1. Introduction
In 2011, 45% of pregnancies in the United States and 59% in Georgia were unintended [
1]. Pharmacist-prescribed self-adminstered hormonal contraception (HC) is one strategy that has been implemented in an effort to improve patient access and decrease unintended pregnancy rates. In 2016, California and Oregon successfully implemented pharmacist prescribed self-administered hormonal contraception without a physician’s prescription. Currently more than half of the states in the US have approved this expanded scope of practice [
2]. This trend will likely continue, with more states allowing pharmacists to prescribe hormonal contraception, and in some instances emergency contraception, under state protocols and regulations.
Multiple studies have assessed patient, pharmacist, and pharmacy student attitudes and interest in pharmacist prescribed HC, and much of this data has been anlyzed in a systematic review [
3,
4,
5,
6,
7,
8]. Data indicate that a majority in all three of these groups support this expanded scope of practice, and intend to participate if available in their state. Additionally, data indicate that most pharmacy students view HC prescribing as part of their job description, regardless of whether or not it is approved in their state [
7]. Contemporary national data also demonstrate that regardless of state approval, community pharmacists from across the United States support pharmacist prescribed HC [
6,
8].
To date, few studies have assessed how pharmacists working in both community and non-community practice settings view this expanded scope of practice. One 2018 study conducted in a single state provides some insight, but it is unclear if prescribing HC is now viewed as a standard part of the pharmacist’s role by the profession as a whole, including pharmacists working in non-community practice settings [
9].
Studies evaluating oral emergency contraceptive access in Georgia have found differences in pharmacy access between metropolitan and nonmetropolitan areas for these medications. However, it is unknown if there are differences between metropolitan and nonmetropolitan areas regarding pharmacist interest and attitudes in hormonal contraception prescribing, another aspect of reproductive health.
This study’s primary objective is to assess differences between Georgia community and non-community pharmacists in their perceptions of pharmacist preparedness and scope of practice regarding HC prescribing. The secondary objective is to assess community pharmacist interest in providing this service in Georgia, and compare differences in pharmacist interest, perceptions, comfort, and perceived barriers between metro and nonmetropolitan counties.
2. Materials and Methods
This study was deemed exempt by the University of Georgia’s Institutional Review Board. A voluntary online survey was emailed via Redcap to all pharmacist members in the Georgia Pharmacist Association and Georgia Society of Health-System Pharmacists membership lists in mid-March of 2022, and survey responses were accepted for 1 week. The survey was developed based on previously published research, took approximately 10 to 15 minutes to complete, and was administered entirely online. The survey collected demographic information and perceptions regarding pharmacist prescribed HC if it were permitted in the state of Georgia. Likert style questions assessed pharmacists’ interest, perceptions, comfort, and perceived barriers regarding pharmacist prescribed HC. The full survey is available to view in Supplementary Materials, Figure S1. Responses were included in data analysis if they were completed by Georgia pharmacists with an active license, as verified by the State Board of Pharmacy online license lookup tool. All survey participants received a $15 Amazon gift card via email for survey completion.
Pharmacists were categorized as community pharmacists if they worked full or part time in a community pharmacy. Pharmacists were categorized as non-community if they worked in other practice settings, including hospital, ambulatory care clinics, managed care, industry, or other. Respondents were classified by metropolitan or nonmetropolitan areas using the 2013 National Center for Health Statistics (NCHS) Urban-Rural Classification Scheme in the different Georgia counties.[
10]
Descriptive statistics were used and reported as percentages based on survey results. Likert square responses were dichotomized and Chi square testing identified differences between groups.
3. Results
Of the 2592 pharmacists who received the survey, 454 responded. Of these, 19 responses were excluded for being out of state, 7 had an unverifiable license number, and 121 had an email address that did not correspond with the reported license number. Three hundred and seven pharmacists with a verified active Georgia license completed the survey, for a response rate of 11.8%. Out of the 307 respondents, 144 (46.9%) were identified as community pharmacists and 163 (53.1%) as non-community pharmacists.
Table 1.
Pharmacist Demographics (n=307).
Table 1.
