1. Introduction
The novel coronavirus (COVID-19) emerged in 2019 and primarily spreads through respiratory droplets and close contact. It causes various symptoms including fever, cough, and fatigue, and can lead to severe respiratory issues, particularly in older adults and those with chronic conditions. A significant number of COVID-19 survivors experience long-term symptoms, known as ‘Long COVID’, including reduced lung function and persistent fatigue [
1,
2]. The virus primarily spreads through respiratory means (especially coughing, sneezing, and close conversation), contaminated surfaces, and biological materials [
3]. Clinical symptoms of acute COVID-19 infection include fever, sore throat, cough, fatigue, and gastrointestinal symptoms. Respiratory failure heart, and kidney damage can occur in more severe cases. This is particularly common among older individuals and those with underlying chronic conditions. According to a report, around 60 days after the initial symptoms of COVID-19, only 13% of patients hospitalized for COVID-19 showed no COVID-19-related symptoms, while 32% experienced one or more symptoms. Among them, 55% had three or more symptoms [
4,
5].
The persistence of symptoms with COVID-19 for more than three months after the first onset of symptoms is called “Long COVID-19” [
6]. Recent studies have revealed that more than 60% of COVID-19 survivors experience symptoms not described by an alternative diagnosis [
7]. This was found by reduced FVC, FEC1, and FEV1/FEV values compared to the average population. In a meta-analysis combining data from 18 studies, a 1-year follow-up was conducted on 8,591 survivors of COVID-19. The most common eight symptoms reported were fatigue/weakness (28%), shortness of breath (18%), joint/muscle pain (26%), depression (23%), anxiety (22%), memory loss (19%), difficulty concentrating (18%), and insomnia (12%). Additionally, there were very few reported cases during the early stages of the COVID-19 pandemic. Among those hospitalized, “severe” symptoms threatening their health were observed. Apart from patients admitted with “severe” COVID-19, it is highly likely that millions of people were infected with SARS-CoV-2 without undergoing official COVID-19 testing and receiving hospital treatment [
1,
8]. These patients are classified as having “mild” COVID-19, as they only required home care and were expected to recover from the infection [
9]. Patients with “mild” COVID-19 may still complain of persistent post-COVID-19 symptoms for weeks after the onset [
10]. In particular, fatigue (94.9%) and dyspnoea (89.5%) were the most post-COVID-19 symptoms. This means the presence of multiple symptoms and, in turn, unmet healthcare needs of this sample of “mild” and “Serious” patients with recovery COVID-19 about three months after the infection. The phenomenon that symptoms persist months after the infection suggests the presence of a “post-COVID-19 syndrome” [
11]. In addition, patients with post-COVID-19 symptoms exhibit FVC, FEC1, and FEV1/FEV values with reduced lung function compared to standard groups [
12].
Cardiopulmonary physical therapy focuses on treating and rehabilitating patients with acute and chronic respiratory diseases by the guidelines for treating patients with COVID-19 for physical healers released [
13]. However, given the highly contagious nature of SARS-CoV-2, a robust respiratory rehabilitation plan must be in place to make optimal use of a limited rehabilitation workforce and reduce risk to health professionals [
14]. The effects of respiratory muscle training include increased HPQoL, exercise resistance, strength and endurance of respiratory muscles, improved lung function, and reduced fatigue and dyspnea [
13,
15]. According to a recent study, respiratory rehabilitation for elderly patients with COVID-19 can improve their respiratory function and quality of life and reduce anxiety compared to groups without any intervention [
16]. In this connection, HBMT (home-breathing muscle training) for patients with long-term fatigue and dyspnea after COVID-19 showed improved quality of life (QOL) and respiratory function compared to fake-trained groups [
17].
Until recently, the apps developed to manage COVID-19 mainly focused on contact tracking, symptom monitoring, and information apps [
18]. Nevertheless, recently, remedial education and video guides on the principles of lung rehabilitation and easy exercises at home have been attracting attention for providing it and can be used for guidance and follow-up after discharge with families after discharge [
19]. Completing the recommended exercise process and adhering to these exercises brings about long-term benefits, including reduced pain, improved physical function, and reaching agreed goals [
20]. Long-term adherence can also significantly improve a patient’s quality of life. It can positively benefit the economy as it can decrease the burden on healthcare systems, as patients can self-manage more effectively [
21]. However, a well-established problem when implementing rehabilitation interventions is the adherence rate to home exercise programs [
22]. Kakao is a fast-growing software company focused on providing innovative smartphone applications. The company is rooted in the Korean mobile communication market, where customer demands for high-speed connectivity have grown sharply. That is why Kakao programs are so accessible to Koreans [
23]. Recently, Kakao created a breathing exercise app to improve the symptoms of COIVD-19 aftereffects. However, until now, No studies have analyzed the effect of this breathing exercise app. This study will examine at the relationship between respiratory function and fatigue in COVID-19-cured patients through the “Kakao Health care breathing exercise (KBE)”.
