Submitted:
02 August 2024
Posted:
05 August 2024
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brown JS, Amend SR, Austin RH, Gatenby RA, Hammarlund EU, Pienta KJ. Updating the definition of cancer. Mol Cancer Res. 2023;21(11):1142–7. [CrossRef]
- Ruiz de la Hermosa García-Pardo A, Rodríguez Maldonado Y, Martínez Savoini E, Gómez de Antonio R, Allo Miguel G, Garcia Alonso FJ, et al. Estudio prospectivo sobre las complicaciones de los estomas digestivos. Revista de Gastroenterología del Perú. 2019;39(3):215–21. Avaliable at: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1022-51292019000300003.
- Goodman W, Allsop M, Downing A, Munro J, Taylor C, Hubbard G, et al. A systematic review and meta-analysis of the effectiveness of self-management interventions in people with a stoma. J Adv Nurs. 2022;78(3):722–38. [CrossRef]
- Liu X-J, Han J, Su X. Influence of continuous nursing on surgical site wound infection and postoperative complication for colorectal cancer patients with stoma: A meta-analysis. Int Wound J. 2023;. [CrossRef]
- Domínguez-Santamaría JM. Ostomías. In Book Manual Práctico de Enfermería Comunitaria, 2nd ed.; Martínez-Riera JR & Del Pino-Casado JM. Eds.; Elsevier: Barcelona, Spain, 2014; pp. 489–498.
- Lai E, Peterson AC, Liu G, Karimuddin A, Crump RT, Sutherland JM. Psychometric validation of the Stoma-QOL questionnaire in a Canadian cross-sectional sample of colostomy and ileostomy patients. Scand J Gastroenterol. 2018;53(6):721–6. [CrossRef]
- Zewude WC, Derese T, Suga Y, Teklewold B. Quality of life in patients living with stoma. Ethiopian Journal of Health Sciences. 2021;31(5):993. [CrossRef]
- Liao C, Qin Y. Factors associated with stoma quality of life among stoma patients. Int J Nurs Sci. 2014;1(2):196–201. [CrossRef]
- Post MWM. Definitions of quality of life: what has happened and how to move on. Top Spinal Cord Inj Rehabil. 2014;20(3):167–80. [CrossRef]
- Kovoor JG, Jacobsen JHW, Stretton B, Bacchi S, Gupta AK, Claridge B, et al. Depression after stoma surgery: a systematic review and meta-analysis. BMC Psychiatry. 2023;23(1):352. [CrossRef]
- Escalante Y. Actividad física, ejercicio físico y condición física en el ámbito de la salud pública. Rev Esp Salud Publica. 2011;85(4):325–8. [CrossRef]
- Doege J, Ayres JM, Mackay MJ, Tarakemeh A, Brown SM, Vopat BG, et al. Defining return to sport: A systematic review. Orthop J Sports Med. 2021;9(7):23259671211009589. [CrossRef]
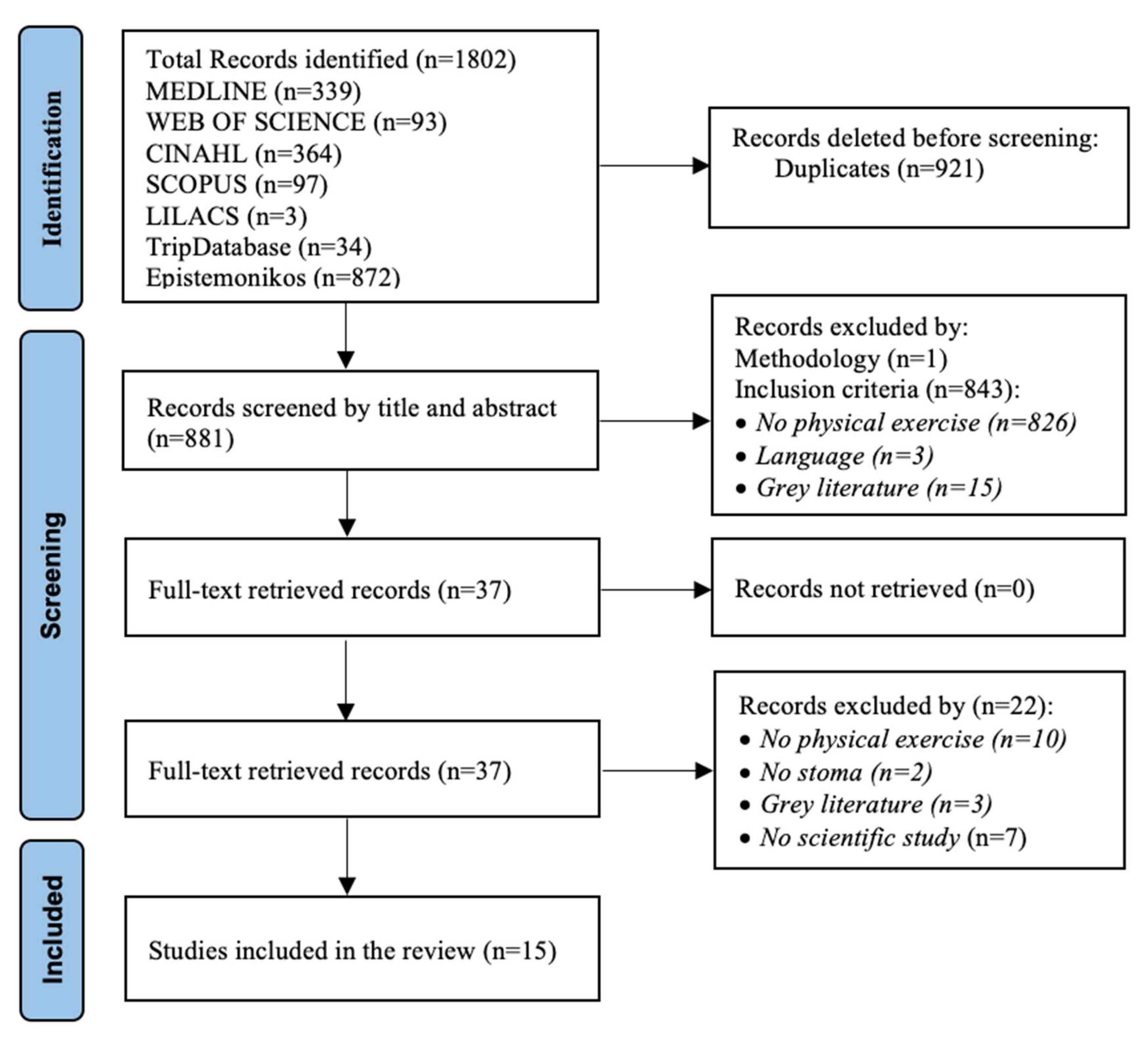
- Tricco A, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467-473. [CrossRef]
- Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, et al. PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev. 2021;10(1):39. [CrossRef]
- Park J, Rivard SJ, Maguire L, Varlamos C, Duby A, Hendren S. Parastomal hernia rates and exercise after ostomy surgery. Dis Colon Rectum. 2023;66(6):823–30. [CrossRef]
- Goodman W, Downing A, Allsop M, Munro J, Taylor C, Hubbard G, et al. Quality of life profiles and their association with clinical and demographic characteristics and physical activity in people with a stoma: a latent profile analysis. Qual Life Res. 2022;31(8):2435–44. [CrossRef]
