1. Introduction
Colonic malignancy can lead to lower digestive tract obstruction in 10-19% of the cases [
1,
2]. Surgery has traditionally been the treatment of choice for acute bowel obstruction due to colonic malignancy. As emergency surgery has been identified as an independent risk factor for mortality by the French Association of Surgeons (AFC) [
1,
3], other treatment methods have been proposed, such as endoscopic treatment using a self-expanding metal stent (SEMS) [
7]. The choice of the surgical approach for obstructive colon cancer depends on the location and stage of the tumor, the general condition of the patient and the experience of the surgeon [
1]. Our aim is to highlight the incidence of colonic malignancy as a cause of bowel obstruction and to compare the treatment options in a regional General Hospital of Greece, with the international literature.
2. Materials and Methods
In this retrospective study, a sample of 197 patients, who underwent emergency surgery from January 2012 to July 2022, at the General Hospital of Katerini in Greece, due to bowel obstruction, was studied. We excluded from our research all these cases, that the indication for the surgery was a kind of complication of bowel obstruction, such as perforation at the site of the tumor or proximally (presence of free air on radiological control) or the formation of an abscess or inflammation.
The initial categorization was done with the help of Google Forms® (structured questionnaire with closed type questions) and the Microsoft Excel® program. The patients were initially classified based on their gender, the date of surgery, their age group (with ages ranging from 26 to 92 years) and the etiology of the bowel obstruction. From the sample of patients studied, a total of 197 cases of patients, that met the inclusion criteria, emerged. Initially, the patients were divided based on the cause of the obstruction. From the sample of 197 patients, in 73 (37%) the cause of the obstruction was colonic malignancy. Other causes were adhesions (43%), small bowel malignancy (3%), various hernias (13%) and inflammation (3%).
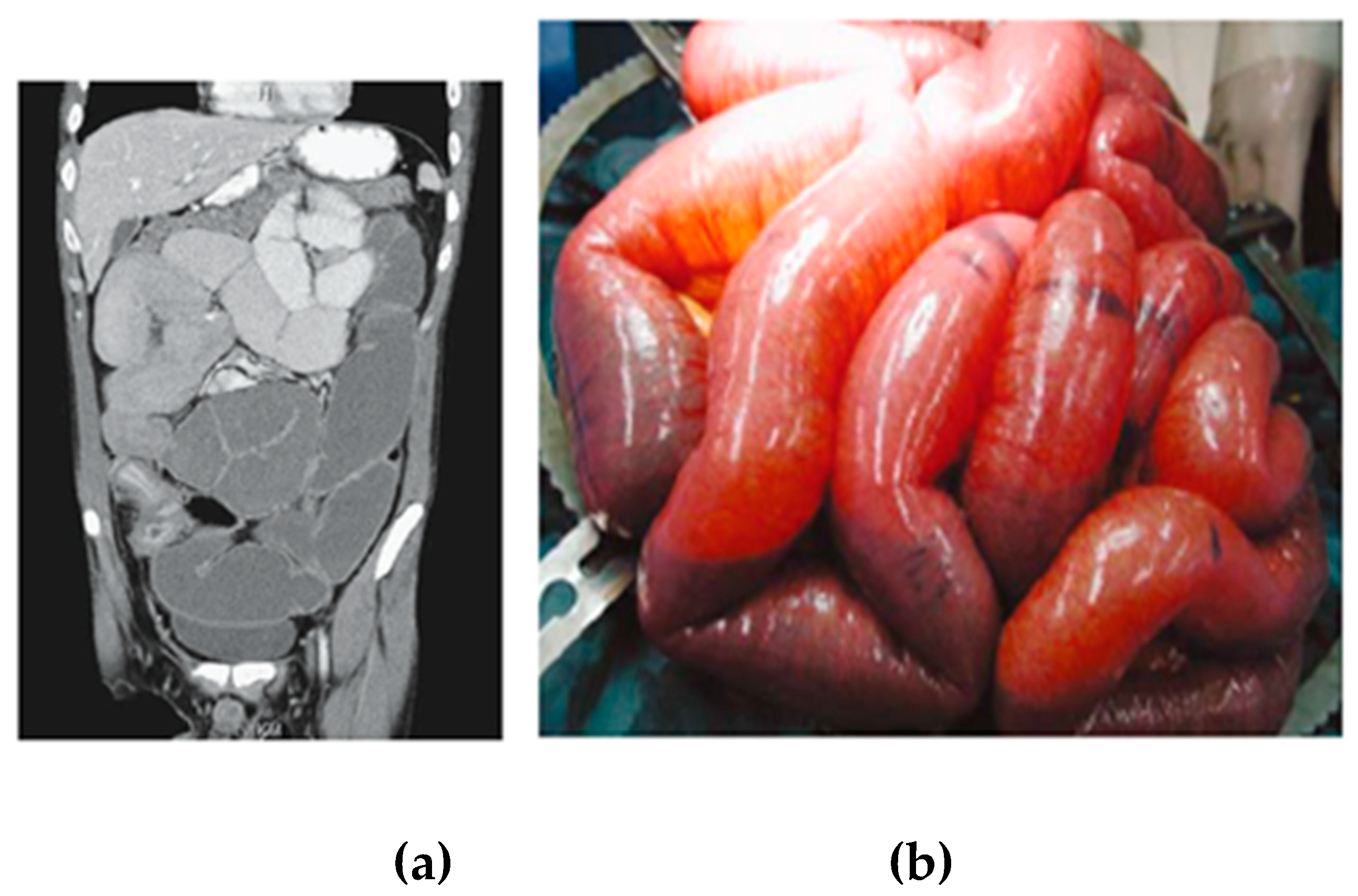
Figure 1.
