1. Introduction
Currently, it is widely accepted that temporomandibular disorders have a multifactorial etiology [
1,
2]. One of the major etiologic factors of TMD is an orthopedically unstable musculoskeletal position, depicted by an increased CR–MI discrepancy at the dental and condylar levels. The position of the CR, the most orthopedically stable musculoskeletal position of the condyles in the fossa, is considered a highly reproducible reference point for final post-orthodontic and post-prosthodontic reestablishing of the maxillo–mandibular relationship [
3,
4]. Most orthopedically unstable patients are reported to develop certain signs and symptoms that are related to temporomandibular joint or masticatory muscle disorders [
5,
6,
7]. The treatment of orthodontic patients with the signs and symptoms of TMD caused by an unstable musculoskeletal position represents a distinct challenge for every orthodontist that is laborious and time-consuming [
8,
9]. Based on his and earlier findings, Okeson emphasized the importance of orthopedic stability. “Establishing an orthopedically stable relationship between the occlusal position of the teeth and the joint position is important for a proper masticatory function throughout the patient’s lifetime. Although in most situations orthodontic therapy neither causes nor prevents TMD, the orthodontist is in an excellent position to provide orthopedic stability in the masticatory structures. Treatment goals directed toward establishing orthopedic stability in the masticatory structures should be a routine part of all orthodontic therapy. Achieving these goals will most likely reduce the patient’s risk factors for developing TMD” [
10]. This implies that a stable position of the condyles in the fossa that considers the coincident positions of the CR and MI should be the primary goal of orthodontic treatment from the aspect of condylar and masticatory structure health [
11,
12]. Mounting diagnostic casts on an articulator and using a condylar position indicator (CPI) are recommended to evaluate the differences between the CR and MI at the condylar level and find the occlusal interferences responsible for those discrepancies [
5,
11,
12,
13]. Studies comparing the amounts of condylar displacement between the symptomatic and asymptomatic populations determined that condylar displacement was significantly greater in symptomatic individuals [
5,
14,
15,
16]. The positioning of the MI mandible must avoid occlusal interferences and adopt a deviated pattern of closure, which results in condylar distraction followed by orthopedic instability and defective programming of the masticatory muscles. Orthopedic stability is most efficaciously achieved via stabilization splint therapy which, by deprogramming the muscle engrams, eliminates the patient’s neuromuscular response to a deviated closure pattern dictated by the habitual position of MI [
17,
18].
Hence, the orthodontic diagnosis is most commonly made from the position of the MI, and an increased discrepancy between the CR and MI could also be a reason for inaccuracy in the orthodontic diagnosis [
19]. Deprogramming of the neuromuscular system might induce substantial changes in the interarch relationship and thus alter the dentofacial characteristics of the patient, directly interfering with a correct orthodontic diagnosis [
20,
21]. Recent studies have confirmed that the stable musculoskeletal position provided by stabilization splint therapy represents a major objective when making the correct orthodontic diagnosis and evaluating the overall condylar health of orthodontic patients with TMD [
22,
23,
24]. Even asymptomatic individuals with an increased CR–MI discrepancy need neuromuscular deprogramming to obtain a more accurate measurement of condylar displacement and to avoid inaccurate orthodontic diagnosis and treatment planning [
25,
26,
27]. To evaluate these changes, cephalometric head films are analyzed before and after muscle deprogramming with splint therapy.
Accordingly, the first hypothesis of this study was that there is a correlation between the signs and symptoms of TMD and increased CR–MI differences measured at the condyle level using a CPI. The second hypothesis was that neuromuscular deprogramming with a stabilization splint can have an impact on the orthodontic diagnosis after the condyles are placed in a stable musculoskeletal position.
The objectives of the study were as follows:
- -
To compare the mean values of sixteen variables from lateral cephalograms analyzed before and after neuromuscular deprogramming with a stabilization splint
- -
To statistically compare the prevalence of the anamnestic and clinical findings of TMDs evaluated before and after neuromuscular deprogramming with a stabilization splint;
- -
To evaluate the differences between the CR and MI at the level of the condyles using a CPI;
- -
To compare the prevalence of TMDs, condylar displacement, and cephalometric measurements among males and females.
2. Materials and Methods
2.1. Subjects
The sample for this study consisted of 60 patients (aged 18 to 30 years) diagnosed with the signs and symptoms of condylar distraction in the temporomandibular joint structures. The investigation was performed in the Demirović private practice for orthodontics and dentofacial orthopedics. The inclusion criteria were no history of orthodontic treatment, prosthetic treatment, orthognathic surgery, TMJ treatment, head or jaw trauma, muscle contracture, myositis, pain of odontogenic origin, or periodontal disease. Patients with rheumatoid arthritis or other systemic diseases were excluded from the study. Ethical approval of the research protocol was given by the Ethics Committee, School of Dental Medicine, University of Sarajevo.