- Krogsgaard M, Andersen RM, Danielsen AK, Thomsen T, Klausen TW, Christensen BM, et al. Physical activity after colorectal cancer surgery-a cross sectional study of patients with a long-term stoma. Support Care Cancer. 2022;30(1):555–65. [CrossRef]
- Mo J, Thomson CA, Sun V, Wendel CS, Hornbrook MC, Weinstein RS, et al. Healthy behaviors are associated with positive outcomes for cancer survivors with ostomies: a cross-sectional study. J Cancer Surviv. 2021;15(3):461–9. [CrossRef]
- Saunders S, Brunet J. A qualitative study exploring what it takes to be physically active with a stoma after surgery for rectal cancer. Support Care Cancer. 2019;27(4):1481–9. [CrossRef]
- Lowe BG, Alsaleh E, Blake H. Assessing physical activity levels in people living with a stoma. Nurs Stand. 2019;35(1):70–7. [CrossRef]
- Kindred MM, Pinto BM, Dunsiger SI. Association of body esteem with fitness and body fat among colorectal cancer survivors: Secondary analyses from a randomized trial. Int J Behav Med. 2019;26(6):619–28. [CrossRef]
- Russell S. Parastomal hernia and physical activity. Are patients getting the right advice? Br J Nurs. 2017;26(17):S12–8. [CrossRef]
- Russell S. Physical activity and exercise after stoma surgery: overcoming the barriers. Br J Nurs. 2017;26(5):S20–6. [CrossRef]
- Krouse RS, Wendel CS, Garcia DO, Grant M, Temple LKF, Going SB, et al. Physical activity, bowel function, and quality of life among rectal cancer survivors. Qual Life Res. 2017;26(11):3131–42. [CrossRef]
- Wiskemann J, Schommer K, Jaeger D, Scharhag-Rosenberger F. Exercise and cancer: Return to work as a firefighter with ostomy after rectal carcinoma – a case report. Medicine (Baltimore). 2016;95(29):e4309. [CrossRef]
- Sica J, Stebbing J. Inspiring confidence: helping a young ostomate return to sport. Gastrointest Nurs. 2016;14(4):16–20. [CrossRef]
- Anderson AS, Steele R, Coyle J. Lifestyle issues for colorectal cancer survivors--perceived needs, beliefs and opportunities. Support Care Cancer. 2013;21(1):35–42. [CrossRef]
- Courneya KS, Friedenreich CM, Arthur K, Bobick TM. Physical exercise and quality of life in postsurgical colorectal cancer patients. Psychol Health Med. 1999;4(2):181–7. [CrossRef]
- Isaacs P. Marathon without a colon: salt and water balance in endurance running ileostomates. Br J Sports Med. 1984;18(4):295–300. [CrossRef]
- Marrero-González CM, Pérez-Herrera A, García-Hernández AM. La sexualidad cuando se porta una ostomía. Una revisión de los estudios cualitativos entre 2012 y 2022. Ene. 2023;17(1). Available at: https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1988-348X2023000100006.
- Tao H, Songwathana P, Isaramalai SA, Zhang Y. Personal awareness and behavioural choices on having a stoma: a qualitative metasynthesis. J Clin Nurs. 2014;23(9-10):1186-1200. [CrossRef]
- Ding D, Nguyen B, Gebel K, Bauman A, Bero L. Duplicate and salami publication: a prevalence study of journal policies. Int J Epidemiol. 2020;49(1):281-288. [CrossRef]
- Niu N, Du S, Yang D, et al. Risk factors for the development of a parastomal hernia in patients with enterostomy: a systematic review and meta-analysis. Int J Colorectal Dis. 2022;37(3):507-519. [CrossRef]
