Submitted:
03 July 2024
Posted:
04 July 2024
You are already at the latest version
Abstract
Keywords:
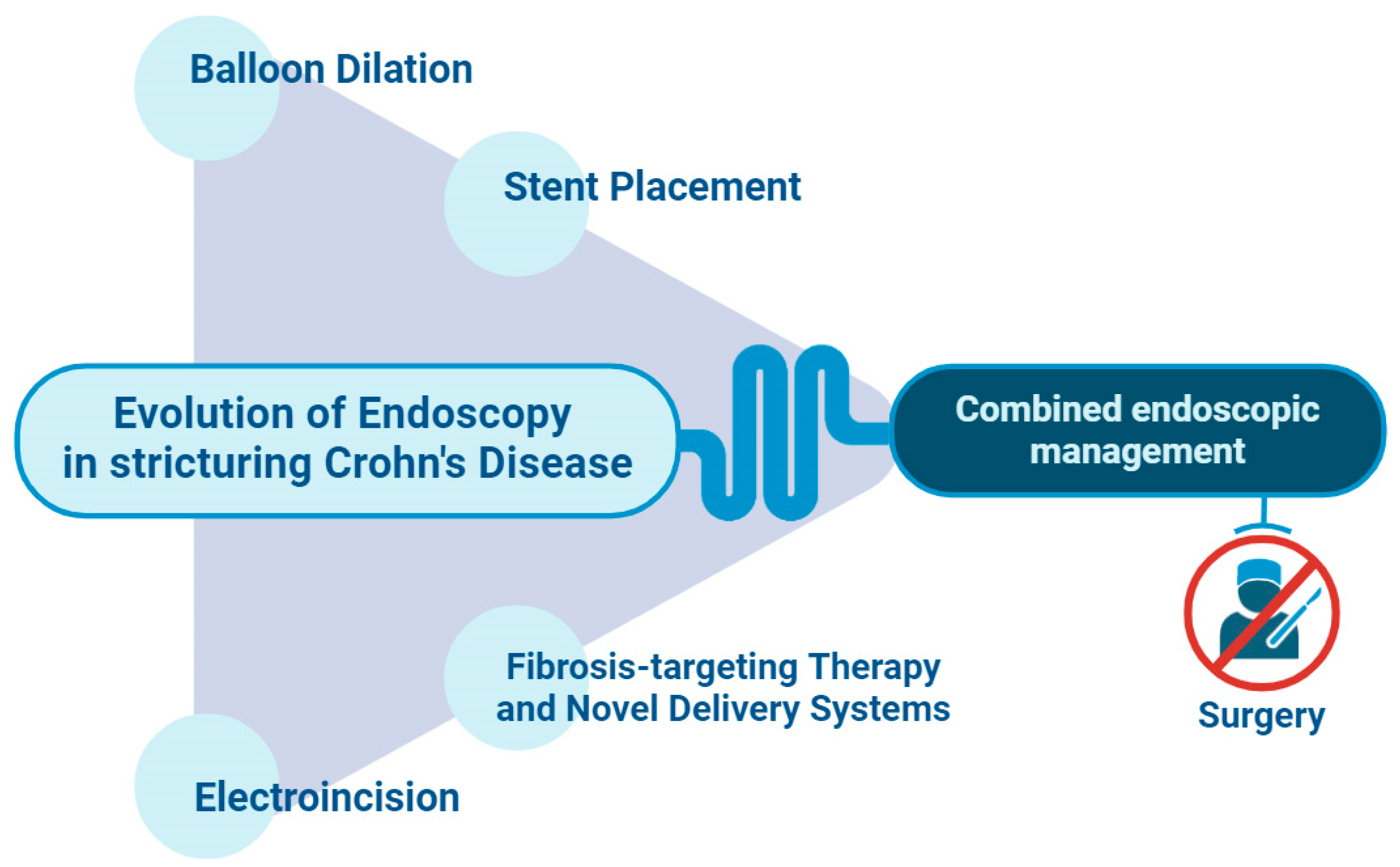
1. Introduction
2. Endoscopic Balloon Dilation
2.1. Endoscopic Balloon Dilation as the Standard Endoscopic Procedure for Short Strictures in Crohn’s Disease
2.2. Intralesional Corticosteroid Injection
2.3. Endoscopic Balloon Dilation in the Upper Gastrointestinal Tract
2.4. Focus on Dilation during Enteroscopy, a Stand-alone Situation?
3. Endoscopic Electroincision: Stricturotomy and Strictureplasty
4. The Graveyard of Endoscopic Techniques: Is There Room for a Second Chance?
4.1. Anti-TNF Intralesional Injection
4.2. Self-Expanding Metal Stents
4.3. Lumen-Apposing Metal Stents
4.4. Biodegradable Stents
5. New Techniques and Future Scenarios for Stenosis and Fibrosis Treatment in IBD Involving Pathogenesis and Molecular Pathways
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Torres, J.; Mehandru, S.; Colombel, J.-F.; Peyrin-Biroulet, L. Crohn’s disease. Lancet 2017, 389, 1741–1755. [Google Scholar] [CrossRef] [PubMed]
- Rieder, F.; Zimmermann, E.M.; Remzi, F.H.; Sandborn, W.J. Crohn’s disease complicated by strictures: a systematic review. Gut 2013, 62, 1072–1084. [Google Scholar] [CrossRef] [PubMed]
- Gasche, C.; Scholmerich, J.; Brynskov, J.; DʼHaens, G.; Hanauer, S.B.; Irvine, J.E.; Jewell, D.P.; Rachmilewitz, D.; Sachar, D.B.; Sandborn, W.J.; Sutherland, L.R. A simple classification of crohnʼs disease: report of the working party for the world congresses of gastroenterology, vienna 1998. Inflammatory bowel diseases 2000, 6, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Nikolaus, S.; Schreiber, S. Diagnostics of inflammatory bowel disease. Gastroenterology 2007, 133, 1670–1689. [Google Scholar] [CrossRef] [PubMed]
- Rieder, F.; Latella, G.; Magro, F.; Yuksel, E.S.; Higgins, P.D.R.; Di Sabatino, A.; de Bruyn, J.R.; Rimola, J.; Brito, J.; Bettenworth, D.; van Assche, G.; Bemelman, W.; d’Hoore, A.; Pellino, G.; Dignass, A.U. European crohn’s and colitis organisation topical review on prediction, diagnosis and management of fibrostenosing crohn’s disease. J Crohns Colitis 2016, 10, 873–885. [Google Scholar] [CrossRef] [PubMed]
- Maaser, C.; Sturm, A.; Vavricka, S.R.; Kucharzik, T.; Fiorino, G.; Annese, V.; Calabrese, E.; Baumgart, D.C.; Bettenworth, D.; Borralho Nunes, P.; Burisch, J.; Castiglione, F.; Eliakim, R.; Ellul, P.; González-Lama, Y.; Gordon, H.; Halligan, S.; Katsanos, K.; Kopylov, U.; Kotze, P.G. ; European Crohn’s and Colitis Organisation [ECCO] and the European Society of Gastrointestinal and Abdominal Radiology [ESGAR] ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis 2019, 13, 144–164. [Google Scholar] [CrossRef] [PubMed]
- Lopes, S.; Rodrigues-Pinto, E.; Andrade, P.; Afonso, J.; Baron, T.H.; Magro, F.; Macedo, G. Endoscopic balloon dilation of Crohn’s disease strictures-safety, efficacy and clinical impact. World J. Gastroenterol. 2017, 23, 7397–7406. [Google Scholar] [CrossRef] [PubMed]
- Pokala, A.; Shen, B. Update of endoscopic management of Crohn’s disease strictures. Intest. Res. 2020, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Shen, B.; Kochhar, G.; Navaneethan, U.; Farraye, F.A.; Schwartz, D.A.; Iacucci, M.; Bernstein, C.N.; Dryden, G.; Cross, R.; Bruining, D.H.; Kobayashi, T.; Lukas, M.; Shergill, A.; Bortlik, M.; Lan, N.; Lukas, M.; Tang, S.-J.; Kotze, P.G.; Kiran, R.P.; Dulai, P.S.; Sandborn, W.J. Practical guidelines on endoscopic treatment for Crohn’s disease strictures: a consensus statement from the Global Interventional Inflammatory Bowel Disease Group. Lancet Gastroenterol. Hepatol. 2020, 5, 393–405. [Google Scholar] [CrossRef]
