidentiality of individual information. Participants were not reimbursed for participating in the study. The study was conducted following the Declaration of Helsinki of 1975 [
13] and approved by the Research Bioethics of Clinica de Obesidad y Envejecimiento SAS, Bogotá, Colombia. (Code 2020-0113-RC3, November 20th, 2020).
2.2. General Patient Information
The first six columns of the database contain the patients' general information, obtained directly by asking each patient during the medical interview. The first column represents the patient's number, and the second column is the day of mastopexy surgery. Columns 3 and 4 represent age (in years) and the age groups organised in decennial groups (<30; 30-39; 40-49; 50-59 and 60-69 years group). Column 5 is a nominal qualitative variable that collects the participant's ethnicity within three levels: African-Colombian, Hispanic-White, and Mixed. It is important to highlight that in this work, the individual's self-identification with an ethnic group was respected. Column 6 is a qualitative nominal, giving the participant's marital status. This variable is organised into four levels (Single, Married, Divorced and Common-Law relationship)
2.3. Anthropometric variables
Columns 7 to 11 collect ponderal-related variables whose data were obtained during the physical examination. Weight (Column 7) was determined by a calibrated digital scale InBody 270 (InBody, Seoul, South Korea), expressed in kilograms, and rounded to one decimal point, with the patient barefoot and wearing light clothing. Height (Column 8) was expressed in metres with two decimal points and measured by a stadiometer (Seca 274, Hamburg, Germany) mounted on the wall for this purpose. Before noting the measurement, the patient was asked to remove any footwear and/or head ornaments. With the buttocks, the shoulder blades, and the back of the head against the board, the head is oriented in the Frankfurt horizontal plane (FH plane), and the headpiece gets firmly placed on the head. The reading was noted to the nearest tenth of a centimetre. The head is in the Frankfort horizontal plane when the horizontal line from the ear canal to the lower border orbit is parallel to the floor [
14]. Body mass index or BMI (Column 9) was calculated by applying Quetelet's equation (weight/height). The subjects were classified according to the World Health Organization (Ponderal classification WHO, column 10) as underweight below 18.50 kg/m
2, normal weight between 18.50 and 24.99 kg/m
2, overweight between 25.00 and 29.99 kg/m
2, obese class I (Obesity I) between 30.00 and 34.99 kg/m
2, obese class II (Obesity II) between 35.00 and 39.99 kg/m
2, and obese class III (Obesity III) equal and beyond 40.00 kg/m
2. Previous weight loss is a qualitative dichotomous variable with two levels (Yes/no) (Column 11).
2.4. Surgical Complications Record
Post-operative complications were defined as any deviations from the anticipated uneventful recovery course that were not inherent to the surgical procedure, excluding treatment failures. This study employed the Clavien-Dindo Classification System (CDCS) for a standardised and objective assessment of surgical complications [
15]. The CDCS has been validated for various surgical procedures, including bariatric surgery [
16], abdominoplasty [
17], and lower body contouring [
18,
19]. This analysis evaluated the type of complication, any interventions undertaken, and the resulting outcomes. The complications are classified according to the five grades: Grade I: Complications requiring neither surgical nor medical intervention. Grade II: Complications managed with pharmacological treatment alone. Grade III: Complications necessitating non-major surgical, radiological, or endoscopic interventions, further subdivided into Grade IIIa: Interventions performed without general anaesthesia. Grade IIIb: Interventions requiring general anesthesia. Grade IV: Life-threatening complications requiring intensive care unit management, including Grade IVa: Single-organ failure (including dialysis). Grade IVb: Multi-organ failure. Grade V: Death. Consistent with CDCS recommendations, patients with multiple complications were categorised based on the most severe complication. For this study, Grades I, II, and IIIa were classified as minor complications, while Grades IIIb, IV, and V were classified as major complications.
In this regard, column 12 (complication incidence) presents complications frequency in a dichotomous way, Column 13 (Clavien-Dindo type) presents the complications grade, while column 14 (Complication type) exhibits the exact complication name. Column 15 (Complication treatment) collects the treatment received.