- Manole TE, Daniel I, Alexandra B, Dan PN, Andronic O. Risk Factors for the Development of Parastomal Hernia: A Narrative Review. Saudi J Med Med Sci. 2023;11(3):187-192. [CrossRef]
- Munro J, Goodman W, Oliphant R, et al. Hernia Active Living Trial (HALT): a feasibility study of a physical activity intervention for people with a bowel stoma who have a parastomal hernia/bulge. Pilot Feasibility Stud. 2023;9(1):111. [CrossRef]
- Taylor C, Munro J, Goodman W, et al. Hernia Active Living Trial (HALT): an exercise intervention in people with a parastomal hernia or bulge. Br J Nurs. 2023;32(22):S4-S11. [CrossRef]
- Krogsgaard M, Thomsen T, Vinther A, Gögenur I, Kaldan G, Danielsen AK. Living with a parastomal bulge - patients’ experiences of symptoms. J Clin Nurs. 2017;26(23-24):5072-5081. [CrossRef]
- Borglit T, Krogsgaard M, Theisen SZ, Juel Rothmann M. Assessment of a support garment in parastomal bulging from a patient perspective: a qualitative study. Int J Qual Stud Health Well-being. 2022;17(1):2039428. [CrossRef]
- Munro J, Hubbard G, Goodman W, Beeken R, Oliphant R. Lived Experience of Parastomal Bulging: A Mixed Methods Study. J Abdom Wall Surg. 2024;3:12478. [CrossRef]
| Date Database |
Search Strategies |
|---|---|
| 2023 October 30 Medline |
((((((((“Surgical Stomas”[Mesh] OR “Stoma, Surgical” OR “Stomata, Surgical” OR “Surgical Stomata” OR “Stomas, Surgical”) OR (“Ostomy”[Mesh] OR “Ostomies”)) OR (“Colostomy”[Mesh] OR “Colostomies”)) OR (“Ileostomy”[Mesh] OR “Ileostomies” OR “Tube Ileostomy” OR “Ileostomies, Tube” OR “Ileostomy, Tube” OR “Tube Ileostomies” OR “Incontinent Ileostomy” OR “Ileostomies, Incontinent” OR “Ileostomy, Incontinent” OR “Incontinent Ileostomies” OR “Loop Ileostomy” OR “Ileostomies, Loop” OR “Ileostomy, Loop” OR “Loop Ileostomies” OR “Continent Ileostomy” OR “Continent Ileostomies” OR “Ileostomies, Continent” OR “Ileostomy, Continent”)) OR (“Enterostomy”[Mesh] OR “Enterostomies”)) OR (“Cecostomy”[Mesh] OR “Cecostomies” OR “Tube Cecostomy” OR “Cecostomies, Tube” OR “Cecostomy, Tube” OR “Tube Cecostomies”)) OR (“Duodenostomy”[Mesh] OR “Duodenostomies”)) OR (“Jejunostomy”[Mesh] OR “Jejunostomies”)) AND (((“Sports”[Mesh] OR “Sport” OR “Athletics” OR “Athletic”) OR (“Exercise”[Mesh] OR “Exercises” OR “Physical Activity” OR “Activities, Physical” OR “Activity, Physical” OR “Physical Activities” OR “Exercise, Physical” OR “Physical Exercise” OR “Physical Exercises” OR “Acute Exercise” or “Acute Exercises” OR “Exercise, Acute” OR “Exercises, Acute” OR “Exercise, Isometric” OR “Exercises, Isometric” OR “Isometric Exercises” OR “Isometric Exercise” OR “Exercise, Aerobic” OR “Aerobic Exercise” OR “Aerobic Exercises” OR “Exercises, Aerobic” OR “Exercise Training” OR “Exercise Trainings” OR “Training, Exercise” OR “Trainings, Exercise”)) OR (“Return to Sport”[Mesh] OR “Return to Sports” OR “Sport, Return to” OR “Sports, Return to” OR “to Sport, Return” OR “to Sports, Return” OR “Return to Play” OR “Play, Return to” OR “to Play, Return” OR “Return to Sporting Activities” OR “Resumption of Sporting Activity” OR “Activity Resumption, Sporting” OR “Activity Resumptions, Sporting” OR “Sporting Activity Resumption” OR “Sporting Activity Resumptions” OR “Resumption of Recreational Activities” OR “Activities Resumption, Recreational” OR “Activities Resumptions, Recreational” OR “Recreational Activities Resumption” OR “Recreational Activities Resumptions” OR “Return to Recreational Activities”)) |
