1. Introduction
The majority of lung cancer cases, the neoplasm with the highest mortality rate, are only diagnosed in advanced stages of the disease. The main histopathological category is non-small cell lung cancer (NSCLC; 85% of cases), which, in turn, includes: adenocarcinomas (AdC), squamous cell carcinomas (SCC), and large cell carcinomas (LCC) [
1]. Common factors such as smoking, comorbidities, histopathological diagnosis (histological type, molecular mutations, positive tumor immunostaining) correlate with the aggressiveness of the disease, prognosis, survival, and treatment response [
2]. The most frequent mutant genes are p53, Kirsten rat sarcoma viral oncogene (KRAS), epidermal growth factor receptor (EGFR), mesenchymal-epithelial transition factor (MET) [
3], and anaplastic lymphoma kinase (ALK) [
1,
2]. Systemic inflammation amplification correlates with an unfavorable prognosis in neoplastic patients. C Reactive Protein (CRP) can directly interact with components of the extracellular matrix (fibroblasts) [
4], which represent constituents of the tumor stroma [
5,
6,
7,
8].
An elevated value of the neutrophil-lymphocyte ratio (NLR) is associated with increased peritumoral macrophage infiltration and increased values of other biomarkers, such as IL1, IL7, IL8, or IL17 [
4]. The systemic inflammatory response is associated with changes in neutrophil values (neutrophilia) and relative lymphocytopenia [
9]. Hematological tests are routinely performed for cancer patients in a variety of clinical scenarios and represent an easily measurable objective parameter capable of expressing the severity of the systemic inflammatory response in neoplastic patients [
10]. NLR may represent the balance between pro-tumoral inflammatory status and anti-tumoral immune response [
10]. Increased inflammatory biomarkers have been shown to be associated with an unfavorable prognosis in both neoplastic diseases and infectious diseases, such as pulmonary tuberculosis, bronchiectasis [
11] , or SARS-Cov-2 infection [
12]. The connection between inflammation and carcinogenesis supports the fact that determining inflammatory biomarkers, along with the lymphocyte/neutrophil ratio or platelets/lymphocyte ratio, could represent new directions for estimating the evolution and prognosis of neoplastic diseases [
13].
2. Materials and Methods
A retrospective study of patients with lung cancer was conducted at the Clinical County Hospital Mureș, Târgu Mureș. The patients were hospitalised between February 1st 2023 to December 31st 2023.
This human study was performed in accordance with the Declaration of Helsinki and it was approved by the ethics committee of Clinical County Hospital Mureș - approval: 6089/28.05.2024. All adult participants provided written informed consent to participate in this study.
Patients with a histopathologically confirmed diagnosis of lung cancer following endobronchial biopsy during the period of February 1st to December 31th 2023 were included in the lung cancer patient group. The control group consisted of patients admitted to the Pulmonology Clinic of the same hospital during the same period analyzed (February 1th to December 31th 2023), with non-neoplastic diagnoses. The hospital admission period was similar in order to have statistical compatibility between the two analyzed groups.
The analysis of the data presented in this study is part of a larger ongoing research and constitutes the INOLUNG Study (innovation, lung).
Inclusion criteria for patients in the lung cancer group: 1) patients with histopathological confirmation of lung cancer; 2) patients over 18 years of age; 3) patients for whom the analyzed variables were available. Exclusion criteria for the lung cancer patient group: 1) patients with clinical or imaging suspicion of lung cancer but without histopathological confirmation; 2) patients under 18 years of age; 3) patients for whom the analyzed variables were not available.
Inclusion criteria for patients in the control group: patients hospitalized for continuous hospitalization in the Pulmonology Clinic of the Clinical County Hospital Mureș during the period of February 1th to December 31th 2023. Exclusion criteria for patients in the control group: 1) patients hospitalized in the Pulmonology Clinic at a time other than February 1th to December 31th 2023; 2) patients hospitalized with suspicion of lung cancer; 3) patients hospitalized with a diagnosis of pulmonary tuberculosis or SarsCov2 infection.
The analyzed parameters included: histopathological type (NSCLC - squamous cell carcinoma or adenocarcinoma; SCLC), molecular mutations (EGFR, ALK, PD-L1), parameters from the complete blood count (hemoglobin level, leukocyte count, platelet count, NLR, PLR, lymphocyte count), inflammatory markers (C-reactive protein), associated comorbidities, disease stage.
Statistical Analysis
Raw data were collected retrospectively from medical records and centralized în Microsoft Excel spreadsheets. Statistical analysis was performed in R statistical environment (version 4.3.3, released in Feb 29th 2024). Continuous variables were checked for gaussian distribution using the Shapiro-Wilk test. Comparisons between groups regarding numerical variables were performed using Wilcoxon’s or Kruskal-Wallis’ rank sum tests. Categorical variables were compared using Fisher's Exact Test for count data. Prior to fitting multiple logistic regression models, we performed an analysis of missing data followed by multiple imputation via chained equations. Throughout the study, a statistical significance threshold of 0.05 was used.
3. Results
In concordance with the inclusion and exclusion criteria, we included data from 380 patients: 115 in the cancer group and 265 in the control group. The characteristics of the participants are summarized in
Table 1.
