Submitted:
19 July 2024
Posted:
23 July 2024
You are already at the latest version
Abstract
Keywords:
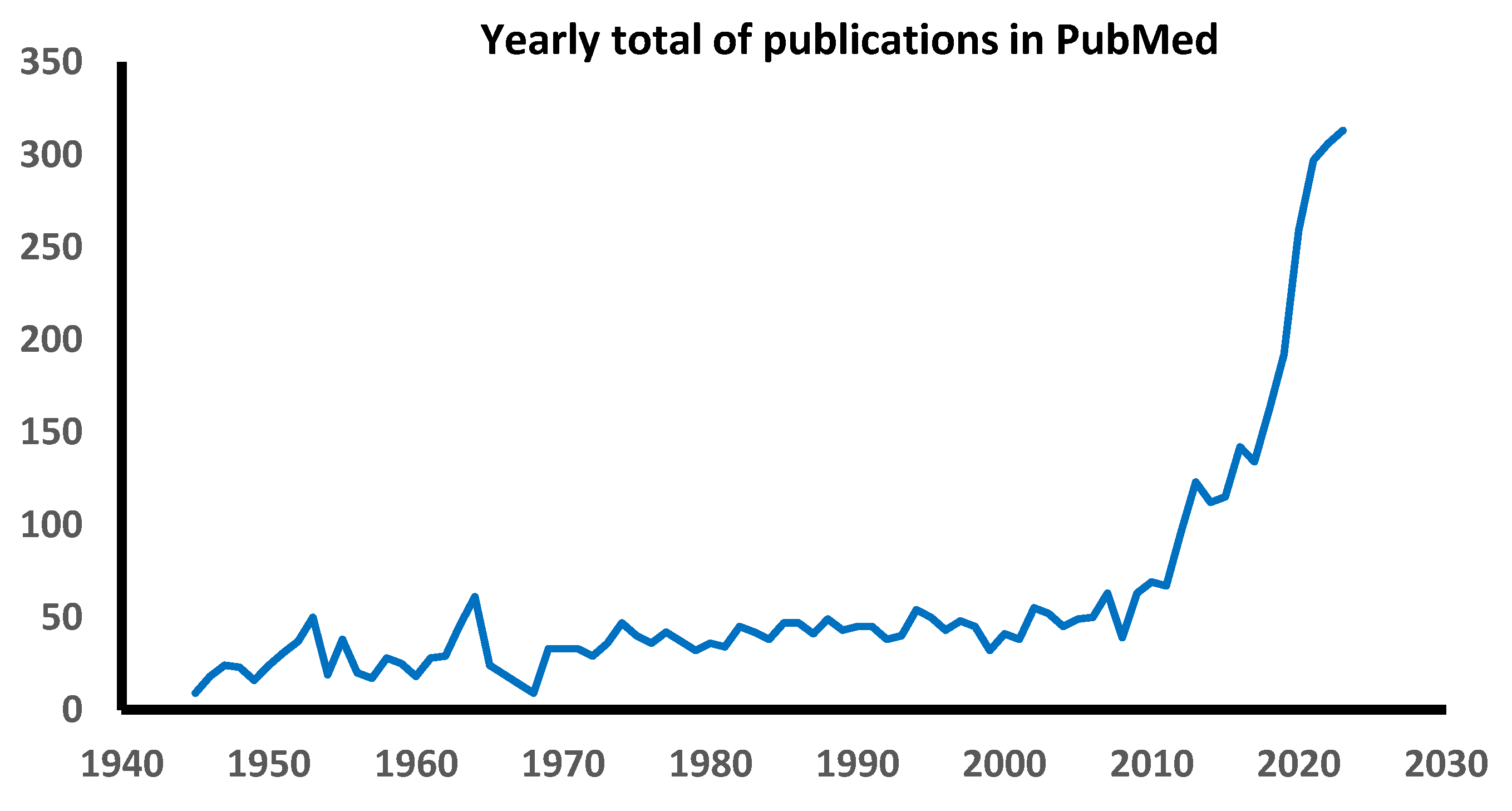
1. Introduction
2. Clinical Characteristics of FND
3. Biomarkers for FND
3.1. Advanced Structural Brain Imaging Findings in FND
3.2. Genetic Analyses
3.3. Low-Grade Inflammatory Biomarkers
3.3. Autonomic Disturbance in Canonical Neurological Disease and FND
3.3.1. Increased Cardiac Contraction Rate
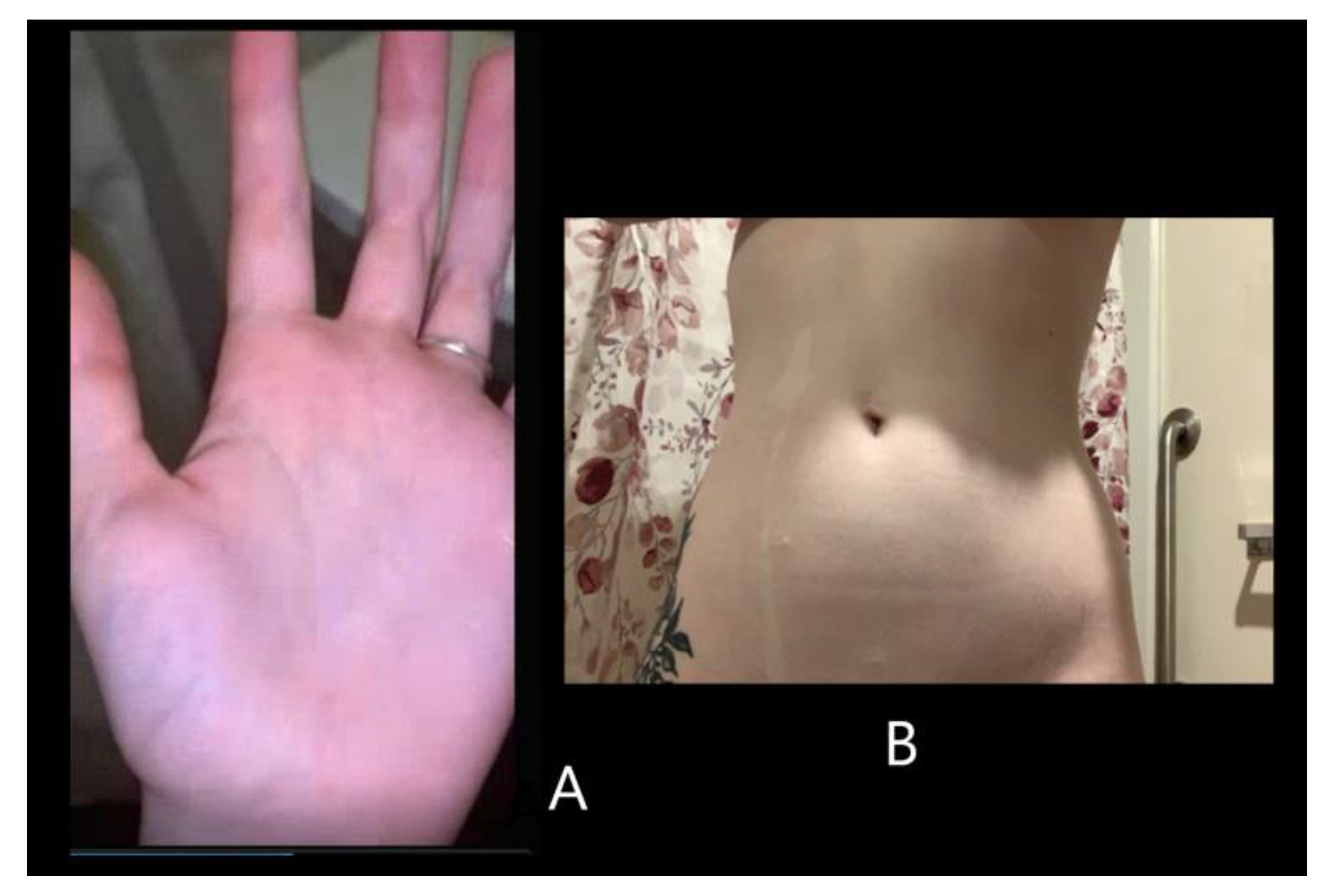
3.3.2. Superficial Tissue Blood Flow and Temperature Changes
3.3.3. Gastrointestinal Motility Disturbances
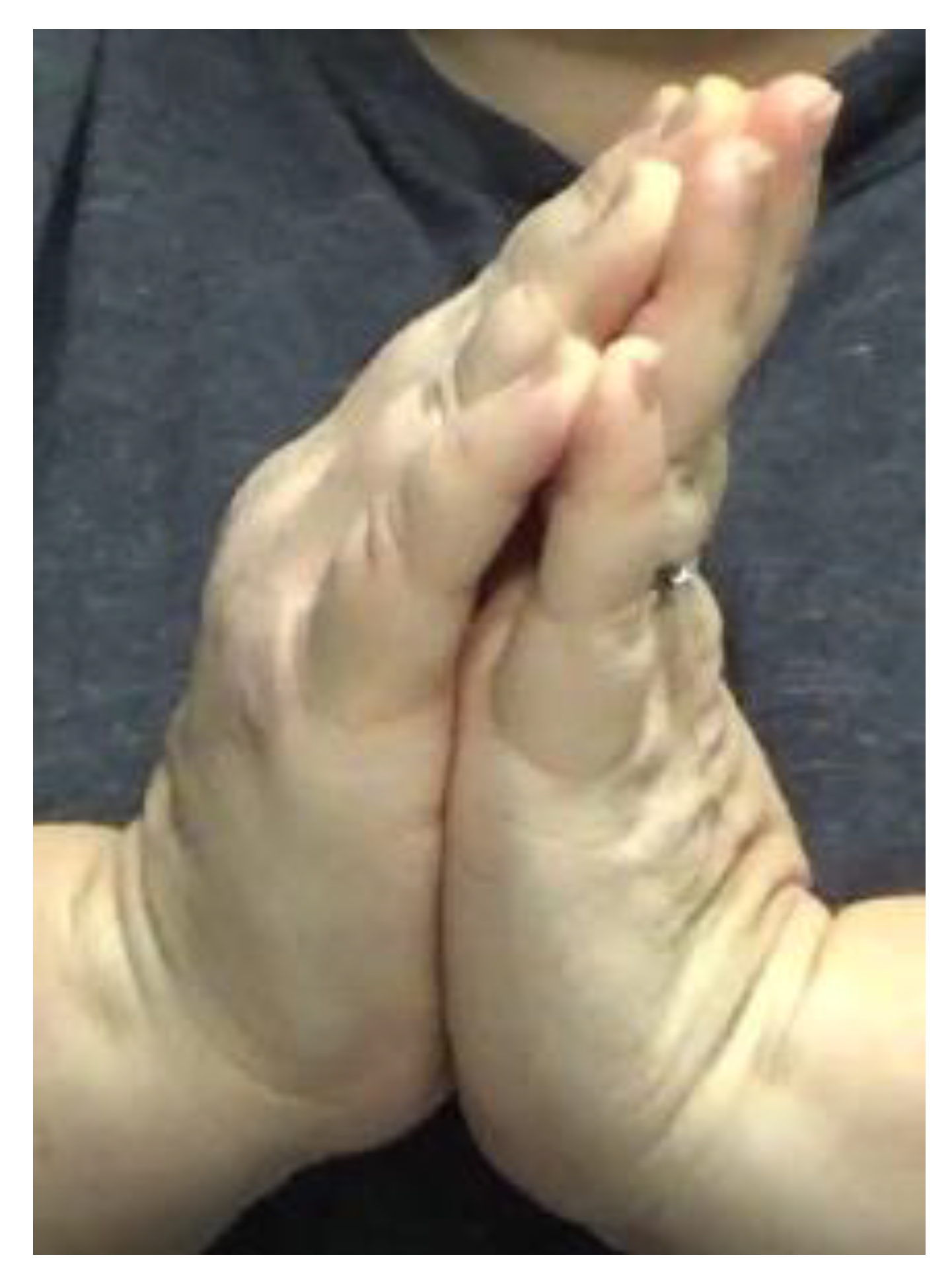
3.3.4. Joint Hypermobility Disturbances
3.3.5. Behavioral Biomarkers of FND Shared With Canonical Neurodegenerative Disorders
Clinical Blending between FND and Canonical Neurological Disease

Emotional Upset Effects on Symptoms
Exaggeration of Symptoms
Expectation Effects on Symptoms
Context-Specific Changes on Walking Ability
Competing Voluntary Activities that Can Reduce Symptoms
Cognitive Impairments
Positive Response to Psychotherapy on Motor Symptoms
Lower Extremity Dysesthesia and Compulsion To Move The Limbs
4. Rehabilitation for FND
5. Other Treatments
6. Discussion
- There is no gold standard for diagnosing FND. In our review of studies of FND biomarkers [212], we found that there are three main rival methods: the Fahn-Williams method and its variants [192], the method outlined in the various editions of the Diagnostic and Statistical Manual of Mental Disorders [213], and the referring physician’s personal judgement. Without a consensus diagnostic method for FND, rapid progress in research for treatment will likely be hindered.