Cases of obstructive colonic malignancy from our clinic’s archive (a) Computer tomography scan (b) Intraoperative image showing the small bowel dilation due to the colonic malignancy.
Figure 1.
Cases of obstructive colonic malignancy from our clinic’s archive (a) Computer tomography scan (b) Intraoperative image showing the small bowel dilation due to the colonic malignancy.
Our study was then focused on the cases where the cause of the obstruction was colon cancer, that is the 73 patients. Out of these, 39 (53%) were male and 34 (47%) female. The youngest patient was 43 years old and the oldest 92 years old, while the average age of the patients was 75 years. A further classification was then conducted based on the tumor location, with the most frequent location being in the sigmoid colon (30%) and rectum (22%). A correlation was then made between the type of operation chosen, tumor resection with or without a prophylactic stoma installation or a simple installation of a diverting stoma, and the tumor location. We also calculated if there is a variation in surgical management and the percentage of tumor resection depending on the year of the operation, throughout the decade. In addition, the surgical management in cases of generalized peritoneal carcinomatosis was further studied and a total of 20 patients with peritoneal implants at the time of surgery, aged from 76 to 92 years, emerged. For these patients, the type of the operation chosen and the resection or not of the primary tumor, was also calculated and evaluated.
3. Results
Our research concluded that colonic malignancy was a frequent cause of emergency surgery at the General Hospital of Katerini (37% of the patients in our research), a much higher percentage compared to what is described by the international literature (10-19%). This fact could perhaps be justified by the lack of preventive endoscopic control in the district’s population.We found that resection was performed in 46 (63%) patients, while in the remaining 27 a diverting stoma was installed, without resection of the primary tumor. (
Table 1).
Of those who underwent tumor resection, 29 (63%) underwent resection and anastomosis in primary time, while 17 (36%) underwent Hartmann's operation. Out of all the patients who underwent resection and anastomosis, in 10 a prophylactic ileostomy was installed. In particular, the following operations were carried out:
• 13 right colectomies with anastomosis in primary time and prophylactic ileostomies in 3 of them,
• 4 left colectomies with anastomosis in primary time and a prophylactic ileostomy in one of them,
• 2 subtotal colectomies with anastomosis in primary time and a prophylactic ileostomy in one of them,
• 4 sigmoid colon resections with anastomosis in primary time and a prophylactic ileostomy in one of them,
• 4 transverse colon resections with anastomosis in primary time and prophylactic ileostomies in 2 of them and
• 2 low anterior resections with anastomosis in primary time with prophylactic ileostomies in both of them.
In total, we had 29 tumor resections and anastomosis in primary time with prophylactic ileostomies in 10 of them.
Hartmann's operation was chosen only in cases of cancer of the left colon, specifically in 14 cases of sigmoid cancer, 2 cases rectum cancer and 1 case of cancer of the descending colon. In cases where resection of the primary tumor was not performed, the installation of some type of diverting stoma was chosen. Specifically, 12 diverting transverse colostomies, 11 diverting ileostomies and 4 diverting sigmoid colostomies, were installed, with most cases involving patients with left colon cancer. In total, therefore, of the 73 patients, 17 ended up with a Hartmann's stoma, 27 with a simple diverting stoma and 10 with and anastomosis and a prophylactic stoma, that is we had 54 stomas in total (73% of patients ending up with a stoma after surgery). No particular difference was observed between men and women regarding the stoma installation, while it seems that most cases were between the ages of 76-85 years.