2.5. Breast Surgery and Measurements
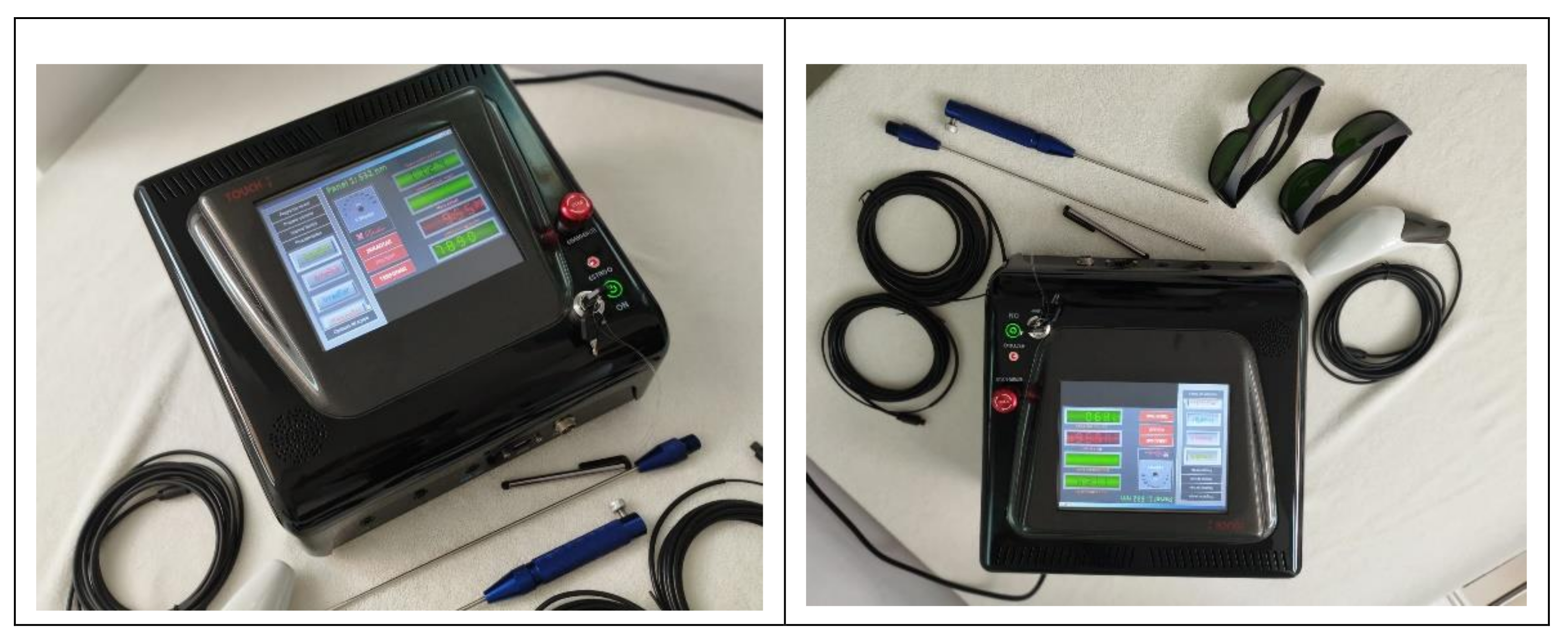
A laser lipolysis device (Lipolaser LPL9002™, Colombia) was employed throughout the procedure. This low-power cold laser device has wavelengths of 532, 650 and 980 nanometres (
Figure 1). This equipment complies with international safety standards for electro-medical devices (IEC 601-1) and laser equipment (IEC 825). Each multifrequency low-power laser fibre was placed within a 1.2 mm calibre atraumatic 30 cm long cannula. The surgical procedure usually lasts 40 to 60 minutes approximately, and all regions undergo the same four-step technique as follows:
The first laser applied was the 532 nm and 900-milliwatt green laser, which produces a vasoconstrictive effect, ensuring little or no blood loss. The cannula was inserted through the two previous incisions, followed by slow forward and backward movements in the mid-thickness of the flap in each region for one to three minutes. The second laser applied was the 650 nm red laser. The primary function of this laser is to induce adipocyte lysis, leading to the release of triacylglycerides in areas targeted for fat extraction. The laser exposure time will be sufficient to achieve fat dilution perceived by fat consistency changes by palpation (from a solid to a liquid phase), and the absence of resistance to the laser cannula passage indicates complete adipose tissue liquefaction. Once the fat was adequately liquefied, it was meticulously aspirated, mirroring the laser application sequence, ensuring removal throughout the entire thickness of the flap by slow, controlled movements, using straight and curved cannulas of 5, 4, or 3 mm in diameter connected to a suction device (Wells Johnson Co., Tucson, AZ, USA). Finally, a 980 nm and 900-milliwatt infrared laser was applied for 5 minutes in each zone into the subdermal space to promote skin retraction. In the case of laser-assisted lipolysis mastopexy with implant placement, the prosthesis was placed after laser therapy through a subareolar incision, and then, the implant was placed in a neuromuscular position.
