Submitted:
10 July 2024
Posted:
11 July 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Data collection, Variables Definition and Grouping
2.3. Statistical Analysis
3. Results
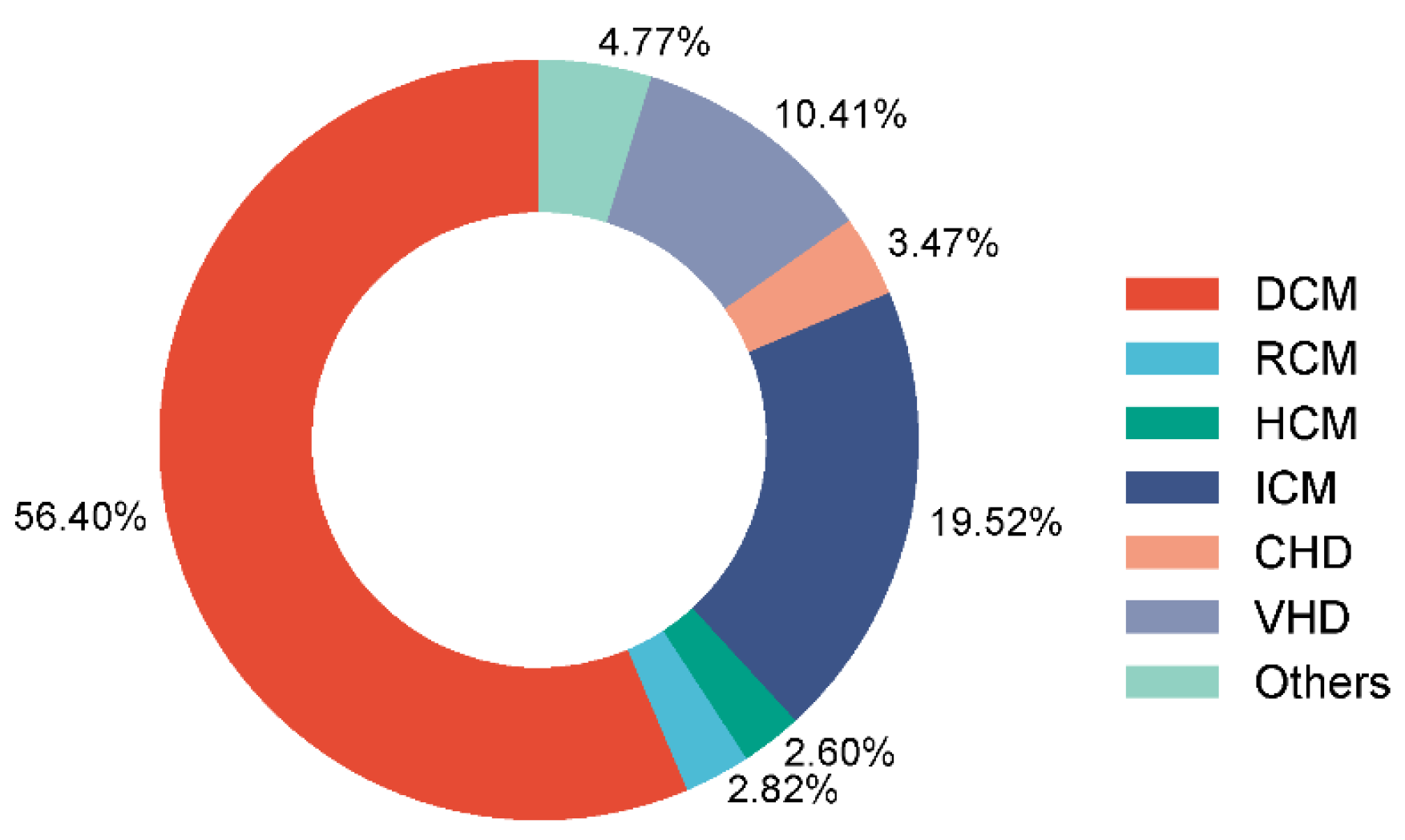
3.1. Patients’ Characteristics
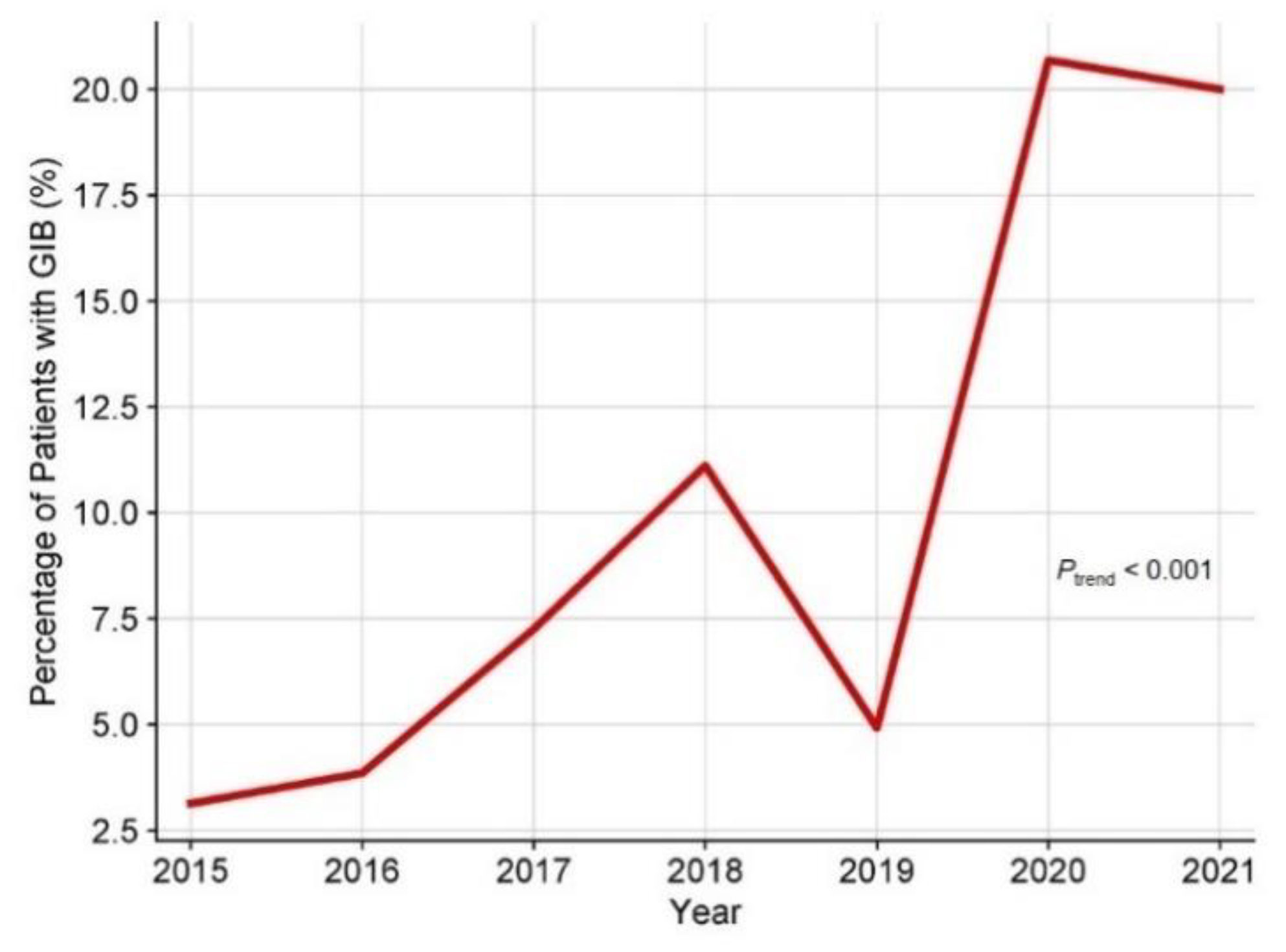
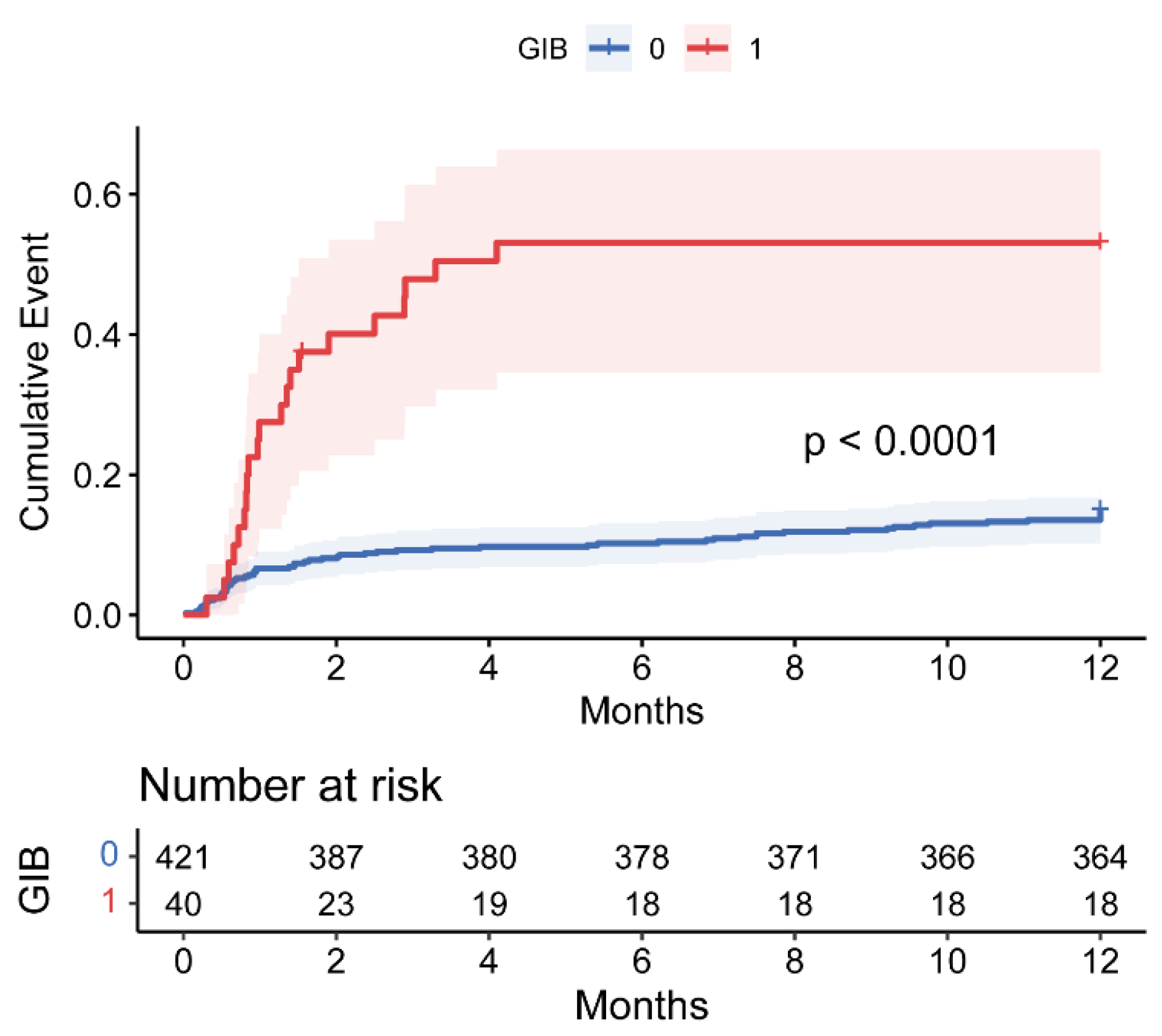
3.2. Postoperative GIB and Survival in HT Patients
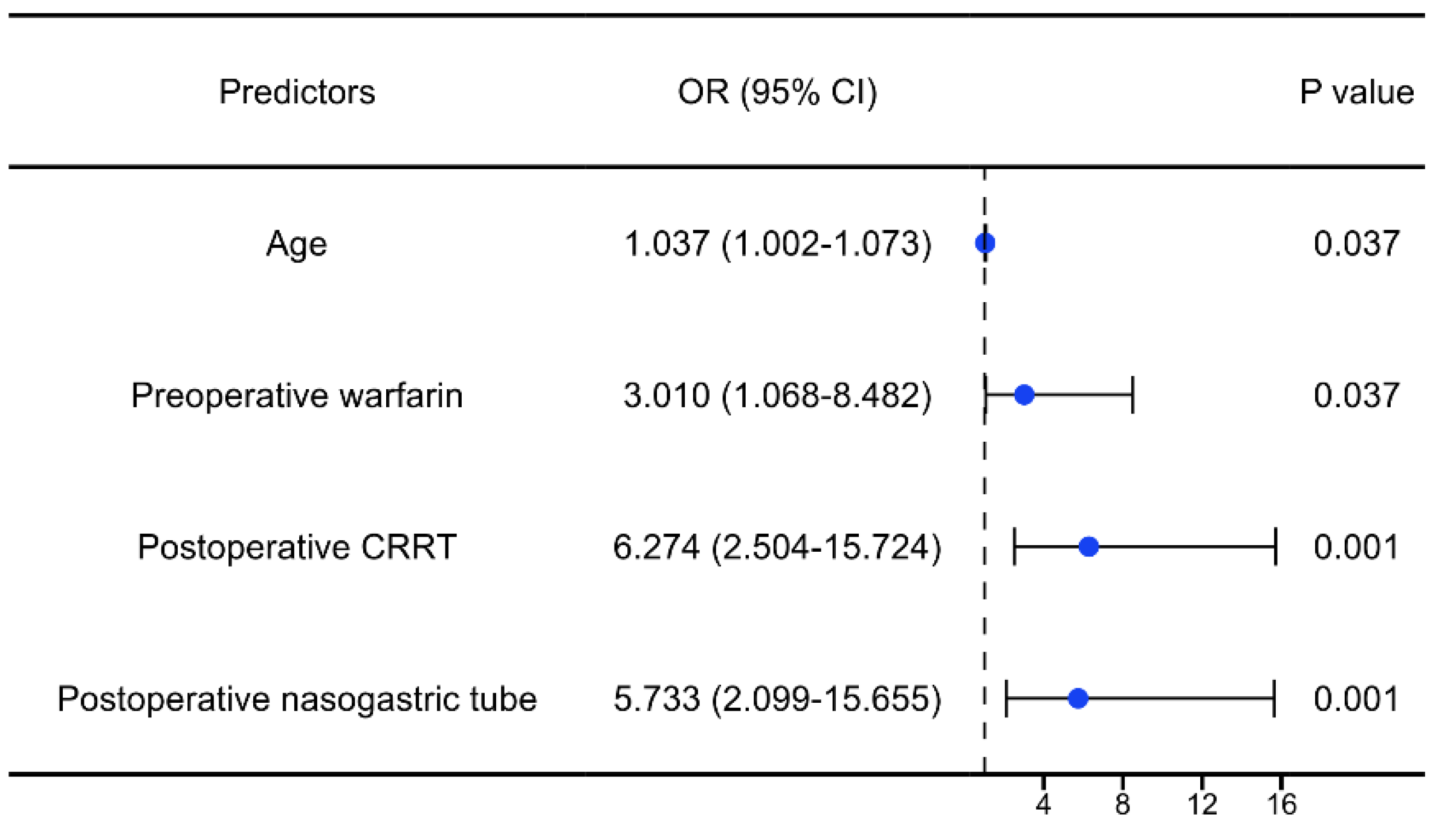
3.3. Risk Factors of Postoperative GIB in HT Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jou, S.; Mendez, S.R.; Feinman, J.; Mitrani, L.R.; Fuster, V.; Mangiola, M.; Moazami, N.; Gidea, C. Heart transplantation: advances in expanding the donor pool and xenotransplantation. Nat. Rev. Cardiol. 2024, 21, 25–36. [CrossRef]
- Asleh, R., Alnsasra, H., Villavicencio, M.A., Daly, R.C., Kushwaha, S.S. Cardiac Transplantation: Physiology and Natural History of the Transplanted Heart. Comprehensive Physiology. 2023;13(3):4719-65.
- Shoji, S., Kuno, T., Kohsaka, S., Amiya, E., Asleh, R., Alvarez, P., Kampaktsis, P., Staffa, S.J., Zurakowski, D., Doulamis, I., Briasoulis, A. Incidence and long-term outcome of heart transplantation patients who develop postoperative renal failure requiring dialysis. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2022;41(3):356-64.
