Submitted:
29 September 2024
Posted:
01 October 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. The role of local antibacterial protection in cemented one-stage hip revision surgery
| Author | Year | Number of patients | Number of patients free from infection at follow-up | Percent of patients free from infection at follow-up | Follow-up (months) | Selection bias | Local antimicrobial protection | |||
| Min | Max | Mean | ||||||||
| Buchholz [39] | 1981 | 582 | 448 | 76.8 | 24 | 132 | No | Yes | ||
| Miley [40] | 1982 | 46 | 40 | 87 | 32 | 48.5 | Yes | Yes | ||
| Wroblewski [41] | 1986 | 102 | 93 | 91.2 | 38.8 | No | Yes | |||
| Sanzen [42] | 1988 | 102 | 77 | 75.5 | 24 | 108 | No | Yes | ||
| Raut [43] | 1995 | 57 | 49 | 86.0 | 24 | 151 | 88 | No | Yes | |
| Mulcahy [44] | 1996 | 15 | 15 | 100 | 24 | Yes | Yes | |||
| Ure [45] | 1998 | 20 | 20 | 100 | 42 | 205.2 | 118.8 | Yes | Yes | |
| Callaghan [46] | 1999 | 12 | 10 | 83.3 | 120 | Yes | Yes | |||
| Oussedik [47] | 2010 | 11 | 11 | 100 | 66 | 105.7 | 81.6 | Yes | Yes | |
| Klouche [48] | 2012 | 38 | 38 | 100 | 24 | 61 | 35 | No | No | |
| Zeller [49] | 2014 | 157 | 149 | 94.9 | 28.1 | 66.9 | 41.6 | Yes | No | |
| Jenny [50] | 2014 | 65 | 55 | 84.6 | 36 | 72 | Yes | Yes | ||
| Total | 1208 | 1005 | - | - | - | |||||
| Minimum | 11 | - | 75 | 24.0 | 61.0 | 35.0 | ||||
| Maximum | 583 | - | 100.0 | 120.0 | 205.2 | 118.8 | ||||
| Mean | 39.5 | - | 83.2 | 40.2 | 109.5 | 66.6 | ||||
| SD* | 38.8 | - | - | 27.9 | 46.9 | 30.4 | ||||
3. The role of local antibacterial protection in cementless one-stage hip revision surgery
| Author | Year | Number of patients | Number of patients free from infection at follow-up | Percent of patients free from infection at follow-up | Follow-up (months) | Selection bias | Local antimicrobial protection | ||
| Min | Max | Mean | |||||||
| Garcia [56] | 2004 | 7 | 7 | 100 | 24 | No | No | ||
| Rudelli [57] | 2008 | 32 | 30 | 93.8 | 63 | 183 | 103 | Not reported | No |
| Winkler [58] | 2008 | 37 | 34 | 91.9 | 24 | 96 | 52.8 | Yes | Antibiotic-loaded allografts |
| Yoo [59] | 2009 | 12 | 10 | 83.3 | 39.6 | 135.6 | 86.4 | Yes | No |
| Wolf [60] | 2014 | 37 | 21 | 56.8 | 24 | No | No | ||
| Bori [61] | 2014 | 24 | 23 | 95.8 | 25 | 94 | 45 | Yes | No |
| Li [62] | 2015 | 6 | 6 | 100.0 | 78 | 187.2 | 103.2 | Yes | No |
| Born [63] | 2016 | 28 | 28 | 100.0 | 24 | 180 | 84 | Yes | No |