| 2023 November 9 Scopus |
(INDEXTERMS (“Surgical stomas”) OR INDEXTERMS (“Colostomy”) OR INDEXTERMS (“Ileostomy”) OR INDEXTERMS (“Peritoneal Stomata”)) AND (INDEXTERMS (“Exercise”) OR INDEXTERMS (“Return to Sports”) OR INDEXTERMS (“Return to Sports”)) |
| 2023 November 13 Web of Science |
TS=(“Surgical Stomas” OR “Colostomy” OR “Ileostomy” OR “Peritoneal Stomata”) AND TS=(“Return to Sports” OR “Return to Sport” OR “Exercise”) |
| 2023 November 13 Cinahl |
TX (“Surgical Stomas” OR “Colostomy” OR “Ileostomy” OR “Peritoneal stomata”) AND TX (“Return to Sport” OR “Exercise”) |
| 2023 November 13 Lilacs |
(“ESTOMA QUIRURGICO”) [Palabras] or (“ESTOMA”) or (“COLOSTOMIA”) [Palabras] and (“EJERCICIO”) or (“DEPORTE/ACTIVIDAD”) or (“EJERCICIO FISICO”) [Palabras] |
| 2024 March 16 TripDatabase |
((return AND to AND sport AND exercise AND surgical AND stomas)) |
| 2024 March 16 Epistemonikos |
(title:(exercise) OR abstract:(exercise)) OR (title:(“return to sport”) OR abstract:(“return to sport”)) AND (title:(“surgical stomas”) OR abstract:(“surgical stomas”)) OR (title:(Colostomy) OR abstract:(Colostomy)) OR (title:(ileostomy) OR abstract:(ileostomy)) OR (title:(“peritoneal stomata”) OR abstract:(“peritoneal stomata”)) |
| Author (year); Design; Country |
Aim | Conclusions | JBI1 Qualityitems (%) |
|---|---|---|---|
| Park et al. (2023) Cross-sectional; USA [15] |
To determine rates and risk factors for parastomal hernias in patients with permanent ostomies | Parastomal hernia rates remain high in current surgical practice. There is an association between PA2 and the presence of parastomal hernia, with a higher rate among those who exercise less | 5/8 (62.5) |
| Goodman et al. (2022) Cross-sectional; UK [16] |
To identify subgroups in the QoL3 of people with stomas. To assess whether belonging to these groups is associated with demographic, clinical and PA characteristics | Some latent profiles associated with demographic and clinical variables were identified, but additional variables should be identified in the future to provide the basis for targeting and tailoring future interventions to specific subgroups of people with a stoma | 5/8 (62.5) |
| Krogsgaard et al. (2022) Cross-sectional; Germany [17] |
To examine the level of PA and explore factors influencing PA in cancer survivors with a stoma | Half of patients met or exceeded the guideline recommendations. Of the patients who did not meet the recommendations, some could meet them by slightly increasing moderate or vigorous activity | 8/8 (100) |
| Mo et al. (2021) Cross-sectional; USA [18] |