- Kainuma, A.; Ning, Y.; Kurlansky, P.A.; Wang, A.S.; Latif, F.; Farr, M.A.; Sayer, G.T.; Uriel, N.; Takayama, H.; Naka, Y.; et al. Deep vein thrombosis and pulmonary embolism after heart transplantation. Clin. Transplant. 2022, 36, e14705. [CrossRef]
- Vest, A.R.M.; Cherikh, W.S.; Noreen, S.M.; Stehlik, J.; Khush, K.K.M. New-onset Diabetes Mellitus After Adult Heart Transplantation and the Risk of Renal Dysfunction or Mortality. Transplantation 2022, 106, 178–187. [CrossRef]
- Schwarzova, K.; Damle, S.; Sellke, F.W.; Robich, M.P. Gastrointestinal complications after cardiac surgery. Trauma Surg. Acute Care Open 2024, 9, e001324. [CrossRef]
- Fan, H.; Zheng, Z.; Feng, W.; Wang, W.; Song, Y.; Lin, Y.; Hu, S. Risk factors and prevention of upper gastrointestinal hemorrhage after a coronary artery bypass grafting operation. Surg. Today 2010, 40, 931–935. [CrossRef]
- Converse, M.P.; Sobhanian, M.; Taber, D.J.; Houston, B.A.; Meadows, H.B.; Uber, W.E. Effect of Angiotensin II Inhibitors on Gastrointestinal Bleeding in Patients With Left Ventricular Assist Devices. Circ. 2019, 73, 1769–1778. [CrossRef]
- Berg, D., Lebovics, E., Kai, M., Spielvogel, D. The Predicament of Gastrointestinal Bleeding in Patients With a Continuous-Flow Left Ventricular Assist Device: Pathophysiology, Evaluation, and Management. Cardiology in review. 2019;27(5):222-9.
- Henricksen, E.J., Tremblay-Gravel, M., Moayedi, Y., Yang, W., Lee, R., Ross, H.J., Hiesinger, W., Teuteberg, J.J., Khush, K.K. Use of direct oral anticoagulants after heart transplantation. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 2020;39(4):399-401.
- Patel, S.R.; Oh, K.T.; Ogriki, T.; Sims, D.; Shin, J.J.; Madan, S.; Saeed, O.; Goldstein, D.J.; Jorde, U.P. Cessation of Continuous Flow Left Ventricular Assist Device–Related Gastrointestinal Bleeding After Heart Transplantation. Asaio J. 2018, 64, 191–195. [CrossRef]
- Li, Z.-Q.; Zhang, W.; Guo, Z.; Du, X.-W.; Wang, W. Risk factors of gastrointestinal bleeding after cardiopulmonary bypass in children: a retrospective study. Front. Cardiovasc. Med. 2023, 10, 1224872. [CrossRef]
- Bhagra, S.K.; Pettit, S.; Parameshwar, J. Cardiac transplantation: indications, eligibility and current outcomes. Heart 2019, 105, 252–260. [CrossRef]
- Halm, U., Halm, F., Thein, D., Mohr, F.W., Mössner, J. Helicobacter pylori infection: a risk factor for upper gastrointestinal bleeding after cardiac surgery? Critical care medicine. 2000;28(1):110-3.
- Krawiec, F.; Maitland, A.; Duan, Q.; Faris, P.; Belletrutti, P.J.; Kent, W.D. Duodenal ulcers are a major cause of gastrointestinal bleeding after cardiac surgery. J. Thorac. Cardiovasc. Surg. 2017, 154, 181–188. [CrossRef]
- Briasoulis, A.; Inampudi, C.; Pala, M.; Asleh, R.; Alvarez, P.; Bhama, J. Induction immunosuppressive therapy in cardiac transplantation: a systematic review and meta-analysis. Hear. Fail. Rev. 2018, 23, 641–649. [CrossRef]
- Rizk, J.; Mehra, M.R. WITHDRAWN: Anticoagulation management strategies in heart transplantation. Prog. Cardiovasc. Dis. 2020, 63. [CrossRef]
- Haberbusch, M.; De Luca, D.; Moscato, F. Changes in Resting and Exercise Hemodynamics Early After Heart Transplantation: A Simulation Perspective. Front. Physiol. 2020, 11. [CrossRef]
- Su, Y., Zhu, C., Wang, B., Zheng, H., McAlister, V., Lacefield, J.C., Quan, D., Mele, T., Greasley, A., Liu, K., Zheng, X. Circular RNA Foxo3 in cardiac ischemia-reperfusion injury in heart transplantation: A new regulator and target. American journal of transplantation : official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2021;21(9):2992-3004.
