1. Introduction
Since long spinal fusion for degenerative lumbar disease can theoretically increase biomechanical stress along with natural degeneration on the adjacent segments, a problematic complication called proximal junctional failures (PJF) may occur more or less postoperatively. Incidence of PJF and various potential risk factors associated with PJF have been reported and stratified in the literatures.[
1,
2,
3,
4,
5,
6,
7,
8,
9,
10] Among them, there have been consistent reports opposed to the selection of upper instrumented vertebra (UIV) at thoracolumbar junction in long instrumented spinal fusion.[
5,
10,
11] This was understood due to thoracolumbar junction was a transitional zone from the less flexible thoracic spine to the flexible lumbar spine, and Kim et al. 10 explained concretely that stopping at or distal to T11 and T12 without costosternal articulation could not have a biomechanical advantage of thoracic cage on the adjacent segment in correction surgery for adult spinal deformity (ASD). Swank et al. [
12] previously investigated surgical outcomes of long lumbar fusion from L1 or L2 to sacrum for various spinal pathologies. They reported high rate of reoperation (35%), low rate of clinical success, and concluded that instrumented lumbosacral fusions with UIV at L1 or L2 could not be recommended. However, there are some recent literatures with opposing point of view regarding proximal adjacent segment degeneration after long spinal fusion. [
4,
12,
13] Bess et al. [
14] demonstrated that the distribution of forces across and supra-adjacent to the UIV via posterior polyester tethers could allay the risk of PJF which could potentially mitigate the risk of PJF Other literatures claimed thoracolumbar junction could be considered selectively as UIV without certain potential risk factors. [
4,
12]
Although the determination of UIV has been a controversial issue in long spinal instrumented fusion for correction of ASD, [
11,
12,
14,
15] which still has no definite answer up to date. To the best of our knowledge, there have been a paucity of study investigating the risk factors associated with PJF following long instrumented spinal fusion from L1 to sacrum. The purpose of this study was to investigate the incidence and the risk factors of PJF following long instrumented fusion from L1 to sacrum and to shed new light on L1 vertebra as UIV for degenerative lumbar disease with mild to moderate sagittal imbalance.
2. Materials and Methods
1) Study design & patient population
