Introduction
Total hip arthroplasty is one of the most successful surgical interventions, generally reporting excellent outcomes and low complication rates [
1]. The evolution of modern cemented joint arthroplasty traces back to Charnley, who initiated the use of acrylic bone cement for securing femoral head prostheses within the femur in 1958 [
2]. Polymethyl methacrylate (PMMA) is a synthetic polymer commonly used in medical applications. PMMA bone cement possesses unique mechanical properties that make it an ideal material for the fixation of implants in orthopedic surgery [
3]. These properties include biomechanical stability, as PMMA cement quickly stabilizes the implant in bone tissue, providing immediate fixation and anchorage. It also improves load distribution on the contact surface between the implant and bone, reducing stress concentrations. PMMA cement fills and levels off the implant–bone interface, enhancing the fit and stability of the implant within the bone. Additionally, it stiffens the spongiosa around the implant, further improving the anchorage of the implant in the bone. PMMA cement is easy to apply during surgery, allowing for the efficient and effective fixation of implants. Furthermore, PMMA has been proven to be nontoxic and compatible with human tissue, ensuring biocompatibility and reducing the risk of adverse reactions [
3].
In 1970, Buchholz and Engelbrecht were the first to explore the potential of incorporating antibiotics into bone cement [
4]. The use of antibiotic-loaded bone cement (ALBC) as a local antibiotic delivery system in orthopedic surgery has yielded significant findings. ALBC achieves high local antibiotic concentrations at the implant–cement–bone interface, ensuring targeted effects and minimizing systemic burden, thus reducing adverse effects. It is effective in preventing prosthetic joint infections due to its broad-spectrum antimicrobial effect. Antibiotics are released following diffusion, sustaining their activity. Combination therapies, such as gentamicin with clindamycin, further enhance antimicrobial efficacy. PMMA bone cement serves as an effective local antibiotic delivery system that is crucial in preventing infections in orthopedic surgery [
3].
Although cemented hip arthroplasty remains largely standard in the treatment of medial femoral neck fractures in older individuals in traumatology [
5], the introduction of cementless arthroplasty, particularly with proximally anchoring straight stem prostheses, has experienced a significant surge [
6,
7]. The literature has shown that cementless and cemented stems exhibit good long-term outcomes in hip arthroplasty, with comparable survival rates [
8,
9]. However, the limits of cementless arthroplasty are evident, particularly in older patients, as shown by increased complications, especially periprosthetic fractures and infections. The German Hip Registry (EPRD) shows a divergence of 1% in terms of excess cumulative revision probability with follow-up times up to 7 years [
10].
To mitigate the elevated risk of periprosthetic fractures, the exploration of alternative prosthetic options is warranted. In this context, one measure recommended by the German EPRD advocates the utilization of cemented hip stems in elective procedures for patients over 75 years old [
10]. This recommendation is supported by the literature demonstrating a reduced risk associated with cemented stems compared to cementless hips in this age population [
11,
12,
13]. Research further suggests that the choice of stem design significantly influences periprosthetic fracture occurrence in total hip arthroplasty (THA), with short stems generally posing a lower risk than straight stems [
12,
14]. Although the adoption of cementless short stems has rapidly expanded in recent years [
15], cemented short stems remain comparatively less established within the orthopedic community. Given their limited availability and utilization, their conceptualization and adoption within the orthopedic field are notably nascent.
In our clinic, a tertiary care endoprosthesis center with approximately 500 hip arthroplasty procedures performed last year, the proportion of cemented hip arthroplasty procedures has steadily increased in recent years, reaching approximately 20%. This shift occurred after a period during which almost exclusively cementless short-stem endoprostheses were used in elective cases, while cemented standard stems were consistently used in trauma cases.
Since 2021, a calcar-guided cemented short-stem model (A2 stem, ARTIQO, Lüdinghausen, Germany) has been available in our clinic and utilized in both elective and trauma cases (the latter in combination with a bipolar head). Approximately 160 cemented short-stem prostheses have been implanted in our clinic since their introduction. Of these, 28 patients were recruited to participate in a larger prospective multicenter study, which included a total of 121 patients overall. This prospective study was designed to collect clinical and radiographic data on the A2 stem after up to 10 years of follow-up.
