1. Introduction
A recent publication [
1] on COVID-19 coping [
2] considered extraversion as one of the Big Five [
3,
4] personality traits most socially relevant concerning positive COVID-19 coping [
5,
6,
7,
8,
9]. In a March 2023 Google Scholar search of “COVID-19 coping extraversion [number] wave”, fourteen individual countries were searched, as well as Europe as a whole (
Table 1). The results for Japan were unique. For most countries, research regarding extraversion and coping began during the first wave of COVID-19 [
10], and coping positively improved with subsequent COVID-19 waves [
11] and with the introduction of vaccines in December 2020 [
12]. The exceptions are Israel/Palestine and the United States—where the research on COVID-19 coping went from positive to neutral—and Norway, where public sentiment initially was positive and became negative [
1]. However, in no other country did a decrease in COVID-19 coping result because healthcare providers questioned vaccines after their introduction. In the other countries searched, vaccine introduction reduced the perceived threat of COVID-19 for healthcare providers [
13,
14]. For Japan, by wave five, with the vaccination program well underway, negative results were surprisingly recorded in research on healthcare providers [
1,
15].
This unanticipated result in association with the research on COVID-19 coping and extraversion for healthcare providers in Japan coincided with the particular introduction of vaccines in Japan—vaccines were introduced later in this country than in other countries because supply and bureaucratic problems created challenges with vaccine procurement and distribution [
16]. Yet, irrespective of these difficulties, during the initial introduction of vaccines in Japan in the fourth COVID-19 wave, there was no identification of vaccine hesitancy in healthcare providers [
15]. However, by the fifth wave of the pandemic, negative sentiment toward vaccines by those caring for COVID-19 patients focused scientific research in this area, with concerns about side effects from one vaccine (AstraZeneca) outweighing fears of infection [
15].
The following study aims to investigate the extent of this anomaly in Japanese healthcare providers regarding COVID-19 vaccine hesitancy through a scoping review of “Japan COVID-19 vaccine hesitancy” undertaken following PRISMA guidelines [
17]. The intent is to provide a more thorough assessment of this unusual research result regarding the negative reconsideration of vaccines by healthcare providers in Japan. In this regard, there are two research questions.
Q1 Did healthcare providers develop increasing vaccine hesitancy over subsequent COVID-19 pandemic waves?
Q2 If so, what was the reason?
2. Materials and Methods
The reported study of the effect of extraversion on COVID-19 coping conducted over up to five COVID-19 waves selected Google Scholar as the search engine [
1]. Arguing that, although there are inaccuracies, duplications, omissions, and misattributions in the publications returned in Google Scholar [
18], it was the most comprehensive academic search engine [
19,
20]. Furthermore, Google Scholar compares well with Scopus, with an estimated 12.6% duplicates to Google Scholar’s 10% [
20], and outperforms the coverage of either Web of Science or Scopus [
20]. However, Google Scholar was evaluated as unsuitable for primary review searches in 2020 [
20], considering it a supplementary source of evidence. For this reason, the decision is to exclude Google Scholar in this scoping review and to focus on a search of primary databases only.
There is no researched guidance on the number of databases to search for a scoping review other than to advise that at least one database should be searched [
21]. However, with the intent of providing the most extensive reach for this scoping review, the search is of six databases relevant to healthcare (Cochrane COVID-19 Study Register, ProQuest, PubMed, OVID, Scopus, and Web of Science)—databases, unlike Google Scholar, considered to return consistent results irrespective of the date of the search [
20].
