1. Introduction
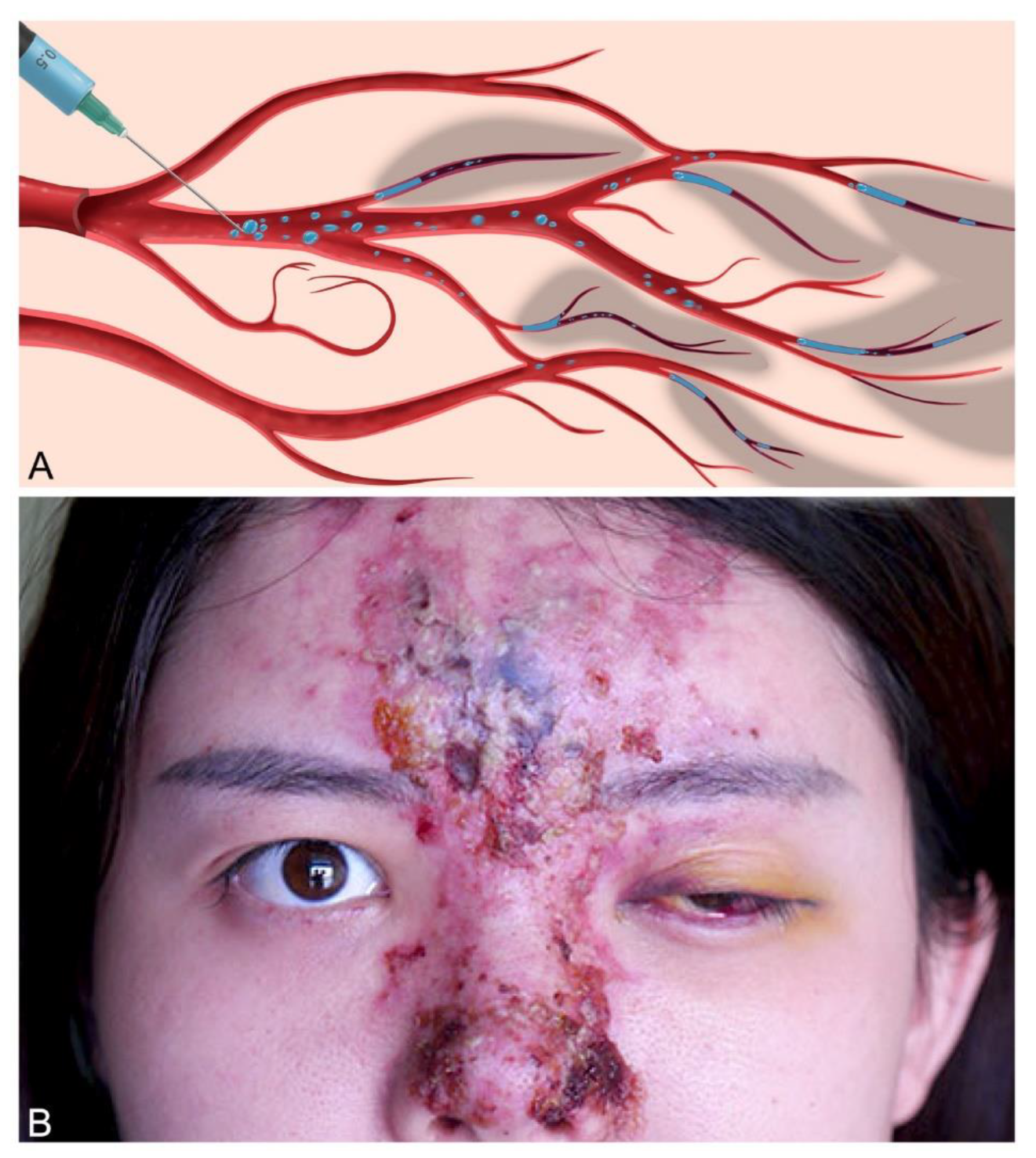
Iatrogenic arterial embolization stemming from accidental intravascular injection of therapeutic colloids and suspensions represents a potentially devastating medical etiology leading to acute soft tissue infarction [
1]. Depending on the affected vessel, the resultant negative sequelae can range from limb loss and facial disfigurement (known as
embolia cutis medicamentosa or
Nicolau syndrome) to pulmonary embolism, blindness, and acute cerebral stroke (
Figure 1) [
2,
3,
4,
5] Despite its rare incidence, the frequency of these injuries has risen substantially owing to the recent growth in the popularity of injectable gel implants, specifically hyaluronic acid (HA) colloidal mixtures employed in cosmetic facial rejuvenation and orthopedic joint viscosupplementation[
6,
7]. The pathomechanism of injury is presumed to arise from the inadvertent gel inoculation of an artery with subsequent localized occlusion and/or distal dispersal of embolic fragments [
8,
9,
10]. Given the variable nature of arterial networks, which demonstrate differing degrees of vascular redundancy, perfusion rates, and ischemic tolerance, the occurrence and magnitude of tissue injury can range from minor to extensive [
11,
12,
13].
The recently-alarming 30-fold increase in the incidence of this devastating condition has motivated new efforts to elucidate its primary mechanism of injury, highlighted by a dedicated United States Food and Drug Administration (FDA) panel on the subject, with the goal of informing future preventative and therapeutic interventions [
6,
14]. Etiologically, the rate and degree to which HA gels fragment and disperse upon arterial inoculation represents a potentially critical factor influencing the point of occlusion and mechanism of tissue underperfusion/ischemia, potentially offering insight into treatment strategies [
15]. Nonetheless, despite a comprehensive, application-specific body of literature on the physicochemical parameters and in vivo behavior of these implantable gels, little is known regarding their behavior as intravascular embolic agents, including their fragmentation, dispersal, and occlusive potential under physiological, human conditions [
16,
17,
18]. In this study, we introduce the Pulsatile Unit for the Laboratory Simulation of Arterioembolic Restrictions (PULSAR) as an artificial model of facial arterial HA gel inoculation and evaluate the embolic particularization and dispersibility of four HA gels of differing strengths and viscoelastic profiles.
3. Discussion
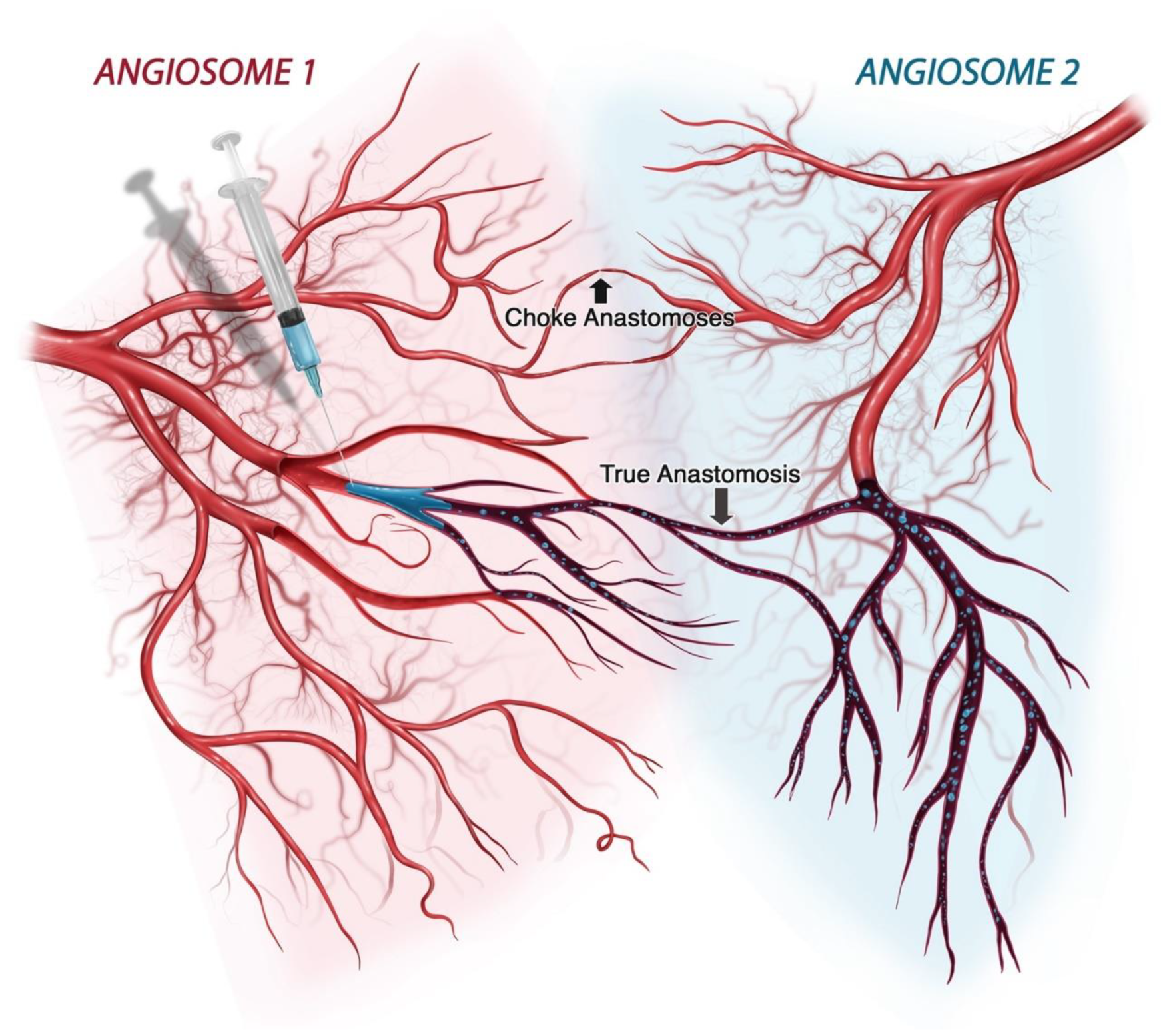
The susceptibility of soft tissues to iatrogenic arterial embolization depends on the degree of tissue tolerance to hypoxemia and the extent of perfusion deficit generated by the embolic load. In humans, arterial networks demonstrate significant regional differences in configuration, reflecting variability in perfusion redundancy [
19]. While some tissues exhibit an end-arterial arrangement sustained by one feeding vessel (e.g., retinal and distal cerebral circulation) others feature a robust perfusion system nourished by multiple neighboring angiosomes interconnected via true direct anastomoses (e.g., skin and muscle) (
Figure 11) [
20,
21,
22]. Such redundancy, necessary for thermoregulation and functional muscular hyperemia, also plays a protective role in instances of embolic occlusions, demanding a more distal target of blockade and/or larger volumes of gel inocula to sufficiently disrupt tissue perfusion to the point of ischemia [
15]. Conversely, an end-arterial design is potentially vulnerable to even small-volume proximal occlusions, though even redundant networks become increasingly end-arterial distally. Resultantly, the macrovascular fragmentation profile of an intra-arterial gel bolus, and its potential for microvascular dissemination, plays a pivotal role on the spatial distribution of an embolic agent and the likelihood of ischemic injury vs. non-injurious hypoperfusion. Therapeutically, the configuration of arterial occlusion bears special significance, particularly in instances involving enzymatically degradable HA gels, for which early intervention with hyaluronidase can be curative [
23,
24]. Thus, knowledge of the fragmentation profile of a gel embolus is necessary to better predict the locus of occlusion and the likelihood of ischemia at any given inoculation volume.
To date, the experimental characterization of iatrogenic arterioembolic injuries resulting from implantable hydrogels has mostly relied on research within animal models, specifically the rabbit auricular/femoral and rat femoral/epigastric arterial systems, employing live arterial inoculations with a limited number of filler products [
25,
26,
27,
28,
29,
30,
31]. Despite clinical and histological evidence suggesting microfragmentation of HA gel inocula with distal dispersal, the extent to which the initial gel bolus is mechanically disintegrated and its rate of dispersion, particle size distribution, and configuration of proximal versus distal occlusion, have not been conclusively established for gels of different mechanical parameters in humans [
32,
33,
34,
35,
36]. This gap in knowledge is a consequence of the intrinsic limitations within animal model systems, in which high-quality, real-time visualization of the gel behavior is not permissible, non-human physiological parameters are employed, and the testing of multiple gels with differing rheological parameters poses too high a financial, logistical, and animal sacrifice burden.
In the present study, the establishment of a novel artificial testing environment for the mechanical testing of gel emboli within a physiologically relevant, pulsatile macrofluidic system offers the opportunity for real-time evaluation of gel fragmentation and dispersal. In this study, calibration analysis confirms the ability of the PULSAR system to maintain controlled fluid pressures and specific flow rates within the natural range of human physiology, offering a significant advancement over previous experimental designs [
37,
38]. Furthermore, given the wide range of vessel diameters encompassed by the PULSAR network, the system can be adapted for studies employing a multitude of vascular parameters. In this study, our inoculation testing design aimed to specifically simulate the facial artery and its proximal branches due to the high incidence of injuries (58%) affecting the facial angiosome [
6]. Given the variable range of flow rates characteristic of the proximal facial artery, the PULSAR system was also capable of successfully maintaining different flow settings for the evaluation of flow rate effects on fragmentation, particle size, and obstructive potential at low, medium, and high physiological rates.