2.2. Assessment of the Signs and Symptoms of TMD
A clinical assessment for TMD was performed according to the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) before and after therapy with a stabilization splint [
28]. A clinical assessment of all patients was conducted by the same trained examiner, an expert in the clinical evaluation of the signs and symptoms of TMD. The RDC/TMD protocol comprises of two axes: Axis I is used to assess the clinical signs and symptoms based on standardized diagnostic criteria, and Axis II is used to evaluate psychosocial distress and pain-related disability. Prior to palpation examination, finger pressure was calibrated to 0.5 or 1.0 kg using a digital algometer (depending on the area examined (temporomandibular joint structures, masticatory muscles)).
2.3. Assessment of Condylar Displacement before and after the Splint Therapy
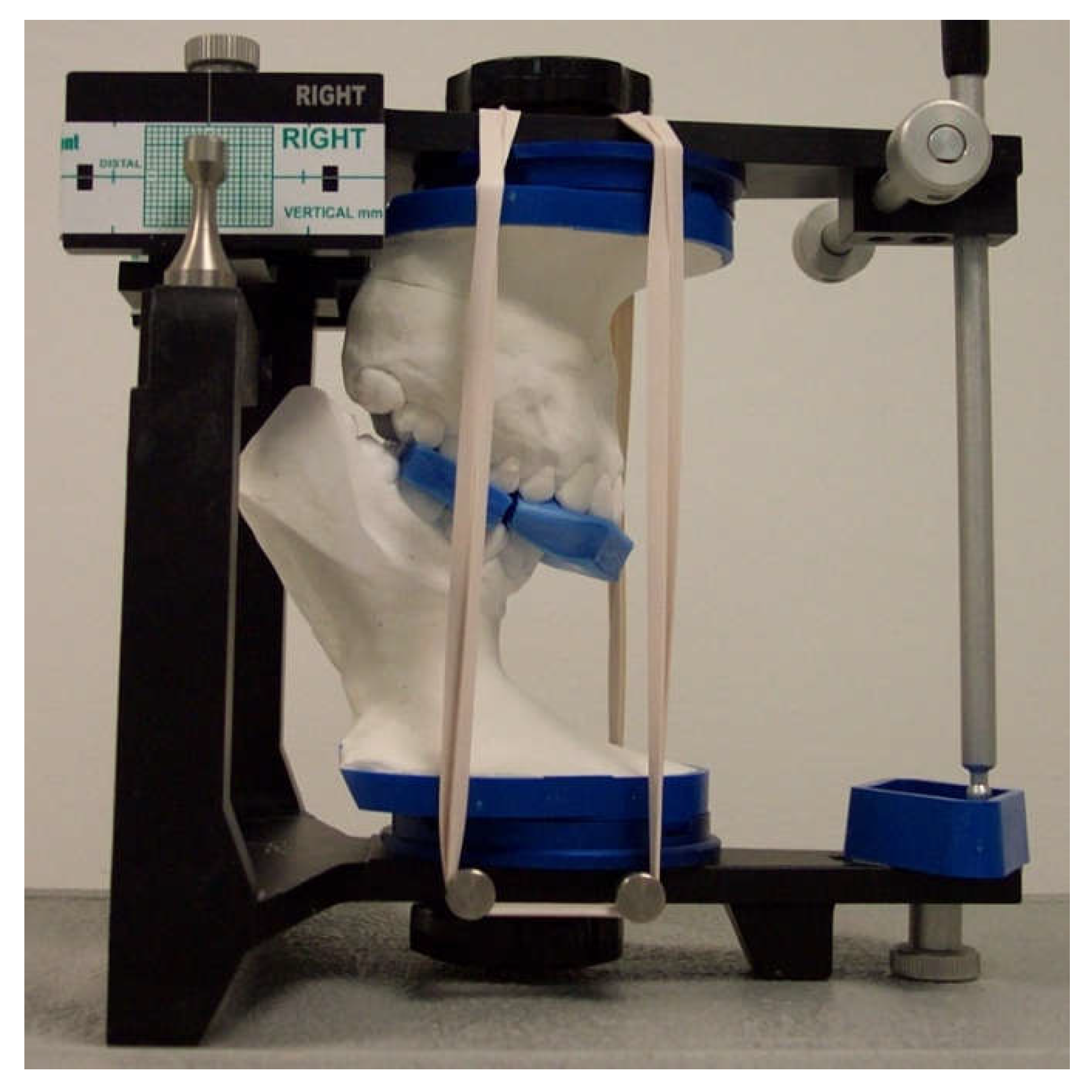
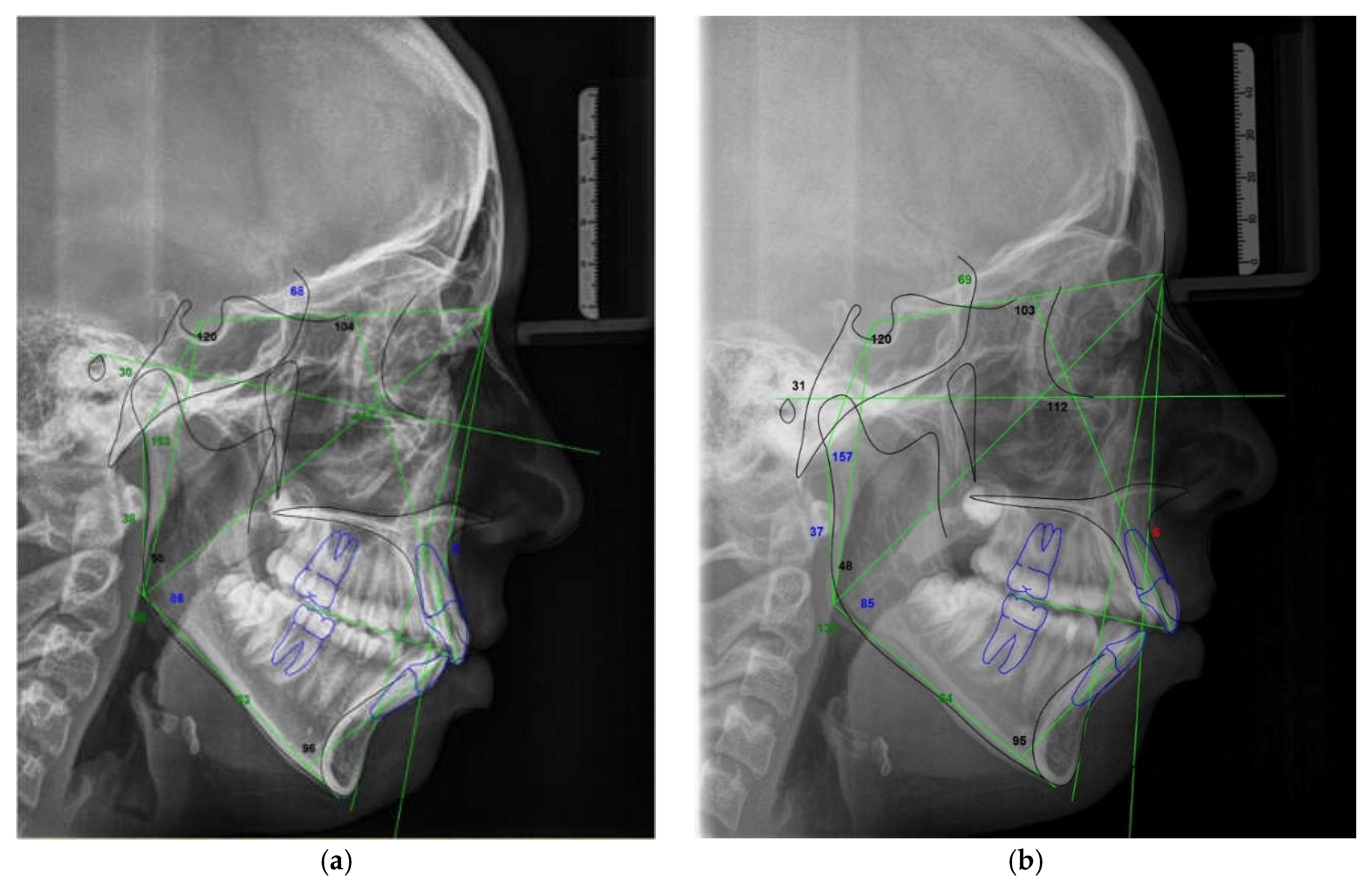
To assess the condylar position, diagnostic casts of all participants were mounted on a semi-adjustable articulator (Panadent Corp, Grand Terrace, CA, USA) using an estimated face-bow and CR bite registration taken with blue wax (Delar Corp, Lake Oswego, OR, USA) according to Roth’s power centric technique. To obtain a high degree of accuracy and verification of the articulator mounting, a split cast method was used. The anterior portion of the wax was folded in 4 layers over the incisor teeth region (canine–canine). For bite registration in the MI position, a single layer of hard pink wax (Beauty Pink Wax X Hard, Integra Miltex, York, PA, USA) was used. The mounted models were placed in a condylar position indicator articulator (Panadent Corp, Grand Terrace, CA, USA) to measure the amount of condylar discrepancy between the MI and CR positions using an initial MI and CR bite registration record. For the neuromuscular deprogramming, a hard acrylic stabilization splint was constructed according to the principles of a mutually protected occlusal scheme on models mounted in the CR position. All participants used the acrylic stabilization splint for approximately 6 months until a stable musculoskeletal position of the condyles in the CR was achieved (
Figure 1).
The indicator of a stable musculoskeletal position of the condyles in the fossa was three successive CR records with identical values measured at the condyle level using the CPI, easy manipulation of the mandible, and a stable mandibular position. After neuromuscular deprogramming, newly obtained dental casts were mounted on a semi-adjustable articulator according to the new CR bite registration. Afterwards, dental casts were placed in the CPI articulator where final MI and CR bite registrations were used to measure the condylar discrepancy between the CR and MI positions (
Figure 2).
The linear displacement of the condylar processes in a given axis was measured using graph paper and a magnifying glass with 0.1 mm measuring lines. All procedures were performed by the same trained operator except for the articulator mountings, which were carried out by a laboratory technician.
2.4. Radiologic Evaluation
Radiographic records were taken considering the natural head position, and they included the initial lateral cephalogram (T0) taken in the MI position before the splint therapy and the final lateral cephalogram (T1) taken in the CR position after the neuromuscular deprogramming with a stabilization splint. Sixteen cephalometric variables related to the maxillo–mandibular relationship, vertical skeletal relationship, size of the mandible, and dental relationship were evaluated on lateral cephalograms taken in the MI position before the splint therapy and on lateral cephalograms taken in the CR position after the splint therapy. Digital tracings and superimpositions of the pre-splint and post-splint lateral cephalograms were performed with Dolphin Imaging software, version 11.8 (Dolphin Imaging and Management, Chatsworth, CA, USA).
2.5. Statistical Analysis
The data are expressed as the mean ± standard deviation or number of cases with percentage, depending on the type of data. Cronbach’s alpha reliability test was used to evaluate the reliability of the sample size.
To compare the tested signs and symptoms of TMD before and after the splint therapy, Chi-square and Fisher’s exact test were used, while the differences in dentofacial characteristics between the T0 and T1 and differences in the condylar displacements were evaluated using the Wilcoxon signed-rank test. Spearman’s correlation test was used to evaluate the relationship between the CR–MI differences and the signs and symptoms of TMD. The level of significance was set at 95% (p < 0.05). The data were compared using the statistical package IBM Statistics SPSS v 23.0 (IBM Corp., Armonk, NY, USA).
3. Results
A statistically significant difference was observed between the results for the anamnestic and diagnostic criteria of the RDC/TMD protocol evaluated before and after the splint therapy. Out of 60 patients, 33 (55%) reported recurrent (75.8%) or persistent (24.2%) facial pain before the start of the splint therapy. After the splint therapy, no patient reported persistent pain, recurrent pain was reported by 1 (3.0%), and one-time pain was reported by 2 (6.1%) patients. RDC/TMD patients answered six questions on the history questionnaire regarding facial pain that were evaluated on a 0 to 10 numeric rating scale (NRS). When comparing the results obtained before and after the splint therapy, the level of facial pain reported by patients was significantly reduced after the splint therapy (
Table 1).
