1. Introduction
Viruses are unique among living organisms in that their genetic material can be either RNA or DNA. These nucleic acid molecules are routinely extracted for diagnostic and research purposes from viral cultures, human clinical specimens, and samples from animals and the environment. Although nucleic acid extraction is a routine procedure for many laboratories, for biosafety level 4 (BSL-4) laboratories handling high consequence pathogens such as Ebola virus (EBOV), Marburg virus (MARV) and Lassa virus (LASV), verification of viral inactivation in samples to be removed from BSL-4 is crucial to ensure personnel and environmental safety during downstream analyses conducted in lower containment laboratories.
A variety of methods and commercial kits are available to isolate nucleic acids from samples [
1,
2,
3]. Regardless of what method or kit is used, the essential steps involved in the nucleic acid extraction process remain the same: sample lysis, removal of unwanted biomolecules such as proteins and lipids, and purification/concentration of nucleic acids. These steps are accomplished through a variety of mechanical methods, chemical processes, or a combination of both. When chemical methods are used, lysis buffers containing lytic enzymes, chaotropic compounds, denaturing agents or detergents are employed to accomplish sample lysis. For instance, the QIAamp® Viral RNA mini kit (Cat. No. 52906, Qiagen Corp., Valencia, CA,) is routinely used in BSL-4 laboratories to isolate viral RNA and employs AVL lysis buffer, which contains 50%-70% guanidine thiocyanate (GITC) [
4]. GITC lyses cells and viruses, and denatures proteins including nucleases [
5,
6].
AVL lysis buffer has been used for nucleic acid extraction from a variety of enveloped and non-enveloped viruses contained in samples and cultures. Past studies evaluating the effectiveness of AVL included severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [
4,
7], EBOV [
8,
9,
10], Venezuelan equine encephalitis virus [
8,
11], Eastern equine encephalitis virus, Western equine encephalitis virus, Rift Valley fever virus, MARV, Dengue virus, West Nile virus [
8], Chikungunya virus, La Crosse virus [
12], Middle East respiratory syndrome-related coronavirus (MERS) [
13], African swine fever virus [
14], Foot-and-mouth disease virus [
15], adenovirus 5, Echovirus 11, and human immunodeficiency virus 1 [
16]. A consistent finding across these studies was that AVL lysis buffer treatment alone could not accomplish complete viral inactivation. Additional measures, such as alcohol [
9,
13], heat [
9,
17,
18] or detergent [
6,
19] treatment, were required to achieve effective viral inactivation. Therefore, the addition of ethanol to the virus culture-AVL lysis buffer mixture, as per QIAamp Viral RNA Mini Handbook instructions [
20], has been implemented before samples can be removed from our BSL-4 laboratory.
The presence of GITC (or other such caustic chemicals) in the AVL lysis buffer-treated sample mixtures presents a significant challenge when attempting to detect surviving infectious viral particles using cell cultures. These chemicals, even at low concentrations, cause cytotoxicity [
8,
12,
21] or impair the overall health of the cell cultures, which may render the cells unable to support the growth of any infectious viruses present in the lysed sample. Furthermore, the cytotoxicity or chemical-induced alterations in cell morphology cannot be easily distinguished from virus-induced cell lysis or cytopathic effects (CPE), which is characterized by rounding of cells, syncytia formation or appearance of inclusion bodies caused by replicating virus [
22].
A variety of approaches have been developed to reduce, neutralize or remove the effects of the toxic chemicals on cell cultures, including neutralization with other suitable chemicals, ultra-centrifugation to separate out viral particles, prolonged dialysis to remove toxic chemicals, gel filtration, or the use of size exclusion centrifugal filter columns. Use of size exclusion spin columns to remove cytotoxic chemicals from virus-containing samples has been successfully employed by several previous studies [
4,
13,
19,
21]. Following this approach, our study utilized the Amicon Ultra Centrifugal Filter column to achieve the same goal, removing toxic chemicals from infectious viral particles. Our objective was to evaluate the effectiveness of the standard AVL lysis buffer procedure in inactivating Ebola, Marburg, and Lassa virus cultures without any interference from toxic chemicals using Amicon spin columns.
2. Materials and Methods
2.1. Cell line, Viruses, and Medium
African green monkey Vero E6 cells (CRL-1586; American Type Culture Collection, Manassas, VA, US) were used for the initial stock virus culture preparation, and also for viral recovery assays after AVL-ethanol treatment. The cells were maintained in Dulbecco’s modified Eagle’s medium (DMEM, Hyclone SH3024302) supplemented with 10% fetal bovine serum (FBS; Gibco 12484028) and 10 Units/ml of penicillin/streptomycin (PS, Gibco 10378016), referred to henceforth as cell culture medium (CCM). Vero E6 cells for virus culture and recovery assays were maintained in DMEM with 2% FBS and 10 units/ml PS, referred to henceforth as virus culture medium (VCM). All Vero E6 cell cultures, whether virus-infected or not, were incubated in a humidified incubator at 37°C and 5% CO2.