- Seldom considered has been the extensive list of alternate paroxysmal neurological disorders that are not known to be affected by self-attention or emotional excitation, and which lack distinctive features on conventional clinical neuroimaging. These include frontal lobe epilepsy, paroxysmal dyskinesia, and autoimmune encephalitis [214]. This list obliges the involvement of a neurologist who is highly experienced with assessing FND (indicated above) vs. the alternate neurological disorders, thus to direct the patient to appropriate management.
- Even when a neurologist with expertise in FND may be involved, current clinical practice often limits the time to evaluate new patients to 30 minutes, due to economic pressures and meeting the demands of a large practice [214]. In contrast, as much as an hour is necessary to conduct a thorough historical intake and comprehensive neurological evaluation, and provide empathetic patient and family education and care planning. Furthermore, the patient’s concurrent cognitive limitations (described in section 3.3.5.7) can limit or slow these steps. As a result, the modern medical practice milieu may prolong evaluating and ultimately arranging care for persons who may have FND or other paroxysmal disorders.
- Even with involving a neurologist who is expert with FND, optimal care, including treatment by a neuropsychologist and rehabilitative physical therapists, occupational therapists, or speech-language pathologists, can be limited because of the relatively few medical centers that can provide these services with commensurate expertise with FND. Consequently, there can be a considerable waitlist for patients to be seen, along with the hardship for arranging travel to such places.
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Hassan, J.; Taib, S.; Yrondi, A. Structural and functional changes associated with functional/dissociative seizures: a review of the literature. Epilepsy Behav 2024, 152, 109654. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.J.; Stone, J.; Lang, A.E. From psychogenic movement disorder to functional movement disorder: it's time to change the name [review]. Mov Disord 2014, 29, 849–852. [Google Scholar] [CrossRef] [PubMed]
- Gilmour, G.S.; Jenkins, J.D. Inpatient treatment of functional neurological disorder: a scoping review. Can J Neurol Sci 2021, 48, 204–217. [Google Scholar] [CrossRef] [PubMed]
- Lidstone, S.C.; Costa-Parke, M.; Robinson, E.J.; Ercoli, T.; Stone, J. Functional movement disorder gender, age and phenotype study: a systematic review and individual patient meta-analysis of 4905 cases. J Neurol Neurosurg Psychiatry 2022, 93, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Snijders, A.H.; van de Warrenburg, B.P.; Giladi, N.; Bloem, B.R. Neurological gait disorders in elderly people: clinical approach and classification [review]. Lancet Neurol 2006, 6, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Cuénod, P.; Smaga, D.; Degive, C.; Della Santa, D.R. La main spastique psychogène. Ann Chir Main Memb Super 1996, 15, 100–108, [in French]. [Google Scholar] [CrossRef]
- LaFrance, W.C.; Baker, G.A.; Duncan, R.; Goldstein, L.H.; Reuber, M. Minimum requirements for the diagnosis of psychogenic nonepileptic seizures: a staged approach: a report from the International League Against Epilepsy Nonepileptic Seizures Task Force. Epilepsia 2013, 54, 2005–2018. [Google Scholar] [CrossRef] [PubMed]
- Geroin, C.; Petracca, M.; Di Tella, S.; Marcuzzo, E.; Erro, R.; Cuoco, S.; Ceravolo, R.; Mazzucchi, S.; Pilotto, A.; Padovani, A.; et al. Elderly onset of functional motor disorders: clinical correlates from the Italian registry. Mov Disord Clin Pract 2024, 11, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Perjoc, R.S.; Roza, E.; Vladacenco, O.A.; Teleanu, D.M.; Neacsu, R.; Teleanu, R.I. Functional neurological disorder—old problem new perspective [review]. Int J Environ Res Public Health 2023, 20, 1099. [Google Scholar] [CrossRef] [PubMed]
- Mark, V.W. Functional neurological disorder: extending the diagnosis to other disorders, and proposing an alternate disease term—Attentionally-modifiable disorder. NeuroRehabilitation 2022, 50, 179–207. [Google Scholar] [CrossRef] [PubMed]
- Araújo, R.; van de Warrenburg, B.; Lang, A.; Lees, A.; Bloem, B.R. The Waiting Room: neurological observations made outside the movement disorder specialist's consulting office. Pract Neurol 2019, 19, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, A.P.; Teasell, R.W. Behavioural interventions in the rehabilitation of acute v. chronic non-organic (conversion/factitious) motor disorders. Br J Psychiatry 2004, 185, 140–146. [Google Scholar] [CrossRef]
- Gooch, J.L.; Wolcott, R.; Speed, J. Behavioral management of conversion disorder in children. Arch Phys Med Rehabil 1997, 78, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Ramsay, N.; Stone, J.; Fadiloglu, K.; Baxter, M.; Hutchison, C.; Bennett, K.; Moullaali, T.; Mathur, J.; Bridson, J.; Hoeritzauer, I. Functional neurological disorder: a common reason for a neurology inpatient referral. Eur J Neurol 2023, 30, 3886–3889. [Google Scholar] [CrossRef] [PubMed]
- Kathol, R.G.; Cox, T.A.; Corbett, J.J.; Thompson, H.S. Functional visual loss. Follow-up of 42 cases. Arch Ophthalmol 1983, 101, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Tinazzi, M.; Geroin, C.; Marcuzzo, E.; Cuoco, S.; Ceravolo, R.; Mazzucchi, S.; Pilotto, A.; Padovani, A.; Romito, L.M.; Eleopra, R.; et al. Functional motor phenotypes: to lump or to split? J Neurol 2021, 268, 4737–4743. [Google Scholar] [CrossRef] [PubMed]
- van der Hoeven, R.M.; Broersma, M.; Pijnenborg, G.H.; Koops, E.A.; van Laar, T.; Stone, J.; van Beilen, M. Functional (psychogenic) movement disorders associated with normal scores in psychological questionnaires: a case control study. J Psychosom Res 2015, 79, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Asadi-Pooya, A.A.; Farazdaghi, M.; Asadi-Pooya, H.; Fazelian, K. Depression, anxiety, stress, and suicide risk in patients with functional seizures vs. those with epilepsy. Acta Neurol Belg in press.