- Kim, S.H.; Han, K.; Kang, G.; Lee, S.W.; Park, C.-M.; Cho, J.; Choi, J.W.; Park, S.J.; Kang, M.; Kim, T.J.; et al. Risk of Postoperative Gastrointestinal Bleeding and Its Associated Factors: A Nationwide Population-Based Study in Korea. J. Pers. Med. 2021, 11, 1222. [CrossRef]
- Hsu, J.L.; Chen, K.A.; Butler, L.R.; Bahraini, A.; Kapadia, M.R.; Gomez, S.M.; Farrell, T.M. Application of machine learning to predict postoperative gastrointestinal bleed in bariatric surgery. Surg. Endosc. 2023, 37, 7121–7127. [CrossRef]
- Lenti, M.V.; Pasina, L.; Cococcia, S.; Cortesi, L.; Miceli, E.; Dominioni, C.C.; Pisati, M.; Mengoli, C.; Perticone, F.; Nobili, A.; et al. Mortality rate and risk factors for gastrointestinal bleeding in elderly patients. Eur. J. Intern. Med. 2019, 61, 54–61. [CrossRef]
- Harel, Z.; Chertow, G.M.; Shah, P.S.; Harel, S.; Dorian, P.; Yan, A.T.; Saposnik, G.; Sood, M.M.; Molnar, A.O.; Perl, J.; et al. Warfarin and the Risk of Stroke and Bleeding in Patients With Atrial Fibrillation Receiving Dialysis: A Systematic Review and Meta-analysis. Can. J. Cardiol. 2017, 33, 737–746. [CrossRef]
- Kaneko, T.; Aranki, S.F. Anticoagulation for Prosthetic Valves. Thrombosis 2013, 2013, 1–4. [CrossRef]
- Eikelboom, J.W.; Connolly, S.J.; Brueckmann, M.; Granger, C.B.; Kappetein, A.P.; Mack, M.J.; Blatchford, J.; Devenny, K.; Friedman, J.; Guiver, K.; et al. Dabigatran versus Warfarin in Patients with Mechanical Heart Valves. New Engl. J. Med. 2013, 369, 1206–1214. [CrossRef]
- Asleh, R.; Schettle, S.; Briasoulis, A.; Killian, J.M.; Stulak, J.M.; Pereira, N.L.; Kushwaha, S.S.; Maltais, S.; Dunlay, S.M. Predictors and Outcomes of Renal Replacement Therapy After Left Ventricular Assist Device Implantation. Mayo Clin. Proc. 2019, 94, 1003–1014. [CrossRef]
- Elizabeth Parsons, C., Nelson, R., Book, L.S., Kyle Jensen, M. Renal replacement therapy in infants and children with hepatorenal syndrome awaiting liver transplantation: a case-control study. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2014;20(12):1468-74.
- Granholm, A.; Krag, M.; Marker, S.; Alhazzani, W.; Perner, A.; Møller, M.H. Predictors of gastrointestinal bleeding in adult ICU patients in the SUP-ICU trial. Acta Anaesthesiol. Scand. 2021, 65, 792–800. [CrossRef]
- Sparrow, C.T.; Nassif, M.E.; Raymer, D.S.; Novak, E.; LaRue, S.J.; Schilling, J.D. Pre-Operative Right Ventricular Dysfunction Is Associated With Gastrointestinal Bleeding in Patients Supported With Continuous-Flow Left Ventricular Assist Devices. JACC: Hear. Fail. 2015, 3, 956–964. [CrossRef]
- Zhou, Z.; Liu, C.; Yang, Y.; Wang, F.; Zhang, L.; Fu, P. Anticoagulation options for continuous renal replacement therapy in critically ill patients: a systematic review and network meta-analysis of randomized controlled trials. Crit. Care 2023, 27, 1–17. [CrossRef]
- Sanaie, S.; Mirzalou, N.; Shadvar, K.; Golzari, S.E.J.; Soleimanpour, H.; Shamekh, A.; Bettampadi, D.; Safiri, S.; Mahmoodpoor, A. A comparison of nasogastric tube insertion by SORT maneuver (sniffing position, NGT orientation, contralateral rotation, and twisting movement) versus neck flexion lateral pressure in critically ill patients admitted to ICU: a prospective randomized clinical trial. Ann. Intensiv. Care 2020, 10, 1–8. [CrossRef]
- Nelson, R., Edwards, S., Tse, B. Prophylactic nasogastric decompression after abdominal surgery. The Cochrane database of systematic reviews. 2007;2007(3):Cd004929.
- Lin, Y.; Chen, M.; Peng, Y.; Chen, Q.; Li, S.; Chen, L. Feeding intolerance and risk of poor outcome in patients undergoing cardiopulmonary bypass surgery. Br. J. Nutr. 2021, 126, 1340–1346. [CrossRef]
- Lavi, R.; Katznelson, R.; Cheng, D.; Minkovich, L.; Klein, A.; Carroll, J.; Karski, J.; Djaiani, G. The Effect of Nasogastric Tube Application During Cardiac Surgery on Postoperative Nausea and Vomiting—A Randomized Trial. J. Cardiothorac. Vasc. Anesthesia 2011, 25, 105–109. [CrossRef]
- Kotfis, K.; Szylińska, A.; Listewnik, M.; Lechowicz, K.; Kosiorowska, M.; Drożdżal, S.; Brykczyński, M.; Rotter, I.; Żukowski, M. Balancing intubation time with postoperative risk in cardiac surgery patients – a retrospective cohort analysis. Ther. Clin. Risk Manag. 2018, 14, 2203–2212. [CrossRef]
- Marks, D.; Cox, A.; Prodromou, A.; Gadelrab, R.; Pakzad, F.; Harrison, R. Fatal consequences of nasogastric intubation: a clinical reminder. J. R. Soc. Med. 2009, 102, 157–159. [CrossRef]
- Mistry, R.C., Vijayabhaskar, R., Karimundackal, G., Jiwnani, S., Pramesh, C.S. Effect of short-term vs prolonged nasogastric decompression on major postesophagectomy complications: a parallel-group, randomized trial. Archives of surgery (Chicago, Ill : 1960). 2012;147(8):747-51.
- Gomes, C.A., Jr., Andriolo, R.B., Bennett, C., Lustosa, S.A., Matos, D., Waisberg, D.R., Waisberg, J. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. The Cochrane database of systematic reviews. 2015;2015(5):Cd008096.