2. Materials and Methods
2.1. Study Design
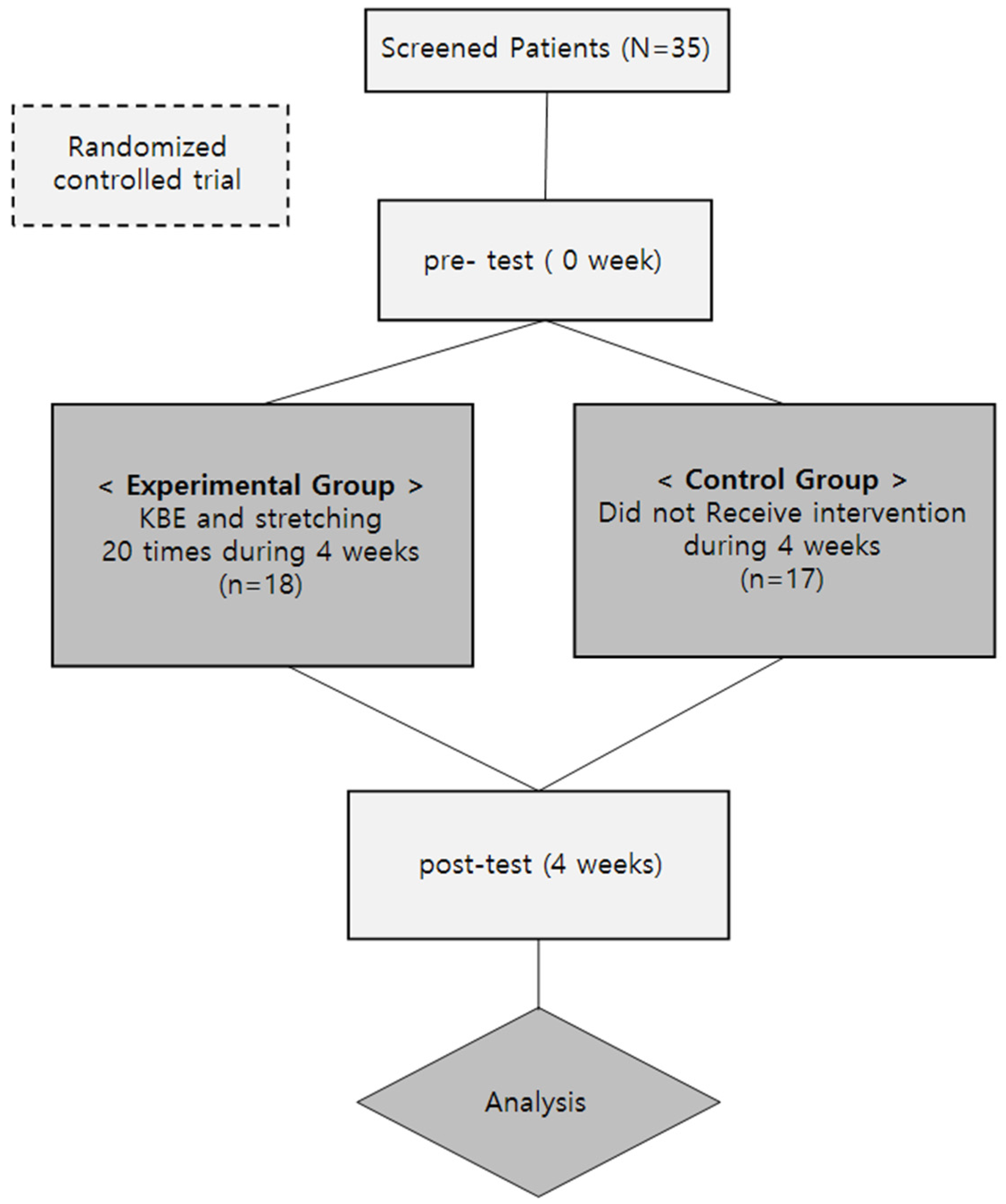
This study is an open randomized controlled trial. Participants (n=35) were randomly assigned to either a training group (T.G.) or a control group (C.G.) in a 1:1 ratio. Randomization was stratified by gender and performed using a block randomization method. It was classified by gender of the subjects and randomly assigned to experimental and control groups using block randomization. Randomization was performed via an Interactive Web Randomization System and maintained by a third party.
2.2. Participants
This study was conducted on 35 COVID-19-recovered patients, college students at S University in A city. All patients received prior consent before participating in the study. The inclusion criteria are as follows: (1) 19 to 30 years old; (2) A person who has been diagnosed with COVID-19 and has been completely cured through the release of quarantine; (3) ≥ six months after the onset of other acute diseases. Exclusion criteria were: (1) A person with moderate or severe heart disease; (2) A person with severe ischemic or hemorrhagic stroke or neurodegenerative disease; (3) a person with visual, auditory, or vestibular problems; (4) People who had other respiratory conditions..
2.3. Measurement Equipment
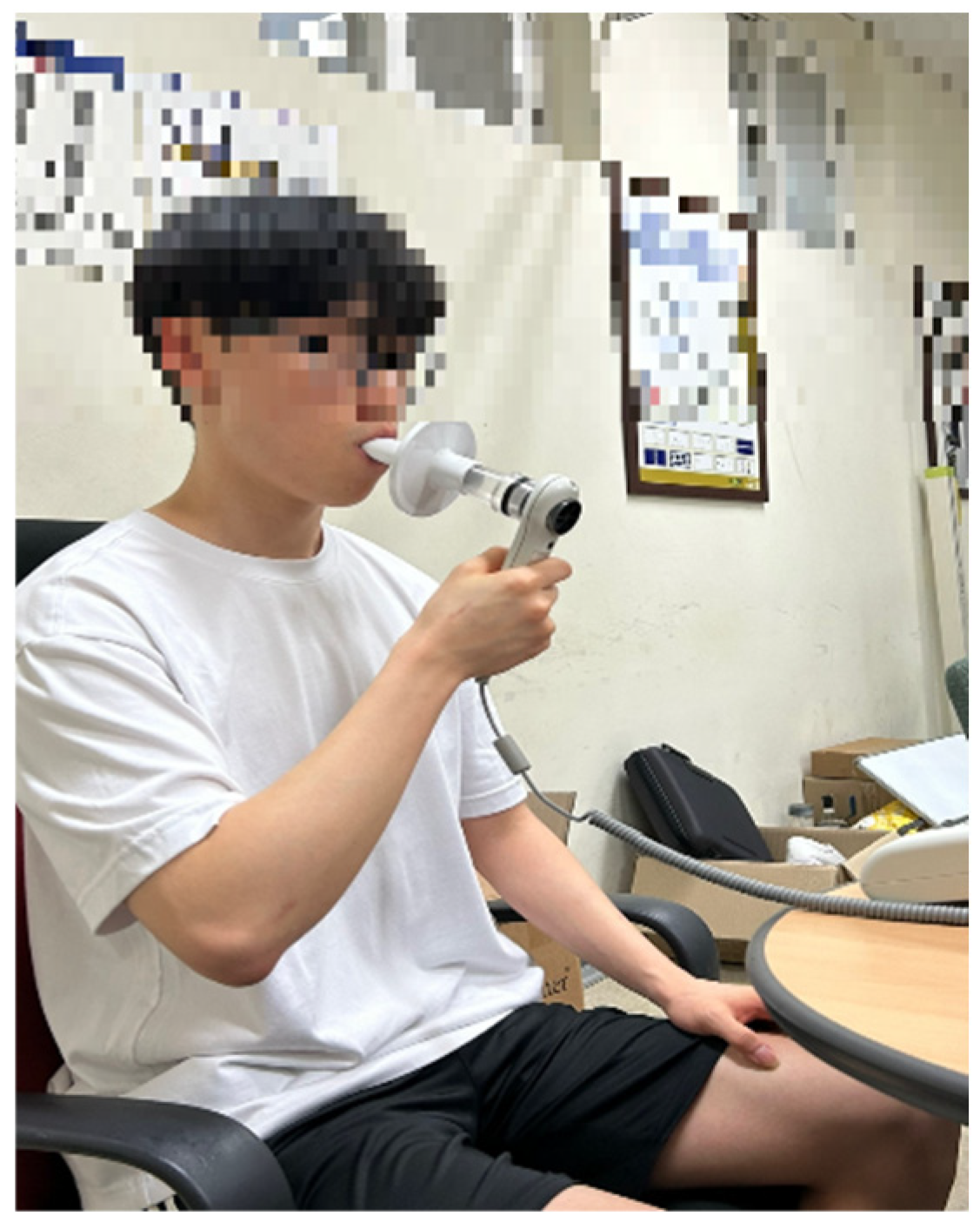
2.3.1. Measuring Lung Capacity (Pulmonary Functional)
By desktop spirometer (Model et al., COSMED, Italian) for assessing respiratory function. The following parameters related to respiratory function were measured: (1) Forced Expiratory Volume in 1 second (FEV1), (2) Forced Vital Capacity (FVC), (3) Forced Expiratory Volume in 1 second / Forced Vital Capacity (FEV1/FVC), (4) Peak Expiratory Flow (PEF) [
Figure 1].
2.3.2. Measuring Lung Capacity (Pulmonary Functional)
By desktop spirometer (Model et al., COSMED, Italian) for assessing respiratory function. The following parameters related to respiratory function were measured: (1) Forced Expiratory Volume in 1 second (FEV1), (2) Forced Vital Capacity (FVC), (3) Forced Expiratory Volume in 1 second / Forced Vital Capacity (FEV1/FVC), (4) Peak Expiratory Flow (PEF) [