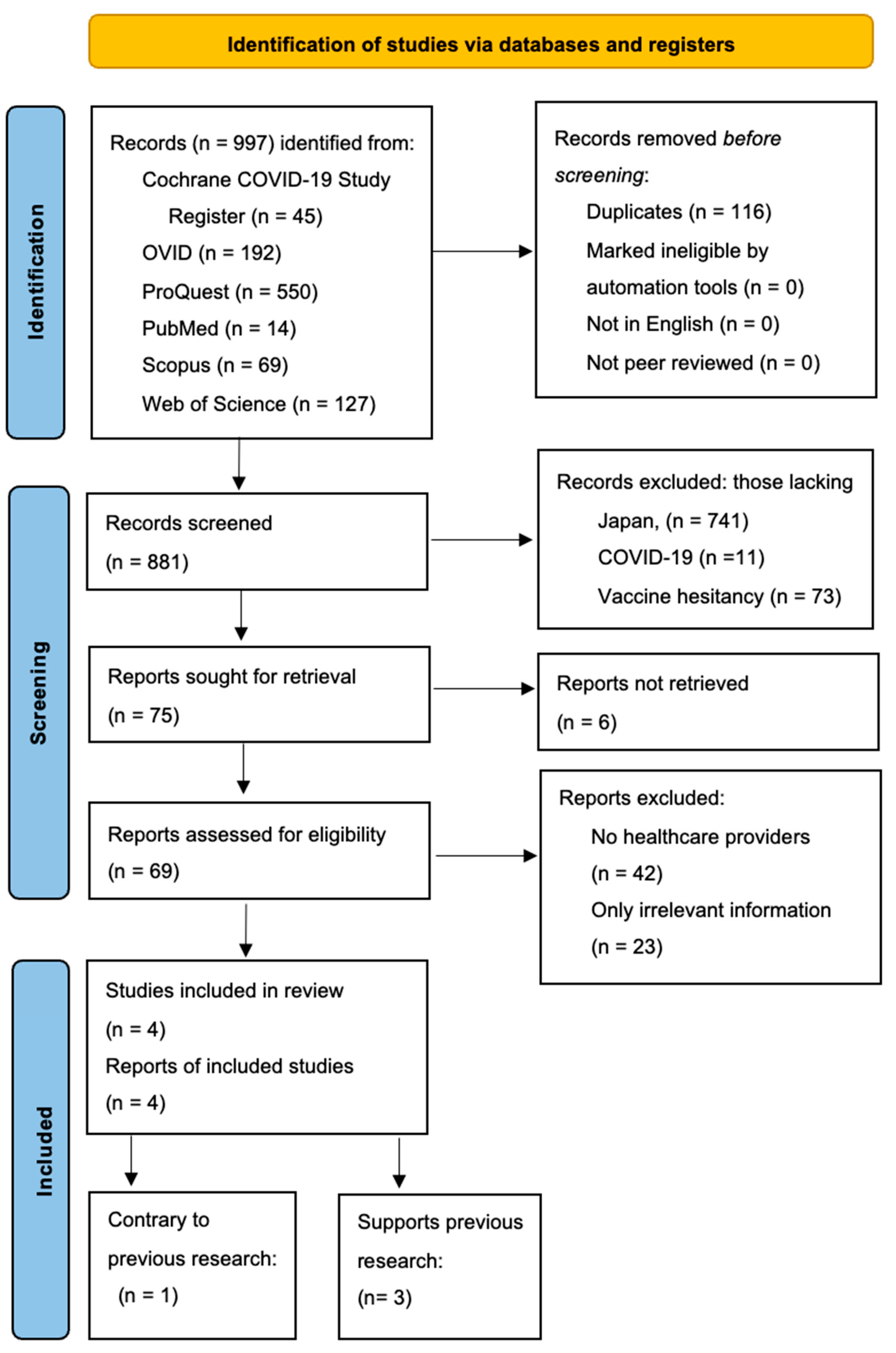
Developed is a PRISMA flow of information diagram specific to scoping reviews based on the most recent PRISMA template [
22]. Furthermore, included is the PRISMA Scoping Review Checklist in a supplementary file (
Table S1) outlining the process undertaken in this review. No registered review protocol exists for this scoping review.
As this scoping review concerns a COVID-19 investigation, the International Prospective Register of Systematic Reviews (PROSPERO) guidelines are relevant [
23]. Advisement for systematic review is when the research question addresses the feasibility, appropriateness, meaningfulness, or effectiveness of a treatment or practice [
24]. Systematic reviews usually require a meta-analysis when such data are amenable for analysis [
25]. As this study instead is intended to identify the extent of research available on a search of “COVID-19, Japan, vaccine hesitancy”, it is a scoping review rather than a systematic review [
24], and registration with PROSPERO is thus not permitted [
23].
“COVID-19, Japan, vaccine hesitancy” were the keywords searched for each database. There was no inclusion of more specific terms to limit the search to produce the most returns that might be relevant to this study. After the reports were screened for duplicates, whether they were marked ineligible by automation tools, not in English, or published in other than a peer-reviewed journal, a screening of the records then took place for inclusion of each of the keywords. Next, the reports were sought for retrieval, eliminating those unretrievable. An assessment of eligibility occurred for those remaining, excluding those reports that did not mention healthcare providers or, if they did, only irrelevant information regarding vaccine hesitancy. An example of irrelevancy is if an article mentions healthcare providers and vaccine hesitancy concerning patient vaccine hesitancy after consulting their healthcare provider. Lastly, of those studies included for review, the reports were classified into those supporting the research finding regarding the March 2023 search of Google Scholar and those that did not.