2.2. Stock Virus Culture Preparation
Ebola virus variant Makona (EBOV/Mak, Ebola virus/H. sapiens-tc/GIN/2014/Makona-C07; GenBank accession no. KJ660348), originally isolated from a clinical sample [
23], was genetically modified to express enhanced green fluorescent protein (eGFP) [
24]. A stock of EBOV/Mak expressing eGFP (EBOV-eGFP) was prepared by infecting ten T175 flasks of Vero E6 cells at a multiplicity of infection of 0.01. Expression of eGFP, observed under a fluorescent microscope (EVOS
® FL digital inverted fluorescence microscope, using EVOS light cube GFP 2.0), was evident in the infected Vero E6 cells at day 3 post-infection, but flasks were harvested 9 days post-infection once 80% of the cell monolayer exhibited pronounced cytopathic effect (CPE). Flasks were frozen at −80°C, thawed the following day, and the contents were clarified by low-speed centrifugation at 5000 × g for 10 minutes at 4°C to pellet cellular debris. A previously published method was used to prepare concentrated stock virus cultures [
25]; briefly, the clarified supernatants from all flasks were pooled, and overlaid onto a 7-ml 20% sucrose cushion in ultra-centrifuge tubes and spun at 134,000 x g for 2 hours using a SW 32 Ti Rotor (Beckman Coulter) at 4°C. The resulting viral pellets were suspended in 500 µl of VCM/tube and left overnight at 4°C. Virus suspensions were pooled, aliquotted, and frozen at −80°C until needed. The titre of the stock virus was 8.8 log
10 TCID
50/ml.
A Marburg virus isolated from bats, designated as 371Bat [
26], was genetically modified to express the Zs Green fluorescent protein (MARV-ZsG) [
27] and kindly provided by Jonathan Towner, U.S Centers for Disease Control and Prevention, Atlanta, GA. A stock culture of concentrated MARV-ZsG (6.95 log
10 TCID
50/ml) was prepared in ten T175 Vero E6 cell culture flasks as detailed above for EBOV-eGFP. Similar to EBOV, green fluorescence was evident in cell cultures at day 3, but flasks were harvested 14 days post infection when 80% of the cell monolayer exhibited pronounced CPE.
Lassa virus Josiah, genetically modified to express GFP (LASV-GFP) was obtained from Jens Kuhn, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD [
28]. A stock culture of concentrated LASV-GFP (9.2 log
10 TCID
50/ml) was prepared in ten T175 Vero E6 flasks as detailed above for EBOV-eGFP. However, unlike EBOV and MARV, LASV failed to yield pronounced CPE in cell cultures; expression of GFP was evident as early as 1 day post-infection, and flasks were harvested at day 4 post infection when 100% of the cell monolayer showed fluorescence.
2.3. Removal of Toxic Chemicals using Amicon Filter Columns
