1. Introduction
Colorectal cancer (CRC) is the third most common cancer worldwide and the second leading cause of cancer-related deaths [
1]. At diagnosis, approximately 25% of patients present with metastatic disease, with the liver (55%) and peritoneum (25%) being the most frequently involved sites [
2]. Peritoneal involvement is associated with a poor prognosis, with survival times ranging from 5 to 7 months without treatment and extending to 7-16 months with systemic chemotherapy alone.
Over the past thirty years, the use of hyperthermic intraperitoneal chemotherapy (HIPEC) in conjunction with cytoreductive surgery (CRS) has gained traction. This procedure involves removing macroscopically visible disease via CRS to allow optimal penetration of chemotherapeutic agents into the tissue; hyperthermia (41-43°C) enhances the effects of the chemotherapeutics Mitomycin C and Oxaliplatin used in intraperitoneal administration and has a known direct cytotoxic effect [
1]. The introduction of CRS+HIPEC has led to an increase in survival up to 45 months in selected patient groups. Careful selection of patients for this procedure is crucial. Risk factors to consider include the extent of peritoneal disease measured by the Peritoneal Cancer Index (PCI), the completeness of cytoreduction, lymph node status, tumor differentiation and histology of signet-ring cells; recently, mutations in KRAS and BRAF and microsatellite instability (MSI) status also seem to play an emerging role in the stratification and selection of these patients [
