1. Introduction
Since its inception in the 1970s, computed tomography (CT) has been a valuable tool in diagnosing diseases, revolutionizing medicine. Its role becomes particularly crucial in emergency cases [
1,
2]. Consequently, the utilization of CT in emergency departments has shown a rise over the years [
3].
Polytrauma is a common presentation in the emergency department, often resulting from severe accidents. Polytrauma is defined as a condition involving multiple traumatic injuries that could result in systemic effects and potentially lead to life-threatening complications. This includes damage to at least two body regions or organ systems [
4]. Whole-body CT scans, also known as panCT and polytrauma CT, have been the gold standard in the management of poly-traumatic patients. PanCT is a comprehensive CT scan that covers multiple body regions and significantly improves the chances of survival [
5]. Accordingly, there has been a growing trend in the utilization of panCT in emergency departments [
6].
The increasing reliance on panCT examinations in emergency departments is a pressing concern that warrants immediate and thorough investigation. Many studies have explored the trends in the utilization of panCT scans in the management of emergency cases and have found signs of overutilization [
7,
8,
9,
10,
11]. Overutilization, also called overuse, is defined as the excessive or inappropriate use of CT scans beyond what is clinically necessary [
12]. This trend is driven by various factors, including the desire for rapid diagnosis, fear of missing injuries, and medico-legal concerns [
8]. While these reasons are valid, the overutilization of panCT examinations is leading to unnecessary radiation exposure to patients, which potentially increases the risk of cancer [
9,
13,
14].
Despite these concerns, there is a lack of comprehensive research examining the extent of panCT overuse on a national scale. This study aims to analyze the current utilization patterns of panCT scans in emergency departments in Riyadh, Saudi Arabia, and investigate the potential overutilization of such examinations. The findings from this research could inform policy decisions and clinical guidelines, promoting more careful use of panCT examinations in emergency departments.
2. Materials and Methods
2.1. Study Design and Participants
The study received ethical approval from the author's institutions (Ref. No. E-23-8257). The study employed a retrospective cohort study design, focusing on trauma patients admitted to the emergency department (ED) who underwent a whole-body CT scan, also known as panCT, at a major academic hospital in Riyadh, Saudi Arabia. The study included all stable trauma patients, adult or pediatric, who underwent a panCT scan for one year (from January 1st, 2023, to December 31st, 2023).
2.2. PanCT Stable Trauma Protocol
The panCT trauma imaging protocol is typically prescribed for high mechanism trauma, including motor vehicle accidents (MVA), pedestrian or bicycle accidents, falls from height, physical assaults, or penetrating trauma such as gunshot wounds, to rule out acute injuries. In our hospital, the panCT trauma protocol has two categories based on the initial trauma evaluation: unstable or stable. Unstable protocol is designed for patients who are seriously injured and hemodynamically unstable, while stable trauma protocol is intended for hemodynamically stable patients. This study included an analysis of patients who underwent the stable trauma protocol.
All panCT scans were performed on Siemens SOMATOM Force eco (Siemens Healthineers, Munich, Germany). The scan field in the stable trauma protocol extended from the vertex of the skull to the symphysis pubis. The stable trauma protocol involved the following series: non-contrast head and neck (H&N), contrast-enhanced chest-abdomen arterial phase, and contrast-enhanced abdomen-pelvis venous phase. Delayed images of the abdomen and pelvis could be acquired as needed. Axial images of the head, cervical spine, chest, abdomen, and pelvis, along with coronal and sagittal reformats, were usually obtained to prepare for the interpretations by radiologist consultants.
2.3. Data Collection
The final approved radiology reports for all panCT scans performed from January 1st, 2023, to December 31, 2023, were retrieved from the Picture Arching and Communication System (PACS) and anonymized to ensure the confidentiality and anonymity of patient information. All patient names and medical record numbers were removed. De-identified patient-related data, such as date of admission, gender, age, radiation dose report, and the final approved radiology report, were collected. No patient-identifying data were collected.
2.4. PanCT Reports Review
The final approved radiology reports were reviewed along with de-identified data (date of admission, gender, age, and radiation dose as reported by the CT scanner). All panCT radiology reports followed a consistent structure, featuring separate sections for each of the head and neck, spine, chest, abdomen, and pelvis areas. Two radiology specialists licensed by the Saudi Commission for Health Sciences (SCHS) independently reviewed the anonymized radiology reports.
Any suboptimal study due to motion artifact, improper position, or beam hardening artifact, as noted in the reports, was excluded from the study. In addition, any incomplete studies or missing scans were also excluded.
The reports were classified into negative or positive based on their findings. A positive report indicates any acute traumatic injury, major or minor, to the head, spine, chest, abdomen, or pelvis. Conversely, a negative report means no acute traumatic injury was indicated in these areas. Incidental findings, including cysts or masses, chronic findings, or findings from previous traumas, were disregarded.
Additional classification was performed for reports containing positive findings. These include a positive report indicating injuries only in the head and neck (H&N) region, a positive report indicating injuries only in the chest-abdomen-pelvis (CAP) region, and a positive report indicating injuries in both the H&N and CAP regions. This additional classification of the positive reports may contribute to adopting more selective CT imaging.
2.5. Injury Severity Score (ISS) Calculation
ISS is a widely used scoring tool for multiple injuries in different body regions [
15,
16]. ISS was calculated based on the CT reports using an online calculation tool [
17]. Each injury is assigned an abbreviated injury scale (AIS) score to calculate the ISS. The AIS scoring system ranks injuries by severity from 1 to 6. The sum of the squares of the highest three AIS scores is calculated to obtain the ISS. The Injury Severity Score (ISS) ranges from 1 to 75. Scores between 1 and 8 are considered minor; Scores between 9 and 15 are moderate; Scores between 16 and 24 are severe; Scores above 24 are considered critical.