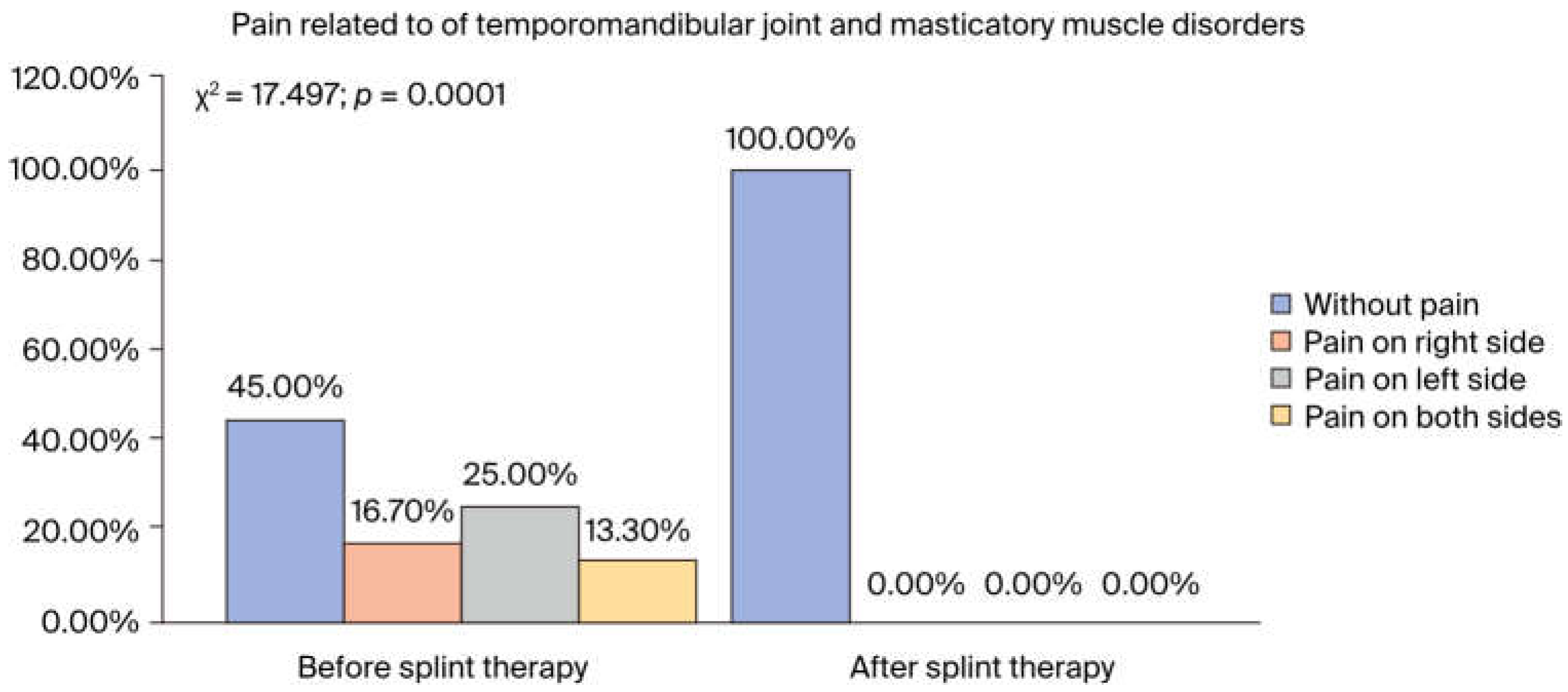
Before the splint therapy, pain related to temporomandibular joint and masticatory muscle disorders was reported by 55% of patients, on the right side by 16.7%, the left side by 25%, and both sides by 13.3%, while after the splint therapy, none of the patients reported pain in these structures (
p < 0.001) (
Figure 3).
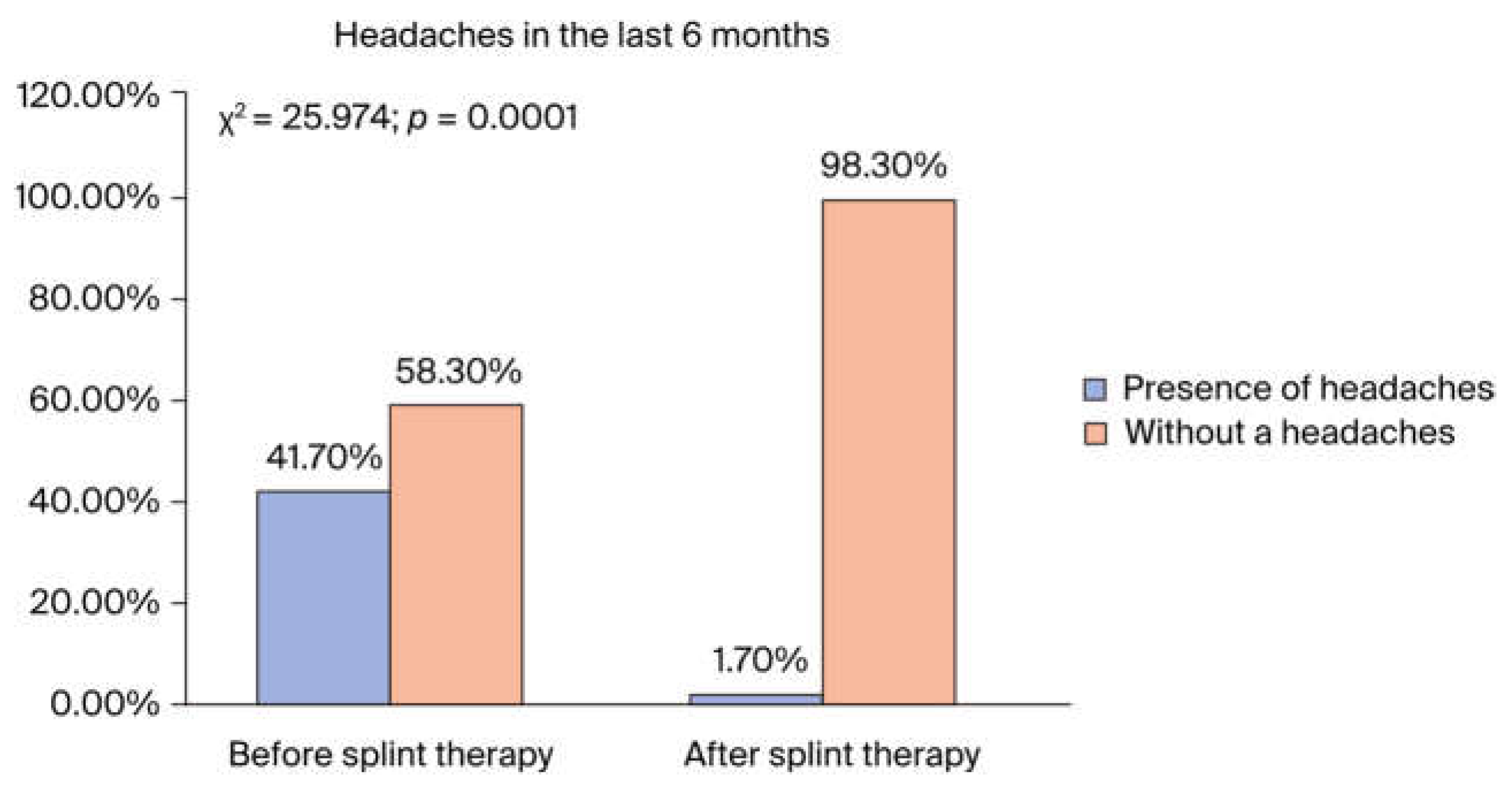
The self-reported headache frequency was 41.7% before the splint therapy, and after the splint therapy, only 1.7% of patients reported headaches (
Figure 4).
The self-reported prevalence of jaw clicking before the splint therapy was 70%, and after the splint therapy, it was reduced to 8.3% (
p < 0.001). Before the splint therapy, 40% of participants reported a locked jaw, while after the therapy, none of the participants reported jaw locking (
p < 0.001). Data regarding the other symptoms of TMD related to jaw dysfunction are presented in
Table 2.