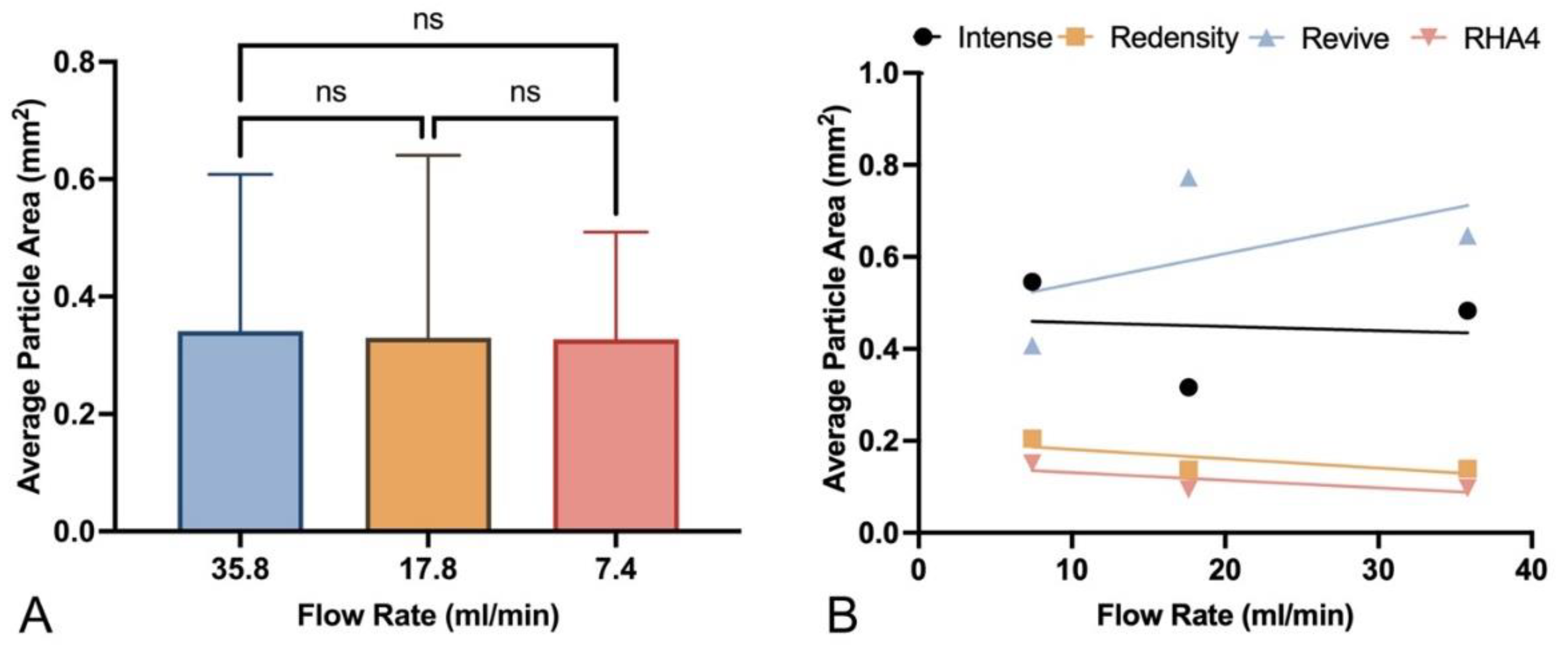
The experimental findings in this study confirm that HA gel fillers undergo substantial fragmentation into microparticles, with potential for wide dissemination, upon macrovascular inoculation, at all tested flow rates. Embolic particles were largely ovoid, encompassing a large range of sizes, from a few micrometers to greater than 1 mm, with the highest frequency occurring between approximately 60-800 μm in minor axis and 90-1400 μm in major axis. These findings agree with prior in vitro laser diffraction analysis of HA gel particles in aqueous dispersions as well as histological studies suggesting the capacity for arterial inoculations to launch microemboli capable of disrupting the distal microcirculation [
39,
40]. Furthermore, the presence of large particles greater than 1.5 mm was primarily encountered with inoculations employing Belotero Revive, a relatively viscous gel with a high tan(δ) of 1.27 and predominantly fluid behavior, which contrasts with the more elastic gel profile of the other tested products (tan(δ) values of 0.12, 0.39, 0.44). Notably, despite having the largest fragment sizes, Belotero Revive did not result in luminal obstruction of any branch within the PULSAR system, regardless of flow rate, consistent with prior rat femoral artery experiments using uncrosslinked HA solutions with tan(δ) >1 [
41].
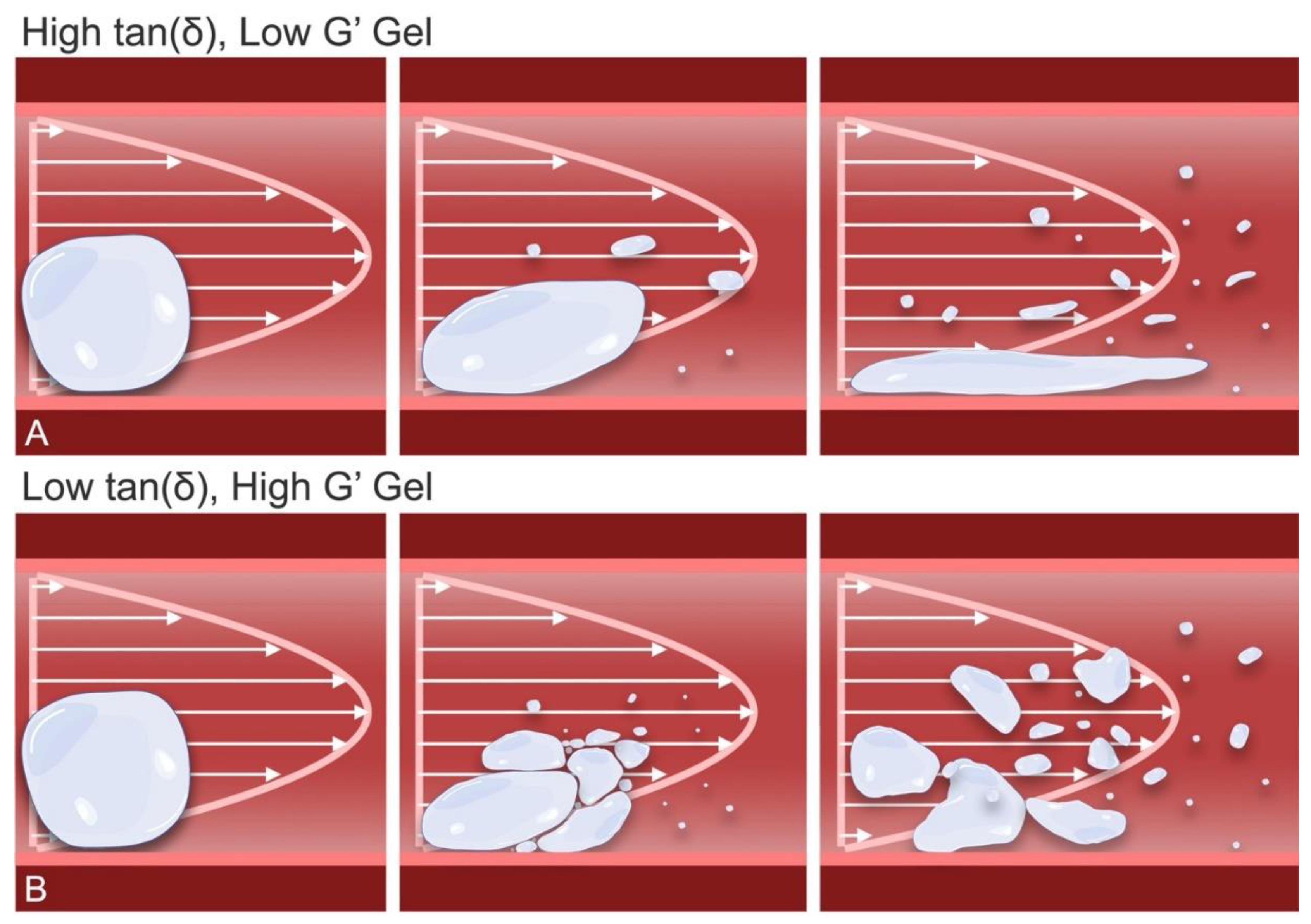
The likely cause for the reduced macro-occlusive capacity of relatively viscous, fluid HA products like Belotero Revive relates to their ability to easily deform with flow [
16,
42]. The combination of low gel strength and a high viscous partitioning renders the product highly pliable, allowing the gel to adaptively streamline its shape in response to intraluminal stress differentials, reducing its exposure to shear stress and deforming into long filamentous strands without achieving permanent macrovascular occlusion (
Figure 12A). Nonetheless, continuous distal dispersal of these thin gels is likely to result in eventual microfragmentation through brittle or extensional failure, suggesting that they may ultimately disperse into even smaller microparticles <(100 μm) within human microvascular networks, as previously histologically documented [
43]. Additional studies employing microfluidic networks will offer further insight into the dynamic microvascular behavior of gels like Revive. Importantly, despite their greater ability to evade proximal flow obstruction, thin uncrosslinked HA gels may still result in distal microvascular occlusion at sufficiently small vessel diameters, though their low degrees of chemical crosslinking are also likely to permit an accelerated rate of degradation, potentially shortening the duration of hypoperfusion [
15]. For this reason, such HA mixtures have traditionally shown limited injury potential in the skin, though highly susceptible tissues, such as the retina, are still at significant risk for injury given their short ischemic tolerance times [
41,
44,
45].
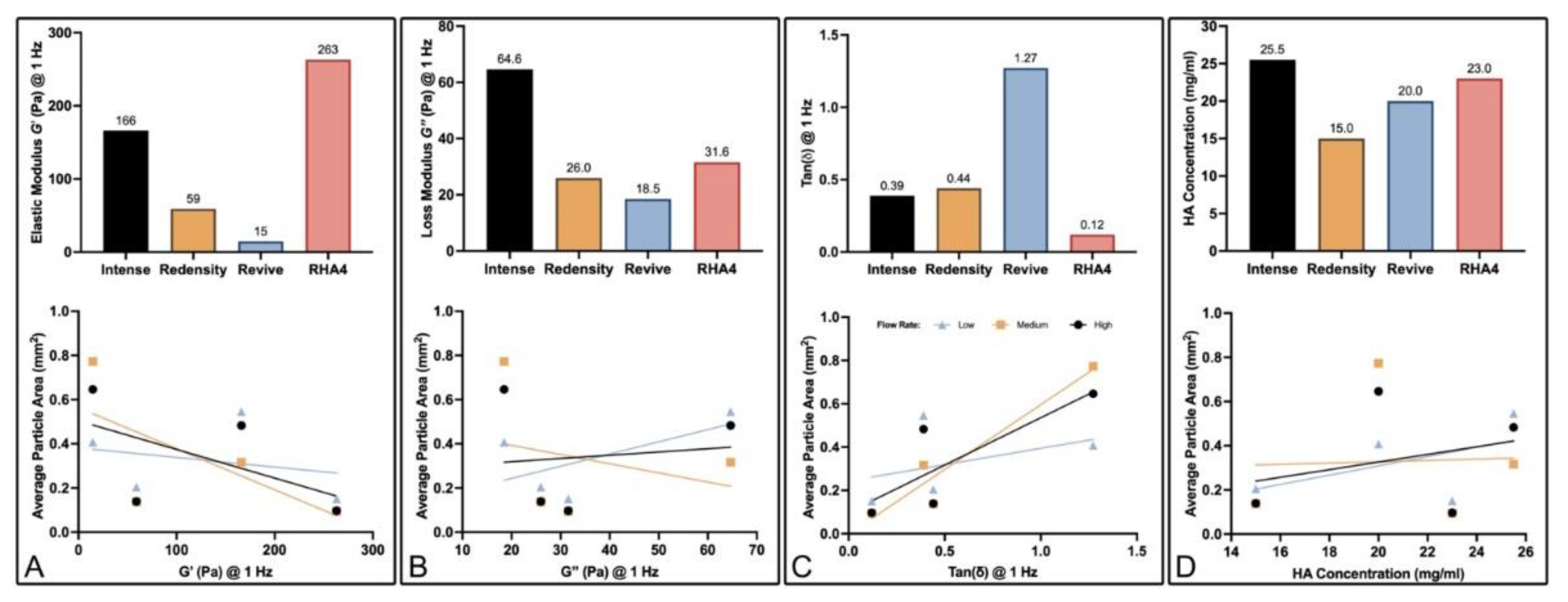
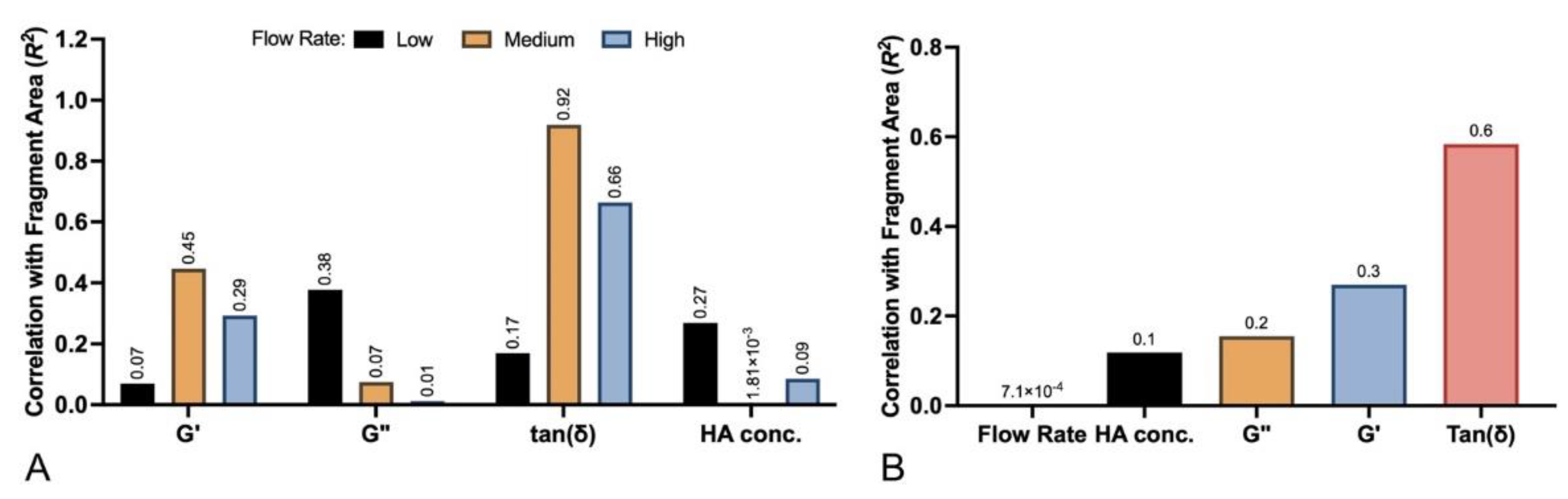
In contrast, the remaining fillers tested in this study (Intense, RHA4, and Redensity) demonstrated the more brittle behavior expected of viscoelastic solids (i.e., tan(δ) < 1). The decreased pliability of these products, given their higher elastic partitions, resulted in a tendency toward small particle fragmentation both during needle/cannula extrusion and intraluminal dispersion (
Figure 12B). Accordingly, the particle sizes for these fillers displayed significantly greater dependency on gel tan(δ) than any other tested physical parameter. The smallest average particle size was encountered with RHA4, which features a tan(δ) of 0.12, followed by Intense (0.39) and Redensity (0.44). Interestingly, the elastic strength (G’) of a product did not show high correlation with gel particle size, presumably because HA implants are not strong enough to resist shear stresses during cannulated extrusion into macrovascular environments. Such a feature is a necessary property of injectable HA gels, which must be able to flow during extrusion via thin needles and microcannulas [
46].