3,
4].
However, 8% of patients with advanced CRC present with both liver metastases (LM) and peritoneal metastases (PM). Traditionally, the simultaneous presence of LM and PM was considered a contraindication to surgical treatment. Today, this is no longer an absolute contraindication, although the role of combined surgery remains controversial. According to some studies, combined resection of CRS+HIPEC and liver resection is associated with increased postoperative morbidity [
5,
6,
7] ; in contrast, other studies report no increase in postoperative complications from the addition of concomitant liver resection [
8,
9,
10]. However, there seems to be no difference in the rate of reintervention and postoperative mortality compared with patients undergoing CRS+HIPEC alone [
5,
6]. Several studies have shown that CRS+HIPEC, including resection of liver metastases, can increase the survival of these patients. Careful preoperative assessment of patients combined with a tailored surgical approach (one-step vs. two-step liver surgery, laparoscopic techniques, etc.) is mandatory to achieve an increase in survival without a significant increase in morbidity [
2,
8,
9].
2. Materials and Methods
Our study analyzes 41 patients who underwent liver resection for colorectal cancer metastases at our center between October 2021 and February 2024. Of these, 7 underwent concomitant CRS+HIPEC surgery because they had synchronous liver and peritoneal metastases. We collected patient demographics including sex, age, Charlson Comorbidity Index (CCI), date of surgery, operative time, total length of stay, and metastasis characteristics (number, unilobar/bilobar location, size). The development of postoperative complications was documented and reported using the Clavien-Dindo classification (CD). (
Table 1)
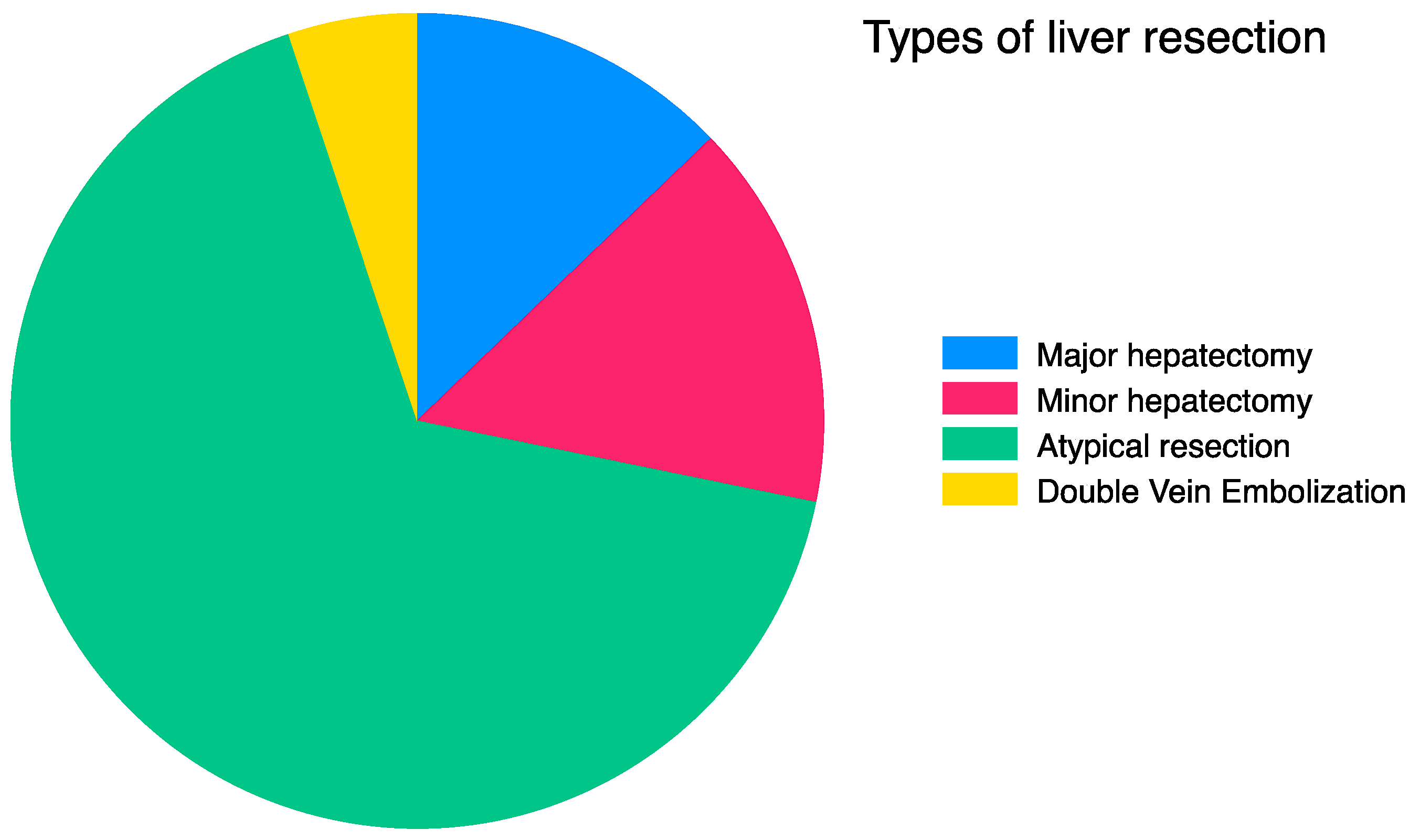
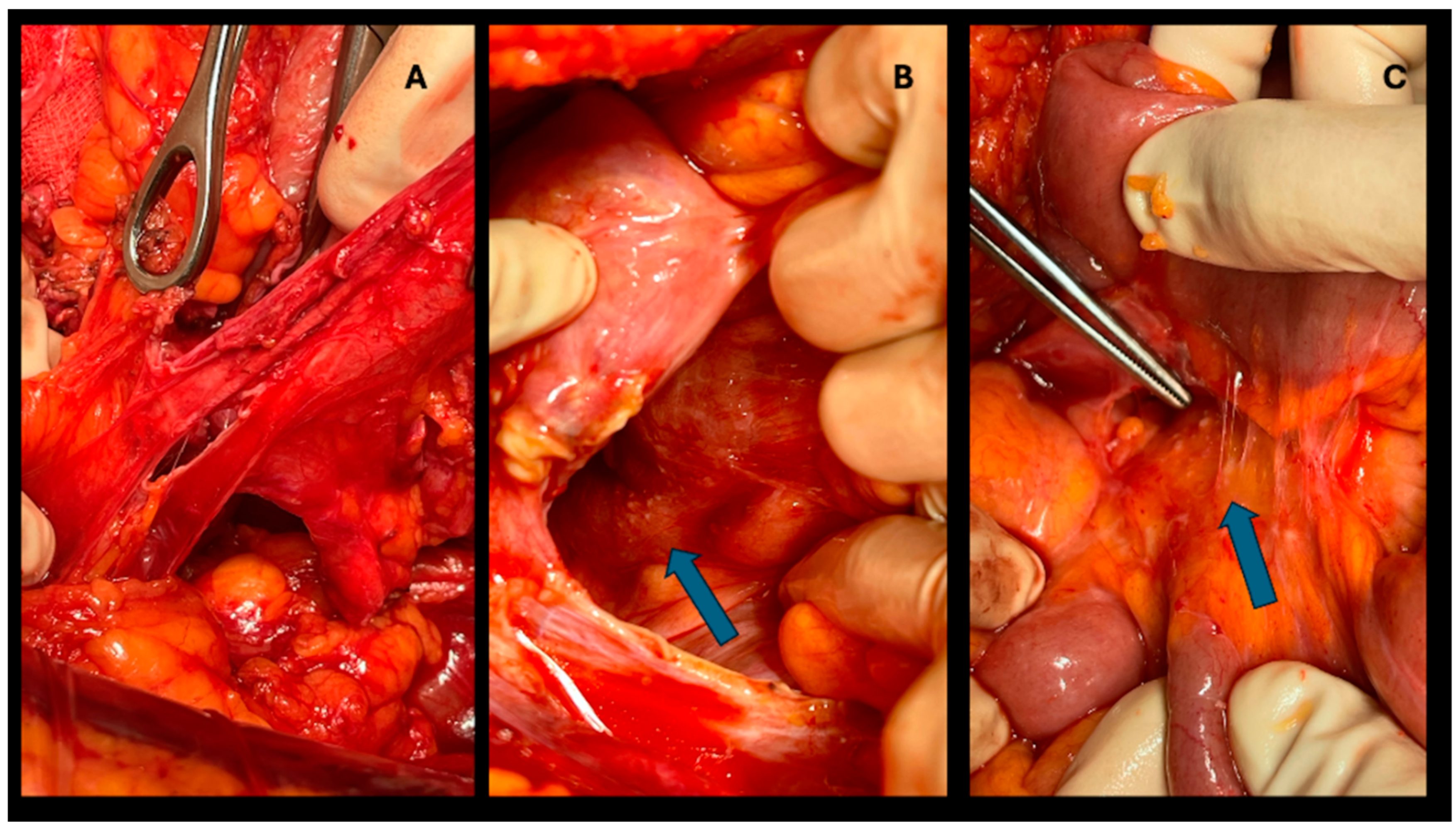
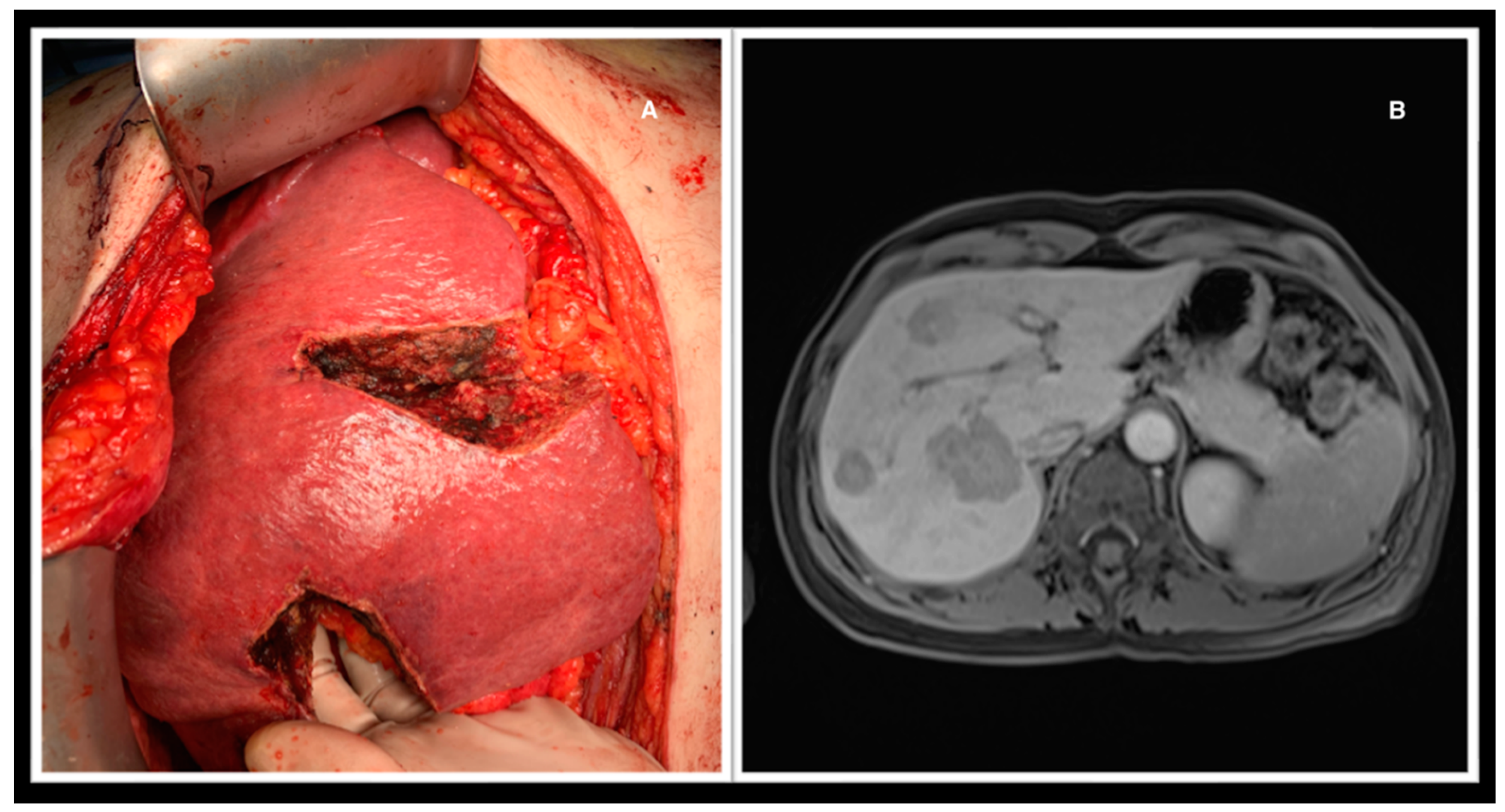
Hepatic resections were all performed in an open setting. The type of surgery to be performed was decided based on imaging examinations (CT, MRI, or both), anatomical complexity, and whether CRS+HIPEC was performed concomitantly. Operations performed included major hepatectomy (three or more liver segments; n=6), minor hepatectomy (less than three segments; n=6), atypical resection (n=26), and double-vein embolization (n=2) [
11]. (
Figure 1) (
Figure 2) (
Figure 3)