- Adamik, B.; Kübler, A.; Gozdzik, A.; Gozdzik, W. Prolonged Cardiopulmonary Bypass is a Risk Factor for Intestinal Ischaemic Damage and Endotoxaemia. Hear. Lung Circ. 2017, 26, 717–723. [CrossRef]

| Non-GIB (n=421) | GIB (n=40) | P values | |
|---|---|---|---|
| Age (years) | 50.00 (39.00-57.00) | 54.50 (47.50-58.00) | 0.024 |
| Gender, male (%) | 84 (20.0) | 11 (27.5) | 0.259 |
| BMI (kg/m2) | 23.02 ± 3.97 | 22.02 ± 2.89 | 0.120 |
| Blood type | 0.774 | ||
| A, n (%) | 146 (34.7) | 12 (30.0) | |
| B, n (%) | 116 (27.6) | 11 (27.5) | |
| AB, n (%) | 31 (7.4) | 2 (5.0) | |
| O, n (%) | 128 (30.4) | 15 (37.5) | |
| Current smoking, n (%) | 174 (41.3) | 12 (30.0) | 0.163 |
| Current drinking, n (%) | 116 (27.6) | 7 (17.5) | 0.170 |
| Medical history | |||
| Hypertension, n (%) | 70 (16.6) | 3 (7.5) | 0.131 |
| Hyperlipemia, n (%) | 28 (6.7) | 0 (0.0) | 0.157 |
| Diabetes, n (%) | 85 (20.2) | 8 (20.0) | 0.977 |
| Gastrointestinal disease, n (%) | 48 (11.4) | 5 (12.5) | 0.796 |
| NYHA classification | 0.932 | ||
| II, n (%) | 1 (0.2) | 0 (0.0) | |
| III, n (%) | 18 (4.3) | 2 (5.0) | |
| IV, n (%) | 402 (95.5) | 38 (95.0) | |
| Cardiac operation, n (%) | 121 (28.7) | 17 (42.5) | 0.069 |
| Dialysis, n (%) | 4 (1.0) | 0 (0.0) | 1.000 |
| Preoperative data | |||
| RBC (×1012/L) | 4.49 (4.08-4.89) | 4.16 (3.72-4.69) | 0.004 |
| Hb (g/L) | 138.00 (122.00-149.00) | 127.50 (105.75-141.25) | 0.004 |
| WBC (×109/L) | 6.36 (4.96-8.00) | 5.97 (4.46-6.93) | 0.089 |
| PLT (×109/L) | 172.50 (138.25-221.75) | 173.00 (119.25-235.25) | 0.782 |
| albumin (g/L) | 39.50 (36.60-42.30) | 37.90 (34.90-40.30) | 0.025 |
| AST (mmol/L) | 28.00 (21.00-41.00) | 26.00 (18.25-38.00) | 0.737 |
| ALT (mmol/L) | 28.00 (18.00-46.00) | 23.50 (13.25-44.75) | 0.226 |
| TBIL (mmol/L) | 22.00 (14.20-33.50) | 27.05 (13.68-40.85) | 0.737 |