- Nardone, O.M.; Cannatelli, R.; Zardo, D.; Ghosh, S.; Iacucci, M. Can advanced endoscopic techniques for assessment of mucosal inflammation and healing approximate histology in inflammatory bowel disease? Therap. Adv. Gastroenterol. 2019, 12, 1756284819863015. [Google Scholar] [CrossRef]
- Santacroce, G.; Zammarchi, I.; Tan, C.K.; Coppola, G.; Varley, R.; Ghosh, S.; Iacucci, M. Present and future of endoscopy precision for inflammatory bowel disease. Dig. Endosc. 2024, 36, 292–304. [Google Scholar] [CrossRef] [PubMed]
- Klag, T.; Wehkamp, J.; Goetz, M. Endoscopic Balloon Dilation for Crohn’s Disease-Associated Strictures. Clin. Endosc. 2017, 50, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Bettenworth, D.; Bokemeyer, A.; Kou, L.; Lopez, R.; Bena, J.F.; El Ouali, S.; Mao, R.; Kurada, S.; Bhatt, A.; Beyna, T.; Halloran, B.; Reeson, M.; Hosomi, S.; Kishi, M.; Hirai, F.; Ohmiya, N.; Rieder, F. Systematic review with meta-analysis: efficacy of balloon-assisted enteroscopy for dilation of small bowel Crohn’s disease strictures. Aliment. Pharmacol. Ther. 2020, 52, 1104–1116. [Google Scholar] [CrossRef] [PubMed]
- Reutemann, B.A.; Turkeltaub, J.A.; Al-Hawary, M.; Waljee, A.K.; Higgins, P.D.R.; Stidham, R.W. Endoscopic balloon dilation size and avoidance of surgery in stricturing crohn’s disease. Inflamm. Bowel Dis. 2017, 23, 1803–1809. [Google Scholar] [CrossRef] [PubMed]
- Bettenworth, D.; Gustavsson, A.; Atreja, A.; Lopez, R.; Tysk, C.; van Assche, G.; Rieder, F. A Pooled Analysis of Efficacy, Safety, and Long-term Outcome of Endoscopic Balloon Dilation Therapy for Patients with Stricturing Crohn’s Disease. Inflamm. Bowel Dis. 2017, 23, 133–142. [Google Scholar] [CrossRef]
- Bettenworth, D.; Mücke, M.M.; Lopez, R.; Singh, A.; Zhu, W.; Guo, F.; Matsui, T.; James, T.W.; Herfarth, H.; Goetz, M.; Mao, R.; Kurada, S.; Hampe, J.; Matthes, K.; Karstensen, J.G.; Valli, P.V.; Duijvestein, M.; D’Haens, G.; Jairath, V.; Qiu, T.B.; Rieder, F. Efficacy of Endoscopic Dilation of Gastroduodenal Crohn’s Disease Strictures: A Systematic Review and Meta-Analysis of Individual Patient Data. Clin. Gastroenterol. Hepatol. 2019, 17, 2514–2522.e8. [Google Scholar] [CrossRef] [PubMed]
- Lian, L.; Stocchi, L.; Remzi, F.H.; Shen, B. Comparison of endoscopic dilation vs surgery for anastomotic stricture in patients with crohn’s disease following ileocolonic resection. Clin. Gastroenterol. Hepatol. 2017, 15, 1226–1231. [Google Scholar] [CrossRef]
- Chen, Y.; Sun, Z.; Li, Z.; Duan, M.; Zhou, Y.; Li, Y.; Zhu, W.; Guo, Z. Comparison of endoscopic balloon dilation and surgery for duodenal stricture in patients with Crohn’s disease. Scand. J. Gastroenterol. 2024, 59, 39–45. [Google Scholar] [CrossRef]
- Lan, N.; Shen, B. Endoscopic stricturotomy versus balloon dilation in the treatment of anastomotic strictures in crohn’s disease. Inflamm. Bowel Dis. 2018, 24, 897–907. [Google Scholar] [CrossRef]
- Lan, N.; Stocchi, L.; Delaney, C.P.; Hull, T.L.; Shen, B. Endoscopic stricturotomy versus ileocolonic resection in the treatment of ileocolonic anastomotic strictures in Crohn’s disease. Gastrointest. Endosc. 2019, 90, 259–268. [Google Scholar] [CrossRef]