After obtaining approval by the appropriate ethics committee (institutional review board of our institution), a retrospective review of clinical and radiographic data was performed. This study was performed with degenerative lumbar disease patients who had undergone instrumented spinal fusion between March 2006 and December 2019 at a single institution.
The inclusion criteria were as follows: (1) preoperative diagnosis of degenerative lumbar diseases (spinal stenosis, spondylolisthesis, adjacent segment disease following previous spinal fusion, lumbar degenerative kyphosis); (2) completion of a long-segment spinal instrumented fusion surgery from L1 vertebra to the sacrum regardless of iliac fixation; and (3) a postoperative follow-up period of at least 2 years. The exclusion criteria were as follows: (1) sagittal balance as C7 sagittal vertical axis (C7SVA) more than 15cm on lateral whole spine radiograph in standing position; (2) inadequate visibility for measuring radiographic parameters in whole spine standing lateral radiographs at regular pre- and postoperative visits; (3) history of pedicle subtraction osteotomy (PSO) or other equivalent procedures ; (4) postoperative surgical site infection requiring revisional operation for index surgery, but not for PJF; (5) if they lacked either baseline or postoperative imaging at regular (preoperative, postoperative 3 months, 1-year and 2-year) follow-up.
2) Data collection
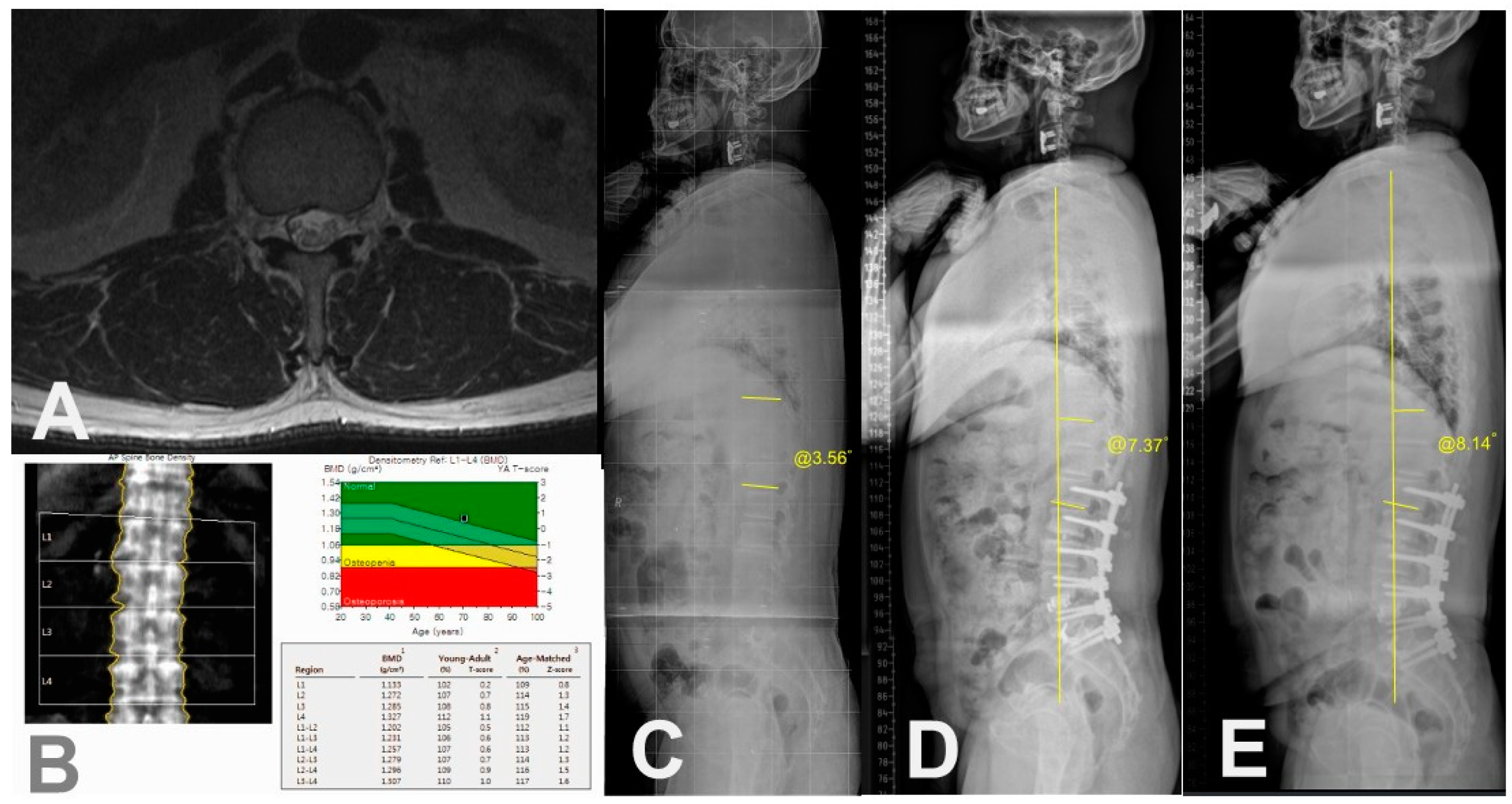
The following demographic and surgical data were collected: age at surgery ; sex (female/male); bone mineral density (BMD, T-score); body mass index (BMI, kg/m2); smoking; previous spinal fusion; American Society of Anesthesiologist physical status (ASA) grading; iliac fixation; disc degeneration by Pfirrmann grade [
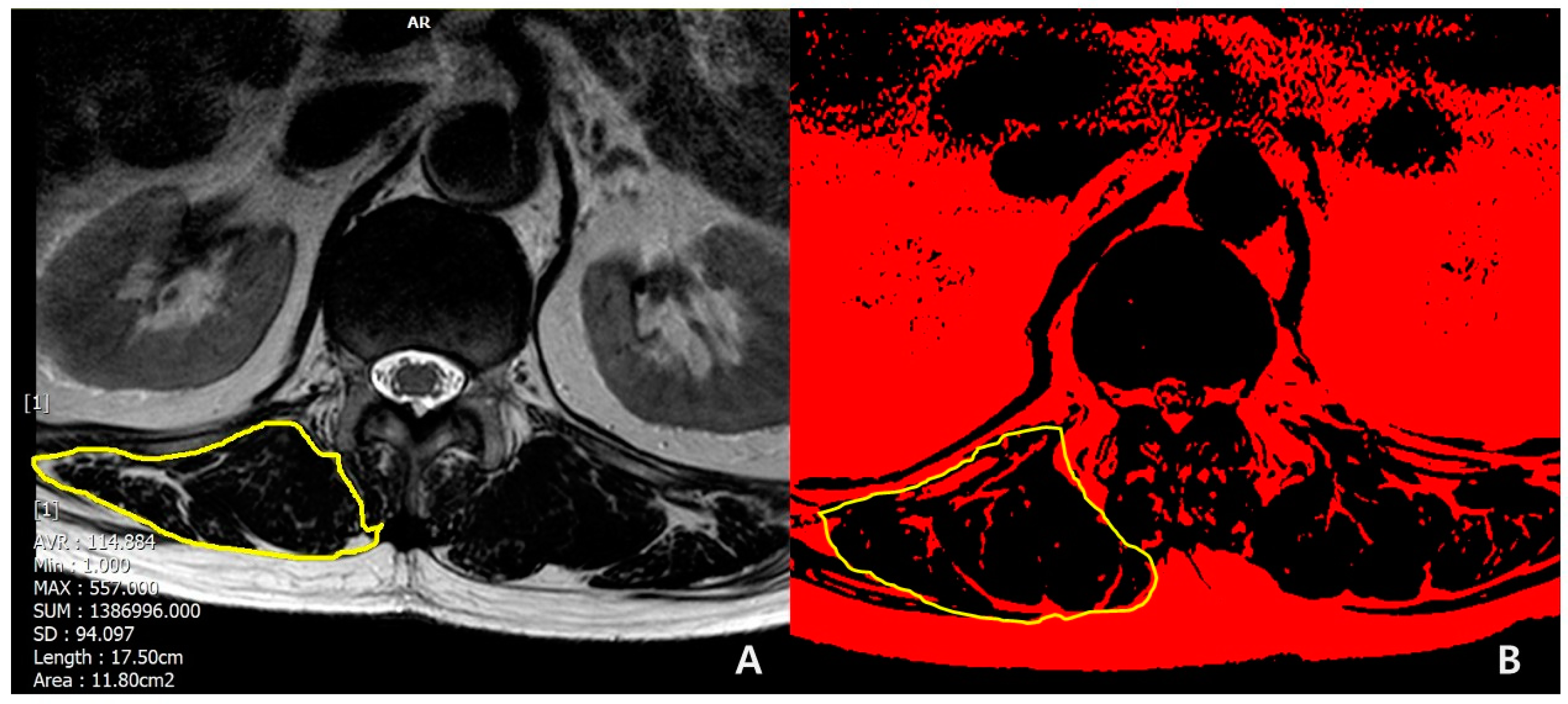
16] at T12-L1 segment (1,2,3: mild to moderate; 4,5: severe); muscularity status at T12-L1 (cross-sectional area [CSA], cm
2) and fat infiltration grade (mild to moderate, if <50%; severe, if ≥ 50%) in erector spinae muscle at T12-L1 in T2-weighted axial magnetic resonance (MR) images using Picture Archiving and Communication System (PACS) by Philips ACHIEVA 3.0T (Philips Healthcare, UK) and the ImageJ software. The region of interest (ROI) for erector spinae muscle at T12-L1 level was outlined polygonally with manipulation of graphic cursor and handled with pseudocoloring method.[
17] (
Figure 1) Then, CSA (
Figure 1A) were calculated and fat infiltration grade (
Figure 1B) was determined.