To describe lifestyle behaviors and their relationships with health-related QoL in cancer survivors with ostomies | Improved QoL is associated with adherence to PA guidelines among cancer survivors with ostomies. Results have clinical relevance for ostomy self-care and establishing lifestyle recommendations | 8/8 (100) |
| Saunders & Brunet (2019) Qualitative; Germany [19] |
To explore the experiences of rectal cancer survivors with a stoma and the impact on their engagement in PA | The stories provided experiences related to cancer and the stoma, highlighting reasons for and barriers to PA. The results helped to identify useful strategies for those learning to be physically active with a stoma | 7/9 (77.7) |
| Lowe, Alsaleh & Blake (2019) Cross-sectional; UK [20] |
To assess PA levels in adults with a stoma. To investigate the relationship between activity levels, exercise self-efficacy, perceived benefits and barriers to exercise, depression, body image and stoma-related QoL | Most participants were physically inactive. Interventions that reduce barriers to exercise and support self-efficacy in people with stoma may help them increase their PA levels, as well as reduce the risk of chronic diseases associated with sedentary lifestyles | 8/8 (100) |
| Kindred et al. (2019) RCT; USA [21] |
To examine the relationship between changes in fitness and body fatness with changes in body esteem among colorectal cancer survivors after testing the effects of a PA intervention | Improving physical fitness and body composition may enhance self-esteem among these cancer survivors; however, there are differences according to gender and stage of disease | 11/13 (84.6) |
| Russell (2017) Cross-sectional; UK [22] |
To investigate the physical health and well-being of people living with stomas in the UK | There are gaps in care regarding advice on PA, abdominal exercises and prevention and treatment of stoma hernias. More research and training for patients and healthcare professionals is needed | 2/8 (25) |
| Russell (2017) Cross-sectional; UK [23] |
To investigate the physical health and well-being of people living with stomas in the UK | PA levels drop significantly after stoma surgery; the vast majority of people living with a stoma do not meet PA guidelines. Those diagnosed with cancer or parastomal hernia are even less active | 2/8 (25) |
| Krouse et al. (2017) Cross-sectional; USA [24] |
To examine the relationships between PA, health-related QoL and bowel function in rectal cancer survivors | Meeting or exceeding PA guidelines was associated with increased QoL. The results suggest that women may benefit from increased PA, while men with ostomies may face challenges that require further study. There is a need to identify PA strategies that improve compliance and benefits in patients | 8/8 (100) |
| Wiskemann et al. (2016) Case report; Germany [25] |
To report on how a firefighter with rectal carcinoma and an ostomy was trained to recover fitness for work | Colorectal cancer survivors with ostomies may be able to recover fitness for demanding physical tasks, such as firefighting, through an individualized and supervised training programme | 8/8 (100) |
| Sica (2016) Case report; UK [26] |