According to the physical findings, after the splint therapy, a statistically significant reduction in muscular and temporomandibular joint pain was achieved for mouth opening and lateral excursion (p < 0.001). Tenderness to palpation in masticatory muscles and TMJ structures was recorded and graded as none, mild, moderate, or severe pain. Pain that was registered in the right and left masseter muscle (superficial, middle, and deep portions), temporalis (anterior, middle, posterior), posterior mandibular region (stylohyoid/posterior digastric region), submandibular region (medial pterygoid/suprahyoid/anterior digastric region) before the splint therapy was significantly reduced or completely disappeared after the splint therapy (p < 0.05 and p < 0.001). Before the splint therapy, tenderness was present in 96.7% of patients on the left and in 90% of patients on the right lateral pole, while after the therapy this was reduced to 8.3% on the left and 6.7% on the right lateral pole (p < 0.001). When comparing the results obtained before and after the splint therapy, a highly significant reduction in pain was observed in the lateral pterygoid area, tendon of temporalis, and posterior attachment after the splint therapy (p < 0.001).
When compared before and after, the mean CPI values of condylar displacement were significantly reduced on both sides of the vertical (
p < 0.001), horizontal (
p < 0.05), and transverse planes of space after the splint therapy (
p < 0.001). Alongside these findings, a significant reduction was found in both the male and female groups in the mean CPI values of condylar displacements on the right and left sides of the vertical (
p < 0.001), horizontal (
p < 0.05), and transverse planes (
p < 0.001) of space after the splint therapy. The frequency of directions of condylar displacements are presented in
Table 3.
Table 3.
Comparison of changes in condylar position evaluated before and after the splint therapy.
Table 3.
Comparison of changes in condylar position evaluated before and after the splint therapy.
| Changes in Direction of Condylar Displacement |
|---|
| n = 60 |
Before the Splint Therapy |
After the Splint Therapy |
| |
Right |
Left |
Right |
Left |
| |
Percentage |
Percentage |
| Posterior-inferior |
66.7% |
75% |
41.6% |
48.3% |
| Anterior-inferior |
26.6% |
20% |
6.7% |
11.7% |
| Straight inferior |
6.7% |
5% |
46.7% |
33.3% |
| Coincident CR-MI |
- |
- |
5% |
6.7% |
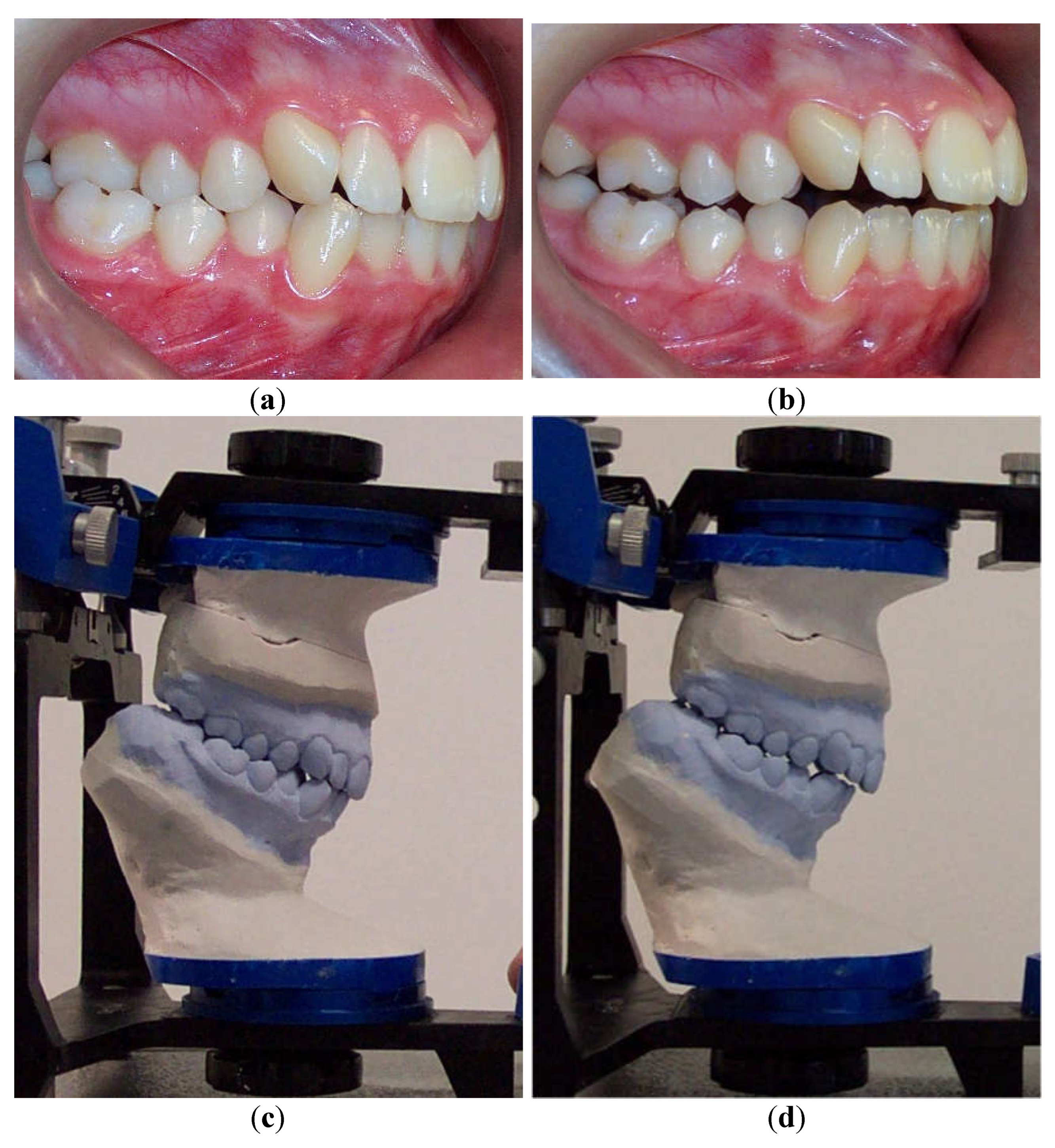
According to Spearman’s correlation, test results of the anamnestic and diagnostic criteria of RDC/TMD were strongly positively correlated (
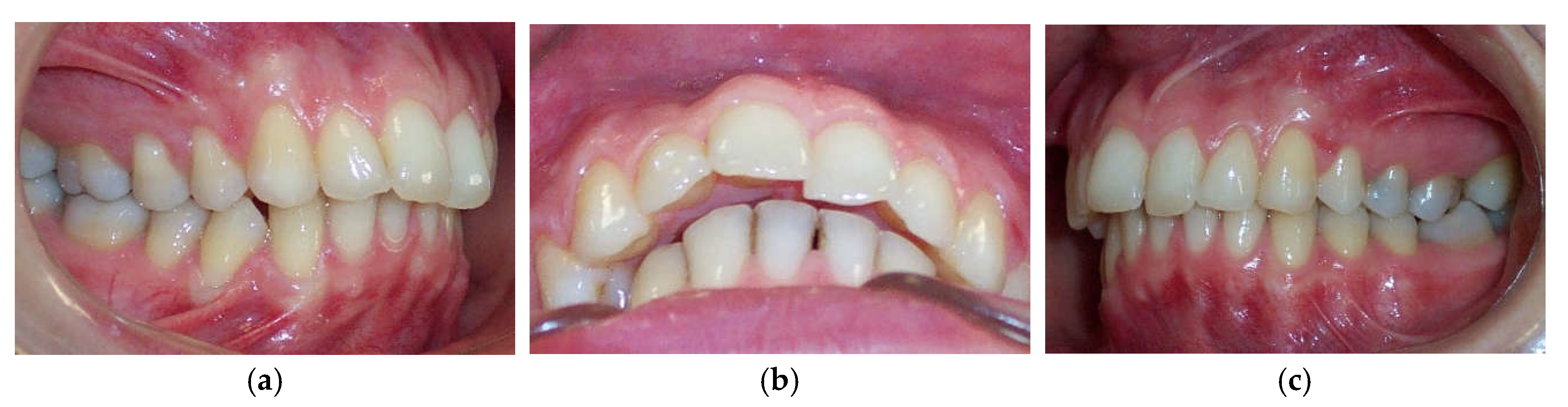
p < 0.05) with the condylar displacements in the vertical and transverse planes before the splint therapy. When compared before and after, interarch relationship changes were observed intraorally and from models mounted on a semi-adjustable articulator after the neuromuscular deprogramming (
Figure 5).