A compilation of the returns in individual documents is the method used to record the results for each database searched (see List S1—List S6). Once arranged alphabetically, an examination of the content of each list followed. Regarding each database on List S1—List S6, every aspect of the PRISMA process was noted for each search using a color-coded scheme. Most relevantly, green indicates an included article. A comment beside the article title recognizes duplication in another database search. If duplicated within the same database, the inclusion is only once; within another database, it is also included only once, with the preference for recording the article given to the database with more returns (Web of Science). The top of the first page of each of the six Lists provides the results.
A complete record of all returns before consideration of whether the articles returned were retrievable or contained healthcare providers was made, including the included returns of all databases and the relevant information from the article (see List S7). Again, color-coding differentiates those returns that do not mention healthcare providers. For this particular list, all included articles are colored black. Noted beside the title of the returned article is whether the returns were not retrievable.
A final list is only those returns that include healthcare providers (List S8). Without consideration of vaccine hesitancy, those articles that merely mention healthcare providers are colored red—they are excluded. The titles of those that presented information contrary to the review of Google Scholar conducted in March 2023 [
1] are colored blue. The titles of the articles that correspond to the results of the March 2023 [
1] search are colored green.
The charting was done independently by the author.
3. Results
Figure 1 represents the results of the PRISMA search process.
Two subsections divide the results. The first corresponds to the various searches undertaken, providing commentary on conducting these types of searches. The second regards the articles returned that met all the criteria for inclusion.
3.1. Searches
The databases selected to search are those relevant to healthcare considered well-suited to meeting PRISMA guidelines—they are found suitable for their coverage and high precision of the search query, including their reproducibility of search results [
26]. Consequently, it is relevant to consider whether the results from the searches performed substantiate this view of their suitability as search engines. The investigation will regard the number and type of returns for the searches of each database (see
Table 1).
The Cochrane COVID-19 Study Register is a database of only COVID-19-related publications. In this regard, it should produce the most relevant and unique returns. However, of the 45 returns (see List S1), 42 were duplicates—all of them, except for two, in Web of Science. The two not duplicated in Web of Science were duplicated in ProQuest. Most of the results also returned in the Scopus search as well. Four of those that are duplicates appear on the final List S8. Only three articles were not duplicates, and two were unretrievable. The one retrievable contained irrelevant information regarding the search criteria. Thus, a register that should have provided all the relevant articles regarding this search produced only half the final number. Although there were no returns unique to this search that were relevant to this investigation—of the duplicated returns—two are part of the relevant articles on the final list (see List S8).
The OVID search was unusual. The initial search of the three keywords resulted in no returns. To improve the possibility of producing returns, “vaccine hesitancy” was removed from the search (also limited to English language and human) (see List S2). This modified search produced 192 results. Surprisingly, Japan was not part of 187 of these returns, although it was one of the two keywords. Four returns were duplicates (ultimately, ones not part of the final list), and the remaining report did not include healthcare providers. The results were that none of the returns of this modified search produced any relevant studies.
The ProQuest search offered the most returns at 550 (see List S3). Nevertheless, primarily, this was because the search engine retained articles that did not include Japan—remaining true even after modification to the parameter included the following limitations: not Malaysia, not India, not Thailand, not Italy, not China, not Hong Kong. These additional limitations still produced the same number of returns with the same articles from Malaysia, India, Thailand, Italy, China, and Hong Kong (among studies of other countries). The search was on 10 July. The date should not be relevant, as the returns for a primary database should be the same on any date (unless there is a new publication). However, with the same parameters for the search, on 11 July, the number of returns ballooned to 778, while a search on 12 July reduced the returns to 700. The author analyzed the returns from 10 July, as the increase in the returns over subsequent days was unlikely relevant material. Of the 550 returns, 520 did not mention Japan. There were 11 duplicates with either Scopus or Web of Science (or both). Unlike the Cochrane COVID-19 Study Register or the OVID searches, some returns did not include COVID-19 (1) or vaccine hesitancy (10). Of the eight that remained, seven didn’t include healthcare providers, and of the one that did, it was irrelevant information. The final result was that, of this vast number of returns, there were no articles relevant to the considerations of this study.
Apart from OVID, PubMed produced the smallest number of returns at fourteen. Of these, nine were missing Japan (see List S4). There were four duplicates and one not including vaccine hesitancy, resulting in no returns relevant to this investigation. Of the four duplicates, none became part of the final list (see List S8).
For the Scopus search, there were 69 returns (see List S5). There were 55 duplicates; 54 were with Web of Science and one with ProQuest. Like ProQuest, there were returns with no COVID-19 (4) or no vaccine hesitancy (9). The remaining unique return contained irrelevant information. Regarding the final list, List S8, two reports relevant for consideration from the Web of Science were those in Scopus—the same publications duplicated in the Cochrane COVID-19 Study Register.