Not reported | Having a stoma and recovering from major surgery can be a challenging and lengthy process. Finding the right pouching system is an integral part of recovery and can help give you the confidence to start resuming previous activities, including sport | 5/8 (62.5) |
| Anderson et al. (2013) Qualitative; UK [27] |
To explore perceived needs for advice on diet, activity and beliefs about the role of lifestyle in reducing disease recurrence | Lifestyle changes can lead to perceived blame and stigmatization. Personalized, evidence-based counselling on lifestyle choices appears to be a much-needed part of care planning and should be incorporated into survivorship programmes | 7/9 (77.7) |
| Courneya et al. (1999) Cohortes; Canada [28] |
To examine the relationship between physical exercise and QoL in patients with colorectal cancer | Small changes in exercise from pre-diagnosis to post-surgery are positively associated with QoL in patients with colorectal cancer, but experimental research is needed before definitive conclusions can be drawn | 5/11 (45.4) |
| Isaacs (1984) Case series; UK [29] |
To detail fluid and electrolyte balance data in a team of ileostomized marathon runners who regularly run long distances | Healthy ileostomates after adequate training are successful marathoners, but the prevalence of a slight depletion in sodium level in ileostomates suggests that it may also be advisable for them to take glucose or electrolyte solutions when competing at any ambient temperature or when preparing for a marathon in hot environments | 6/10 (60) |
| 1 JBI: Joanna Briggs Institute; 2 PA: Physical Activity; 3 QoL: Quality of Life | |||
| Author (year) Design |
N (Type of stoma) Data collection |
Themes and Sub-themes |
|---|---|---|
| Saunders & Brunet (2019) [19] Qualitative (No specified approach) |
N=15 (Not specified) Semi-structured interviews |
Themes: Reasons for physical activity Sub-themes: Fun, health benefits (mental and physical), sense of accomplishment, weight control, sense of normalcy, taking time for themselves away from daily responsibilities |
|
Themes: Physical activity discourages Sub-themes: Negative side effects of cancer and treatments, uncertainty in unfamiliar environments, physical restrictions, fear of injury, unclear orientation, stoma, shyness in public and private, negative previous experiences | ||
|
Themes: Implications for practice Sub-themes: Social support and support networks, counseling, previous experiences, experimentation, safe environment, skills and confidence | ||
| Anderson et al. (2013) [27] Qualitative (No specified approach) |
N=40 (Not Specified) 6 focal groups |
Themes: Beliefs about the role of diet, physical activity and lifestyle in reducing long-term disease risk |
| Themes: Health maintenance actions | ||
| Themes: Interest in receiving guidance on diet, activity and lifestyle to reduce risk and disease progression | ||
| Themes: What are the forms, schedules and modes of guidance on nutrition, physical activity and lifestyle? |
| Author (year); Design |
Stoma type. Patient characteristics |
Case results |
|---|---|---|