Pharmacist Demographics (n=307).
| Characteristic |
Totaln=307 n (%) |
Communityn=144 n (%) |
Non-communityn=163 n (%) |
| Gender |
|
|
|
| Male |
100 (32.6) |
64 (44.4) |
36 (22.1) |
| Female |
207 (67.4) |
80 (55.6) |
127 (77.9) |
| Region |
|
|
|
| Metropolitan |
252 (82.1) |
105 (72.9) |
147 (90.2) |
| Nonmetropolitan |
55 (17.9) |
39 (27.1) |
16 (9.8) |
| Years in Practice |
|
|
|
| 1-15 |
182 (59.3) |
76 (52.8) |
106 (65.0) |
| 16-30 |
74 (24.1) |
38 (26.4) |
36 (22.1) |
| >30 |
51 (16.6) |
30 (20.8) |
21 (12.9) |
| Age in years |
|
|
|
| 24-40 |
168 (54.7) |
67 (46.5) |
101 (62.0) |
| 41-55 |
89 (29.0) |
48 (33.3) |
41 (25.1) |
| >55 |
50 (16.3) |
29 (20.1) |
21 (12.9) |
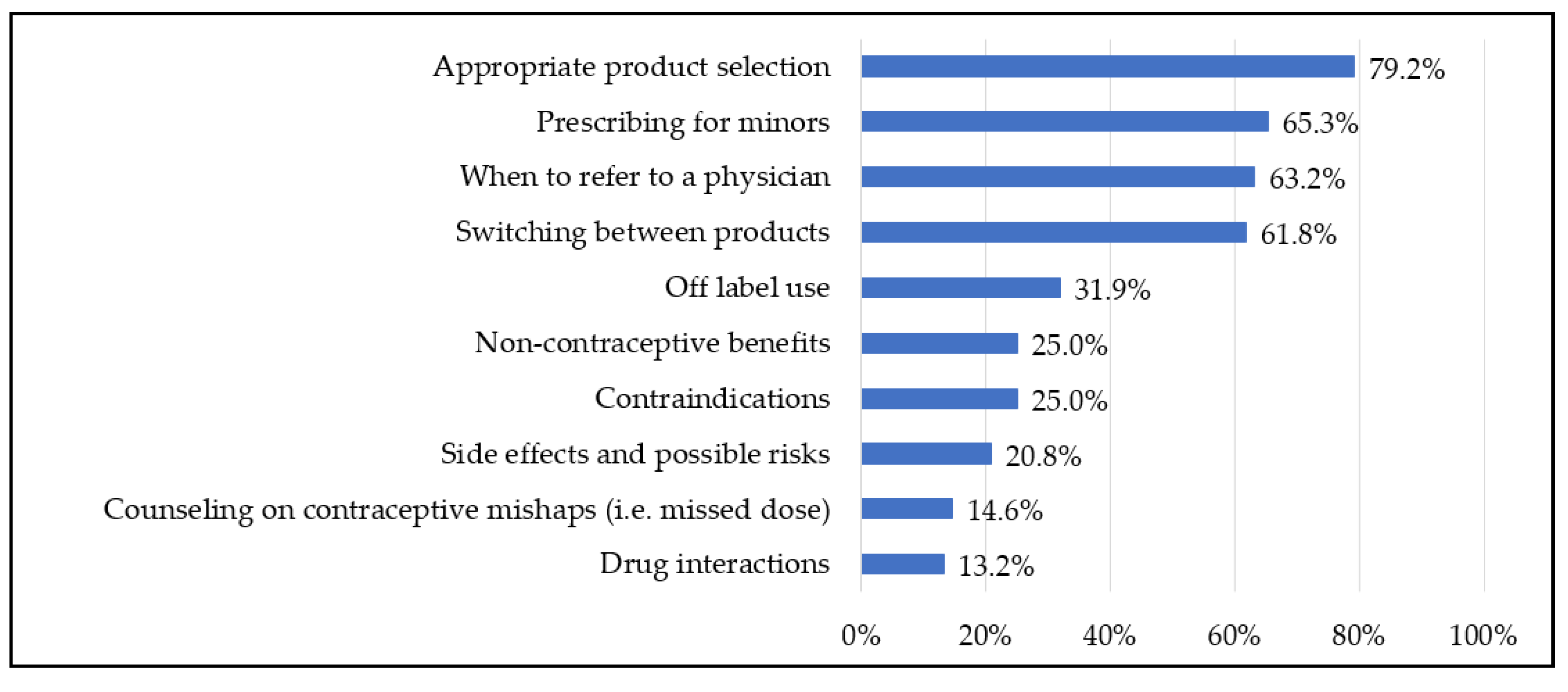
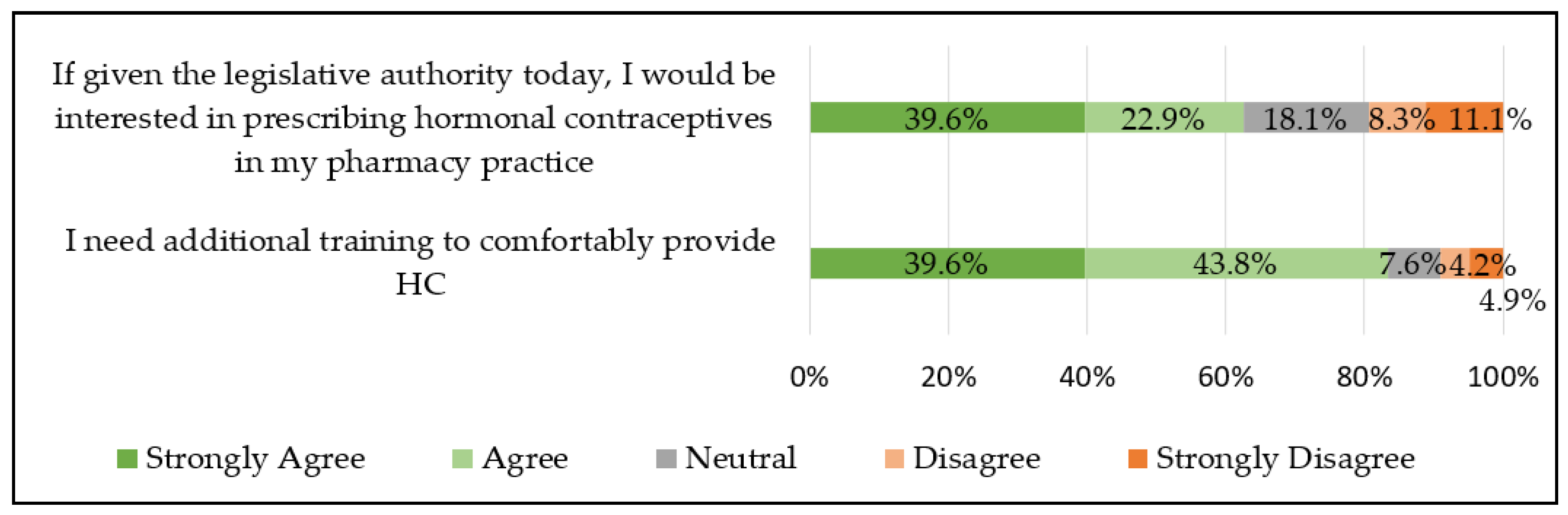