Among patients in the lung cancer group, 88 were diagnosed with NSCLC (44 adenocarcinomas, 44 squamous cell carcinomas) and 27 with SCLC. The presence of mutations was assessed for EGFR, ALK, and PD-L1 genes in 68 patients with NSCLC. Molecular analysis for PD-L1 failed in one patient, due to insufficient sample quantity. EGFR mutations were detected in 7 patients (10.3% of the 68 tested), whereas ALK and PD-L1 mutations were identified in 1 (1.5%) and 25 (37.3%) patients, respectively. EGFR mutations involved exon 18 in one case (1.5%), exon 19 in two cases (2.9%), exon 20 in one (1.5%), and exon 21 in three cases (4.4%).
We did not observe differences in terms of age or gender distribution between patients with or without EGFR mutations. However, regarding the histological type of the tumor, adenocarcinomas were more frequent than squamos cell carcinomas in patients with EGFR mutations (85.7% vs. 14.3%, p = 0.046,
Table 2).
We observed no association of age, gender or histological subtype with the presence of mutations in PD-L1 in patients with NSCLC. PD-L1 mutation status did not seem to influence NLR or PLR values in these patients either (
Table 3).
Disease stage at the time of diagnosis was not associated with either EGFR or PD-L1 mutations (p = 1 and 0.860, respectively). Mortality, assessed from medical records 14 months after the beginning of the study, was not influenced by PD-L1 mutations, but tended to associate with EGFR mutations, without reaching statistical significance level (p = 0.085).
Smoking is a known risk factor for lung cancer. In our study, the median number of packs-year in cancer patients was 4 times higher than in control patients (p < 0.001,
Table 1). Also, the prevalence of COPD in lung cancer patients was higher than in controls (p < 0.001). When examining the association of EGFR mutations with smoking, we observed that cancer patients with EGFR mutations had a significantly lower tobacco cigarettes consumption than those with wild-type EGFR (median of 5 [inter-quartile range, IQR: 0;17.5]