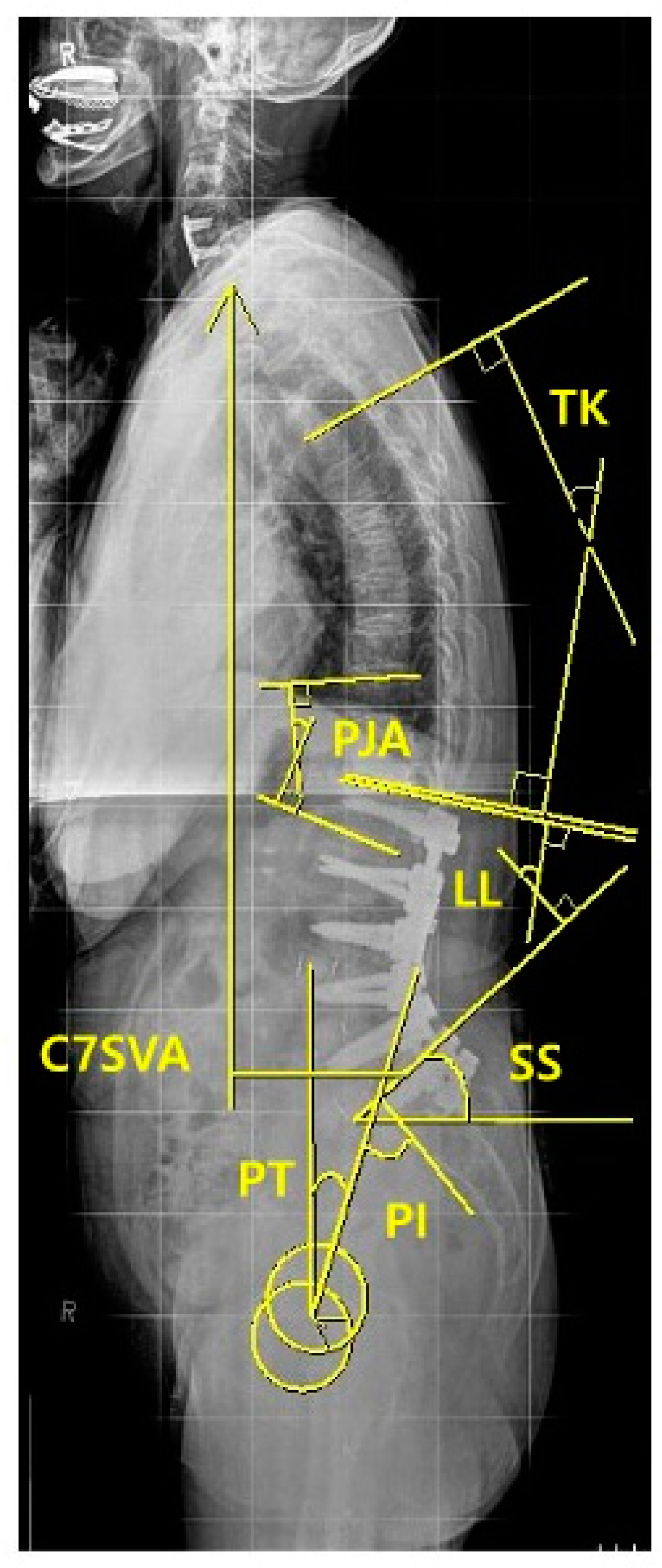
For radiographic assessment of spinopelvic parameters, standing 36-inch-long cassette AP and lateral radiographs of the whole spine were measured at the preoperative, the immediate postoperative, and the regular postoperative outpatient visits (3, 6, 9 months, 1-, 2-year and the final follow-up), respectively. On the radiographs, C7 sagittal vertical axis (C7SVA), thoracic kyphosis (TK) [
18], thoracolumbar kyphosis (TLK) [
18,
19], lumbar lordosis (LL) [
18], sacral slope (SS) [
18], pelvic tilt (PT) [
18], pelvic incidence (PI) [
18,
19,
20] and proximal junctional angle (PJA) were measured (
Figure 2). We also collected and analyzed the change (preoperative minus postoperative) of each radiographic parameter between the preoperative and the immediate (3 months) postoperative.