2.6. Statistical Analysis
Descriptive and inferential statistics were performed using Python programming language (version 3.10) in the Google Colab environment (Python 3.10). Logistic regression was performed to assess the impact of the independent variables (age and gender) on the dependent variable (panCT radiology report finding; either positive or negative). In addition, two-proportion Z-test was performed to compare the percentage of negative panCT scans to values found in similar studies. The significance level was set at 0.05. The following Python libraries were utilized to perform the statistical analysis and data visualization: pandas for data manipulation and analysis, statsmodels for fitting the logistic regression model and performing statistical tests, numpy & scipy for numerical operations and calculations, seaborn for data visualization, and matplotlib for creating plots.
3. Results
The emergency department at our hospital receives an average of 200 -250 visits per day, for which 2-3 panCT examinations are usually requested. In 2023, around 800 panCT trauma scans were performed. After considering the inclusion and exclusion criteria, 599 panCT scans were included in the analysis.
Of those 599 panCT scans, 531 were adults, and 68 were pediatric patients. The adults were 402 males and 129 females, while the pediatric patients were 56 males and 12 females.
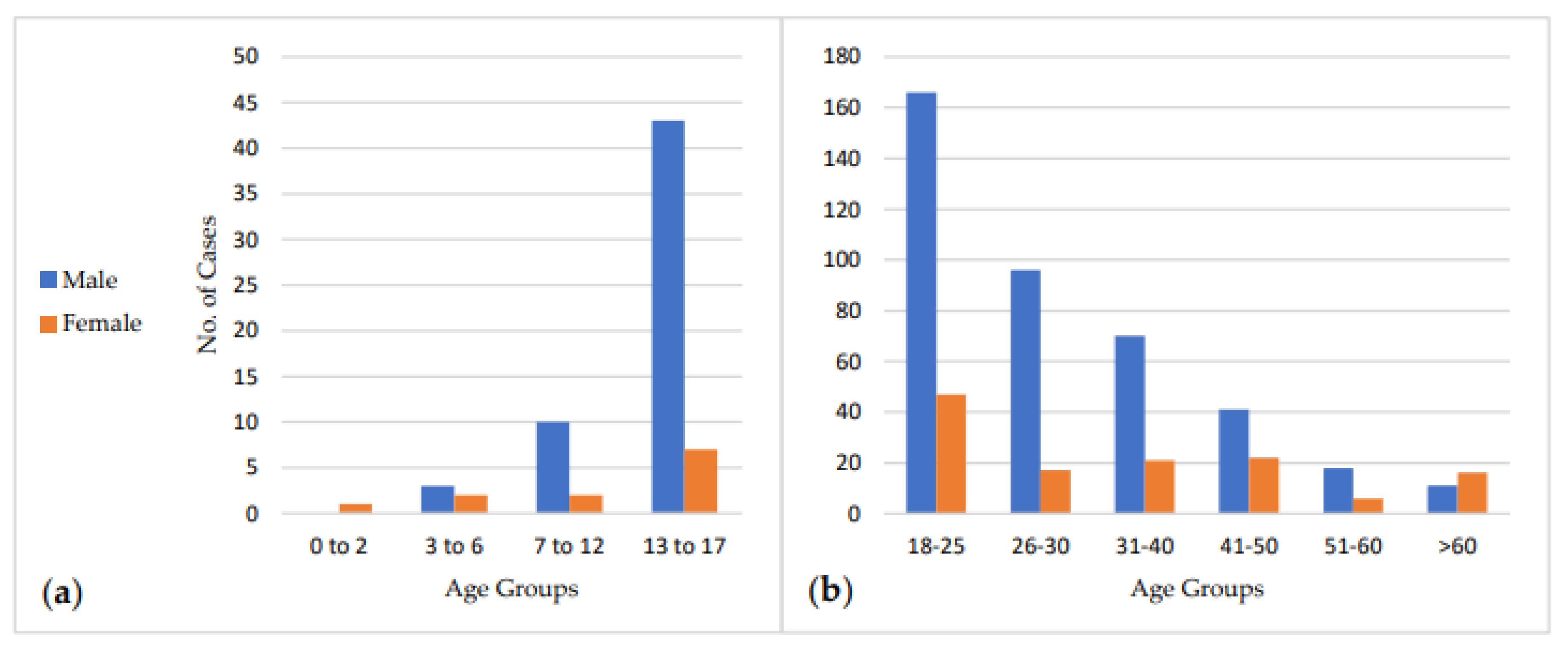
Figure 1 (a and b) shows the age distributions of adults and pediatric patients. Most pediatric patients (74%) were in the 13-17 age group. For adults, 40% of the patients were in the 18-25 age group.