- Lan, N.; Hull, T.L.; Shen, B. Endoscopic stricturotomy and ileo-colonic resection in patients with primary Crohn’s disease-related distal ileum strictures. Gastroenterol Rep (Oxf) 2020, 8, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Loras, C.; Andújar, X.; Gornals, J.B.; Sanchiz, V.; Brullet, E.; Sicilia, B.; Martín-Arranz, M.D.; Naranjo, A.; Barrio, J.; Dueñas, C.; Foruny, J.R.; Busquets, D.; Monfort, D.; Pineda, J.R.; González-Huix, F.; Pérez-Roldán, F.; Pons, V.; González, B.; Reyes Moreno, J.; Sainz, E. ; Grupo Español de Trabajo de la Enfermedad de Crohn y Colitis Ulcerosa (GETECCU) Self-expandable metal stents versus endoscopic balloon dilation for the treatment of strictures in Crohn’s disease (ProtDilat study): an open-label, multicentre, randomised trial. Lancet Gastroenterol. Hepatol. 2022, 7, 332–341. [Google Scholar] [CrossRef]
- East, J.E.; Brooker, J.C.; Rutter, M.D.; Saunders, B.P. A pilot study of intrastricture steroid versus placebo injection after balloon dilatation of Crohn’s strictures. Clin. Gastroenterol. Hepatol. 2007, 5, 1065–1069. [Google Scholar] [CrossRef] [PubMed]
- Di Nardo, G.; Oliva, S.; Passariello, M.; Pallotta, N.; Civitelli, F.; Frediani, S.; Gualdi, G.; Gandullia, P.; Mallardo, S.; Cucchiara, S. Intralesional steroid injection after endoscopic balloon dilation in pediatric Crohn’s disease with stricture: a prospective, randomized, double-blind, controlled trial. Gastrointest. Endosc. 2010, 72, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Feleshtynskiy, Y.; Mylianovska, A.; Pirogovsky, V.; Dyadyk, O. Evaluation of the endoscopic treatment with topical prednisolone administration for intestinal strictures in Crohn’s disease. Pol. Przegl. Chir. 2021, 94, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Chittajallu, V.; Omar, Y.A.; Simons-Linares, C.R.; Chahal, P. Endoscopic balloon dilation management for benign duodenal stenosis. Surg. Endosc. 2023, 37, 3610–3618. [Google Scholar] [CrossRef] [PubMed]
- Hirai, F.; Andoh, A.; Ueno, F.; Watanabe, K.; Ohmiya, N.; Nakase, H.; Kato, S.; Esaki, M.; Endo, Y.; Yamamoto, H.; Matsui, T.; Iida, M.; Hibi, T.; Watanabe, M.; Suzuki, Y.; Matsumoto, T. Efficacy of Endoscopic Balloon Dilation for Small Bowel Strictures in Patients With Crohn’s Disease: A Nationwide, Multi-centre, Open-label, Prospective Cohort Study. J Crohns Colitis 2018, 12, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Gionchetti, P.; Dignass, A.; Danese, S.; Magro Dias, F.J.; Rogler, G.; Lakatos, P.L.; Adamina, M.; Ardizzone, S.; Buskens, C.J.; Sebastian, S.; Laureti, S.; Sampietro, G.M.; Vucelic, B.; van der Woude, C.J.; Barreiro-de Acosta, M.; Maaser, C.; Portela, F.; Vavricka, S.R.; Gomollón, F. ; ECCO 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 2: Surgical Management and Special Situations. J Crohns Colitis 2017, 11, 135–149. [Google Scholar] [CrossRef]
- Adamina, M.; Bonovas, S.; Raine, T.; Spinelli, A.; Warusavitarne, J.; Armuzzi, A.; Bachmann, O.; Bager, P.; Biancone, L.; Bokemeyer, B.; Bossuyt, P.; Burisch, J.; Collins, P.; Doherty, G.; El-Hussuna, A.; Ellul, P.; Fiorino, G.; Frei-Lanter, C.; Furfaro, F.; Gingert, C.; Zmora, O. ECCO guidelines on therapeutics in crohn’s disease: surgical treatment. J Crohns Colitis 2020, 14, 155–168. [Google Scholar] [CrossRef]