Figure 1].
2.3.3. Measuring Fatigue (Fatigue Severity Scale)
Post-COVID-19 patient fatigue evaluation through an evaluation tool that quantified the perceived exertion. FFS is a 9-item scale that measures the severity of fatigue and its effect on a person’s activities and lifestyle in patients with various disorders. It was initially devised for people with Multiple Sclerosis (MS) or systemic lupus erythematosus. It includes nine items, each consisting of a statement for which respondents are asked to indicate their level of agreement from 1 (strongly disagree) to 7 (strongly agree). The Assessment of Two Groups before and after intervention was assessed using the FSS [
24,
25].
2.4. Experimental Procedures
They (T.G.) were trained in breathing exercise to do at home. It consisted of 2 sections: (1) Stretching exercise and (2) Kakao health care Breathing exercise. (Kakao et al.). (South Korea, Kakao). They performed breathing exercise at home for four weeks (10 min/day for four days/week). They were asked to practice these exercise separately at home during the experiment. To ensure that the subjects could follow the program correctly, an experimenter taught them the program until they could exercise on their own. They received a video clip of the exercise that can be opened and followed via smartphone. Also, through a kakao chat or phone call, they were reminded to follow the exercise routine four times a week. The experimental group recorded their progress after completing the exercise, and the experimenters checked the progress once a week. Among them, individuals who did not achieve at least 80% compliance with the exercise were excluded from the experiment. Measurements were conducted a total of two times, once before the start of the experiment and again after the 4-week intervention. Pre-tests were conducted within 24 hours before the first time of the experiment, and post-tests within 24 hours after the latest investigation [
Figure 2].