vs. 40 [IQR: 30;50] packs-year, p = 0.002), suggesting that EGFR mutagenesis occurs independently of smoking or that smoking promotes carcinogenesis through mechanisms that do not involve EGFR mutations. The number of cigarette pack-years was not associated with PD-L1 mutations (p = 0.542).
Regarding other comorbidities, although the diagnosis of COPD was most frequently associated with lung cancer, as mentioned, analyzing the 2 groups of patients we observed that the association of cardiovascular pathologies as well as renal pathologies was relatively similar in the group of cancer patients and in the control group, while the association of diabetes mellitus was higher in the control group versus the group of cancer patients (n=26; 26% versus n=20.18%) (
Table 1). Asthma appears to be more common in patients with EGFR mutation than in those without mutation (50% vs. 6.8%, p = 0.014), but this result is recommended to be interpreted with caution given the small number of cases.
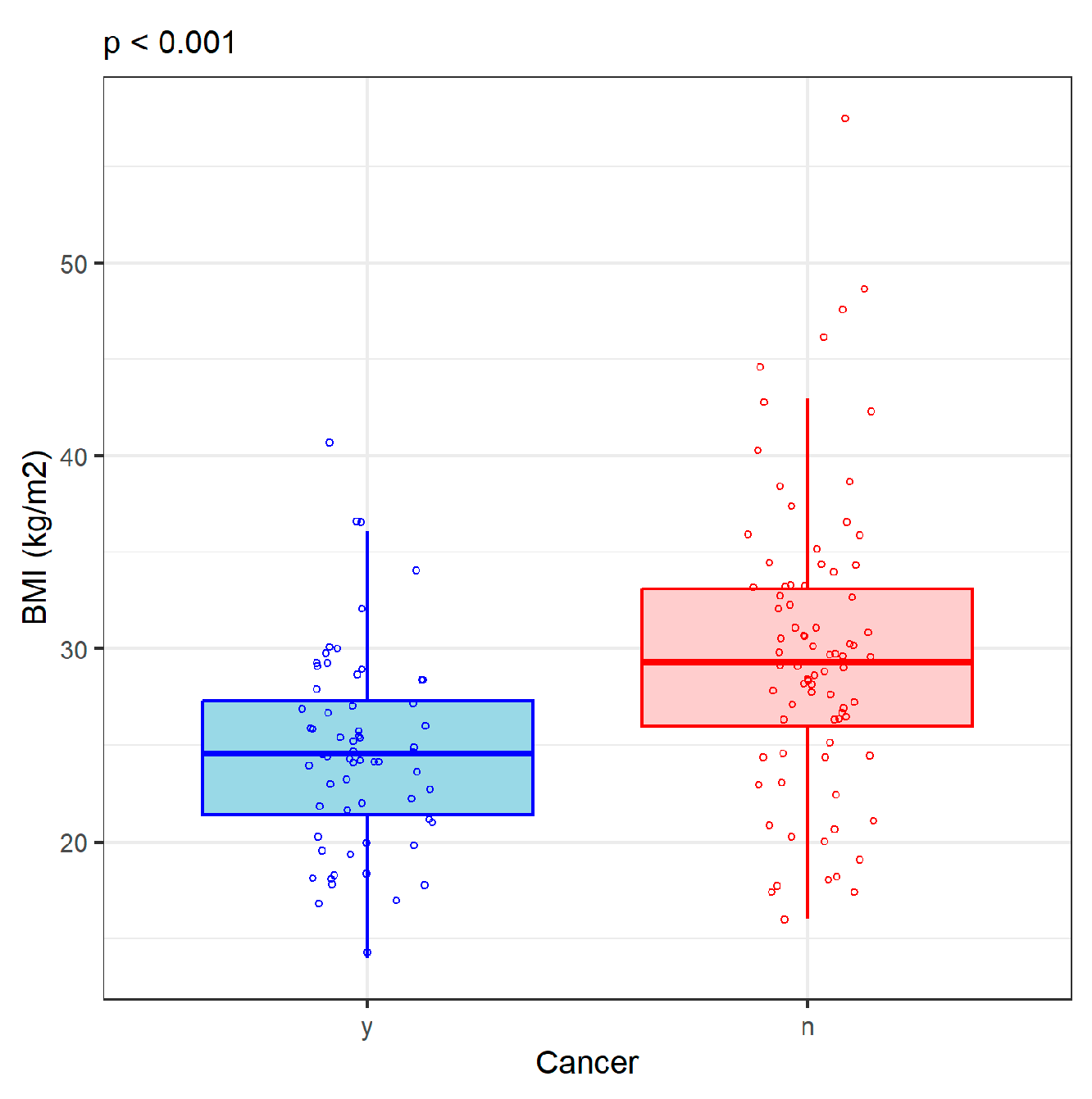
Nutrition status was poorer in lung cancer patients compared with controls; a condition reflected by the lower BMI in the former group (p < 0.001) (
Figure 1). Hemoglobin levels were also lower (p < 0.001) in the cancer group, despite the higher proportion of males than females in this group compared with the control group (
Table 1). However, neither BMI or hemoglobin values were associated with tumor histological type (p = 0.934 and p = 0.669).
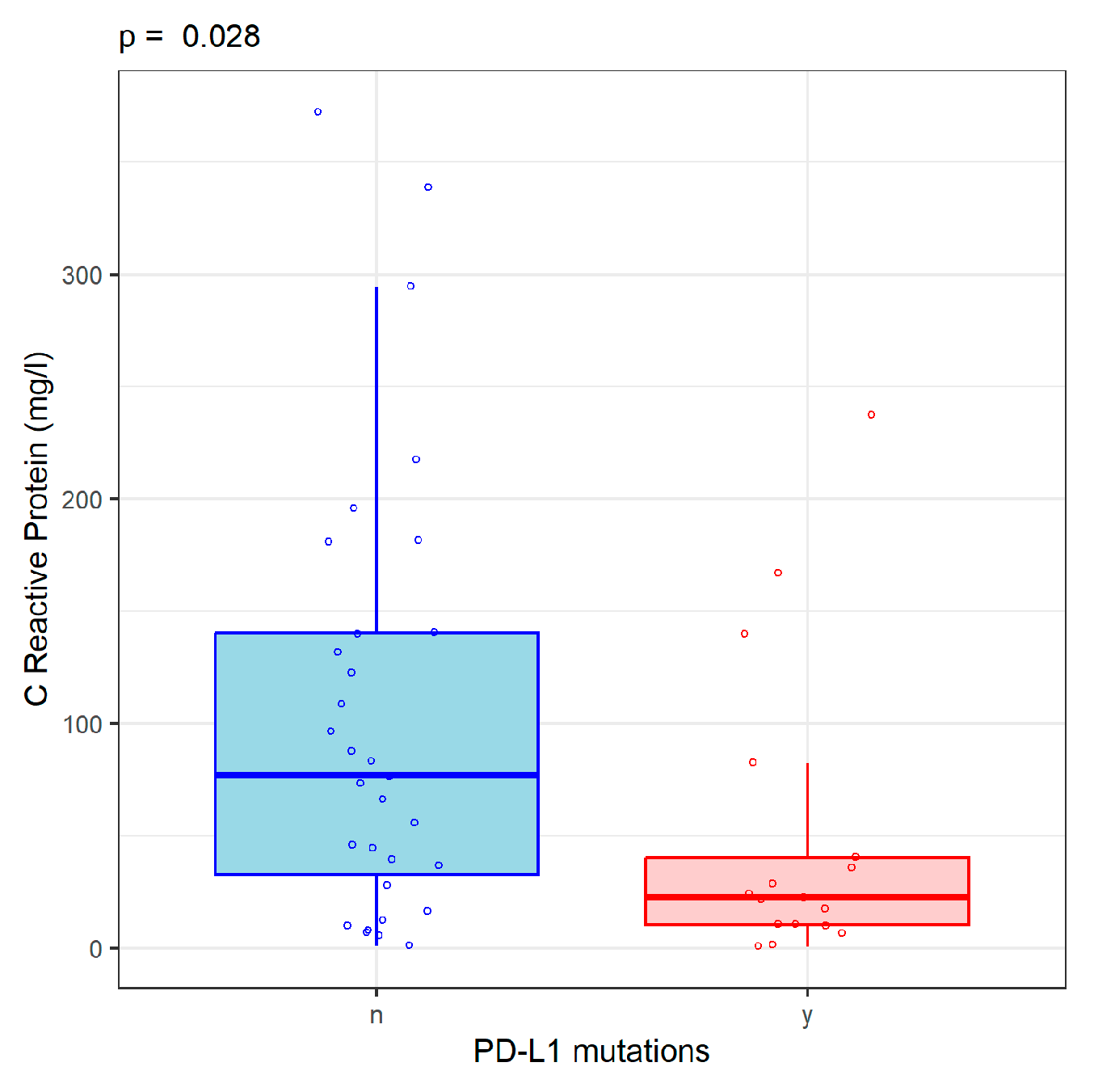
Serum C-reactive protein (CRP) was assessed in cancer patients as a non-specific marker of inflammation. CRP values did not differ according with the histological type of lung cancer (p = 0.242) and were not associated with the presence of mutations in EGFR (p=0.679). CRP values were significantly lower in NSCLC patients with PD-L1 mutations than in those without PD-L1 mutations (22.7 [IQR: 10.4;40.3] vs. 76.7 [IQR: 32.6;140] mg/l, p = 0.029) (
Figure 2).
