Submitted:
04 July 2024
Posted:
05 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
1.1. Goal
2. Research Methodology for Statistical Analysis
- ▪ Health expenditures a share of GDP, from 2009 to 2019 (OECD, 2024)
- ▪ Government consolidated gross debt, as a share of GDP, from 2009 to 2019 (Eurostat, 2024)
- ▪ Case fatality rate (CFR) on 30 December 2020 and 2022 (JHU, 2023)
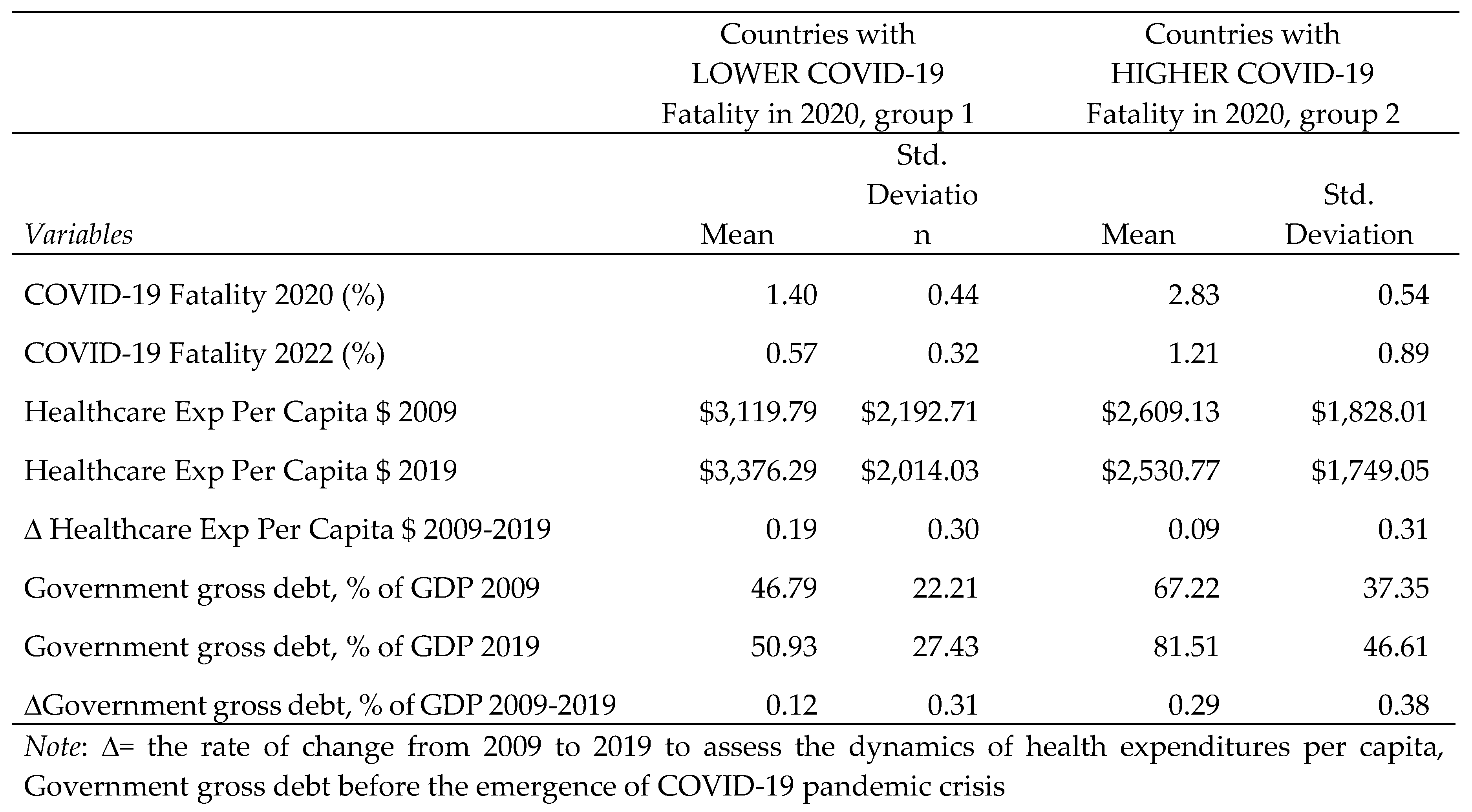
- Group 1, Countries with lower COVID-19 fatality rates in 2020 than the sample arithmetic mean.
- Group 2, Countries with higher COVID-19 fatality rates in 2020 than the sample arithmetic mean.
3. Results and Analysis of Findings
4. Discussion and Public Policy Implications to Face Complex Emergencies and Global Crises
5. Conclusions
- high public debt over time reduces health expenditures and increases the vulnerability of countries to face emergencies, such as COVID-19 pandemic crisis.
- more economic resources the nations spend in health sector, the better they are likely to face emergencies and reduce the case fatality rates.
- when countries experience a 1% increase in healthcare expenditure per capita, in general they have a 1.2% reduction in the COVID-19 fatality rate.