- Simhan, S.; Thijs, V.; Mancuso, S.; Tsivgoulis, G.; Katsanos, A.; Alexandrov, A.V.; Kanaan, R.A. The outcome of acute functional neurological disorder: a meta-analysis of stroke-mimic presentations [review]. J Neurol 2020, 267, 1353–1357. [Google Scholar] [CrossRef] [PubMed]
- Ryznar, E.; Wilcox, D. Functional coma: two case reports and a review of the literature. Psychosomatics 2019, 60, 343–351. [Google Scholar] [CrossRef]
- Trimble, M.; Reynolds, E.H. A brief history of hysteria: from the ancient to the modern. Handb Clin Neurol 2016, 139, 3–10. [Google Scholar] [PubMed]
- Stone, J.; Reuber, M.; Carson, A. Functional symptoms in neurology: mimics and chameleons [review]. Pract Neurol 2013, 13, 104–113. [Google Scholar] [CrossRef]
- Keane, J.R. Hysterical gait disorders. 60 cases. Neurology 1989, 39, 586–589. [Google Scholar] [CrossRef] [PubMed]
- Heruti, R.J.; Reznik, J.; Adunski, A.; Levy, A.; Weingarden, H.; Ohry, A. Conversion motor paralysis disorder: analysis of 34 consecutive referrals. Spinal Cord 2002, 40, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Gutkin, M.; McLean, L.; Brown, R.; Kanaan, R. Systematic review of psychotherapy for adults with functional neurological disorder. J Neurol Neurosurg Psychiatry 2021, 92, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Freud, S. Über den psychischen Mechanismus hysterische Phänomene: vorläufige Mittelung. In Studien über Hysterie und anderen Werke aus den Jahren 1892-1899; S. Fischer Verlage: Frankfurt, 1899; pp. 81–98, [in German]. [Google Scholar]
- Kanaan, R.A.; Armstrong, D.; Wessely, S.C. Neurologists' understanding and management of conversion disorder. J Neurol Neurosurg Psychiatry 2011, 82, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Carson, A.; Ludwig, L.; Welch, K. Psychologic theories in functional neurologic disorders [review]. Handb Clin Neurol 2016, 139, 105–120. [Google Scholar] [PubMed]
- Milano, B.A.; Moutoussis, M.; Convertino, L. The neurobiology of functional neurological disorders characterised by impaired awareness [review]. Front Psychiatry 2023, 14, 1122865. [Google Scholar] [CrossRef] [PubMed]
- McLoughlin, C.; McGhie-Fraser, B.; Carson, A.; Olde Hartman, T.; Stone, J. How stigma unfolds for patients with Functional Neurological Disorder. J Psychosom Res 2024, 181, 111667. [Google Scholar] [CrossRef]
- Joos, A.; Herrmann, C.; Lahmann, C.; Flottman, M.; Jansen, T.; Schede, C.; Maner, P.; Schorner, K.; von Husen, D.K.; Jobges, M.; et al. Biopsychosocial complexity in functional neurological disorder. Gen Hosp Psychiatry 2023, 84, 44–46. [Google Scholar] [CrossRef] [PubMed]
- MacDuffie, K.E.; Grubbs, L.; Best, T.; LaRoche, S.; Mildon, B.; Myers, L.; Stafford, E.; Rommelfanger, K.S. Stigma and functional neurological disorder: a research agenda targeting the clinical encounter. CNS Spectr 2021, 26, 587–592. [Google Scholar] [CrossRef] [PubMed]
- Raynor, G.; Baslet, G. A historical review of functional neurological disorder and comparison to contemporary models. Epilepsy Behav Rep 2021, 16, 100489. [Google Scholar] [CrossRef] [PubMed]
- Varma, A.R.; Moriarty, J.; Costa, D.C.; Gaćinovic, S.; Schmitz, E.B.; Ell, P.J.; Trimble, M.R. HMPAO SPECT in non-epileptic seizures: preliminary results. Acta Neurol Scand 1996, 94, 88–92. [Google Scholar] [CrossRef] [PubMed]
- Vuilleumier, P.; Chicherio, C.; Assal, F.; Schwartz, S.; Slosman, D.; Landis, T. Functional neuroanatomical correlates of hysterical sensorimotor loss. Brain 2001, 124, 1077–1090. [Google Scholar] [CrossRef] [PubMed]
- Atmaca, M.; Aydin, A.; Tezcan, E.; Poyraz, A.K.; Kara, B. Volumetric investigation of brain regions in patients with conversion disorder. Prog Neuropsychopharmacol Biol Psychiatry 2006, 30, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Atmaca, M.; Baykara, S.; Mermi, O.; Yildirim, H.; Akaslan, U. Pituitary volumes are changed in patients with conversion disorder. Brain Imaging Behav 2015, 10, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Labate, A.; Cerasa, A.; Mula, M.; Mumoli, L.; Gioia, M.C.; Aguglia, U.; Quattrone, A.; Gambardella, A. Neuroanatomic correlates of psychogenic nonepileptic seizures: a cortical thickness and VBM study. Epilepsia 2012, 53, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Weber, S.; Bühler, J.; Vanini, G.; Loukas, S.; Bruckmaier, R.; Aybek, S. Identification of biopsychological trait markers in functional neurological disorders. Brain 2023, 146, 2627–2641. [Google Scholar] [CrossRef]
- Perez, D.L.; Matin, N.; Williams, B.; Tanev, K.; Makris, N.; LaFrance, W.C.; Dickerson, B.C. Cortical thickness alterations linked to somatoform and psychological dissociation in functional neurological disorders. Hum Brain Mapp 2018, 39, 428–439. [Google Scholar] [CrossRef] [PubMed]
- Perez, D.L.; Matin, N.; Barsky, A.; Costumero-Ramos, V.; Makaretz, S.J.; Young, S.S.; Sepulcre, J.; LaFrance, W.C.; Keshavan, M.S.; Dickerson, B.C. Cingulo-insular structural alterations associated with psychogenic symptoms, childhood abuse and PTSD in functional neurological disorders J Neurol Neurosurg Psychiatry 2017, 88, 491-497.
- Nicholson, T.R.; Aybeck, S.; Kempton, M.J.; Daly, E.M.; Murphy, D.G.; David, A.S.; Kanaan, R. A structural MRI study of motor conversion disorder: evidence of reduction in thalamic volume. J Neurol Neurosurg Psychiatry 2014, 85, 227–229. [Google Scholar] [CrossRef]
- Tomic, A.; Agosta, F.; Sarasso, E.; Petrovic, I.; Basaia, S.; Pesic, D.; Kostic, M.; Fontana, A.; Kostic, V.S.; Filippi, M. Are there two different forms of functional dystonia? A multimodal brain structural MRI study. Mol Psychiatry 2020, 25, 3350–3359. [Google Scholar] [CrossRef] [PubMed]
- Espay, A.J.; Maloney, T.; Vannest, J.; Norris, M.M.; Eliassen, J.C.; Neefus, E.; Allendorfer, J.B.; Lang, A.E.; Szaflarski, J.P. Impaired emotion processing in functional (psychogenic) tremor: a functional magnetic resonance imaging study. Neuroimage: Clinical 2018, 17, 179–187. [Google Scholar] [CrossRef]
- Tatekawa, H.; Kerr, W.T.; Savic, I.; Engel, J.; Salamon, N. Reduced left amygdala volume in patients with dissociative seizures (psychogenic nonepileptic seizures). Seizure 2020, 75, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Liu, X.; Zhao, X. Neuroimaging studies in peristent postural-perceptual dizziness and related disease: a systematic review. J Neurol 2022, 269, 1225–1235. [Google Scholar] [CrossRef] [PubMed]
- Kerr, W.T.; Tatekawa, H.; Lee, J.K.; Karimi, A.H.; Sreenivasan, S.S.; O'Neill, J.; Smith, J.M.; Hickman, L.B.; Savic, I.; Nasrullah, N.; et al. Clinical MRI morphological analysis of functional seizures compared to seizure-naive and psychiatric controls. Epilepsy Behav 2022, 134, 108858. [Google Scholar] [CrossRef]
- Maurer, C.W.; LaFaver, K.; Limachia, G.S.; Capitan, G.; Ameli, R.; Sinclair, S.; Epstein, S.A.; Hallett, M.; Horovitz, S.G. Gray matter differences in patients with functional movement disorders. Neurology 2018, 91, e1870–e1879. [Google Scholar] [CrossRef] [PubMed]
- Mcsweeney, M.; Reuber, M.; Hoggard, N.; Levita, L. Cortical thickness and gyrification patterns in patients with psychogenic non-epileptic seizures. Neurosci Lett 2018, 678, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Labate, A.; Martino, I.; Caligiuri, M.E.; Fortunato, F.; Bruni, A.; Segura-Garcia, C.; Arcuri, P.; De Fazio, P.; Cerasa, A.; Gambardella, A. Orbito-frontal thinning together with a somatoform dissociation might be the fingerprint of PNES. Epilepsy Behav 2021, 121, 108044. [Google Scholar] [CrossRef] [PubMed]
- Aybek, S.; Nicholson, T.R.; Draganski, B.; Daly, E.; Murphy, D.G.; David, A.S.; Kanaan, R.A. Grey matter changes in motor conversion disorder. J Neurol Neurosurg Psychiatry 2014, 85, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Ristić, A.J.; Daković, M.; Kerr, M.; Kovačević, M.; Parojčić, A.; Sokić, D. Cortical thickness, surface area and folding in patients with psychogenic nonepileptic seizures. Epilepsy Res 2015, 112, 84–91. [Google Scholar] [CrossRef] [PubMed]
- Kozlowska, K.; Griffiths, K.R.; Foster, S.L.; Linton, J.; Williams, L.M.; Korgaonkar, M.S. Grey matter abnormalities in children and adolescents with functional neurological symptom disorder. Neuroimage Clin 2017, 15, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Perez, D.L.; Williams, B.; Matin, N.; LaFrance, W.C.; Costumero-Ramos, V.; Fricchione, G.L.; Sepulcre, J.; Keshavan, M.S.; Dickerson, B.C. Corticolimbic structural alterations linked to health status and trait anxiety in functional neurological disorder. J Neurol Neurosurg Psychiatry 2017, 88, 1052–1059. [Google Scholar] [CrossRef]
- Sojka, P.; Slovák, M.; Vechetová, G.; Jech, R.; Perez, D.L.; Serranová, T. Bridging structural and functional biomarkers in functional movement disorder using network mapping. Brain Behav 2022, 12, e2576. [Google Scholar] [CrossRef] [PubMed]
- Zelinski, L.; Diez, I.; Perez, D.L.; Kotz, S.A.; Wellmer, J.; Schlegel, U.; Popkirov, S.; Jungilligens, J. Cortical thickness in default mode network hubs correlates with clinical features of dissociative seizures. Epilepsy Behav 2022, 128, 108605. [Google Scholar] [CrossRef] [PubMed]
- Maiti, B.; Perlmutter, J. Imaging in movement disorders [review]. Continuum 2023, 29, 194–218. [Google Scholar] [PubMed]
- Xu, X.; Han, Q.; Lin, J.; Wang, L.; Wu, F.; Shang, H. Grey matter abnormalities in Parkinson's disease: a voxel-wise meta-analysis. Eur J Neurol 2020, 27, 653–659. [Google Scholar] [CrossRef] [PubMed]
- Gorno-Tempini, M.L.; Murray, R.C.; Rankin, K.P.; Weiner, M.W.; Miller, B.L. Clinical, cognitive and anatomical evolution from nonfluent progressive aphasia to corticobasal syndrome: a case report. Neurocase 2004, 10, 426–436. [Google Scholar] [CrossRef] [PubMed]