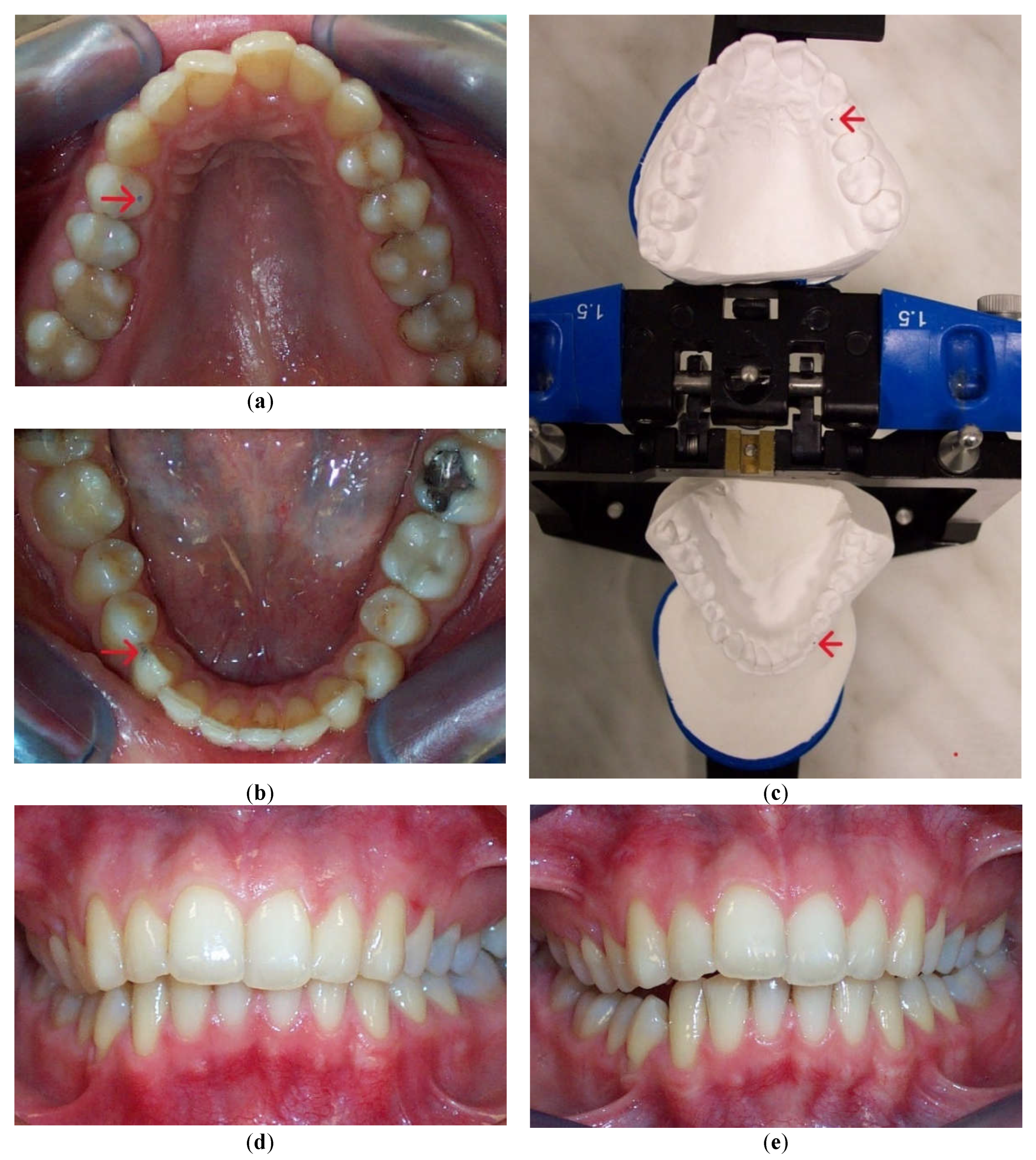
To accurately evaluate the effect of interarch relationship changes on dentofacial characteristics, cephalometric analysis of lateral cephalograms was performed before and after the splint therapy (
Figure 6).
There was no significant increase in cephalometric parameters related to the maxillo–mandibular relationship (SNA angle,
p = 0.431 and SNB angle,
p = 0.275), vertical skeletal relationship, or size of the mandible (mandibular length,
p = 0.958 and ramus height,
p = 0.985) (
Table 3).
Table 3.
Comparison of mean ± standard deviation values of cephalometric variables analyzed before and after splint therapy.
Table 3.
Comparison of mean ± standard deviation values of cephalometric variables analyzed before and after splint therapy.
| n = 60 |
Before Splint Therapy
Mean |
After Splint Therapy
Mean |
Z |
p Value |
| Maxillo–mandibular relationship |
| SNA angle (°) |
81.30 ± 4.01 |
81.84 ± 3.98 |
−0.787 |
0.431 |
| SNB angle (°) |
78.86 ± 4.58 |
78.08 ± 4.89 |
−1.092 |
0.275 |
| ANB angle (°) |
2.43 ± 2.54 |
3.73 ± 2.80 |
−2.704 |
0.007 |
| Wits appraisal (mm) |
0.59 ± 3.15 |
1.57 ± 3.51 |
2.286 |
0.022 |
| Vertical skeletal relationship |
|
|
| Saddle angle (N-S-Ar) ° |
120.61 ± 5.6 |
120.23 ± 5.67 |
−0.299 |
0.765 |
| Articular angle (S-Ar-Go) ° |
146.68 ± 7.75 |
148.67 ± 7.07 |
−1.441 |
0.150 |
| Mandibular angle (Ar-Go-Gn) ° |
127.28 ± 7.99 |
127.67 ± 7.92 |
−0.381 |
0.704 |
| Sum of angles ° |
394.60 ± 7.43 |
395.61 ± 7.44 |
−1.559 |
0.119 |
| Total anterior facial height (mm) |
115.66 ± 6.73 |
117.27 ± 7.03 |
−1.176 |
0.24 |
| Total posterior facial height (mm) |
75.49 ± 7.65 |
75.31 ± 7.48 |
−0.060 |
0.952 |
| Total anterior/posterior facial height |
65.28 ± 5.55 |
64.22 ± 5.33 |
−0.963 |
0.335 |
| (S-Go/N-Me) % |
| Maxillo-mandibular angle (PP-MP) (°) |
28.79 ± 7.47 |
29.84 ± 7.38 |
−0.672 |
0.502 |
| Size of mandible |
| Mandibular length (Go-Me) mm |
69.21 ± 5.72 |
69.18 ± 5.53 |
−0.052 |
0.958 |
| Ramus height (Ar-Me) mm |
43.81 ± 5.92 |
43.74 ± 5.97 |
−0.018 |
0.985 |
| Dental relationship |
| Overjet (mm) |
3.14 ± 1.76 |
4.79 ± 2.32 |
4.856 |
0.0001 |
| Overbite (mm) |
1.75±1.80 |
0.45±1.59 |
-4.119 |
0.0001 |
When comparing the mean values measured before and after the splint therapy in the female group, we observed a significant increase in the mean values for ANB angle (p = 0.006), Wits appraisal (p = 0.007), and overjet (p = 0.0001), while for overbite, a significant decrease in mean values was found (p = 0.0001) after the splint therapy. In the male group, the mean values for overjet significantly increased (p = 0.019) and those for overbite significantly decreased (p = 0.023) after the splint therapy.
For all other cephalometric parameters related to the maxillo–mandibular relationship, vertical skeletal relationship, and mandible size, a significant difference in mean values evaluated before and after the splint therapy was not evidenced. It was found that, in patients with a large CR–MI discrepancy after deprogramming the neuromuscular system, the mandible was positioned more posteriorly and rotated more in a clockwise direction, enhancing a hyperdivergent facial type. The result of the Cronbach’s alpha analysis (0.705) was above 0.7, so the sample size was considered reliable.
4. Discussion
The orthodontic treatment of patients with the signs and symptoms of TMD represents a distinct challenge when the diagnosis and treatment plan are considered. Myriad studies have shown that condylar displacements related to an unstable musculoskeletal position of the condyles in the fossa are the primary etiologic factors of TMJ and masticatory muscle disorders [
5,
6,
7,
8,
9,
10,
12,
13,
14,
15,
16,
20,
22,
23,
24,
29,
30]. Occlusal interferences are regarded as being most responsible for the development of orthopedic instability. Increased activity of the lateral pterygoid muscle provoked by a periodontal proprioceptive response from the teeth involved in premature contact causes the mandible to avoid these prematurities, displacing the condyles out of the fossa [
9,
31]. Condylar distraction creates an overactivity of elevator muscles and thus leads to an imbalance between the antagonistic masticatory muscles. The more the condyle is distracted out of the fossa, the more the muscle imbalance is enhanced and the discrepancy between the CR and MI increased, imperceptibly leading to the development of TMDs and orofacial pain [
31].