Community Pharmacist Interest and Comfort: Metropolitan vs. Nonmetropolitan
The majority of community pharmacists “strongly agree” or “agree” that they were personally interested in prescribing HC if given the legislative authority (Total 62.5%; Metropolitan 62.9% vs Nonmetropolitan 61.5%, p = 0.86). Most also “strongly agree” or “agree” that they would need additional training (Total 83.3%; Metropolitan 85.7% vs Nonmetropolitan 76.9%, p = 0.21). See
Figure 2.
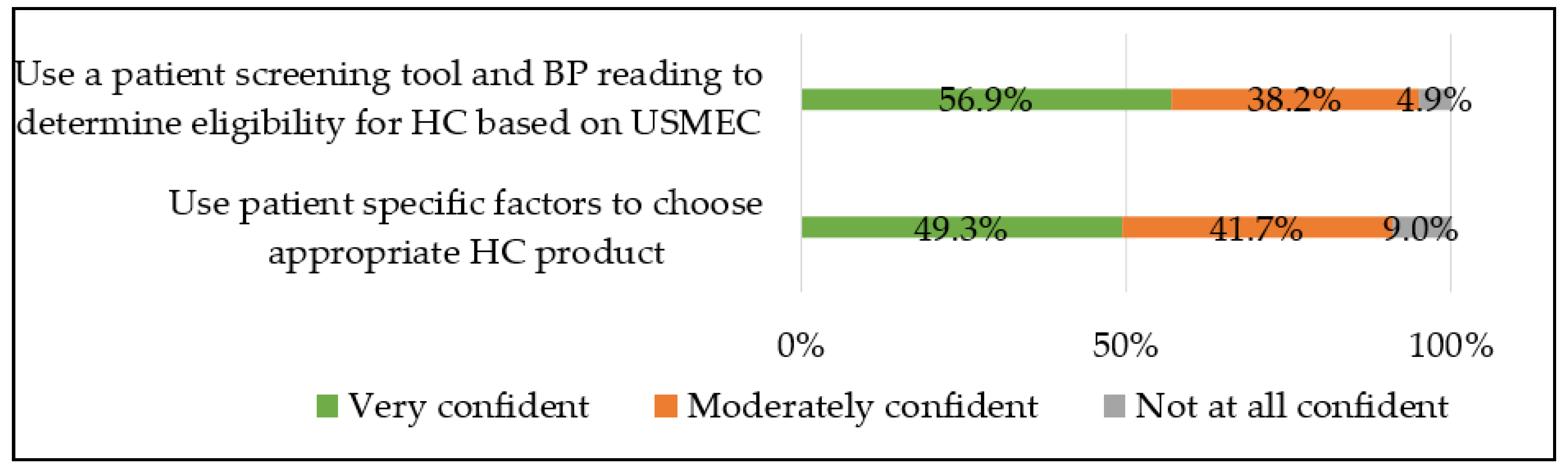
A majority of community pharmacists reported being “very” or “moderately confident” in using a patient screening tool and blood pressure reading to determine eligibility for HC (Total 95.1%; Metropolitan 96.1% vs Nonmetropolitan 92.3%, p=0.5) and using patient specific factors (i.e. past