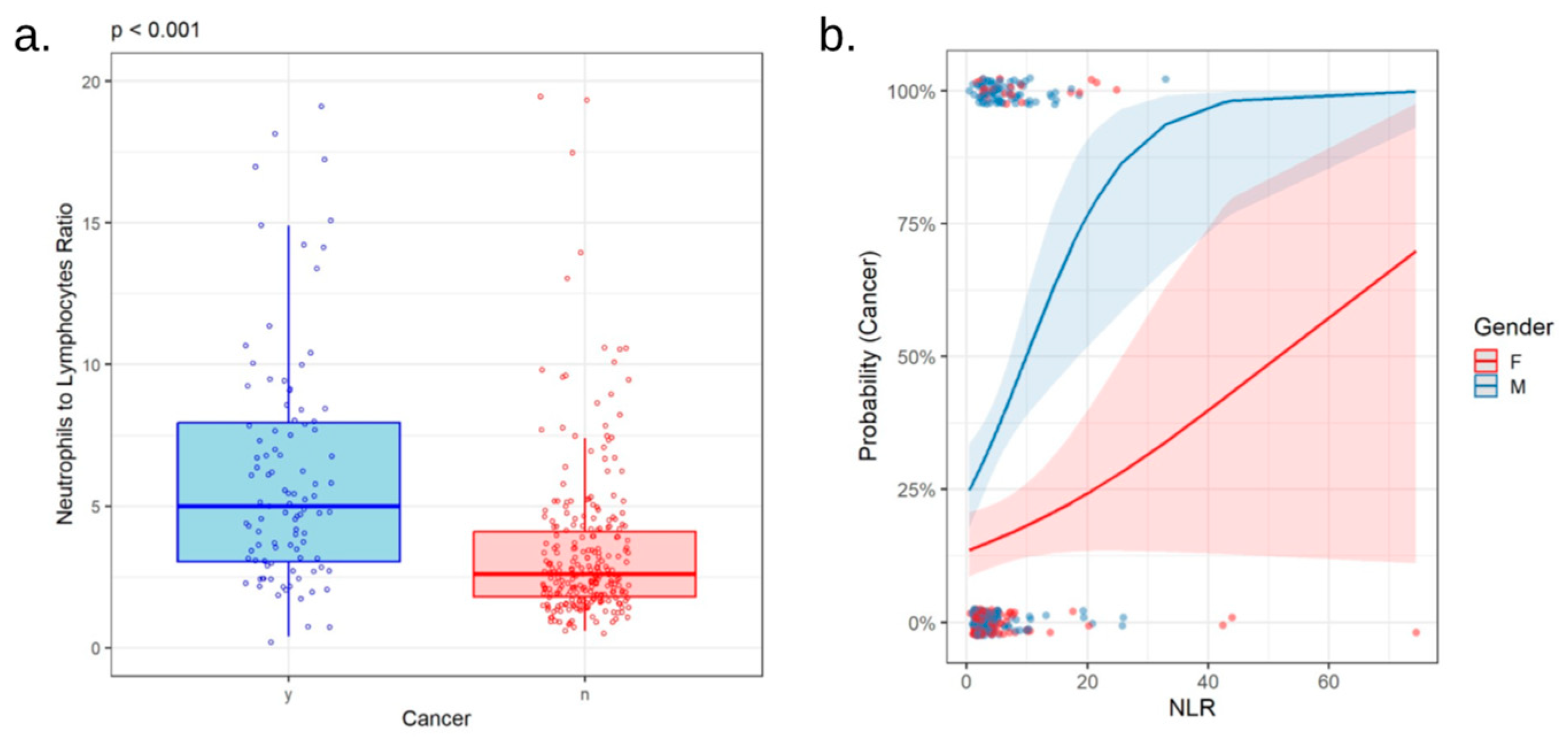
Complete blood count revealed higher numbers of neutrophils and platelets, as well as lower number of lymphocytes in patients with lung cancer compared with controls (p < 0.001, p < 0.001, p = 0.002, respectively;
Table 1). Accordingly, both NLR and PLR were higher in cancer patients (p < 0.001 for both,
Figure 3a and 4a). Neither NLR or PLR varied with tumor histological type. In patients with adenocarcinoma, squamous cell carcinoma and SCLC, NLR values were 5.30 [3.27;8.47], 5.30 [3.50;8.55], and 4.45 [2.58;7.30] respectively (p = 0.580), whereas PLR values were 218 [150;366], 215 [156;326], and 208 [130;324] respectively (p = 0.448). NLR and PLR were not associated with the presence of mutations in EGFR (p = 0.664 and p = 0.645) or PD-L1 (p = 0.233 and p = 0.316) genes.