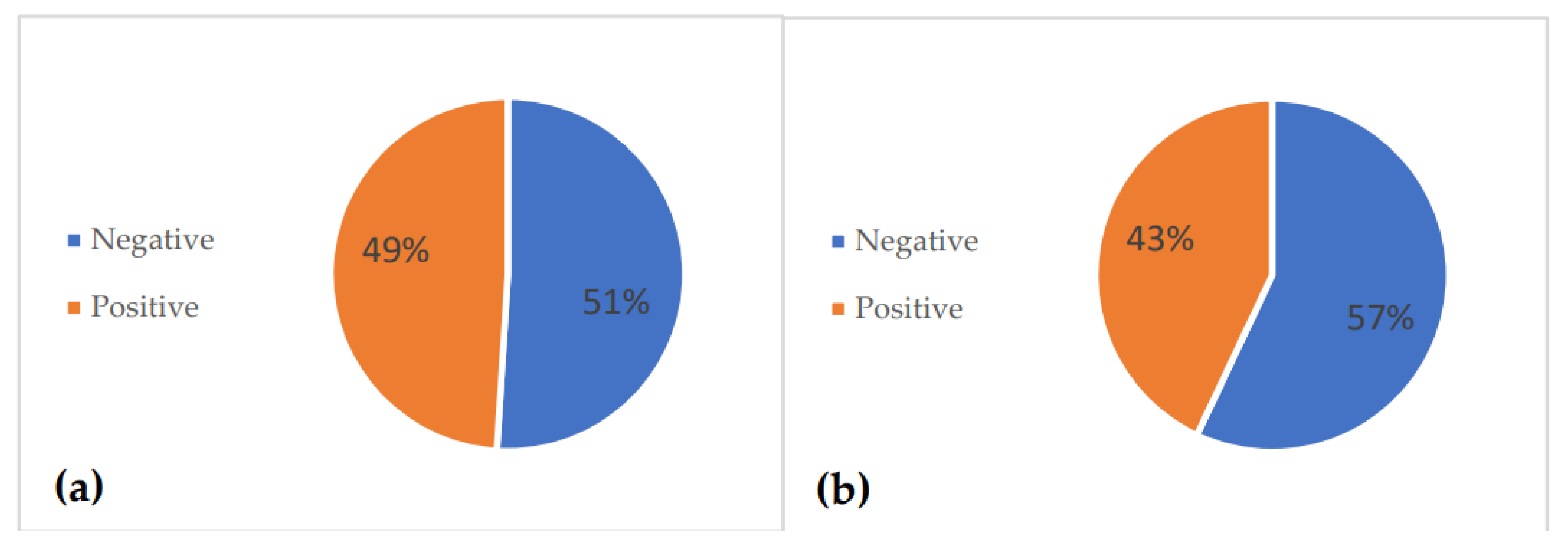
Figure 2 depicts the percentages of negative and positive panCT scans for pediatric and adult patients. The overall percentage of negative panCT scans was 56%, while the positive scans were 44%. In pediatric patients, the percentage of negative scans was 51%, while the positive scans were 49%. In adults, the percentage of negative scans was 57%, while the positive scans were 43%.
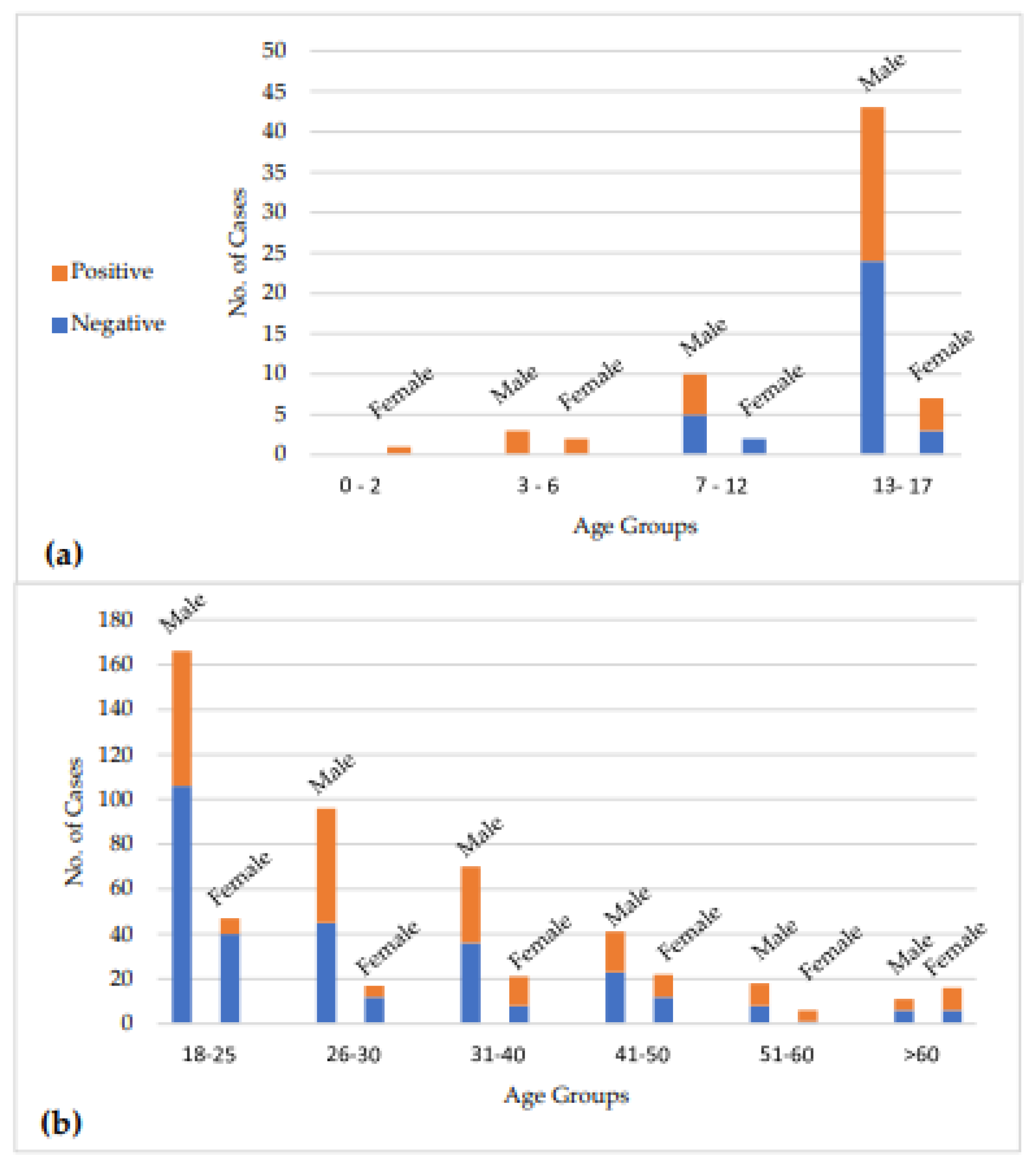
Figure 3 depicts the number of negative and positive scans according to age and gender. In pediatric cases, the percentages of negative scans were 0%, 0%, 58%, and 54% for age groups 0-2, 3-6, 7-12, and 13-17 years, respectively. In adult cases, the percentage of negative scans was 69%, 50%, 48%, 56%, 38%, and 44% for age groups 18-25, 26-30, 31-40, 41-50, 51-60, and >60, respectively. The highest rate of negative scans in pediatric patients was in the 7-12 age group, with seven negative reports out of 12. In adults, the 18-25 age group had the highest rate of negative reports, with 146 out of 213 reports being negative.