| Ebied [64] | 2016 | 33 | 32 | 97.0 | 48 | 96 | 60 | Yes | Antibiotic-loaded allografts |
| Whiteside [65] | 2017 | 21 | 20 | 95.2 | 25 | 157 | 63 | No | Intra-articular antibiotic infusion |
| Lange [66] | 2018 | 56 | 51 | 91.1 | 24 | 48 | No | Gentamicin collagen fleece | |
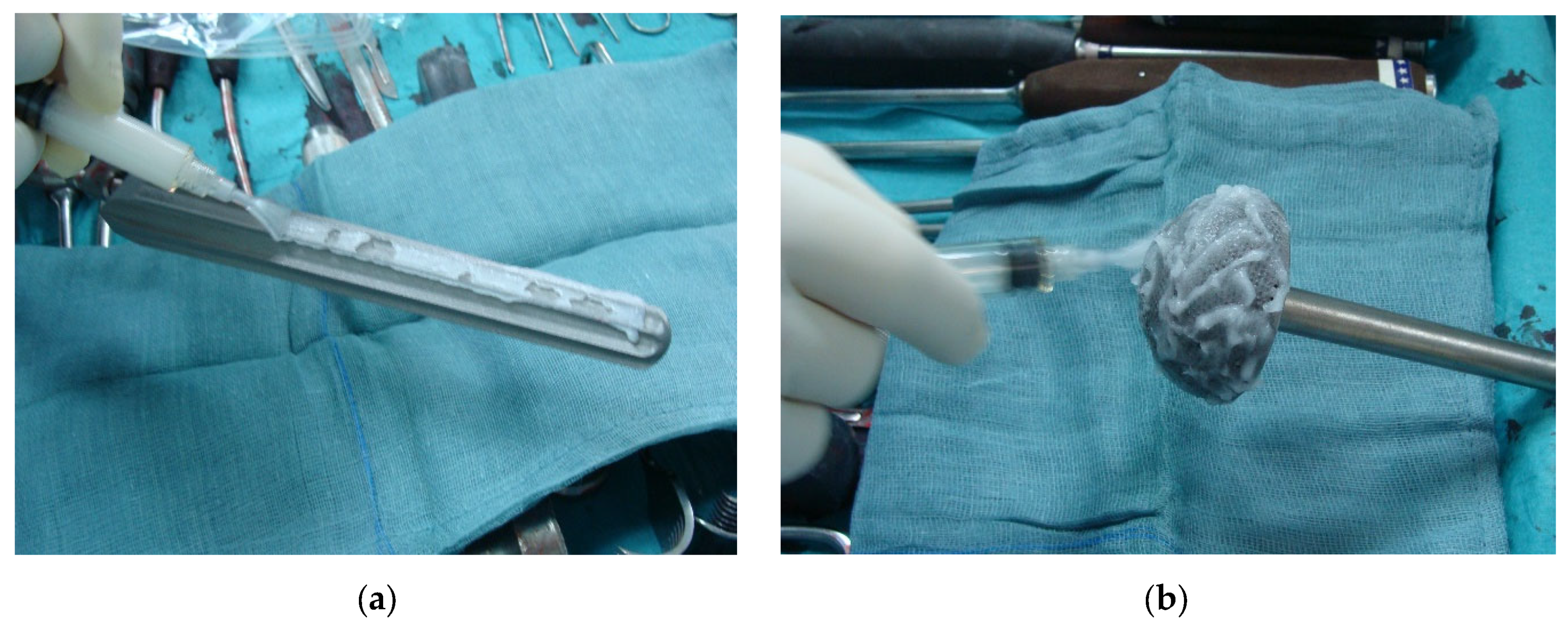
| Capuano [67] | 2018 | 5 | 5 | 100.0 | 24 | 36 | 29.3 | No | Antibiotic-loaded hydrogel coating |
| Ji [68] | 2019 | 111 | 99 | 89.2 | 24 | 107 | 58 | No | Vancomicin or Imipenem powder and intra-articular antibiotic infusion |
| Pellegrini [69] | 2021 | 10 | 10 | 100.0 | 24 | 60 | 37.2 | Yes | Antibiotic-loaded hydrogel coating |
| Ji [70] | 2022 | 29 | 26 | 89.7 | 24 | 133 | 85 | No | Intra-articular antibiotic infusion |
| Dersch [71] | 2022 | 38 | 35 | 92.1 | 24 | 187.2 | 67.2 | Yes | Antibiotic-loaded allografts |
| Mangin [72] | 2023 | 35 | 32 | 91.4 | 24 | 132 | 60 | Yes | No |
| Total | 521 | 469 | - | - | - | ||||
| Minimum | 5 | - | 56.8 | 24.0 | 36.0 | 29.3 | |||
| Maximum | 111 | - | 100.0 | 78 | 187.2 | 103.2 | |||
| Mean | 30.6 | - | 90.0 | 31.9 | 127.4 | 65.5 | |||
| SD* | 25.0 | - | - | 16.2 | 48.4 | 22.5 | |||
| Local antibacterial protection | Number of patients | Number of patients free from infection at follow-up | Percent of patients free from infection at follow-up (mean, min, max) | Follow-up (months) (mean and SD*) |
|---|---|---|---|---|
| None [56,57,59,60,61,62,63,72] | 181 | 157 | 86.7 (56.8-100) | 80.3 ± 23.4 |
| Intra-articular antibiotic infusion or local antibiotic vancomicin powder [65,68,70] | 161 | 145 | 90.1 (89.2-95.2) | 68.7 ± 14.4 |
| Gentamicin-loaded collagen fleece [66] | 56 | 51 | 91.1 | 48 |
| Antibiotic-loaded allografts [58,64,71] | 108 | 101 | 93.5 (91.9-92.1) | 60.0 ± 7.2 |
| Antibiotic-loaded hydrogel coating [67,69] | 15 | 15 | 100.0 | 30.1 ± 6.8 |
3. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Dobson PF, Reed MR. Prevention of infection in primary THA and TKA. EFORT Open Rev. 2020 Oct 26;5(10):604-613. [CrossRef]
- Day CW, Costi K, Pannach S, Atkins GJ, Hofstaetter JG, Callary SA, Nelson R, Howie DW, Solomon LB. Long-Term Outcomes of Staged Revision Surgery for Chronic Periprosthetic Joint Infection of Total Hip Arthroplasty. J Clin Med. 2021 Dec 27;11(1):122. [CrossRef]