Currently, condylar displacement or an increased CR–MI discrepancy is equated with the orthopedically unstable musculoskeletal position of the condyles in the fossa. Okeson classified orthopedic instability between the CR and MI as the primary factor in temporomandibular and masticatory muscle disorders [
32]. Earlier investigations pointed out the importance of CR–MI coincidence at the level of the condyles as the guarantee of a stable musculoskeletal position of the condylar processes in the fossa [
7,
8,
10,
11,
12,
14,
23,
24,
26,
27]. To eliminate CR–MI discrepancies and obtain an orthopedically stable position of the condyles in the fossa, the neuromuscular system needs deprogramming, and for this purpose, stabilization splint therapy has been proven to be the most effective [
33]. The more complete condylar seating provided by stabilization splint therapy induces muscle relaxation, reduces pain in muscles and TMJ structures, and has a positive effect on intracapsular disorders [
32,
34,
35,
36]. Notwithstanding the above, some studies have reported no relationship between occlusion and TMD; such studies were based only on questionnaires, hand-held cast analysis, or pure intraoral observations, where researchers did not use any instrumentation modality for TMDs [
37,
38,
39,
40]. Although Manfredini et al., in their systematic review, found that features of CR–MI slide and mediotrusive contacts have a clinically significant association with TMD, they disregarded the role of occlusion and even encouraged clinicians to abandon the principles of gnathology [
41]. The measurement of condylar displacement using CPI instrumentation represents the only way to evaluate the position of condylar processes in three dimensions, as cases of transverse plane condylar displacement cannot be detected by means of clinical examination, analysis of hand-articulated casts, the use of radiography, or scan imaging. In our study, articulator mountings of all dental casts were performed before and after the neuromuscular deprogramming with a stabilization splint and subsequently evaluated for condylar displacements with the CPI device. Results of this study demonstrated that the mean values of condylar displacement obtained after the splint therapy significantly decreased for all three spatial planes in comparison to those measured before the splint therapy. Our findings concurred with the results of similar studies [
7,
29,
42]. All subjects had a significant condylar displacement present in at least one plane of space before splint therapy. Condylar displacements registered before the splint therapy were mostly in the posteroinferior, anteroinferior, and straight inferior directions, in agreement with the findings of similar studies [
12,
14,
16,
43]. After the splint therapy, the direction of condylar displacement indicated that the condyles were converging toward the CR position as the difference between the CR and MI decreased. This was most distinctly demonstrated by a significant increase in the percentage of minor displacements in the straight inferior and in cases where the CR and MI positions were coincident, with no condylar displacement.
The significant reduction in condylar displacement and the achievement of an orthopedically stable musculoskeletal position following the splint therapy directly correlated with the improvement in TMD symptomatology. Hence, the pain related to the area of the temporomandibular joint and masticatory muscles reported by 55% of patients before the splint therapy was completely eliminated after the splint therapy, and this result was the same for the intermittent jaw locking. Following the splint therapy, headache symptoms were reduced for more than 90% of patients, corresponding with the study findings of Kemper and Okeson [
44]. After the splint therapy, jaw clicking was reduced for more than 80% of patients. Clinical findings regarding the signs of tenderness on palpation in the masticatory muscles, lateral pole, temporalis tendon, and posterior attachment inside the ear showed a statistically significant reduction in signs after the splint therapy. Crawford reported a significant increase in the signs and symptoms of TMD as the condylar displacement in vertical and horizontal planes was raised from 1 to 2 mm [
12]. He et al. demonstrated that 72.9% of pre-treated orthodontic patients with signs and symptoms of TMD had a condylar displacement greater than 1 mm in the vertical and horizontal and 0.5 mm in the transverse plane, while only 11.4% of asymptomatic patients in the control group had increased condylar displacement. They then concluded that the condylar displacements identified in symptomatic patients were a significant contributory factor to the development of signs and symptoms of TMD [
15]. This study found that the significant reduction in condylar displacement obtained via the splint therapy directly correlated with the improvement or elimination of signs and symptoms of TMD, concurring with the findings of similar investigations [
7,
12,
22,
23,
24,
29]. Moreover, our results agreed with those of authors who found a positive correlation between therapy with an occlusal splint constructed in the CR position and improvement in TMD symptomatology, albeit that in these investigations, CPI evaluation was not used [
45,
46,
47,
48,
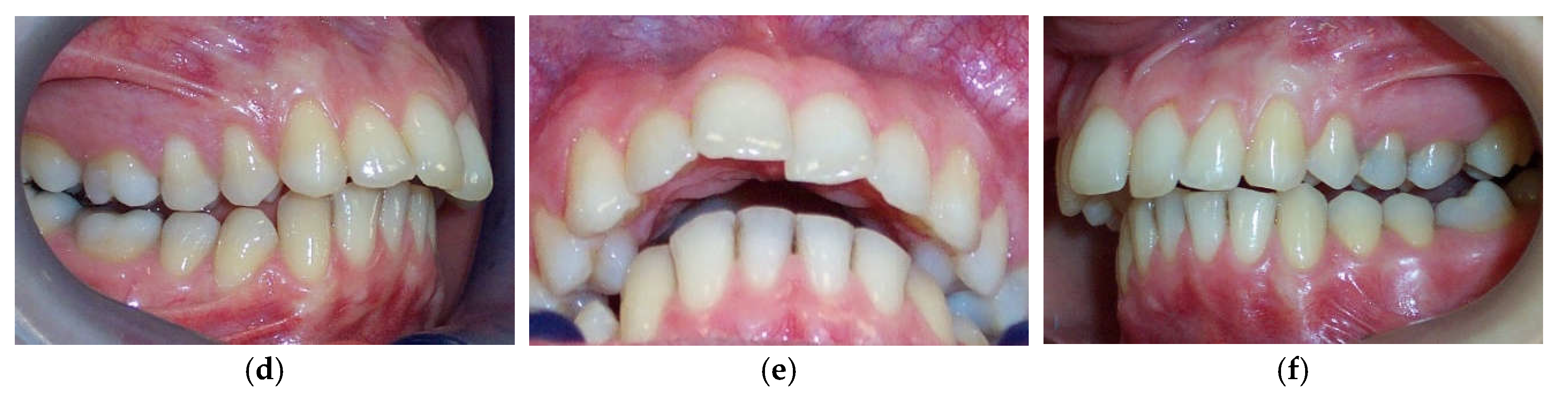
49]. Furthermore, a significant increase in condylar displacement between the CR and MI generates changes in the dental relationship that can be observed intraorally in the CR position and from dental casts mounted in the CR. Changes in dental interarch characteristics that occur following deprogramming of the neuromuscular system are presented in
Figure 7 and
Figure 8.
The changes in dental interarch relationship characteristics that occur after the splint therapy might alter the type of dental malocclusion and indirectly affect a correct orthodontic diagnosis. To accurately evaluate the impact of interarch relationship changes on facial characteristics and orthodontic diagnostic procedures, an evaluation of cephalometric data was performed. We analyzed differences in cephalometric measurements between the cephalograms traced in the MIP before and in the CR position after the neuromuscular deprogramming and evaluated the eventual changes in dentofacial characteristics. Eight linear and eight angular cephalometric variables were evaluated on pre- and post-lateral cephalograms. After comparison before and after the splint therapy, the results of this study showed statistically significant differences for overjet, overbite, ANB angle, and Wits appraisal variables, in agreement with earlier studies in which authors found differences for similar parameters [
20,
21,
37]. The significantly larger values of ANB, overjet, Wits appraisal, and the smaller value of the overbite variable most substantially contributed to changes in dentofacial characteristics, whereby most subjects acquired a more dolichofacial skeletal pattern and retrognathic position of the mandible in the CR position. Our findings were in close agreement with similar investigations by other authors [
20,
21,
22,
23,
24,
37].
The values of the angular measurements that determine the vertical skeletal relationship (Bjork polygon angles, articular angle, maxillo–mandibular angle) also increased after the neuromuscular deprogramming, but without statistical significance. Nevertheless, an increase in specified angular measurements and a decrease in total anterior/posterior facial height ratio were additional indicators of incurred changes in dentofacial characteristics after the splint therapy (clockwise rotation and posterior positioning of the mandible) was completed. Previous studies have shown how substantial changes in dentofacial characteristics that occur after neuromuscular deprogramming might have a significant effect on orthodontic diagnostic procedures [
19,
20,
21,
37,
50,
51,
52]. In accordance with obtained data, earlier authors have recommended that analysis of the lateral cephalograms should be carried out from the most stable musculoskeletal position designated as the CR position to avoid orthodontic misdiagnosis [
19,
20,
21,
27,
46]. The results of our study were in line with the findings of the most recent studies, which confirmed the theory that the orthodontic diagnosis and plan of treatment should start from the CR as the most orthopedically stable position of the condyles in the fossa [
22,
24,
25,
27,
53]. Orthodontic diagnosis should be based on post-splint records; thus, the most accurate and definitive orthodontic diagnosis and treatment plan can be provided.