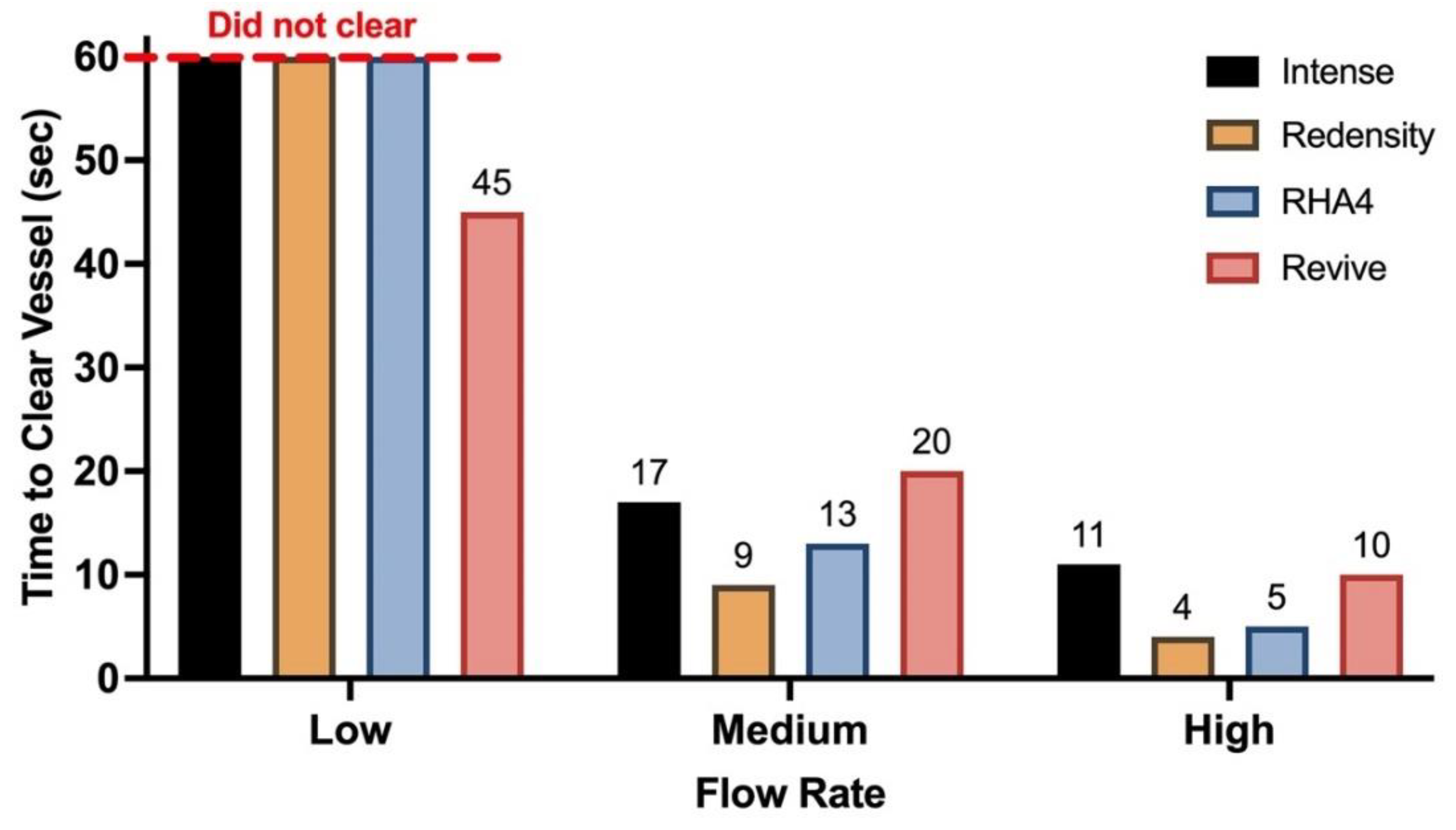
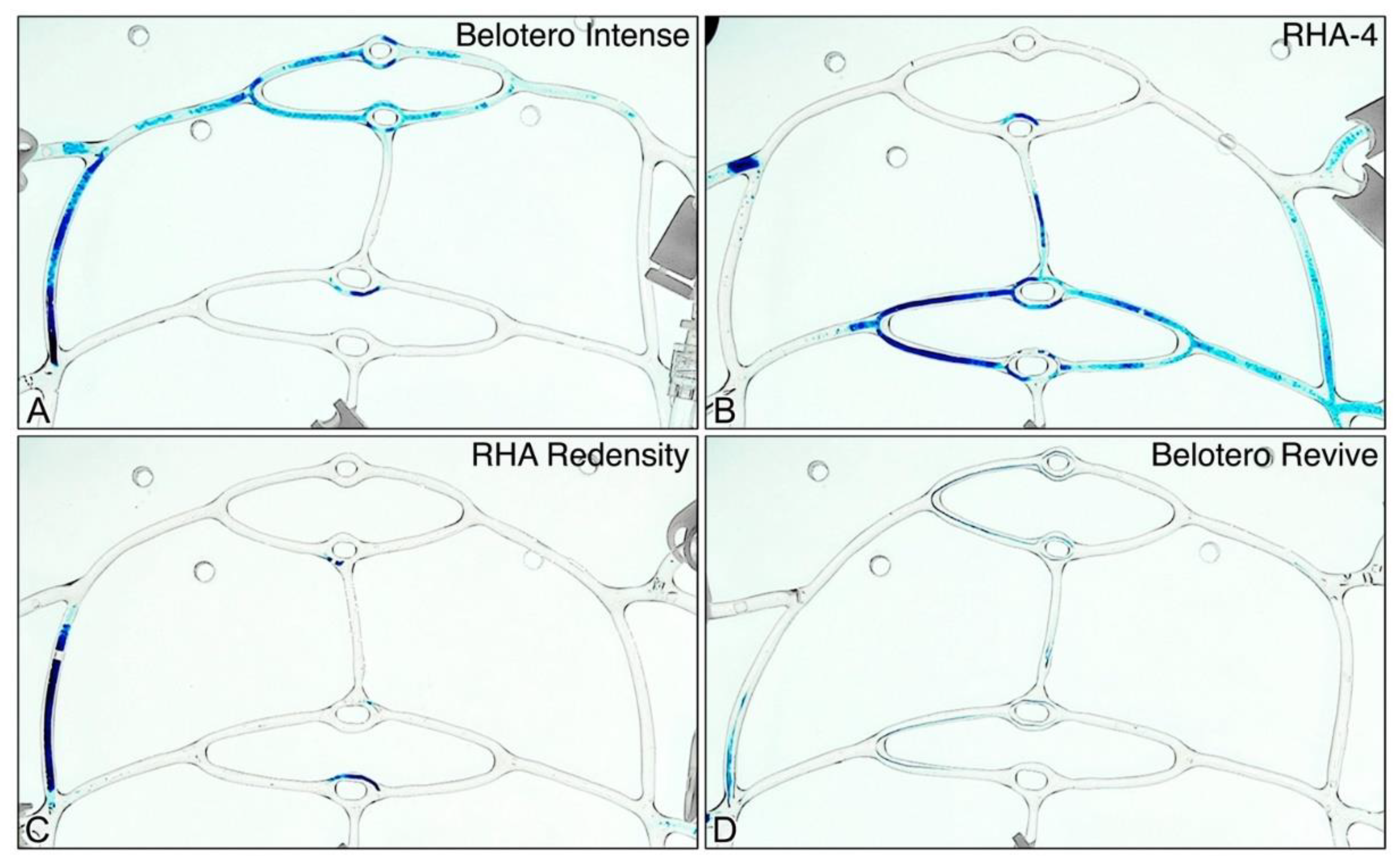
The higher elastic partition and/or strength of Intense, RHA4, and Redensity also correlated with their greater tendency toward complete branch occlusion. Although no product was able to sustain complete system obstruction at medium and high flow rates, all three products resulted in partial occlusion through blockade of a 1st generation branch, preventing distal flow within the affected segment. Products with the lowest tan(δ), specifically RHA4 and Intense, resulted in relatively longer filler plugs compared to Redensity, which features a lower elastic strength and higher tan(δ). Proximal macrovascular occlusion therefore appears to be facilitated by increased gel strength and elastic partition, as well as decreased flow rates. This dynamic interplay between flow parameters and mechanical gel properties likely creates a relatively random distribution of patent and occluded daughter branches as the filler disperses distally, resulting in irregular patterns of dysperfusion (
Figure 13). Such irregular distribution of microvascular occlusions likely within an dermal angiosome contributes to the similarly irregular appearance of ischemic skin in cases of filler-induced vascular occlusion, referred to as
livedo racemosa [
13,
47].
The findings presented in this study offer new clinical insight into the characterization of HA dermal fillers as iatrogenic embolic agents, with significant potential ramifications into our understanding of the mechanism of filler-associated ischemic injuries and relevant therapeutic interventions. Etiologically, the fragmentation of all gels into filler microparticles of varying sizes suggests that a distal, microvascular perfusion deficit plays a role in the mechanism of injury. This was further confirmed by the inability of all gel inoculations to achieve any degree of permanent macrovascular/proximal occlusion at physiologically medium and high flow rates, with branch occlusion occurring only at low flow. Resultantly, the embolic occlusive target is likely directed at vessels ranging from 100-1000μm in diameter, but potentially smaller given that a microfluidic network was not experimentally employed in this study. Certainly, the identification of microparticles < 50 μm suggests a role for a distal microvascular injury impacting distal arterioles and capillaries as well. These smaller microparticles may arise from the original inoculation or dislodge from proximal impacted gel plugs, which can act as reservoirs for secondary embolization, especially as the gel is partially degraded enzymatically and mechanically dispersed. These findings support the treatment of affected tissue beds through extravascular “flooding” of ischemic soft tissues with hyaluronidase, which have repeatedly demonstrated clinical efficacy, even if dosing standards have not yet been fully established [
23,
29,
48]. Such targeting of the distal microvasculature maximizes surface area exposure for gel degradation of distal emboli while limiting diffusion distances across vessel walls [
49]. Nonetheless, given that proximal gel plugs are possible with large volume inoculations of low tan(δ) gels into low flow vessels, simultaneous ultrasound-guided arterial mapping of proximal branches with selective treatment of occluded segments is likely of therapeutic benefit in some instances, as suggested by several recent case series [
50,
51].
Several limitations of the present study exist, which relate to the complex multitude of parameters that affect these types of injuries, including gel rheology, inoculation mechanics, fluid dynamics of the affected networks, and the functional biological nature of arterial systems. Critically, the volume and rate parameters of arterial inoculations are likely to influence the probability of proximal occlusion with any given product, variations of which were not explored in this study. For example, the rapid introduction of a large amount of gel proximally can lead to an accelerated increase in BMF viscosity, halting all flow through the affected arterial segment proximally. In this study, the rate of inoculation was kept within a “natural-feel” range of clinical injection at 0.01ml/sec, with a uniform bolus size of 0.2 ml used for all inoculations, but higher rates may be more likely to induce proximal obstruction. Similarly, the inoculation bolus size is also likely to alter the intra-arterial dissemination of fillers and their ultimate distribution within arterial networks. Additionally, given that gel properties can be partially altered by extrusion via small bore needles and microcannulas, the instrument used to inoculate an artery could shape the dynamic process of filler dispersal and microemboli formation [
52,
53]. Larger-diameter instruments may result in a predominance of larger particle sizes, facilitating proximal occlusion in physiological environments, while thinner needles may predispose to greater microfragmentation with distal embolic effects. Finally, given recent evidence suggesting a role for the coagulation system in exacerbating the occlusive potential of intra-arterial gel mixtures, the artificial design of our system, which employs a non-hematological BMF simulant, precludes the assessment of this component [
28,
29,
30,
31,
54]. The elucidation of the role of these additional variables will serve as an impetus for additional studies of HA gel inoculations employing microfluidic networks, variations in needle/cannula size and length, a range of injection volumes and rates, and physiological BMF solutions.