Table 1 shows the logistic regression results. Logistic regression analysis was performed to assess the impact of gender and age on the likelihood of negative findings. The model is statistically significant overall, with a Likelihood Ratio (LLR) test p-value of 0.02030. However, the R-squared was 0.009494. Age significantly impacts whether the finding is negative or positive (p-value=0.001). On the other hand, gender has no statistically significant impact on the finding (p-value=0.182).
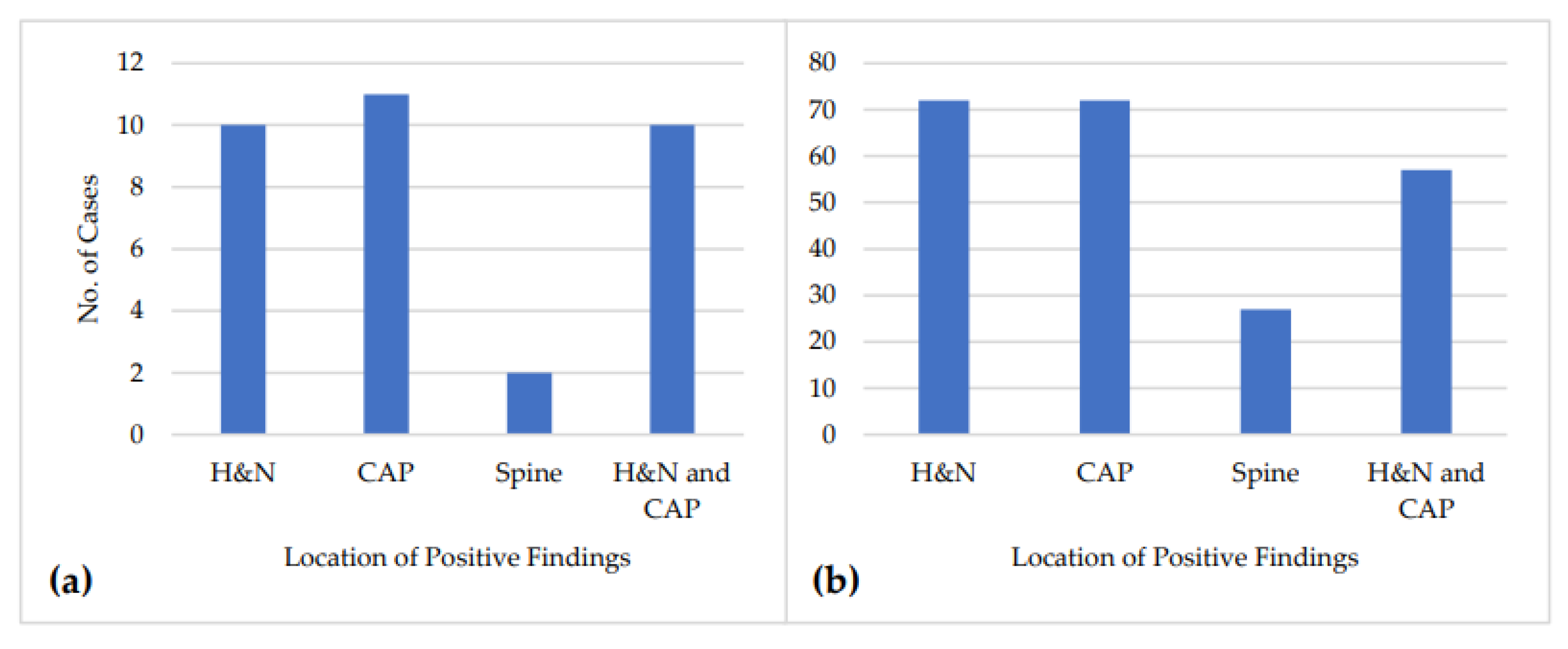
The positive reports were further subclassified to H&N-only injury, CAP-only injury, spine-only injury, or injury in both H&N and CAP regions. For pediatric patients, 30% of the positive scans reported injuries only in the H&N region, 33% of the positive reports reported injuries only in the CAP region, 6% of the positive reports reported injury only in the spine, and 30% of the positive reports reported injuries in both the H&N and CAP regions. For adults, 32% of the positive reports indicated injuries only in the H&N region, 32% of the positive reports indicated injuries only in the CAP region, 12% of the positive reports indicated injury only in the spine, and 25% of the positive reports indicated injuries in both the H&N and CAP regions.
Figure 4 shows the subclassification of the positive findings for pediatric and adult cases.