The Web of Science return (see List S6) represents the reference for the duplicated returns, providing the reason the list includes no duplicates. There were 127 returns. Web of Science was the only database for which exclusions are under every category: no Japan (25), no COVID-19 (6), no vaccine hesitancy (34), not retrieved (4), no healthcare providers (34), and irrelevant information (19). Three studies eliminated were irrelevant because they tested vaccine hesitancy in healthcare providers at only one time point [
27,
28,
29]. However, that it is the only database producing exclusions in each category is a result of eliminating duplicates before all other considerations. Other searches would have produced exclusions in additional categories had this not been the process. The duplicate elimination process follows the PRISMA flow of information chart method [
22].
3.2. Relevant Returns
Table 2 lists the relevant returns with their citation numbers and provides a breakdown of the search engines that produced them. There are four relevant articles. Web of Science returned all four. Cochrane COVID-19 Study Register and Scopus returned two.
An interesting point regarding the two articles returned by the Cochrane COVID-19 Study Register and Scopus is that they are the same. Furthermore, these search engines returned only articles supporting earlier research that Japanese healthcare providers developed increasing vaccine hesitancy over subsequent pandemic waves. Web of Science was the sole search engine that returned an article contrary to this previous research.
Table 3 identifies that all the articles were published either in 2021 or 2022, and there was no assessment of vaccine hesitancy in Japanese healthcare providers returned regarding a more recent date. Considering those publications that supported the understanding of Japanese healthcare providers becoming increasingly hesitant about COVID-19 vaccines over subsequent waves, it is evident that these publications were in journals devoted to vaccines. The one return that provided information contrary to the view that Japanese healthcare providers became increasingly hesitant over subsequent pandemic waves concerning COVID-19 vaccines was a medical journal.
The content of
Table 4 includes each of the citation numbers of the relevant articles returned plus a sample of the type of information published that identifies the article was either supportive or not of the March 2023 returns of the Google Scholar search concerning whether healthcare providers developed increasing vaccine hesitancy over successive COVID-19 waves.
3.3. Results of the Four Articles
Association of Vaccine Confidence and Hesitancy in Three Phases of COVID-19 Vaccine Approval and Introduction in Japan [
30] is one of the three returned articles published in the MDPI journal
Vaccines. It represents the most relevant article of all the returns and was returned by three different databases (Cochrane COVID-19 Study Register, Scopus, and Web of Science), investigating the vaccine hesitancy of Japanese healthcare providers over three periods. This research is a study of healthcare providers undertaken as part of a more comprehensive study of the views of Japanese citizens. In this investigation of 7000 citizens, healthcare providers represented 808 (11.2%) of those studied at T1, 824 (11.4%) at T2, and 830 (11.5%) at T3. The three separate interviews were in January 2021, before vaccine approval; in June, the start of elderly vaccination; and in September, with vaccination of approximately 70% of the target population with at least one dose, when vaccine hesitancy for the total population was 17.5%, 65.3%, and 19.4%, respectively. Thus, for the total population, vaccine hesitancy continued and peaked in June. From this perspective, the vaccine hesitancy of healthcare providers, although following the same trend of a higher percentage of vaccine hesitancy in June, was comparatively low at 17.1%, 18.9%, and 5.4% in these three intervals. This trend reveals that in January, before vaccine approval, healthcare providers had almost the same vaccine hesitancy as the larger population. However, in June, when vaccine hesitancy by the general population escalated, the vaccine hesitancy of healthcare providers was kept down, with only a slight rise from the January results. What is especially notable is that there was an elimination of almost all vaccine hesitancy in healthcare providers by September, when vaccine hesitancy by the general population was higher than before vaccines were approved.
Attitudes of Medical Students toward COVID-19 Vaccination: Who Is Willing to Receive a Third Dose of the Vaccine? [
31], represents the second article noting an increase in vaccine hesitancy of healthcare providers published in
Vaccines. It was returned only by Web of Science. Published on 8 November 2021, the time from submission of this manuscript to its publication is only one month, perhaps because it is the earliest of the studies on vaccine hesitancy in healthcare providers returned. Unlike the previous article in
Vaccines, this study did not test Japanese medical students at different periods. Making this study still relevant is that the research asked medical students who had received the second dose of the vaccine whether they would be willing to receive the third dose. Among all the participants, 89.1% (442/496) received the second dose of the vaccine, and 84.5% (419/496) of the participants were willing to receive a third dose. Although this was a hypothetical response, it is clear that fewer medical students were willing to receive the third dose than had received the second dose. Although most of the students (75.6%; 375/496) agreed that the vaccines provide a high degree of protection against COVID-19, 67.3% (334/496) were concerned about the sustainability of immunity by the vaccine. Furthermore, a nonnegligible number of medical students (46.0%; 228/496) stated that the vaccine development was too rapid.