An interim analysis of internal clinical data, including EPRD manufacturer data, revealed that although the overall revision rates for primary hip arthroplasty are low, cemented standard stems exhibit slightly higher revision rates. This may be attributed, at least in part, to patient selection criteria favoring older patients and those with poorer bone quality. Interestingly, cemented short stems do not contribute to the revision rates associated with cemented standard stems in elective and trauma cases, suggesting potentially lower complication rates than expected.
The aim of the current study was to assess both the clinical outcomes and complications associated with the use of this cemented short-stem design.
Materials and Methods
This prospective study adhered to the principles of the Helsinki Declaration and obtained approval from the ethics committee of the Medical Association of Lower Saxony, Germany. The study did not restrict inclusion to specific indications within the intended use of the prosthesis. From September 2021 to April 2023, a total of 28 unilateral cemented THA procedures were conducted using an A2 stem (Artiqo GmbH, Lüdinghausen, Germany) and a cementless ANA.NOVA Alpha Cup (Implantec, Mödling, Austria). Different antibiotic-loaded cement types were used during this patient series, including Palacos® R+G (Heraeus Medical, Wehrheim, Germany) and Optipac® (ZimmerBiomet, Warsaw, IN, USA). The cohort consisted of 25 females and 3 males, with an average age of 80.6 ± 4.3 (range, 71.0–90.0) years and an average weight of 68.2 ± 10.5 (range, 48.0–90.0) kg. The indications for implantation were primary osteoarthritis (n = 27) and rheumatoid arthritis (n = 1).
The CE-marked cemented calcar-guided A2 stem (
Figure 1) was developed based on the design philosophy of the cementless A2 short stem. It is constructed from a stainless-steel implant compliant with ISO 5832-9 standards and features a smooth surface that allows for the use of bone cement. This stem is intended for use in trauma patients with displaced femoral neck fractures or in older individuals. Moreover, the cemented stem serves as an intraoperative backup solution in cases where the primary stability of the cementless version may be inadequate, such as instances of poor bone quality. The stem is available in nine sizes, ranging from 2 to The instrument set is universally applicable and remains identical for both the cemented and cementless versions.
All surgeries utilized a minimally invasive direct anterior approach [
16]. The stem can be implanted using either an “undersizing” cementing technique (where the stem is one size smaller than the rasp) or a “line-to-line” technique (where the stem and rasp are identical in size). In our clinic, all stems were implanted using the undersizing technique. Following cup implantation, the femoral canal was prepared, and trial reduction ensured an optimal range of motion, joint stability, and correct leg length. The cementation procedure was performed according to a contemporary technique described in the literature [
17]. In brief, a CEMSTOP® cement restrictor (Teknimed, Vic-en-Bigorre, France) was introduced into the femoral medullary canal. The cement restrictor was positioned 1 cm distal to the tip of the prosthesis. To prepare the bone bed, the femoral medullary canal was flushed with pulse lavage. The high-viscosity bone cement (PALACOS®, Heraeus Medical GmbH, Wehrheim, Germany) was mixed at room temperature using a vacuum system for approximately 30 seconds. Subsequently, at the beginning of minute 2, the cement was retrogradely introduced into the femoral canal using a cement gun with a pressure holder. The cement curing was observed for 12 minutes.
Following surgery, the patients were encouraged to bear weight fully on the operated leg from the first postoperative day, with physiotherapy initiated thereafter.
The demographic data, comorbidities, Harris Hip Score (HHS) [
18], and patient-administered HOOS-Physical Function Shortform (HOOS-PS) [
19] were assessed preoperatively and during follow-up, whereas the Forgotten Joint Score (FJS) [
20] was used during follow-up. Patient activity was determined using the UCLA Activity Scale (UCLA) [
21]. Radiographic evaluation included standing anterior–posterior and lateral radiographs of the proximal femur preoperatively, immediately postoperatively, and during follow-up, analyzing subsidence, osteolysis, and bone resorption using Gruen zones [
22]. Periarticular ossification was classified according to the Brooker classification [
23]. Leg length inequality was assessed radiographically and clinically. The rehabilitation protocol included immediate weight bearing.