- Scheltens, P.; Blennow, K.; Breteler, M.M.; de Strooper, B.; Frisoni, G.B.; Salloway, S.; Van der Flier, W.M. Alzheimer's disease [review]. Lancet 2016, 388, 505–517. [Google Scholar] [CrossRef]
- MacIver, C.L.; Tax, C.M.W.; Jones, D.K.; Peall, K.J. Structural magnetic resonance imaging in dystonia: a systematic review of methodological approaches and findings. Eur J Neurol 2022, 29, 3418–3448. [Google Scholar] [CrossRef] [PubMed]
- Phan, T.X.; Baratono, S.; Drew, W.; Tetreault, A.M.; Fox, M.D.; Darby, R.R. Increased cortical thickness in Alzheimer's disease. Ann Neurol 2024, 95, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Nalls, M.A.; Blauwendraat, C.; Vallerga, C.L.; Heilbron, K.; Bandres-Ciga, S.; Chang, D.; Tan, M.; Kia, D.A.; Noyce, A.J.; Xue, A.; et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson's disease: a meta-analysis of genome-wide association studies. Lancet Neurol 2019, 18, 1091–1102. [Google Scholar] [CrossRef] [PubMed]
- Patsopoulos, N.A. Genetics of multiple sclerosis: an overview and new directions [review]. Cold Spring Harb Perspect Med 2018, 8, a028951. [Google Scholar] [CrossRef] [PubMed]
- Reich, D.S.; Lucchinetti, C.F.; Calabresi, P.A. Multiple sclerosis [review]. N Engl J Med 2018, 378, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Munts, A.G.; Koehler, P.J. How psychogenic is dystonia? Views from past to present [review]. Brain 2010, 133, 1552–1564. [Google Scholar] [CrossRef] [PubMed]
- Frucht, L.; Perez, D.L.; Callahan, J.; MacLean, J.; Song, P.C.; Sharma, N.; Stephen, C.D. Functional dystonia: differentiation from primary dystonia and multidisciplinary treatments [review]. Front Neurol 2021, 11, 605262. [Google Scholar] [CrossRef] [PubMed]
- Spagnolo, P.A.; Norato, G.; Maurer, C.W.; Goldman, D.; Hodgkinson, C.; Horovitz, S.; Hallett, M. Effects of TPH2 gene variation and childhood trauma on the clinical and circuit-level phenotype of functional movement disorders. J Neurol Neurosurg Psychiatry 2020, 91, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Asadi-Pooya, A.A.; Simani, L.; Asadollahi, M.; Rashidi, F.S.; Ahmadipour, E.; Alavi, A.; Roozbeh, M.; Akbari, N.; Firouzabadi, N. Potential role of FKBP5 single-nucleotide polymorphisms in functional seizures. Epilepsia Open 2023, 8, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Faissner, S.; Plemel, J.R.; Gold, R.; Yong, V.W. Progressive multiple sclerosis: from pathophysiology to therapeutic strategies [review]. Nat Rev Drug Discov 2019, 18, 905–922. [Google Scholar] [CrossRef] [PubMed]
- Frank-Cannon, T.C.; Alto, L.T.; McAlpine, F.E.; Tansey, M.G. Does neuroinflammation fan the flame in neurodegenerative diseases? [Review.]. Mol Neurodegener 2009, 4, 47. [Google Scholar] [CrossRef] [PubMed]
- Yacoubian, T.A.; Fang, Y.D.; Gerstenecker, A.; Amara, A.; Stover, N.; Ruffrage, L.; Collette, C.; Kennedy, R.; Zhang, Y.; Hong, H.; et al. Brain and systemic Inflammation in de novo Parkinson's disease. Mov Disord 2023, 38, 743–754. [Google Scholar] [CrossRef] [PubMed]
- van der Feltz-Cornelis, C.; Brabyn, S.; Ratcliff, J.; Varley, D.; Aligar, V.; Gilbody, S.; Clarke, C.; Lagos, D. Assessment of cytokines, microRNA and patient related outcome measures in conversion disorder/functional neurological disorder (CD/FND): the CANDO clinical feasibility study. Brain Behav Immun-Health 2021, 13, 100228. [Google Scholar] [CrossRef]
- Kozlowska, K.; Chung, J.; Cruickshank, B.; McLean, L.; Scher, S.; Dale, R.C.; Mohammad, S.S.; Singh-Grewal, D.; Prabhuswamy, M.Y.; Patrick, E. Blood CRP levels are elevated in children and adolescents with functional neurological symptom disorder. Eur Child Adolesc Psychiatry 2019, 28, 491–504. [Google Scholar] [CrossRef] [PubMed]
- Hartig, M.; Prokisch, H.; Meitinger, T.; Klopstock, T. Mitochondrial membrane protein-associated neurodegeneration (MPAN) [review]. Int Rev Neurobiol 2013, 110, 73–84. [Google Scholar] [PubMed]
- Skowronska, M.; Buksinska-Lisik, M.; Kmiec, T.; Litwin, T.; Kurkowska-Jastrzębska, I.; Czlonkowska, A. Is there heart disease in cases of neurodegeneration associated with mutations in C19orf12? Parkinsonism Relat Disord 2020, 80, 15–18. [Google Scholar] [CrossRef] [PubMed]
- Parikh, S.M.; Diedrich, A.; Biaggioni, I.; Robertson, D. The nature of the autonomic dysfunction in multiple system atrophy [review]. J Neurol Sci 2002, 200, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Aboudrar, S.; Benjelloun, H.; Benazzouz, A.; Bendahmanne, S.; Coghlan, L.; Kanouni, N.; Abouqal, R.; Benomar, M. Évaluation de l’activité vagale par le test de la respiration profonde (Deep-Breathing). Neurophysiol Clin 2007, 37, 41–46, [in French]. [Google Scholar] [CrossRef] [PubMed]
- Paredes-Echeverri, S.; Maggio, J.; Begue, I.; Pick, S.; Nicholson, T.R.; Perez, D.L. Autonomic, endocrine, and inflammation profiles in functional neurological disorder: a systematic review and meta-analysis. J Neuropsychiatry Clin Neurosci 2022, 34, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Chudleigh, C.; Savage, B.; Cruz, C.; Lim, M.; McClure, G.; Palmer, D.M.; Spooner, C.J.; Kozlowska, K. Use of respiratory rates and heart rate variability in the assessment and treatment of children and adolescents with functional somatic symptoms. Clin Child Psychol Psychiatry 2019, 24, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Santens, P.; Crevits, L.; van Der Linden, C. Raynaud's phenomenon in a case of multiple system atrophy. Mov Disord 1996, 11, 586–588. [Google Scholar] [CrossRef] [PubMed]
- Pietzarka, K.; Reimann, M.; Schmidt, C.; Herting, B.; Schöls, L.; Reichmann, H.; Berg, D.; Schrader, C.; Ziemssen, T. The cold hand sign in multiple system atrophy: skin perfusion revisited. J Neural Transm 2010, 117, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Klein, C.; Brown, R.; Wenning, G.; Quinn, N. The "cold hands sign" in multiple system atrophy. Mov Disord 1997, 12, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Asahina, M.; Kikkawa, Y.; Suzuki, A.; Hattori, T. Cutaneous sympathetic function in patients with multiple system atrophy. Clin Auton Res 2003, 13, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Köllensperger, M.; Geser, F.; Seppi, K.; Stampfer-Kountchev, M.; Sawires, M.; Scherfler, C.; Boesch, S.; Mueller, J.; Koukouni, V.; Quinn, N.; et al. Red flags for multiple system atrophy. Mov Disord 2008, 23, 1093–1099. [Google Scholar] [CrossRef] [PubMed]
- Horimoto, Y.; Aiba, I.; Yasuda, T.; Ohkawa, Y.; Katayama, T.; Yokokawa, Y.; Goto, A.; Ito, Y. Longitudinal MRI study of multiple system atrophy - when do the findings appear, and what is the course? J Neurol 2002, 249, 847–854. [Google Scholar] [CrossRef]
- Carmona-Abellan, M.; Del Pino, R.; Murueta-Goyena, A.; Acera, M.; Tijero, B.; Berganzo, K.; Gabilondo, I.; Gomez-Esteban, J.C. Multiple system atrophy: clinical, evolutive and histopathological characteristics of a series of cases. Neurología 2023, 38, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Onofrj, M.; Bonanni, L.; Manzoli, L.; Thomas, A. Cohort study on somatoform disorders in Parkinson disease and dementia with Lewy bodies. Neurology 2010, 74, 1598–1606. [Google Scholar] [CrossRef]
- Mark, V.W. Purple feet. 2022 Available online at 2022FNDSAbstracts.pdf (fndsociety.org).
- Reich, S.G. The cold hands sign in MSA. Neurology 2003, 60, 719. [Google Scholar] [CrossRef] [PubMed]
- Kinnier Wilson, S.A. The approach to the study of hysteria [review]. J Neurol Psychopathol 1931, 11, 193–206. [Google Scholar] [CrossRef]
- Lacy, B.E.; Mearin, F.; Chang, L.; Chey, W.D.; Lembo, A.J.; Simren, M.; Spiller, R. Bowel disorders [review]. Gastroenterology 2016, 150, 1393–1407. [Google Scholar] [CrossRef]
- Hallett, M.; Aybek, S.; Dworetzky, B.A.; McWhirter, L.; Staab, J.P.; Stone, J. Functional neurological disorder: new subtypes and shared mechanisms [review]. Lancet Neurol 2022, 21, 537–550. [Google Scholar] [CrossRef] [PubMed]
- Charney, M.; Foster, S.; Shukla, V.; Zhao, W.; Jiang, S.H.; Kozlowska, K.; Lin, A. Neurometabolic alterations in children and adolescents with functional neurological disorder. Neuroimage Clin 2023, 41, 103557. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Baudoin, R.; Hans, S.; Akst, L.M. History of otolaryngology: globus pharyngeus as "globus hystericus". Otolaryngol Head Neck Surg 2023, 168, 889–892. [Google Scholar] [CrossRef] [PubMed]
- Talman, L.; Safarpour, D. An overview of gastrointestinal dysfunction in Parkinsonian syndromes [review]. Semin Neurol 2023, 43, 583–597. [Google Scholar] [PubMed]
- Annaházi, A.; Schemann, M. Contribution of the enteric nervous system to autoimmune diseases and irritable bowel syndrome [review]. Adv Exp Med Biol 2022, 1383, 1–8. [Google Scholar] [PubMed]
- Nisticò, V.; Iacono, A.; Goeta, D.; Tedesco, R.; Giordano, B.; Faggioli, R.; Priori, A.; Gambini, O.; Demartini, B. Hypermobile spectrum disorders symptoms in patients with functional neurological disorders and autism spectrum disorders: a preliminary study. Front Psychiatry 2022, 13, 943098. [Google Scholar] [CrossRef] [PubMed]
- Ross, J.; Grahame, R. Joint hypermobility syndrome [review]. BMJ 2011, 342, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Ellington, M.; Francomano, C.A. Chiari I malformations and the deritable disorders of connective tissue [review]. Neurosurg Clin N Am 2023, 34, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.A.; Greenberg, J.K.; Steinmetz, M.P.; Vorster, S.; Nevzati, E.; Spiessberger, A. C1-2 hypermobility and its impact on the spinal cord: a finite element analysis. J Neurosurg Spine in press.