Interestingly, the correlation of PLR with the probability of lung cancer differs between men and women (p = 0.005 for the interaction between the terms PLR and gender in logistic regression for the presence of cancer,
Figure 4b). The same trend was observed for the interplay of NLR and gender in association with cancer, although at the limit of statistical significance in our group (p = 0.056,
Figure 3b).
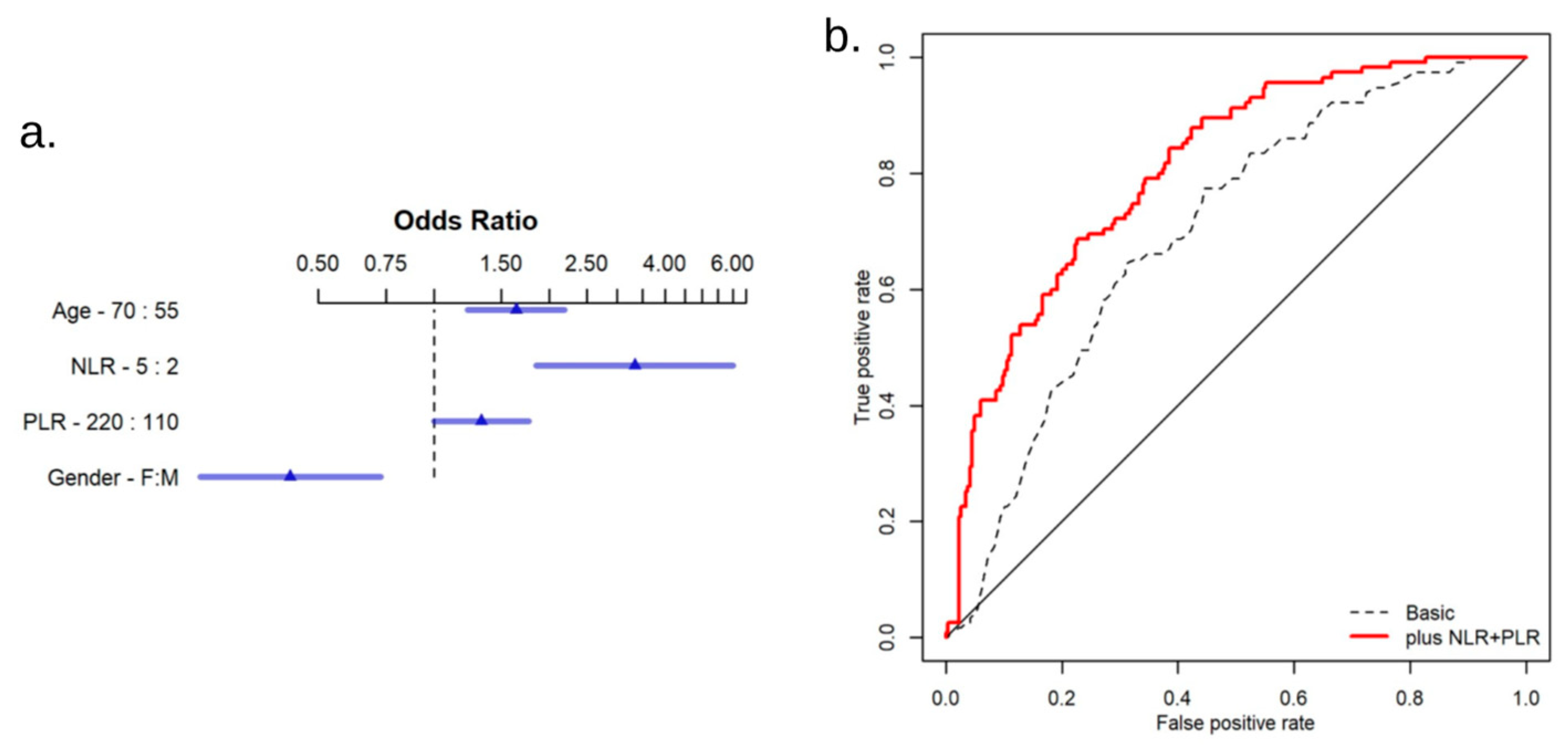
Given the differences in age and gender distribution between our cancer and control groups, we sought to verify whether these variables may be confounders for the differences observed for NLR and PLR in these groups. However, when adjusting for gender and age in multiple logistic regression, NLR and PLR retained their significance as predictive factors for the diagnosis of lung cancer (p < 0.001 and p = 0.048, respectively,
Figure 5a). In addition, a logistic predictive model based on age, gender, NLR and PLR, showed superior discriminative power between cancer and control patients, compared with a predictive model including only age and gender (AUC of 0.777 [ 0.772 - 0.782]
vs. 0.700 [ 0.694 - 0.706],
Figure 5b).