Statistics
For continuous variables, the data were presented as mean ± standard deviation (SD); for categorical variables, the data were presented as counts.
Results
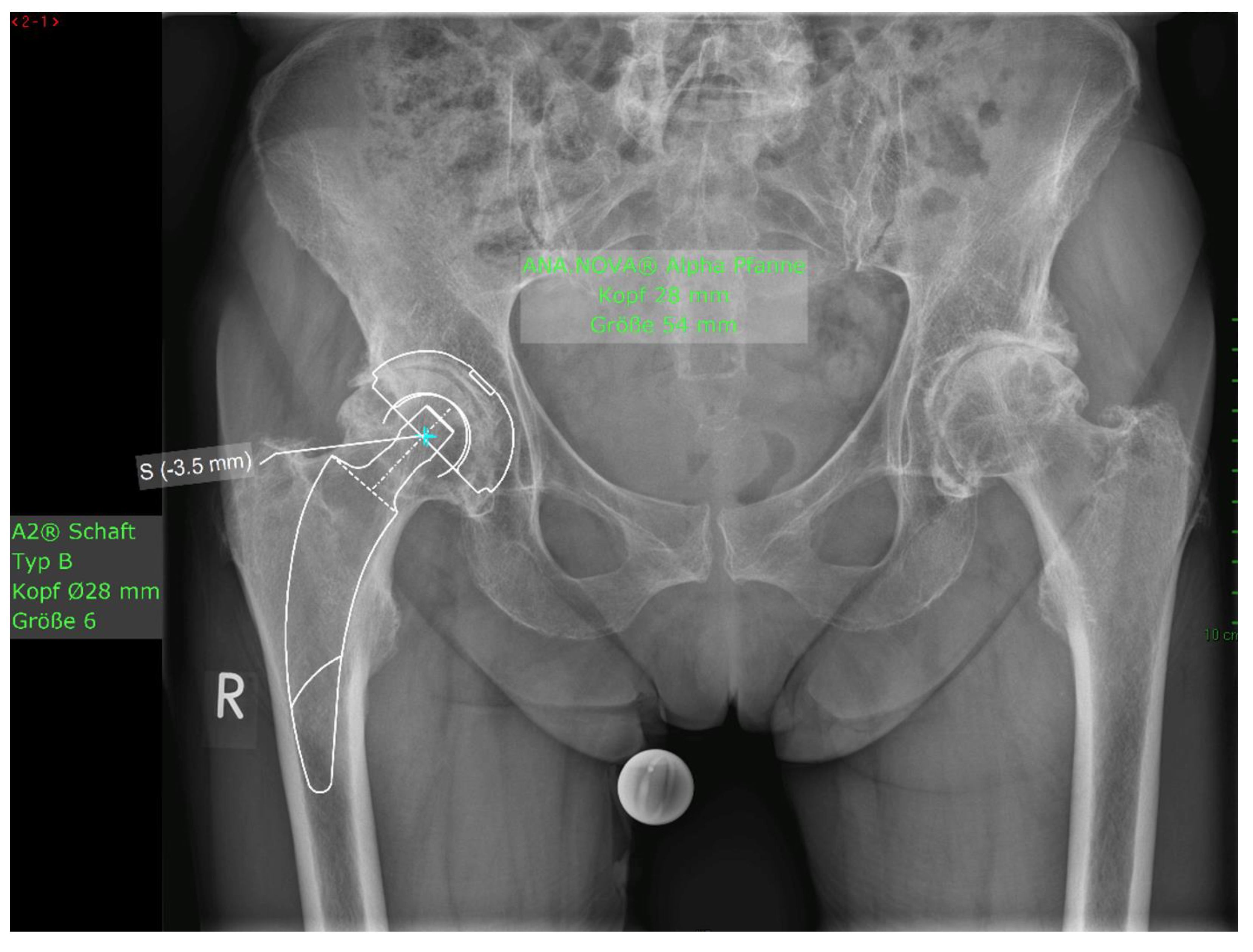
Of the 28 patients who underwent surgery, 5 withdrew their consent and 2 patients died due to unrelated causes. One prosthesis was explanted at 2 months postoperatively due to undersizing of the cement stopper, resulting in an inadequate cement mantle, which subsequently led to 14 mm of subsidence in the weeks following implantation. Hence, there were 20 patients with a 1-year follow-up. The mean HHS increased from 49.4 ± 13.9 preoperatively to 93.6 ± 6.9 at the final follow-up. No pain was reported by 19 patients at the final follow-up, with only occasional slight pain in one patient. The mean UCLA score increased from 3.5 ± 1.5 preoperatively to 5.1 ± 1.9 at the one-year follow-up. The mean HOOS-PS score increased from 44.2 ± 22.1 preoperatively to 60.0 ± 28.6 at the one-year follow-up. The FJS score was 68.3 ± 14.6 at the one-year follow-up. One patient experienced leg shortening of 10 mm. Periarticular ossification Brooker 1 was identified in three patients. One patient experienced axial subsidence of 2 mm. There were no postoperative infections. No radiolucent lines were observed, and none of the patients presented with osteolysis. A representative case is presented. Preoperative planning facilitated the achievement of anatomic restoration, as depicted in Figure
Figure 3 demonstrates the correct postoperative positioning of the femoral stem and a complete cement mantle.