- countries must reduce public debt with good governance and institutions without reducing the allocation of economic resources to the healthcare sector in order to improve the preparedness to unforeseen emergencies and crises, such as pandemics, natural disasters, conflicts, and other environmental catastrophes.
| 1 | Cf. also, Down et al., 2020; Elo et al., 2022; El-Sadr et al., 2023; Fisman, 2022; Flaxman et al., 2020; Galvani et al., 2022; Goolsbee and Syverson, 2021; Götz al., 2024; Haghighi and Takian, 2024; Haldane et al., 2021; Coccia 2023, 2023b, 2024, Coccia and Benati, 2028, 2018°; Kluge et al., 2020; Legido-Quigley et al., 2020; Levin et al., 2020; Magazzino et al., 2022; McKee, 2020, Miranda et al., 2024; Núñez-Delgado et al., 2021, 2023, 2024, 2024a, 2024b; Coccia, 2018b, 2028c, 2022h, 2023c, 2023d, 2024; Kapitsinis, 2020; Kargi et al., 2023, 2023°, 2023b; Khan et al., 2020; Kim et al., 2022; Coccia and Bontempi, 2023, Galvão et al., 2021; Homburg, 2020; Jacques et al., 2023; Penkler et al., 2020; Rađenović et al., 2021; Roche, 2023. |
References
- Abel, J. G., & Gietel-Basten, S. (2020). International remittance flows and the economic and social consequences of COVID-19. Environment and Planning A: Economy and Space, 52(8), 1480-1482.
- Aboelnaga S, Czech K, Wielechowski M, Kotyza P, Smutka L, Ndue K. 2023. COVID-19 resilience index in European Union countries based on their risk and readiness scale. PLoS One. 18(8):e0289615. [CrossRef] [PubMed] [PubMed Central]
- Agoraki MK, Kardara S, Kollintzas T, et al. (2023) Debt-to-GDP changes and the great recession: European Periphery versus European Core. Int J Finance Econ 28: 3299–3331.
- Ahmed, S.M., Khanam, M., Shuchi, N.S. 2024. COVID-19 pandemic in Bangladesh: A scoping review of governance issues affecting response in public sector. Public Health in Practice, 7, 100457.
- Aizenman J, Ito H (2023) Post COVID-19 exit strategies and emerging markets economic challenges. Rev Int Econ 31: 1–34.
- Akan, A.P.; Coccia, M. (2022). Changes of Air Pollution between Countries Because of Lockdowns to Face COVID-19 Pandemic. Applied Sciences 12 (24), 12806. [CrossRef]
- Akan, A.P.; Coccia, M. 2023. Transmission of COVID-19 in cities with weather conditions of high air humidity: Lessons learned from Turkish Black Sea region to face next pandemic crisis, COVID, vol. 3, n. 11, 1648-1662. [CrossRef]
- Alesina A, Favero C, Giavazzi F (2019) Austerity: When it works and when it doesn’t, Princeton University Press. [CrossRef]
- Allen Douglas W. 2022. Covid-19 Lockdown Cost/Benefits: A Critical Assessment of the Literature, International Journal of the Economics of Business, 29(1), 1-32. [CrossRef]
- Almeida, A. 2024. The trade-off between health system resiliency and efficiency: evidence from COVID-19 in European regions, European Journal of Health Economics, 25(1), pp. 31–47.
- Amarlou, A., & Coccia, M. (2023). Estimation of diffusion modelling of unhealthy nanoparticles by using natural and safe microparticles. Nanochemistry Research, 8(2), 117-121. [CrossRef]
- Angelopoulos A. N., Pathak R., Varma R., Jordan M. I. (2020). On Identifying and Mitigating Bias in the Estimation of the COVID-19 Case Fatality Rate. Harvard Data Science Review. [CrossRef]
- Ardito L., Coccia M., Messeni Petruzzelli A. 2021. Technological exaptation and crisis management: Evidence from COVID-19 outbreaks. R&D Management, vol. 51, n. 4, pp. 381-392. [CrossRef]
- Bacchiocchi E, Borghi E, Missale A (2011) Public investment under fiscal constraints. Fiscal Studies 32: 11–42.
- Ball, P. (2021) What the COVID-19 pandemic reveals about science, policy, and society. Interface Focus, 11 (6). 20210022. [CrossRef]
- Banik, A., Nag, T., Chowdhury, S. R., & Chatterjee, R. (2020). Why do COVID-19 fatality rates differ across countries? An explorative cross-country study based on select indicators. Global Business Review, 21(3), 607-625.