The AVL buffer treatment process typically involves mixing 140 µl of virus culture with 560 µl of AVL lysis buffer followed by 10 minutes of incubation. The entire 700 µl mixture is then transferred to a fresh tube containing 560 µl of 95% ethanol and inversion-mixed before removal from BSL-4. To remove toxic chemicals from this mixture, we employed the Amicon Ultra-0.5 ml 100 K Centrifugal Filter column (Cat. No. UFC510008, Millipore Sigma). These columns, made of regenerated cellulose membrane, are designed to concentrate/purify macromolecules and microorganisms from biological samples while simultaneously allowing the removal of small molecules, such as salts and chemicals [
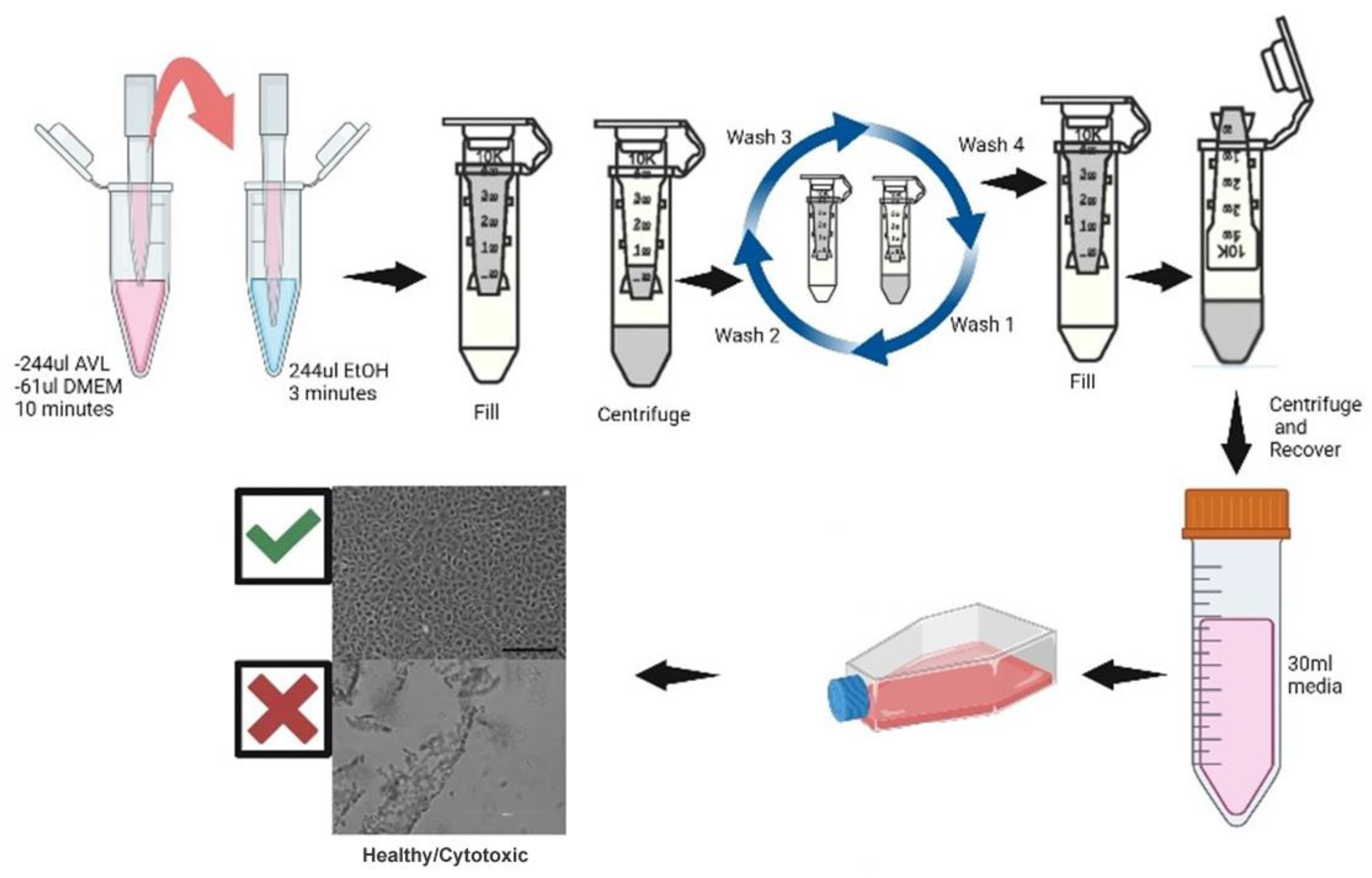
29]. Because the Amicon spin column has a volume limitation of approximately 500 µl, we scaled down the volumes used in our assays proportionately while maintaining the ratios of the BSL-4 sample removal protocol. A reduced volume of 61 µl of virus culture was mixed with 244 µl of AVL lysis buffer and incubated for 10 minutes; 244 µl of 95% ethanol was then added to the mixture and incubated for another 3 minutes prior to proceeding with the filter column centrifugation procedure, as described below.
2.4. Control Assays
The following four control assays were performed prior to the virus inactivation assay to ensure that the residual chemicals from the lysed sample mixture were successfully removed: cytotoxicity control, interference control, low-titre positive control and negative control. Ten T175 flasks were seeded with Vero E6 cells to obtain 80% confluency on the following day: three flasks each for the cytotoxicity control, low-titre positive control, interference control, and one flask for the negative control.
Cytotoxicity controls were done to verify the removal of toxic chemicals from the mixture to ensure no cytotoxicity occurred in cell cultures. These controls were done in replicates of three; 244 µl of AVL buffer, 61 µl of VCM and 244 µl of 95% ethanol were mixed and the entire volume of mixture from each replicate was transferred to three Amicon spin columns. Columns were centrifuged at 14000 x g until approximately 100 µl of retentate remained in the column. The flow through filtrate from the collection tubes was discarded. An additional 400 µl of VCM was added to the column, mixed by inversion, and centrifuged. The process was repeated three more times for a total of four washes to remove chemical residues. After the final wash, 400 µl of VCM was added to each column retentate, gently mixed by pipetting a few times and incubated at room temperature for two minutes. Each column was transferred to new collection tubes in an inverted orientation (
Figure 1), and centrifuged at 1200 x g for two minutes to elute into the collection tubes. Eluate from each replicate tube was mixed with 30 ml of VCM, inoculated onto three T175 flasks containing Vero E6 cells and incubated. The cell monolayer was monitored for abnormalities (cytotoxicity, altered morphology, slow growth) for 14 days in comparison to the untreated cell monolayer (negative control).