Figure 2.
Methods for measuring A) CSA and B) FI of erector spinae muscle.
Figure 2.
Methods for measuring A) CSA and B) FI of erector spinae muscle.
Figure 3.
Measurement of Sagittal Spinopelvic Parameters.
Figure 3.
Measurement of Sagittal Spinopelvic Parameters.
3. Results
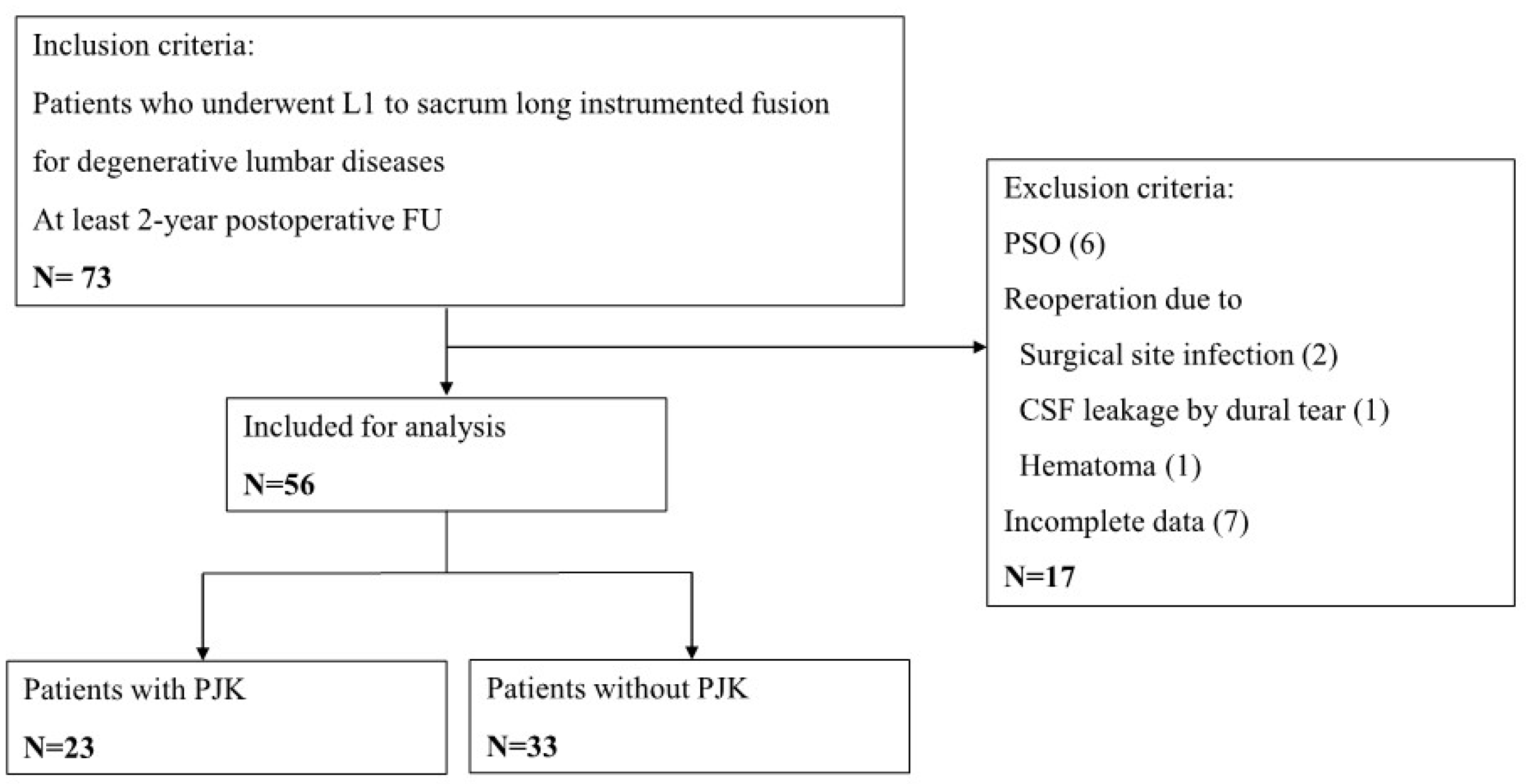
1) Baseline demographics and PJK incidence of included patients
Among the 73 consecutively treated degenerative lumbar disease patients with completion of instrumented spinal fusion from L1 to the sacrum, a total of 56 patients met the study inclusion criteria and were recruited as the study cohort. There were 46 women (82.1 %) and 10 men (17.9 %). The age of patients was 67.3 ± 7.9 (range, 45-79) years and BMI was 26.1± 3.9 (range, 19.3-40.1) kg/m2. There were 18 (32.1%) osteoporotic patients. Iliac fixation was supplemented in 30 (53.6%) patients. Eighteen (32.1%) patients had previous history of spinal fusion. Through the total follow-up period, PJK were diagnosed in 23 (41.1%) out of 56 patients. Of these, 20 (87.0%) were observed within postoperative 1 year. The demographics data and incidence of PJK were further summarized in
Table 1 and
Table 2.