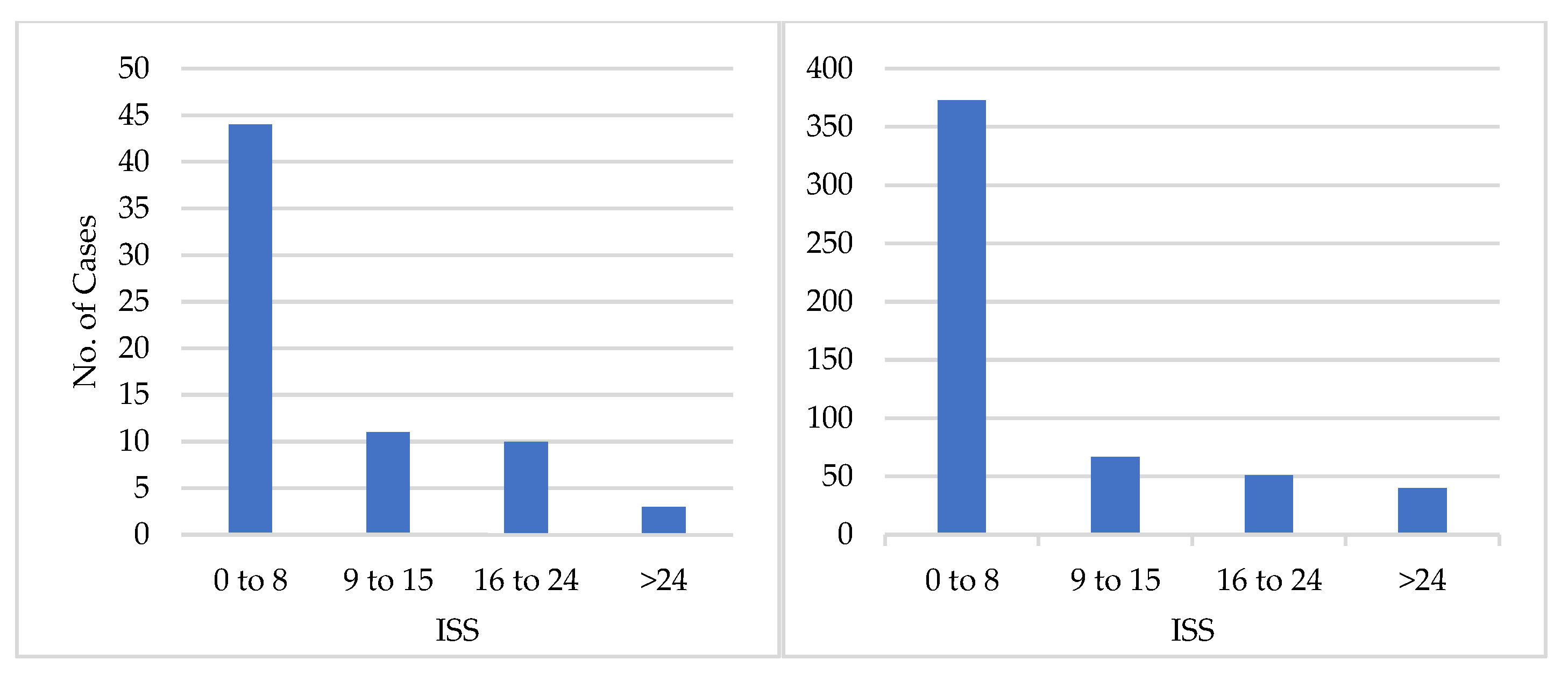
Figure 5 shows the results of the ISS calculation based on the reports’ findings. For adults, 373 (70%) reports scored between 1 and 8, while only 40 (8%) reports had an ISS above 24. For pediatrics, 44 (65%) reports had an ISS between 1 and 8, while only 3 (4%) had an ISS above 24.
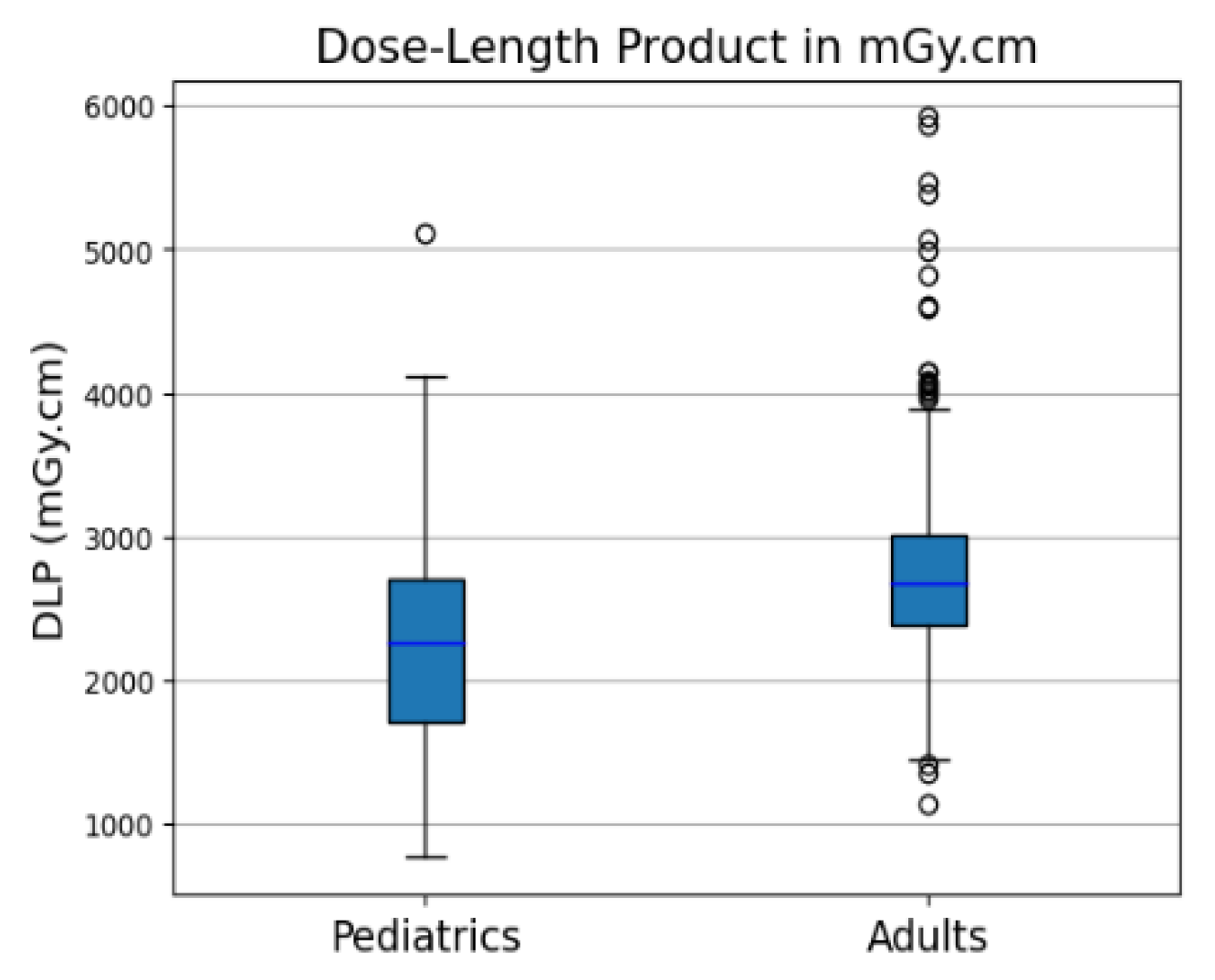
The total Dose-Length Product (DLP) for all imaging phases in the panCT scan, as reported by the CT scanner, was collected for each case. The pediatric DLP had the following values: the median was 2264 mGy.cm; the 25
th percentile was 1656 mGy.cm; the 75
th percentile was 2714 mGy.cm. The adult DLP has the following values: the median was 2666 mGy.cm; the 25
th percentile was 2372 mGy.cm; the 75
th percentile was 3011 mGy.cm.