| Wiskemann et al. (2016) Case report; Germany [25] |
Permanent colostomy. Male, 44-years-old. Rectal adenocarcinoma. Firefighter. Performed aerobic exercise (running, swimming, rowing) and resistance (weight training with weights and machines). Since the diagnosis has been inactive. To return to work must pass ergometric tests. Training program, 9 months: 0-2 preparation: 1.3 sessions/week. 2-4 supervised individual training: 2.3 sessions/week. 4-6: group training: 3 sessions/week 6-9: autonomous training. |
European Organization of Research and Treatment in Cancer Questionnaire about Quality of Life 30 (EORTC QoL 30): Score: 66.67. Pain and diarrhea decreased 50%, insomnia and loss of appetite disappeared stool control at 9 months. Subscales showed reduction of fatigue (30% mental fatigue, 64% physical fatigue) during first 4 months of training. Distress was reduced 50% at 9 months. At baseline, 6 physical problems (pain, fatigue, sleep, dry/itchy skin, dry/obstructed nose and sexual problems), 2 emotional problems (worries, sadness) and 1 family problem (partner). At 9 months, only 2 problems remained in the physical section (indigestion, dryness and nasal obstruction). |
| Sica (2016) [26] Case report |
Ileostomy. Woman, 28-year-old. Symptoms began while she was studying at university to become an elementary school teacher. Prior to surgery, she danced jazz, street and contemporary dance. After the stoma, decided to take up running and currently attends classes at a local gym. |
Back to the sport: When started to get her strength back, she began trying different classes at a local gym. Although she feels good, she tries to do the exercises in the least harmful way possible. |
| Isaacs (1984) [29] Case series |
Ileostomy. Five men aged 22, 37, 40, 42, 56 and 56 with colostomy or ileostomy for ulcerative colitis participated in the 1983 London Marathon. Questionnaires about their ileostomy function, diet, training program, and experience. In each subject, urine and ileostomy secretions data were collected 3-4 hours before the race and 5-6 hours after on calibrated scales. Before, they were weighed with running equipment, blood pressure and obtained heart rate and venous blood specimen. Procedure repeated within 5 minutes of the end of the race. |
Weight loss: Between 1-3 kg. Ileostomy flow: The ileostomy discharged volume and sodium concentration showed no change during the race, but potassium concentration increased in contrast to the unchanged urine. Total water and potassium losses during the race were minimum. Plasma biochemistry: Sodium levels lower. Urea and total protein higher compared to non-ostomized runners. After the race, increased blood urea, uric acid and bilirubin occurred in all subjects. |
| Author (year) Design |
Sample size (N) Type of stoma PA1 |
Instruments | Statistical data |
|---|---|---|---|
| Park et al. (2023) [15] Cross-sectional |
N=443 Male: n=266; 61.9%; Female: n=165; 37.9%; Non-binary n=1; 0.2%. Urostomy: n=212; 47.9%; Colostomy: n=132; 36.1%; Ileostomy: n=99; 22.3% Parastomal hernia: No: n=327; 75.3%; Yes: n=129; 29.3% PA: Not reported |