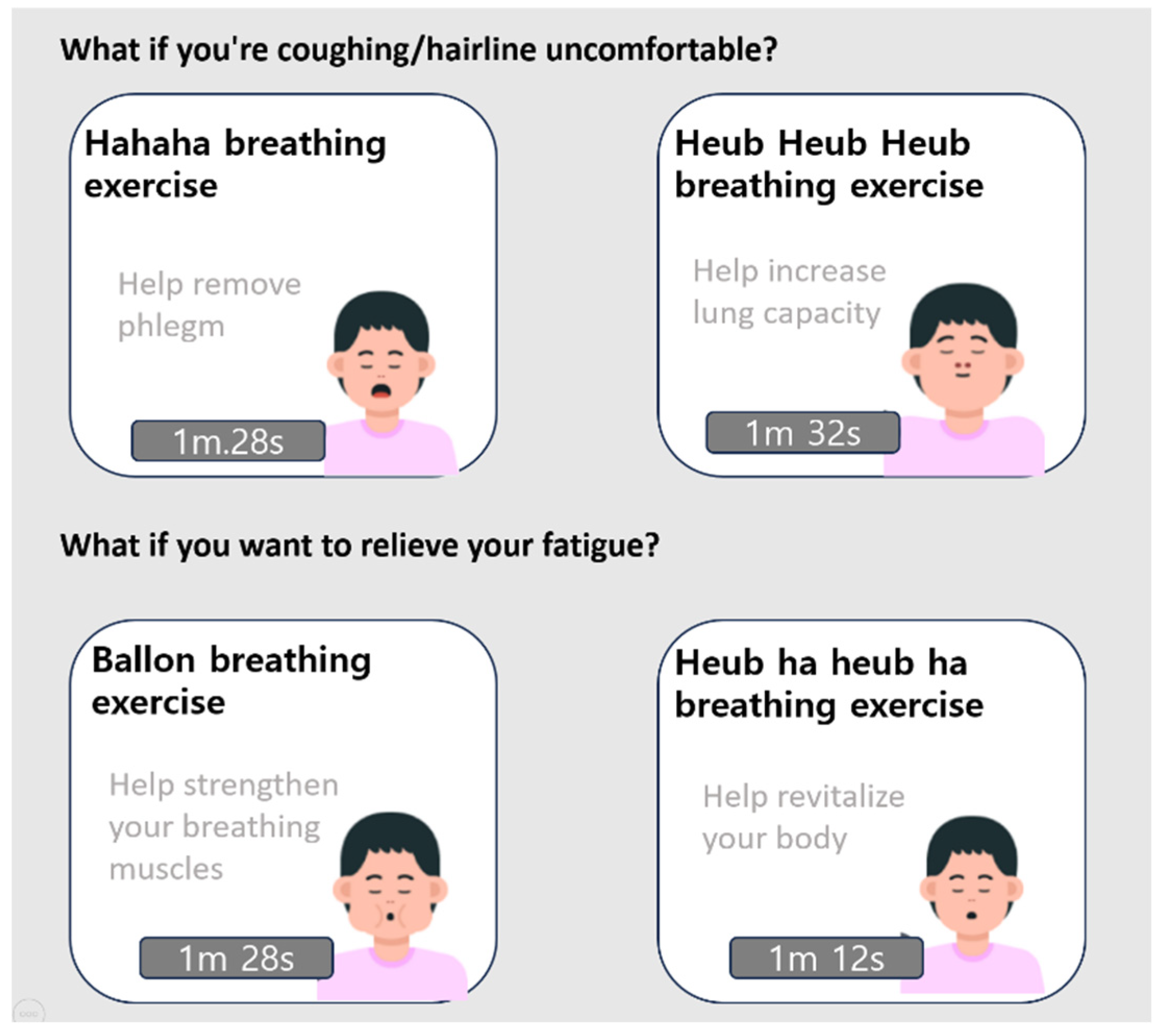
2.4.1. Application of Breathing Exercise
The “KBE” was developed to improve symptoms such as coughing, phlegm, and chronic fatigue, known as aftereffects, with mild breathing exercise under the slogan “COVID-19, let us rest satisfactorily and rest well”. It consists of four exercises: exercise to relieve coughing and phlegm and exercise to recover from fatigue. KBE referred to the guidelines on aftereffects of COVID-19 presented on the PASC Dashboard of the American Society of Rehabilitation Medicine. In addition, KBE shows exercise guide videos to make it easier to follow exercise. It guides you through exhalation, inspiration, and expansion time, and you can enjoy the process by listening to the sound of breathing together
The “balloon breathing exercise” is similar to “Pursed lips breathing”. Regular breathing is performed once at the beginning and end of the exercise. While following the breathing exercise video, you take a 3-second inhalation and a 1-second expansion, puffing out the cheeks as you exhale. This process is repeated four times, and the total duration is 1 minute and 28 seconds. Lip pursing breathing involves inhaling through the nose and exhaling through pursed lips, which helps reduce breathlessness, decrease respiratory rate, and minimize dynamic hyperinflation during exercise training with the aim of overall endurance improvement. Additionally, supplemental oxygen at 20% has been successfully used during exercise training to alleviate the respiratory muscle workload [
26,
27].
The “hahaha breathing exercise” technique helps with mucus clearance and is similar to the “huff cough” method. Normal breathing is performed once at the beginning and end of the exercise. While following the breathing exercise video, you inhale once and then exhale with a “ha~” sound three times. This process is repeated four times, and the total duration is 1 minute and 28 seconds. Using forced expiratory maneuvers like the huff cough can help propel secretions. Huff cough is performed as an open glottis maneuver that utilizes forced expiration, enabling the movement of mucus by dynamically compressing the same pressure points in the airway, thus increasing the linear velocity of the expiratory flow. When initiating forced expiration at lower lung volumes, the isobaric points move toward the periphery and smaller airways. Forced expiration at higher lung volumes, on the other hand, shifts the isobaric points centrally towards the larger central airways [
27].
The “heub heub heub breathing exercise” helps increase lung capacity. Regular breathing is performed once at the beginning and end of the exercise. While following the breathing exercise video, you inhale three times to make the “heub~” sound and then exhale. This process is repeated four times, and the total duration is 1 minute and 32 seconds.
The “heub ha heub ha breathing exercise” helps with physical activation. Regular breathing is performed once at the beginning and end of the exercise. While following the breathing exercise video, you inhale rapidly to make the “heub” sound and then exhale rapidly to make the “ha” sound, following the speed as provided in the instructional video. This process is repeated six times, and the total duration is 1 minute and 12 seconds [
Figure 3].