4. Discussion
NLR and PLR, two novel inflammatory biomarkers, are part of the predictive profile of cancer patients [
14]. Some studies in the literature used these parameters to evaluate the response of cancer patients to oncological treatment, especially immunotherapy [
15,
16]. Beyond this aspect correlated with targeted oncological therapy, few studies have addressed the predictive potential diagnostic model of these new inflammatory biomarkers [
17,
18].
The NLR and PLR values in patients with lung cancer have been particularly used in patients with NSCLC. Although the objective of our study aimed to analyze these parameters in NSCLC patients, in the cohort of lung cancer patients (n=115), 27 patients with SCLC were included. In a systematic review published in 2021 by Larsen et al. [
19], the correlation between the increased NLR value in SCLC patients and increased mortality was presented. In our study, the NLR value was lower in patients with SCLC than in those with NSCLC, but mortality could not be fully analyzed as it is a parameter to be evaluated in a subsequent follow-up.
In other research, NLR and PLR have been used in clinical practice to evaluate postoperative prognostic potential [
15], but the cancer patients included in our study were in advanced stages of the disease, where surgical intervention is no longer recommended, so this parameter was not monitored.
The coexistence of a diagnosis of lung cancer and COPD increased the NLR and PLR values [
21], a finding also present in our study.
Research conducted by Dan Pu et al. highlighted that in NSCLC patients with present PD-L1 mutation, an increased NLR value is associated with a poor prognosis, serving as individual predictive factors [
16,
22]. The cutoff values used were 5 for NLR and 200 for PLR [
22]. In our study, the average NLR value was positioned below this cutoff value (4.50 [2.85;5.92]), and the same result was found for PLR (198 [141;304]). The limitation of our study, not analyzing the differentiated group of patients with PD-L1 mutation, stems from the restricted number of patients, thus the data would not have presented statistical validity.
As early as 2014, the study led by Kim et all claimed that cigarette smoking over 30 pack-years is an independent negative predictive factor of targeted treatment with EGFR-TKI [
23]. Although our research did not include assessing the impact of immunotherapy, when examining the association of EGFR mutations with smoking, we observed that cancer patients with EGFR mutations had a significantly lower tobacco cigarettes consumption than those with wild-type EGFR. On the other hand, we did not observe differences in terms of age or gender distribution between patients with or without EGFR mutations.
Analyzing other data from the literature, we found the same cutoff value of 5 for NLR [
24], values above 5 being associated with a low performance index and poor survival [
14]. For PLR, the cutoff value of approximately 200 also correlates with survival and clinical status, values above 200 in PLR are associated with a poor prognosis [
2,
6]. In our study, the average NLR value in the group of cancer patients was 5.3, and the average PLR value was 217. These average values are above the limit found in the literature, which could be explained by the fact that most patients were in advanced stages of the disease at the time of diagnosis. The comparative analysis of these parameters versus the control group confirms the validity of using NLR and PLR as inflammatory biomarkers, even though the data are insufficient to support their predictive model.
The assessment of these two parameters, NLR and PLR, was made, both in our study and in the literature, with the aim of being used as potential diagnostic factors for lung cancer patients [
10], especially those with NSCLC [
25,
26]. The utility of these two easily accessible ratios from routine patient analyses has been used not only for lung cancer but also for hepatocellular carcinoma, gastric cancer, or prostate cancer [
13,
27]. Along with these two parameters, other accessible patient characteristics such as age, gender, body mass index, inflammatory profile, serological, immunohistochemical, or molecular determinations can also be used [
28,
29]. Regarding gender, a study conducted on chinese patients published in 2021 revealed NLR in male was significantly higher than in female, but this study included healthy adults [
30]. In our study also, the probability of lung cancer differs between men and women, even if our population included lung cancer patients. The cumulative analysis of these could contribute to the creation of a predictive model of the evolution of lung cancer patients. In our patient cohort, these parameters were analyzed separately, trying to establish whether they could be contributing factors to this predictive model.
This study constitutes a pilot project by creating a local database, this aspect being a limitation of the study, as it was carried out in a single site. By expanding this cohort, a predictive model with statistical significance could be developed to guide therapeutic management. Another hypothesis would be whether these two parameters could be used as adjunct factors in the diagnostic stage of lung cancer patients, their increased value necessitating a more detailed screening of patients.
One of the limitations of our study include the fact that the NLR value was assessed at the time of oncological diagnosis when the biopsy sample was taken and the NLR value was not assessed pre- and post-oncological treatment or pre- and post-immunotherapy. Another limitation is that we only used Caucasian individuals, and the value of inflammatory biomarkers may vary.