Figure 1 and Figure 2 depict the Lipolaser LPL9002™, employed in this study.
This study employed two primary outcome measures to assess the efficacy of laser-assisted mastopexy based on nipple-areola complex (NAC) position. Firstly, the temporal changes in NAC distance (SNND) at pre-operative, one-month, two-month, and three-month post-operative were recorded. In this regard, columns 16 and 17 (NSSD before surgery RB and NSSD before surgery RL) contain the SNND before surgery for the right and left breast, respectively. Therefore, columns 18, 19, 20, 21, 22 and 23 collect data on SNND for each breast in centimetres for the 1st month, 2nd month, and 3rd month. For the SNND, the patient was standing upright with arms relaxed. Then, the sternal notch at the top of the breastbone is located, and with a non-stretchy measuring tape, start at the sternal notch and extend it directly over the nipple, ensuring it lays flat against the chest wall. The distance in centimetres for each nipple must be recorded, and for improved accuracy, it is recommended to have another person take the measurement and use a flat surface to ensure proper posture.
On the other hand, the Regnault classification system was employed to provide a simple and standardised method for assessing breast ptosis in three different degrees based on the relative position of the nipple to the inframammary fold (IMF). In grade I (Pseudoptosis), the nipple is at the level of the IMF or up to 1 cm below. In grade II (Moderate Ptosis), the nipple is 1 to 3 cm below the IMF but is not the most dependent part of the breast. In grade III (Severe Ptosis), the nipple is more than 3 cm below the IMF or sits at the inferior pole of the breast (the lowest point) [
20]. In this regard, the evolution in the different ptosis degrees proportions at three months post-surgery were recorded in columns 24, 25, 26, and 27 (Ptosis degree at baseline, Ptosis degree 1st month, Ptosis degree 2nd month, Ptosis degree 3rd month) and compared.
2.6. Personal History and Habits
This section consists of 10 columns that collect data on variables related to personal history, some psychobiological habits, and serum prolactin levels. Column 29 (Pregnancy numbers) is a quantitative discrete variable describing the number of pregnancies in each patient, and column 30 (breastfeeding) reflects the information on whether the patient has ever breastfed her children.
Prolactin (column 30) is the serum prolactin concentration in ng/dL. Alcohol consumption and Tobacco consumption (Columns 31 and 32) are dichotomous variables (yes/no) about the current consumption of these products. Frequently, medication (column 33) includes drugs and supplements often consumed (at least three times a week). Diseases history (Column 34) registers non-communicable chronic diseases, and Contraception (column 35) provides data related to the anti-conception methods used by the patients. Previous breast surgery (Column 36) recollects the history of breast surgery at any age different to the mastopexy to be undergone. Menses (Column 37) record the cyclic behaviour (or not) or even no menses (Natural, surgical or pathologic).
2.7. Type of Surgery
Breast prosthesis placement (Prosthesis placement, column 38) informs the current breast implant placement (during the mastopexy), while Breast reduction (column 39) informs if, during the mastopexy, a breast reduction was made.
3. Methods
The patient's clinical evaluation and surgical procedures were conducted between October 2022 and June 24th 2023.
3.1. Participants and Sample Size
A non-experimental longitudinal retrospective cohort study was done on 231 women undergoing a scarless low-level laser-assisted mastopexy technique at the Clínica de Obesidad y Envejecimiento SAS, Bogotá, Colombia, assessing sternal notch-to-nipple distance (SNND), and the breast ptosis degree by the Regnault classification system at the first, second, and third post-operative month. Additionally, the incidence and nature of complications within the first 30 days post-surgery were evaluated. Individuals could participate in the study if they were at least 18 years old. There were no exclusion criteria. However, some patients were excluded from the final Dataset because it did not provide demographic data. No power analysis nor effect size was conducted for this study because the goal was to achieve a sufficient sample size that allows comparisons between subgroups (e.g., four-time points in SNND and differences in ptosis degree proportions).