- Lenguerrand E, Whitehouse MR, Beswick AD, Kunutsor SK, Webb JCJ, Mehendale S, Porter M, Blom AW; National Joint Registry for England, Wales, Northern Ireland, the Isle of Man, and the States of Guernsey. Mortality and re-revision following single-stage and two-stage revision surgery for the management of infected primary hip arthroplasty in England and Wales. Bone Joint Res. 2023 May 9;12(5):321-330. [CrossRef]
- Blom AW, Lenguerrand E, Strange S, Noble SM, Beswick AD, Burston A, Garfield K, Gooberman-Hill R, Harris SRS, Kunutsor SK, Lane JA, MacGowan A, Mehendale S, Moore AJ, Rolfson O, Webb JCJ, Wilson M, Whitehouse MR; INFORM trial group. Clinical and cost effectiveness of single stage compared with two stage revision for hip prosthetic joint infection (INFORM): pragmatic, parallel group, open label, randomised controlled trial. BMJ. 2022 Oct 31;379:e071281. [CrossRef]
- Svensson K, Rolfson O, Kärrholm J, Mohaddes M. Similar Risk of Re-Revision in Patients after One- or Two-Stage Surgical Revision of Infected Total Hip Arthroplasty: An Analysis of Revisions in the Swedish Hip Arthroplasty Register 1979⁻2015. J Clin Med. 2019 Apr 10;8(4):485. [CrossRef]
- George DA, Logoluso N, Castellini G, Gianola S, Scarponi S, Haddad FS, Drago L, Romano CL. Does cemented or cementless single-stage exchange arthroplasty of chronic periprosthetic hip infections provide similar infection rates to a two-stage? A systematic review. BMC Infect Dis. 2016 Oct 10;16(1):553. [CrossRef]
- Zahar A, Gehrke TA. One-Stage Revision for Infected Total Hip Arthroplasty. Orthop Clin North Am. 2016 Jan;47(1):11-8. [CrossRef]
- Buchholz HW, Elson RA, Heinert K. Antibiotic-loaded acrylic cement: current concepts. Clin Orthop Relat Res. :1984: 96–108.
- Wroblewski BM. One-stage revision of infected cemented total hip arthroplasty. Clin Orthop Relat Res. :1986: 103–107.
- Zeller V, Lhotellier L, Marmor S, Leclerc P, Krain A, Graff W, Ducroquet F, Biau D, Leonard P, Desplaces N, Mamoudy P. One-stage exchange arthroplasty for chronic periprosthetic hip infection: results of a large prospective cohort study. J Bone Joint Surg Am. 2014;96:e1. [CrossRef]
- Callaghan JJ, Katz RP, Johnston RC. One-stage revision surgery of the infected hip. A minimum 10-year followup study. Clin Orthop Relat Res. :1999: 139–143. [CrossRef]
- Ure KJ, Amstutz HC, Nasser S, Schmalzried TP (1998) Direct exchange arthroplasty for the treatment of infection after total hip replacement. An average ten-year follow-up. J Bone Joint Surg Am 80:961–968.