Figure 2.
Figure Case #1 Female patient, 81 years old, with osteoporotic bone, coxa vara, and a Dorr C femur.
Figure 2a Preoperative planning for a cemented A2 stem combined with a cementless ANA.NOVA Alpha Cup. The image shows good reconstruction of the leg length and offset.
Figure 2b and
Figure 2c. Postoperative anteroposterior (2b) and axial (2c) radiographic imaging 1 week postoperatively. Correct position of the stem and complete cement mantle.
Figure 2.
Figure Case #1 Female patient, 81 years old, with osteoporotic bone, coxa vara, and a Dorr C femur.
Figure 2a Preoperative planning for a cemented A2 stem combined with a cementless ANA.NOVA Alpha Cup. The image shows good reconstruction of the leg length and offset.
Figure 2b and
Figure 2c. Postoperative anteroposterior (2b) and axial (2c) radiographic imaging 1 week postoperatively. Correct position of the stem and complete cement mantle.
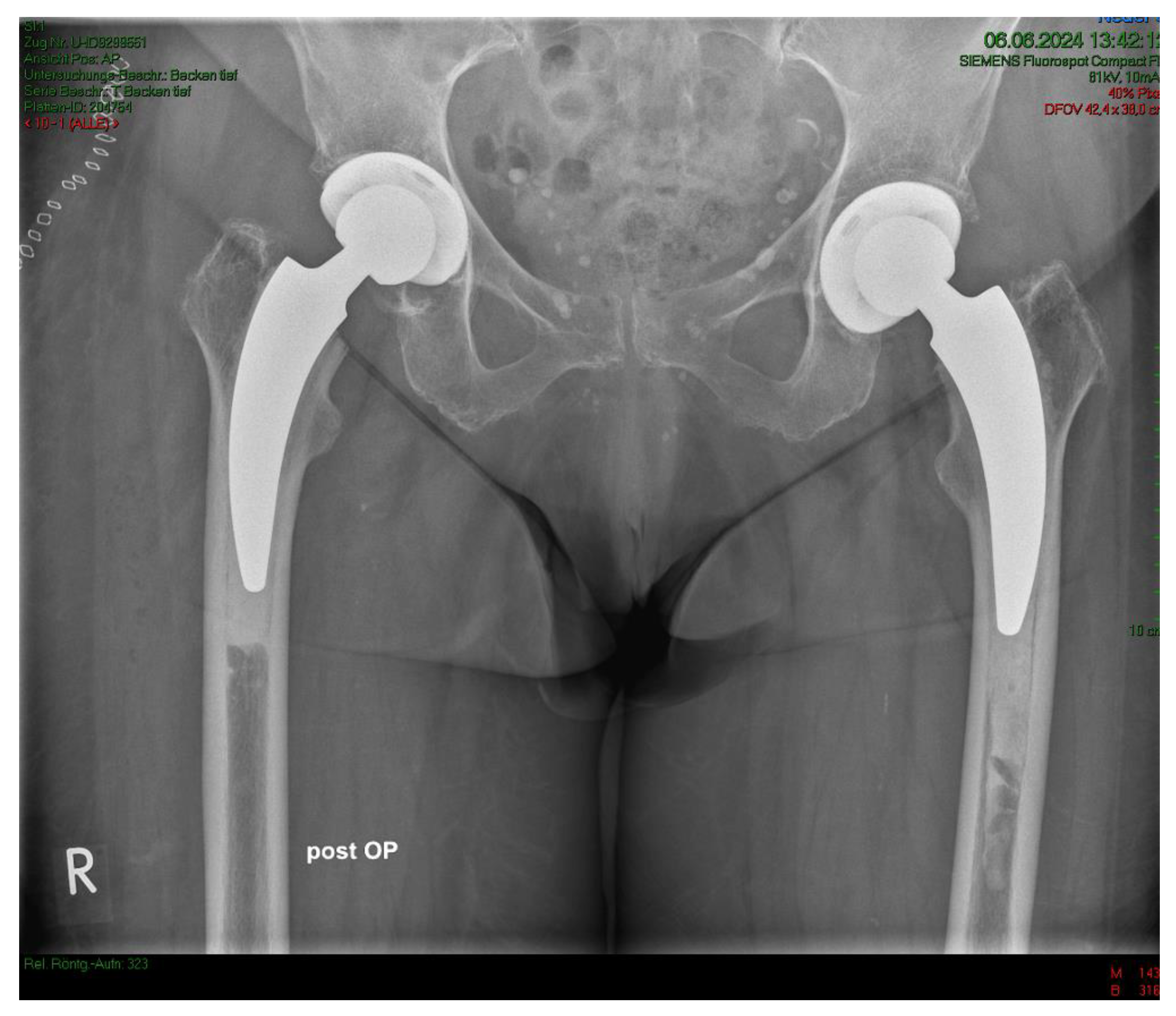
Figure 3.
a Case #2 Osteoarthritis, female, 85 years old, bilateral sequential implantation of an A2 stem, Dorr B-C femora.
Figure 3.
a Case #2 Osteoarthritis, female, 85 years old, bilateral sequential implantation of an A2 stem, Dorr B-C femora.
Figure 3.
b Left side: slight distalization of the cement stopper.
Figure 3.
b Left side: slight distalization of the cement stopper.
Figure 3.
c Right side: no positional change of the cement stopper during the operation.
Figure 3.
c Right side: no positional change of the cement stopper during the operation.
Figure 4.
a Case #3 Osteoarthritis, female, 81 years old, preoperative planning.
Figure 4.
a Case #3 Osteoarthritis, female, 81 years old, preoperative planning.
Figure 4.
b Correct positioning 1 week postoperatively. Homogeneous cement mantle. Correct implant position.
Figure 4.
b Correct positioning 1 week postoperatively. Homogeneous cement mantle. Correct implant position.
Discussion
Calcar-guided short-stem total hip arthroplasty is rapidly advancing in hip reconstruction, combining the benefits of short-stem implants with a minimally invasive surgical technique. Cementless calcar-guided stems have been shown to offer stem stability, preserve bone stock, and optimize the anatomical reconstruction of offset, antetorsion, and the antetilt of the femoral neck [
15,
24,
25].
Although various studies have reported good outcomes using the uncemented version of the A2 short-stem femoral implant [
15,
25], this series represents the first reported utilization of the cemented femoral variant. This study found that primary THA using a short calcar-guided cemented stem achieved favorable short-term results in elderly patients.