COVID-19 Vaccine hesitance and vaccine passports: a cross-sectional conjoint experiment in Japan [
32] is the only article returned that did not find an increase in vaccine hesitancy among healthcare providers. Returned solely by Web of Science, this article is also unique to those returned in being published in a medical journal
, BMJ Open, rather than one devoted to vaccines. Of all the returns, this article took the longest to be accepted. The submission is on 6 January 2022, and the acceptance is on 1 June 2022. Healthcare providers were among the sample of 5000 Japanese adults for this study. Healthcare providers represented 6.4% of those studied or 320 participants. The first part of this study of 5000 occurred from 21 July 2021 to 23 July 2021; the follow-up study was between 10 November 2021 and 20 November 2021, including 4367, or 87.3% of those participating in the original investigation. Unfortunately, the authors do not provide a breakdown of the percentage of healthcare providers who participated in the second part of the study; they add healthcare providers with essential workers without providing the change in vaccine hesitancy but generally claim they are less likely to be vaccine-hesitant. The article indicates that when healthcare providers are vaccine-hesitant, the factors are side effects, safety, and vaccine mistrust. Without the article’s specific focus on healthcare providers in the second period, it is difficult to compare this publication that did not find an increase in vaccine hesitancy with the subsequent pandemic wave with the others that did.
Differences in COVID-19 Vaccine Acceptance, Hesitancy, and Confidence between Healthcare Workers and the General Population in Japan [
33] is the third article published in
Vaccines. It was received by the journal on 22 October 2021, revised on 12 November 2021, accepted on 18 November 2021, and published on 24 November 2021, meaning that the revisions requested were likely minor and the reviewers were sufficiently engaged with the contents of the article to review its first version and its revision quickly. Among a more extensive investigation of vaccine hesitancy in the Japanese population, this study looked at vaccine hesitancy in healthcare providers. The problem with this study regarding the current investigation is the two periods selected for comparison. The first period was pre-COVID-19—when Japan had one of the lowest vaccine acceptance rates in the world [
34]. The authors differentiated healthcare providers from the general population based on these results, including physicians, nurses, pharmacists, and physical and occupational therapists, as part of their study among the 755 healthcare providers (medical clerks make up the additional 275 participants in the total of 1030 healthcare workers). The results of vaccine hesitancy follow—general population, 17.5%; doctors, 11.7%; nurses, 18.5%; pharmacists, 17.1%; physical/occupational therapists, 13.8%. Female sex, younger age, being a nurse, influenza vaccine hesitancy, and concern about the frequency of adverse events were positively associated with vaccine hesitancy in the study. Although this study did investigate vaccine hesitancy at two points, the first was pre-COVID-19, and the second was before the vaccine was available; therefore, the usefulness of these results for this current study is limited.
4. Discussion
This study is in response to a previous Google Scholar search during March 2023 that identified Japan as unique in its healthcare providers developing increased COVID-19 vaccine hesitancy in subsequent waves of the pandemic. The purpose was to determine if this held in other studies from a search of “COVID-19, Japan, vaccine hesitancy”, and, if so, why this might be the case. The original research had identified healthcare providers as developing increased vaccine hesitancy between wave four and wave five [
15]. Further research in [
1] speculated that the reason for this vaccine hesitancy in Japan might be the negative sentiment of the general public toward vaccines that dominated, with concerns about side effects from AstraZeneca in particular outweighing fears of infection [
35]. For this reason, the consideration was that a fuller investigation of vaccine hesitancy in Japanese healthcare providers was warranted.