Low-titre positive controls were done to demonstrate that an inoculum containing exceptionally low levels of the virus can still be detected in Vero E6 cell cultures. Stock virus culture was diluted in VCM to ≤103 TCID50/ml. In replicates of three, 10 µl of diluted virus culture was mixed with 30 ml of VCM and inoculated onto three T175 flasks and incubated for 14 days.
Interference controls were done to determine the effects on viral replication caused by any potential residual chemicals leftover after the Amicon column processing. A replicate of three eluate-VCM mixtures was prepared as detailed for the cytotoxicity controls; 10 µl of ≤103 TCID50/ml diluted virus culture was added to each mixture and inoculated onto three T175 flasks of Vero E6 cells. If there was no impact by any remaining chemicals to the added virus, then the cell monolayer would be expected to exhibit CPE similar to the low-titre positive controls.
A negative control was prepared to have a point of reference for healthy cells to compare with the other three controls. CCM was aspirated from a T175 flask, 30 ml of VCM was added and incubated for 14 days.
2.5. Virus Inactivation Assay and Sub Passage
Six T175 flasks with Vero E6 cells at 80% confluency were prepared as above: three flasks for the viral inactivation assay, and one flask each for the cytotoxicity control, low-titre positive control and negative control. For the viral inactivation assay, in replicates of three, 244 µl of AVL lysis buffer was mixed with 61 µl of stock virus culture, and incubated for 10 minutes, after which 244 µl of 95% ethanol was added, mixed by inverting the tubes and incubated for another 3 minutes. The entire volume of inactivation assay mixtures was transferred to corresponding Amicon columns, centrifuged, washed and eluted as described above. Eluates from each column were mixed with 30 ml of VCM and inoculated onto the Vero E6 flasks. Cell cultures were monitored for 14 days for signs of viral growth in comparison to the control flasks for abnormalities such as cytotoxicity, altered morphology, and slow growth.
Inactivation assay flasks showing no signs of viral growth were sub passaged for confirmation. Sub passaging involved transferring 1 ml of medium from each T175 flask to a well containing 3 ml of VCM in a 6-well plate with Vero E6 cells. The inoculated plate was incubated for another 14 days and monitored for fluorescence/CPE. The inactivation assay samples were considered free of infectious virus only if this passage also showed no signs of viral replication. All the flasks and plates that showed CPE/fluorescence were scored as positive (“+”), indicating the presence of virus, or negative (“-“), indicating the absence of detectable virus.
3. Results
3.1. Control Assays
To assess whether Amicon column filtration could effectively remove the residual chemicals in an AVL buffer-based nucleic acid extraction, a single cytotoxicity control experiment consisting of three replicates was performed. VCM without virus was mixed with AVL lysis buffer and ethanol, processed through Amicon spin columns and inoculated onto Vero E6 cells. After 14 days, no cytotoxicity was observed on the cell monolayer (
Table 1), suggesting that the sample processing through the Amicon column effectively removed residual chemicals, preventing it from negatively affecting the health of the cell monolayer and generating false positive results.
To assess whether any potential chemical residues remaining after Amicon column processing could interfere with viral replication (interference control), we repeated the above experiment but spiked the eluate with 1 ml of stock virus diluted to 0.7 log
10 TCID
50/ml of MARV-ZsG, 0.8 log
10 TCID
50/ml of LASV-GFP, or 0.8 log
10 TCID
50/ml of EBOV-eGFP prior to infecting the Vero E6 flasks. After 14 days, CPE and fluorescence were observed (
Table 1), indicating that Amicon filtration effectively removed residual chemicals, thus preventing them from interfering with viral replication, even when inoculated with viral titers equal to their limit of detection.
A negative control flask consisting of untreated Vero E6 cells maintained in VCM exhibited no CPE or fluorescence (
Table 1). Low-titre positive control flasks for each virus demonstrated green fluorescence within few days of incubation after infection (
Table 1).
3.2. Inactivation Assay after AVL Lysis Buffer & Ethanol Treatment
This assay was performed after all the control assays had been evaluated and deemed satisfactory, and it was done to determine whether our AVL lysis buffer and ethanol incubation protocol in BSL-4 was sufficient to inactivate high titer cultures of EBOV, MARV, and LASV. We performed a series of inactivation validation assays. High titre stock cultures of EBOV-eGFP, MARV-ZsG or LASV-GFP containing 6.95 - 9.0 log
10 TCID
50/ml of virus was used to mix with AVL/ethanol to generate volumes containing 6.47 - 8.02 log
10 TCID
50 of virus per test. Each virus culture was processed through Amicon spin columns to remove toxic chemicals and used to inoculate flasks of Vero E6 cells, as described above. A total of three experiments were conducted for EBOV and LASV, while only two experiments were conducted for MARV. Each experiment consisted of 3 biological replicates. After 14 days, no CPE or fluorescence was observed in any replicate from any of the initial assays or subsequent passages (
Table 2,
Table 3 and
Table 4), indicating no detectable virus was present in any of the samples after AVL lysis buffer and ethanol treatment.