Given the increasingly aging population in Western industrialized nations, coupled with the high demand of this elderly population for maintaining or regaining mobility into advanced age, as well as age-related high morbidity and reduced immune competence, the question of whether cemented THA offers any advantages in geriatric patients arises. In the elderly, the risk of periprosthetic femoral fracture with cementless total hip arthroplasty, especially in Dorr C femora [
26], increases due to deteriorating bone quality [
27]. Moreover, the risk of infection increases with advancing age and multimorbidity. Significantly reduced infection rates by approximately 30% with cementless short-stem prostheses compared with standard stem prostheses have been reported [
15]. By using a cemented short-stem prosthesis, an additional layer of protection against infection may be added. In hip arthroplasty, the use of ALBC has been shown to contribute significantly to infection reduction [
28]. When implants are introduced, there is a risk of biofilm formation on the implant surface, which can lead to chronic infections [
29]. Systemic antibiotics may not effectively prevent colonization of the implant. However, locally released antibiotics can provide high concentrations at the implant site, protecting the foreign material from microbial contamination. PMMA bone cement is commonly used as a carrier for local antibiotic therapy. A meta-analysis conducted in the United States demonstrated that the application of ALBC can reduce infection rates by approximately 50% in primary hip arthroplasty [
28]. Individual patient considerations should guide treatment decisions, but the use of ALBC remains an essential measure to mitigate infections associated with implants [
29].
From a biomechanical perspective, employing a short cemented stem is feasible, although it requires a flawless bone cement interface attainable through modern cementation methods. In their biomechanical study on osteoporotic bone, Azari et al. demonstrated that the line-to-line technique and the undersized technique are equivalent and that both techniques are suitable for calcar-guided short stems [
30]. The authors concluded that regardless of the specific cementation technique, cemented short stems appear promising in patients with low bone quality [
30].
Cemented calcar-guided short-stem THA offers conceptual advantages over standard cemented THA. By virtue of its reduced dimensions compared to standard THA, short-stem designs necessitate a reduced insertion force. This enables the introduction of bone cement at a stage characterized by higher viscosity, thereby guaranteeing secure fixation of the implant within the medullary cavity. In comparison to standard THA, in cemented short-stem THA, the cement volume is lower and the bony surface that comes in contact with the cement involves cancellous metaphyseal bone rather than dense diaphyseal cortical bone. These differences result in lower intraosseous pressures due to the enhanced permeability of the cement into the metaphyseal spongy bone. In our own biomechanical study, we observed that the use of an A2-cemented short stem compared with a cemented straight stem resulted in a reduction in intramedullary pressure [
31]. Although high intramedullary pressure per se is an important factor in the genesis of bone cement implantation syndrome, the extent of embolization is proportional to the intramedullary pressure [
32].
The limitations of the current study include its relatively small sample size and lack of statistical power to adequately detect and assess perioperative complications. Additionally, the follow-up period was relatively short, potentially limiting the ability to assess the long-term outcomes and complications associated with the cemented short-stem design. Furthermore, the absence of a control group hinders the ability to directly compare outcomes with alternative treatment modalities or standard practices, thereby limiting the interpretability of the results in the context of broader clinical practice.
In summary, our short-term experience with this particular cemented short stem with ALBC is promising, demonstrating excellent functional outcomes, no infections, and no aseptic loosening attributable to the stem design. This series highlights the critical role of modern cementing techniques, including jet lavage and cement pressurization, alongside proper cement stopper utilization, in achieving successful outcomes in THA. Leveraging preliminary data from ongoing in vitro studies suggesting reduced periprosthetic complications associated with ALBC fixation in short-stem THA, these implant designs warrant further investigation as a potential solution for the elderly population undergoing THA. However, further studies, including larger cohorts and registry data, are needed to confirm these assertions and determine their clinical relevance.
Author Contributions
Conceptualization, B.R., M.W., and A.Y.; methodology, B.R.; formal analysis, B.R. and G.W.; investigation, B.R. and G.W.; data curation, B.R. and G.W.; writing—original draft preparation, B.R.; writing—review and editing, B.R., M.W., G.W., and A.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are not publicly available for privacy reasons.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Charnley, J. Acrylic cement in orthopaedic surgery. Brit J Surg 1970, 57, 874. [Google Scholar]
- Kühn, B.M.; Lieb, E.; Berberich, C. PMMA bone cement: what is the role of local antibiotics.