- Bamba, S.; Sakemi, R.; Fujii, T.; Takeda, T.; Fujioka, S.; Takenaka, K.; Kitamoto, H.; Umezawa, S.; Sakuraba, H.; Inokuchi, T.; Fukata, N.; Mizuno, S.; Yamashita, M.; Shinzaki, S.; Tanaka, H.; Takedatsu, H.; Ozaki, R.; Moriya, K.; Ishii, M.; Kinjo, T.; Hibi, T. A nationwide, multi-center, retrospective study of symptomatic small bowel stricture in patients with Crohn’s disease. J. Gastroenterol. 2020, 55, 615–626. [Google Scholar] [CrossRef]
- Baars, J.E.; Theyventhiran, R.; Aepli, P.; Saxena, P.; Kaffes, A.J. Double-balloon enteroscopy-assisted dilatation avoids surgery for small bowel strictures: A systematic review. World J. Gastroenterol. 2017, 23, 8073–8081. [Google Scholar] [CrossRef]
- Yamamoto, H.; Yano, T.; Araki, A.; Esaki, M.; Ohtsuka, K.; Ohmiya, N.; Oka, S.; Nakase, H.; Bamba, S.; Hirai, F.; Hosoe, N.; Matsuda, T.; Mitsui, K.; Watanabe, K.; Ogata, H.; Katsuki, S.; Matsumoto, T.; Fujishiro, M.; Fujimoto, K.; Inoue, H. Guidelines for endoscopic balloon dilation in treating Crohn’s disease-associated small intestinal strictures (supplement to the Clinical Practice Guidelines for Enteroscopy). Dig. Endosc. 2022, 34, 1278–1296. [Google Scholar] [CrossRef]
- Fukumoto, A.; Tanaka, S.; Yamamoto, H.; Yao, T.; Matsui, T.; Iida, M.; Goto, H.; Sakamoto, C.; Chiba, T.; Sugano, K. Diagnosis and treatment of small-bowel stricture by double balloon endoscopy. Gastrointest. Endosc. 2007, 66, S108–12. [Google Scholar] [CrossRef] [PubMed]
- Fukatsu, H.; Kawamoto, H.; Harada, R.; Tsutsumi, K.; Fujii, M.; Kato, H.; Hirao, K.; Nakanishi, T.; Mizuno, O.; Ogawa, T.; Ishida, E.; Okada, H.; Sakaguchi, K. Quantitative assessment of technical proficiency in performing needle-knife precut papillotomy. Surg. Endosc. 2009, 23, 2066–2072. [Google Scholar] [CrossRef]
- Simmons, D.T.; Baron, T.H. Electroincision of refractory esophagogastric anastomotic strictures. Dis. Esophagus 2006, 19, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Tringali, A.; Milluzzo, S.M.; Perri, V.; Schepis, T.; Bove, V.; Costamagna, G. Endoscopic electroincision of challenging benign biliopancreatic strictures. Endosc. Int. Open 2022, 10, E1297–E1301. [Google Scholar] [CrossRef]
- Shen, B.; Lian, L.; Kiran, R.P.; Queener, E.; Lavery, I.C.; Fazio, V.W.; Remzi, F.H. Efficacy and safety of endoscopic treatment of ileal pouch strictures. Inflamm. Bowel Dis. 2011, 17, 2527–2535. [Google Scholar] [CrossRef]
- Lan, N.; Shen, B. Endoscopic Stricturotomy with Needle Knife in the Treatment of Strictures from Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2017, 23, 502–513. [Google Scholar] [CrossRef] [PubMed]
- Kouladouros, K.; Reissfelder, C.; Kähler, G. Endoscopic Stricturoplasty with Linear Stapler: An Efficient Alternative for the Refractory Rectal Anastomotic Stricture. Dig. Dis. Sci. 2023, 68, 4432–4438. [Google Scholar] [CrossRef]
- Herman, K.; Kiran, R.P.; Shen, B. Insulated tip/needle-knife endoscopic stricturotomy is safe and effective for treatment of non-traversable anorectal strictures. Endosc. Int. Open 2024, 12, E231–E236. [Google Scholar] [CrossRef]
- Ning, S.-B.; Yang, H.; Li, B.; Zhang, Y.; Huang, S.; Peng, B.; Lin, H.; Kurban, M.; Li, M.; Guo, Q. Balloon-assisted enteroscopy-based endoscopic stricturotomy for deep small bowel strictures from Crohn’s disease: First cohort study of a novel approach. Dig. Liver Dis. 2023, 55, 1397–1402. [Google Scholar] [CrossRef] [PubMed]