- Al-Harbi, T.M.; Al-Rammah, H.; Al-Zahrani, N.; Liu, Y.; Sleiman, P.M.A.; Dridi, W.; Hakonarson, H. Rare neurological manifestations in a Saudi Arabian patient with Ehlers-Danlos syndrome and a novel homozygous variant in the TNXB gene. Am J Med Genet A 2022, 188, 618–623. [Google Scholar] [CrossRef] [PubMed]
- Jahromi, L.S.M.; Sayyadi, A.; Askarian, A.; Dabbaghmanesh, A.; Roshanzamir, S. Visual evoked potential in generalized joint hypermobility: a case-control study. Brain Behav 2024, 14, e3493. [Google Scholar] [CrossRef]
- Wissel, B.D.; Dwivedi, A.K.; Merola, A.; Chin, D.; Jacob, C.; Duker, A.P.; Vaughan, J.E.; Lovera, L.; LaFaver, K.; Levy, A.; et al. Functional neurological disorders in Parkinson disease. J Neurol Neurosurg Psychiatry 2018, 89, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Onofrj, M.; Russo, M.; Carrarini, C.; Delli Pizzi, S.; Thomas, A.; Bonanni, L.; Espay, A.J.; Sensi, S.L. Functional neurological disorder and somatic symptom disorder in Parkinson's disease. J Neurol Sci 2022, 433, 120017. [Google Scholar] [CrossRef]
- Pareés, I.; Saifee, T.A.; Kojovic, M.; Kassavetis, P.; Rubio-Agusti, I.; Sadnicka, A.; Bhatia, K.P.; Edwards, M.J. Functional (psychogenic) symptoms in Parkinson's disease. Mov Disord 2013, 28, 1622–1627. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Mayordomo, V.; Kojović, M.; López-Valdés, E.; ALonso-Frech, F.; Horga, A.; Fernández-Rodríguez, R.; Pareés, I. Functional neurological symptoms as initial presentation of Creutzfeldt-Jakob disease: case series [letter]. J Neurol 2023, 270, 1141–1146. [Google Scholar] [CrossRef]
- Carson, A.J.; McWhirter, L. Cognitive behavioral therapy: principles, science, and patient selection in neurology [review]. Semin Neurol 2022, 42, 114–122. [Google Scholar] [CrossRef]
- Lieberman, A. Are freezing of gait (FOG) and panic related? J Neurol Sci 2006, 248, 219–222. [Google Scholar] [CrossRef]
- Weiss, H.D.; Pontone, G.M. "Pseudo-syndromes" associated with Parkinson disease, dementia, apathy, anxiety, and depression [review]. Neurol Clin Pract 2019, 9, 354–359. [Google Scholar] [CrossRef]
- Marrie, R.A.; Patel, R.; Bernstein, C.N.; Bolton, J.M.; Graff, L.A.; Marriott, J.J.; Hitchon, C.A.; Figley, C.R.; Kornelsen, J.; Fisk, J.D. Anxiety and depression affect performance on the symbol digit modalities test over time in MS and other immune disorders. Mult Scler J 2021, 27, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Soto, E.; Cruz-Gómez, Á.J.; Gutiérrez, R.; González, M.; Sanmartino, F.; Rashid-Lopez, R.; Espinosa-Rosso, R.; Forero, L.; González-Rosa, J.J. Predicting neuropsychological impairment in relapsing remitting multiple sclerosis: the role of clinical measures, treatment, and neuropsychiatry symptoms. Arch Clin Neuropsychol 2021, 36, 475–484. [Google Scholar] [CrossRef]
- Leavitt, V.M.; Brandstadter, R.; Fabian, M.; Sand, I.K.; Klineova, S.; Krieger, S.; Lewis, C.; Lublin, F.; Miller, A.; Pelle, G.; et al. Dissociable cognitive patterns related to depression and anxiety in multiple sclerosis. Mult Scler J 2020, 26, 1247–1255. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.P.; Feinstein, A. The link between depression and performance on the Symbol Digit Modalities Test: mechanisms and clinical significance. Mult Scler J 2019, 25, 118–121. [Google Scholar] [CrossRef]
- Landrø, N.I.; Celius, E.G.; Sletvold, H. Depressive symptoms account for deficient information processing speed but not for impaired working memory in early phase multiple sclerosis (MS). J Neurol Sci 2004, 217, 211–216. [Google Scholar] [CrossRef]
- Perrochon, A.; Holtzer, R.; Laidet, M.; Armand, S.; Assal, F.; Lalive, P.H.; Allali, G. Postural control is associated with cognition and fear of falling in patients with multiple sclerosis. J Neural Transm 2017, 124, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Laidet, M.; Herrmann, F.R.; Armand, S.; Assal, F.; Lalive, P.H.; Allali, G. Does fear of falling predict gait variability in multiple sclerosis? J Neurol Sci 2017, 380, 212–214. [Google Scholar] [CrossRef]
- Xing, Z.; Hu, Y.; Teng, F.; Song, Y.; Wu, Z.; Hong, R.; Zhang, Z.; Gu, H.; Peng, K.; He, Y.; et al. A prediction rule for the dystonic spread of blepharospasm: a 4-year prospective cohort study. Ann Neurol in press.
- Pareés, I.; Saifee, T.A.; Kassavetis, P.; Kojovic, M.; Rubio-Agusti, I.; Rothwell, J.C.; Bhatia, K.P.; Edwards, M.J. Believing is perceiving: mismatch between self-report and actigraphy in psychogenic tremor. Brain 2012, 135, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Kramer, G.; Dominguez-Vega, Z.T.; Laarhoven, H.S.; Brandsma, R.; Smit, M.; van der Stouwe, A.M.; Elting, J.W.J.; Maurits, N.M.; Rosmalen, J.G.; Tijssen, M.A. Similar association between objective and subjective symptoms in functional and organic tremor. Parkinsonism Relat Disord 2019, 64, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Rommelfanger, K.S. The role of placebo in the diagnosis and treatment of functional neurologic disorders [review]. Handb Clin Neurol 2016, 139, 607–617. [Google Scholar]
- Bogousslavsky, J. Jean-Martin Charcot and his legacy [review]. Front Neurol Neurosci 2014, 35, 44–55. [Google Scholar] [PubMed]
- Witek, N.; Stebbins, G.T.; Goetz, C.G. What influences placebo and nocebo responses in Parkinson's disease? [Review.]. Mov Disord 2018, 33, 1204–1212. [Google Scholar] [CrossRef] [PubMed]
- Ellis, T.; Boudreau, J.K.; DeAngelis, T.R.; Brown, L.E.; Cavanaugh, J.T.; Earhart, G.M.; Ford, M.P.; Foreman, K.B.; Dibble, L.E. Barriers to exercise in people with Parkinson disease. Phys Ther 2013, 93, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, J.J.; Trenkwalder, C.; Mestre, T.A. Placebo and nocebo responses in other movement disorders besides Parkinson's disease: how much do we know? [Review.]. Mov Disord 2018, 33, 1228–1235. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.X.; Zhang, N.N.; Zhao, H.X.; Song, J. Nocebo effect in multiple system atrophy: systematic review and meta-analysis of placebo-controlled clinical trials [review]. Neurol Sci 2022, 43, 899–905. [Google Scholar] [CrossRef] [PubMed]
- Shafiq, F.; Mitsikostas, D.D.; Zis, P. Nocebo in motor neuron disease: systematic review and meta-analysis of placebo-controlled clinical trials [review]. Amyotroph Lateral Scler Frontotemporal Degener 2017, 18, 576–582. [Google Scholar] [CrossRef] [PubMed]
- McKee, K.; Glass, S.; Adams, C.; Stephen, C.D.; King, F.; Parlman, K.; Perez, D.L.; Kontos, N. The inpatient assessment and management of motor functional neurological disorders: an interdisciplinary perspective. Psychosomatics 2018, 59, 358–369. [Google Scholar] [CrossRef] [PubMed]
- Paramanandam, V.; Lizarraga, K.J.; Soh, D.; Algarni, M.; Rohani, M.; Fasano, A. Unusual gait disorders: a phenomenological approach and classification. Expert Rev Neurother 2019, 19, 119–132. [Google Scholar] [CrossRef] [PubMed]
- An, E.J.; Sim, W.S.; Kim, S.M.; Kim, J.Y. Suitability of visual cues for freezing of gait in patients with idiopathic Parkinson's disease: a case-control pilot study. J Neuroeng Rehabil 2023, 20, 91. [Google Scholar] [CrossRef] [PubMed]
- García Ruiz, P.J.; Rojo, A.; Sánchez Bernardos, V.; Romero, A.; Cubo, E.; Aguilar, M. Bloqueo (freezing) del gateo o bloqueo de la marcha cuadrúpeda. Neurología 2004, 19, 77–79, [in Spanish]. [Google Scholar]
- Huang, X.; Dong, K.; Gan, C.; Xu, Z.; Lei, D.; Dong, X.; Liu, H.; Chen, X. Effect of rhythmically cued exercise interventions on functions in patients with Parkinson disease: a meta-analysis [review]. Phys Ther in press.