Statistical analysis was performed with StataBE18 software. Simple linear regression was used to determine which parameters influenced the development of postoperative complications (as measured by CD), with significance established at p<0.05. Multiple linear regression was then conducted to identify any independent variables affecting the CD outcome, with significance also established at p<0.05. The study was approved by our bioethics committee.
3. Results
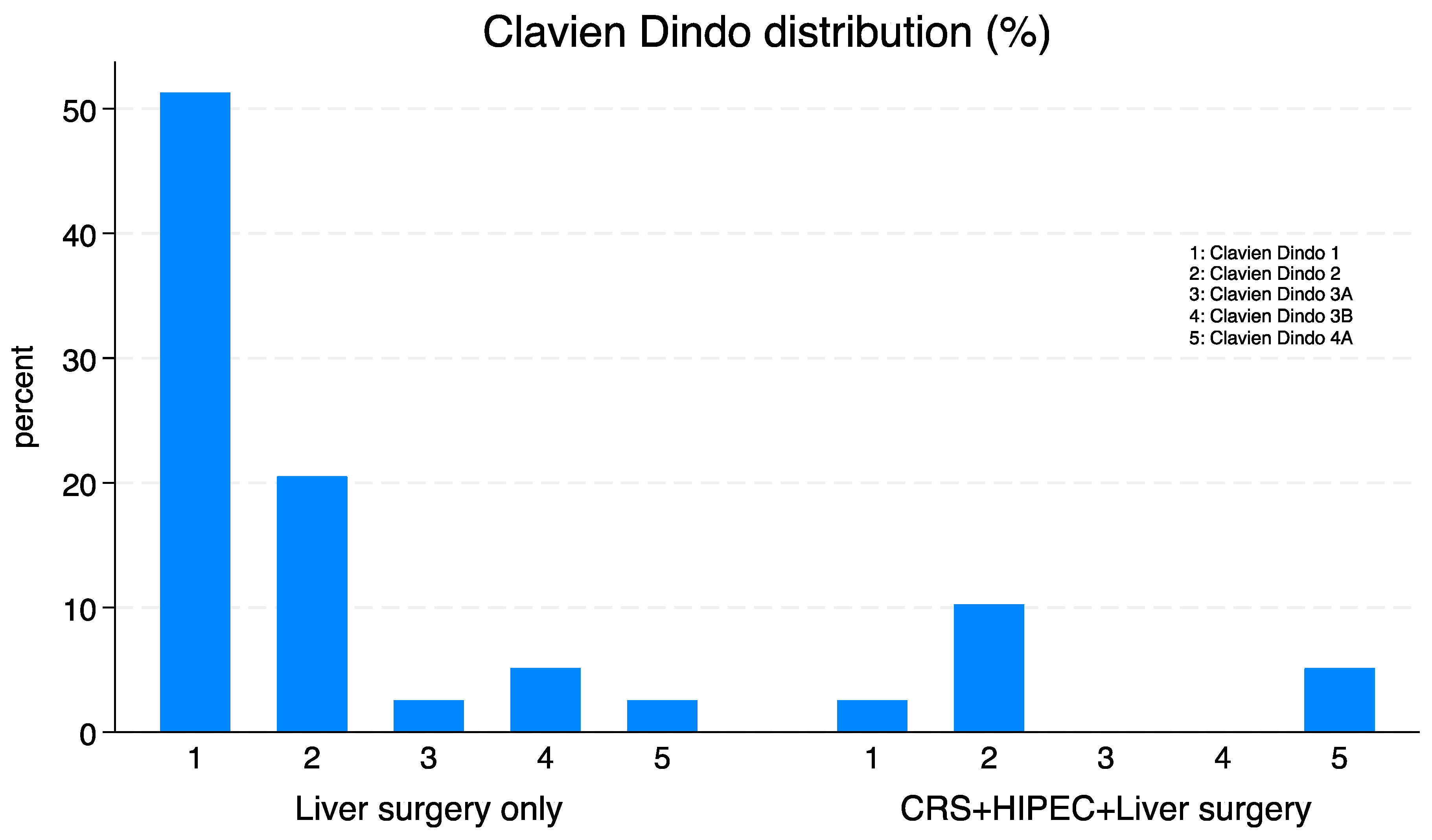
Simple linear regression showed that the CRS+HIPEC procedure, operative time, and length of hospital stay significantly impacted CD outcome (p<0.05). In contrast, the type of liver resection, number and size of metastases, unilobar/bilobar location, and Charlson Comorbidity Index (CCI) were not significant. Multiple linear regression did not identify any independent variables that could influence the CD outcome. (
Table 2) (
Figure 4)
4. Discussion
There is now evidence that the CRS+HIPEC procedure offers a survival advantage in patients with peritoneal metastases from CRC compared with chemotherapy alone, although careful patient selection is necessary [
3]. In recent years, there has been a shift regarding advanced CRC with concomitant peritoneal and liver metastases: liver involvement is no longer considered a contraindication to cytoreduction. Again, patient selection plays a key role in maximizing the benefits and minimizing the risks associated with this procedure [
2,
8,
10]. The issue of perioperative morbidity in patients undergoing CRS+HIPEC and liver resection is controversial: some studies do not show a significant difference between patients treated with combined resection and those with CRS+HIPEC alone, while others suggest it is a therapeutic alternative with increased risk of postoperative complications; some studies advocate a two-step approach with a liver-first strategy to limit disease progression between surgeries [
2,
8,
9,
10] . Our study shows that the CRS+HIPEC procedure, operative time, and total length of stay influence the development of complications in the immediate postoperative period, whereas the addition of different types of liver resection does not significantly impact this outcome. Many factors likely contribute to the development of postoperative complications, which could not be accounted for due to the limited number of patients in the study. The performance of combined resection must be carefully tailored to the individual patient. Moreover, this approach requires thorough preoperative evaluation and should be performed in specialized centers, involving a multidisciplinary team of peritoneal neoplasm specialists, hepatobiliary surgeons, radiologists, oncologists and anatomic pathologists. This multidisciplinary approach is essential to achieving a survival advantage without a significant increase in morbidity.