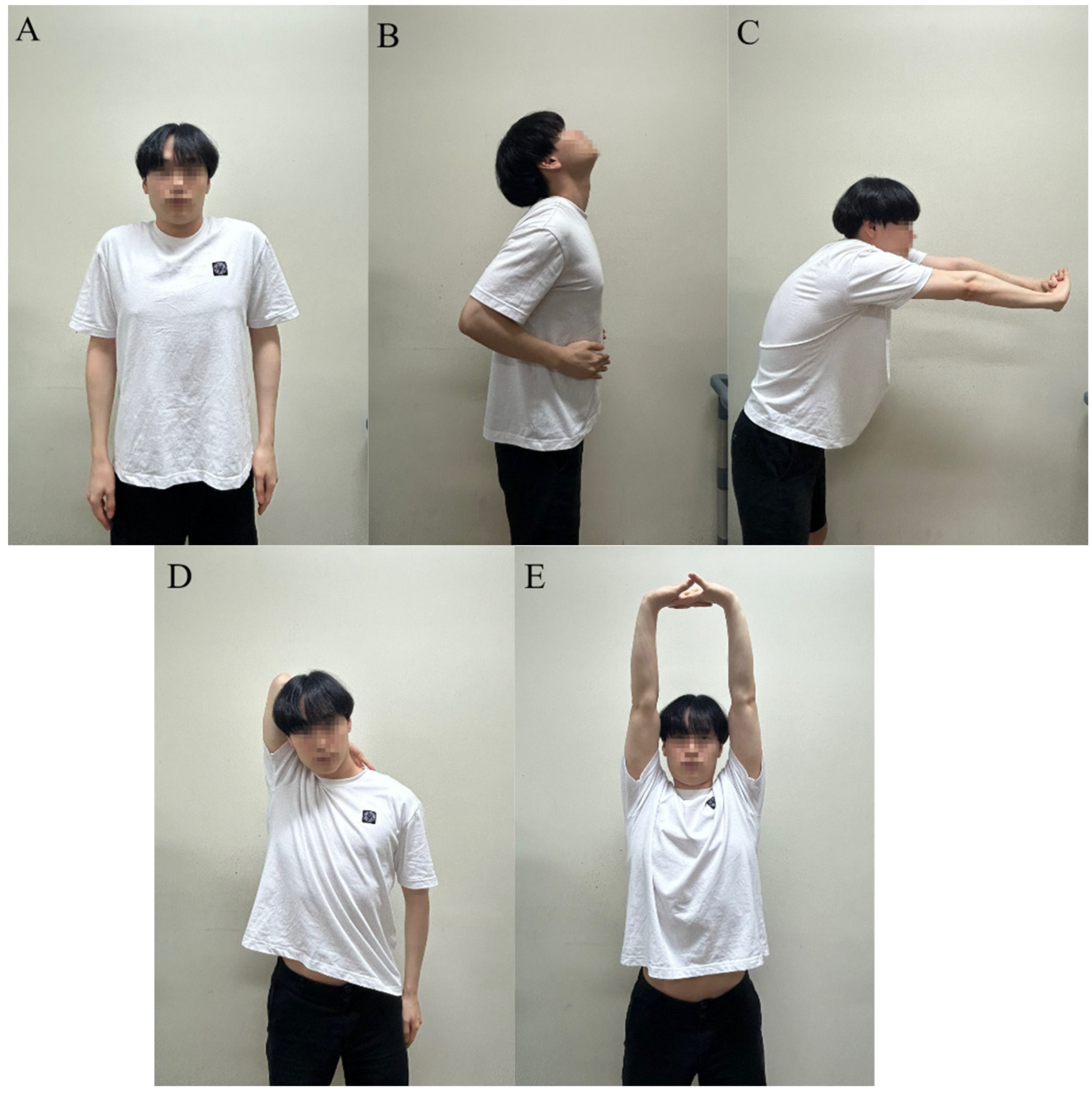
2.4.2. Stretching Exercise
Respiratory muscle stretching was done under the guidance of a rehabilitation therapist. RMSG consists of fo five sections [29].
Pattern 1: ‘Elevating and pulling back the shoulders’ As you gradually breathe in through your nose, slowly elevate and pull back both shoulders. After taking a deep breath, slowly breathe out through your mouth, relax, and lower your shoulders.
Pattern 2: ‘Stretching the upper chest’ Put both hands on your upper chest. Pull back your elbows and pull down your chest while lifting your chin and inhaling a deep breath through your nose. Expire slowly through your mouth and loosen up.
Pattern 3: ‘Stretching the back muscle’ Please hold your hand in front of your chest. When you inhale slowly through your nose, gently move your hands back and forth while stretching your back. After taking a deep inspiration, slowly breathe and return to your original position.
Pattern 4: ‘Stretching the lower chest.’ Hold the edges of the face towel with both hands extended to shoulder height. After taking a deep inspiration, slowly exhale and move your arms upward. After taking a deep breath, lower your hand and breathe normally.
Pattern 5: ‘Elevating the elbow’ Grip one hand behind your head. Take a deep breath through your nose. While gradually exhaling through your mouth, stretch your trunk by raising your elbow as tall as is easily possible. Return to the original position while breathing normally (
Figure 4).
A: Elevating and pulling back theshoulders; B: Stretching the upper chest; C: Stretching the backmuscle; D:Elevating the elbow Stretching; E: Stretching the lower chest.
2.5. Data Analysis
This statistic was performed with SPSS version 24.0. In this study, normality was verified through Shapiro Wilk verification for normality verification. The Chi-square test was used to compare the study groups for the categorical variables. The intragroup data were compared with the paired t-test. The intergroup comparison of the improvement (differences of pre–post values) between groups was evaluated with an independent sample t-test. The statistical significance level was set to the 95% confidence level.
Figure 5.
Research Procedure.
Figure 5.
Research Procedure.
3. Results
A total of 35 patients were assessed for eligibility. There were no statistically significant differences between the two groups of patients [
Table 1].
Inter-group analysis showed that the training group (T.G.) had significantly higher FEV1 (3.88 ± 1.13 vs 4.37 ± 1.00, p = 0.002), FEV1/FVC% (75.16 ± 10.71 vs 84.46 ± 6.45, p = 0.005), and PEF (7.74 ± 2.79 vs 8.92 ± 2.50, p = 0.003) compared to the control group (C.G.). There was no significant difference in FVC (5.08 ± 1.15 vs 5.16 ± 1.10, p = 0.181). The lung function parameters FVC (4.99 ± 0.95 vs 4.93 ± 0.99, P = 0.456), FEV1 (3.94 ± 0.88 vs 3.95 ± 0.92, P = 0.268), FEV1/FVC% (78.17 ± 9.28 vs 78.64 ± 9.34, P = 0.418), and PEF (7.12 ± 2.78 vs 7.64 ± 2.90, P = 0.067) in the C.G did not show any significant differences. The T.G. and the C.G. were compared after four weeks of respiratory rehabilitation in terms of lung function parameters. There was a statistically significant difference found between the two groups in FEV1 (0.491 ± 0.568 vs 0.124 ± 0.451, P = 0.010) and FEV1/FVC% (9.30 ± 12.189 vs 0.471 ± 9.227, P = 0.022). However, there was no statistically significant difference between FVC (0.083± 0.227 vs -0.055 ± 0.364, P = 0.181) and PEF (1.176 ± 1.462 vs 0.520 ± 1.359, P = 0.179) [
Table 2].