Figure 6 shows a box plot of the reported total DLP (mGy.cm) for the panCT scans included in the study.
4. Discussion
The purpose of this study was to determine the possibility of overuse of panCT scans in the emergency department through the assessment of the utilization trends and findings of panCT scans done within one year in a major academic hospital in Riyadh, Saudi Arabia. The findings showed that 56% of the panCT scans were negative (no acute traumatic injuries), which may be regarded as a warning sign of overuse. This is in agreement with other studies that have pointed to the overuse of panCT scans in the emergency departments [
8,
19,
20,
21,
22].
The overall negative panCT scan rate in this study is 56% which is in agreement with the study by Salam Findakly et al. (2023) who had a negative panCT scan rate of 59.4% (p=0.299) [
23]. However, a statistically different result is observed when comparing the percentage of negative panCT scans in our study (57% for adults) with other studies as presented in
Table 2. We found a significantly higher rate of negative scans than in the studies by Bolbol Akram et al. (30%), Nisreen H Maghraby et al. (20. 4%), Hamidh A. Almusayliem et al. (27. 9%), and Violante Mulas et al. (47. 6%) [
24,
25,
26,
27]. The higher negative scan rate in this study may suggest that there is overuse of panCT examinations, which in turn means that patients are being exposed to unnecessary radiation.
There was no statistically significant correlation between gender and negative panCT findings. On the other hand, based on the logistic regression (
Table 1), age was found to be a predictor (p=0.009). This age-related trend should be further examined to establish age-dependent recommendations for the use of panCT scans in polytrauma cases.
The subclassification of the positive findings by the body region indicated that over one-third of the positive scans had injuries in either the H&N or CAP region, while a smaller proportion had injuries in both regions. This result indicates that, in some cases, a more selective CT imaging strategy, which would be limited to the area of interest, could be considered, thus potentially decreasing the patient’s radiation dose.
In addition, using the ISS derived from the radiology reports, it was observed that the majority of the cases (70% in adults and 65% in pediatrics) had an ISS of 1-8, which is a score for mild injuries. A few patients (8% for adults and 4% for pediatrics) had ISS greater than 24, which is a score for critical injury. This finding also supports the possibility of overuse of panCT scans, as a large number of patients may not have needed a whole-body CT and more selective imaging protocols could have been used.
The radiation dose from panCT scans should also be considered. The panCT scans included in this study had median DLP values of 2264 mGy.cm for pediatric patients and 2666 mGy.cm for adult patients, which highlights that these examinations are associated with high radiation exposure. The potential long-term effects of such radiation doses, especially in pediatric patients, emphasize the need for careful use of these scans [
13].
Based on the findings of this study, the following implications can be considered. The high rate of negative panCT scans and the prevalence of minor injuries indicate that the use of panCT imaging should be more selective, focusing on the areas of interest. This may help in the prevention of the overuse of panCT examinations and the associated radiation dose. Furthermore, there is a potential benefit of evidence-based guidelines and decision support tools to enhance the appropriate usage of panCT scans in emergency departments. For example, the American College of Radiology (ACR) Appropriateness Criteria and guidelines from other international organizations offer extensive guidance on the imaging of different clinical conditions, including trauma [
28,
29]. Following such recommendations and guidelines may help to reduce the overuse of panCT scans and encourage the use of more selective imaging techniques. Also, by reducing the overuse of panCT scans in emergency departments, we can improve the workload management for the radiology personnel. This would allow the radiology staff to concentrate on severe trauma cases where there are proven benefits of panCT examinations.
This study has the following limitations that should be noted. First, because this was a retrospective study, we could not collect information on the clinical context and the decision-making that led to the ordering of panCT scans. Details of the patient’s symptoms, vital signs, and triage assessments at the time of admission, such as Glasgow coma scale, may have been useful in determining the appropriateness of the panCT. Secondly, this study was conducted at a single academic medical center, which may affect the generalizability of the findings. Future studies that include more hospitals in Saudi Arabia would be required to confirm the findings and make more general conclusions about the possible overuse of panCT scans in emergency departments in the country.
Implementing quality improvement programs may help to prevent the overuse of panCT scans in emergency departments. These programs would involve regular observation of the patterns of ordering diagnostic imaging examinations, trend analysis to determine any possibility of overuse, and providing feedback to healthcare providers.