- Gehrke T, Zahar A, Kendoff D. One-stage exchange: it all began here. Bone Joint J. 2013;95-B:77–83.
- Lum ZC, Holland CT, Meehan JP. Systematic review of single stage revision for prosthetic joint infection. World J Orthop. 2020 Dec 18;11(12):559-572. [CrossRef]
- Gehrke T, Kendoff D. Peri-prosthetic hip infections: in favour of one-stage. Hip Int. 2012;22 Suppl 8:S40–S45. [CrossRef]
- Luu, A., Syed, F., Raman, G., Bhalla, A., Muldoon, E., Hadley, S., et al. (2013). Two-stage arthroplasty for prosthetic joint infection: a systematic review of acute kidney injury, systemic toxicity and infection control. J. Arthroplasty 149, e1. [CrossRef]
- Salvati, E. A., Callaghan, J. J., Brause, B. D., Klein, R. F., and Small, R. D. (1986). Reimplantation in infection. elution of gentamicin from cement and beads. Clin. Orthop. Relat. Res. 83–93.
- Walenkamp, G. H. (2007). “Antibiotic loaded cement: from research to clinical evidence,” in Infection and Local Treatment in Orthopedic Surgery, ed. E. Meani (Berlin: Springer), 170–175. [CrossRef]
- Sanz-Ruiz, P., Villanueva-Martinez, M., and Berberich, C. (2018b). “Benefit and risks of anti biotic-loaded bone cements,” in Management of Periprosthetic Joint Infection, ed. D. Kuhn (Heidelberg: Springer-Verlag), 217–218.
- Kendoff DO, Gehrke T, Stangenberg P, Frommelt L, Bösebeck H. Bioavailability of gentamicin and vancomycin released from an antibiotic containing bone cement in patients undergoing a septic one-stage total hip arthroplasty (THA) revision: a monocentric open clinical trial. Hip Int. 2016 Jan-Feb;26(1):90-6. [CrossRef]
- Miclau, T., Edin, M. L., Lester, G. E., Lindsey, R. W., and Dahners, L. E. (1995). Bone toxicity of locally applied aminoglycosides. J. Orthop. Trauma 9, 401–406. [CrossRef]
- Edin, M. L., Miclau, T., Lester, G. E., Lindsey, R. W., and Dahners, L. E. (1996). Effect of cefazolin and vancomycin on osteoblasts in vitro. Clin. Orthop. Relat. Res. 333, 245–251. [CrossRef]
- Isefuku, S., Joyner, C. J., and Simpson, A. H. (2003). Gentamicin may have an adverse effect on osteogenesis. J. Orthop. Trauma. 17, 212–216. [CrossRef]
- Hansen, E. N., Adeli, B., Kenyon, R., and Parvizi, J. (2014). Routine use of antibiotic laden bone cement for primary total knee arthroplasty: impact on infecting microbial patterns and resistance profiles. J. Arthroplasty. 29, 1123–1127. [CrossRef]
- Tootsi K, Heesen V, Lohrengel M, Enz AE, Illiger S, Mittelmeier W, Lohmann CH. The use of antibiotic-loaded bone cement does not increase antibiotic resistance after primary total joint arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022 Sep;30(9):3208-3214. [CrossRef]
- Schmitt DR, Killen C, Murphy M, Perry M, Romano J, Brown N. The Impact of Antibiotic-Loaded Bone Cement on Antibiotic Resistance in Periprosthetic Knee Infections. Clin Orthop Surg. 2020 Sep;12(3):318-323. [CrossRef]
- Sabater-Martos M, Verdejo MA, Morata L, Muñoz-Mahamud E, Guerra-Farfan E, Martinez-Pastor JC, Soriano A. Antimicrobials in polymethylmethacrylate: from prevention to prosthetic joint infection treatment: basic principles and risk of resistance. Arthroplasty. 2023 Mar 2;5(1):12. [CrossRef]
- Xu T, Wu KL, Jie K. Comprehensive meta-analysis of antibiotic-impregnated bone cement versus plain bone cement in primary total knee arthroplasty for preventing periprosthetic joint infection. Chin J Traumatol. 2022 Nov;25(6):325-330. [CrossRef]
- Opalko M, Bösebeck H, Vogt S. Properties and clinical application safety of antibiotic-loaded bone cement in kyphoplasty. J Orthop Surg Res. 2019 Jul 27;14(1):238. [CrossRef]
- Blersch BP, Sax FH, Mederake M, Benda S, Schuster P, Fink B. Effect of Multiantibiotic-Loaded Bone Cement on the Treatment of Periprosthetic Joint Infections of Hip and Knee Arthroplasties-A Single-Center Retrospective Study. Antibiotics (Basel). 2024 Jun 3;13(6):524. [CrossRef]
- van Vugt TAG, Arts JJ, Geurts JAP. Antibiotic-Loaded Polymethylmethacrylate Beads and Spacers in Treatment of Orthopedic Infections and the Role of Biofilm Formation. Front Microbiol. 2019 Jul 25;10:1626. [CrossRef]
- Langlais F. Ciments orthopédiques aux antibiotiques: du laboratoire a la validation clinique [Antibiotic-loaded bone cements: from laboratory studies clinical evaluation]. Bull Acad Natl Med. 2004;188(6):1011-22.