Author Contributions
Writing – original draft: O.C.; data curation: O.C.; methodology: all authors; supervision: A.L., M.MA.; validation: M.MA.; writing – review and editing: M.MA.; project administration: M.MA.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- van Stein, R.M.; Aalbers, A.G.J.; Sonke, G.S.; van Driel, W.J. Hyperthermic Intraperitoneal Chemotherapy for Ovarian and Colorectal Cancer: A Review. JAMA Oncol. 2021, 7, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Di Carlo, S.; Cavallaro, G.; La Rovere, F.; Usai, V.; Siragusa, L.; Izzo, P.; et al. Synchronous liver and peritoneal metastases from colorectal cancer: Is cytoreductive surgery and hyperthermic intraperitoneal chemotherapy combined with liver resection a feasible option? Front Surg. 2022, 9, 1006591. [Google Scholar] [CrossRef] [PubMed]
- Tonello, M.; Baratti, D.; Sammartino, P.; Di Giorgio, A.; Robella, M.; Sassaroli, C.; et al. Microsatellite and RAS/RAF Mutational Status as Prognostic Factors in Colorectal Peritoneal Metastases Treated with Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy (HIPEC). Ann Surg Oncol. 2022, 29, 3405–3417. [Google Scholar] [CrossRef] [PubMed]
- Qin, R.X.; Lim, J.H.; Ly, J.; Fischer, J.; Smith, N.; Karalus, M.; et al. Long-term survival following cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in Waikato, Aotearoa New Zealand: a 12-year experience. ANZ J Surg. 2024, 94, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Polderdijk, M.C.E.; Brouwer, M.; Haverkamp, L.; Ziesemer, K.A.; Tenhagen, M.; Boerma, D.; et al. Outcomes of Combined Peritoneal and Local Treatment for Patients with Peritoneal and Limited Liver Metastases of Colorectal Origin: A Systematic Review and Meta-Analysis. Ann Surg Oncol. 2022, 29, 1952–1962. [Google Scholar] [CrossRef] [PubMed]
- Morales-Soriano, R.; Pineño-Flores, C.; Morón-Canis, J.M.; Molina-Romero, F.J.; Rodriguez-Pino, J.C.; Loyola-Miró, J.; et al. Simultaneous Surgical Approach with Hyperthermic Intraperitoneal Chemotherapy (HIPEC) in Patients with Concurrent Peritoneal and Liver Metastases of Colon Cancer Origin. J Clin Med. 2023, 12. [Google Scholar] [CrossRef] [PubMed]
- Cloyd, J.M.; Abdel-Misih, S.; Hays, J.; Dillhoff, M.E.; Pawlik, T.M.; Schmidt, C. Impact of Synchronous Liver Resection on the Perioperative Outcomes of Patients Undergoing CRS-HIPEC. J Gastrointest Surg. 2018, 22, 1576–1584. [Google Scholar] [CrossRef] [PubMed]
- Lo Dico, R.; Faron, M.; Yonemura, Y.; Glehen, O.; Pocard, M.; Sardi, A.; et al. Combined liver resection and cytoreductive surgery with HIPEC for metastatic colorectal cancer: Results of a worldwide analysis of 565 patients from the Peritoneal Surface Oncology Group International (PSOGI). Eur J Surg Oncol. 2021, 47, 89–100. [Google Scholar] [CrossRef] [PubMed]
- Berger, Y.; Aycart, S.; Tabrizian, P.; Agmon, Y.; Mandeli, J.; Heskel, M.; et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy in patients with liver involvement. J Surg Oncol. 2016, 113, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Randle, R.W.; Doud, A.N.; Levine, E.A.; Clark, C.J.; Swett, K.R.; Shen, P.; et al. Peritoneal surface disease with synchronous hepatic involvement treated with Cytoreductive Surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). Ann Surg Oncol. 2015, 22, 1634–1638. [Google Scholar] [CrossRef] [PubMed]
- Korenblik, R.; Heil, J.; Smits, J.; James, S.; Olij, B.; Bechstein, W.O.; et al. Liver regeneration after portal and hepatic vein embolization improves overall survival compared with portal vein embolization alone: mid-term survival analysis of the multicentre DRAGON 0 cohort. Br J Surg. 2024, 111. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).