Some studies have developed prediction algorithms and clinical decision rules for imaging in certain conditions, including head injury and cervical spine trauma. The Canadian CT Head Injury/Trauma Rule [
30], the PECARN (Pediatric Emergency Care Applied Research Network) rules [
31], CHALICE (Children’s Head injury Algorithm for the prediction of Important Clinical Events) Rule [
32] , and the National Emergency X-Radiography Utilization Study (NEXUS) criteria [
33] are examples of such prediction models and rules. These models incorporate several clinical and patient variables to predict patients suitable for imaging. The same could be done for the use of panCT scans in polytrauma care management. These models could help emergency physicians make better decisions about the necessity of a panCT scan, thus decreasing the rate of its overuse while ensuring that high-risk patients will be provided with the necessary imaging.
5. Conclusions
This study showed that 56% of the panCT scans were negative, and the majority of the patients (70%) had minor injuries, which suggests the possibility of overusing panCT scans in the emergency department. The logistic regression analysis showed that age was the only predictor of negative findings. Given the associated high radiation dose from panCT scans, the study findings showed the importance of monitoring the ordering patterns of imaging studies, especially panCT examinations. The use of selective CT imaging in polytrauma cases can help minimize the radiation dose to some patients while ensuring that the necessary imaging is performed for high-risk patients. Reducing the overutilization of panCT scans improves patient safety standards and helps to optimize resource management in emergency and radiology departments.
Author Contributions
Conceptualization, AH, MA & HA; methodology, HA, AH ,MA & AS; software, HA&AS; validation, KE&MM; formal analysis, HA.; investigation, AH&MA; resources, AH&MA; data curation, HA.; writing—original draft preparation, HA.; writing—review and editing, KE, MM&AA.; visualization, HA.; supervision, HA & AA; project administration, MM. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of King Saud University (Ref. No. E-23-8257; date of approval:6 November,2023).
Informed Consent Statement
Patient consent form was waived due to the retrospective nature of the study.
Data Availability Statement
The data are available upon request from the corresponding author.
Acknowledgments
The authors extend their appreciation to the College of Applied Medical Sciences Research Center and the Deanship of Scientific Research at King Saud University for funding this work.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hagi, S.; Khafaji, M.; Ahmed, N.; Al Nowami, M. Current Trends in Computed Tomography Referral Practice Experience at a Large Academic Hospital; 2014; Vol. 11;.
- Kocher, K.E.; Meurer, W.J.; Fazel, R.; Scott, P.A.; Krumholz, H.M.; Nallamothu, B.K. National Trends in Use of Computed Tomography in the Emergency Department. Ann Emerg Med 2011, 58. [CrossRef]
- Bellolio, M.F.; Bellew, S.D.; Sangaralingham, L.R.; Campbell, R.L.; Cabrera, D.; Jeffery, M.M.; Shah, N.D.; Hess, E.P. Access to Primary Care and Computed Tomography Use in the Emergency Department. BMC Health Serv Res 2018, 18. [CrossRef]
- Romano, F.; Iacobellis, F.; Guida, F.; Laccetti, E.; Sorbo, A.; Grassi, R.; Scaglione, M. Traumatic Injuries: Mechanisms of Lesions. In Diagnostic Imaging in Polytrauma Patients; Springer International Publishing, 2017; pp. 35–55 ISBN 9783319620541.
- Miele, V.; Addeo, G.; Cozzi, D.; Danti, G.; Bonasera, L.; Trinci, M.; Grassi, R. Management of Polytrauma Patients. In Diagnostic Imaging in Polytrauma Patients; Springer International Publishing, 2017; pp. 1–34 ISBN 9783319620541.
- Fathi, M.; Mirjafari, A.; Yaghoobpoor, S.; Ghanikolahloo, M.; Sadeghi, Z.; Bahrami, A.; Myers, L.; Gholamrezanezhad, A. Diagnostic Utility of Whole-Body Computed Tomography/Pan-Scan in Trauma: A Systematic Review and Meta-Analysis Study. Emerg Radiol 2024, 31, 251–268. [CrossRef]
- Mohamed, H.; Teoh, K. Outcome of Selective CT vs. Pan-CT Scan in Elderly Trauma Patients: A Retrospective Cohort Study in a Level 1 Trauma Center. Chinese Journal of Traumatology - English Edition 2021, 24, 249–254. [CrossRef]
- Oosthuizen, G. V.; Bruce, J.L.; Bekker, W.; Shangase, N.; Laing, G.L.; Clarke, D.L. Pan Computed Tomography for Blunt Polytrauma: Are We Doing Too Many? South African Medical Journal 2016, 106, 801–803. [CrossRef]
- Elster, A.D. Is the Use of Pan-Computed Tomography for Blunt Trauma Justified? A Prospective Evaluation. Yearbook of Diagnostic Radiology 2011, 2011, 178–180. [CrossRef]
- Shojaee, M.; Kariman, H.; Manouchehrifar, M.; Heydari, K.; Sohrabi, S. Pan vs. Selective Computed Tomography Scans in Management of Multiple Trauma Patients; a Brief Report; 2017; Vol. 5;.
- Debnath, J. Is Routine Pan Computed Tomography for Patients with Blunt Trauma Justified? Ann Emerg Med 2012, 60, 244.
- Miglioretti, D.L.; Smith-Bindman, R. Overuse of Computed Tomography and Associated Risks. Am Fam Physician 2011, 83, 1252–1254.
- Miglioretti, D.L.; Johnson, E.; Williams, A.; Greenlee, R.T.; Weinmann, S.; Solberg, L.I.; Feigelson, H.S.; Roblin, D.; Flynn, M.J.; Vanneman, N. The Use of Computed Tomography in Pediatrics and the Associated Radiation Exposure and Estimated Cancer Risk. JAMA Pediatr 2013, 167, 700–707.