- Cara A, Ferry T, Laurent F, Josse J. Prophylactic Antibiofilm Activity of Antibiotic-Loaded Bone Cements against Gram-Negative Bacteria. Antibiotics (Basel). 2022 Jan 21;11(2):137. [CrossRef]
- Nijhof MW, Stallmann HP, Vogely HC, Fleer A, Schouls LM, Dhert WJ, Verbout AJ. Prevention of infection with tobramycin-containing bone cement or systemic cefazolin in an animal model. J Biomed Mater Res. 2000 Dec 15;52(4):709-15.
- Nijhof MW, Fleer A, Hardus K, Vogely HC, Schouls LM, Verbout AJ, Dhert WJ. Tobramycin-containing bone cement and systemic cefazolin in a one-stage revision. Treatment of infection in a rabbit model. J Biomed Mater Res. 2001;58(6):747-53. [CrossRef]
- Jenny JY, Hamon M, Klein S, Reiter-Schatz A, Rondé-Oustau C, Boéri C, Wisniewski S, Gaudias J. Cement Loaded With High-Dose Gentamicin and Clindamycin Reduces the Risk of Subsequent Infection After One-Stage Hip or Knee Arthroplasty Exchange for Periprosthetic Infection: A Preliminary Study. J Arthroplasty. 2021 Dec;36(12):3973-3978. [CrossRef]
- Szymski D, Walter N, Krull P, Melsheimer O, Lang S, Grimberg A, Alt V, Steinbrück A, Rupp M. The Prophylactic Effect of Single vs. Dual Antibiotic-Loaded Bone Cement against Periprosthetic Joint Infection Following Hip Arthroplasty for Femoral Neck Fracture: An Analysis of the German Arthroplasty Registry. Antibiotics (Basel). 2023 Apr 8;12(4):732. [CrossRef]
- Sprowson A.P., Jensen C., Chambers S., Parsons N.R., Aradhyula N.M., Carluke I., Inman D., Reed M.R. The Use of High-Dose Dual-Impregnated Antibiotic-Laden Cement with Hemiarthroplasty for the Treatment of a Fracture of the Hip. Bone Jt. J. 2016;98-B:1534–1541. [CrossRef]
- Buchholz H, Elson R, Engelbrecht E, Lodenkamper H, Rottger J, Siegel A: Management of deep infection of total hip replacement. J Bone Joint Surg 1981, 63-B(3):342-353.
- Miley GB, Scheller AD, Turner RH: Medical and surgical treatment of the septic hip with one-stage revision arthroplasty. Clin Orthop Relat Res 1982, 170(76-82).
- Wroblewski BM. One-stage revision of infected cemented total hip arthroplasty. Clin Orthop Relat Res. 1986 Oct;(211):103-7. [CrossRef]
- Sanzen L, Carlsson A, Josefsson G, Lindberg LT: Revision operations on infected total hip arthroplasties. Clin Orthop Relat Res 1988, 229:165-172.
- Raut VV, Siney PD, Wroblewski BM. One-stage revision of infected total hip replacements with discharging sinuses. J Bone Joint Surg Br. 1994 Sep;76(5):721-4.