In addition, each replicate experiment also included a simultaneously run low-titre positive control, to demonstrate that low titers of the virus can be detected, and negative control, to provide a point of reference for cell damage due to any residual toxic chemicals after Amicon column filtration. After 14 days, all low-titer positive control flasks exhibited CPE and fluorescence (
Table 2,
Table 3 and
Table 4). Importantly, they demonstrated the sensitivity of this assay, as we were able to detect as low as ≤0.8 log
10 TCID
50 of infectious virus, the limit of detection for our assay. Negative controls did not exhibit any CPE or fluorescence, serving as a visual reference for the other flasks during microscopy and also as a cross contamination indicator (
Table 2,
Table 3 and
Table 4).
4. Discussion
Unlike the variety of inanimate media that are routinely used for the recovery and detection of most bacterial species, viruses require living host systems such as embryonated eggs, laboratory animals or cell cultures for their recovery and detection in samples. However, if such a sample contains any toxic chemicals, these chemicals may negatively affect the health of the embryos [
30], animals [
31] or cells [
13,
32]. Toxic chemicals in AVL and other buffers that are required for lysing the viral particles to extract RNA molecules present a significant challenge to subsequent assays undertaken to determine the presence of surviving infectious viral particles. These chemicals can cause death of embryonated eggs, laboratory animals or cell cultures when inoculated with the sample/chemical mixture. When cell cultures are used, the presence of infectious virus is verified routinely by microscopic observation of virus induced CPE. Chemicals in the lysate mixture may lyse or damage the cell monolayer, mimicking virus induced cytolysis or CPE, thus leading to false positives (indicating a virus is present when it is not). Alternatively, the same chemicals may damage any remaining virus particles, interfering with the virus’s ability to replicate, and producing false negatives.
The Amicon centrifugal ultra filtration effectively removed the toxic chemicals from the virus culture/lysis buffer mixture while retaining the viral particles to be subsequently eluted off the filter column such that we were able to detect as low as ≤0.8 log10 TCID50 virus in our cell culture. In addition, we also diluted the eluates recovered from each column 75-fold in VCM to further reduce the effect of any potential breakthrough toxic chemicals. To confirm that the diluted eluate is sufficiently free of toxic chemicals, we performed cytotoxicity and interference assays. These assays investigated the impact of residual chemicals on the Vero E6 cell monolayer (cytotoxicity assay) and on virus replication (interference assay).
A single experiment was performed consisting of three biological replicates. After 14 days, the cells showed no cytotoxicity or signs of cellular damage, suggesting that the column filtration process along with 75-fold dilution effectively removed the effects of harmful chemicals. Interference assays—which were performed similarly except with spiked-in low-titre EBOV-eGFP, MARV-ZsG, or LASV-GFP—showed signs of viral replication (CPE) and green fluorescence comparable to that of the low-titre positive controls, indicating that the virus replicated normally at levels equal to the limit of detection of our assay without interference from chemicals. Together, these data suggest that the Amicon spin column procedure was suitable for removing the effects of residual chemicals without affecting the integrity of the Vero E6 cell monolayer, which supported viral replication with a sensitivity equal to that of the low-titre positive control.
To assess whether our long-established AVL lysis buffer and ethanol incubation protocol in BSL-4 was sufficient to inactivate EBOV, MARV, and LASV, we performed a series of inactivation validation assays. High-titer stock cultures of EBOV-eGFP, MARV-ZsG, or LASV-GFP virus were used to mix with AVL/ethanol, generating volumes containing 6.47 - 8.02 log10 TCID50 of virus per test. Each virus culture sample was mixed with AVL lysis buffer and ethanol, processed through Amicon spin columns, and used to inoculate Vero E6 flasks. After 14 days, no virus was detected in any of the replicate assays or their subsequent passages, indicating that AVL lysis buffer and ethanol treatment inactivated EBOV, MARV, and LASV.
One minor limitation of this study was the constraint on sample volume processing. In our standard BSL-4 protocol for AVL extraction, we use 140 µl of virus culture combined with 560 µl of AVL lysis buffer and 560 µl of 95% ethanol. However, the Amicon filter column had a maximum capacity of approximately 500 µl. To adapt to this limitation, we scaled down our volumes to 61 µl of virus culture, 244 µl of AVL lysis buffer, and 244 µl of 95% ethanol. Interestingly, a study by Burton et al. showed that larger 2-ml volumes processed through Vivaspin 2.0 columns, which worked successfully in BSL-2, "did not translate well" in BSL-4 for removing chemicals from the AVL lysis buffer. Subsequently, they also had to resort to smaller 500-µl volumes and Amicon spin columns [
19], as we did with our experiments for this study.