- Çalik, M.; Ersoy, A.H.; Ekin, E.E.; Öztürk, D.; Güleç, S.G. Assessment of Cost-Effectiveness of Computerized Cranial Tomography in Children with Mild Head Trauma. Diagnostics 2022, 12, 2649.
- Stevenson, M.; Segui-Gomez, M.; Lescohier, I.; Di Scala, C.; McDonald-Smith, G. An Overview of the Injury Severity Score and the New Injury Severity Score. Injury Prevention 2001, 7, 10–13.
- Baker, S.P.; o’Neill, B.; Haddon Jr, W.; Long, W.B. The Injury Severity Score: A Method for Describing Patients with Multiple Injuries and Evaluating Emergency Care. Journal of Trauma and Acute Care Surgery 1974, 14, 187–196.
- Baker, S. Injury Severity Score (ISS) Available online: https://www.mdcalc.com/calc/1239/injury-severity-score-iss (accessed on 19 July 2024).
- Python Https://Colab.Research.Google.Com/.
- Jame, S.Z.B.; Majdzadeh, R.; Sari, A.A.; Rashidian, A.; Arab, M.; Rahmani, H. Indications and Overuse of Computed Tomography in Minor Head Trauma. Iran Red Crescent Med J 2014, 16. [CrossRef]
- Jindal, A.; Velmahos, G.C.; Rofougaran, R. Computed Tomography for Evaluation of Mild to Moderate Pediatric Trauma: Are We Overusing It? In Proceedings of the World Journal of Surgery; January 2002; Vol. 26, pp. 13–16.
- Melnick, E.R.; Shafer, K.; Rodulfo, N.; Shi, J.; Hess, E.P.; Wears, R.L.; Qureshi, R.A.; Post, L.A. Understanding Overuse of Computed Tomography for Minor Head Injury in the Emergency Department: A Triangulated Qualitative Study. Academic Emergency Medicine 2015, 22, 1474–1483. [CrossRef]
- OhAnA, O.; sOffer, shelly; ZiMlichMAn, eyAl; KlAng, eyAl Overuse of Ct and Mri in Paediatric Emergency Departments 1; 2018;
- Findakly, S.; Zia, A.; Kavnoudias, H.; Mathew, J.; Varma, D.; Di Muzio, B.; Lee, R.; Moriarty, H.K.; Joseph, T.; Clements, W. The Use of Whole-Body Trauma CT Should Be Based on Mechanism of Injury: A Risk Analysis of 3920 Patients at a Tertiary Trauma Centre. Injury 2023, 54, 110828.
- Akram, B.; Abdulhakam, A.; Osman EA, S.; Abdullah Al-mater, A. Whole-Body Computed Tomography for Polytrauma Patients in the Emergency Department: Recommended or Unnecessary Radiation. International Journal of Surgery Research and Practice 2022, 9. [CrossRef]
- Maghraby, N.H.; Alshaqaq, H.M.; AlQattan, A.S.; Alfaraj, A.F.; Alghamdi, O.A.; Alzawad, M.J.; Farcy, D.A. Negative Whole-Body Computed Tomography Scans in Polytrauma Patients: A Retrospective Cohort Study. Open Access Emergency Medicine 2020, 305–313.
- Almusayliem, H.A.; Kommosani, L.A.; Malebary, R.M.; Althagafi, M.A.; Alghanmi, R.A.; Nematallah, Q.S.; Bakhsh, A.; Bakhsh, A.A. Yield of Whole-Body Computed Tomography at a Low-Volume Emergency Department: A 5-Year Experience. Saudi Med J 2021, 42, 428.
- Mulas, V.; Catalano, L.; Geatti, V.; Alinari, B.; Ragusa, F.; Golfieri, R.; Orlandi, P.E.; Imbriani, M. Major Trauma with Only Dynamic Criteria: Is the Routine Use of Whole-Body CT as a First Level Examination Justified? Radiol Med 2022, 1–7.
- Shyu, J.Y.; Khurana, B.; Soto, J.A.; Biffl, W.L.; Camacho, M.A.; Diercks, D.B.; Glanc, P.; Kalva, S.P.; Khosa, F.; Meyer, B.J. ACR Appropriateness Criteria® Major Blunt Trauma. Journal of the American College of Radiology 2020, 17, S160–S174.
- Gunes Tatar, I.; Aydin, H.; Kizilgoz, V.; Yilmaz, K.B.; Hekimoglu, B. Appropriateness of Selection Criteria for CT Examinations Performed at an Emergency Department. Emerg Radiol 2014, 21, 583–588. [CrossRef]
- Stiell, I.G.; Wells, G.A.; Vandemheen, K.; Clement, C.; Lesiuk, H.; Laupacis, A.; McKnight, R.D.; Verbeek, R.; Brison, R.; Cass, D. The Canadian CT Head Rule for Patients with Minor Head Injury. The Lancet 2001, 357, 1391–1396.
- Kuppermann, N.; Holmes, J.F.; Dayan, P.S.; Hoyle, J.D.; Atabaki, S.M.; Holubkov, R.; Nadel, F.M.; Monroe, D.; Stanley, R.M.; Borgialli, D.A. Identification of Children at Very Low Risk of Clinically-Important Brain Injuries after Head Trauma: A Prospective Cohort Study. The Lancet 2009, 374, 1160–1170.
- Dunning, J.; Daly, J.P.; Lomas, J.P.; Lecky, F.; Batchelor, J.; Mackway-Jones, K. Derivation of the Children’s Head Injury Algorithm for the Prediction of Important Clinical Events Decision Rule for Head Injury in Children. Arch Dis Child 2006, 91, 885–891.
- Hoffman, J.R.; Mower, W.R.; Wolfson, A.B.; Todd, K.H.; Zucker, M.I. Validity of a Set of Clinical Criteria to Rule out Injury to the Cervical Spine in Patients with Blunt Trauma. New England Journal of Medicine 2000, 343, 94–99.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).