- Barro, R. J., (2020). Non-Pharmaceutical Interventions and Mortality in U.S. Cities during the Great Influenza Pandemic, 1918-1919. NBER Working Paper, No. 27049. [CrossRef]
- Benach, J., Cash-Gibson, L., Rojas-Gualdrón, D. F., Padilla-Pozo, Á., Fernández-Gracia, J., Eguíluz, V. M., & COVID-SHINE group (2022). Inequalities in COVID-19 inequalities research: Who had the capacity to respond? PloS one, 17(5), e0266132. [CrossRef]
- Benati I., Coccia M. (2022a). Global analysis of timely COVID-19 vaccinations: Improving governance to reinforce response policies for pandemic crises. International Journal of Health Governance, 27(3): 240-253. [CrossRef]
- Benati I.,Coccia M. (2022). Effective Contact Tracing System Minimizes COVID-19 Related Infections and Deaths: Policy Lessons to Reduce the Impact of Future Pandemic Diseases. Journal of Public Administration and Governance, 12(3), 19-33. [CrossRef]
- Bo, Y., Guo, C., Lin, C., Zeng, Y., Li, H. B., Zhang, Y.,... & Lao, X. Q. (2021). Effectiveness of non-pharmaceutical interventions on COVID-19 transmission in 190 countries from 23 January to 13 April 2020. International Journal of Infectious Diseases, 102, 247-253.
- Bontempi E., Coccia M., 2021. International trade as critical parameter of COVID-19 spread that outclasses demographic, economic, environmental, and pollution factors, Environmental Research, vol. 201, n. 111514. [CrossRef]
- Bontempi E., Coccia M., Vergalli S., Zanoletti A. (2021). Can commercial trade represent the main indicator of the COVID-19 diffusion due to human-to-human interactions? A comparative analysis between Italy, France, and Spain, Environmental Research, 201, 111529. [CrossRef]
- Brauner, J. M., Mindermann, S., Sharma, M., Johnston, D., Salvatier, J., Gavenčiak, T.,... & Kulveit, J. (2020). The effectiveness of eight nonpharmaceutical interventions against COVID-19 in 41 countries. MedRxiv. [CrossRef]
- Cao, Y., Hiyoshi, A., & Montgomery, S. (2020). COVID-19 case-fatality rate and demographic and socioeconomic influencers: worldwide spatial regression analysis based on country-level data. BMJ open, 10(11), e043560.
- Chowdhury T., Chowdhury H., Bontempi E., Coccia M., Masrur H., Sait S. M., Senjyu T. (2022). Are mega-events super spreaders of infectious diseases similar to COVID-19? A look into Tokyo 2020 Olympics and Paralympics to improve preparedness of next international events. Environmental Science and Pollution Research, 30(4). [CrossRef]
- Coccia M (2017) Asymmetric paths of public debts and of general government deficits across countries within and outside the European monetary unification and economic policy of debt dissolution. The Journal of Economic Asymmetries 15: 17-31. [CrossRef]
- Coccia M. (2014). Socio-cultural origins of the patterns of technological innovation: What is the likely interaction among religious culture, religious plurality and innovation? Towards a theory of socio-cultural drivers of the patterns of technological innovation, Technology in Society, vol. 36, n. 1, pp. 13-25. [CrossRef]
- Coccia M. (2016). Radical innovations as drivers of breakthroughs: characteristics and properties of the management of technology leading to superior organizational performance in the discovery process of R&D labs, Technology Analysis & Strategic Management, vol. 28, n. 4, pp. 381-395. [CrossRef]
- Coccia M. (2018). General properties of the evolution of research fields: a scientometric study of human microbiome, evolutionary robotics and astrobiology, Scientometrics, vol. 117, n. 2, pp. 1265-1283. [CrossRef]
- Coccia M. (2018a). An introduction to the theories of institutional change, Journal of Economics Library, vol. 5, n. 4, pp. 337-344.
- Coccia M. (2019). Comparative Institutional Changes. A. Farazmand (ed.), Global Encyclopedia of Public Administration, Public Policy, and Governance, Springer. [CrossRef]
- Coccia M. (2019a). Intrinsic and extrinsic incentives to support motivation and performance of public organizations, Journal of Economics Bibliography, vol. 6, no. 1, pp. 20-29.
- Coccia M. (2019b). Comparative Incentive Systems. In: Farazmand, A. (eds) Global Encyclopedia of Public Administration, Public Policy, and Governance. Springer, Cham. [CrossRef]
- Coccia M. (2019c). Theories of Development. A. Farazmand (ed.), Global Encyclopedia of Public Administration, Public Policy, and Governance, Springer. [CrossRef]
- Coccia M. (2020). An index to quantify environmental risk of exposure to future epidemics of the COVID-19 and similar viral agents: Theory and Practice. Environmental Research, volume 191, n. 110155. [CrossRef]
- Coccia M. (2020a). Effects of Air Pollution on COVID-19 and Public Health, Research Article-Environmental Economics-Environmental Policy, ResearchSquare. [CrossRef]
- Coccia M. (2020b). Asymmetry of the technological cycle of disruptive innovations. Technology Analysis & Strategic Management, vol. 32, n. 12, p. 1462-1477. [CrossRef]
- Coccia M. (2020c). Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID, Science of the Total Environment, 729, 138474. [CrossRef]
- Coccia M. (2020d). How (Un)sustainable Environments are Related to the Diffusion of COVID-19: The Relation between Coronavirus Disease 2019, Air Pollution, Wind Resource and Energy. Sustainability 12(22), 9709. [CrossRef]
- Coccia M. (2021). Comparative Critical Decisions in Management. In: Farazmand A. (eds), Global Encyclopedia of Public Administration, Public Policy, and Governance. Springer Nature, Cham. [CrossRef]
- Coccia M. (2021a). The relation between length of lockdown, numbers of infected people and deaths of COVID-19, and economic growth of countries: Lessons learned to cope with future pandemics similar to COVID-19. Science of The Total Environment, vol. 775, n. 145801. [CrossRef]
- Coccia M. (2021b). Pandemic Prevention: Lessons from COVID-19. Encyclopedia, vol. 1, n. 2, pp. 433-444. [CrossRef]
- Coccia M. (2021c). Different effects of lockdown on public health and economy of countries: Results from first wave of the COVID-19 pandemic. Journal of Economics Library, 8(1), 45-63.