medical history, medication history, preferences) to choose an appropriate hormonal contraceptive (Total 91%; Metropolitan 93.3% vs Nonmetropolitan 84.6%,p = 0.24). See
Figure 3.
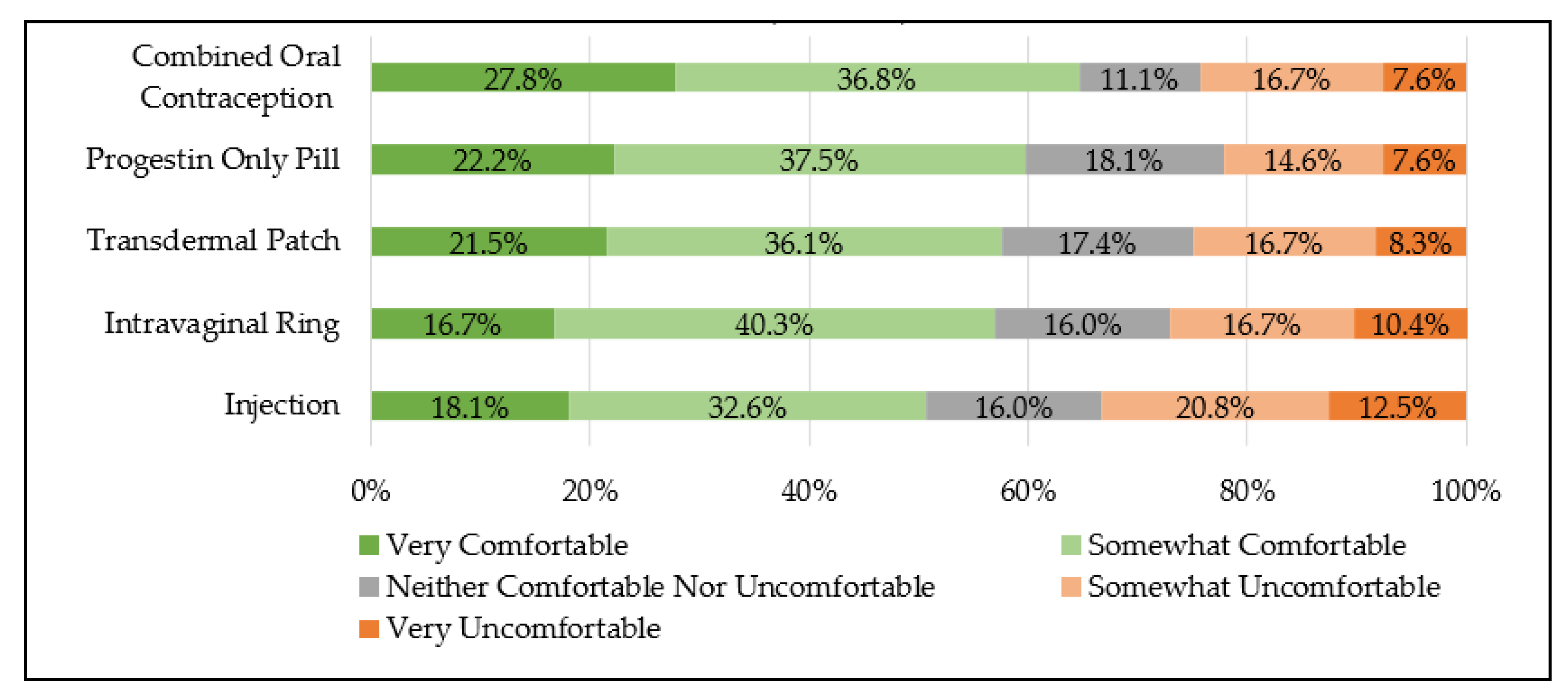
Regardless of metropolitan or nonmetropolitan location, a majority of community pharmacists reported being “very” or “somewhat comfortable” with counseling on all contraceptive products, including combined oral contraception (Total 64.6%; Metropolitan 62.9% vs. Nonmetropolitan 69.2%, p=0.48), progestin only pills (Total 59.7%; Metropolitan 60.0% vs. Nonmetropolitan 59.0%, p=0.91), transdermal patches (Total 57.6%; Metropolitan 61.0% vs. Nonmetropolitan 48.7%, p=0.19), intra-vaginal rings (Total 56.9%; Metropolitan 61.0% vs. Nonmetropolitan 46.2%, p=0.11), and injections (Total 50.7%; Metropolitan 52.4% vs. Nonmetropolitan 46.2%, p=0.51). See