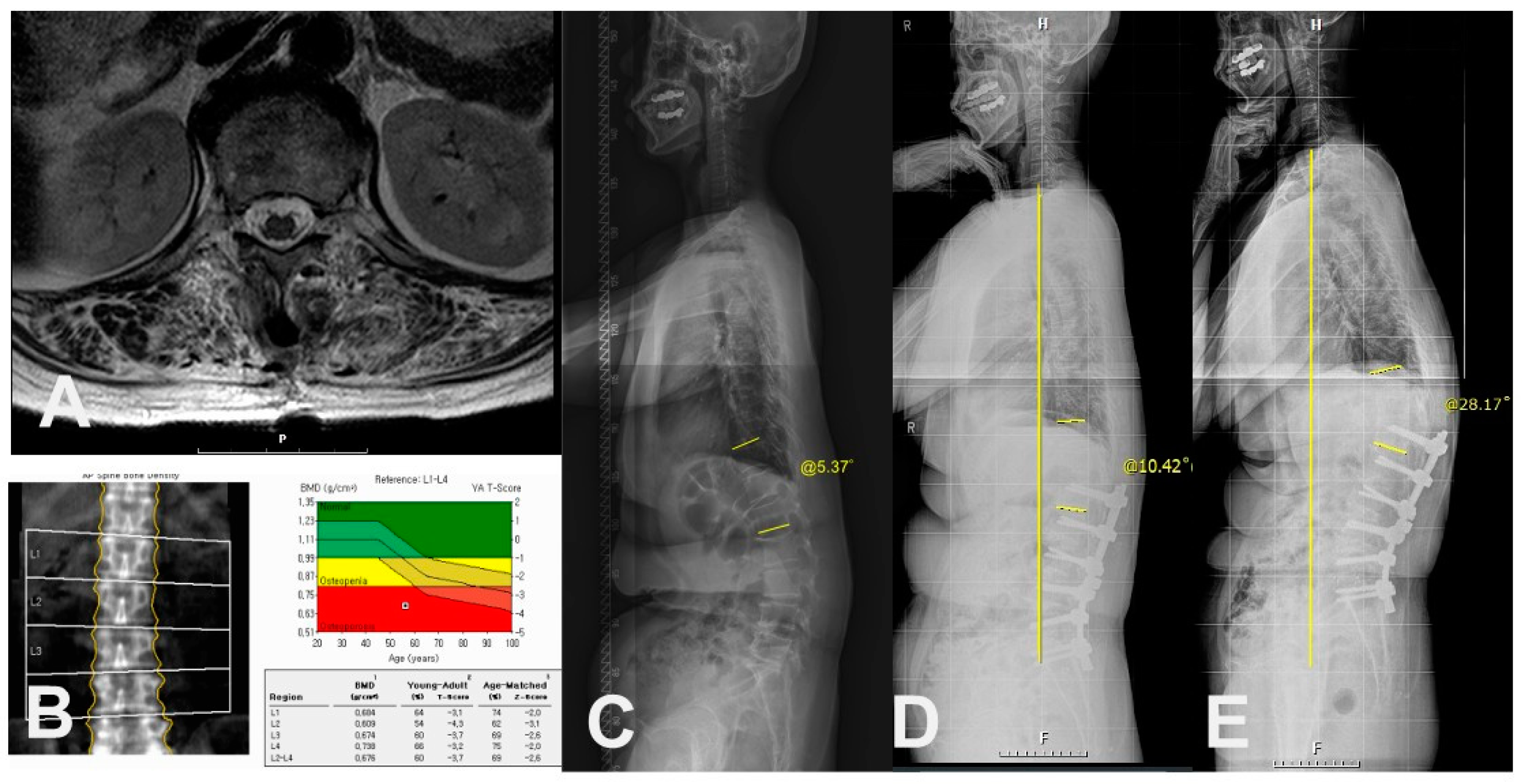
2) Univariate analysis of demographic or surgical risk factors
In univariate analysis of demographics, PJK group showed more frequent in female (100% in PJK vs 73% in non-PJK, p=0.011), osteoporosis (60.9% in PJK vs 12.1% in non-PJK, p<0.001). Also, PJK group showed the lower mean value of the lowest T-score in BMD (-2.4 ± 0.8 in PJK vs -1.5 ± 1.1 in non-PJK, p=0.006) and BMI (24.4 ± 2.4 in PJK vs 27.1 ± 4.3 in non-PJK, p=0.004) with statistical significance. In comparison of muscular quantity between the groups, there were smaller CSA (cm
2, 23.8 ± 4.2 vs 32.2 ± 10.1, p<0.001) in erector spinae muscle at T12-L1 in PJK group than non-PJK group. Also, in comparison of muscular quality between the groups, PJK group showed more frequent severe (≥50%) fat infiltration in erector spinae muscle at T12-L1 with statistical significance (p<0.001) (
Table 3) (
Figure 4 and
Figure 5).
There were no significant differences in age at surgery, ASA grade, previous spinal fusion, smoking, iliac fixation, and disc degeneration status at T12-L1 between the groups. Follow-up period (months) was different (61.1 ± 40.6 in PJK vs -23.6 ± 24.2 in non-PJK, p<0.001) (
Table 3).