While the results indicate that the nucleic acid extraction protocol validated here may also be effective at inactivating other RG4 viruses, which are also all enveloped viruses, further validation studies are necessary to confirm this effectiveness. Such studies should ideally be conducted with RG4 viruses not only in cultures but also in clinical samples. Given that there are over two dozen RG4 viruses spanning nine viral families [
33,
34]—
Arenaviridae (e.g., Lassa virus),
Filoviridae (e.g., EBOV),
Flaviviridae (e.g., Kyasanur Forest disease virus),
Herpesviridae (e.g., Cercopithecine herpesvirus 1),
Nairoviridae (e.g., Crimean-Congo hemorrhagic fever virus),
Orthomyxoviridae (e.g., Alphainfluenzavirus influenzae H1N1 reconstructed 1918 strain) [
35],
Paramyxoviridae (e.g., Nipah virus),
Poxviridae (e.g., Variola virus), and
Rhabdoviridae (e.g., Bas-Congo virus) [
36]—it is crucial to validate this protocol's efficacy across this diverse group. This will ensure the accuracy and reliability of the protocol for each specific high-consequence pathogenic virus.
5. Conclusions
This study’s findings showed no detectable viable virus present when high-titer Ebola, Marburg, or Lassa virus culture was incubated with AVL lysis buffer for 10 minutes, followed by an equal volume of 95% ethanol for 3 minutes, using a method with a sensitivity of ≤0.8 log10 TCID50 as the limit of detection. These results further support the effectiveness of our established protocol in inactivating these high-consequence pathogens, and they support the safe transfer of treated samples from BSL-4 to lower biosafety level laboratories for further analysis, thereby facilitating essential ongoing research and diagnostic activities while maintaining stringent safety standards.
The robustness of this inactivation method across three different viruses suggests its potential applicability to other similar high-consequence pathogens, though further testing is required.
Author Contributions
Conceptualization, T.C., L.B. and J.K.; methodology, T.C., A.L. J.K.; investigation, T.C. and A.L.; writing—original draft preparation, J.K.; writing—review and editing, T.C., A.L. and L.B. All authors have read and agreed to the published version of the manuscript.
Funding
This work has been funded by the Government of Canada, through the Public Health Agency of Canada, and received no external funding.
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Not Applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Tan, S.C.; Yiap, B.C. DNA, RNA, and Protein Extraction: The Past and The Present. J. Biomed. Biotechnol. 2009, 2009, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.; Rampazzo, R.D.C.P.; Costa, A.D.T.; Krieger, M.A. Current Nucleic Acid Extraction Methods and Their Implications to Point-of-Care Diagnostics. BioMed Res. Int. 2017, 2017, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Mullegama, S.V.; Alberti, M.O.; Au, C.; Li, Y.; Toy, T.; Tomasian, V.; Xian, R.R. Nucleic Acid Extraction from Human Biological Samples. In Biobanking; Yong, W.H., Ed.; Methods in Molecular Biology; Springer New York: New York, NY, 2019; ISBN 978-1-4939-8933-1. [Google Scholar]
- Pastorino, B.; Touret, F.; Gilles, M.; Luciani, L.; De Lamballerie, X.; Charrel, R.N. Evaluation of Chemical Protocols for Inactivating SARS-CoV-2 Infectious Samples. Viruses 2020, 12, 624. [Google Scholar] [CrossRef] [PubMed]
- Avelin, V.; Sissonen, S.; Julkunen, I.; Österlund, P. Inactivation Efficacy of H5N1 Avian Influenza Virus by Commonly Used Sample Preparation Reagents for Safe Laboratory Practices. J. Virol. Methods 2022, 304, 114527. [Google Scholar] [CrossRef] [PubMed]