Based on the international literature, obstruction of the left colon is more common than the right, as the intraluminal diameter of the colon is the narrowest between the splenic flexure and the rectosigmoid junction. This is confirmed by the results of our research, from which it appears that the most frequent cause of obstructive cancer, which led patients to surgery, was in the sigmoid and rectum, and then in the ascending colon and cecum.
Depending on the location of the tumor, we observed a variation in the choice of operation per case (
Table 2). In particular, we observed that resection of the tumor was highest in the cases of sigmoid colonic malignancy and lowest in the cases of rectal malignancy. Regarding the installation of a prophylactic diverting stoma after an excision and anastomosis, it seems that it is the preference of the surgeons of the General Hospital of Katerini to install a prophylactic diverting stoma in patients with left colectomies and anastomosis, in relation to those with right colectomies and ileo-transverse anastomosis. This fact is in line with the provisions of the international literature, where prophylactic ileostomy in ileocolic anastomoses is recommended less often and in specific cases. Hartmann's operation was chosen only in cases of cancer of the left colon and mainly of the sigmoid. Specifically, in cases of occlusive sigmoid cancer, there was a clear preference for this operation.
Regarding the variation of surgical options for patients with obstructive colon cancer at the General Hospital of Katerini, in relation to the year of the operation, it is worth noting that during the time period 2020-2021 and therefore amidst COVID pandemic, there was an increase in the frequency of performing a simple diversion stoma without resection of the primary tumor, compared to the previous years (
Table 3). This fact is particularly interesting and could perhaps be attributed to the delayed arrival of patients at the Hospital due to their fear of the pandemic, as well as to the pressure on the surgeons to perform a quick decongestive operation. It is worth noting that during the pandemic at the General Hospital of Katerini, all scheduled operations were suspended and for a period of time, even the emergency ones.
In cases of generalized carcinomatosis, it is observed that the surgeons of the General Hospital of Katerini choose the installation of a diversion stoma and a non-excision of the primary tumor. Something worth noting is that in all cases of patients with bowel obstruction due to colon malignancy, surgical treatment was the only treatment option, because in the study period it was not possible to install an endoscopic stent, due to a lack of staff, materials and expertise in our hospital. All of the above contributes to 73% of patients eventually ending up with some type of stoma after the first surgery.
4. Discussion
The obstruction of the gastrointestinal system(GI) is a frequent surgical emergency, with high morbidity and mortality [
8]. Incarcinated hernias and postoperative adhesions are the most frequent causes of obstruction [
8] while the lower GI obstruction accounts for 2% to 4% of all admissions to surgical clinics and, while four to five times less common than small bowel obstruction, it accounts for at least 25% of all intestinal obstructions [
11]. Colorectal cancer is also quite common as a cause of obstruction [
8], as colonic malignancy can lead to large bowel obstruction in 10-19% of the cases[
1,
2]. Other causes of intestinal obstruction are intussusception, torsion, and tuberculosis [
8].
In 2017, the World Society of Surgical Emergencies (WSES) guidelines for colorectal cancer emergencies, that is obstruction and perforation, were published [
4]. Based on these, the treatment of bowel obstruction due to colorectal cancer must be individualized and differs depending on which part of the bowel is affected by the malignancy [
4].
The treatment of obstructive cancer of the right colon is analyzed in the international literature less than that of the left colon [
4], which can be justified by various anatomical reasons (better mobilization of the right colonic flexure, easier ileocolic anastomosis due to of small bowel motility, optimal blood supply to the terminal ileum and right colon compared to certain critical zones of the left colon and rectum, whose blood supply depends on the patency of the labial artery and hypogastric vessels) [
4] .
Regarding obstructive right colon cancer, according to the 2017 WSES guidelines, right colectomy with primary anastomosis is the operation of choice, while a valid alternative, if a primary anastomosis is considered unsafe, is colectomy with a terminal ileostomy [
4]. In cases where the cancer is considered unresectable, an ileotransverse anastomosis or a loop ileostomy is suggested as a palliative treatment, in preference to internal bypass, to avoid the electrolyte disturbances accompanying an ileostomy [
4]. The use of stents for cases of obstructive right colon cancer is suggested as a palliative treatment in cases of unresectable end-stage tumor, while it is not indicated as a bridge to surgery [
4]. In critically ill patients right colectomy with end ileostomy should be considered the operation of choice and in severely unstable patients loop ileostomy without resection is recommended [
4].