3) Univariate analysis of radiographic risk factors after L1-sacrum instrumented fusion
In comparison of preoperative radiographic parameters between the groups, PT (°) was larger in PJK group than non-PJK group (34.0 ± 7.2 vs 25.8 ± 13.0, p=0.032). There were no significant differences in preoperative TK, TLK, LL, SS, PI, C7SVA and PJA (p>0.05).
In comparison of immediate (3 months) postoperative radiographic parameters, PJK group showed larger immediate postoperative TLK (23.5 ± 9.9 vs 8.7 ± 12.2, p<0.001) and PJA (20.9 ± 7.7 vs 10.7 ± 8.1, p<0.001), respectively. However, there were no differences in other immediate postoperative parameters (p >0.05).
Although the changed amount of LL was larger in PJK group, there was no statistical difference (36.6 ± 27.7 vs 24.8 ± 27.2, p=0.180). There was no significant difference in the changes of other radiographic parameters from the preoperative to the immediate postoperative values between the two groups. (
Table 4)
4) Logistic regression analysis of potential risk factors associated with PJK after L1-sacrum instrumented fusion
The variables with a p-value <0.05 in
Table 2 and
Table 3 were selected after univariate analyses and analyzed further with logistic regression analysis. Logistic regression analysis revealed that severe (>50%) fat infiltration in erector spinae muscle (OR=43.60, CI 4.10-463.06, R
2N 0.730, p=0.002) and osteoporosis (OR=20.49, CI 1.58-264.99, R
2N 0.730, p=0.021) were statistically significant (
Table 5). Female sex (p=0.167), BMI (p=0.620), axial CSA of erector spinae muscle at T12-L1 (p=0.082), preoperative PT (p=0.852), immediate postoperative TLK (p=0.161) and PJA (p=0.124) were not statistically significant. (
Table 5)
4. Discussion
Causes of PJK following long instrumented spinal fusion can be explained with problems of soft tissue (intervertebral disc, paravertebral muscle, posterior ligamentous complex, et cetera.) and/or of bony structures (UIV or UIV +1 fracture, loss of mechanical stability between instruments and bony vertebra). According to the published systematic review articles [
21,
22], age, female gender, and low BMD/osteoporosis were demographic risk factors for PJK. The current study revealed that osteoporosis and severe (>50%) fat infiltration in erector spinae muscle at the proximal junction (T12-L1 level) were independent risk factors for PJK following instrumented fusion from L1 to the sacrum, but age was not a risk factor. Therefore, if a surgeon plans to operate patients with instrumented fusion from L1 to the sacrum, we suggest that patients with osteoporosis and severe fat infiltration in erector spinae muscle at T12-L1 should be avoided or treated with a different surgical plan.
Interestingly, it was observed that most of PJK (88%) developed as a result of bony structural problems such as adjacent vertebral compression fractures. Ha et al. [
14] reported bony failure such as compression fracture at the proximal junction was more prevalent in the patients with distal thoracic vertebra as a UIV, whereas subluxation was more prevalent in the patients with proximal thoracic vertebra as a UIV. The observed outcome that fractures at the TLJ were the main cause of PJK was considered a quite understandable result in that it suggests osteoporosis is a condition with a high risk of fracture [
23] and the location is mainly at the TLJ. On the other hand, the degeneration of the T12-L1 intervertebral disc which is the boundary of the thoracic and lumbar spine was not a significant risk factor of PJK, which is believed to be due to stabilization of the adjacent segment to the fusion as the degeneration of the intervertebral disc. This is in line with the concept mentioned in the past literature that the degeneration process of intervertebral disc could be subdivided into three stages: (1) temporary dysfunction; (2) unstable phase; and (3) stabilization. [
24] Based on the above, if fusion for the elderly patient is stopped at the thoracolumbar junction, it is considered that the problem of bony structure would be higher than that of soft tissue.
Reoperations were performed early after index surgery in the cases of PJK (PJF) accompanied by severe clinical symptoms due to screw loosening or adjacent vertebral fracture. According to the criteria for exclusion from the study, therefore, they were excluded from statistical analysis because of reoperation within 1 year.
As an analysis of muscle quantity (CSA) and quality (FI), only severe (>50%) FI was found as a significant risk factor. Muscle size may vary depending on the patient’s body size, fat infiltration itself is associated with aging meaning that muscle function has decreased, and thus is thought to adversely affect maintaining dynamic spinal stability.
Age did not reveal any statistical significance in this study, and which can predict that limited fusion with L1 as UIV can be performed regardless of age for patients who maintain the state of the musculoskeletal system. Because functional age representing bone density or muscle conditions differs from chronological age itself, which can be improved through resistance exercise. [
25]
The current study showed that LL, PT, and SVA before surgery were not significant risk factors in logistic regression model, which was different from previous literatures that reported that large amount of correction were risk factors for PJK. [
26,
27,
28,
29] In this study, it is believed that the amount of correction was not enough to cause PJK even in patients who received relatively large corrections, since PSO or the other equivalent procedure was not performed.
In terms of surgical risk factors, it was reported that using hooks at UIV and the selection of UIV above T8 could reduce the occurrence of PJK, while pelvic fixation was significantly associated with increased occurrence of PJK. [
21,
22] Pelvic fixation is thought to increase PJK in addition to the known risk factor of proximal fixation segment at the thoracolumbar junction (L1 vertebra) in the patients of this study.