4. Conclusions
This study is the first to evaluate the role of gel parameters on the dispersal behavior of HA fillers within an artificial model of arterial embolism. The use and validation of the PULSAR system allowed for precise control and simulation of physiological conditions, thus providing a clinically relevant platform for evaluating the intravascular behavior of HA fillers. The experimental results demonstrate that HA fillers undergo substantial fragmentation upon intra-arterial injection, producing ovoid embolic particles of varying sizes, with the highest frequency observed between 60-800 μm in minor axis and 90-1400 μm in major axis. Fillers with higher tan(δ) values exhibited greater microfragmentation, suggesting that gel strength and viscoelastic partitioning play an important role in determining particle size and dispersibility following intravascular injection. HA gels with lower tan(δ) values yielded smaller, more uniform fragments due to more brittle failure, whereas those with higher tan(δ) produced larger, filamentous strands due to their increased pliability. Altering flow rates within a physiological range did not significantly influence the size distribution of embolic particles, indicating that the physical properties of the gels predominantly govern their fragmentation behavior. Nonetheless, decreased flow rate settings showed a greater predisposition for complete, proximal branch occlusion, whereas physiologically medium to high facial arterial flow rates resisted proximal macrovascular occlusion altogether. Ultimately, this research advances our understanding of the pathomechanisms underlying iatrogenic arterial embolization by HA fillers and suggests a mechanism by which micro-emboli disperse and cover larger surface areas within a functional angiosome distal to the site of cannulation, leading to cerebroretinal ischemia. The insights gained from this study could inform the development of therapeutic protocols, potentially reducing the incidence of severe complications such as tissue ischemia, blindness, and stroke. Future studies should explore the role of additional rheological, vascular, and inoculation variables, including gel cohesion, microvascular networks, and inoculation volume, rate, and needle/cannula gauge/length.
5. Materials and Methods
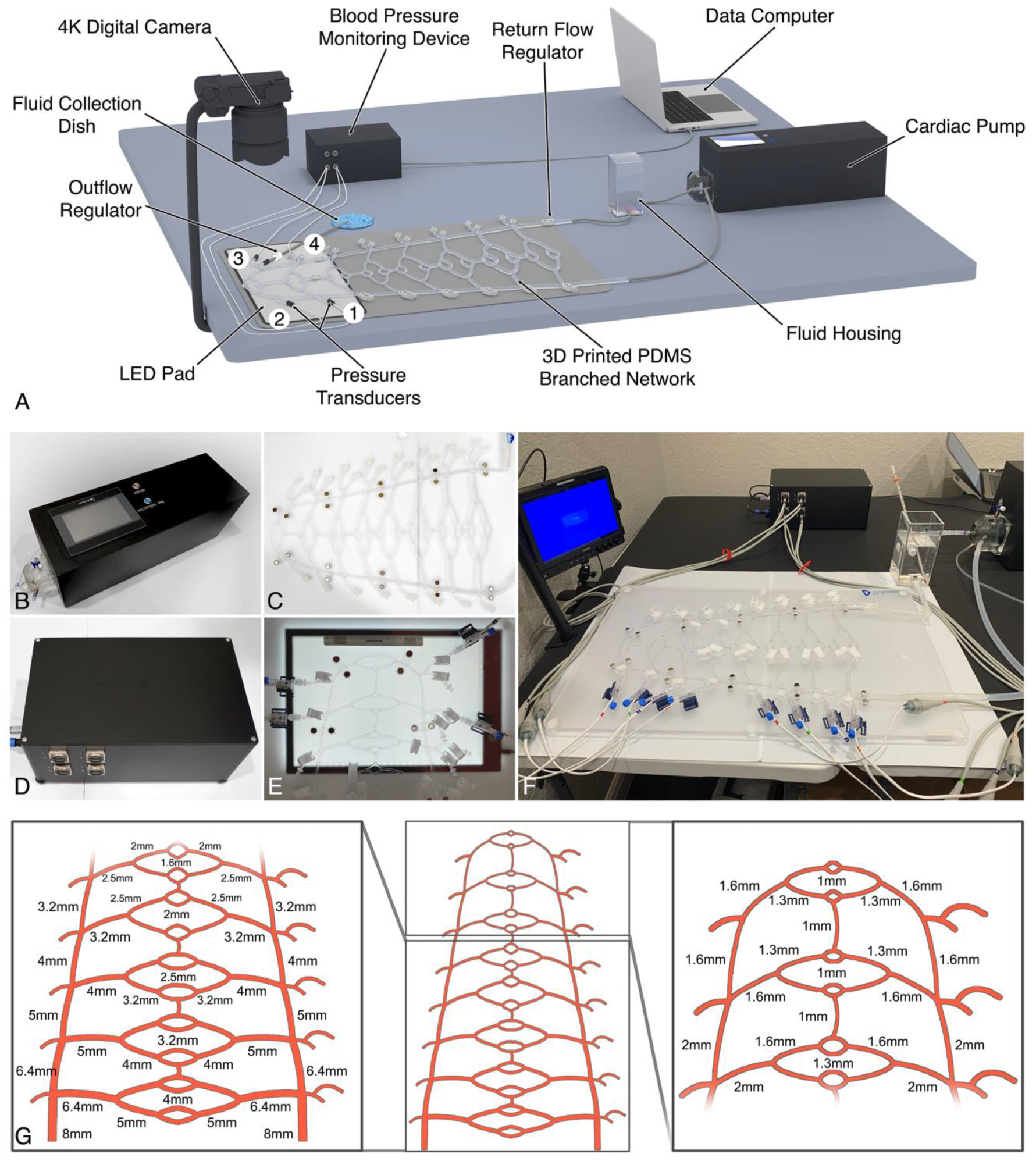
5.1. Vascular Model Design and Assembly
An experimental physiological model of the human soft tissue macrocirculation was developed to simulate the pulsatile, laminar flow environment of the distal common carotid and proximal facial arterial branches (Pulsatile Unit for the Laboratory Simulation of Arterioembolic Restrictions, PULSAR), as illustrated in
Figure 14. The components of the system include a modified cardiac pump (EDU-Heart Pump, Trandomed, Ningbo, China), calibrated to mimic the range of flow rates observed in the human common carotid artery, connected to a 3D-printed polydimethylsiloxane (PDMS) tubular branched circuit (Peripheral Vessel Model (custom), Trandomed, Ningbo, China) [
55]. The circuit, composed of Shore A-44 PDMS elastomer with a longitudinal tensile strength of 4.91 MPa, falling within the range for small arteries, incorporates an initial input diameter of 8 mm followed by seven sequential branching generations obeying Murray’s law of minimum work, resulting in progressively narrower branches down to the smallest diameter of 1 mm [
56,
57,
58]. Each main branching generation was designed with a twice-bifurcating “vascular bed” interconnected by anastomotic branches, with the distal beds mimicking the facial artery and its proximal branches (range of ~1-2 mm in diameter). The design incorporates 24 individual access ports — 8 on the supply side and 16 on the return side of the vascular beds — to facilitate fluid sampling, pressure monitoring, and diameter-specific outflow extensions. Continuous fluid pressure measurements were recorded directly from fluid pressure transducers connected to each respective port, processed via an 8-channel monitoring system (BP Monitoring System, Trandomed, Ningbo, China) featuring a sampling rate of 4000 Hz and a range of 0-200 mmHg.
5.2. System Priming with Blood Mimicking Fluid
The circulating blood-mimicking fluid (BMF) consisted of a 50% mixture, by volume, of glycerol and water. This mixture was prepared by combining 500 ml of 99.5% glycerol with 500 ml of deionized distilled water (Sigma-Aldrich, Inc., St. Louis, MO), using a magnetic hot plate stirrer (Scilogex SCI340-HS, Rocky Hill, CT) [
59]. The glycerol was heated to 50˚C and stirred at 250 rpm. Subsequently, the distilled water was gradually introduced into the vortex and stirred at 600 rpm for 15 minutes or until the mixture became homogeneous. The mixture was then allowed to cool to 20˚C before circulation within the model. Once cooled, the BMF was gradually introduced into the system by first filling the pump cavity, followed by the BMF housing, and then the tubular network, with distal clamps positioned at each port to prevent leakage. All air pockets contained within the tubular network and at each port were suctioned out of the system and subsequently replaced with BMF for complete system priming.
5.3. System Calibration and Validation
Calibration of the PULSAR unit was performed in triplicates across a physiological range of heart rates (specifically 60, 70, 80, 90, and 100 bpm) and relevant stroke volumes (3, 4, and 4.5 ml/beat), aiming to stay within the physiological blood pressure range (95-165/65-105 mmHg) and common carotid artery flow rates (140-620 ml/min) for the general population [
60,
61,
62,
63,
64]. Pressure calibration was achieved by adjusting the outflow regulator clamp controlling the BMF return path toward the fluid housing and by control of an additional regulator (Flow Controller Extension Set, Amsino International, Pomona, CA) at the distal sampling line connected to port 3 (
Figure 14A). Flow rates were directly measured from the inoculation access port (port 1) over 10 seconds, also performed in triplicates. Blood pressure measurements were recorded over 1 minute and exported into digital spreadsheets in Microsoft Excel software version 16.83 (Microsoft Corp., Redmond, WA) with calculation of average systolic and diastolic pressures, mean arterial pressure (MAP), and Reynolds number for each setting (fluid density 1120 kg/m³, dynamic viscosity 0.00674 Pa·s, vessel diameter 0.002 m). Additionally, laminar flow was further confirmed via direct visualization through the opened distal outflow from port 1.
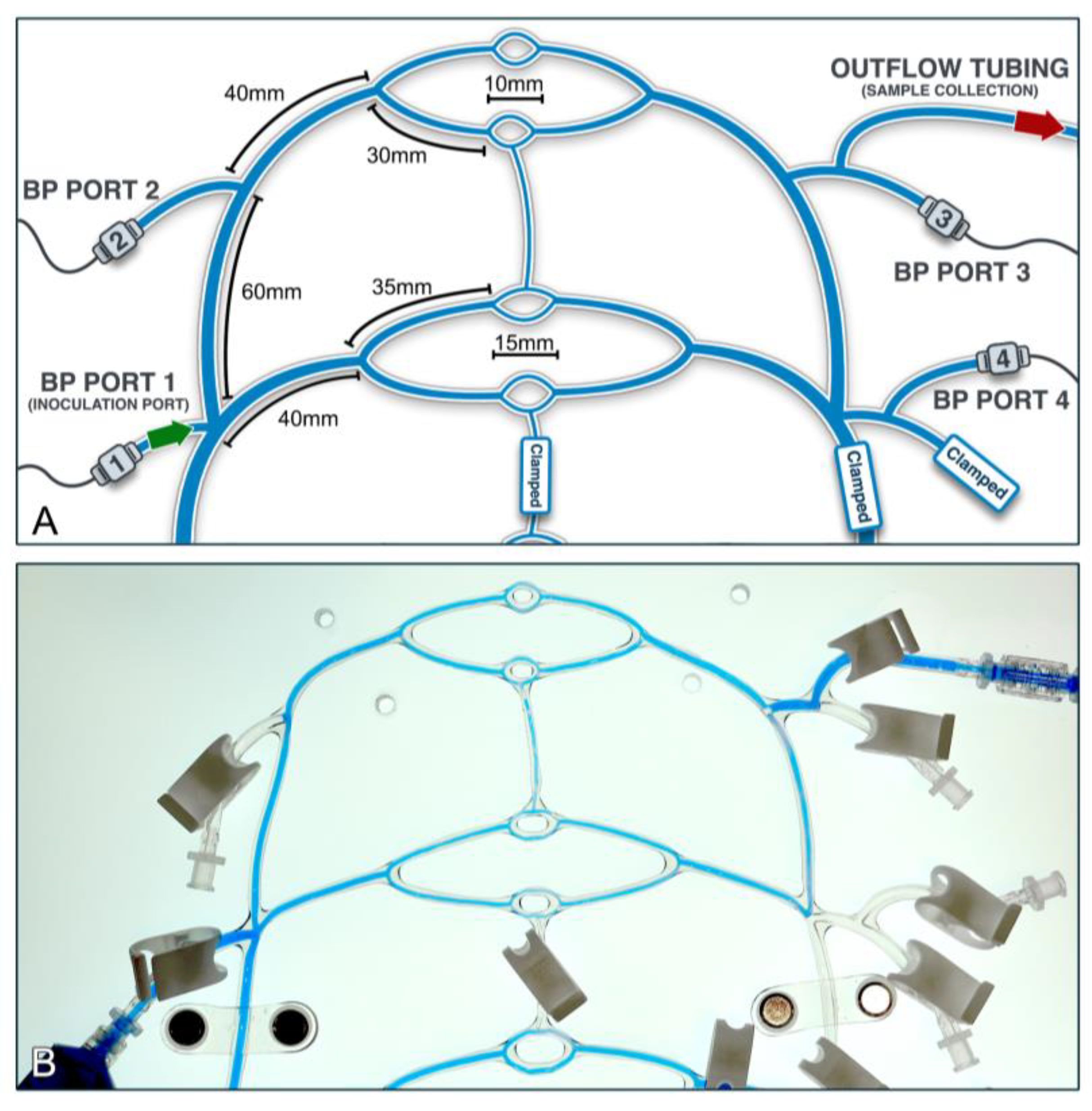
Following whole system calibration, the circuit was further adjusted for facial artery simulation (
Figure 15). Modifications included clamping the distal return tubing for the two distal vascular beds in order to isolate the distal network (encompassing the 2 mm-diameter tubing and its 1.6 mm diameter daughter branches) for simulation of the proximal paramandibular facial artery in humans (diameter 0.9-2.5mm) [
65,
66,
67]. Repeat system calibration was again carried out, aiming to mimic physiological blood pressure while maintaining flow rates within the facial artery range (7.3-35.3 ml/min) [
68,
69,
70,
71]. Finally, upon completion, three different heart rate and stroke volume settings were established to span low (~10 ml/min), medium (~18 ml/min), and high (~36 ml/min) flow rates for the experimental system inoculations.
5.4. Gel Inoculation and Videographic Capture of Embolic Dissemination
Simulated inoculation of HA gel into the intra-arterial milieu was achieved through the delivery of a 0.2 ml bolus of four different FDA-approved dermal fillers featuring extremes of gel strength (G’) and viscoelastic partitionings (tan(δ)), chosen from two product manufacturers. Specifically, RHA Redensity and RHA4 (Revance Aesthetics, Nashville, TN), representing the manufacturer’s Preserved Network Technology® (PNT) crosslinking process and Belotero Revive and Belotero Intense (Merz Aesthetics, Raleigh, NC), which feature Cohesive Polydensified Matrix® (CPM) crosslinking technology. The chemical and physical properties of each product are listed in
Table 4, with
Table 5 summarizing the meaning of basic rheological parameters [
72].