- Coccia M. (2021d). Recurring waves of Covid-19 pandemic with different effects in public health, Journal of Economics Bibliography, vol. 8, n. 1, pp. 28-45.
- Coccia M. (2021e). High health expenditures and low exposure of population to air pollution as critical factors that can reduce fatality rate in COVID-19 pandemic crisis: a global analysis. Environmental Research, 199, 111339. [CrossRef]
- Coccia M. (2021f). How do low wind speeds and high levels of air pollution support the spread of COVID-19? Atmospheric Pollution Research, vol. 12, n.1, pp. 437-445. [CrossRef]
- Coccia M. (2021g). Evolution and structure of research fields driven by crises and environmental threats: the COVID-19 research. Scientometrics, vol. 126, n. 12, pp. 9405-9429. [CrossRef]
- Coccia M. (2021h). The impact of first and second wave of the COVID-19 pandemic: comparative analysis to support control measures to cope with negative effects of future infectious diseases in society. Environmental Research, vol. 197, n. 111099. [CrossRef]
- Coccia M. (2021i). Effects of human progress driven by technological change on physical and mental health, STUDI DI SOCIOLOGIA, 2021, n. 2, pp. 113-132. [CrossRef]
- Coccia M. (2021L). Effects of the spread of COVID-19 on public health of polluted cities: results of the first wave for explaining the dejà vu in the second wave of COVID-19 pandemic and epidemics of future vital agents. Environmental Science and Pollution Research. 28(15), 19147-19154. [CrossRef]
- Coccia M. (2021m). Critical decisions for crisis management: An introduction. J. Adm. Soc. Sci., vol. 8, n.1, pp. 1-14.
- Coccia M. (2022). Meta-analysis to explain unknown causes of the origins of SARS-COV-2. Environmental Research, vol. 111, Article n. 113062.
- Coccia M. (2022a). COVID-19 Vaccination is not a Sufficient Public Policy to face Crisis Management of next Pandemic Threats. Public Organization Review, 1-15. [CrossRef]
- Coccia M. (2022b). Effects of strict containment policies on COVID-19 pandemic crisis: lessons to cope with next pandemic impacts. Environmental Science and Pollution Research, 30(1). 2020-2028. [CrossRef]
- Coccia M. (2022c). Improving preparedness for next pandemics: Max level of COVID-19 vaccinations without social impositions to design effective health policy and avoid flawed democracies. Environmental Research, 213, 113566. [CrossRef]
- Coccia M. (2022d). Optimal levels of vaccination to reduce COVID-19 infected individuals and deaths: A global analysis. Environmental Research, 204, 112314. [CrossRef]
- Coccia M. (2022e). Preparedness of countries to face COVID-19 pandemic crisis: Strategic positioning and underlying structural factors to support strategies of prevention of pandemic threats, Environmental Research, 203, 111678. [CrossRef]
- Coccia M. (2022f). COVID-19 pandemic over 2020 (with lockdowns) and 2021 (with vaccinations): similar effects for seasonality and environmental factors. Environmental Research, vol. 208, n. 112711. [CrossRef]
- Coccia M. (2022g). The Spread of the Novel Coronavirus Disease-2019 in Polluted Cities: Environmental and Demographic Factors to Control for the Prevention of Future Pandemic Diseases. In: Faghih, N., Forouharfar, A. (eds) Socioeconomic Dynamics of the COVID-19 Crisis. Contributions to Economics: 351-369. Springer, Cham. [CrossRef]
- Coccia M. (2023). High potential of technology to face new respiratory viruses: mechanical ventilation devices for effective healthcare to next pandemic emergencies, Technology in Society, 73, 102233. [CrossRef]
- Coccia M. (2023a). Sources, diffusion and prediction in COVID-19 pandemic: lessons learned to face next health emergency. AIMS Public Health, 10(1), 145. [CrossRef]
- Coccia M. (2023b). COVID-19 Vaccination is not a Sufficient Public Policy to face Crisis Management of next Pandemic Threats. Public Organiz Rev 23, 1353–1367. [CrossRef]
- Coccia M. (2024). Basic role of medical ventilators to lower COVID-19 fatality and face next pandemic crises. Journal of Social and Administrative Sciences, 11(1), 1–26. Retrieved from https://journals.econsciences.com/index.php/JSAS/article/view/246.