Whereas several literatures defined PJK as being 1) PJA ≥ 10° and 2) 10° greater than the preoperative measurement, [
14,
30] we used 1) PJA ≥ 20 ° as a proposed critical value of PJK in the current study. There were two reasons for this cut-off value of PJK. First, 10° or 15° of PJK in the literatures failed to demonstrate such a critical angle in terms of clinical outcomes, Bridwell et al. evaluated “20” degrees as a critical angle to diagnose PJK. [
31] However, even with ≥20 ° as a critical angle for PJK, there were not any significant clinical differences in the pre- and postoperative ODI but with only trend between PJK group and non-PJK group.
This study has several limitations. It is a retrospective study with relatively small number of patients. However, it indicated that the risk factors which had statistically significant association with the PJK, despite the limited sample size. To clarify the significance of these variables, replication studies and further researches with a larger sample size are considered to help validate and strengthen the findings. In addition, most of PJKs occurred relatively early (within postoperative 1 year) in the current study. It is thought that the meaning of PJK occurring early after surgery and after a long period of time would be different. In this regard, it is also necessary to conduct research with a long follow-up period. Moreover, we could not investigate surgical factors potentially affecting early failures such as graft materials for fusion, improper screw placement at the UIV, and lordosis distribution index.
5. Conclusions
This study found severe (≥50%) fat infiltration in erector spinae muscle at T12-L1 and osteoporosis were significant independent risk factors of PJK in patients undergone L1-sacrum instrumented fusion. To avoid the early-onset PJK, consideration of these factors is important before planning long instrumented spinal fusion from L1 to the sacrum for patients with degenerative lumbar disease. However, since age itself is not a risk factor, L1 can be selected as UIV even in elderly patients if there is no muscle-related risk factor and osteoporosis.
List of Abbreviations
PJK: Proximal junctional kyphosis
PJA: Proximal junctional angle
ASD: Adult spinal deformity
TK: Thoracic kyphosis
TLK: Thoracolumbar kyphosis
LL: Lumbar lordosis
PT: Pelvic tilt
SS: Sacral slope
PI: Pelvic incidence
SVA: Sagittal vertical axis
BMI: Body mass index
BMD: Bone mineral density
ASA: American Society of Anesthesiologists
CSA: Cross-sectional area
MR: Magnetic resonance
SRS: Scoliosis Research Society
ODI: Oswestry disability
Author Contributions
KYH: study concept/design, critical revision; JA: draft manuscript writing, critical revision; YHK, YCK: critical revision; KTK: supervision/critical revision; SMK, JBP: acquisition of data/critical revision.
Funding
There was no funding source.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Kyung Hee University Hospital at Gangdong (approval number: KHNMC- 2022-01-011).
Informed Consent Statement
Written informed consent was obtained from all participants.
Data Availability Statement
The patients’ data were collected in Kyung Hee University Hospital at Gangdong. The datasets generated and/or analysed during the current study are available from the corresponding author (KYH) on reasonable request.
Conflicts of Interest
The authors declare no personal competing interests in any of the materials, or devices described in this article. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. (JA: nothing to disclose, YHK: nothing to disclose, YCK: nothing to disclose, KTK: nothing to disclose, KYH: nothing to disclose, SMK: nothing to disclose JBP: nothing to disclose).
References
- Watanabe, K.; Lenke, L.G.; Bridwell, K.H.; Kim, Y.J.; Koester, L.; Hensley, M. Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: analysis of morphological features. Spine 2010, 35, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Park, W.M.; Choi, D.K.; Kim, K.; Kim, Y.J.; Kim, Y.H. Biomechanical effects of fusion levels on the risk of proximal junctional failure and kyphosis in lumbar spinal fusion surgery. Clin Biomech 2015, 30, 1162–1169. [Google Scholar] [CrossRef] [PubMed]
- Ono, K.; Ohmori, K.; Hori, T. Clinical and Radiological Outcomes of Corrective Surgery on Adult Spinal Deformity Patients: Comparison of Short and Long Fusion. Adv Orthop. 2019, 2019, 9492486. [Google Scholar] [CrossRef] [PubMed]
- Hyun, S.J.; Kim, Y.J.; Rhim, S.C. Patients with proximal junctional kyphosis after stopping at thoracolumbar junction have lower muscularity, fatty degeneration at the thoracolumbar area. Spine J. 2016, 16, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Yagi, M.; Nyugen, J.; Cunningham, M.E.; Boachie-Adjei, O. Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res. 2012, 470, 1633–1639. [Google Scholar] [CrossRef] [PubMed]
- Hassanzadeh, H.; Gupta, S.; Jain, A.; El Dafrawy, M.H.; Skolasky, R.L.; Kebaish, K.M. Type of Anchor at the Proximal Fusion Level Has a Significant Effect on the Incidence of Proximal Junctional Kyphosis and Outcome in Adults After Long Posterior Spinal Fusion. Spine Deform. 2013, 1, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Koike, Y.; Kotani, Y.; Terao, H.; Iwasaki, N. Risk Factor Analysis of Proximal Junctional Kyphosis after Surgical Treatment of Adult Spinal Deformity with Oblique Lateral Interbody Fusion. Asian Spine J. 2021, 15, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Lafage, R.; Line, B.G.; Gupta, S. , et al. Orientation of the Upper-most Instrumented Segment Influences Proximal Junctional Disease Following Adult Spinal Deformity Surgery. Spine 2017, 42, 1570–1577. [Google Scholar] [CrossRef] [PubMed]