| Cr (μmol/L) | 88.65 (72.43-108.33) | 87.35 (72.65-119.78) | 0.996 |
| BUN (mmol/L) | 7.31 (5.84-9.57) | 7.55 (6.30-11.09) | 0.291 |
| TG (mmol/L) | 1.06 (0.78-1.43) | 0.95 (0.74-1.29) | 0.381 |
| LDL-C (mmol/L) | 2.14 (1.69-2.63) | 2.09 (1.61-2.76) | 0.876 |
| APTT (s) | 39.00 (36.20-43.25) | 40.60 (38.18-46.50) | 0.027 |
| INR | 1.17 (1.07-1.37) | 1.31 (1.16-1.60) | 0.003 |
| NT-proBNP (pg/mL) | 3079.15 (1471.25-6723.78) | 3930 (1310-7974) | 0.597 |
| LVEF (%) | 24.20 (20.00-29.00) | 22.20 (16.00-29.50) | 0.264 |
| Preoperative treatment | |||
| Warfarin, n (%) | 45 (10.7) | 10 (25.0) | 0.017 |
| Heparin, n (%) | 97 (23.0) | 11 (27.5) | 0.525 |
| LMWH, n (%) | 108 (25.7) | 8 (20.0) | 0.431 |
| Aspirin, n (%) | 77 (18.3) | 10 (25.0) | 0.300 |
| Clopidogrel, n (%) | 21 (5.0) | 3 (7.5) | 0.453 |
| Intubation, n (%) | 6 (1.4) | 1 (2.5) | 0.473 |
| IABP, n (%) | 6 (1.4) | 2 (5.0) | 0.147 |
| ECMO, n (%) | 7 (1.7) | 3 (7.5) | 0.047 |
| Intraoperative data | |||
| Pulmonary artery systolic pressure (mmHg) | 48.00 (34.00-61.25) | 50.00 (40.00-59.00) | 0.557 |
| Cross clamp time (min) | 30.00 (26.00-36.00) | 33.00 (26.00-43.50) | 0.087 |
| CPB time (min) | 106.00 (91.00-130.00) | 133.00 (103.50-154.75) | < 0.001 |
| Operation time (min) | 240.00 (210.00-300.00) | 300.00 (242.50-360.00) | < 0.001 |
| Postoperative data | |||
| First 24 hours of drainage (mL) | 350.00 (250.00-520.00) | 375.00 (152.50-530.00) | 0.700 |
| Intubation time (min) | 2160.00 (1401.25-3254.25) | 6210.00 (2510.25-16530.00) | < 0.001 |
| CRRT, n (%) | 48 (11.4) | 26 (65.0) | < 0.001 |
| IABP, n (%) | 161 (38.2) | 21 (52.5) | 0.078 |
| ECMO, n (%) | 17 (4.0) | 9 (22.5) | < 0.001 |
| Nasogastric tube, n (%) | 97 (23.0) | 31 (77.5) | < 0.001 |