- Coccia M., Benati I. (2018). Comparative Evaluation Systems, A. Farazmand (ed.), Global Encyclopedia of Public Administration, Public Policy, and Governance, Springer. [CrossRef]
- Coccia M., Benati I. (2018a). Comparative Studies. Global Encyclopedia of Public Administration, Public Policy, and Governance –section Bureaucracy (edited by Ali Farazmand). Chapter No. 1197-1, pp. 1-7, Springer, Cham. [CrossRef]
- Coccia, M. (2018b). An introduction to the methods of inquiry in social sciences. Journal of Social Administrative Science, 5(2), 116-126.
- Coccia, M. (2018c). An introduction to the theories of national and regional economic development, Turkish Economic Review, vol. 5, n. 4, pp. 350-358.
- Coccia, M. (2022h). Probability of discoveries between research fields to explain scientific and technological change. Technology in Society, vol. 68, February, n. 101874. [CrossRef]
- Coccia, M. (2023c). COVID-19 Pandemic Crisis: Analysis of origins, diffusive factors and problems of lockdowns and vaccinations to design best policy responses Vol.2. KSP Books, Kadikoy, Istanbul, Turkey, 2023. ISBN: 978-625-7813-54-9 (e-Book).
- Coccia, M. (2023d). Effects of strict containment policies on COVID-19 pandemic crisis: lessons to cope with next pandemic impacts. Environmental science and pollution research, 30(1), 2020–2028. [CrossRef]
- Coccia, M. (2024a). Digital Pathology Ecosystem: Basic Elements to Revolutionize the Diagnosis and Monitoring of Diseases in Health Sector. In: Faghih, N. (eds) Digital Entrepreneurship. Contributions to Management Science. pp. 111-134, Springer, Cham. [CrossRef]
- Coccia, M., Benati I. (2024). Negative effects of high public debt on health systems facing pandemic crisis: Lessons from COVID-19 in Europe to prepare for future emergencies[J]. AIMS Public Health, 11(2): 477-498. [CrossRef]
- Coccia, M., Benati I. (2024a). Effective health systems facing pandemic crisis: lessons from COVID-19 in Europe for next emergencies, International Journal of Health Governance. [CrossRef]
- Coccia, M., Bontempi E. (2023). New trajectories of technologies for the removal of pollutants and emerging contaminants in the environment. Environmental Research, vol. 229, n. 115938. [CrossRef]
- Crivelli E, Leive A, Stratmann MT (2010) Subnational health spending and soft budget constraints in OECD countries. International Monetary Fund.
- Dowd, J. B., Andriano, L., Brazel, D. M., Rotondi, V., Block, P., Ding, X.,... & Mills, M. C. (2020). Demographic science aids in understanding the spread and fatality rates of COVID-19. Proceedings of the National Academy of Sciences, 117(18), 9696-9698.
- ECB (2016) Government debt reduction strategies in the Euro area. Econ Bull 4: 1–20.
- Elo I.T., Luck A., Stokes A.C., Hempstead K., Xie W., Preston S.H. (2022). Evaluation of Age Patterns of COVID-19 Mortality by Race and Ethnicity from March 2020 to October 2021 in the US. JAMA Network Open, 5(5), e2212686-e2212686. [CrossRef]
- El-Sadr, W. M., Vasan, A., & El-Mohandes, A. (2023). Facing the New Covid-19 Reality. The New England journal of medicine, 388(5), 385–387. [CrossRef]
- Essers D, Cassimon D (2022) Towards HIPC 2.0? Lessons from past debt relief initiatives for addressing current debt problems. JGD 13: 187–231.
- Eurostat (2024) Database. https://ec.europa.eu/eurostat/data/database (accessed July 2024).
- Fisman D. (2022). Universal healthcare and the pandemic mortality gap. Proceedings of the National Academy of Sciences of the United States of America, 119(29), e2208032119. [CrossRef]
- Flaxman, S., Mishra, S., Gandy, A., Unwin, H.J.T., Mellan, T.A., Coupland, H.,Whittaker, C., (...), Bhatt, S. (2020). Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature, 584(7820), 257-261.
- Galvani, A. P., Parpia, A. S., Pandey, A., Sah, P., Colón, K., Friedman, G., Campbell, T., Kahn, J. G., Singer, B. H., & Fitzpatrick, M. C. (2022). Universal healthcare as pandemic preparedness: The lives and costs that could have been saved during the COVID-19 pandemic. Proceedings of the National Academy of Sciences of the United States of America, 119(25), e2200536119. [CrossRef]
- Galvão MHR, Roncalli AG. 2021. Factors associated with increased risk of death from covid-19: a survival analysis based on confirmed cases. Rev Bras Epidemiol. 23:e200106. Portuguese, English. [CrossRef] [PubMed]
- Goolsbee, A., Syverson, C. (2021). Fear, lockdown, and diversion: Comparing drivers of pandemic economic decline 2020. Journal of public economics, 193, 104311. [CrossRef]
- Götz, P., Auping, W.L., Hinrichs-Krapels, S. 2024. Contributing to health system resilience during pandemics via purchasing and supply strategies: an exploratory system dynamics approach. BMC Health Services Research, 24(1), 130.