The treatment of obstructive left-sided colon cancer is more analyzed in the international literature compared to right-sided colon cancer, and there are more treatment and surgical options available. In general, obstruction of the left colon is more common than the right colon as the intraluminal diameter of the colon is the narrowest between the splenic flexure and the rectosigmoid junction [
1]. In cases of obstructive cancer of the left colon and rectum, the surgical treatment can be either directly the primary resection of the tumor or an initial management of the obstruction and then an oncological resection as an elective procedure later [
1].
Based on the 2017 WSES guidelines, treatment options for obstructive left colon and rectal cancer include loop diverting colostomy, primary resection and anastomosis with or without prophylactic ileostomy, resection and colostomy (Hartmann's Procedure), endoscopic stenting with self-expanding metal stents (SEMS) and decompression using an endoscopic rectal tube [
4]. Primary tumor resection aims to achieve an oncological resection of the cancer and treat the obstruction at the same time [
1]. In cases where primary resection of the tumor is chosen, a resection and anastomosis with or without an ileostomy has been increasingly preferred by surgeons in relation to resection and colostomy, that is Hartmann’s operation, which is recommended for cases of patients considered to be at high risk and when treated in an emergency situation [
4]. A simple colostomy without tumor resection should be reserved for unresectable tumors or for critically ill patients, who are too unfit for major surgery or general anesthesia [
4].
Our research shows that there is a tendency by the surgeons of the General Hospital of Katerini to choose the most convenient and rapid surgical approach when operating on patients with malignant colonic obstruction. It is worth noting that this decision is affected by many factors, such as the inability to adequate staging with tomographs in district hospitals, lack of special radiological and serological tests, but also the absence of specialist doctors, such as oncologists (and therefore an oncology board) in these hospitals. This fact may also be related to the lack of a gastroenterologic team and the ability of bridging to surgery through endoprosthesis. The surgeon is in the end the one who will ultimately decide on the type of operation to be performed and will, therefore, affect both the final oncological outcome and the patient's quality of life, as in the majority of cases patients end up with a stoma.
5. Conclusions
With our research, the deviation of the reality at the district hospitals of Greece in relation to the predicted by the international literature, regarding the obstructive colon cancer is reflected. Our recommendation is for further studies in the rest of the greek hospitals to be carried out, with the aim of creating better guidelines regarding the emergency treatment of obstructive colon cancer in the country's district hospitals.
Author Contributions
Conceptualization, Investigation, Writing—Original Draft Preparation: Ismini Kountouri; Periklis Dimasis; Ioannis Katsarelas. Writing—Review and Editing: Ismini Kountouri; Periklis Dimasis; Ioannis Katsarelas; Afroditi Kotarela; Nikolaos Bakalis; Miltiadis Chandolias; Maria Martha Galani Manolakou; Nikolaos Gkiatas; Dimitra Manolakaki.. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
None of the data in the paper reveal the patients’ identity.
Data Availability Statement
All relevant data are within the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Gainant A, Emergency management of acute colonic cancer obstruction, Journal of Visceral Surgery, 2012 Volume 149, Issue 1: 1-10. [CrossRef]
- Kim YJ, Surgical treatment of obstructed left-sided colorectal cancer patients. Ann Coloproctol, 2014, Dec,30 :245-6. [CrossRef]
- Luca Ansaloni, Roland E Andersson, Franco Bazzoli, Fausto Catena, Vincenzo Cennamo, Salomone Di Saverio, Lorenzo Fuccio, Hans Jeekel, Ari Leppäniemi, Ernest Moore, Antonio D Pinna, Michele Pisano, Alessandro Repici, Paul H Sugarbaker & Jean-Jaques Tuech, Guidelines in the management of obstructing cancer of the left colon: consensus conference of the world society of emergency surgery (WSES) and peritoneum and surgery (PnS) society, World J Emerg Surg, 2010, Issue 5, Article number: 29:1749-7922. [CrossRef]
- Pisano M, Zorcolo L, Merli C et al., 2017 WSES guidelines on colon and rectal cancer emergencies: obstruction and perforation, World J Emerg Surg, 2018, 13, no 36. [CrossRef]
- Yoo RN, Cho HM, Kye BH. Management of obstructive colon cancer: Current status, obstacles, and future directions, World J Gastrointest Oncol, 2021 Dec 15,13 :1850-1862. [CrossRef]
- Cortet M, Grimault A, Cheynel N, Lepage C, Bouvier AM, Faivre J, Patterns of recurrence of obstructing colon cancers after surgery for cure: a population-based study, Colorectal Dis 2013, 15: 1100-1106. [CrossRef]
- Seo SY, Kim SW, Endoscopic Management of Malignant Colonic Obstruction. Clin Endosc. 2020 Jan, 53,1:9-17. [CrossRef]
- Udo IA, Ugochukwu O. Acute Intestinal Obstruction: A 1-Year Prospective Audit into Causes, J West Afr Coll Surg, 2023 Jul-Sep,13,3:6-9. [CrossRef]
- Tong, JWV, Lingam P and Shelat VG, Adhesive small bowel obstruction – an update, Acute Med. Surg., 7: 587.