Fatigue There was no statistically significant difference found between the two groups. (P = 0.181). But, there was a statistically significant difference in the T.G group. Inter-group analysis revealed (P = 0.032), and C.G. showed no significant differences (P = 0.125) [
Table 3].
4. Discussion
This study focuses on the medical challenges faced by COVID-19 recovered patients with mild to moderate symptoms who were isolated and did not require hospitalization. Our findings suggest that home-based breathing exercises combined with stretching can significantly improve respiratory function, particularly FEV1 and FEV1/FVC%, but have limited effects on fatigue. These results are consistent with previous studies showing the benefits of respiratory rehabilitation in improving lung function.
Previous studies reported that lung function parameters, including FVC, FEV1, and FEV1/FVC (%), improved over time when compared between the experimental and C.G. However, no significant differences were found between the adjusted groups. In this study, similar improvements in lung function parameters, excluding FVC within the groups, were observed over time. However, significant differences were found between the groups regarding FEV1 and FEV1/FVC (%). A possible explanation could be related to the tendency for shorter tracking periods in clinical trials that have reported the most significant benefit of digital interventions, potentially resulting in decreased revenue as the usage period lengthens. There are various reasons for a decline in exercise adherence over time, but it is primarily confirmed that exercise motivation decreases as time passes [30]. Furthermore, unlike the exercise regimen that included only bracing exercises, as mentioned in the previous paper, the recent study incorporated exercises at a higher level of intensity, including lower limb muscle strength training and aerobic exercises. However, the post-COVID-19 rehabilitation program recommends conducting moderate-intensity exercises, prioritizing safety, instead of low-intensity exercises. Finally, it emphasizes that pulmonary rehabilitation programs can vary in effectiveness based on individual needs and functional impairments, which is relevant in this context [31,32].
According to a recent meta-analysis, it has been found that 32% (n=25,268) of post-COVID-19 individuals experience fatigue for more than 12 weeks after recovery [33]. Unlike other persistent symptoms such as dehydration, cough, and weakness, fatigue persists and worsens over time. The etiology of such fatigue remains unclear, but it is known to be complex and multifactorial in its mechanistic aspects. Clear immunological findings related to fatigue have not been observed in COVID-19 patients. Therefore, non-pharmacological interventions are recommended to treat fatigue in these patients [34]. This study’s fatigue severity scale significantly decreased only in the experimental group (P = 0.032). The between-group effect size showed a marginal reduction in fatigue severity after intervention (P = 0.125). A recent study reported a significant reduction in fatigue severity when breathing exercise accompanied by chest expansion and arm movements were conducted for six weeks. Despite the non-significant difference between the baseline and the 2-week mark, there was a significant difference between the baseline and 6-week measurements [35]. Through this study, it can be observed that four weeks of breathing exercise also have an effect on reducing fatigue severity.
The KBE in this study incorporates various breathing techniques, including respiratory control, pursed breathing, and diaphragmatic breathing. These deep breathing techniques can benefit anyone, but they play a particularly crucial role in the recovery process of individuals with COVID-19. These exercises can be done at home during self-isolation and easily incorporated into daily life. Deep breathing exercises have shown the potential to reduce anxiety and stress, commonly experienced by individuals who have had severe symptoms or have been hospitalized. These breathing exercises can help recover diaphragmatic function and enhance lung capacity. Our primary goal is to enhance the ability to practice deep breathing during rest and all activities [36]. Furthermore, pursed lip breathing involves inhaling through the nose and exhaling through pursed lips. This technique aims to reduce airway collapse, decrease the respiratory rate, and improve endurance during exercise training [
26]. Recent research has demonstrated that oxygen supplementation through pursed lip breathing can help reduce the workload on respiratory muscles during exercise training [37]. Finally, stretching techniques that included stretching the neck, upper chest, pectoral muscles, lateral chest, and mobilization of the posterior joints were found to increase lung compliance by up to 50 mL [38,39]. Our study showed a significant improvement in the T.G. (treatment group) after four weeks of respiratory rehabilitation training. These results may be attributed to including various respiratory muscles, including the diaphragm, intercostal, and abdominal muscles, in respiratory rehabilitation training. These muscles play a crucial role in maintaining respiratory function. Functional deficits in these muscles can lead to breathlessness, paradoxical breathing, increased extension of the chest muscles during respiration, and reduced chest wall movement during respiration. Slower breathing rates lead to reduced energy consumption, enhanced lung ventilation, and improved blood oxygenation levels. From a clinical perspective, although the results of this study may not have shown that home-based bracing exercise is more effective than standard rehabilitation therapy, it does suggest that home-based bracing exercise can be an effective intervention for improving respiratory parameters in patients with post-acute COVID-19. Furthermore, it is worth noting that older patients are more likely to choose inpatient rehabilitation. In comparison, younger patients are inclined towards outpatient rehabilitation due to its better compatibility with their home or work commitments. Especially for a significant portion of outpatient rehabilitation patients, it is crucial to establish personalized home-based rehabilitation plans or transition them to long-term rehabilitation phases at outpatient centers. This approach promotes physical activity and helps maintain a healthy lifestyle for these individuals [
20].
5. Conclusions
The 4-week home-based breathing exercise (KBE) and stretching program significantly improved pulmonary function (FEV1, FEV1/FVC%, PEF) in COVID-19 recovered patients, particularly in FEV1 and FEV1/FVC% when compared to the control group. However, no significant improvements in fatigue levels were observed. These findings suggest that home-based breathing exercises can be an effective intervention for improving lung function in COVID-19 patients.