- Lewandowski, K.; Bell, A.; Miles, R.; Carne, S.; Wooldridge, D.; Manso, C.; Hennessy, N.; Bailey, D.; Pullan, S.T.; Gharbia, S.; et al. The Effect of Nucleic Acid Extraction Platforms and Sample Storage on the Integrity of Viral RNA for Use in Whole Genome Sequencing. J. Mol. Diagn. 2017, 19, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Auerswald, H.; Yann, S.; Dul, S.; In, S.; Dussart, P.; Martin, N.J.; Karlsson, E.A.; Garcia-Rivera, J.A. Assessment of Inactivation Procedures for SARS-CoV-2. J. Gen. Virol. 2021, 102. [Google Scholar] [CrossRef] [PubMed]
- Blow, J.A.; Dohm, D.J.; Negley, D.L.; Mores, C.N. Virus Inactivation by Nucleic Acid Extraction Reagents. J. Virol. Methods 2004, 119, 195–198. [Google Scholar] [CrossRef]
- Smither, S.J.; Weller, S.A.; Phelps, A.; Eastaugh, L.; Ngugi, S.; O’Brien, L.M.; Steward, J.; Lonsdale, S.G.; Lever, M.S. Buffer AVL Alone Does Not Inactivate Ebola Virus in a Representative Clinical Sample Type. J. Clin. Microbiol. 2015, 53, 3148–3154. [Google Scholar] [CrossRef]
- Haddock, E.; Feldmann, F.; Feldmann, H. Effective Chemical Inactivation of Ebola Virus. Emerg. Infect. Dis. 2016, 22, 1292–1294. [Google Scholar] [CrossRef]
- Patterson, E.I.; Warmbrod, K.L.; Bouyer, D.H.; Forrester, N.L. Evaluation of the Inactivation of Venezuelan Equine Encephalitis Virus by Several Common Methods. J. Virol. Methods 2018, 254, 31–34. [Google Scholar] [CrossRef]
- Ngo, K.A.; Jones, S.A.; Church, T.M.; Fuschino, M.E.; George, K.St.; Lamson, D.M.; Maffei, J.; Kramer, L.D.; Ciota, A.T. Unreliable Inactivation of Viruses by Commonly Used Lysis Buffers. Appl. Biosaf. 2017, 22, 56–59. [Google Scholar] [CrossRef]
- Kumar, M.; Mazur, S.; Ork, B.L.; Postnikova, E.; Hensley, L.E.; Jahrling, P.B.; Johnson, R.; Holbrook, M.R. Inactivation and Safety Testing of Middle East Respiratory Syndrome Coronavirus. J. Virol. Methods 2015, 223, 13–18. [Google Scholar] [CrossRef] [PubMed]
- McCleary, S.; McCarthy, R.R.; Strong, R.; Edwards, J.; Crooke, H. Inactivation of African Swine Fever Virus by Reagents Commonly Used in Containment Laboratories. J. Virol. Methods 2021, 295, 114203. [Google Scholar] [CrossRef] [PubMed]
- Wood, B.A.; Mioulet, V.; Henry, E.; Gray, A.; Azhar, M.; Thapa, B.; Diederich, S.; Hoffmann, B.; Beer, M.; King, D.P.; et al. Inactivation of Foot-and-Mouth Disease Virus A/IRN/8/2015 with Commercially Available Lysis Buffers. J. Virol. Methods 2020, 278, 113835. [Google Scholar] [CrossRef] [PubMed]
- Seeburg, U.; Urda, L.; Otte, F.; Lett, M.J.; Caimi, S.; Mittelholzer, C.; Klimkait, T. Virus Inactivation by Formaldehyde and Common Lysis Buffers. Viruses 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- McAdams, Z.; Gustafson, K.; Ericsson, A. The Effect of Common Viral Inactivation Techniques on 16S rRNA Amplicon-Based Analysis of the Gut Microbiota. Microorganisms 2021, 9. [Google Scholar] [CrossRef]
- Blow, J.A.; Mores, C.N.; Dyer, J.; Dohm, D.J. Viral Nucleic Acid Stabilization by RNA Extraction Reagent. J. Virol. Methods 2008, 150, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Burton, J.E.; Easterbrook, L.; Pitman, J.; Anderson, D.; Roddy, S.; Bailey, D.; Vipond, R.; Bruce, C.B.; Roberts, A.D. The Effect of a Non-Denaturing Detergent and a Guanidinium-Based Inactivation Agent on the Viability of Ebola Virus in Mock Clinical Serum Samples. J. Virol. Methods 2017, 250, 34–40. [Google Scholar] [CrossRef]
- QIAmp Viral RNA Mini Handbook.Pdf.
- Olejnik, J.; Leon, J.; Michelson, D.; Chowdhary, K.; Galvan-Pena, S.; Benoist, C.; Mühlberger, E.; Hume, A.J. Establishment of an Inactivation Method for Ebola Virus and SARS-CoV-2 Suitable for Downstream Sequencing of Low Cell Numbers. Pathog. Basel Switz. 2023, 12. [Google Scholar] [CrossRef]
- Albrecht, T.; Fons, M.; Boldogh, I.; Rabson, A.S. Effects on Cells. In Medical Microbiology; Baron, S., Ed.; University of Texas Medical Branch at Galveston: Galveston (TX), 1996 ISBN 978-0-9631172-1-2.