- Biondo S, Gálvez A, Ramírez E, Frago R, Kreisler E, Emergency surgery for obstructing and perforated colon cancer: patterns of recurrence and prognostic factors, Tech Coloproctol , 2019 Dec,23,12:1141-1161. [CrossRef]
- Verheyden C, Orliac C, Mill. let I, Taourel P, Large-bowel obstruction: CT findings, pitfalls, tips and tricks, Eur J Radiol, 2020 Sep,130:109155.
- Bower KL, Lollar DI, Williams SL, Adkins FC, Luyimbazi DT, Bower CE, Small Bowel Obstruction, Surg Clin North Am, 2018 Oct,98,5:945-971.
- Rami Reddy SR, Cappell MS. A Systematic Review of the Clinical Presentation, Diagnosis, and Treatment of Small Bowel Obstruction. Curr Gastroenterol Rep. 2017 Jun,19,6:28.
- Quere P, Facy O, Manfredi S, Jooste V, Faivre J, Lepage C, Bouvier AM. Epidemiology, Management, and Survival of Peritoneal Carcinomatosis from Colorectal Cancer: A Population-Based Study. Dis Colon Rectum, 2015 Aug;58,8:743-52.
- Laval G, Marcelin-Benazech B, Guirimand F, Chauvenet L, Copel L, Durand A, Francois E, Gabolde M, Mariani P, Rebischung C, Servois V, Terrebonne E, Arvieux C, French Society for Palliative Care, French Society for Digestive Surgery; French Society for Gastroenterology, French Association for Supportive Care in Oncology, French Society for Digestive Cancer, Recommendations for bowel obstruction with peritoneal carcinomatosis, J Pain Symptom Manage, 2014 Jul,48,1:75-91.
Table 1.
Tumor resection depending on its location.
Table 1.
Tumor resection depending on its location.
| Tumor location |
Excision of the tumor |
No excision |
| Rectum Ca |
4 |
8 |
| Sigmoid colon Ca |
18 |
9 |
| Descending colon Ca |
2 |
1 |
| Splenic Flexure Ca |
6 |
2 |
| Transverse colon Ca |
3 |
3 |
| Ascending colon Ca |
7 |
2 |
| Cecum colon Ca |
6 |
2 |
Table 2.
Type of operation by tumor location.
Table 2.
Type of operation by tumor location.
| Tumor location |
Resection and anastomosis |
Resection and prophylactic stoma |
Hartmanns’ |
No resection - diverting stoma |
| Rectum Ca |
0 |
2 |
2 |
8 |
| Sigmoid colon Ca |
3 |
1 |
14 |
9 |
| Descending colon Ca |
1 |
0 |
1 |
1 |
| Splenic Flexure Ca |
3 |
3 |
0 |
2 |
| Transverse colon Ca |
2 |
1 |
0 |
3 |
| Ascending colon Ca |
6 |
1 |
0 |
2 |
| Cecum colon Ca |
4 |
2 |
0 |
2 |
Table 3.
Operations per year.
Table 3.
Operations per year.
| Time period |
Resection and anastomosis |
Resection and prophylactic stoma |
Hartmanns’ |
No resection - diverting stoma |
| 2022 |
3 |
2 |
2 |
2 |
| 2020-2021 |
4 |
1 |
3 |
12 |
| 2018-2019 |
2 |
2 |
4 |
5 |
| 2016-2017 |
4 |
3 |
4 |
1 |
| 2014-2015 |
3 |
2 |
2 |
0 |
| 2012-2013 |
3 |
0 |
2 |
7 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).