6. Limitation
This study acknowledges the evidence for the effectiveness of home-based KBE and Stretching programs but recognizes several limitations that should be considered. Firstly, this study did not show significant improvements in pulmonary respiratory function (FEV, PEF, FVC) after the intervention, possibly due to the relatively short duration of the respiratory rehabilitation period. Secondly, this review could not provide adequate evidence for the effects of Breathing Exercise on severe lung injury patients (mild to moderate lung injury) and the long-term (>1 year) effects of Breathing Exercise in the following patients due to the included population. Thirdly, due to data limitations, the review could not evaluate the effects of Breathing Exercises on comorbidities after COVID-19. Therefore, caution is needed in interpreting and generalizing the results of this review. Fourthly, this study relied on participants’ self-discipline for exercise progress. Therefore, consideration should be given to whether the exercise intervention was effectively implemented. Fifth, as far as we know, there is no breathing exercise program like KBS. Therefore, there may be a need for more evidence for KBS. Finally, The wide variation in COVID-19 confirmation dates makes distinguishing between the acute and chronic phases challenging.
Author Contributions
Conceptualization, C.-H.J., M.-W.N. and Y.-G.N.; methodology, J.-H.H. and J.-S.K.; formal analysis, J.-H.Y. and S.-G.K.; investigation, C.-H.J. and M.-W.N.; writing—original draft preparation, C.-H.J.; writing—review and editing, C.-H.J., M.-W.N. and Y.-G.N.; supervision, Y.-G.N.; authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the Declaration of Helsinki and was approved by the Institutional Review Board of Sun Moon University (ID: SM-202309-025-3, Approval date: 21 Dec 2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study and written informed consent has been obtained from the participants to publish this paper.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2022R1C1C2007812).
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Wu, Y.; Chen, C.; Chan, Y. The outbreak of COVID-19: An overview. 2020, 83, 217-220.
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K. S.; Lau, E. H.; Wong, J. Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl.J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Cao, Q.; Hong, Z.; Tan, Y.; Chen, S.; Jin, H.; Tan, K.; Wang, D.; Yan, Y. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak–an update on the status. Mil. Med. Res. 2020, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Carfì, A.; Bernabei, R.; Landi, F. Persistent symptoms in patients after acute COVID-19. JMIR Nurs. 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Yong, S. J. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect. Dis. 2021, 53, 737–754. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-Las-Peñas, C.; Palacios-Ceña, D.; Gómez-Mayordomo, V.; Florencio, L. L.; Cuadrado, M. L.; Plaza-Manzano, G.; Navarro-Santana, M. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Eur. J. Intern. Med. 2021, 92, 55–70. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Pei, S.; Chen, B.; Song, Y.; Zhang, T.; Yang, W.; Shaman, J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science. 2020, 368, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Stringhini, S.; Wisniak, A.; Piumatti, G.; Azman, A. S.; Lauer, S. A.; Baysson, H.; De Ridder, D.; Petrovic, D.; Schrempft, S.; Marcus, K. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): A population-based study. Lancet 2020, 396, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, R. T.; Lynch, J. B.; Del Rio, C. Mild or moderate Covid-19. N. Engl.J. Med. 2020, 383, 1757–1766. [Google Scholar] [CrossRef]
- BMJ Opin. Covid-19 and fatigue—a game of snakes and ladders. Available online: https://blogs.bmj.com/bmj/2020/05/19/paul-garner-covid19-and-fatigue-a-game-of-snakes-and-ladders/ (accessed on 10 December 2020).
- Goërtz, Y.M.; Van Herck, M.; Delbressine, J. M.; Vaes, A. W.; Meys, R.; Machado, F. V.; Houben-Wilke, S.; Burtin, C.; Posthuma, R.; Franssen, F. M. Persistent symptoms 3 months after a SARS-CoV-2 infection: the post-COVID-19 syndrome? ERJ Open Res. 2020, 6. [Google Scholar] [CrossRef] [PubMed]
- Salem, A. M.; Al Khathlan, N.; Alharbi, A. F.; Alghamdi, T.; AlDuilej, S.; Alghamdi, M.; Alfudhaili, M.; Alsunni, A.; Yar, T.; Latif, R. The long-term impact of COVID-19 pneumonia on the pulmonary function of survivors. Int. J. Gen. Med. 2021, 3271–3280. [Google Scholar] [CrossRef]
- Soleimanifar M, Hazrati E. Pulmonary Rehabilitation and Physiotherapy Management of Respiratory Conditions in Patient with COVID-19: Narrative Review. Mil Caring Sci. 2020. 63-72.
- Kader, M.; Hossain, M. A.; Reddy, V.; Perera, N. K. P.; Rashid, M. Effects of short-term breathing exercises on respiratory recovery in patients with COVID-19: a quasi-experimental study. BMC Sports Sci. Med. Rehabil. 2022, 14, 60. [Google Scholar] [CrossRef] [PubMed]
- Kusumawardani, R. I.; Tinduh, D.; Poerwandari, D.; Marhana, I. A.; Melaniani, S. The effectiveness of incentive spirometry exercise on pulmonary function in COVID-19 survivors: a randomized controlled trial study. Bali Medical Journal. 2023, 12, 539–544. [Google Scholar] [CrossRef]
- Liu, K.; Zhang, W.; Yang, Y.; Zhang, J.; Li, Y.; Chen, Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement. Ther. Clin. Pract. 2020, 39, 101166. [Google Scholar] [CrossRef] [PubMed]
- Del Corral, T.; Fabero-Garrido, R.; Plaza-Manzano, G.; Fernández-de-Las-Peñas, C.; Navarro-Santana, M.; López-de-Uralde-Villanueva, I. Home-based respiratory muscle training on quality of life and exercise tolerance in long-term post-COVID-19: Randomized controlled trial. Ann. Phys. Rehabil. Med. 2023, 66, 101709. [Google Scholar] [CrossRef] [PubMed]
- Hanson, J.; Couch, D.; Yap, K. Mobile Health Apps That Help With COVID-19 Management: Scoping Review. JMIR Nurs. 2020, 3. [Google Scholar]
- Nopp, S.; Moik, F.; Klok, F. A.; Gattinger, D.; Petrovic, M.; Vonbank, K.; Koczulla, A. R.; Ay, C.; Zwick, R. H. Outpatient pulmonary rehabilitation in patients with long COVID improves exercise capacity, functional status, dyspnea, fatigue, and quality of life. Respiration. 2022, 101, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Peek, K.; Sanson-Fisher, R.; Mackenzie, L.; Carey, M. Interventions to aid patient adherence to physiotherapist prescribed self-management strategies: a systematic review. Physiotherapy. 2016, 102, 127–135. [Google Scholar] [CrossRef]
- Public Health England (PHE). Health Matters: Physical Activity-Prevention and Management of Long-Term Conditions. Available online: https://www.gov.uk/government/publications/health-matters-physical-activity/health-matters-physical-activityprevention-and-management-of-long-term-conditions (accessed on 20 March 2021).