Table 4 data was obtained from Leffler et al.’s and Faivre et al.’s previously reported values [
73,
74]. Prior to inoculation, 1 ml of each gel was mixed with 100 μl of 1% aqueous toluidine blue (Carolina Biological Supply Company, Burlington, NC), analogous to other aqueous dispersal protocols [
75,
76]. The gel product and the dye were each transferred into separate 1 ml syringes (1 ml Luer Lock Tip Syringe, Exelint, Redondo Beach, CA). The gel-containing and dye-containing syringes were then connected via a Luer-to-Luer connector (Rapidfill Connector, Baxter Healthcare, Deerfield, IL) and subsequently mixed back and forth 20 times until the gel was uniformly dyed.
Inoculation was performed upon activation of the PULSAR system and verification of pressure and flow parameters. The gel bolus was subsequently introduced into port 1 and extruded into the circulating fluid employing a 27G, 50 mm microcannula (Steriglide, TSK Laboratories, Vancouver, BC) at a clinically appropriate extrusion rate of 0.01 ml/sec, akin to other clinical/experimental evaluations [
77,
78]. The dispersal profile of the filler within the distal system was subsequently captured via continuous high-resolution video recording with a 4K, 24.2 megapixel digital single lens reflex (DSLR) camera (Alpha 6600, E18-135 mm Lens, Sony, New York, NY) over a span of 5 minutes post-inoculation or until all of the visible inoculum dissipated from the system or resulted in terminal, static flow restriction. In between inoculations, the circulating fluid was fully cleared from the inoculated tubing and any filler remnants flushed out of the system through the fluid collection port.
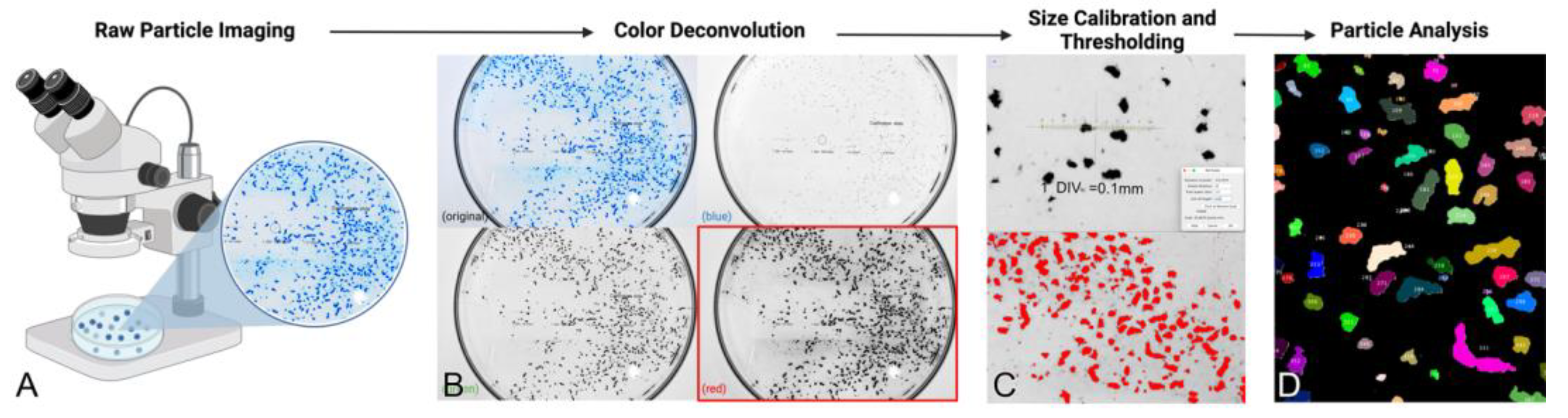
5.5. Macroscopic and Microscopic Imaging of Embolic Gel Fragments
Macroscopic particle size evaluation was performed by collection of circulating fluid directly from the return tubing onto a 100 x 20 mm Petri dish (Pyrex Dish, Corning, Rosemont, IL) equipped with a 0.01 mm glass calibrating ruler (Microscope Calibration Slide, MUHWA Scientific, Zhanjiang, CN). Still images of the returning fluid were obtained for each product inoculation immediately upon collection with a high-resolution (50 µm) photographic setup employing a 4K, 20.9-megapixel DSLR camera (D7500, Nikon, Melville, NY) and a macro lens (Nikkor 105 mm f/2.8G, Nikon, Melville, NY) backlit by an LED lighting pad (LitEnergy A4 Ultra-thin LED Lightbox, GGE Corp. Shenzhen, CN). Returning fluid sampling was also microscopically evaluated for identification of microparticles <50 µm. A 100 μl sample of the returning circulating fluid containing the dispersed inoculum was evaluated via light microscopy at 100X magnification (B120 binocular compound microscope, Amscope, Irvine CA) with digital capture employing a 5-megapixel color eyepiece camera (MD-500, Amscope, Irvine CA). The particle field was scanned and randomly sampled through capture of five different view fields via dedicated microimaging software (Amlite, Amscope, Irvine CA).
5.6. Gel Particle Size and Clearance Analysis
Captured high resolution images were analyzed for particle size using ImageJ (ImageJ, U. S. National Institutes of Health, Bethesda, Maryland, USA). Gel remnants were quantified as the combined area encompassed by dyed fragments remaining within the system at the termination of the inoculation session utilizing image analysis software with the following protocol. First, high resolution macroscopic images were opened in ImageJ and underwent RGB color deconvolution to isolate the red, green, and blue image splits. The red split image was chosen for particle analysis as it best isolates the blue particle fragments. Next, the image size was calibrated using the calibration slide glass. After calibration, a standard image threshold was applied and adjusted to threshold the in-field particle fragments. The threshold was applied, leaving white contrasted particles against a black background. Finally, using the ‘analyze particle’ tool with lower bound 4 square pixel particle size cutoff, each particle’s area, major and minor axes lengths, perimeter, circularity, and aspect ratios were computed and overlay masks were applied to each image for visualization (
Figure 4). This protocol was also used to analyze light microscopy images. All images were opened in ImageJ and analyzed with the following workflow: Image → Color → Split Channels. On Red Channel image split: Image → Adjust → Threshold → Apply (after adjustment). Analyze → Set Measurements → Select (Area, standard deviation, integrated density, shape descriptors, perimeter). Process → Binary → Fill Holes. Process → Binary → Watershed. Define ROI with freehand selection. Analyze → Analyze Particles → Size (pixels2): 4-infinity; Select (Display results, exclude on edges, include holes, overlay, summarize) → OK.
To determine the time to clearance, high-definition videos were opened in ImageJ as audio video interleave (AVI) files. Snapshots were acquired of the AVIs at 0.1 sec intervals. Each snapshot was then merged into a stack with the following command flow: Image → Stacks → Images to Stack. The generated stack had a color threshold applied to all images comprising the stack with the following command flow: Image → Adjust → Color Threshold. The RBG and brightness thresholds were set to primarily highlight the blue dyed gel fragments. Once the thresholds were set and applied to the stack, the following command flow was applied to quantify the time-dependent embolic burden within the observed channels: Image → Stacks → Measure Stack. Measurements were defined with the following command flow: Analyze → Set Measurements → Area, Shape Descriptor, Area Fraction, Integrated Density. The stack measurement was exported to the ImageJ results tab and plotted with the x and y axis defined as the time and % area, respectively. Thus, it was possible to quantitatively observe when the area spike related to the intravascular filler traversing the network cleared the PULSAR network. This data was graphed as columnar data.
5.7. Statistical Analysis
Statistical analysis was conducted using GraphPad Prism (GraphPad Prism Version 10.2.3, GraphPad Software, LLC, San Diego CA). Distribution plots for each filler were constructed without any data trimming. Either one or two-way ANOVA analysis was used to test for significance between and within groups when appropriate. Linear regression analysis was conducted when appropriate. Significance was denoted as *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. In cases where all pairwise comparisons could not fit in the graphs, the p values from the analyses are listed in the supporting information, as respectively indicated. Plotted values above each bar graph represent the mean value of that group. Data figures and illustrations were created using BioRender design software (BioRender, Toronto, CA).
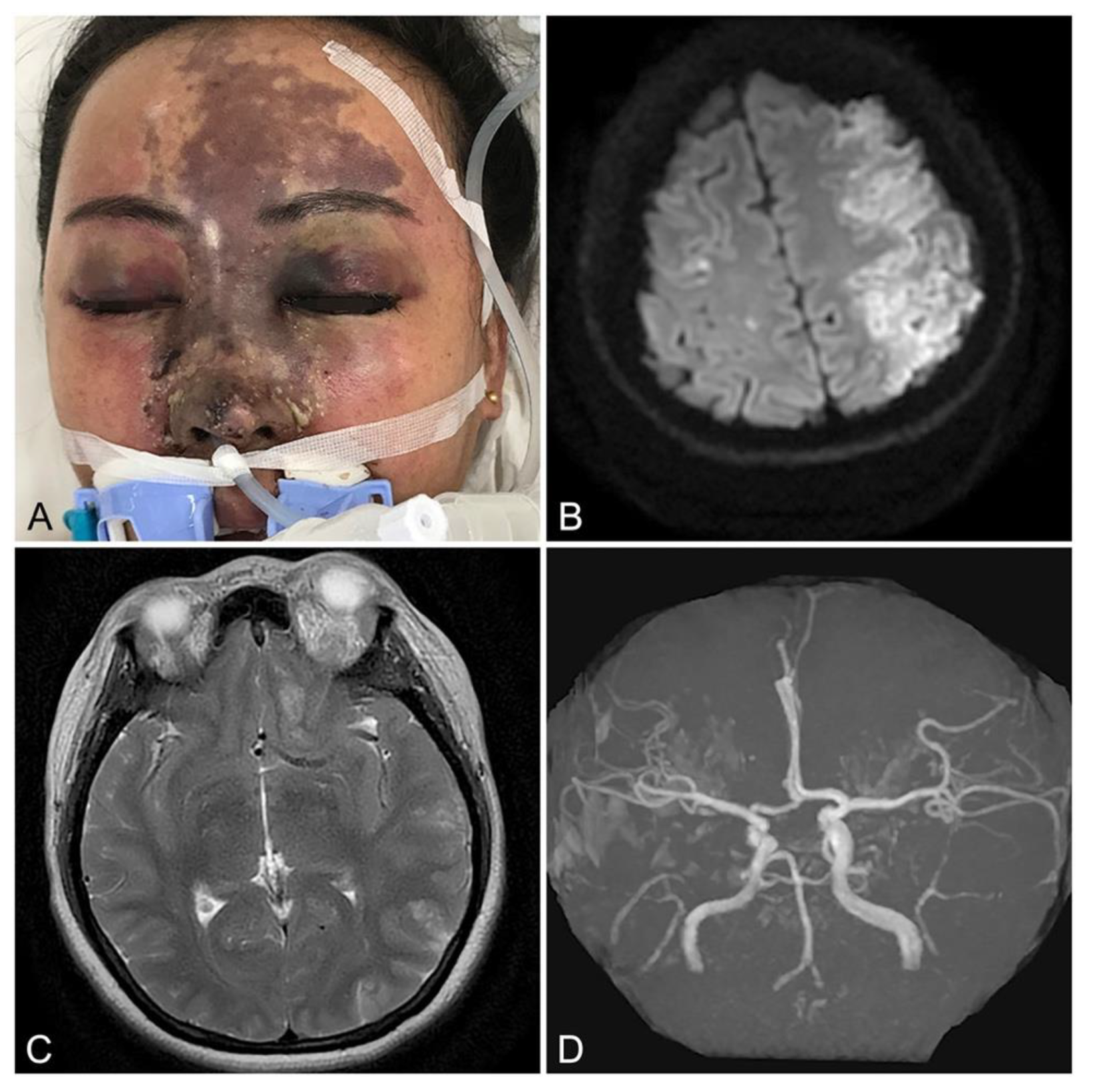
Figure 1.
Example of extensive facial soft tissue ischemia with neuroophthalmological sequelae resulting from iatrogenic filler embolization: (A) - Appearance of 40 year-old female 5 days following arterioembolic injury resulting from dorsal nasal hyaluronic acid filler augmentation, revealing ischemic changes of the frontonasal skin of the face. (B) Diffusion weighted axial magnetic resonance imaging (MRI) demonstrating left hemi-frontoparietal cerebral infarction. (C) T2-weighted axial MRI revealing edema and ischemic changes affecting the left optic nerve and orbital soft tissues. D) Magnetic resonance angiography demonstrating intact proximal cerebral circulation (circle of Willis and anterior, middle, and posterior cerebral arteries), suggesting a distal embolic etiology. Reproduced with permission from Yang et al. [
3], 2020, Springer Nature.
Figure 1.
Example of extensive facial soft tissue ischemia with neuroophthalmological sequelae resulting from iatrogenic filler embolization: (A) - Appearance of 40 year-old female 5 days following arterioembolic injury resulting from dorsal nasal hyaluronic acid filler augmentation, revealing ischemic changes of the frontonasal skin of the face. (B) Diffusion weighted axial magnetic resonance imaging (MRI) demonstrating left hemi-frontoparietal cerebral infarction. (C) T2-weighted axial MRI revealing edema and ischemic changes affecting the left optic nerve and orbital soft tissues. D) Magnetic resonance angiography demonstrating intact proximal cerebral circulation (circle of Willis and anterior, middle, and posterior cerebral arteries), suggesting a distal embolic etiology. Reproduced with permission from Yang et al. [
3], 2020, Springer Nature.