Figure 4.
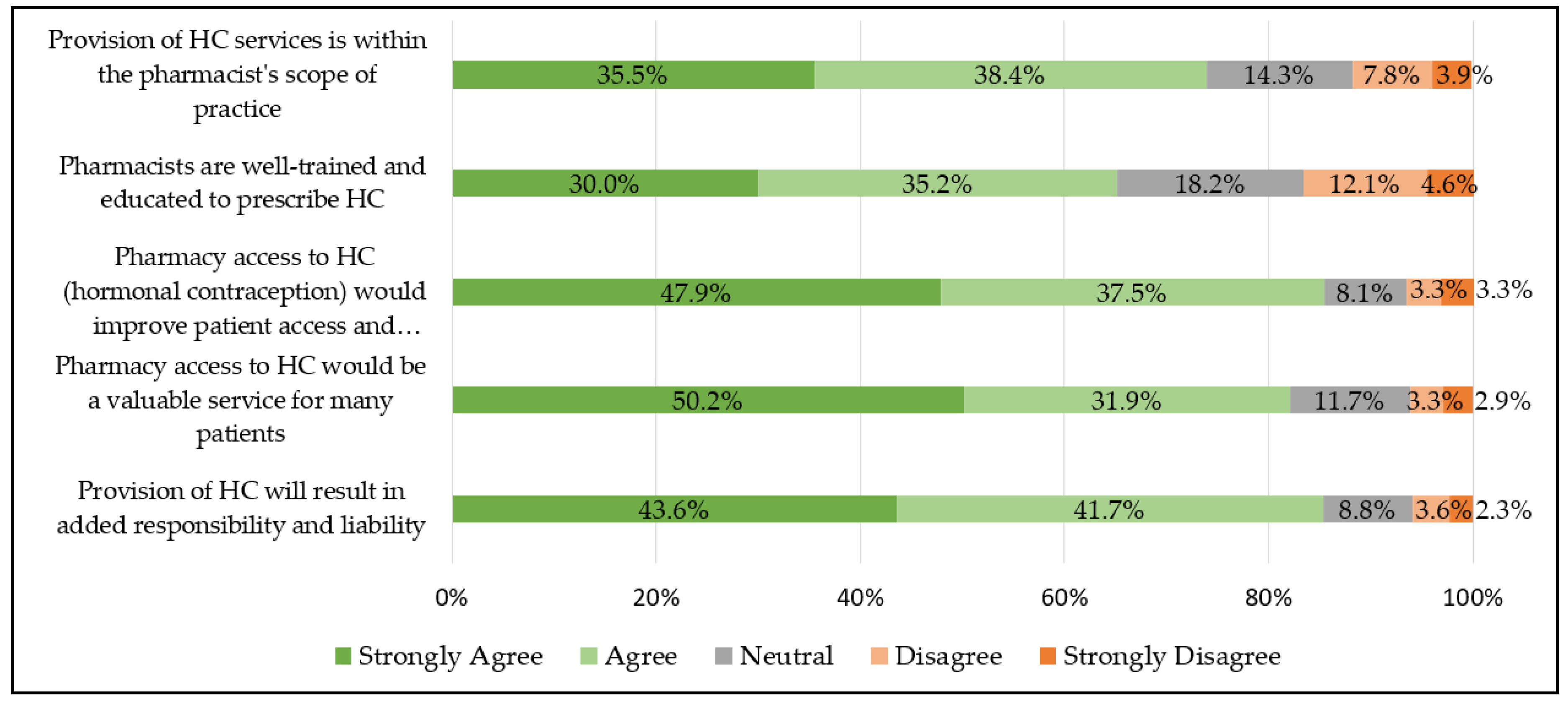
4. Discussion
A majority of Georgia pharmacists, both in community and non-community practice, believe that prescribing HC is within the pharmacists scope of practice (74%) and that pharmacists are well trained and educated for this role (65%). Previously published national and state level data clearly demonstrate that community pharmacists believe prescribing HC is within their scope of practice and pharmacists are adequately prepared for this role; however, most literature does not report the perspectives of non-community pharmacists, and therefore are limited in their assessment of the profession as a whole [
3,
4,
5,
6,
7,
8].