- Haghighi, H., Takian, A. 2024. Institutionalization for good governance to reach sustainable health development: a framework analysis. Globalization and Health, 20(1), 5.
- Haldane, V., De Foo, C., Abdalla, S.M., Jung, A., Tan, M.M., Wu, S., Chua, A.Q., Verma, M., Shrestha, P., Singh, S., Perez, T., Tan, S.M., Bartoš, M., Mabuchi, S., Bonk, M., McNab, C., Werner, G.K., Panjabi, R., Nordström, A., & Legido-Quigley, H. (2021). Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nature Medicine, 27, 964 - 980.
- Homburg, S., (2020). Effectiveness of corona lockdowns: evidence for a number of countries. The Economists’ Voice, 17(1),20200010.
- Iwata Y, IIboshi H (2023) The nexus between public debt and the government spending multiplier: fiscal adjustments matter. Oxf Bull Econ Stat 85: 830–858. [CrossRef]
- Jacques, O., Arpin, E., Ammi, M., & Noël, A. (2023). The political and fiscal determinants of public health and curative care expenditures: evidence from the Canadian provinces, 1980-2018. Canadian journal of public health = Revue canadienne de sante publique, 1–9. Advance online publication. [CrossRef]
- JHU (2023). Johns Hopkins Center for System Science and Engineering, 2023-COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://www.arcgis.com/apps/dashboards/bda7594740fd40299423467b48e9ecf6 (accessed on 18 May 2023).
- Kapitsinis N. (2020). The underlying factors of the COVID-19 spatially uneven spread. Initial evidence from regions in nine EU countries. Regional Science Policy and Practice, 12(6), 1027-1045.
- Karanikolos M, Azzopardi-Muscat N, Ricciardi W, et al. (2022) The impact of austerity policies on health systems in Southern Europe. Social Welfare Issues in Southern Europe, Routledge, 119–139.
- Kargı B., Mario Coccia, Bekir Cihan Uçkaç (2023). Findings from the first wave of COVID-19 on the different impacts of lockdown on public health and economic growth. International Journal of Economic Sciences. Vol. XII, No. 2 / 2023, pp. 21-39. [CrossRef]
- Kargı B., Mario Coccia, Bekir Cihan Uçkaç (2023a). How does the wealth level of nations affect their COVID19 vaccination plans? Economics, Management and Sustainability. 8(2): 6-19. [CrossRef]
- Kargı B., Mario Coccia, Bekir Cihan Uçkaç (2023b). The Relation Between Restriction Policies against Covid-19, Economic Growth and Mortality Rate in Society. Migration Letters, Vol. 20, n. 5, pp. 218-231.
- Khan, J. R., Awan, N., Islam, M. M., & Muurlink, O. (2020). Healthcare capacity, health expenditure, and civil society as predictors of COVID-19 case fatalities: a global analysis. Frontiers in public health, 8, 347.
- Kim, K. M., Evans, D. S., Jacobson, J., Jiang, X., Browner, W., & Cummings, S. R. (2022). Rapid prediction of in-hospital mortality among adults with COVID-19 disease. PloS one, 17(7), e0269813. [CrossRef]
- Kluge H. H. P., Nitzan D., Azzopardi-Muscat N. (2020). COVID-19: reflecting on experience and anticipating the next steps. A perspective from the WHO Regional Office for Europe. Eurohealth, 26(2), 13-15.
- Legido-Quigley, H., Asgari, N., Teo, Y. Y., Leung, G. M., Oshitani, H., Fukuda, K.,... & Heymann, D. (2020). Are high-performing health systems resilient against the COVID-19 epidemic? The Lancet, 395(10227), 848-850.
- Levaggi R, Menoncin F (2013) Soft budget constraints in health care: evidence from Italy. Eur J Health Econ 14: 725–737.
- Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G. 2020. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. 35(12):1123-1138. [CrossRef]
- Magazzino C., Mele M., Coccia M. (2022). A machine learning algorithm to analyze the effects of vaccination on COVID-19 mortality. Epidemiology and infection, 150, e168. [CrossRef]
- McKee M. A (2020). European roadmap out of the covid-19 pandemic. British Medical Journal, 369.
- Miranda, J., Barahona, O.M., Krüger, A.B., Lagos, P., Moreno-Serra, R. 2024. Central America and the Dominican Republic at Crossroads: The Importance of Regional Cooperation and Health Economic Research to Address Current Health Challenges, Value in Health Regional Issues, 39, pp. 107–114.