- Baize, S.; Pannetier, D.; Oestereich, L.; Rieger, T.; Koivogui, L.; Magassouba, N.; Soropogui, B.; Sow, M.S.; Keïta, S.; De Clerck, H.; et al. Emergence of Zaire Ebola Virus Disease in Guinea. N. Engl. J. Med. 2014, 371, 1418–1425. [Google Scholar] [CrossRef]
- Wong, G.; He, S.; Leung, A.; Cao, W.; Bi, Y.; Zhang, Z.; Zhu, W.; Wang, L.; Zhao, Y.; Cheng, K.; et al. Naturally Occurring Single Mutations in Ebola Virus Observably Impact Infectivity. J. Virol. 2018, 93, e01098–18. [Google Scholar] [CrossRef]
- Cutts, T.; Kasloff, S.; Safronetz, D.; Krishnan, J. Decontamination of Common Healthcare Facility Surfaces Contaminated with SARS-CoV-2 Using Peracetic Acid Dry Fogging. J. Hosp. Infect. 2021, 109, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Towner, J.S.; Amman, B.R.; Sealy, T.K.; Carroll, S.A.R.; Comer, J.A.; Kemp, A.; Swanepoel, R.; Paddock, C.D.; Balinandi, S.; Khristova, M.L.; et al. Isolation of Genetically Diverse Marburg Viruses from Egyptian Fruit Bats. PLoS Pathog. 2009, 5, e1000536. [Google Scholar] [CrossRef] [PubMed]
- Albariño, C.G.; Guerrero, L.W.; Chakrabarti, A.K.; Nichol, S.T. Transcriptional Analysis of Viral mRNAs Reveals Common Transcription Patterns in Cells Infected by Five Different Filoviruses. PLOS ONE 2018, 13, e0201827. [Google Scholar] [CrossRef] [PubMed]
- Caì, Y.; Iwasaki, M.; Beitzel, B.; Yú, S.; Postnikova, E.; Cubitt, B.; DeWald, L.; Radoshitzky, S.; Bollinger, L.; Jahrling, P.; et al. Recombinant Lassa Virus Expressing Green Fluorescent Protein as a Tool for High-Throughput Drug Screens and Neutralizing Antibody Assays. Viruses 2018, 10, 655. [Google Scholar] [CrossRef] [PubMed]
- Amicon Ultra-0.5 Centrifugal Filter Unit | UFC510008. Available online: https://www.emdmillipore.com/CA/en/product/Amicon-Ultra-0.5-Centrifugal-Filter-Unit,MM_NF-UFC510008 (accessed on 25 April 2024).
- Wright, H.S. Test Method for Determining the Viricidal Activity of Disinfectants Against Vesicular Stomatitis Virus. Appl. Microbiol. 1970, 19, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Klein, M. The Inavtivation of Viruses by Germicides. Proc Annu Meet Chem Spec Manuf Assoc 1963, 116–118. [Google Scholar]
- Colavita, F.; Quartu, S.; Lalle, E.; Bordi, L.; Lapa, D.; Meschi, S.; Vulcano, A.; Toffoletti, A.; Bordi, E.; Paglia, M.G.; et al. Evaluation of the Inactivation Effect of Triton X-100 on Ebola Virus Infectivity. J. Clin. Virol. Off. Publ. Pan Am. Soc. Clin. Virol. 2017, 86, 27–30. [Google Scholar] [CrossRef] [PubMed]
- Department of Internal Medicine, Morsani College of Medicine, Tampa, Florida 33606, USA; Shapshak, P. Dangerous Risk Group-4 (RG-4) Emergent Viruses. Bioinformation 2023, 19, 345–347. [Google Scholar] [CrossRef]
- Logue, J.; Solomon, J.; Niemeyer, B.F.; Benam, K.H.; Lin, A.E.; Bjornson, Z.; Jiang, S.; McIlwain, D.R.; Nolan, G.P.; Palacios, G.; et al. Innovative Technologies for Advancement of WHO Risk Group 4 Pathogens Research. In Global Virology III: Virology in the 21st Century; Shapshak, P., Balaji, S., Kangueane, P., Chiappelli, F., Somboonwit, C., Menezes, L.J., Sinnott, J.T., Eds.; Springer International Publishing: Cham, 2019; pp. 437–469. ISBN 978-3-030-29021-4. [Google Scholar]
- Tumpey, T.M.; Basler, C.F.; Aguilar, P.V.; Zeng, H.; Solórzano, A.; Swayne, D.E.; Cox, N.J.; Katz, J.M.; Taubenberger, J.K.; Palese, P.; et al. Characterization of the Reconstructed 1918 Spanish Influenza Pandemic Virus. Science 2005, 310, 77–80. [Google Scholar] [CrossRef]
- Steffen, I.; Liss, N.M.; Schneider, B.S.; Fair, J.N.; Chiu, C.Y.; Simmons, G. Characterization of the Bas-Congo Virus Glycoprotein and Its Function in Pseudotyped Viruses. J. Virol. 2013, 87, 9558–9568. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).