To the authors knowledge, one other study assesses both community and non-community pharmacist perspectives. It was conducted in North Carolina in 2018 when pharmacist prescribed HC was not yet authorized, although this expanded scope was ultimately granted in 2022 [
9]. Over half of all pharmacists agreed that prescribing HC allows pharmacists to practice at a higher level, rural areas would benefit from pharmacist prescribed HC, and increased access to HC is an important public health issue. Surprisingly, data indicated that noncommunity pharmacists were more likely than community pharmacists to agree with the aforementioned statements regarding pharmacist prescribed HC [
9].
This Georgia based survey found, similar to North Carolina pharmacists, a majority of pharmacists “agreed” or “strongly agreed” that pharmacy access would be a valuable service for many patients (82%) and pharmacy access would improve patient access and adherence (85%). Although there were many similiarites between these two survey studies, there were a few notable differences. Approximately 65% Georgia pharmacists “agreed” or “strongly agreed” that pharmacists are well trained/educated to prescribe HC, compared to less than 50% of North Carolina pharmacists [
9]. This may be in part because the North Carolina study was conducted 3 years eariler, and pharmacist confidence in the doctor of pharmacy education and training for this activity may have contiued to increase over this time.
Taken together, these two studies indicate that pharmacists, regardless of practice type or state regulations, now perceive pharmacist prescribed self administered hormonal contraception as an established activity within the community pharmacy scope of practice. Regardless of practice site, pharmacists believe it is a valuable service for patients and will improve patient access and adherence.
When comparing the perspectives of community pharmacists in metropolitan and non-metropolitan areas there were relatively few differences. Regardless of location in Georgia, a majority of community pharmacists (62%) are interested in prescribing hormonal contraception. This is similar to other national contemporary studies which indicate 65% of pharmacists are interested in providing direct access to hormonal contraception [
6]. Community pharmacists in metropolitan and non-metropolitan regions believe pharmacist prescribed HC is good for patient care.
Additionally, most Georgia community pharmacists indicated they felt comfortable using a patient screening tool and BP reading to determine eligibility for HC based on the United States Medical Elegibility Criteria for Contraceptive Use (USMEC), and use patient specific factors to choose appropriate HC product. As other national studies have also identified, although most believe pharmacists are well prepared, over 80% still desire additional training prior to offering this service [
11]. This may be related to the fact that although pharmacists complete contraception training in their degee program, years many have passed they received formal education in this area, and they desire contiuing education to stay abreast of current trends and practice updates. This point is often addressed by the state board of pharmacy by requiring additional certification and/or continuing education in this area in order to provide this service.
However, more community pharmacists in metropolitan areas believed that pharmacists are well trained and educated to prescribe HC and that it is within their scope of practice. Another study in Oregon found that pharmacists in urban areas were more likely to indicate they were planning to offer pharmacist prescribed contraception [
12]. In contrast, perceptions of pharmacist prescribed HC in other states have not demonstrated a difference between rural and urban areas. One study conducted in New Mexico following implementation of pharmacist prescribing found that rural pharmacists were as likely as their urban counterparts to prescribe hormonal contraception [
13]. Another conducted in North Carolina found attitudes regarding pharmacist prescribed hormonal contraception did not significantly differ by geographic region [
14]. Although the objectives of this Georgia based survey did not specifically set out to evaluate gender, the authors noted that gender may have potentially contributed to this difference in this study, as 46% of participants in non-metro areas were male compared to only 29% in metro areas.