- Mulcahy DM, O’Byrne JM, Fenelon GE. One stage surgical management of deep infection of total hip arthroplasty. Ir J Med Sci. 1996 Jan-Mar;165(1):17-9. [CrossRef]
- Ure KJ, Amstutz HC, Nasser S, Schmalzried TP. Direct-exchange arthroplasty for the treatment of infection after total hip replacement. An average ten-year follow-up. J Bone Joint Surg Am. 1998;80:961–968. [CrossRef]
- Callaghan JJ, Katz RP, Johnston RC. One-stage revision surgery of the infected hip. A minimum 10-year followup study. Clin Orthop Relat Res 1999 Dec;369: 139-43. [CrossRef]
- Oussedik SI, Dodd MB, Haddad FS: Outcomes of revision total hip replacement for infection after grading according to a standard protocol. J Bone Joint Surg 2010, 92-B(9):1222-1226.
- Klouche S1, Leonard P, Zeller V, Lhotellier L, Graff W, Leclerc P, Mamoudy P, Sariali E. Infected total hip arthroplasty revision: one- or two-stage procedure? Orthop Traumatol Surg Res. 2012 Apr;98(2):144-50. Epub 2012 Feb 24. [CrossRef]
- Zeller V, Lhotellier L, Marmor S, Leclerc P, Krain A, Graff W, Ducroquet F, Biau D, Leonard P, Desplaces N, Mamoudy P. One-stage exchange arthroplasty for chronic periprosthetic hip infection: results of a large prospective cohort study. J Bone Joint Surg Am. 2014 Jan 1;96(1):e1. [CrossRef]
- Jenny JY, Lengert R, Diesinger Y, Gaudias J, Boeri C, Kempf JF. Routine one-stage exchange for chronic infection after total hip replacement. Int Orthop. 2014 Dec;38(12):2477-81. [CrossRef]
- Marmor S, Kerroumi Y, Meyssonnier V, Lhotellier L, Mouton A, Graff W, Zeller V. One-Stage Exchange Arthroplasty for Fistulizing Periprosthetic Joint Infection of the Hip: An Effective Strategy. Front Med (Lausanne). 2020 Oct 16;7:540929. [CrossRef]
- Parvizi J, Gehrke T, Chen AF. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Joint J. 2013 Nov;95-B(11):1450-2. [CrossRef]
- Manning L, Bori G, Klement MR. Does the Use of Cemented or Cementless Components at the Time of Reimplantation Affect the Success of Treating Chronic Periprosthetic Joint Infections (pjis)? If Yes, What Is the Optimal Antibiotic(s), Dosage and Cement to Maximize Antibiotic Delivery and Mechanical Properties of the Cement? International Consensus Meeting (icm) on Orthopaedic Infections. (2018). Available online at: https://icmphilly.com/questions/does-the-use-of-cemented-or-cementless-components-at-the-time-of-reimplantation-affect-the-success-of-treating-chronic-periprosthetic-joint-infections-pjis-if-yes-what-is-the-optimal-antibiotic/ (accessed 2024).
- Scanlon CM, Gemayel AC, Buehring W, Slover JD, Malchau H. Are current rates of uncemented fixation in total hip arthroplasty supported by the literature? An update on the uncemented paradox. Hip Int. 2024 May 3:11207000241249673. [CrossRef]
- Elbardesy H, Anazor F, Mirza M, Aly M, Maatough A. Cemented versus uncemented stems for revision total hip replacement: A systematic review and meta-analysis. World J Orthop. 2023 Aug 18;14(8):630-640. [CrossRef]
- García S, Soriano A, Esteban P, Almela M, Gallart X, Mensa J. Utilidad de la adición de antibiótico al cemento en el recambio en 1 tiempo en la infección crónica de una prótesis total de cadera [Usefulness of adding antibiotic to cement in one stage exchange of chronic infection in total hip arthroplasty]. Med Clin (Barc). 2005 Jun 25;125(4):138-9.