- Diebo, B.G.; Shah, N.V.; Stroud, S.G.; Paulino, C.B.; Schwab, F.J.; Lafage, V. Realignment surgery in adult spinal deformity : Prevalence and risk factors for proximal junctional kyphosis. Orthopade. 2018, 47, 301–309. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, S.S.; Suk, S.I. Incidence of proximal adjacent failure in adult lumbar deformity correction based on proximal fusion level. Asian Spine J. 2007, 1, 19–26. [Google Scholar] [CrossRef]
- Shufflebarger, H.; Suk, S.I.; Mardjetko, S. Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine 2006, 31, S185–S194. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Lee, C.S.; Park, J.S.; Lee, K.J. Should Thoracolumbar Junction Be Always Avoided as Upper Instrumented Vertebra in Long Instrumented Fusion for Adult Spinal Deformity?: Risk Factor Analysis for Proximal Junctional Failure. Spine 2020, 45, 686–693. [Google Scholar] [CrossRef]
- Bess, S.; Harris, J.E.; Turner, A.W. , et al. The effect of posterior polyester tethers on the biomechanics of proximal junctional kyphosis: a finite element analysis. J Neurosurg Spine. 2017, 26, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Ha, Y.; Maruo, K.; Racine, L. , et al. Proximal junctional kyphosis and clinical outcomes in adult spinal deformity surgery with fusion from the thoracic spine to the sacrum: a comparison of proximal and distal upper instrumented vertebrae. J Neurosurg Spine. 2013, 19, 360–369. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Lee, C.S.; Chung, S.S.; Lee, J.Y.; Kang, S.S.; Park, S.H. Different Risk Factors of Proximal Junctional Kyphosis and Proximal Junctional Failure Following Long Instrumented Fusion to the Sacrum for Adult Spinal Deformity: Survivorship Analysis of 160 Patients. Neurosurgery 2017, 80, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Pfirrmann, C.W.; Metzdorf, A.; Zanetti, M.; Hodler, J.; Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001, 26, 1873–1878. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.C.; Cha, J.G.; Kim, Y.; Kim, Y.I.; Shin, B.J. Quantitative analysis of back muscle degeneration in the patients with the degenerative lumbar flat back using a digital image analysis: comparison with the normal controls. Spine 2008, 33, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Janssen, M.M.; Drevelle, X.; Humbert, L.; Skalli, W.; Castelein, R.M. Differences in male and female spino-pelvic alignment in asymptomatic young adults: a three-dimensional analysis using upright low-dose digital biplanar X-rays. Spine 2009, 34, E826–E832. [Google Scholar] [CrossRef] [PubMed]
- Vialle, R.; Levassor, N.; Rillardon, L.; Templier, A.; Skalli, W.; Guigui, P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005, 87, 260–267. [Google Scholar] [CrossRef]
- Fukushima, K.; Miyagi, M.; Inoue, G. , et al. Relationship between spinal sagittal alignment and acetabular coverage: a patient-matched control study. Arch Orthop Trauma Surg. 2018, 138, 1495–1499. [Google Scholar] [CrossRef]
- Zou, L.; Liu, J.; Lu, H. Characteristics and risk factors for proximal junctional kyphosis in adult spinal deformity after correction surgery: a systematic review and meta-analysis. Neurosurg Rev. 2019, 42, 671–682. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Phan, K.; Cheung, Z.B. , et al. Surgical, Radiographic, and Patient-Related Risk Factors for Proximal Junctional Kyphosis: A Meta-Analysis. Global Spine J. 2019, 9, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.T.; Lane, J.M. Osteoporosis: a review. Clin Orthop Relat Res. 2004, 126–134. [Google Scholar] [CrossRef]
- Kirkaldy-Willis, W.H.; Farfan, H.F. Instability of the lumbar spine. Clin Orthop Relat Res. 1982, 110–123. [Google Scholar] [CrossRef]
- Marques, E.A.; Wanderley, F.; Machado, L. , et al. Effects of resistance and aerobic exercise on physical function, bone mineral density, OPG and RANKL in older women. Exp Gerontol. 2011, 46, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Byun, C.W.; Cho, J.H.; Lee, C.S.; Lee, D.H.; Hwang, C.J. Effect of overcorrection on proximal junctional kyphosis in adult spinal deformity: analysis by age-adjusted ideal sagittal alignment. Spine J. 2022, 22, 635–645. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Bridwell, K.H.; Lenke, L.G. , et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine 2014, 39, E576–E580. [Google Scholar] [CrossRef] [PubMed]
- Maruo, K.; Ha, Y.; Inoue, S. , et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine 2013, 38, E1469–E1476. [Google Scholar] [CrossRef] [PubMed]
- Yagi, M.; King, A.B.; Boachie-Adjei, O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine 2012, 37, 1479–1489. [Google Scholar] [CrossRef]
- Fujimori, T.; Inoue, S.; Le, H. , et al. Long fusion from sacrum to thoracic spine for adult spinal deformity with sagittal imbalance: upper versus lower thoracic spine as site of upper instrumented vertebra. Neurosurg Focus 2014, 36, E9. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Lenke, L.G.; Cho, S.K. , et al. Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery 2013, 72, 899–906. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).