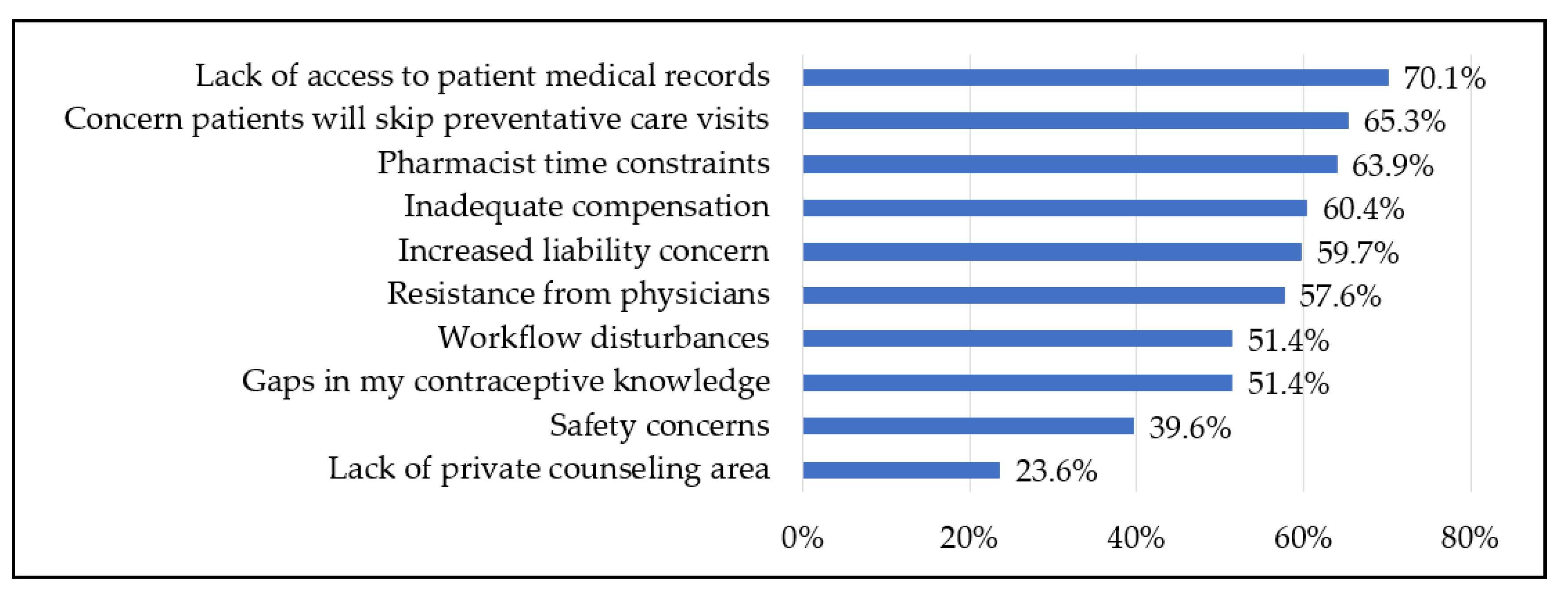
Similar to other national studies, pharmacist identified barriers included concerns regarding lack of access to medical records, missing preventative care, time constraints, inadequate compensation, increased liability, resistance from physicians, workflow disturbances, gaps in contraceptive knowledge [
3,
4,
5,
6,
7,
9]. However, the continued expansion of this service across the United States demonstrates the profession of pharmacy is able to to mitigate or overcome these barriers [
2,
15].
Limitations of this study include its small size and analysis of data from just one state. The results of this voluntary study may have been subject to selection bias and nonresponse bias.
Conclusion
This study found that in a state without pharmacist prescribing, the vast majority of pharmacists, regardless of practice site, believe that 1) pharmacists are adequately educated to prescribe HC, 2) prescribing HC is part of pharmacists professional scope of practice, and 3) pharmacists are interested in prescribing HC. Metropolitan pharmacists were more likely to believe that 1) pharmacists are well trained and educated to prescribe HC and 2) it is within their scope of practice. There were no other differences identified between metropolitan and non-metropolitan community pharmacists in their interest and perceptions regarding pharmacist prescribed contraception.