Concerning the inconvenience of mounting every patient’s cast, a standardized procedure of mounting the casts of patients with an unstable musculoskeletal position of the condylar processes to identify masked CR–MI discrepancies should be practiced. Increased hyperdivergence and mandibular retrusion attained as a result of unmasked CR–MI discrepancies could exacerbate Class II malocclusion and cause remarkable changes in orthodontic treatment planning. These changes imply that the non-extraction case might be converted to an extraction case or non-surgical to surgical treatment planning. The findings of this study suggest that, to identify masked CR–MI discrepancies and avoid orthodontic misdiagnosis, mounting the casts of patients who present the signs and symptoms of TMD associated with orthopedic joint instability should be a standardized procedure. Furthermore, a substantial amelioration of TMD symptomatology and achievement of orthopedic condylar stability after the splint therapy represent a valid argument for the merits of the stabilization splint as a standardized procedure for patients with orthopedic instability accompanied by TMDs. Progression of development of TMD
In order to reduce a potential risk for development of signs and symptoms of TMDs orthodontists should check on orthopedic instability and accordingly provide a treatment the patients
4.1. Advantages and Limitations of the Study
The advantage of this study was that correlation between the TMD symptomatology and amount of condylar displacement was analyzed and its positive correlation directly addressed to question of increased controversy regarding the relationship between the occlusion and TMDs. As advantageous, this study has presented how important is to establish orthopedically stable musculoskeletal position when condylar and masticatory structure health is considered and how orthopedically stable condylar position is in direct correlation with making of an accurate orthodontic diagnosis. Limitation of the present study was disuse of cone beam computed tomography (CBCT) or magnetic resonance imaging (MRI) on the TMJ condyle and TMJ disc.
4.2. Further Directions for Research
Longitudinal studies using experimental animal models and MRI should be performed to evaluate the long-term effect of orthopedic instability on dynamic functions of the masticatory muscle and TMJ system. A greater number of similar studies would provide a sufficient data for conducting a meta-analysis which would enable orthodontists to thoroughly consider an importance for establishing of an orthopedically stable position of the condyles in the fossa. Further research should be directed towards investigation of factors that affect patient’s individual capacity of adaptation to condition of orthopedically unstable musculoskeletal position demonstrated by increased CR-MI disharmony. Considering the presence of masked interocclusal relationships in patients with orthopedic instability, classification of patients according to type of malocclusion might be excluded as a part of methodology in the future studies. After an orthopedic stability was established by splint therapy, focus of further research should be on development of most convenient treatment strategies on how to maintain an orthopedic stability during following stages of orthodontic therapy. Effectiveness of occlusal splint therapy performed by occlusal splint constructed using conventional articulator and occlusal splint constructed using virtual articulator should be compared in the future investigations. Greater sample size might further enhance reliability and validity of the study results.
5. Conclusions
The stable musculoskeletal position and more coincident CR–MI relationship obtained after stabilization splint therapy were positively correlated with the reduction/elimination of the signs and symptoms of TMD.
Mean condylar displacements registered after deprogramming the neuromuscular system proved to be significantly lower than those attained before neuromuscular deprogramming in the cases of all three spatial planes.
During change from orthopedically unstable (MI) to orthopedically stable musculoskeletal position (CR), the mandible moved backward and rotated clockwise, contributing to a more dolichofacial skeletal pattern.
There were no statistically significant differences between genders
In patients with the signs and symptoms of TMD and unstable musculoskeletal position, deprogramming the neuromuscular system with stabilization splint therapy is highly indicated to ameliorate TMDs and facilitate making of a definitive orthodontic diagnosis from an orthopedically stable musculoskeletal position.
When indicated, orthodontists are required to establish musculoskeletally stable relationship between the positions of MI and CR in order to reduce potential risk factors for development of signs and symptoms of TMD.
Author Contributions
Conceptualization, K.D. and E.N.; methodology, K.D.; acquisition, analysis, resources and investigation, K.D;, drafting the work, K.D.; reviewing, K.D., V.Dz. and E.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the School of Dental Medicine, University of xxxxxxxx.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to gratefully acknowledge Muhamed Ajanovic at the Department of Prosthodontics, University of Sarajevo, for his valuable contribution to the study and Dubravko Vanicek for his assistance in analysis, statistical data processing, and editing.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Marklund, S.; Wänman, A. Risk factors associated with incidence and persistence of signs symptoms of temporomandibular disorders. Acta Odontol. Scand. 2010, 68, 289–299.
- Liu, F.; Steinkeler, A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent. Clin. N. Am. 2013, 57, 465–479. PMID: 23809304. [CrossRef]
- Dawson, P.E. Evaluation, Diagnosis, and Treatment of Occlusal Problems, 2nd ed.; Mosby; St. Louis, MO, USA, 1989; Volume 28, pp. 41–45.
- Lee GH, Lee SM, Park JH. The role of mandibular stabilization in orthognathic surgery. Semin. Orthod. 2019, 25, 188-204.
- Padala, S.; Padmanabhan, S.; Chithranjan, A.B. Comparative evaluation of condylar position in symptomatic (TMJ dysfunction) and asymptomatic individuals. Indian J. Dent. Res. 2012, 23, 122. PMID: 22842268. [CrossRef]
- Pullinger, A.G.; Seligman, D.A. Quantification and validation of predictive values of occlusal variables in temporomandibular disorders using a multifactorial analysis. J. Prosthet. Dent. 2000, 83, 66–75.
- He, S.; Wang, S.; Song, F.; Wu, S.; Chen, J.; Chen, S. Effect of the use of stabilization splint on masticatory muscle activities in TMD patients with centric relation-maximum intercuspation discrepancy and absence of anterior/lateral guidance. Cranio 2021, 39, 424–432. PMID: 31429383. [CrossRef]
- Roth, R.H.; Rolfs, D.A. Functional occlusion for the orthodontist. Part II. J. Clin. Orthod. 1981, 15, 100–123.
- Roth, R.H. Functional occlusion for the orthodontist. Part III. J. Clin. Orthod. 1981, 15, 174–198.23.
- Okeson, J.P. Evolution of occlusion and temporomandibular disorder in orthodontics: Past, present, and future. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 216–223. PMID: 25925651. [CrossRef]
- Dawson, P.E. New definition for relating occlusion to varying conditions of the temporomandibular joint. J. Prosthet. Dent. 1995, 74, 619–627. PMID: 8778387. [CrossRef]
- Crawford, S.D. Condylar axis position, as determined by the occlusion and measured by the CPI instrument, and signs and symptoms of temporomandibular dysfunction. Angle. Orthod. 1999, 69, 103–116. PMID: 10227550. [CrossRef]
- Roth, R.H. Functional occlusion for the orthodontist. J. Clin. Orthod. 1981, 15, 32–51. PMID: 6940863.
- Cordray, F.E. Articulated dental cast analysis of asymptomatic and symptomatic populations. Int. J. Oral Sci. 2016, 8, 126–132. PMID: 27357324. [CrossRef]
- He, S.S.; Deng, X.; Wamalwa, P.; Chen, S. Correlation between centric relation–maximum intercuspation discrepancy and temporomandibular joint dysfunction. Acta Odontol. Scand. 2010, 68, 368–376. PMID: 209426. [CrossRef]
- Weffort, S.Y.; de Fantini, S.M. Condylar displacement between centric relation and maximum intercuspation in symptomatic and asymptomatic individuals. Angle. Orthod. 2010, 80, 835–842. PMID: 20578853. [CrossRef]
- Kuzmanovic Pficer, J.; Dodic, S.; Lazic, V.; Trajkovic, G.; Milic, N.; Milicic, B. Occlusal stabilization splint for patients with temporomandibular disorders: Meta-analysis of short and long term effects. PLoS ONE 2017, 12, e0171296. PMID: 28166255. [CrossRef]
- Okeson, J.P., Ikeda, K. Orthodontic therapy and the patient with temporomandibular disorder. In: Graber, L.W., Vanarsdall, R.L. Jr., Vig, K.W., editors. Orthodontics: Current Principles and Techniques. 5th ed Philadelphia: Mosby; 2011, P. 178-184.