- Swaminath, A.; Lichtiger, S. Dilation of colonic strictures by intralesional injection of infliximab in patients with Crohn’s colitis. Inflamm. Bowel Dis. 2008, 14, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Hendel, J.; Karstensen, J.G.; Vilmann, P. Serial intralesional injections of infliximab in small bowel Crohn’s strictures are feasible and might lower inflammation. United European Gastroenterol. J. 2014, 2, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, D.; Avellini, C.; Beltrami, C.A.; Pasqual, E.; Zearo, E. Selective effect of infliximab on the inflammatory component of a colonic stricture in Crohn’s disease. Int. J. Colorectal Dis. 2006, 21, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Loras Alastruey, C.; Andújar Murcia, X.; Esteve Comas, M. The role of stents in the treatment of Crohn’s disease strictures. Endosc. Int. Open 2016, 4, E301–8. [Google Scholar] [CrossRef]
- Loras, C.; Pérez-Roldan, F.; Gornals, J.B.; Barrio, J.; Igea, F.; González-Huix, F.; González-Carro, P.; Pérez-Miranda, M.; Espinós, J.C.; Fernández-Bañares, F.; Esteve, M. Endoscopic treatment with self-expanding metal stents for Crohn’s disease strictures. Aliment. Pharmacol. Ther. 2012, 36, 833–839. [Google Scholar] [CrossRef]
- Levine, R.A.; Wasvary, H.; Kadro, O. Endoprosthetic management of refractory ileocolonic anastomotic strictures after resection for Crohn’s disease: report of nine-year follow-up and review of the literature. Inflamm. Bowel Dis. 2012, 18, 506–512. [Google Scholar] [CrossRef]
- Attar, A.; Maunoury, V.; Vahedi, K.; Vernier-Massouille, G.; Vida, S.; Bulois, P.; Colombel, J.F.; Bouhnik, Y. ; GETAID Safety and efficacy of extractible self-expandable metal stents in the treatment of Crohn’s disease intestinal strictures: a prospective pilot study. Inflamm. Bowel Dis. 2012, 18, 1849–1854. [Google Scholar] [CrossRef]
- Das, R.; Singh, R.; Din, S.; Lund, J.; Krishnamoorthy, R.; Hearing, S.; Norton, B.; Williams, J.; Fraser, C.; Goddard, A.; Cole, A. Therapeutic resolution of focal, predominantly anastomotic Crohn’s disease strictures using removable stents: outcomes from a single-center case series in the United Kingdom. Gastrointest. Endosc. 2020, 92, 344–352. [Google Scholar] [CrossRef]
- Branche, J.; Attar, A.; Vernier-Massouille, G.; Bulois, P.; Colombel, J.F.; Bouhnik, Y.; Maunoury, V. Extractible self-expandable metal stent in the treatment of Crohn’s disease anastomotic strictures. Endoscopy 2012, 44 Suppl 2 UCTN, E325–6. [Google Scholar] [CrossRef]
- Attar, A.; Branche, J.; Coron, E.; Privat, J.; Caillo, L.; Chevaux, J.-B.; Vuitton, L.; Amiot, A.; Belkhodja, H.; Dray, X.; Ponchon, T.; Bouhnik, Y.; Baumann, C.; Peyrin-Biroulet, L. An Anti-migration Self-expandable and Removable Metal Stent for Crohn’s Disease Strictures: A Nationwide Study From GETAID and SFED. J Crohns Colitis 2021, 15, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Loras, C.; Ruiz-Ramirez, P.; Romero, J.; Andújar, X.; Bargallo, J.; Bernardos, E.; Boscá-Watts, M.M.; Brugiotti, C.; Brunet, E.; Busquets, D.; Cerrillo, E.; Cortina, F.J.; Díaz-Milanés, J.A.; Dueñas, C.; Farrés, R.; Golda, T.; González-Huix, F.; Gornals, J.B.; Guardiola, J.; Julià, D. ; Grupo Español de Trabajo de la Enfermedad de Crohn y Colitis Ulcerosa GETECCU Endoscopic treatment (endoscopic balloon dilation/self-expandable metal stent) vs surgical resection for the treatment of de novo stenosis in Crohn’s disease (ENDOCIR study): an open-label, multicentre, randomized trial. Trials 2023, 24, 432. [Google Scholar] [CrossRef] [PubMed]