- Núñez-Delgado A., Bontempi E., Coccia M., Kumar M., Farkas K., Domingo, J. L. 2021. SARS-CoV-2 and other pathogenic microorganisms in the environment, Environmental Research, vol. 201, n. 111606. [CrossRef]
- Núñez-Delgado, Avelino, Elza Bontempi, Yaoyu Zhou, Esperanza Álvarez-Rodríguez, María Victoria López-Ramón, Mario Coccia, Zhien Zhang, Vanesa Santás-Miguel, and Marco Race. 2024. "Editorial of the Topic “Environmental and Health Issues and Solutions for Anticoccidials and other Emerging Pollutants of Special Concern”" Processes 12, no. 7: 1379. [CrossRef]
- Núñez-Delgado, Avelino, Zhien Zhang, Elza Bontempi, Mario Coccia, Marco Race, and Yaoyu Zhou. 2023. Editorial on the Topic “New Research on Detection and Removal of Emerging Pollutants” Materials, vol. 16, no. 2: 725. [CrossRef]
- Núñez-Delgado, Avelino, Zhien Zhang, Elza Bontempi, Mario Coccia, Marco Race, and Yaoyu Zhou. 2024. Topic Reprint, New Research on Detection and Removal of Emerging Pollutants, Volume I, MDPI, mdpi.com/topics. [CrossRef]
- Núñez-Delgado, Avelino, Zhien Zhang, Elza Bontempi, Mario Coccia, Marco Race, and Yaoyu Zhou. 2024a. Topic Reprint, New Research on Detection and Removal of Emerging Pollutants, Volume II, MDPI, mdpi.com/topics. [CrossRef]
- OECD (2024). Health expenditure and financing. https://stats.oecd.org/Index.aspx?DataSetCode=SHA (accessed on 15 June 2024).
- Penkler, M., Müller, R., Kenney, M., & Hanson, M. (2020). Back to normal? Building community resilience after COVID-19. The Lancet Diabetes & Endocrinology, 8(8), 664-665.
- Rađenović T., Radivojević V., Krstić B., Stanišić T., Živković S.(2021). The Efficiency of Health Systems in Response to the COVID-19 Pandemic: Evidence from the EU Countries. Problemy Ekorozwoju – Problems Of Sustainable Development, 17(1), 7-15.
- Roche (2023). Growing healthcare capacity to improve access to healthcare. https://www.roche.com/about/strategy/access-to-healthcare/capacity/ (accessed on 27June 2023).
- Sagan, A., Erin, W., Dheepa, R., Marina, K., & Scott, L. G. (2021). Health system resilience during the pandemic: It’s mostly about governance. Eurohealth, 27(1), 10-15.
- Sagan, A., Thomas, S., McKee, M., Karanikolos, M., Azzopardi-Muscat, N., de la Mata, I.,... & World Health Organization. (2020). COVID-19 and health systems resilience: lessons going forwards. Eurohealth, 26(2), 20-24.
- Sanyaolu, A., Okorie, C., Marinkovic, A., Patidar, R., Younis, K., Desai, P.,... & Altaf, M. (2020). Comorbidity and its impact on patients with COVID-19. SN comprehensive clinical medicine, 2, 1069-1076. [CrossRef]
- Shakor, J. K., Isa, R. A., Babakir-Mina, M., Ali, S. I., Hama-Soor, T. A., & Abdulla, J. E. (2021). Health related factors contributing to COVID-19 fatality rates in various communities across the world. The Journal of Infection in Developing Countries, 15(09), 1263-1272.
- Singh, A. 2024. Dealing with Uncertainties During COVID-19 Pandemic: Learning from the Case Study of Bombay Mothers and Children Welfare Society (BMCWS), Mumbai, India. Journal of Entrepreneurship and Innovation in Emerging Economies, 10(1), pp. 97–118.
- Smith, R. W., Jarvis, T., Sandhu, H. S., Pinto, A. D., O'Neill, M., Di Ruggiero, E., Pawa, J., Rosella, L., & Allin, S. (2023). Centralization and integration of public health systems: Perspectives of public health leaders on factors facilitating and impeding COVID-19 responses in three Canadian provinces. Health policy (Amsterdam, Netherlands), 127, 19–28. [CrossRef]
- Soltesz, K., Gustafsson, F., Timpka, T., Jaldén, J., Jidling, C., Heimerson, A.,... & Bernhardsson, B. (2020). The effect of interventions on COVID-19. Nature, 588(7839), E26-E28.
- Sorci, G., Faivre, B., & Morand, S. (2020). Explaining among-country variation in COVID-19 case fatality rate. Scientific reports, 10(1), 18909.
- Souliotis K, Papadonikolaki J, Papageorgiou M, et al. (2018) The impact of crisis on health and health care: Thoughts and data on the Greek case. Arch Hell Med 35: 9–16.
- Theodoropoulou S (2022) Recovery, resilience and growth regimes under overlapping EU conditionalities: the case of Greece. CEP 20: 201–219.
- Tisdell, C. A. (2020). Economic, social and political issues raised by the COVID-19 pandemic. Economic analysis and policy, 68, 17-28.
- Uçkaç, B.C., Coccia, M., & Kargi, B. (2023). Diffusion COVID-19 in polluted regions: Main role of wind energy for sustainable and health, International Journal of Membrane Science and Technology, 10(3), 2755-2767. [CrossRef]
- Uçkaç, B.C., Coccia, M., & Kargı, B., (2023a). Simultaneous encouraging effects of new technologies for socioeconomic and environmental sustainability. Bulletin Social-Economic and Humanitarian Research, 19(21), 100-120.