3.2. Data Collection
Data was collected in an electronic clinical record system. The raw data from the electronic medical record system were subsequently exported as a .csv file to be processed in Excel 365 A2 to perform the data audits. If necessary, data were recoded, and scale and subscale scores were computed.
3.3. Data Handling
Reliability, Consistency, and Accuracy. All data was rigorously evaluated to identify and correct errors, inconsistencies, or biases to avoid bias in the validity of study findings and conclusions. The scientific data auditing process included 1) Data acquisition review, 2) Data management review, 3) Data Analysis Review, and 4) Reporting Review. Once the data audit was finished, the formal data analysis was done to answer the research question.
Statistical analysis was performed using the R statistical computing environment [
21] running in Jamovi, a free, open-source statistical software program built in R programming language [
22]. Categorical variables were displayed in tables as absolute, relative and cumulative frequencies. Proportion comparisons were made using Pearson's chi-square or Fisher's exact tests. The proportion changes in MP degree along time measures were compared with Friedman's test and the Durbin-Conover post-hoc test for pairwise contrast. On the other hand, quantitative variables were expressed as means ± SD (in parenthesis) or medians and percentiles as appropriate. If normality and homoscedasticity were met, quantitative variables comparisons were made using Student t-tests (for two groups) or repeated measures ANOVA (for more than two-time measures). Welch's t-test or Trimmed means Robust Anova was employed in cases where these assumptions were unmet. A p-value < 0.05 was considered statistically significant.
3.4. Strengths and Limitations
To the best of our knowledge, this is the first study exploríng the effect of multifrequency low-level laser-assisted mastopexy in a large patient cohort and quantifying the surgical success by both evaluating the number of patients achieving a non-breast ptosis state and by monthly SNND. Our results showed a significant improvement in breast ptosis, with 90% of patients achieving a non-ptosis state by the third month with minimal scarring. Compared to traditional techniques, this procedure leaves minimal to no scars and minimal damage to surrounding tissues compared to conventional matopexy techniques. The study reported a complication rate of only 4%, which is lower than traditional mastopexy procedures.
Among the limitations of this procedure is the lack of similar studies, which makes it difficult to compare it to established methods. There is no open dataset with results assessing other mastopexy techniques measuring the same outcomes during the three months. Regrettably, this study only followed patients for three months, and the long-term effectiveness of the lift and skin tightening is unknown. Nevertheless, we still follow this patient cohort to assess the SNDD in the medium and long term.
Authors Contributions
Conceptualisation, G.C-V., NV, AMOP, and VB; methodology, D.R-P. and VB; validation, G.C-V., NV, AMOP, D.R-P. and VB; formal analysis, D.R-P. and VB; investigation, G.C-V., NV and AMOP; resources, G.C-V., NV, AMOP, D.R-P. and VB; data curation, D.R-P. and VB; writing—original draft preparation, G.C-V., NV, AMOP, D.R-P. and VB; writing—review and editing, G.C-V., NV, AMOP, D.R-P. and VB; supervision, G.C-V., NV, AMOP, and VB; funding acquisition, G.C-V., D.R-P. and VB All authors have read and agreed to the published version of the manuscript.
Funding
Internal funds for research strengthening from Universidad Simón Bolívar, Vicerrectoría de Investigación, Extensión e Innovación, Barranquilla, Colombia.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Full data supporting the reported results can be found at the Harvard Dataverse Repository. Cubillos, G. (2024). Laser-Assisted mastopexy dataset (V1 ed., p. 1). Harvard Dataverse.
https://doi.org/doi:10.7910/DVN/6MGOZF.
References
- Torres-Arciniegas SC, Solis-Chaves P, Herrera-Mora G, Chacón-Quirós M. Preservation of breast ligamentous structures in mastopexy: achieving aesthetic excellence with minimal complications. Sci Art Plast Surg J. 2024;1:2–10.
- He T, Fisher GJ, Kim AJ, Quan T. Age-related changes in dermal collagen physical properties in human skin. PLoS One. 2023;18(12):e0292791.