- Hebb, C.; Raynor, G.; Perez, D.L.; Nappi-Kaehler, J.; Polich, G. The use of rhythmic auditory stimulation for functional gait disorder: a case report. Neurorehabilitation 2022, 50, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Snijders, A.H.; Bloem, B.R. Cycling for freezing of gait. N Engl J Med 2010, 362, e46. [Google Scholar] [CrossRef] [PubMed]
- Albanese, A.; Di Giovanni, M.; Lalli, S. Dystonia: diagnosis and management [review]. Eur J Neurol 2019, 26, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Ramos, V.F.M.L.; Karp, B.I.; Hallett, M. Tricks in dystonia: ordering the complexity [review]. J Neurol Neurosurg Psychiatry 2014, 85, 987–993. [Google Scholar] [CrossRef]
- Butler, M.; Shipston-Sharman, O.; Seynaeve, M.; Bao, J.; Pick, S.; Bradley-Westguard, A.; Ilola, E.; Mildon, B.; Golder, D.; Rucker, J.; et al. International online survey of 1048 individuals with functional neurological disorder. Eur J Neurol 2021, 28, 3591–3602. [Google Scholar] [CrossRef]
- Sadnicka, A.; Daum, C.; Meppelink, A.M.; Manohar, S.; Edwards, M. Reduced drift rate: a biomarker of impaired information processing in functional movement disorders. Brain 2020, 143, 674–683. [Google Scholar] [CrossRef] [PubMed]
- Věchetová, G.; Nikolai, T.; Slovák, M.; Forejtová, Z.; Vranka, M.; Straková, E.; Teodoro, T.; Růžička, E.; Edwards, M.J.; Serranová, T. Attention impairment in motor functional neurological disorders: a neuropsychological study. J Neurol in press.
- Roivainen, E.; Peura, M.; Patsi, J. Cognitive profile in functional disorders. Cogn Neuropsychiatry 2023, 28, 424–436. [Google Scholar] [CrossRef] [PubMed]
- de Vroege, L.; Koppenol, I.; Kop, W.J.; Riem, M.M.E.; der Feltz-Cornelis, C.M. Neurocognitive functioning in patients with conversion disorder/functional neurological disorder. J Neuropsychol 2021, 15, 69–87. [Google Scholar] [CrossRef] [PubMed]
- van Wouwe, N.C.; Mohanty, D.; Lingaiah, A.; Wylie, S.A.; LaFaver, K. Impaired action control in patients with functional movement disorders. J Neuropsychiatry Clin Neurosci 2020, 32, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Kozlowska, K.; Palmer, D.M.; Brown, K.J.; Scher, S.; Chudleigh, C.; Davies, F.; Williams, K.M. Conversion disorder in children and adolescents: a disorder of cognitive control. J Neuropsychol 2015, 9, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Pareés, I.; Kassavetis, P.; Saifee, T.A.; Sadnicka, A.; Bhatia, K.P.; Fotopoulou, A.; Edwards, M.J. 'Jumping to conclusions' bias in functional movement disorders. J Neurol Neurosurg Psychiatry 2012, 83, 460–463. [Google Scholar] [CrossRef] [PubMed]
- Voon, V.; Ekanayake, V.; Wiggs, E.; Kranick, S.; Ameli, R.; Harrison, N.A.; Hallett, M. Response inhibition in motor conversion disorder. Movement Disorders 2013, 28, 612–618. [Google Scholar] [CrossRef] [PubMed]
- Silveri, M.C.; Di Tella, S.; Lo Monaco, M.R.; Petracca, M.; Tondinelli, A.; Antonucci, G.; Pozzi, G.; Di Lazzaro, G.; Calabresi, P.; Bentivoglio, A.R. Theory of mind: a clue for the interpretation of functional movement disorders. Acta Neurol Scand 2022, 145, 571–578. [Google Scholar] [CrossRef] [PubMed]
- Silveri, M.C.; Lo Monaco, M.R.; Tondinelli, A.; Petracca, M.; Zinzi, P.; Fragapane, S.; Pozzi, G.; Pagnini, F.; Bentivoglio, A.R.; Di Tella, S. Social cognition in Parkinson's disease and functional movement disorders. Neurol Sci 2024, 45, 3775–3784. [Google Scholar] [CrossRef] [PubMed]
- Sauer, K.S.; Witthoft, M.; Rief, W. Somatic symptom disorder and health anxiety: assessment and management [review]. Neurol Clin 2023, 41, 745–758. [Google Scholar] [CrossRef] [PubMed]
- Espay, A.J.; Ries, S.; Maloney, T.; Vannest, J.; Neefus, E.; Dwivedi, A.K.; Allendorfer, J.B.; Wulsin, L.R.; LaFrance, W.C.; Lang, A.E.; et al. Clinical and neural responses to cognitive behavioral therapy for functional tremor. Neurology 2019, 93, e1787–e1798. [Google Scholar] [CrossRef] [PubMed]
- O'Connell, N.; Watson, G.; Grey, C.; Pastena, R.; McKeown, K.; David, A.S. Outpatient CBT for motor functional neurological disorder and other neuropsychiatric conditions: a retrospective case comparison. J Neuropsychiatry Clin Neurosci 2020, 32, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Rawson, K.S.; Cavanaugh, J.T.; Colon-Semenza, C.; DeAngelis, T.; Duncan, R.P.; Fulford, D.; LaValley, M.P.; Mazzoni, P.; Nordahl, T.; Quintiliani, L.M.; et al. Design of the WHIP-PD study: a phase II, twelve-month, dual-site, randomized controlled trial evaluating the effects of a cognitive-behavioral approach for promoting enhanced walking activity using mobile health technology in people with Parkinson-disease. BMC Neurology 2020, 20, 146. [Google Scholar] [CrossRef] [PubMed]
- Broström, A.; Alimoradi, Z.; Lind, J.; Ulander, M.; Lundin, F.; Pakpour, A. Worldwide estimation of restless legs syndrome: a systematic review and meta-analysis of prevalence in the general adult population. J Sleep Res 2023, 32, e13783. [Google Scholar] [CrossRef] [PubMed]
- Mitterling, T.; Heidbreder, A.; Stefani, A.; Fritz, J.; Ulmer, H.; Poewe, W.; Högl, B. Natural course of restless legs syndrome/Willis-Ekbom disease: long-term observation of a large clinical cohort. Sleep Med 2015, 16, 1252–1258. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Navarro, H.; García-Martín, E.; Agúndez, J.A.G.; Jiménez-Jiménez, F.J. Association between restless legs syndrome and other movement disorders [review]. Neurology 2019, 92, 948–964. [Google Scholar] [CrossRef] [PubMed]
- Lebrato Hernández, L.; Prieto León, M.; Cerdá Fuentes, N.A.; Uclés Sánchez, A.J.; Casado Chocán, J.L.; Díaz Sánchez, M. Restless legs syndrome in patients with multiple sclerosis: evaluation of risk factors and clinical impact. Neurología 2022, 37, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Connor, J.R.; Ponnuru, P.; Lee, B.Y.; Podskalny, G.D.; Alam, S.; Allen, R.P.; Earley, C.J.; Yang, Q.X. Postmortem and imaging based analyses reveal CNS decreased myelination in restless legs syndrome. Sleep Med 2011, 12, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.Y.; Kim, J.; Connor, J.R.; Podskalny, G.D.; Ryu, Y.; Yang, Q.X. Involvement of the central somatosensory system in restless legs syndrome: a neuroimaging study. Neurology 2018, 90, e1834–e1841. [Google Scholar] [CrossRef] [PubMed]
- Mano, T.; Thomas, R.J. Anatomo-functional basis of restless legs syndrome [comment]. Neurology 2018, 90, 945–946. [Google Scholar] [CrossRef] [PubMed]
- Serranová, T.; Slovák, M.; Kemlink, D.; Šonka, K.; Hallett, M.; Růžička, E. Prevalence of restless legs syndrome in functional movement disorders: a case-control study from the Czech Republic. BMJ Open 2019, 9, e024236. [Google Scholar] [CrossRef] [PubMed]
- Mace, C.J.; Trimble, M.R. Ten-year prognosis of conversion disorder. Br J Psychiatry 1996, 169, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Gelauff, J.; Stone, J. Prognosis of functional neurologic disorders [review]. Handb Clin Neurol 2016, 139, 523–541. [Google Scholar] [PubMed]
- Schrag, A.; Trimble, M.; Quinn, N.; Bhatia, K. The syndrome of fixed dystonia: an evaluation of 103 patients. Brain 2004, 127, 2360–2372. [Google Scholar] [CrossRef] [PubMed]
- Weiser, H.I. Motor sensory dysfunction of upper limb due to conversion syndrome. Arch Phys Med Rehabil 1976, 57, 17–19. [Google Scholar]
- Delargy, M.A.; Peatfield, R.C.; Burt, A.A. Successful rehabilitation in conversion paralysis. Br Med J 1986, 292, 1730–1731. [Google Scholar] [CrossRef] [PubMed]
- Leslie, S. Diagnosis and treatment of hysterical conversion reactions. Arch Dis Child 1988, 63, 506–511. [Google Scholar] [CrossRef] [PubMed]
- Speed, J. Behavioral management of conversion disorder: retrospective study. Arch Phys Med Rehabil 1996, 77, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Moene, F.C.; Spinhoven, P.; Hoogduin, K.A.L.; van Dyck, R. A randomised controlled clinical trial on the additional effect of hypnosis in a comprehensive treatment programme for in-patients with conversion disorder of the motor type. Psychother Psychosom 2002, 71, 66–76. [Google Scholar] [CrossRef]
- Schwingenschuh, P.; Pont-Sunyer, C.; Surtees, R.; Edwards, M.J.; Bhatia, K.P. Psychogenic movement disorders in children: a report of 15 cases and a review of the literature. Mov Disord 2008, 23, 1882–1888. [Google Scholar] [CrossRef] [PubMed]
- Dallocchio, C.; Arbasino, C.; Klersy, C.; Marchioni, E. The effects of physical activity on psychogenic movement disorders. Mov Disord 2010, 25, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Czarnecki, K.; Thompson, J.M.; Richard Seime, R.; Geda, Y.E.; Duffy, J.R.; Ahlskog, J.E. Functional movement disorders: successful treatment with a physical therapy rehabilitation protocol. Parkinsonism Relat Disord 2012, 18, 247–251. [Google Scholar] [CrossRef]
- Saifee, T.A.; Kassavetis, P.; Pareés, I.; Kojovic, M.; Fisher, L.; Morton, L.; Foong, J.; Price, G.; Joyce, E.M.; Edwards, M.J. Inpatient treatment of functional motor symptoms: a long-term follow-up study. J Neurol 2012, 259, 1958–1963. [Google Scholar] [CrossRef] [PubMed]