- van Boeckel, P.G.A.; Siersema, P.D. Refractory esophageal strictures: what to do when dilation fails. Curr. Treat. Options Gastroenterol. 2015, 13, 47–58. [Google Scholar] [CrossRef] [PubMed]
- Hallac, A.; Srikureja, W.; Liu, E.; Dhumal, P.; Thatte, A.; Puri, N. Economical effect of lumen apposing metal stents for treating benign foregut strictures. World J. Gastrointest. Endosc. 2018, 10, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Adler, D.G. Lumen-Apposing Metal Stents for the Treatment of Refractory Benign Esophageal Strictures. Am. J. Gastroenterol. 2017, 112, 516–517. [Google Scholar] [CrossRef] [PubMed]
- Mirchin, R.B.; Mahmood, S.K. Lumen-Apposing Metal Stent Used to Treat Malignant Esophageal Stricture. ACG Case Rep. J. 2020, 7, e00362. [Google Scholar] [CrossRef] [PubMed]
- Axelrad, J.E.; Lichtiger, S.; Sethi, A. Treatment of Crohn’s Disease Anastomotic Stricture With a Lumen-apposing Metal Stent. Clin. Gastroenterol. Hepatol. 2018, 16, A25–A26. [Google Scholar] [CrossRef] [PubMed]
- Marcellier, G.; Lorenzo, D.; Hedjoudje, A.; Jais, B.; Bouhnik, Y.; Prat, F. First treatment of Crohn’s disease refractory anastomotic stricture with a lumen-apposing metallic stent suitable for colonoscopy. Endoscopy 2022, 54, E409–E410. [Google Scholar] [CrossRef]
- Hedjoudje, A.; Jais, B.; Stefanescu, C.; Lorenzo, D.; Aubert, A.; Badurdeen, D.; Bouhnik, Y.; Prat, F. Clinical Efficacy of Lumen-Apposing Metallic Stents for Lower Gastrointestinal Anastomotic Strictures. J. Gastrointest. Surg. 2023, 27, 1458–1460. [Google Scholar] [CrossRef]
- Griffiths, E.A.; Gregory, C.J.; Pursnani, K.G.; Ward, J.B.; Stockwell, R.C. The use of biodegradable (SX-ELLA) oesophageal stents to treat dysphagia due to benign and malignant oesophageal disease. Surg. Endosc. 2012, 26, 2367–2375. [Google Scholar] [CrossRef]
- Saito, Y.; Tanaka, T.; Andoh, A.; Minematsu, H.; Hata, K.; Tsujikawa, T.; Nitta, N.; Murata, K.; Fujiyama, Y. Usefulness of biodegradable stents constructed of poly-l-lactic acid monofilaments in patients with benign esophageal stenosis. World J. Gastroenterol. 2007, 13, 3977–3980. [Google Scholar] [CrossRef] [PubMed]
- Krokidis, M.; Burke, C.; Spiliopoulos, S.; Gkoutzios, P.; Hynes, O.; Ahmed, I.; Dourado, R.; Sabharwal, T.; Mason, R.; Adam, A. The use of biodegradable stents in malignant oesophageal strictures for the treatment of dysphagia before neoadjuvant treatment or radical radiotherapy: a feasibility study. Cardiovasc. Intervent. Radiol. 2013, 36, 1047–1054. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-Zúñiga, V.; Moreno-de-Vega, V.; Marín, I.; Boix, J. Biodegradable stents in gastrointestinal endoscopy. World J. Gastroenterol. 2014, 20, 2212–2217. [Google Scholar] [CrossRef] [PubMed]
- Rejchrt, S.; Kopacova, M.; Brozik, J.; Bures, J. Biodegradable stents for the treatment of benign stenoses of the small and large intestines. Endoscopy 2011, 43, 911–917. [Google Scholar] [CrossRef] [PubMed]
- Karstensen, J.G.; Vilmann, P.; Hendel, J. Successful endoscopic treatment of a 12-cm small-bowel Crohn stricture with a custom-made biodegradable stent. Endoscopy 2014, 46 Suppl 1 UCTN, E227–8. [Google Scholar] [CrossRef]