- Ramanadham SR, Rose Johnson A. Breast Lift with and without Implant: A Synopsis and Primer for the Plastic Surgeon. Plast Reconstr surgery Glob open. 2020 Oct;8(10):e3057.
- Knoedler S, Knoedler L, Kauke-Navarro M, Alfertshofer M, Obed D, Broer N, et al. lQuality of Life and Satisfaction after Breast Augmentation-A Systematic Review and Meta-Analysis of Breast-Q Patient-Reported Outcomes. J Plast Reconstr Aesthetic Surg. 2024.
- Fisher GJ, Varani J, Voorhees JJ. Looking older: fibroblast collapse and therapeutic implications. Arch Dermatol. 2008 May;144(5):666–72.
- Coltman CE, Steele JR, McGhee DE. Effect of aging on breast skin thickness and elasticity: implications for breast support. Ski Res Technol Off J Int Soc Bioeng Ski [and] Int Soc Digit Imaging Ski [and] Int Soc Ski Imaging. 2017 Aug;23(3):303–11.
- Swanson, E. Evidence-Based Cosmetic Breast Surgery. Springer International Publishing, editor. 2017.
- Cárdenas-Camarena, L. Various surgical techniques for improving body contour. Aesthetic Plast Surg. 2005;29(6):446–9.
- Stevens WG, Stoker DA, Freeman ME, Quardt SM, Hirsch EM. Mastopexy revisited: a review of 150 consecutive cases for complication and revision rates. Aesthetic Surg J. 2007;27(2):150–4.
- di Summa PG, Oranges CM, Watfa W, Sapino G, Keller N, Tay SK, et al. Systematic review of outcomes and complications in nonimplant-based mastopexy surgery. J Plast Reconstr Aesthet Surg. 2019 Feb;72(2):243–72.
- Presidente de la Republica de Colombia. Decreto 1377 de 2013 (Junio 27). 2013;1–9. Available online: https://www.funcionpublica.gov.co/eva/gestornormativo/norma.php?i=53646.
- Congreso de Colombia. Ley 1581 de 2012 (Octubre 17). 2012;1–9.
- World Medical Association. WMA Declaration of Helsinki: ethical principles for medical research involving human subjects. 1974;353(1):1418–9. Available online: http://www.wma.net/en/30publications/10policies/b3/index.html.
- Varsha G, Krishan K, Rutwik C. Evaluación de altura. 2024. 1–10 p.
- Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009 Aug;250(2):187–96.
- Csendes A, Torres J, Burgos AM. Late marginal ulcers after gastric bypass for morbid obesity. clinical and endoscopic findings and response to treatment. Obes Surg. 2011;21(9):1319–22.
- Basseri B, Levy M, Wang HL, Shaye OA, Pimentel M, Soffer EE, et al. Redefining the role of lymphocytes in gastroesophageal reflux disease and eosinophilic esophagitis. Dis esophagus Off J Int Soc Dis Esophagus. 2010 Jul;23(5):368–76.
- Csendes G P, Cortés A C, Silva F C, Enriquez G O, Garrido I C, Maulen A J. Intestino Delgado Patologico: Resonancia Magnetica Con Contraste Oral Versus Transito Intestinal Con Bario (Resultados Preliminares. Rev Chil Radiol. 2004;10(4):158–64.
- Rohrer JE, Herman DC, Merry SP, Naessens JM, Houston MS. Validity of overall self-rated health as an outcome measure in small samples: a pilot study involving a case series. J Eval Clin Pract. 2009 Apr;15(2):366–9.
- Regnault, P. Breast ptosis. Definition and treatment. Clin Plast Surg. 1976 Apr;3(2):193–203.
- Ibrahim AM, Sinno HH, Izadpanah A, Vorstenbosch J, Dionisopoulos T, Markarian MK, et al. Mastopexy for breast ptosis: Utility outcomes of population preferences. Plast Surg (Oakville, Ont). 2015;23(2):103–7.
- Graf R, Ricardo Dall Oglio Tolazzi A, Balbinot P, Pazio A, Miguel Valente P, da Silva Freitas R. Influence of the Pectoralis Major Muscle Sling in Chest Wall-Based Flap Suspension After Vertical Mammaplasty: Ten-Year Follow-Up. Aesthetic Surg J. 2016 Nov;36(10):1113–21.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).