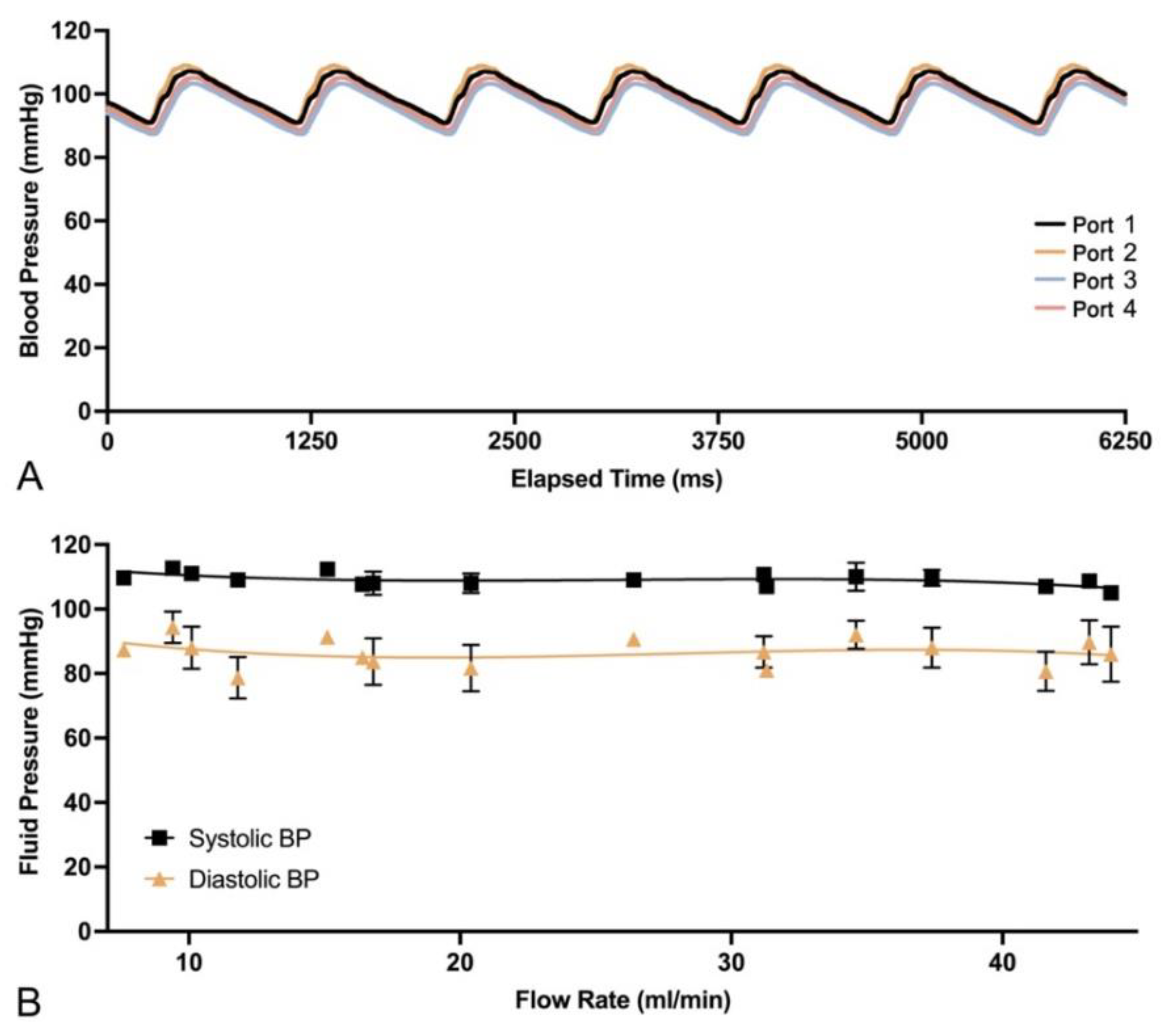
Figure 2.
Data plots for PULSAR system calibration: (A) Illustrative pressure waveform for all four distal ports (1-4) during system activation at 65 bpm. (B) Summary plot of average systolic and diastolic fluid pressures relative to flow rate, showing the ability of the system to maintain physiological pressures at different flow rates.
Figure 2.
Data plots for PULSAR system calibration: (A) Illustrative pressure waveform for all four distal ports (1-4) during system activation at 65 bpm. (B) Summary plot of average systolic and diastolic fluid pressures relative to flow rate, showing the ability of the system to maintain physiological pressures at different flow rates.
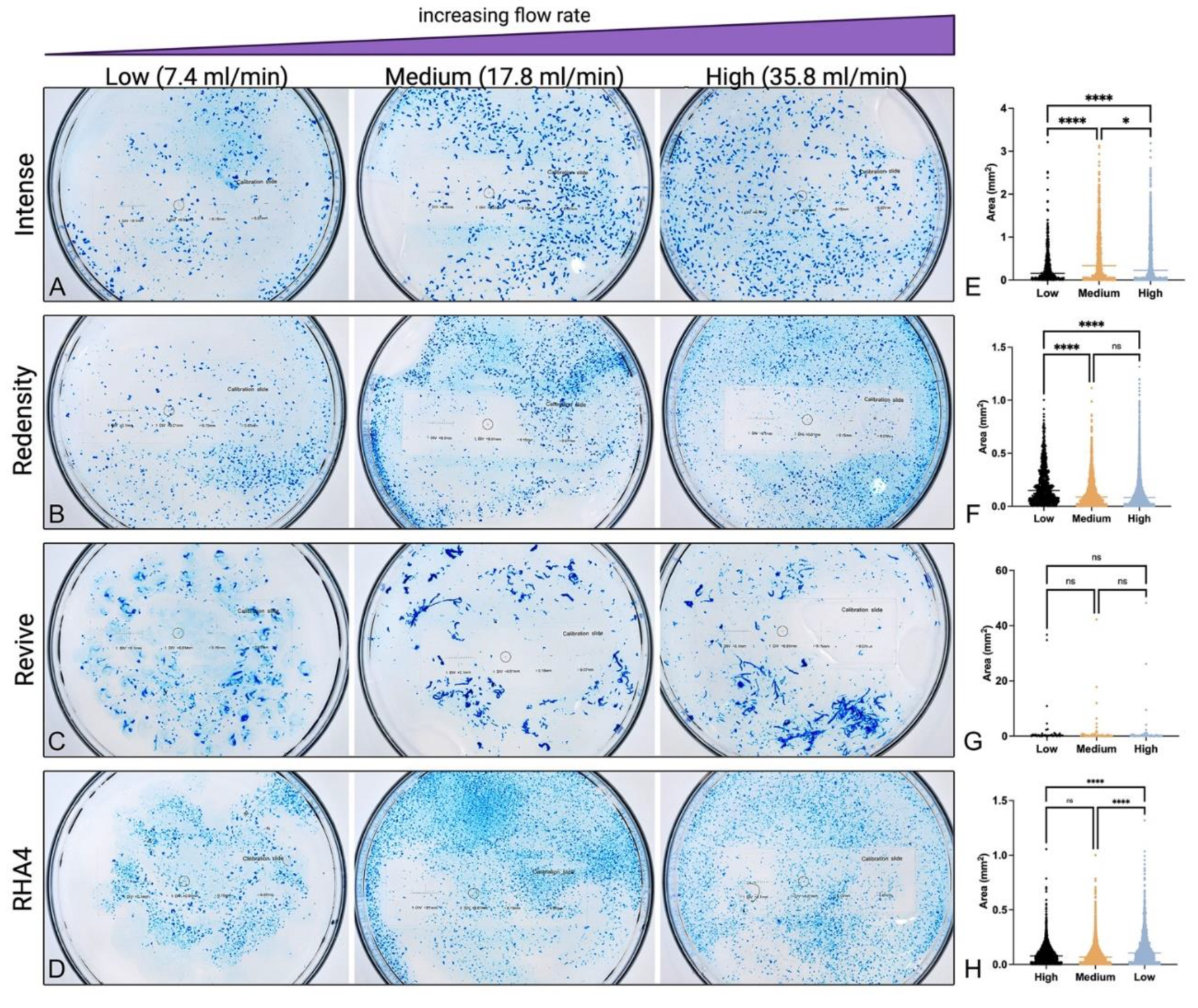
Figure 3.
Appearance and size distribution of embolic gel particles for each of the four tested products: (A-D) High resolution photographic images of embolized gel fragments in returning fluid collected immediately following system inoculation with Belotero Intense, RHA Redensity, Revive, and RHA4 filler products at low, medium, and high flow rates respectively. (E-H) Particle size distributions for each product at different flow rate settings.
Figure 3.
Appearance and size distribution of embolic gel particles for each of the four tested products: (A-D) High resolution photographic images of embolized gel fragments in returning fluid collected immediately following system inoculation with Belotero Intense, RHA Redensity, Revive, and RHA4 filler products at low, medium, and high flow rates respectively. (E-H) Particle size distributions for each product at different flow rate settings.
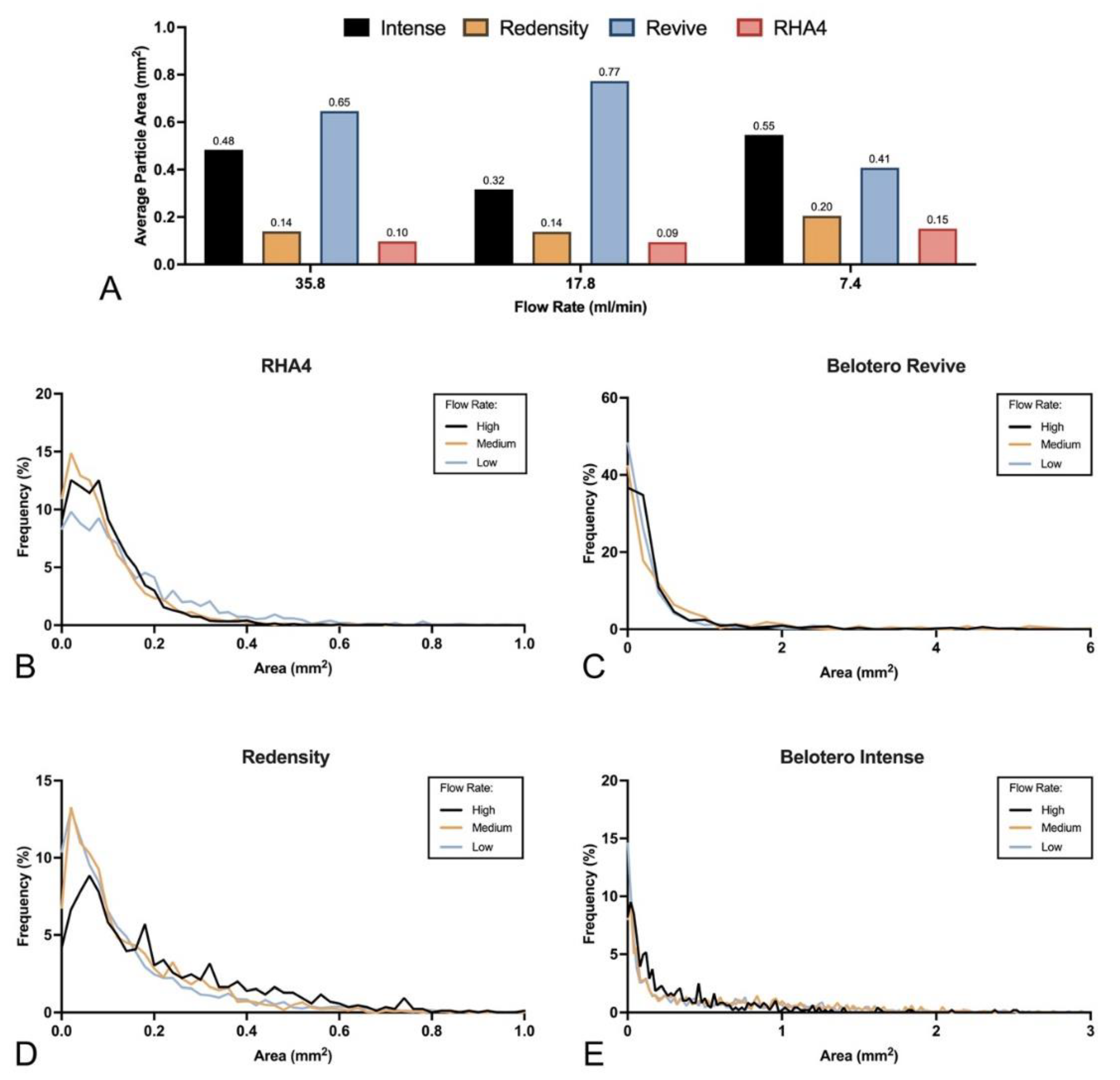
Figure 4.
Average size and distributions for all tested fillers at each flow rate: (A) Average particle size for each product at low, medium, and high flow rates. (B-E) Frequency distributions for gel particle sizes at low, medium, and high flow rates for RHA4, Belotero Revive, RHA Redensity, and Belotero Intense, respectively.
Figure 4.
Average size and distributions for all tested fillers at each flow rate: (A) Average particle size for each product at low, medium, and high flow rates. (B-E) Frequency distributions for gel particle sizes at low, medium, and high flow rates for RHA4, Belotero Revive, RHA Redensity, and Belotero Intense, respectively.