After an extensive search of six relevant databases, there was a return of 997 articles. In following the PRISMA guidelines, only four articles remained from these returns. Three of these articles supported the view that over subsequent waves, healthcare providers developed increasing vaccine hesitancy [
30,
31,
33]. Publication of each of these articles is in
Vaccines. The one article presenting a contrary assessment [
32] is in the medical journal
BMJ Open. Yet, those articles that supported the view that healthcare providers grew increasingly vaccine hesitant did not undertake to study their vaccine hesitancy—the information can be identified by looking through each article for the necessary result—the consequence is that the information lacks clarity. Only the first paper [
30] specifies that between January (before the introduction of vaccines in Japan) and June, there was an increase in vaccine hesitancy in healthcare providers—but the increase was a slight 1.8%. The vaccine hesitancy of the second supporting paper [
31] was purely hypothetical regarding whether medical students would be inclined to get a third dose of the vaccine after receiving the second. The final paper that supports healthcare providers became increasingly vaccine hesitant [
33], although it tests for two different times regarding vaccine hesitancy, one of these times is before COVID-19. Thus, its report of increased vaccine hesitancy for this study becomes irrelevant. The weakness of one paper that presented contrary information on vaccine hesitancy in healthcare providers [
32] is that it provides incomplete results regarding the second testing time of healthcare providers. This study reported on many variables over the two time periods, with healthcare providers being only one. The authors of this study chose to provide less information concerning the vaccine hesitancy of healthcare providers; therefore, the ability to determine why this research did not find the same trend as others is unknown.
The study limitations primarily pertain to the lack of information in answering the research questions confidently. A partial answer responds to the first research question—three studies recognize an increase in vaccine hesitancy in healthcare providers over subsequent waves; however, the data are not convincing for the reasons provided. The studies investigated did not provide the reason because it was uninvestigated—answering the second research question. Furthermore, studies regarding general vaccine hesitancy in Japan are in contradiction. The research in [
30] resulted from a pre-COVID-19 survey of over 280,000 people in 149 countries and regions—it found Japan with one of the lowest rates of vaccine confidence. Yet, another of the returns from the Web of Science—excluded from consideration as not meeting all the study criteria states the opposite—found worldwide that Japan has one of the highest public acceptance rates for the COVID-19 vaccine [
36]. The Japanese problem with the AstraZeneca vaccine noted in [
15] is not part of any other publication. The suggestion is that this vaccine hesitancy followed the 2013 collapse of the human papillomavirus (HPV) immunization program in Japan, resulting from frequent false-positive reports that created the perception that HPV vaccinations were unsafe, showing how negative publicity and government hesitancy later made professional judgment conflicted, contributing to vaccine hesitancy among medical professionals specific to COVID-19 [
37].
In considering future research in this area, the time has now passed to research the vaccine hesitancy among healthcare providers in subsequent waves of COVID-19. Some research found that the healthcare providers of Japan behaved differently than in other countries—there was reason at that time to investigate this further, work undone. Consequently, there was a missed research opportunity. However, in considering the results of the searches performed, future research can investigate the suitability of various databases as primary. One of the reasons Google Scholar is not considered a primary database is that returns are inconsistent [
20]. With consistency as a criterion, reconsideration should be given to ProQuest as a primary database, resulting from the return of 550 articles one day, 778 the next, and 700 on the third for this study. What is also relevant concerning the health-related databases—OVID and PubMed—is that neither was appropriate for investigating vaccine hesitancy among healthcare providers. Only the science databases were valuable in this regard. The Cochrane COVID-19 Study Register, Scopus, and Web of Science returns were similar in most respects. However, there were some differences. Future research can investigate the considerations that permit these databases to return similar results and what aspects produce differences in their returns.
5. Conclusions
The research questions of this study are two. Did Japanese healthcare providers develop increasing vaccine hesitancy over subsequent COVID-19 pandemic waves? If so, what was the reason? The scoping review of six relevant databases produced 997 returns, with only four included. Of those four, three supported that Japanese healthcare providers developed increasing vaccine hesitancy. However, this development was slight, and the data were insufficiently robust for a conclusive assessment. An inability to usefully assess the results also hampered the one article that provided a contrary point of view. None of the articles included considered the reason for vaccine hesitancy among healthcare providers. Yet there is conjecture from another study that the reason for any vaccine hesitancy among this group resulted from the poor outcome of the HPV vaccination program that failed in Japan in 2013. The speculation is that false positives produced by the COVID-19 vaccines were similar to those of 2013, and this may be the reason, if there is any, for the increase in vaccine hesitancy in healthcare providers over subsequent waves of COVID-19. This study highlights the necessity of timely research when unexpected anomalies occur regarding COVID-19 and the value of ensuring databases are appropriate and reliable.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Table S1: Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) Checklist, List 1—List 6: The lists of returns from the six databases searches, List 7: The complete list of returns because exclusion for being unretrievable or lacking healthcare providers, and List 8: The list of reports containing healthcare providers.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created.
Conflicts of Interest
The author declares no conflicts of interest.