- Jack, K.; McLean, S. M.; Moffett, J. K.; Gardiner, E. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man.Ther. 2010, 15, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Kim, T. Kakao in Korea: Increasingly Shaking the Market. Asian Case Res. J. 2016, 20, 55–88. [Google Scholar] [CrossRef]
- De Sire, A.; Moggio, L.; Marotta, N.; Agostini, F.; Tasselli, A.; Drago Ferrante, V.; Curci, C.; Calafiore, D.; Ferraro, F.; Bernetti, A. Impact of rehabilitation on fatigue in post-COVID-19 patients: a systematic review and meta-analysis. Appl. Sci. 2022, 12, 8593. [Google Scholar] [CrossRef]
- Shelgikar, A. V.; Chervin, R. D. Diagnostic Tools for Hypersomnias. Submitted. 2013.
- Lim, P. A.; Ng, Y. S.; Tay, B. K. Impact of a viral respiratory epidemic on the practice of medicine and rehabilitation: severe acute respiratory syndrome. Arch. Phys. Med. Rehabil. 2004, 85, 1365–1370. [Google Scholar] [CrossRef] [PubMed]
- Mayer, A. F.; Karloh, M.; Dos Santos, K.; de Araujo, C. L. P.; Gulart, A. A. Effects of acute use of pursed-lips breathing during exercise in patients with COPD: a systematic review and meta-analysis. Physiotherapy. 2018, 104, 9–17. [Google Scholar] [CrossRef] [PubMed]
- McIlwaine, M.; Bradley, J.; Elborn, J. S.; Moran, F. Personalising airway clearance in chronic lung disease. Eur. Respir. Rev. 2017, 26. [Google Scholar] [CrossRef] [PubMed]
- Ito, M.; Kakizaki, F.; Tsuzura, Y.; Yamada, M. Immediate effect of respiratory muscle stretch gymnastics and diaphragmatic breathing on respiratory pattern. Respiratory Muscle Conditioning Group. Intern. Med. 1999, 38, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Lang, S.; McLelland, C.; MacDonald, D.; Hamilton, D. F. Do digital interventions increase adherence to home exercise rehabilitation? A systematic review of randomised controlled trials. Arch. Physiother. 2022, 12, 24. [Google Scholar] [PubMed]
- Li, J.; Xia, W.; Zhan, C.; Liu, S.; Yin, Z.; Wang, J.; Chong, Y.; Zheng, C.; Fang, X.; Cheng, W.; et al. A telerehabilitation programme in post-discharge COVID-19 patients (TERECO): A randomised controlled trial. Thorax 2021. [CrossRef] [PubMed]
- Santus, P.; Tursi, F.; Croce, G.; Di Simone, C.; Frassanito, F.; Gaboardi, P.; Airoldi, A.; Pecis, M.; Negretto, G.; Radovanovic, D. Changes in quality of life and dyspnoea after hospitalization in COVID-19 patients discharged at home. Multidiscip. Respir. Med. 2020, 15, 713. [Google Scholar] [CrossRef] [PubMed]
- Ceban, F.; Ling, S.; Lui, L.M.W.; Lee, Y.; Gill, H.; Teopiz, K.M.; Rodrigues, N.B.; Subramaniapillai, M.; Di Vincenzo, J.D.; Cao, B.; et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav. Immun. 2022, 101, 93–135. [Google Scholar] [CrossRef] [PubMed]
- Hajibashi, A.; Sarrafzadeh, J.; Amiri, A.; Salehi, R.; Vasaghi-Gharamaleki, B. Effect of progressive muscle relaxation as an add-on to pulmonary telerehabilitation in discharged patients with COVID-19: A randomised controlled trial. Complement. Ther. Clin. Pract. 2023, 51, 101730. [Google Scholar] [CrossRef] [PubMed]
- Mazza, M.G.; Palladini, M.; Villa, G.; de Lorenzo, R.; Rovere Querini, P.; Benedetti, F. Prevalence, trajectory over time, and risk factor of post-COVID-19 fatigue. J. Psychiatr. Res. 2022, 155, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Johns Hopkins medicine. Coronavirus Recovery: Breathing Exercises. Retrieved from. Available online: https://www.hopkinsmedicine.org/health/conditions-and%20diseases/coronavirus/coronavirus%20recovery-breathing-exercises. (accessed on 11 May 2021).
- Lim, P. A.; Ng, Y. S.; Tay, B. K. Impact of a viral respiratory epidemic on the practice of medicine and rehabilitation: severe acute respiratory syndrome. Arch.Phys.Med.Rehabil. Arch Phys Med Rehabil, 2004, 85, 1365–1370. [Google Scholar] [CrossRef] [PubMed]
- Rattes, C.; Campos, S. L.; Morais, C.; Goncalves, T.; Sayao, L. B.; Galindo-Filho, V. C.; Parreira, V.; Aliverti, A.; de Andrade, A. D. Respiratory muscles stretching acutely increases expansion in hemiparetic chest wall. Physiol. Neurobiol. 2018, 254, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Wang, T. J.; Chau, B.; Lui, M.; Lam, G.; Lin, N.; Humbert, S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am. J. Phys. Med. Rehabil. 2020, 99, 769–774. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).