- Buchholz, H.W.; Engelbrecht, H. [Depot effects of various antibiotics mixed with Palacos resins]. Chirurg 1970, 41, 511–515. [Google Scholar] [PubMed]
- Szymski, D.; Walter, N.; Krull, P.; Melsheimer, O.; Grimberg, A.; Alt, V.; Steinbrück, A.; Rupp, M. Aseptic revisions and pulmonary embolism after surgical treatment of femoral neck fractures with cemented and cementless hemiarthroplasty in Germany: an analysis from the German Arthroplasty Registry (EPRD). J Orthop Traumatol 2023, 24, 9. [Google Scholar] [CrossRef] [PubMed]
- Meißner, N.; Halder, A.M.; Schrednitzki, D. Cemented and hybrid total hip arthroplasty lead to lower blood loss in primary total hip arthroplasty: a retrospective study. Arch Orthop Trauma Surg 2023, 143, 6447–6451. [Google Scholar] [CrossRef] [PubMed]
- Klug, A.; Gramlich, Y.; Hoffmann, R.; Pfeil, J.; Drees, P.; Kutzner, K.P. Trends in Total Hip Arthroplasty in Germany from 2007 to 2016: What Has Changed and Where Are We Now? Z Orthop Unfall 2021, 159, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Staats, K.P.; Vertesich, K.; Sigmund, I.K.; Böhler, C.; Windhager, R.; Kolb, A. Thirty-Year Minimum Follow-Up Outcome of a Straight Cementless Rectangular Stem. J Arthroplasty 2024, 39, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Thalody, H.S.; Post, Z.D.; Lutz, R.W.; Czymek, M.; Ong, A.C.; Ponzio, D.Y. Primary Cementless Femoral Stems in Conversion Hip Arthroplasty After Failed Fixation of Intertrochanteric Fractures. Orthopedics 2024, 47, e6–e12. [Google Scholar] [CrossRef] [PubMed]
- Grimberg, A.; Lutzner, J.; Melsheimer, O.; Morlock, M.; Steinbruck, A. Annual Report The German Arthroplasty Registry (EPRD). 2024. [Google Scholar]
- Li, M.; Zeng, Y.; Nie, Y.; Liao, K.; Pei, F.; Yang, J.; Xie, H.; Shen, B. A high risk of postoperative periprosthetic femoral fracture in Dorr type C femurs: a retrospective cohort study with 10-year follow-up data and a preliminary monochromatic image analysis. Int J Surg 2024, 110, 296–305. [Google Scholar] [CrossRef]
- Calkins, T.E.; Goetz, D.D.; Zalewski, J.T.; Jones, C.A.; Gaumer, P.R.; Ford, M.C.; Toy, P.C.; Crockarell, J.R.; Harkess, J.W.; Mihalko, W.M.; Guyton, J.L. Hip arthroplasty femoral stem designs and their association with early postoperative periprosthetic femoral fractures. J Arthroplasty 2023, 38, 849–854. [Google Scholar] [CrossRef]
- Kheir, M.M.; Dilley, J.E.; Speybroeck, J.; Kuyl, E.V.; Ochenjele, G.; McLawhorn, A.S.; Meneghini, R.M. The influence of Dorr type and femoral fixation on outcomes following total hip arthroplasty for acute femoral neck fractures: a multicenter study. J Arthroplasty 2023, 38, 719–725. [Google Scholar] [CrossRef]
- Luger, M.; Feldler, S.; Pisecky, L.; Klasan, A.; Gotterbarm, T.; Schopper, C. Periprosthetic femoral fractures in cementless short versus straight stem total hip arthroplasty: a propensity score matched analysis. J Arthroplasty 2023, 38, 751–756. [Google Scholar] [CrossRef]
- Steinbrück, A.; Grimberg, A.W.; Elliott, J.; Melsheimer, O.; Jansson, V. () Short versus conventional stem in cementless total hip arthroplasty : An evidence-based approach with registry data of mid-term survival. Orthopade 2021, 50, 296–305. [Google Scholar] [CrossRef] [PubMed]
- De Geest, T.; Fennema, P.; Lenaerts, G.; De Loore, G. Adverse effects associated with the direct anterior approach for total hip arthroplasty: a Bayesian meta-analysis. Arch Orthop Trauma Surg 2015, 135, 1183–1192. [Google Scholar] [CrossRef]