References
- Nash, C. Extraversion in COVID-19 Coping and Actionable Insights from Considering Self-Directed Learning. COVID 2023, 3, 831–858. [Google Scholar] [CrossRef]
- Kar, N.; Kar, B.; Kar, S. Stress and Coping during COVID-19 Pandemic: Result of an Online Survey. Psychiatry Research 2021, 295, 113598. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.A. Big-Five Model. In Encyclopedia of Personality and Individual Differences; Zeigler-Hill, V., Shackelford, T.K., Eds.; Springer International Publishing: Cham, 2017; pp. 1–16; ISBN 978-3-319-28099-8. [Google Scholar]
- Anglim, J.; Horwood, S.; Smillie, L.D.; Marrero, R.J.; Wood, J.K. Predicting Psychological and Subjective Well-Being from Personality: A Meta-Analysis. Psychological Bulletin 2020, 146, 279–323. [Google Scholar] [CrossRef] [PubMed]
- Gashi, D.; Gallopeni, F.; Imeri, G.; Shahini, M.; Bahtiri, S. The Relationship between Big Five Personality Traits, Coping Strategies, and Emotional Problems through the COVID-19 Pandemic. Curr Psychol 2023, 42, 29179–29188. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Havewala, M.; Zhu, Q. COVID-19 Stressful Life Events and Mental Health: Personality and Coping Styles as Moderators. Journal of American College Health 2024, 72, 1068–1077. [Google Scholar] [CrossRef] [PubMed]
- Xie, C.-S.; Kim, Y. Post-Traumatic Growth during COVID-19: The Role of Perceived Social Support, Personality, and Coping Strategies. Healthcare 2022, 10, 224. [Google Scholar] [CrossRef] [PubMed]
- Nikčević, A.V.; Marino, C.; Kolubinski, D.C.; Leach, D.; Spada, M.M. Modelling the Contribution of the Big Five Personality Traits, Health Anxiety, and COVID-19 Psychological Distress to Generalised Anxiety and Depressive Symptoms during the COVID-19 Pandemic. Journal of Affective Disorders 2021, 279, 578–584. [Google Scholar] [CrossRef]
- Gibbons, C. Understanding the Role of Stress, Personality and Coping on Learning Motivation and Mental Health in University Students during a Pandemic. BMC Psychol 2022, 10, 261. [Google Scholar] [CrossRef]
- Pilch, I.; Wardawy, P.; Probierz, E. The Predictors of Adaptive and Maladaptive Coping Behavior during the COVID-19 Pandemic: The Protection Motivation Theory and the Big Five Personality Traits. PLoS ONE 2021, 16, e0258606. [Google Scholar] [CrossRef]
- Rogowska, A.; Kuśnierz, C.; Ochnik, D. Changes in Stress, Coping Styles, and Life Satisfaction between the First and Second Waves of the COVID-19 Pandemic: A Longitudinal Cross-Lagged Study in a Sample of University Students. JCM 2021, 10, 4025. [Google Scholar] [CrossRef]
- Lamb, Y.N. BNT162b2 mRNA COVID-19 Vaccine: First Approval. Drugs 2021, 81, 495–501. [Google Scholar] [CrossRef]
- Tavilani, A.; Abbasi, E.; Kian Ara, F.; Darini, A.; Asefy, Z. COVID-19 Vaccines: Current Evidence and Considerations. Metabolism Open 2021, 12, 100124. [Google Scholar] [CrossRef] [PubMed]
- Koltai, J.; Raifman, J.; Bor, J.; McKee, M.; Stuckler, D. COVID-19 Vaccination and Mental Health: A Difference-In-Difference Analysis of the Understanding America Study. American Journal of Preventive Medicine 2022, 62, 679–687. [Google Scholar] [CrossRef]
- Odachi, R.; Takahashi, S.; Sugawara, D.; Tabata, M.; Kajiwara, T.; Hironishi, M.; Buyo, M. The Big Five Personality Traits and the Fear of COVID-19 in Predicting Depression and Anxiety among Japanese Nurses Caring for COVID-19 Patients: A Cross-Sectional Study in Wakayama Prefecture. PLoS ONE 2022, 17, e0276803. [Google Scholar] [CrossRef]
- Lipscy, P.Y. Japan’s Response to the COVID-19 Pandemic. In Japan Decides 2021; Pekkanen, R.J., Reed, S.R., Smith, D.M., Eds.; Springer International Publishing: Cham, 2023; pp. 239–254; ISBN 978-3-031-11323-9. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Journal of Clinical Epidemiology 2009, 62, 1006–1012. [Google Scholar] [CrossRef] [PubMed]
- Healey, M.; Healey, R.L. Searching the Literature on Scholarship of Teaching and Learning (SoTL): An Academic Literacies Perspective: Part 1. TLI 2023, 11. [Google Scholar] [CrossRef]
- Gusenbauer, M. Google Scholar to Overshadow Them All? Comparing the Sizes of 12 Academic Search Engines and Bibliographic Databases. Scientometrics 2019, 118, 177–214. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated Methodological Guidance for the Conduct of Scoping Reviews. JBI Evidence Synthesis 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, n71. [Google Scholar] [CrossRef]
- National Institute for Health and Care Research International Prospective Register of Systematic Reviews. PROSPERO 2020.