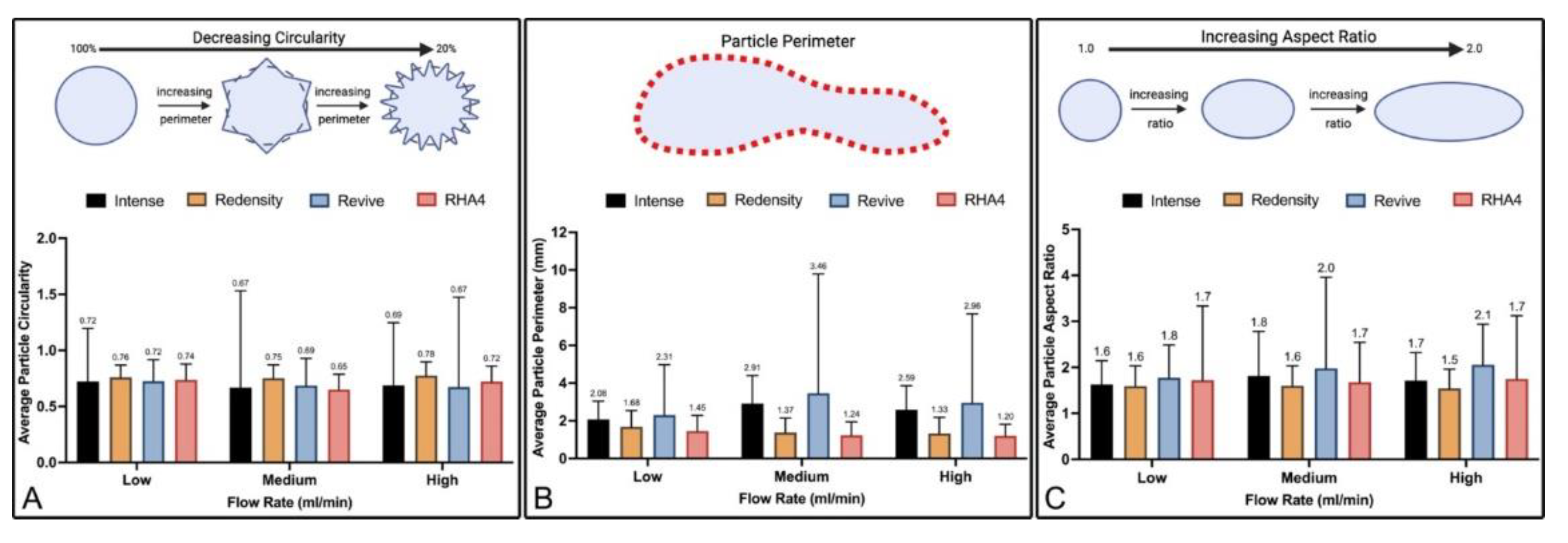
Figure 5.
Gel particle morphological analysis: (A-C) Summary plots of average particle circularity, perimeter, and aspect ratio, respectively, at low, medium, and high flow rates for all products.
Figure 5.
Gel particle morphological analysis: (A-C) Summary plots of average particle circularity, perimeter, and aspect ratio, respectively, at low, medium, and high flow rates for all products.
Figure 6.
HA gel physical and rheological properties and their correlations with average particle size at low, medium, and high flow rates: (A) Elastic modulus. (B) Loss modulus. (C) Tan(ẟ). (D) HA concentration and their correlation plots.
Figure 6.
HA gel physical and rheological properties and their correlations with average particle size at low, medium, and high flow rates: (A) Elastic modulus. (B) Loss modulus. (C) Tan(ẟ). (D) HA concentration and their correlation plots.
Figure 7.
Evaluation of the effect of flow rate on average HA gel particle fragment size: (A) Average particle size for all HA gel products at low, medium, and high flow rates. (B) Correlation of flow rates and average particle size for individual HA gel products.
Figure 7.
Evaluation of the effect of flow rate on average HA gel particle fragment size: (A) Average particle size for all HA gel products at low, medium, and high flow rates. (B) Correlation of flow rates and average particle size for individual HA gel products.
Figure 8.
Comparison of correlation coefficients between gel physical properties and flow rates on particle size: (A) Correlation coefficients between G’, G”, tan(ẟ), and HA concentration and average particle size at each flow rate. (B) Overall correlation coefficients with average particle size for all combined rates.
Figure 8.
Comparison of correlation coefficients between gel physical properties and flow rates on particle size: (A) Correlation coefficients between G’, G”, tan(ẟ), and HA concentration and average particle size at each flow rate. (B) Overall correlation coefficients with average particle size for all combined rates.
Figure 9.
Clearance time of embolic burden for each product at different flow rates.
Figure 9.
Clearance time of embolic burden for each product at different flow rates.
Figure 10.
Appearance of obstructive gel plugs and non-obstructive residue following inoculation for all products at low flow rate (7.4 ml/min): (A-D) Obstructive gel plugs for Belotero Intense, RHA4, RHA Redensity, and Belotero Revive, respectively, showing obstructive branch occlusion for Belotero Intense, RHA4, and Redensity and only non-obstructive residue for Belotero Revive.
Figure 10.
Appearance of obstructive gel plugs and non-obstructive residue following inoculation for all products at low flow rate (7.4 ml/min): (A-D) Obstructive gel plugs for Belotero Intense, RHA4, RHA Redensity, and Belotero Revive, respectively, showing obstructive branch occlusion for Belotero Intense, RHA4, and Redensity and only non-obstructive residue for Belotero Revive.
Figure 11.
Diagrammatic representation of vascular redundancy in tissues resulting from anastomotic connections between and within angiosomes. In human soft tissues, particularly the skin and skeletal muscle, the presence of anastomoses can provide adequate perfusion pressure to affected regions and offer bypass routes that circumvent embolic restrictions. Generally, redundancy is afforded through the presence of large-caliber true anastomoses (also known as direct anastomoses) and small-caliber, functional choke anastomoses (also known as indirect anastomoses). Direct anastomoses, such as those that exist between the ophthalmic and facial angiosomes can also provide a direct route for embolic dissemination of gel particles, potentially enabling the occurrence of retinal ischemic injuries arising from injections in the lower face. Reproduced. with permission from Soares [
1,[1,] 2022, MDPI.
Figure 11.
Diagrammatic representation of vascular redundancy in tissues resulting from anastomotic connections between and within angiosomes. In human soft tissues, particularly the skin and skeletal muscle, the presence of anastomoses can provide adequate perfusion pressure to affected regions and offer bypass routes that circumvent embolic restrictions. Generally, redundancy is afforded through the presence of large-caliber true anastomoses (also known as direct anastomoses) and small-caliber, functional choke anastomoses (also known as indirect anastomoses). Direct anastomoses, such as those that exist between the ophthalmic and facial angiosomes can also provide a direct route for embolic dissemination of gel particles, potentially enabling the occurrence of retinal ischemic injuries arising from injections in the lower face. Reproduced. with permission from Soares [
1,[1,] 2022, MDPI.
Figure 12.
The impact of rheological parameters on the cannulated extrusion and/or intravascular fragmentation of gel particles: (A) High tan(δ), low G’ gels, having greater pliability, can deform more easily in response to flow-related shear stresses during extrusion through needles/cannulas or dispersal within arterial conduits. The deformation behavior of these gels allows for streamlining of their shape, reducing exposure to shear stress and resulting in long filamentous fragments that fail/break in a ductile manner. (B) Low tan(δ), higher G’ gels, though stronger and better able to resist deformation and shear stresses, upon exposure to the sufficiently high shear stresses of needle extrusion or intra-arterial environments, are unable to deform to the same extent as softer, more pliable gels. As a result, these gels tend to fail in a more brittle manner, progressively fragmenting into smaller, non-filamentous particles.
Figure 12.
The impact of rheological parameters on the cannulated extrusion and/or intravascular fragmentation of gel particles: (A) High tan(δ), low G’ gels, having greater pliability, can deform more easily in response to flow-related shear stresses during extrusion through needles/cannulas or dispersal within arterial conduits. The deformation behavior of these gels allows for streamlining of their shape, reducing exposure to shear stress and resulting in long filamentous fragments that fail/break in a ductile manner. (B) Low tan(δ), higher G’ gels, though stronger and better able to resist deformation and shear stresses, upon exposure to the sufficiently high shear stresses of needle extrusion or intra-arterial environments, are unable to deform to the same extent as softer, more pliable gels. As a result, these gels tend to fail in a more brittle manner, progressively fragmenting into smaller, non-filamentous particles.
Figure 13.
The potential effects of microembolic, microvascular dissemination characteristics of a gel on the ischemic injury patterns of the skin: (A) The dissemination of gel microparticles, and their subsequent fragmentation, creates a semi-random distribution within microvascular networks that is influenced by the caliber of individual branches and their corresponding flow rates, as well as filler rheology, particle dimensions, and inoculation volume. Ultimately, the resulting obstructive pattern is characterized by a combination of patent and occluded proximal and distal branches, leading to a variegated distribution of skin ischemia with the percentage of patent branches decreasing with increasing inoculation volume. Adapted with permission from Soares [
1] 2022, MDPI. (B) Appearance of skin injury in a patient 3 days following HA gel injections into the nasal dorsum showing variegated dermal discoloration characteristic of intravascular embolization, with unaffected areas present within affected territories. Reproduced with permission from Salval et al. [
13] 2017, Springer Nature.
Figure 13.
The potential effects of microembolic, microvascular dissemination characteristics of a gel on the ischemic injury patterns of the skin: (A) The dissemination of gel microparticles, and their subsequent fragmentation, creates a semi-random distribution within microvascular networks that is influenced by the caliber of individual branches and their corresponding flow rates, as well as filler rheology, particle dimensions, and inoculation volume. Ultimately, the resulting obstructive pattern is characterized by a combination of patent and occluded proximal and distal branches, leading to a variegated distribution of skin ischemia with the percentage of patent branches decreasing with increasing inoculation volume. Adapted with permission from Soares [
1] 2022, MDPI. (B) Appearance of skin injury in a patient 3 days following HA gel injections into the nasal dorsum showing variegated dermal discoloration characteristic of intravascular embolization, with unaffected areas present within affected territories. Reproduced with permission from Salval et al. [
13] 2017, Springer Nature.
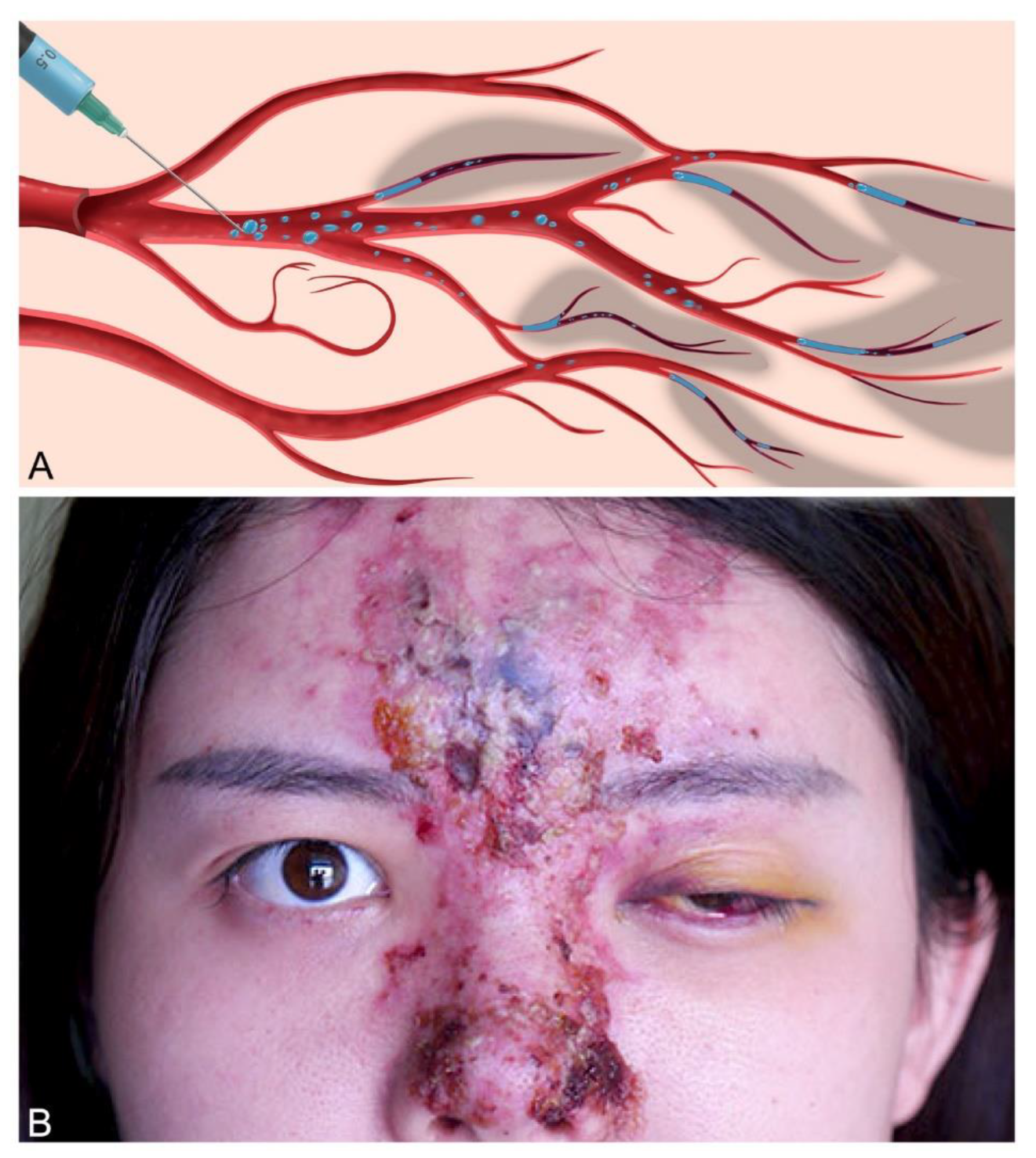
Figure 14.
Experimental Setup and Components of the Pulsatile Unit for the Simulation of Arterioembolic Restrictions (PULSAR) System: (A) The system is composed of a pulsatile pump attached to a 3D printed polydimethylsiloxane dichotomously-branched tubular network obeying Murray’s law of minimum work. The Distal portion of the circuit is designed for simulation of the paramandibular facial artery and its proximal branches, with a vessel diameter ranging from 2 mm down to 1 mm. The circulating fluid, composed of 50% glycerol and water by volume, is stored in the fluid housing and recirculated within the system at 20˚C. Four different ports allow access to the system for inoculation (port 1), circulating fluid collection (port 3), and blood pressure monitoring (ports 1-4). The videographic capture of gel embolization employs a high-resolution digital camera tracking the movement of dyed gel particles against an lighted background. Two different regulators (return flow and outflow regulators allow for blood pressure and flow adjustments, which are tracked through a monitoring device connected to a receiving computer. Particle size analysis evaluated the gel-inoculated fluid directly sampled from the port 3 collection tubing. (B-F) System components showing the pulsatile pump, 3D printed circuit, blood pressure monitoring device, distal circuit setup, and whole circuit setup, respectively. (G) Diagram of the tubular network showing the branch inner diameters.