Author Contributions
Conceptualization, RHS; methodology, RHS, LL, MP; validation, RHS; formal analysis, RHS; data curation, LL, MP; writing—original draft preparation, RHS, LL, MP; writing—review and editing, RHS, LL, MP; project administration, RHS. All authors have read and agreed to the published version of the manuscript.
Funding
This research received funding from the American College of Clinical Pharmacy Women’s Health Research and Practice Network.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of University of Georgia (PROJECTxxxx, date).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to subject privacy.
Acknowledgments
The authors acknowledge Hannah Dinh for assistance with creating the survey tool.
Conflicts of Interest
The authors declare no conflict of interest
References
- Finer LB, Zolna MR. Declines in Unintended Pregnancy in the United States, 2008-2011. N Engl J Med. 2016 Mar 3;374(9):843-52. [CrossRef]
- (7) Birth Control Pharmacist. Policies: Pharmacist Prescribing of Hormonal Contraception. Available at: Policies – Birth Control Pharmacist (Accessed on 30 May 2022).
- Landau SC, Tapias MP, McGhee BT 2006. Birth control within reach: A national survey on women’s attitudes toward and interest in pharmacy access to hormonal contraception. Contraception. 2006;74(6):463-470. [CrossRef]
- Landau S, Besinque K, Chung F, Dries-Daffner I, Maderas NM, McGhee BT, Foster DG. Pharmacist interest in and attitudes toward direct pharmacy access to hormonal contraception in the United States. J Am Pharm Assoc (2003). 2009 Jan-Feb;49(1):43-50. [CrossRef]
- Rafie S, El-Ibiary SY. Student pharmacist perspectives on providing pharmacy-access hormonal contraception services. J Am.
- Rafie S, Cieri-Hutcherson NE, Frame TR, Griffin B, Harris JB, Horlen C, Shealy K, Stein AB, Stone RH, Vest K, Westberg S, Yancey AM. Pharmacists’ Perspectives on Prescribing and Expanding Access to Hormonal Contraception in Pharmacies in the United States. J Pharm Pract. 2021 Apr;34(2):230-238. [CrossRef]
- Rikard R, Elliott J, Dalton E, Stone RH. Pharmacist-Prescribed Hormonal Contraception: Does Didactic Hormonal Contraception Education Affect Student Pharmacist Perceptions of This Professional Activity?. Pharmacy (Basel). 2021;9(3):145. Published 2021 Aug 20. [CrossRef]
- Eckhaus LM, Ti AJ, Curtis KM, Stewart-Lynch AL, Whiteman MK. Patient and pharmacist perspectives on pharmacist-prescribed contraception: A systematic review. Contraception. 2021 Feb;103(2):66-74. [CrossRef]
- Seamon GJ, Burke A, Tak CR, Lenell A, Marciniak MW, Scott MA. Role of Pharmacists in Hormonal Contraceptive Access: A Survey of North Carolina Pharmacists. Pharmacy (Basel). 2020;8(4):191. Published 2020 Oct 16. [CrossRef]
- Ingram DD, Franco SJ. 2013 NCHS urban–rural classification scheme for counties. National Center for Health Statistics. Vital Health Stat 2(166). 2014.
- Stone RH, Rafie S, Griffin B, Shealy K, Stein AB. Pharmacist self-perception of readiness to prescribe hormonal contraception and additional training needs. Curr Pharm Teach Learn. 2020;12(1):27-34. [CrossRef]
- Rodriguez MI, McConnell KJ, Swartz J, Edelman AB. Pharmacist prescription of hormonal contraception in Oregon: Baseline knowledge and interest in provision. J Am Pharm Assoc (2003). 2016;56(5):521-526. [CrossRef]
- Rodriguez MI, Herman AM, Espey E, Hersh AR, Bachyrycz AM. Pharmacists’ perspectives and experience prescribing hormonal contraception in rural and urban New Mexico. J Am Pharm Assoc (2003). 2021;61(2):e140-e144. [CrossRef]
- Parry RA, Seamon G, Scott MA, Tak CR. North Carolina Pharmacists’ Support for Hormonal Contraception Prescription Status Change. J Pharm Pract. 2023;36(4):769-776. [CrossRef]
- Newlon JL, Reed JB, Stone RH, Satterfield KG, Meredith AH. Pharmacist-prescribed hormonal contraception services: A systematic review of implementation studies. J Am Coll Clin Pharm. 2022; 5(1): 85-98. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).