- Parreiras Ferreira, R.; Isaias Seraidarian, P.; Santos Silveira, G.; Campolina Rebello Horta, M.; Martin Palomo, J.; Andrade, I. Jr. How a Discrepancy Between Centric Relation and Maximum Intercuspation Alters Cephalometric and Condylar Measurements. Compend. Contin. Educ. Dent. 2020, 41, e1–e6. PMID: 32250125.
- Lim, W.H.; Choi, B.; Lee, J.Y.; Ahn, S.J. Dentofacial characteristics in orthodontic patients with centric relation-maximum intercuspation discrepancy. Angle. Orthod. 2014, 84, 939–945. PMID: 24673658. [CrossRef]
- Shildkraut, M.; Wood, D.P.; Hunter, W.S. The CR-CO discrepancy and its effect on cephalometric measurements. Angle. Orthod.1994, 64, 333-342.
- Zhao, M.; Wang, P.; Wang, H.; Li, X.; Bai, D.; Tian, Y. Diagnostic and treatment protocol for a patient with temporomandibular disorder using a stabilization splint and temporary anchorage devices. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 666–681. PMID: 33653641. [CrossRef]
- Lee, G.H.; Park, J.H.; Moon, D.N.; Lee, S.M. Protocols for orthodontic treatment of patients with temporomandibular joint disorders. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 373–378.
- Lee, G.H.; Park, J.H.; Sang, M.L.; Kim, E.J.; Lim, S.W.; Moon, D. An orthodontic treatment case of TMD patients with maxillary posterior intrusion using TSADs. Appl. Sci. 2022, 12, 12098.
- Demirovic, K.; Demirovic, E.; Dzemidzic, V.; Nakas, E. Assessment of condylar position in asymptomatic individuals before and after neuromuscular deprogramming with a stabilization splint. Srp. Arh. Celok. Lek. 2023, 151, 165–171. [CrossRef]
- Fantini, S.M.; Paiva, J.B.; Rino Neto, J.; Dominguez, G.C.; Abrao, J.; Vigoritto, J.W. Increase of condylar displacement between centric relation and maximal habitual intercuspation after occlusal splint therapy. Braz. Oral Res. 2005, 19, 176–182. PMID: 16308604. [CrossRef]
- Park, J.H.; Lee, S.M.; Moon, D.N.; Lee, G.H. Clinical application of a maximum intercuspal position-centric relation occlusion conversion of a lateral cephalogram in the treatment of orthodontic patients. Am. J. Orthod. Dentofac. Orthop. Clin. Companion. 2021, 1, 127–135. [CrossRef]
- Dworkin, S.F.; LeResche, L. Research diagnostic Criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J. Craniomandib. Disord. 1992, 6, 301–355.
- Girardot, A. The nature of condylar displacement in patients with temporomandibular pain-dysfunction. Orthod. Rev. 1987, 1, 16–23. PMID: 3479742.
- Demirovic, K.; Ovsenik, M. Relationship between the centric relation—Centric occlusion discrepancy and signs and symptoms of temporomandibular dysfunction, as measured by the condylar position indicator instrument, and effect of splint therapy on temporomandibular dysfunction. South. Eur. J. Orthod. Dentofac. Res. 2014, 1, 31.
- Dawson, P.E. Functional Occlusion: From TMJ to Smile Design; Mosby: St. Louis, MO, USA, 2007.
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 8th ed.; CV Mosby: St. Louis, MO, USA, 2020.
- Magnusson, T.; Adiels, A.M.; Nilsson, H.L.; Helkimo, M. Treatment effect on signs and symptoms of temporomandibular disorders--comparison between stabilisation splint and a new type of splint (NTI). A pilot study. Swed. Dent. J. 2004, 28, 11–20. PMID: 15129601.
- Al-Moraissi, E.A.; Farea, R.; Qasem, K.A.; Al-Wadeai, M.S.; Al-Sabahi, M.E.; Al-Iryani, G.M. Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: Network meta-analysis of randomized controlled trials. Int. J. Oral. Maxillofac. Surg. 2020, 49, 1042–1056. PMID: 31982236. [CrossRef]
- Greco, P.M.; Vanarsdall, R.L., Jr.; Levrini, M.; Read, R. An evaluation of anterior temporal and masseter muscle activity in appliance therapy. Angle. Orthod. 1999, 69, 141–146. PMID: 10227554. [CrossRef]
- Daif, E.T. Correlation of splint therapy outcome with the electromyography of masticatory muscles in temporomandibular disorder with myofascial pain. Acta Odontol. Scand. 2012, 70, 72–77. PMID: 21728748. [CrossRef]
- Pullinger, A.G.; Seligman, D.A.; Solberg, W.K. Temporomandibular disorders. Part II: Occlusal factors associated with temporomandibular joint tenderness and dysfunction. J. Prosthet. Dent. 1988, 59, 363–367. PMID: 3162277. [CrossRef]
- Turp, J.C.; Greene, C.S.; Strub, J.R. Dental occlusion: A critical reflection on past, present and future concepts. J. Oral Rehabil. 2008, 35, 446–453.
- Manfredini, D.; Perinetti, G.; Stellini, E.; Di Leonardo, B.; Guarda-Nardini, L. Prevalence of static and dynamic dental malocclusion features in subgroups of temporomandibular disorder patients: Implications for the epidemiology of the TMD-occlusion association. Quintessence. Int. 2015, 46, 341–349. PMID: 25386633. [CrossRef]
- McNamara, J.A., Jr.; Seligman, D.A.; Okeson, J.P. Occlusion, Orthodontic treatment, and temporomandibular disorders: A review. J. Orofac. Pain. 1995, 9, 73–90. PMID: 7581209.
- Manfredini, D.; Lombardo, L.; Siciliani, G. Temporomandibular disorders and dental occlusion. A systematic Review of association studies: End of an era? J. Oral Rehabil. 2017, 44, 908–923. PMID: 28600812. [CrossRef]
- Yoon, Y.J.; Kim, K.W. The influence of stabilization splint on condylar position and craniofacial morphology. Korean J. Orthod. 1995, 25, 675–688. PMID: 1977034.
- Williamson, E.H.; Evans, D.L.; Barton, W.A.; Williams, B.H. The effect of bite plane use on terminal hinge axis location. Angle. Orthod. 1977, 47, 25–33. PMID: 264774. [CrossRef]
- Kemper, J.T.; Okeson, J.P. Craniomandibular Disorders and Headaches. J. Prosthet. Dent. 1983, 49, 702–705. [CrossRef]
- Dylina, T.J. A common-sense approach to splint therapy. J. Prosthet. Dent. 2001, 86, 539–545. PMID: 11725283. [CrossRef]
- Okeson, J.P.; Kemper, J.T.; Moody, P.M. A study of the use of occlusion splints in the treatment of acute and chronic patients with craniomandibular disorders. J. Prosthet. Dent. 1982, 48, 708–712. PMID: 6961210. [CrossRef]
- Wahlund, K.; List, T.; Larsson, B. Treatment of temporomandibular disorders among adolescents: A comparison between occlusal appliance, relaxation training, and brief information. Acta Odontol. Scand. 2003, 61, 203–211. PMID: 14582587. [CrossRef]
- Clark, G.T. A critical evaluation of orthopedic interocclusal appliance therapy: Design, theory, and overall effectiveness. J. Am. Dent. Assoc. 1984, 108, 359–364. PMID: 6371096. [CrossRef]
- Williamson, E.H.; Lundquist, D.O. Anterior guidance: Its effect on EMG activity of the temporal and masseter muscles. J. Prosthet. Dent. 1983, 49, 816–823.
- Park, J.S.; Kim, J.C.; Hwang, H.S. The effect of CR-CO discrepancy on cephalometric measurements in Class III malocclusion patients. Korean J. Orthod. 1996, 26, 255–266.
- Wood, C.R. Centrically related cephalometrics. Am. J. Orthod. 1977, 71, 156–172.
- Williamson, E.H.; Caves, S.A.; Edenfield, R.J.; Morse, P.K. Cephalometric analysis: Comparisons between maximum intercuspation and centric relation. Am. J. Orthod. 1978, 74, 672–677. PMID: 281875. [CrossRef]
- Lee, G.H.; Park, J.H.; Lee, S.M.; Moon, D.N. Orthodontic Treatment Protocols for Patients with Idiopathic Condylar Resorption. J. Clin. Pediatr. Dent. 2019, 43, 292–303. PMID: 31094632. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).