- Rudelli S, Uip D, Honda E, Lima AL. One-stage revision of infected total hip arthroplasty with bone graft. J Arthroplasty 2008;23(8):1165-77. [CrossRef]
- Winkler H, Stoiber A, Kaudela K, Winter F, Menschik F. One stage uncemented revision of infected total hip replacement using cancellous allograft bone impregnated with antibiotics. J Bone Joint Surg Br 2008;90(12):1580-4. [CrossRef]
- Yoo JJ, Kwon YS, Koo KH, Yoon KS, Kim YM, Kim HJ. One-stage cementless revision arthroplasty for infected hip replacements. Int Orthop. 2009;33(5):1195-1201. [CrossRef]
- Wolf M, Clar H, Friesenbichler J, et al. Prosthetic joint infection following total hip replacement: results of one-stage versus two-stage exchange. Int Orthop 2014;38(7):1363–1368. [CrossRef]
- Bori G, Muñoz-Mahamud E, Cuñé J, Gallart X, Fuster D, Soriano A. One-Stage Revision Arthroplasty Using Cementless Hip Arthroplasties. J Arthroplasty 2014;29:1076–1081.
- Li P, Hou M, Zhu ZQ, Shi ZJ. Cementless Revision for Infected Hip Arthroplasty: an 8.6 Years Follow-up. Orthopaedic surgery. 2015;7(1):37-42. [CrossRef]
- Born P, Ilchmann T, Zimmerli W, Zwicky L, Graber P, Ochsner PE, Clauss M. Eradication of infection, survival, and radiological results of uncemented revision stems in infected total hip arthroplasties. Acta Orthop. 2016 Dec;87(6):637-643. [CrossRef]
- Ebied AM, Elseedy AI, Gamal O. Single-stage revision for periprosthetic hip infection using antibiotic loaded impaction graft. Hip Int. 2016 Nov 10;26(6):573-579. [CrossRef]
- Whiteside LA, Roy ME. One-stage Revision With Catheter Infusion of Intraarticular Antibiotics Successfully Treats Infected THA. Clin Orthop Relat Res. 2017 Feb;475(2):419-429. [CrossRef]
- Lange J, Troelsen A, Solgaard S, Otte KS, Jensen NK, Søballe K; CORIHA Research Group. Cementless One-Stage Revision in Chronic Periprosthetic Hip Joint Infection. Ninety-One Percent Infection Free Survival in 56 Patients at Minimum 2-Year Follow-Up. J Arthroplasty. 2018 Apr;33(4):1160-1165.e1. [CrossRef]
- Capuano N, Logoluso N, Gallazzi E, Drago L, Romanò CL. One-stage exchange with antibacterial hydrogel coated implants provides similar results to two-stage revision, without the coating, for the treatment of peri-prosthetic infection. Knee Surg Sports Traumatol Arthrosc. 2018 Nov;26(11):3362-3367. [CrossRef]
- Ji B, Wahafu T, Li G, Zhang X, Wang Y, Momin M, Cao L. Single-stage treatment of chronically infected total hip arthroplasty with cementless reconstruction: results in 126 patients with broad inclusion criteria. Bone Joint J. 2019 Apr;101-B(4):396-402.
- Pellegrini A, Legnani C. High rate of infection eradication following cementless one-stage revision hip arthroplasty with an antibacterial hydrogel coating. Int J Artif Organs. 2022 Jan;45(1):113-117. [CrossRef]
- Ji B, Li G, Zhang X, Xu B, Wang Y, Chen Y, Cao L. Effective single-stage revision using intra-articular antibiotic infusion after multiple failed surgery for periprosthetic joint infection : a mean seven years’ follow-up. Bone Joint J. 2022 Jul;104-B(7):867-874.
- Dersch G, Winkler H. Periprosthetic Joint Infection (PJI)-Results of One-Stage Revision with Antibiotic-Impregnated Cancellous Allograft Bone-A Retrospective Cohort Study. Antibiotics (Basel). 2022 Feb 25;11(3):310. [CrossRef]
- Mangin M, Aouzal Z, Leclerc G, Sergent AP, Bouiller K, Patry I, Garbuio P. One-stage revision hip arthroplasty for infection using primary cementless stems as first-line implants: About 35 cases. Orthop Traumatol Surg Res. 2023 Nov;109(7):103642. [CrossRef]
- Hansen E, Tetreault M, Zmistowski B, Della Valle CJ, Parvizi J, Haddad FS, Hozack WJ. Outcome of one-stage cementless exchange for acute postoperative periprosthetic hip infection. Clin Orthop Relat Res. 2013 Oct;471(10):3214-22. [CrossRef]
- Riemer K, Lange J. Early periprosthetic hip joint infection managed by cementless one-stage revision - a case series. J Bone Jt Infect. 2022 Feb 25;7(1):43-50. [CrossRef]
- Thakrar RR, Horriat S, Kayani B, Haddad FS. Indications for a single-stage exchange arthroplasty for chronic prosthetic joint infection: a systematic review. Bone Joint J. 2019 Jan;101-B(1_Supple_A):19-24.