| ICU stay (hours) | 214.00 (158.50-279.50) | 424.00 (196.00-714.00) | < 0.001 |
| Postoperative hospital stay (days) | 34.00 (26.00-46.00) | 49.00 (29.25-72.75) | 0.001 |
| In-hospital deaths | 20 (4.8) | 6 (15.0) | 0.018 |
| 30-day deaths | 28 (6.7) | 11 (27.5) | < 0.001 |
| 90-day deaths | 39 (9.3) | 20 (50.0) | < 0.001 |
| 1-year deaths | 63 (15.0) | 21 (52.5) | < 0.001 |
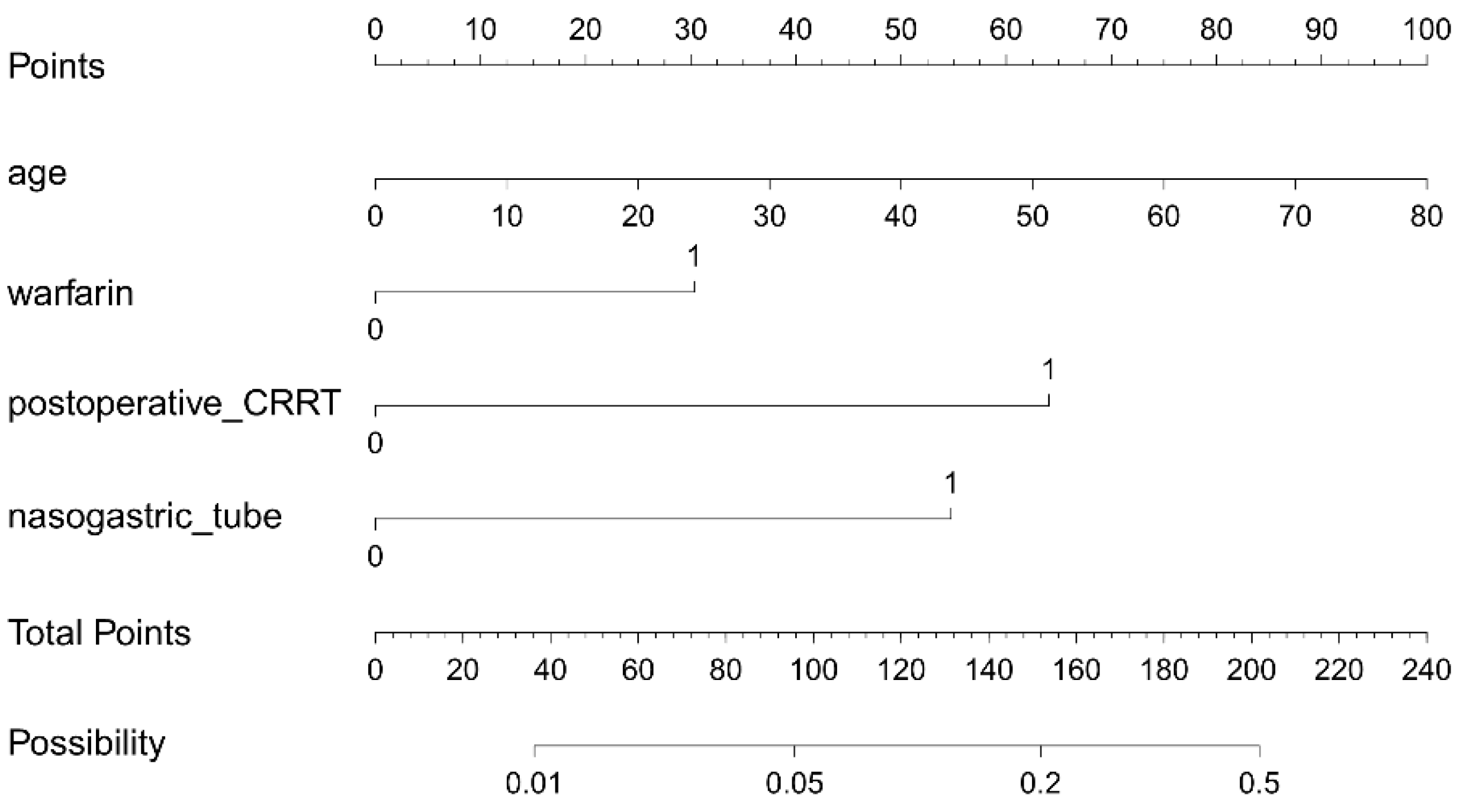
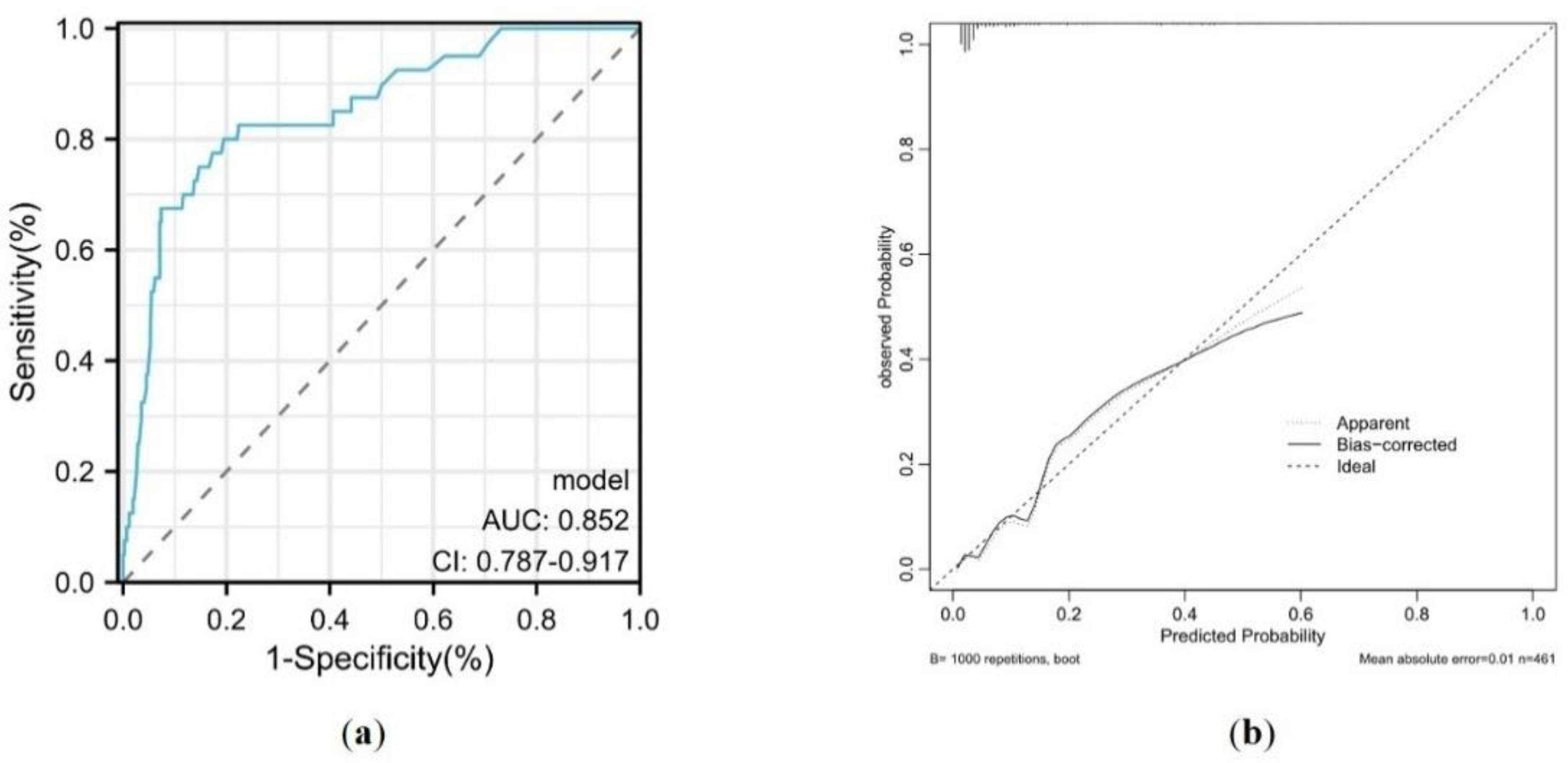
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| OR (95% CI) | P values | OR (95% CI) | P values | |
| Age | 1.04 (1.00-1.07) | 0.027 | 1.04 (1.00-1.07) | 0.037 |
| Male | 1.52 (0.73-3.17) | 0.262 | 1.11 (0.45-2.77) | 0.820 |
| BMI | 0.93 (0.85-1.02) | 0.119 | ||
| Cardiac operation | 1.92 (0.93-3.98) | 0.078 | ||
| Gastrointestinal disease | 1.11 (0.42-2.97) | 0.835 | ||
| RBC | 0.62 (0.39-0.99) | 0.046 | ||
| Hb | 0.98 (0.96-0.99) | 0.003 | ||
| WBC | 0.89 (0.77-1.03) | 0.128 | ||
| albumin | 0.93 (0.87-1.00) | 0.050 | ||
| APTT | 1.01 (0.99-1.04) | 0.244 | ||
| INR | 1.24 (0.89-1.73) | 0.197 | ||
| Preoperative warfarin | 2.79 (1.28-6.07) | 0.010 | 3.01 (1.07-8.48) | 0.037 |
| Preoperative ECMO | 4.80 (1.19-19.32) | 0.027 | 1.741 (0.34-8.94) | 0.507 |
| Cross clamp time | 1.03 (1.00-1.06) | 0.056 | 1.00 (0.96-1.04) | 0.931 |
| CPB time | 1.00 (1.00-1.01) | 0.085 | 1.00 (0.99-1.01) | 0.937 |
| Operation time | 1.01 (1.00-1.01) | 0.001 | 1.00 (0.99-1.00) | 0.362 |
| Postoperative CRRT | 14.43 (7.05-29.53) | < 0.001 | 6.27 (2.50-15.72) | < 0.001 |
| Postoperative IABP | 1.79 (0.93-3.42) | 0.081 | 0.491 (0.21-1.18) | 0.112 |
| Postoperative ECMO | 6.90 (2.84-16.75) | < 0.001 | 2.36 (0.70-7.93) | 0.164 |
| Postoperative nasogastric tube | 11.51 (5.30-25.00) | < 0.001 | 5.73 (2.10-15.66) | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