- Upadhyay, A. K., & Shukla, S. (2021). Correlation study to identify the factors affecting COVID-19 case fatality rates in India. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 15(3), 993-999.
- Verma, A. K., & Prakash, S. (2020). Impact of covid-19 on environment and society. Journal of Global Biosciences, 9(5), 7352-7363.
- Wieland, T. (2020). A phenomenological approach to assessing the effectiveness of COVID-19 related nonpharmaceutical interventions in Germany. Safety Science, 131, 104924.
- Wolff D, Nee S, Hickey NS, Marschollek M. 2021. Risk factors for Covid-19 severity and fatality: a structured literature review. Infection. 49(1):15-28. [CrossRef]
- Zhang, N., Chan, P. T. J., Jia, W., Dung, C. H., Zhao, P., Lei, H.,... & Li, Y. (2021). Analysis of efficacy of intervention strategies for COVID-19 transmission: A case study of Hong Kong. Environment International, 156, 106723.
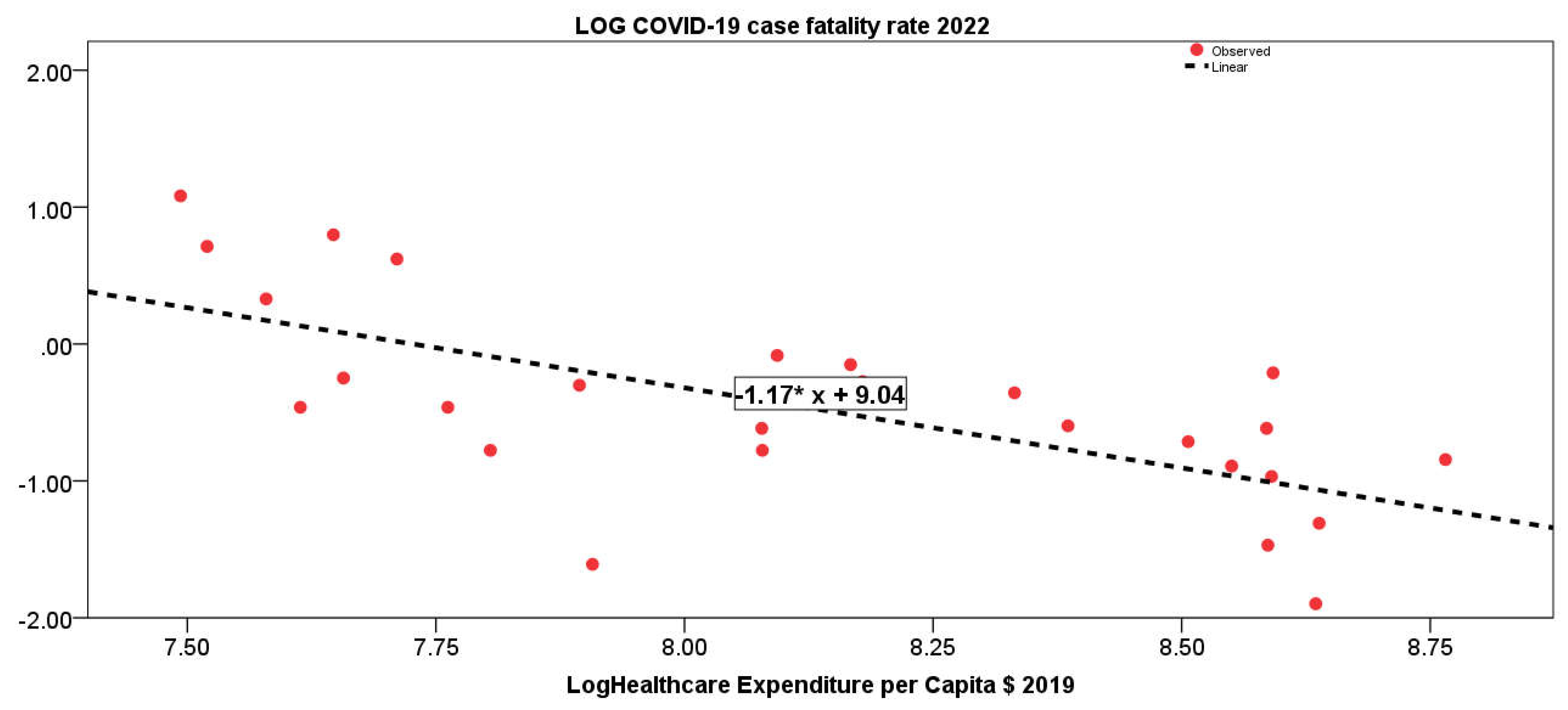
| Log Healthcare Expenditure per Capita $ in 2019 |
|
| Log COVID-19 fatality rate in 2022 | −0.67** |
| Constant | Coefficient of regression β |
Standardized coefficient of regression β |
R2 | F | |
| COVID-19 case fatality rate 2022 | 9.04*** | −1.17*** | −0.67 | 0.45 | 20.79*** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