Figure 14.
Experimental Setup and Components of the Pulsatile Unit for the Simulation of Arterioembolic Restrictions (PULSAR) System: (A) The system is composed of a pulsatile pump attached to a 3D printed polydimethylsiloxane dichotomously-branched tubular network obeying Murray’s law of minimum work. The Distal portion of the circuit is designed for simulation of the paramandibular facial artery and its proximal branches, with a vessel diameter ranging from 2 mm down to 1 mm. The circulating fluid, composed of 50% glycerol and water by volume, is stored in the fluid housing and recirculated within the system at 20˚C. Four different ports allow access to the system for inoculation (port 1), circulating fluid collection (port 3), and blood pressure monitoring (ports 1-4). The videographic capture of gel embolization employs a high-resolution digital camera tracking the movement of dyed gel particles against an lighted background. Two different regulators (return flow and outflow regulators allow for blood pressure and flow adjustments, which are tracked through a monitoring device connected to a receiving computer. Particle size analysis evaluated the gel-inoculated fluid directly sampled from the port 3 collection tubing. (B-F) System components showing the pulsatile pump, 3D printed circuit, blood pressure monitoring device, distal circuit setup, and whole circuit setup, respectively. (G) Diagram of the tubular network showing the branch inner diameters.
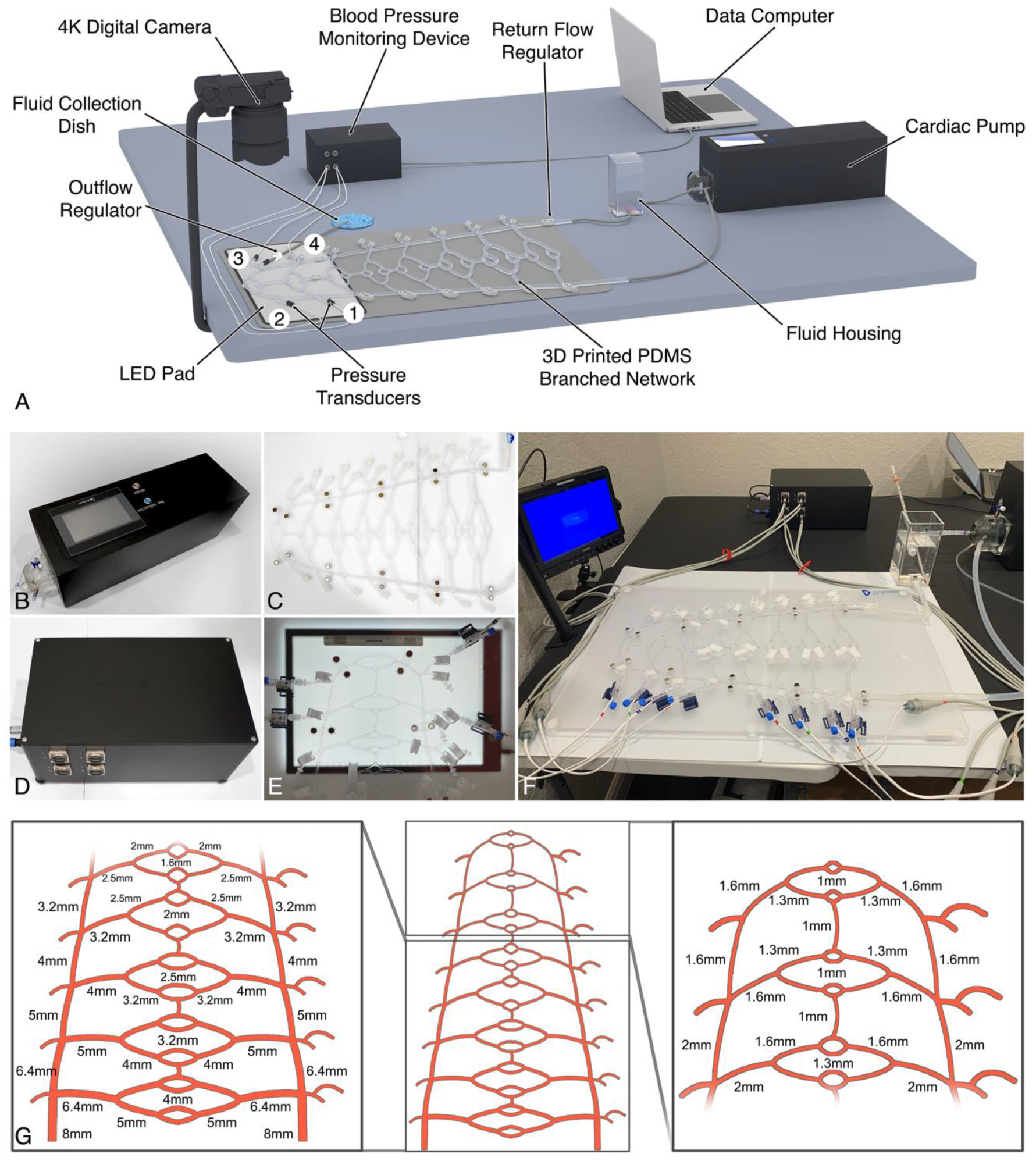
Figure 15.
Experimental setup for simulated proximal facial artery inoculation. (A) Diagrammatic illustration of the distal tubular network setup. Segments of the circuit are clamped off in order to isolate the distal circuit. Inoculation is performed through port 1 access and the circulating fluid containing the embolic particles is collected through port 3. (B) Photograph of the distal circuit containing dyed fluid for visualization of the experimental tubular diameters and setup, inoculation and connecting ports, and relevant clamps.
Figure 15.
Experimental setup for simulated proximal facial artery inoculation. (A) Diagrammatic illustration of the distal tubular network setup. Segments of the circuit are clamped off in order to isolate the distal circuit. Inoculation is performed through port 1 access and the circulating fluid containing the embolic particles is collected through port 3. (B) Photograph of the distal circuit containing dyed fluid for visualization of the experimental tubular diameters and setup, inoculation and connecting ports, and relevant clamps.
Figure 16.
Schematic showing the protocol used to characterize HA gel fragments following inoculation into the PULSAR system: (A) High resolution macroscopic and microscopic images of the HA gel fragments were taken for analysis in ImageJ. (B) Images underwent color channel deconvolution. (C) The red channel images were calibrated and particles were thresholded. (D) Particle analysis was conducted on color-isolated images.
Figure 16.
Schematic showing the protocol used to characterize HA gel fragments following inoculation into the PULSAR system: (A) High resolution macroscopic and microscopic images of the HA gel fragments were taken for analysis in ImageJ. (B) Images underwent color channel deconvolution. (C) The red channel images were calibrated and particles were thresholded. (D) Particle analysis was conducted on color-isolated images.
Table 1.
Post-calibration PULSAR settings at physiologically relevant facial artery settings.
Table 1.
Post-calibration PULSAR settings at physiologically relevant facial artery settings.
| Parameter |
Low Flow
(7.4 ml/min) |
Medium Flow
(17.6 ml/min) |
High Flow
(35.8 ml/min) |
| Heart Rate (beats/min) |
65 |
75 |
80 |
| Stroke Volume (ml/beat) |
2.8 |
3.5 |
4 |
| Cardiac Output (ml/min) |
182 |
262.5 |
320 |
| Average Systolic Pressure (mmHg) |
109.42 ± 1.04 |
107.96 ± 1.1 |
108.69 ± 1.49 |
| Average Diastolic Pressure (mmHg) |
91.76 ± 2.52 |
84.89 ± 4.39 |
86.2 ± 6.46 |
| Average Mean Arterial Pressure (mmHg) |
97.64 ± 2.52 |
92.58 ± 0.41 |
94.17 ± 1.37 |
Table 2.
Summary of gel fragment dimensions and shape.
Table 2.
Summary of gel fragment dimensions and shape.
| Product |
Flow Setting |
Area (mm2) |
Minor Axis (µm)
by Percentile |
Major Axis (µm)
by Percentile |
Perimeter (mm) |
Circularity
(0-1) |
Aspect Ratio |
| 25% |
50% |
75% |
100% |
25% |
50% |
75% |
100% |
Belotero
Intense
|
High |
0.48 ± 0.57 |
149 |
403 |
808 |
1528 |
220 |
659 |
1252 |
3556 |
2.59 ± 1.28 |
0.69 ± 0.56 |
1.71 ± 0.61 |
| Medium |
0.55 ± 0.59 |
216 |
516 |
751 |
1474 |
341 |
802 |
1382 |
3771 |
2.91 ± 1.49 |
0.67 ± 0.86 |
1.82 ± 0.97 |
| Low |
0.32 ± 0.41 |
129 |
279 |
523 |
1760 |
197 |
431 |
832 |
2669 |
2.08 ± 0.97 |
0.72 ± 0.47 |
1.63 ± 0.52 |
| RHA Redensity |
High |
0.14 ± 0.16 |
154 |
242 |
366 |
1034 |
235 |
375 |
557 |
1413 |
1.33 ± 0.86 |
0.78 ± 0.12 |
1.54 ± 0.42 |
| Medium |
0.14 ± 0.14 |
187 |
287 |
421 |
1120 |
286 |
445 |
656 |
1490 |
1.37 ± 0.78 |
0.75 ± 0.12 |
1.6 ± 0.43 |
| Low |
0.2 ± 0.18 |
212 |
383 |
555 |
1259 |
308 |
559 |
824 |
1569 |
1.68 ± 0.86 |
0.76 ± 0.11 |
1.59 ± 0.44 |
| Belotero Revive |
High |
0.65 ± 1.13 |
79 |
206 |
436 |
11354 |
105 |
345 |
784 |
17676 |
2.96 ± 4.71 |
0.67 ± 0.80 |
2.06 ± 0.88 |
| Medium |
0.77 ± 1.97 |
62 |
119 |
412 |
3867 |
90 |
145 |
655 |
14202 |
3.46 ± 6.33 |
0.69 ± 0.24 |
1.98 ± 1.98 |
| Low |
0.41 ± 0.81 |
63 |
190 |
501 |
4412 |
105 |
316 |
809 |
8573 |
2.31 ± 2.67 |
0.72 ± 0.19 |
1.77 ± 0.72 |
| RHA4 |
High |
0.10 ± 0.09 |
174 |
281 |
376 |
1059 |
271 |
444 |
606 |
1511 |
1.2 ± 0.62 |
0.72 ± 0.14 |
1.75 ± 1.37 |
| Medium |
0.09 ± 0.10 |
161 |
248 |
338 |
845 |
250 |
389 |
539 |
1327 |
1.24 ± 0.70 |
0.65 ± 0.14 |
1.68 ± 0.86 |
| Low |
0.15 ± 0.16 |
202 |
340 |
477 |
1285 |
290 |
518 |
717 |
1753 |
1.45 ± 0.83 |
0.74 ± 0.14 |
1.72 ± 1.62 |
Table 3.
Goodness-of-fit between gel fragment size, physical properties, and flow rate.
Table 3.
Goodness-of-fit between gel fragment size, physical properties, and flow rate.
| Property |
Flow Rate |
Average |
| High |
Medium |
Low |
| G' |
0.2928 |
0.4461 |
0.06997 |
0.2696233333 |
| G" |
0.01249 |
0.07421 |
0.3775 |
0.1547333333 |
| tan(δ) |
0.6641 |
0.9191 |
0.1688 |
0.584 |
| HA conc |
0.08515 |
0.00181 |
0.2689 |
0.11862 |
| Flow Rate |
- |
- |
- |
0.0007134 |
Table 4.
Physical properties of filler products employed in this study.
Table 4.
Physical properties of filler products employed in this study.
| Filler |
G' |
G" |
Tan(δ) |
HA concentration (mg/ml) |
| Belotero Intense |
166 |
64.6 |
0.39 |
25.5 |
| RHA Redensity |
59 |
26 |
0.44 |
15 |
| Belotero Revive |
15 |
18.5 |
1.27 |
20 |
| RHA4 |
263 |
31.6 |
0.12 |
23 |
Table 5.
Rheological measurements, symbols, descriptions, and physico-clinical correlates. Adapted from McCarthy & Soares et al. [
72].
Table 5.
Rheological measurements, symbols, descriptions, and physico-clinical correlates. Adapted from McCarthy & Soares et al. [
72].
| Measure |
Symbol |
Description |
Physico-clinical Correlate |
| Elastic (Storage) Modulus |
G' |
Solid-like parameter; ability to store energy through elastic deformation during shear straining. |
A higher G′ indicates a stiffer gel structure that can resist permanent deformation, with a greater ability to return to its initial shape. |
| Viscous (Loss) Modulus |
G" |
Fluid-like parameter; ability to dissipate energy through viscous flow during shear straining. |
A higher G′′ indicates a thicker gel that resists continuous flow, but with a greater tendency toward permanent deformation. |
| Phase Angle |
tan(δ) (G"/G') |
Viscoelastic character of a gel based on the ratio of the viscous to elastic partitions (alternatively, the tangent of phase angle δ). Colloids with tan δ > 1 are more viscous than elastic, behaving more like fluids. Colloids with tan δ < 1 are more elastic than viscous, behaving more like solids. |
Gels with low tan(δ) feel bouncier to the touch. In contrast, gels with a high tan(δ) feel more pliable or deformable. |
| Hyaluronic Acid Concentration (mg/ml) |
HA Conc. |
Concentration of hyaluronic acid within the gel |
Influences the overall gel properties such as gel strength, viscosity, and elasticity |