- Demartini, B.; Batla, A.; Petrochilos, P.; Fisher, L.; Edwards, M.J.; Joyce, E. Multidisciplinary treatment for functional neurological symptoms: a prospective study. J Neurol 2014, 261, 2370–2377. [Google Scholar] [CrossRef] [PubMed]
- Espay, A.J.; Edwards, M.J.; Oggioni, G.D.; Phielipp, N.; Cox, B.; Gonzalez-Usigli, H.; Pecina, C.; Heldman, D.A.; Mishra, J.; Lang, A.E. Tremor retrainment as therapeutic strategy in psychogenic (functional) tremor. Parkinsonism Relat Disord 2014, 20, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Jordbru, A.A.; Smedstad, L.M.; Klungsøyr, O.; Martinsen, E.W. Psychogenic gait disorder: a randomized controlled trial of physical rehabilitation with one-year follow-up. J Rehabil Med 2014, 46, 181–187. [Google Scholar] [CrossRef]
- Nielsen, G.; Ricciardi, L.; Demartini, B.; Hunter, R.; Joyce, E.; Edwards, M.J. Outcomes of a 5-day physiotherapy programme for functional (psychogenic) motor disorders. J Neurol 2015, 262, 674–681. [Google Scholar] [CrossRef] [PubMed]
- Dallocchio, C.; Tinazzi, M.; Bombieri, F.; Arnó, N.; Erro, R. Cognitive Behavioural Therapy and adjunctive physical activity for functional movement disorders (conversion disorder): a pilot, single-blinded, randomized study [letter]. Psychother Psychosom 2016, 85, 381–383. [Google Scholar] [CrossRef]
- Matthews, A.; Brown, M.; Stone, J. Inpatient physiotherapy for functional (psychogenic) gait disorder: a case series of 35 patients. Mov Disord Clin Pract 2016, 3, 603–606. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, G.; Buszewicz, M.; Stevenson, F.; Hunter, R.; Holt, K.; Dudziec, M.; Ricciardi, L.; Marsden, J.; Joyce, E.; Edwards, M.J. Randomised feasibility study of physiotherapy for patients with functional movement symptoms. J Neurol Neurosurg Psychiatry 2017, 88, 484–490. [Google Scholar] [CrossRef]
- Jacob, A.E.; Kaelin, D.L.; Roach, A.R.; Ziegler, C.H.; LaFaver, K. Motor retraining (MoRe) for functional movement disorders: outcomes from a 1-week multidisciplinary program. PM&R 2018, 10, 1164–1172. [Google Scholar]
- Jimenez, X.F.; Aboussouan, A.; Johnson, J. Functional neurological disorder responds favorably to interdisciplinary rehabilitation models. Psychosomatics 2019, 60, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Bullock, K.; Won, A.S.; Bailenson, J.; Friedman, R. Virtual reality-delivered mirror visual feedback and exposure therapy for FND: a midpoint report of a randomized controlled feasibility J Neuropsychiatry Clin Neurosci 2020, 32, 90-94.
- Demartini, B.; Bombieri, F.; Goeta, D.; Gambini, O.; Ricciardi, L.; Tinazzi, M. A physical therapy programme for functional motor symptoms: a telemedicine pilot study. Parkinsonism Relat Disord 2020, 76, 108–111. [Google Scholar] [CrossRef] [PubMed]
- Maggio, J.B.; Ospina, J.P.; Callahan, J.; Hunt, A.L.; Stephen, C.D.; Perez, D.L. Outpatient physical therapy for functional neurological disorder: a preliminary feasibility and naturalistic outcome study in a U.S. cohort. J Neuropsychiatry Clin Neurosci 2020, 32, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Petrochilos, P.; Elmalem, M.S.; Patel, D.; Louissaint, H.; Hayward, K.; Ranu, J.; Selai, C. Outcomes of a 5-week individualised MDT outpatient (day-patient) treatment programme for functional neurological symptom disorder (FNSD). J Neurol 2020, 267, 2655–2666. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, M.; Riello, M.; Bellamoli, V.; Bombieri, F.; Geroin, C.; Di Vico, I.A.; Tinazzi, M. Motor and non-motor outcomes after a rehabilitation program for patients with Functional Motor Disorders: a prospective, observational cohort study. NeuroRehabilitation 2021, 48, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Hebert, C.; Behel, J.M.; Pal, G.; Kasi, R.; Kompoliti, K. Multidisciplinary inpatient rehabilitation for Functional Movement Disorders: a prospective study with long term follow up. Parkinsonism Relat Disord 2021, 82, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Callister, M.N.; Klanderman, M.C.; Boddu, S.P.; Moutvic, M.A.; Geissler, E.N.; Traver, K.J.; Staab, J.P.; Hassan, A. Outpatient motor retraining for functional movement disorder: predictors of a favorable short-term response. Mov Disord Clin Pract 2023, 10, 1377–1387. [Google Scholar] [CrossRef] [PubMed]
- Guy, L.; Caceres, G.A.; Jackson, T.; Gorman, S.; Wilson, J.; Hsieh, Y.; Petty, D.; Harrison, S.; Pick, S. Routine outcomes and evaluation of an 8-week outpatient multidisciplinary rehabilitative therapy program for functional neurological disorder. J Neurol 2024, 271, 1873–1884. [Google Scholar] [CrossRef] [PubMed]
- McCombs, K.E.; MacLean, J.; Finkelstein, S.A.; Goedeken, S.; Perez, D.L.; Ranford, J. Sensory processing difficulties and occupational therapy outcomes for functional neurological disorder. Neurol Clin Pract 2024, 14, e200286. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, G.; Stone, J.; Lee, T.C.; Goldstein, L.H.; Marston, L.; Hunter, R.M.; Carson, A.; Holt, K.; Marsden, J.; Le Novere, M.; et al. Specialist physiotherapy for functional motor disorder in England and Scotland (Physio4FMD): a pragmatic, multicentre, phase 3 randomised controlled trial. Lancet Neurol 2024, 23, 675–686. [Google Scholar] [CrossRef] [PubMed]
- Polich, G.; Zalanowski, S.; Lewis, S.M.; Sugarman, S.; Christopolous, K.; Hebb, C.; Perez, D.L.; Baslet, G.; Shah, P.; Herman, S. Inpatient rehabilitation for acute presentation of motor functional neurological disorder (FND): a retrospective cohort study. Am J Phys Med Rehabil 2024, 103, 99–104. [Google Scholar] [CrossRef]
- Fahn, S.; Williams, D.T. Psychogenic dystonia [review]. Adv Neurol 1988, 50, 431–455. [Google Scholar] [PubMed]
- Gupta, A.; Lang, A.E. Psychogenic movement disorders [review]. Curr Opin Neurol 2009, 22, 430–436. [Google Scholar] [CrossRef]
- Trieschmann, R.B.; Stolov, W.C.; Montgomery, E.D. An approach to the treatment of abnormal ambulation resulting from conversion reaction. Arch Phys Med Rehabil 1970, 51, 198–206. [Google Scholar] [PubMed]
- Ness, D. Physical therapy management for conversion disorder: case series. J Neurol Phys Ther 2007, 31, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Silver, F.W. Management of conversion disorder. Am J Phys Med Rehabil 1996, 75, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Cardenas, D.D.; Larson, J.; Egan, K.J. Hysterical paralysis in the upper extremity of chronic pain patients. Arch Phys Med Rehabil 1986, 67, 190–193. [Google Scholar] [CrossRef] [PubMed]
- Morris, D.M.; Taub, E.; Mark, V.W.; Liu, W.; Brenner, L.; Pickett, T.; Stearns-Yoder, K.; Bishop-McKay, S.; Taylor, A.; Reder, L.; et al. Protocol for a randomized controlled trial of CI therapy for rehabilitation of upper extremity motor deficit: the Bringing Rehabilitation to American Veterans Everywhere project. J Head Trauma Rehabil 2019, 34, 268–279. [Google Scholar] [CrossRef]
- Mark, V.W.; Taub, E. Constraint-induced movement therapy for chronic stroke hemiparesis and other disabilities [review]. Restor Neurol Neurosci 2004, 22, 317–336. [Google Scholar] [PubMed]
- Taub, E.; Ramey, S.L.; DeLuca, S.; Echols, K. Efficacy of Constraint-Induced Movement Therapy for children with cerebral palsy with asymmetric motor impairment. Pediatrics 2004, 113, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Mark, V.W.; Taub, E.; Uswatte, G.; Morris, D.M.; Cutter, G.R.; Adams, T.L.; Bowman, S. Phase II randomized controlled trial of CI therapy in MS. Part I: effects on real-world function. Neurorehabil Neural Repair 2018, 32, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Hoover, C.F. A new sign for the detection of malingering and functional paresis of the lower extremities. JAMA 1908, 51, 746–747. [Google Scholar] [CrossRef]
- Tibben, M.I.; van Opdorp, A.; Bialek, W.; Schaap, J.; Tijssen, M.A.J.; Merkx, M.J.M. Efficacy of hypnosis and catalepsy induction in functional neurological disorders. Mov Disord Clin Pract 2024, 11, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Taib, S.; Ory-Magne, F.; Brefel-Courbon, C.; Moreau, Y.; Thalamas, C.; Arbus, C.; Simonetta-Moreau, M. Repetitive transcranial magnetic stimulation for functional tremor: a randomized, double-blind, controlled study. Mov Disord 2019, 34, 1210–1219. [Google Scholar] [CrossRef] [PubMed]
- Perez, D.; Edwards, M.J.; Nielsen, G.; Kozlowska, K.; Hallett, M.; LaFrance, W.C. Decade of progress in motor functional neurological disorder: continuing the momentum [review]. J Neurol Neurosurg Psychiatry 2021, 92, 668–677. [Google Scholar] [CrossRef] [PubMed]
- Marcolini, E.; Tolchin, B. Functional seizures [review]. Emerg Med Clin N Am 2021, 39, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Pasricha, P.J.; McKnight, M.; Villatoro, L.; Barahona, G.; Brinker, J.; Hui, K.; Polydefkis, M.; Burns, R.; McMahan, Z.H.; Gould, N.; et al. Joint hypermobility, autonomic dysfunction, gastrointestinal dysfunction and autoimmune markers (JAG-A): clinical associations and response to intravenous immunoglobulin therapy. Am J Gastroenterol in press.