In the literature, there are no commonly accepted values for NLR and PLR. As presented, the most commonly used cutoff values are 5 and 200, respectively [
31]. Since there are no universally accepted values, we did not use a cutoff value, but calculated the average value for the two analyzed groups. To facilitate the assessment of these biomarkers, a universally accepted standard value should be established [
10,
13]. This would represent clinical utility both at the time of diagnosis as a predictive factor of evolution and throughout therapy to assess response to treatment, especially targeted immunotherapy [
32].
5. Conclusions
Along with other biometric, clinical, imaging, serological, the value of NLR and PLR can constitute new predictive biomarkers of diagnostic and disease progression in lung cancer patients, especially those with NSCLC.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Figure S1: title; Table S1: title; Video S1: title.
Author Contributions
Conceptualization, C.E.B, M.O. and I.G.C.; methodology, C.E.B, R.M.R, I.G.C, O.S.C.; software, L.S.E, I.A.R.; validation, C.E.B, I.A.R, C.C, D.E.P. and E.S.I.; formal analysis, R.M.R, E.S.I.; investigation, C.E.B, I.G.C.; resources, C.E.B.; data curation, I.A.B,C.E.B.; writing—original draft preparation, C.E.B, R.M.R.; writing—C.E.B, D.E.P; visualization, O.S.C.; supervision, C.E.B, M.O, O.S.C; project administration, C.E.B, I.G.C.; funding acquisition, C.E.B. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the George Emil Palade University of Medicine, Pharmacy, Science, and Technology of Târgu Mureș Research Grant number 171/8/09.01.2024.
Institutional Review Board Statement
This human study was approved by The ethics committee of Clinical County Hospital Mureș - approval: 6089/28.05.2024. All adult participants provided written informed consent to participate in this study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Michaels E, Bestvina CM (2022) Meeting an un-MET need: Targeting MET in non-small cell lung cancer. Front Oncol 12:1004198.
- Mosca M, Nigro MC, Pagani R, De Giglio A, Di Federico A (2023) Neutrophil-to-Lymphocyte Ratio (NLR) in NSCLC, Gastrointestinal, and Other Solid Tumors: Immunotherapy and Beyond. Biomolecules 13:1803. [CrossRef]
- Guo R, Berry LD, Aisner DL, et al (2019) MET IHC is a Poor Screen for MET Amplification or MET exon 14 mutations in Lung Adenocarcinomas: Data from a Tri-Institutional Cohort of the Lung Cancer Mutation Consortium. J Thorac Oncol 14:1666–1671. [CrossRef]
- Guthrie GJK, Charles KA, Roxburgh CSD, Horgan PG, McMillan DC, Clarke SJ (2013) The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol 88:218–230. [CrossRef]
- Køstner AH, Fuglestad AJ, Georgsen JB, et al (2023) Fueling the flames of colon cancer – does CRP play a direct pro-inflammatory role? Front Immunol 14:1170443. [CrossRef]
- Cupp MA, Cariolou M, Tzoulaki I, Aune D, Evangelou E, Berlanga-Taylor AJ (2020) Neutrophil to lymphocyte ratio and cancer prognosis: an umbrella review of systematic reviews and meta-analyses of observational studies. BMC Med 18:360. [CrossRef]
- Diem S, Schmid S, Krapf M, Flatz L, Born D, Jochum W, Templeton AJ, Früh M (2017) Neutrophil-to-Lymphocyte ratio (NLR) and Platelet-to-Lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer 111:176–181. [CrossRef]
- Budin CE, Marginean C, Bordea IR, Enache LS, Enache EL, Grigorescu BL, Biro L, Rusu E, Nemes RM, Todea DA The Influence of Smoking on Nicotine Exposure Biomarkers and Inflammatory Profile Among Foster Care Teenagers, Romania. 5.
- Zahorec R (2001) Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 102:5–14.