- Cassar-Gheiti, A.J.; McColgan, R.; Kelly, M.; Cassar-Gheiti, T.M.; Kenny, P.; Murphy, C.G. Current concepts and outcomes in cemented femoral stem design and cementation techniques: the argument for a new classification system. EFORT Open Rev 2020, 5, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg 1969, 51-A, 737–755. [Google Scholar]
- Davis, A.M.; Perruccio, A.V.; Canizares, M.; Tennant, A.; Hawker, G.A.; Conaghan, P.G.; Roos, E.M.; Jordan, J.M.; Maillefert, J.F.; Dougados, M.; Lohmander, L.S. The development of a short measure of physical function for hip OA HOOS-Physical Function Shortform (HOOS-PS): an OARSI/OMERACT initiative. Osteoarthritis Cartilage 2008, 16, 551–559. [Google Scholar] [CrossRef]
- Behrend, H.; Giesinger, K.; Giesinger, J.M.; Kuster, M.S. The "forgotten joint" as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 2012, 27, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Zahiri, C.A.; Schmalzried, T.P.; Szuszczewicz, E.S.; Amstutz, H.C. Assessing activity in joint replacement patients. J Arthroplasty 1998, 13, 890–895. [Google Scholar] [CrossRef]
- Gruen, T.; McNeice, G.; Amstutz, H. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 1979, 141, 17–27. [Google Scholar] [CrossRef]
- Brooker, A.; Bowerman, J.; Robinson, R.; Riley, L.J. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg (Am) 1973, 55, 1629–1632. [Google Scholar] [CrossRef]
- Ezechieli, M.; Windhagen, H.; Matsubara, M.; Budde, S.; Wirries, N.; Sungu, M. A neck-preserving short stem better reconstructs the centre of rotation than straight stems: a computed tomography-based cadaver study. Arch Orthop Trauma Surg 2022, 142, 1669–1680. [Google Scholar] [CrossRef]
- Budde, S.; Derksen, A.; Hurschler, C.; Fennema, P.; Windhagen, H.; Plagge, J.; Flörkemeier, T.; von Lewinski, G.; Noll, Y.; Schwarze, M. Very early migration of a calcar-guided short stem: a randomized study of early mobilization and the influence of a calcium phosphate coating with 60 patients. Sci Rep 2024, 14, 3837. [Google Scholar] [CrossRef]
- Bigart, K.C.; Nahhas, C.R.; Ruzich, G.P.; Culvern, C.N.; Salzano, M.B.; Della Valle, C.J.; Nam, D. Does Femoral Morphology Predict the Risk of Periprosthetic Fracture After Cementless Total Hip Arthroplasty? J Arthroplasty 2020, 35, S359–s363. [Google Scholar] [CrossRef]
- Konow, T.; Baetz, J.; Melsheimer, O.; Grimberg, A.; Morlock, M. Factors influencing periprosthetic femoral fracture risk. Bone Joint J, 2021; 103-b, 650–658. [Google Scholar]
- Parvizi, J.; Saleh, K.J.; Ragland, P.S.; Pour, A.E.; Mont, M.A. Efficacy of antibiotic-impregnated cement in total hip replacement. Acta Orthop 2008, 79, 335–341. [Google Scholar] [CrossRef]
- Kühn, K.D.; Renz, N.; Trampuz, A. [Local antibiotic therapy]. Unfallchirurg 2017, 120, 561–572. [Google Scholar] [CrossRef]
- Azari, F.; Sas, A.; Kutzner, K.P.; Klockow, A.; Scheerlinck, T.; van Lenthe, G.H. Cemented short-stem total hip arthroplasty: Characteristics of line-to-line versus undersized cementing techniques using a validated CT-based finite element analysis. J Orthop Res 2021, 39, 1681–1690. [Google Scholar] [CrossRef] [PubMed]
- Yaseen, A.; Regenbrecht, B. Der femorale intraossäre Druck in der zementierten Hüfttotalendoprothese. Paper presented at the Endoprothesenkongress Berlin, 8-10.2.2024, Berlin 2024. [Google Scholar]
- Donaldson, A.J.; Thomson, H.E.; Harper, N.J.; Kenny, N.W. Bone cement implantation syndrome. Br J Anaesth 2009, 102, 12–22. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).