- Serranová, T.; Di Vico, I.; Tinazzi, M. Functional movement disorder. Assessment and treatment [review]. Neurol Clin 2023, 41, 583–603. [Google Scholar] [CrossRef] [PubMed]
- Bennett, K.; Diamond, C.; Hoeritzauer, I.; Gardiner, P.; McWhirter, L.; Carson, A.; Stone, J. A practical review of functional neurological disorder (FND) for the general physician. Clin Med 2021, 21, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Joos, A. Ätiopathogenese und Behandlung von Funktionellen Neurologischen Störungen mit Fokus auf Funktionelle (Dissoziative) Anfälle [review]. Swiss Arch Neurol Psychiatry Psychother 2020, 171, w03081, [in German]. [Google Scholar]
- Gilmour, G.S.; Nielsen, G.; Teodoro, T.; Yogarajah, M.; Coebergh, J.A.; Dilley, M.D.; Martino, D.; Edwards, M.J. Management of functional neurological disorder [review]. J Neurol 2020, 267, 2164–2172. [Google Scholar] [CrossRef] [PubMed]
- Kirkwood, B.; Mark, V.W. Consistency of inclusion criteria for functional movement disorder clinical research studies: a systematic review. NeuroRehabilitation 2022, 50, 169–178. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR); American Psychiatric Association: Washington, USA, 2022. [Google Scholar]
- Stone, J. Lessons from a neurologist after 25 years of functional neurological disorder subspeciality practice [review]. Neurol Clin 2023, 41, 569–582. [Google Scholar] [CrossRef] [PubMed]
- Aybek, S.; Chan, A. The borderland of multiple sclerosis and functional neurological disorder: a call for clinical research and vigilance. Eur J Neurol 2023, 30, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Boissy, A.R.; Ford, P.J. A touch of MS: therapeutic mislabeling. Neurology 2012, 78, 1981–1985. [Google Scholar] [CrossRef] [PubMed]

| Volume Findings | Number of Studies | References |
|---|---|---|
| Focal decrease | 11 | [36,37,38,39,40,41,42,43,44,45,46] |
| Focal decrease and increase in different areas | 4 | [47,48,49,50] |
| Focal increase | 3 | [51,52,53] |
| No difference compared to non-FND subjects | 3 | [54,55,56] |
| Study [Reference] | N* | Diagnostic Method** | Intervention† | Dose (Months) | Setting†† | Motor Symptoms Targeted‡ |
|---|---|---|---|---|---|---|
| Weiser, 1976 [163] | 7 | MD referral | PT, counseling | 0.25-2 | Out | paresis |
| Delargy, 1988 [164] | 6 | MD referral | PT | 0.36-2.5 | In | walking |
| Leslie, 1988 [165] | 20 | MD referral | PT | 1-3 | In or Out | walking, paresis |
| Speed, 1996 [166] | 10 | MD referral | PT | 0.14-0.8 | In | walking |
| Heruti, 2002 [24] | 30 | MD referral | PT | Not stated | In | paresis |
| Moene, 2002 [167] | 45 | DSM-III |
PT + hypnosis vs PT |
3 | In | dystonia, walking, tremor, paresis |
| Schrag, 2004 [162] | 26 | Fahn-Williams | PT + CBT | Not stated | Not stated | dystonia, tremor |
| Schwingenschuh, 2008 [168] | 12 | Fahn-Williams | PT + CBT | Not stated | Out | dystonia, walking, tremor |
| Dallochio, 2010 [169] | 16 | Fahn-Williams | Walking therapy | 3 | Out | dystonia, walking, tremor |
| Czarnecki, 2012 [170] | 80 | Fahn-Williams | PT vs TAU | 0.25 | Out | walking, tremor, paresis |
| Saifee, 2012 [171] | 26 | MD referral | PT + CBT | 0.75 | In | dystonia, tremor, paresis |
| Demartini, 2014 [172] | 36 | MD referral |
Multidisciplinary rehab |
1 | In | dystonia, walking, tremor, paresis |
| Espay, 2014 [173] | 10 | MD referral |
Entrainment with biofeedback device |
0.03 | Out | tremor |
| Jordbru, 2014 [174] | 40 | MD referral |
PT + CBT vs waitlist |
0.75 | In | walking |
| Nielsen, 2015 [175] | 47 | Gupta-Lang | PT | 0.25 | Out | dystonia, walking, tremor, paresis |
| Dallochio, 2016 [176] | 29 | Fahn-Williams |
CBT vs CBT + PT vs TAU |
3 | Out | dystonia, walking, tremor |
| Matthews, 2016 [177] | 35 | MD referral | PT | ≤ 2 | In | walking |
| Nielsen, 2017 [178] | 57 | Fahn-Williams | PT vs nonspecific PT | 0.25 | Out | dystonia, walking, tremor |
| Jacob, 2018 [179] | 32 | Fahn-Williams | PT | 0.25 | In | dystonia, walking, tremor |
| Jimenez, 2019 [180] | 49 | DSM-5 | Pain multidisciplinary rehab | 0.25 | Out | FMD |
| Bullock, 2020 [181] | 12 | DSM-5 |
VR motor rehab + mirror feedback |
2 | Out | FMD or sensory symptoms |
| Demartini, 2020 [182] | 18 | Gupta-Lang | PT | 5.25 | Home | dystonia, walking, tremor, paresis |
| Maggio, 2020 [183] | 50 | DSM-5 | PT, CBT, goal setting | 1.5-3 | Out | dystonia, walking, tremor, paresis |
| Petrochilos, 2020 [184] | 78 | MD referral | PT, Multidisciplinary rehab, CBT | 1.4 | Out | dystonia, walking, tremor, paresis |
| Gandolfi 2021 [185] | 33 | Gupta-Lang | PT | 0.25 | Home | dystonia, walking, tremor, paresis |
| Hebert, 2021 [186] | 13 | Fahn-Williams | PT | 0.25-0.5 | In | dystonia, walking, tremor, paresis |
| Callister, 2023 [187] | 201 | Gupta-Lang | PT | 0.25 | In | walking, tremor, paresis |
| Guy, 2024 [188] | 31 | DSM-5 | PT + CBT | 2 | Out | dystonia, tremor, paresis |
| McCombs, 2024 [189] | 77 | MD referral | Sensory-oriented OT | 4 | Out | dystonia, walking, tremor, paresis |
| Nielsen, 2024 [190] | 241 | Gupta-Lang | PT vs TAU | 0.75 | Out | dystonia, walking, tremor, paresis |
| Polich, 2024 [191] | 22 | MD referral | PT | 0.5 | In | walking, paresis |
| Study | Outcome Measure‡‡ |
Immediate Results |
Follow-up (Months) ¶ |
RESULTS¶¶ |
|---|---|---|---|---|
| Weiser, 1976 [163] | Neurol exam | 100% improved | 1-96 | 86% retained gains |
| Delargy, 1988 [164] | Neurol exam | 100% improved | 8-14 | 100% retained gains |
| Leslie, 1988 [165] | Neurol exam | 85% improved | NA | |
| Speed, 1996 [166] | FIM | 100% improved | 7-36 | 78% retained gains |
| Heruti, 2002 [24] | Neurol exam | 55% improved | NA | |
| Moene, 2002 [167] | Neurol exam | 65% improved; no difference between groups | 6 | 84% retained gains; no difference between groups |
| Schrag, 2004 [162] | Neurol exam | 33% improved | NA | |
| Schwingenschuh, 2008 [168] | Neurol exam | 80% improved | NA | |
| Dallochio, 2010 [169] | PMDRS | 70% improved | NA | |
| Czarnecki, 2012 [170] | Neurol exam | 73% improved | 25-33 | Experimental group 60% self-rated improved vs 22% control treatment |
| Saifee, 2012 [171] |
Nonspecific self-assessment |
58% improved | NA | |
| Demartini, 2014 [172] | COPM, CGI | 67% improved | 12 | COPM: 100% retained gains; CGI: 33% retained gains |
| Espay, 2014 [173] | PMDRS | 100% improved | 3-6 | 50% retained gains, the other measures declined |
| Jordbru, 2014 [174] |
Functional Mobility Scale, FIM |
Experimental group generally improved | 12 | 100% gains retained |
| Nielsen, 2015 [175] | CGI | 96% improved | 3 | 85% retained gains |
| Dallochio, 2016 [176] | PMDRS |
Experimental groups improved, unlike TAU |
NA | |
|
Matthews, 2016 [177] |
Modified Rivermead Mobility Index |
Generally improved | NA | |
| Nielsen, 2017 [178] | CGI |
Assessment delayed until 6 m |
6 | Experimental group > control group gains |
| Jacob, 2018 [179] | CGI, PMDRS | 87% improved | 6 | 67% retained (only CGI assessed) |
| Jimenez, 2019 [180] |
In-lab movement measures |
Generally improved | NA | |
| Bullock, 2020 [181] |
Oxford Handicap Scale |
Improved experimental group only | NA | |
| Demartini, 2020 [182] | PMDRS, CGI | Improved (67%) | 6 | 72% retained gains |
| Maggio, 2020 [183] | Subjective change | Improved (34%) | NA | |
| Petrochilos, 2020 [184] | CGI, COPM | Generally improved | 6 | 100% retained gains |
| Gandolfi 2021 [185] | S-FMDRS, other in-lab measures | Generally improved | 3 | Gains lost |
| Hebert, 2021 [186] | CGI | 93% improved | 12 | 77% retained gains on CGI |
| Callister, 2023 [187] |
COPM ability subscale |
84% improved | NA | |
| Guy, 2024 [188] | Lab assessments | Generally improved | 3 | 100% retained gains |
| McCombs, 2024 [189] | Clinician judgement | 62% improved | NA | |
| Nielsen, 2024 [190] | SF-36; CGI | Not reported | 12 | No difference between groups on SF-36; results favored CGI, but statistics not stated |
|
Polich, 2024 [191] |
PT, OT judgement (ordinal scales) Berg Balance Scale |
95% improved | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