- Valero C, Lee M, Hoen D, et al (2021) Pretreatment neutrophil-to-lymphocyte ratio and mutational burden as biomarkers of tumor response to immune checkpoint inhibitors. Nat Commun 12:729. [CrossRef]
- Martinez-García MÁ, Olveira C, Girón R, et al (2022) Peripheral Neutrophil-to-Lymphocyte Ratio in Bronchiectasis: A Marker of Disease Severity. Biomolecules 12:1399. [CrossRef]
- Budin CE, Nemeș AF, Râjnoveanu R-M, et al (2023) The Inflammatory Profile Correlates with COVID-19 Severity and Mortality in Cancer Patients. J Pers Med 13:1235. [CrossRef]
- Zhang H, Zhang L, Zhu K, Shi B, Yin Y, Zhu J, Yue D, Zhang B, Wang C (2015) Prognostic Significance of Combination of Preoperative Platelet Count and Neutrophil-Lymphocyte Ratio (COP-NLR) in Patients with Non-Small Cell Lung Cancer: Based on a Large Cohort Study. PLoS One 10:e0126496. [CrossRef]
- Zhu X, Song H, Chen Y, Han F, Wang Q, Cui Y (2020) Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio in Blood to Distinguish Lung Cancer Patients from Healthy Subjects. Dis Markers 2020:8844698. [CrossRef]
- Khunger M, Patil PD, Khunger A, et al (2018) Post-treatment changes in hematological parameters predict response to nivolumab monotherapy in non-small cell lung cancer patients. PLOS ONE 13:e0197743. [CrossRef]
- Shukuya T, Carbone DP (2016) Predictive Markers for the Efficacy of Anti–PD-1/PD-L1 Antibodies in Lung Cancer. J Thorac Oncol 11:976–988. [CrossRef]
- Mandaliya H, Jones M, Oldmeadow C, Nordman II (2019) Prognostic biomarkers in stage IV non-small cell lung cancer (NSCLC): neutrophil to lymphocyte ratio (NLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR) and advanced lung cancer inflammation index (ALI). Transl Lung Cancer Res 8:886–894. [CrossRef]
- Prodromidou A, Andreakos P, Kazakos C, Vlachos DE, Perrea D, Pergialiotis V (2017) The diagnostic efficacy of platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio in ovarian cancer. Inflamm Res 66:467–475. [CrossRef]
- Winther-Larsen A, Aggerholm-Pedersen N, Sandfeld-Paulsen B (2021) Inflammation scores as prognostic biomarkers in small cell lung cancer: a systematic review and meta-analysis. Syst Rev 10:40. [CrossRef]
- Cao W, Yu H, Zhu S, Lei X, Li T, Ren F, Zhou N, Tang Q, Zu L, Xu S (2022) Clinical significance of preoperative neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in the prognosis of resected early-stage patients with non-small cell lung cancer: A meta-analysis. Cancer Med 12:7065–7076. [CrossRef]
- Ma A, Wang G, Du Y, et al (2022) The clinical relevance of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in chronic obstructive pulmonary disease with lung cancer. Front Oncol 12:902955. [CrossRef]
- Pu D, Xu Q, Zhou L, Zhou Y, Liu J, Ma X (2021) Inflammation-nutritional markers of peripheral blood could predict survival in advanced non-small-cell lung cancer patients treated with PD-1 inhibitors. Thorac Cancer 12:2914–2923. [CrossRef]
- Kim MH, Kim HR, Cho BC, Bae MK, Kim EY, Lee CY, Lee JS, Kang DR, Kim JH (2014) Impact of cigarette smoking on response to epidermal growth factor receptor (EGFR)-tyrosine kinase inhibitors in lung adenocarcinoma with activating EGFR mutations. Lung Cancer 84:196–202.
- Platini H, Ferdinand E, Kohar K, Prayogo SA, Amirah S, Komariah M, Maulana S (2022) Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Prognostic Markers for Advanced Non-Small-Cell Lung Cancer Treated with Immunotherapy: A Systematic Review and Meta-Analysis. Medicina (Kaunas) 58:1069. [CrossRef]
- Platini H, Ferdinand E, Kohar K, Prayogo SA, Amirah S, Komariah M, Maulana S (2022) Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Prognostic Markers for Advanced Non-Small-Cell Lung Cancer Treated with Immunotherapy: A Systematic Review and Meta-Analysis. Medicina (Kaunas) 58:1069. [CrossRef]
- Lamberti G, Sisi M, Andrini E, Palladini A, Giunchi F, Lollini P-L, Ardizzoni A, Gelsomino F (2020) The Mechanisms of PD-L1 Regulation in Non-Small-Cell Lung Cancer (NSCLC): Which Are the Involved Players? Cancers (Basel) 12:3129. [CrossRef]
- Rungsakulkij N, Mingphruedhi S, Suragul W, Tangtawee P, Muangkaew P, Aeesoa S (2018) Platelet-to-lymphocyte ratio and large tumor size predict microvascular invasion after resection for hepatocellular carcinoma. HPB 20:S370.
- Liu J, Li S, Zhang S, Liu Y, Ma L, Zhu J, Xin Y, Wang Y, Yang C, Cheng Y (2019) Systemic immune-inflammation index, neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio can predict clinical outcomes in patients with metastatic non-small-cell lung cancer treated with nivolumab. J Clin Lab Anal 33:e22964. [CrossRef]
- Gu X, Sun S, Gao X-S, et al (2016) Prognostic value of platelet to lymphocyte ratio in non-small cell lung cancer: evidence from 3,430 patients. Sci Rep 6:23893. [CrossRef]
- Wang J, Zhang F, Jiang F, Hu L, Chen J, Wang Y (2021) Distribution and reference interval establishment of neutral-to-lymphocyte ratio (NLR), lymphocyte-to-monocyte ratio (LMR), and platelet-to-lymphocyte ratio (PLR) in Chinese healthy adults. J Clin Lab Anal 35:e23935. [CrossRef]
- Russo A, Russano M, Franchina T, et al (2020) Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), and Outcomes with Nivolumab in Pretreated Non-Small Cell Lung Cancer (NSCLC): A Large Retrospective Multicenter Study. Adv Ther 37:1145–1155. [CrossRef]
- Takada K, Takamori S, Yoneshima Y, et al (2020) Serum markers associated with treatment response and survival in non-small cell lung cancer patients treated with anti-PD-1 therapy. Lung Cancer 145:18–26. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).