- Lum ZC, Holland CT, Meehan JP. Systematic review of single stage revision for prosthetic joint infection. World J Orthop. 2020 Dec 18;11(12):559-572. [CrossRef]
- Carlsson AS, Josefsson G, Lindberg L. Revision with gentamicin-impregnated cement for deep infections in total hip arthroplasties. J Bone Joint Surg Am. 1978;60(8):1059–1064. [CrossRef]
- Wall V, Nguyen TH, Nguyen N, Tran PA. Controlling Antibiotic Release from Polymethylmethacrylate Bone Cement. Biomedicines. 2021 Jan 1;9(1):26. [CrossRef]
- Macaulay W, DiGiovanni CW, Restrepo A, Saleh KJ, Walsh H, Crossett LS, Peterson MG, Li S, Salvati EA. Differences in bone-cement porosity by vacuum mixing, centrifugation, and hand mixing. J Arthroplasty. 2002 Aug;17(5):569-75. [CrossRef]
- Gálvez-López R, Peña-Monje A, Antelo-Lorenzo R, Guardia-Olmedo J, Moliz J, Hernández-Quero J, Parra-Ruiz J. Elution kinetics, antimicrobial activity, and mechanical properties of 11 different antibiotic loaded acrylic bone cement. Diagn Microbiol Infect Dis. 2014 Jan;78(1):70-4. [CrossRef]
- Bertazzoni Minelli E, Della Bora T, Benini A. Different microbial biofilm formation on polymethylmethacrylate (PMMA) bone cement loaded with gentamicin and vancomycin. Anaerobe. 2011 Dec;17(6):380-3. [CrossRef]
- Ensing GT, van Horn JR, van der Mei HC, Busscher HJ, Neut D. Copal bone cement is more effective in preventing biofilm formation than Palacos R-G. Clin Orthop Relat Res. 2008 Jun;466(6):1492-8. [CrossRef]
- Ul Haq I, Khan TA, Krukiewicz K. Etiology, pathology, and host-impaired immunity in medical implant-associated infections. J Infect Public Health. 2024 Feb;17(2):189-203. [CrossRef]
- Lu Y, Cai WJ, Ren Z, Han P. The Role of Staphylococcal Biofilm on the Surface of Implants in Orthopedic Infection. Microorganisms. 2022 Sep 26;10(10):1909. [CrossRef]
- Akay S, Yaghmur A. Recent Advances in Antibacterial Coatings to Combat Orthopedic Implant-Associated Infections. Molecules. 2024 Mar 6;29(5):1172. [CrossRef]
- Onorato F, Masoni V, Gagliardi L, Comba LC, Rivera F. What to Know about Antimicrobial Coatings in Arthroplasty: A Narrative Review. Medicina (Kaunas). 2024 Mar 30;60(4):574. [CrossRef]
- Jamsen E, Stogiannidis J, Malmivaara A, Pajamaki J, Puolakka T, Konttinen YT. Outcome of prosthesis exchange for infected knee arthroplasty: the effect of treatment approach. A systematic review of the literature. Acta Orthopaedica 2009;80(1):67–77. [CrossRef]
- Romanò CL, Malizos K, Capuano N, Mezzoprete R, D’Arienzo M, Van Der Straeten C, Scarponi S, Drago L. Does an Antibiotic-Loaded Hydrogel Coating Reduce Early Post-Surgical Infection After Joint Arthroplasty? J Bone Jt Infect. 2016 Jul 19;1:34-41.
- Malizos K, Blauth M, Danita A, Capuano N, Mezzoprete R, Logoluso N, Drago L, Romanò CL. Fast-resorbable antibiotic-loaded hydrogel coating to reduce post-surgical infection after internal osteosynthesis: a multicenter randomized controlled trial. J Orthop Traumatol. 2017 Jun;18(2):159-169. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