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic Review or Scoping Review? Guidance for Authors When Choosing between a Systematic or Scoping Review Approach. BMC Med Res Methodol 2018, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without Meta-Analysis (SWiM) in Systematic Reviews: Reporting Guideline. BMJ 2020, l6890. [Google Scholar] [CrossRef] [PubMed]
- Gusenbauer, M.; Haddaway, N.R. Which Academic Search Systems Are Suitable for Systematic Reviews or Meta-analyses? Evaluating Retrieval Qualities of Google Scholar, PubMed, and 26 Other Resources. Research Synthesis Methods 2020, 11, 181–217. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, N.; Yamamoto, T.; Uchiumi, C.; Sugaya, N. Socio-Economic and Behavioral Characteristics Associated with COVID-19 Vaccine Hesitancy under a Declared State of Emergency in Japan. Brain, Behavior, & Immunity - Health 2022, 22, 100448. [Google Scholar] [CrossRef]
- Takahashi, S.; Takahashi, N.; Sasaki, S.; Nohara, M.; Kawachi, I. Occupational Disparities in COVID-19 Vaccine Hesitancy in Japan. SSM - Population Health 2022, 19, 101226. [Google Scholar] [CrossRef]
- Ghaznavi, C.; Yoneoka, D.; Kawashima, T.; Eguchi, A.; Murakami, M.; Gilmour, S.; Kaneko, S.; Kunishima, H.; Naito, W.; Sakamoto, H.; et al. Factors Associated with Reversals of COVID-19 Vaccination Willingness: Results from Two Longitudinal, National Surveys in Japan 2021-2022. The Lancet Regional Health - Western Pacific 2022, 27, 100540. [Google Scholar] [CrossRef]
- Tokiya, M.; Hara, M.; Matsumoto, A.; Ashenagar, M.S.; Nakano, T.; Hirota, Y. Association of Vaccine Confidence and Hesitancy in Three Phases of COVID-19 Vaccine Approval and Introduction in Japan. Vaccines 2022, 10, 423. [Google Scholar] [CrossRef] [PubMed]
- Sugawara, N.; Yasui-Furukori, N.; Fukushima, A.; Shimoda, K. Attitudes of Medical Students toward COVID-19 Vaccination: Who Is Willing to Receive a Third Dose of the Vaccine? Vaccines 2021, 9, 1295. [Google Scholar] [CrossRef]
- Okamoto, S.; Kamimura, K.; Komamura, K. COVID-19 Vaccine Hesitancy and Vaccine Passports: A Cross-Sectional Conjoint Experiment in Japan. BMJ Open 2022, 12, e060829. [Google Scholar] [CrossRef]
- Hara, M.; Ishibashi, M.; Nakane, A.; Nakano, T.; Hirota, Y. Differences in COVID-19 Vaccine Acceptance, Hesitancy, and Confidence between Healthcare Workers and the General Population in Japan. Vaccines 2021, 9, 1389. [Google Scholar] [CrossRef] [PubMed]
- De Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping Global Trends in Vaccine Confidence and Investigating Barriers to Vaccine Uptake: A Large-Scale Retrospective Temporal Modelling Study. The Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef] [PubMed]
- Niu, Q.; Liu, J.; Kato, M.; Shinohara, Y.; Matsumura, N.; Aoyama, T.; Nagai-Tanima, M. Public Opinion and Sentiment Before and at the Beginning of COVID-19 Vaccinations in Japan: Twitter Analysis. JMIR Infodemiology 2022, 2, e32335. [Google Scholar] [CrossRef] [PubMed]
- Takamatsu, A.; Honda, H.; Miwa, T.; Tabuchi, T.; Taniguchi, K.; Shibuya, K.; Tokuda, Y. Factors Associated with COVID-19 Booster Vaccine Hesitancy: A Nationwide, Cross-Sectional Survey in Japan. Public Health 2023, 223, 72–79. [Google Scholar] [CrossRef]
- Inokuma, Y.; Kneller, R. Imprecision in Adverse Event Reports Following Immunization against HPV in Japan and COVID-19 in the USA, UK, and Japan—and the Effects of Vaccine Hesitancy and Government Policy. Eur J Clin Pharmacol 2023, 79, 269–278. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).