- Karstensen, J.G.; Christensen, K.R.; Brynskov, J.; Rønholt, C.; Vilmann, P.; Hendel, J. Biodegradable stents for the treatment of bowel strictures in Crohn’s disease: technical results and challenges. Endosc. Int. Open 2016, 4, E296–300. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.C.; Chang, C.; Boschetti, G.; Ungaro, R.; Giri, M.; Grout, J.A.; Gettler, K.; Chuang, L.-S.; Nayar, S.; Greenstein, A.J.; Dubinsky, M.; Walker, L.; Leader, A.; Fine, J.S.; Whitehurst, C.E.; Mbow, M.L.; Kugathasan, S.; Denson, L.A.; Hyams, J.S.; Friedman, J.R.; Kenigsberg, E. Single-Cell Analysis of Crohn’s Disease Lesions Identifies a Pathogenic Cellular Module Associated with Resistance to Anti-TNF Therapy. Cell 2019, 178, 1493–1508.e20. [Google Scholar] [CrossRef] [PubMed]
- Corridoni, D.; Antanaviciute, A.; Gupta, T.; Fawkner-Corbett, D.; Aulicino, A.; Jagielowicz, M.; Parikh, K.; Repapi, E.; Taylor, S.; Ishikawa, D.; Hatano, R.; Yamada, T.; Xin, W.; Slawinski, H.; Bowden, R.; Napolitani, G.; Brain, O.; Morimoto, C.; Koohy, H.; Simmons, A. Single-cell atlas of colonic CD8+ T cells in ulcerative colitis. Nat. Med. 2020, 26, 1480–1490. [Google Scholar] [CrossRef] [PubMed]
- Kurahara, L.H.; Hiraishi, K.; Hu, Y.; Koga, K.; Onitsuka, M.; Doi, M.; Aoyagi, K.; Takedatsu, H.; Kojima, D.; Fujihara, Y.; Jian, Y.; Inoue, R. Activation of myofibroblast TRPA1 by steroids and pirfenidone ameliorates fibrosis in experimental crohn’s disease. Cell. Mol. Gastroenterol. Hepatol. 2018, 5, 299–318. [Google Scholar] [CrossRef]
- Li, X.; Yu, M.; Zhao, Q.; Yu, Y. Prospective therapeutics for intestinal and hepatic fibrosis. Bioeng. Transl. Med. 2023, 8, e10579. [Google Scholar] [CrossRef]
- Solitano, V.; Jairath, V.; Ungaro, F.; Peyrin-Biroulet, L.; Danese, S. TL1A inhibition for inflammatory bowel disease treatment: From inflammation to fibrosis. MED 2024, 5, 386–400. [Google Scholar] [CrossRef] [PubMed]
- Ye, Y.; Zhang, X.; Su, D.; Ren, Y.; Cheng, F.; Yao, Y.; Shi, G.; Ji, Y.; Chen, S.; Shi, P.; Dai, L.; Su, X.; Deng, H. Therapeutic efficacy of human adipose mesenchymal stem cells in Crohn’s colon fibrosis is improved by IFN-γ and kynurenic acid priming through indoleamine 2,3-dioxygenase-1 signaling. Stem Cell Res. Ther. 2022, 13, 465. [Google Scholar] [CrossRef] [PubMed]
- Lian, L.; Huang, Q.; Zhang, L.; Qin, H.; He, X.; He, X.; Ke, J.; Xie, M.; Lan, P. Anti-fibrogenic Potential of Mesenchymal Stromal Cells in Treating Fibrosis in Crohn’s Disease. Dig. Dis. Sci. 2018, 63, 1821–1834. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Kim, W.R.; Kim, D.H.; Kim, J.H.; Yoo, J.H. Human umbilical cord/placenta mesenchymal stem cell conditioned medium attenuates intestinal fibrosis in vivo and in vitro. Stem Cell Res. Ther. 2024, 15, 69. [Google Scholar] [CrossRef] [PubMed]
- Goffin, L.; Fagagnini, S.; Vicari, A.; Mamie, C.; Melhem, H.; Weder, B.; Lutz, C.; Lang, S.; Scharl, M.; Rogler, G.; Chvatchko, Y.; Hausmann, M. Anti-MMP-9 Antibody: A Promising Therapeutic Strategy for Treatment of Inflammatory Bowel Disease Complications with Fibrosis. Inflamm. Bowel Dis. 2016, 22, 2041–2057. [Google Scholar] [CrossRef] [PubMed]
- Pizzoferrato, M.; Puca, P.; Ennas, S.; Cammarota, G.; Guidi, L. Glucagon-like peptide-2 analogues for Crohn’s disease patients with short bowel syndrome and intestinal failure. World J. Gastroenterol. 2022, 28, 6258–6270. [Google Scholar] [CrossRef]
- Costa, B.P.; Gonçalves, A.C.; Abrantes, A.M.; Matafome, P.; Seiça, R.; Sarmento-Ribeiro, A.B.; Botelho, M.F.; Castro-Sousa, F. Teduglutide effects on gene regulation of fibrogenesis on an animal model of intestinal anastomosis. J. Surg. Res. 2017, 216, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, C.D.; Claudel, T.; Mlitz, V.; Riva, A.; Menz, M.; Brusilovskaya, K.; Haller, F.; Baumgartner, M.; Königshofer, P.; Unger, L.W.; Sjöland, W.; Scharnagl, H.; Stojakovic, T.; Busslinger, G.; Reiberger, T.; Marschall, H.-U.; Trauner, M. GLP-2 Improves Hepatic Inflammation and Fibrosis in Mdr2-/- Mice Via Activation of NR4a1/Nur77 in Hepatic Stellate Cells and Intestinal FXR Signaling. Cell. Mol. Gastroenterol. Hepatol. 2023, 16, 847–856. [Google Scholar] [CrossRef] [PubMed]
- Nassani, N.; Alsheikh, M.; Carroll, B.; Nguyen, D.; Carroll, R.E. Theranostic gastrointestinal endoscopy: bringing healing light to the lumen. Clin. Transl. Gastroenterol. 2020, 11, e00119. [Google Scholar] [CrossRef]
- Chen, F.; Liu, Q.; Xiong, Y.; Xu, L. Current Strategies and Potential Prospects of Nanomedicine-Mediated Therapy in Inflammatory Bowel Disease. Int. J. Nanomedicine 2021, 16, 4225–4237. [Google Scholar] [CrossRef]
- Nishida, T.; Takeno, S.; Nakashima, K.; Kariya, M.; Inatsu, H.; Kitamura, K.; Nanashima, A. Salvage photodynamic therapy accompanied by extended lymphadenectomy for advanced esophageal carcinoma: A case report. Int. J. Surg. Case Rep. 2017, 36, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Ertan, A.; Zaheer, I.; Correa, A.M.; Thosani, N.; Blackmon, S.H. Photodynamic therapy vs radiofrequency ablation for Barrett’s dysplasia: efficacy, safety and cost-comparison. World J. Gastroenterol. 2013, 19, 7106–7113. [Google Scholar] [CrossRef] [PubMed]
- Hartwig, O.; Shetab Boushehri, M.A.; Shalaby, K.S.; Loretz, B.; Lamprecht, A.; Lehr, C.-M. Drug delivery to the inflamed intestinal mucosa - targeting technologies and human cell culture models for better therapies of IBD. Adv. Drug Deliv. Rev. 2021, 175, 113828. [Google Scholar] [CrossRef]
- Bon, I.; Cano-Sarabia, M.; de la Ossa, N.; Bartolí, R.; Lorenzo-Zúñiga, V. Development and Characterization of a New Endoscopic Drug-Eluting Platform With Proven Efficacy in Acute and Chronic Experimental Colitis. Front Med (Lausanne) 2020, 7, 415. [Google Scholar] [CrossRef] [PubMed]
| Study Design | Strictures location | Treatment and No of pts |
Technical Success Rate | Long-term Outcomes (years fu) |
Adverse events, % | |
|---|---|---|---|---|---|---|
| Lian et al. [17] 2017 | Retrospective | Ileocolic anastomosis | 176 EBD 131 surgery |
- | average time to surgery/re-surgery delayed by 6.45 years in EBD group | 1.1 (perforation) 8.8 (~ infection) |
| Chen et al. [18] 2024 | Retrospective | Duodenal | 30 EBD 18 surgery |
- | 2.96 years recurrence-free 6.31 years recurrence-free, p=.01 |
0,74 16.67 |
| Lan et al. [19] 2018 | Retrospective | Anastomosis (85.7% ileocolic) | 21 ES 164 EBD |
100% 89.5% |
9.5% surgery (0.8) 33.5% re-surgery (4) |
8.8 (bleeding) 1.1 (perforation) |
| Lan et al. [20] 2019 | Retrospective | Ileocolic anastomosis | 35 ES 147 ICR |
- | 11.3% surgery (0.8) 10.2% re-surgery (2.2), p .83 |
10.2 (~ bleeding) 31.9 (~ ileus) |
| Lan et al. [21] 2020 | Retrospective | Distal ileum, ileocecal valve | 13 ES 32 ICR |
100% 100% |
15.4% surgery (1.8) 18.8% re-surgery (1.5), p .79 |
6,9 (perforation) 25 (~ infection) |
| Loras et al. [22] 2022 | Randomized trial | - | 41 EBD 39 FCSEMS |
- | 80% no re-intervention (1) 51% no re-intervention (1), p .0061 |
2 (perforation) 3 (perforation) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