QoL2: QoL scale: Dimensions: 4; Reliability: Not reported; Likert scale: 4 items. PA: International PA Questionnaire Short Form: Reliability: Not reported; Measure expressed in metabolic equivalents (MET minutes/week). |
QoL: QoL scale: Total Lower if hernia (U=11.99; p=0.004). PA: International PA Questionnaire Short Form: PA: U=8154; Mean=579 (yes hernia) vs. 1689 (no hernia) p=0.001. Correlation between PA intensity and time after ostomy making (r=0.009; p=0.870). |
| Goodman et al. (2022) [16] Cross-sectional |
N=1528 Male: n=289; 20.4%; Female: n=1122; 79.1%; Miss sex: n=8; 0.6% Ileostomy: n=956; 67.7%; Colostomy: n=444; 31.3%; Miss stoma: n=19; 1.3% PA: Not reported (number of days with exercise of 30 minutes or more on which the respiratory rate increased should be noted). |
QoL: Stoma Quality of Life (SQoL): 19 items in 5 subscales (Work/social function; Sexuality and body image; Stoma function; Economic concerns; Skin irritation). Likert scale: 5 items. Score: 0 (never) - 100 (always). Reliability (α=0.89). PA: (additional item): number of days with increased Respiratory Frequency (Range: 0-7). |
QoL: SQoL [Mean (SD3)]: Work/social function: 63.6 (23.0); Sexuality and body image: 61.5 (19.3); Stoma function: 52.8 (20.6); Financial concerns: 81.3 (28.5); Skin irritation: 47.2 (27.9). PA: (days/week): Mean=2.6 (SD=2.3). 4 profiles according to SQoL responses: Profile 1: Good QoL (n=891; 62.8%); Profile 2: Some problems with QoL (n=184; 13.0%); Profile 3 Low QoL (n=181; 12.8%); Profile 4: Financial concerns (n=163; 11.5%). Individuals classified in Profile 3 were less able to stoma for more than 2 years (OR: 0.65; 95% CI: 0.43-0.96; p<0.05) and spend more days physically active (OR: 0.85; 95% CI: 0.78, 0.94; p<0.05), but were more likely to hernia (OR: 3.32; 95% CI: 2.17-5.07; p<0.05). |
| Krogsgaard et al. (2022) [17] Cross-sectional |
N=571 Colorectal cancer and stoma in Denmark Colostomy: n=491; 86%; Ileostomy: n=80; 14% PA: Not reported |
QoL: Colostomy Impact Score: (ad hoc scale) PROMIS items: 7 (odor, leakage, stool consistency, stoma site pain, skin problems, parasternal bulging, help with stoma management) Likert scale: not reported; Score: higher score more complications; Reliability: not reported. PA: Compliant (Active, Very active). Non-compliant (Inactive, Insufficiently active). |
QoL: Colostomy Impact Score: n=313 (55%) higher impact of colostomy on PA; n=358 (45%) lower impact of colostomy on PA. No association between colostomy impact and level of PA (OR: 1.59; 95% CI: 1.02-2.11). PA: Compliers (n=293; 51%): active n=108; 36.86%; very active n=185; 63.13%; >300 minutes n=76; 41%; >151 minutes n=59; 55%; >120 minutes n=69; 37%; 60-120 minutes n=36; 33%. Non-compliers (n=278; 49%): Inactive n=44; 15.8%; Insufficient active n=234; 84.17%; <30-150 minutes n=170; 73%; <59 minutes n=55; 24%. |
| Mo et al. (2021) [18] Cross-sectional |
N=200 Male: 108 (54%); Female: 92 (46%) Colostomy: n=87; 43.5%; Ileostomy: n=46; 23%; Urostomy: n=67; 33.5% PA: Exercise Time recommendation according to intensity: 150 minutes per week if moderate. 75 minutes per week if vigorous. |
QoL: City of Hope Quality of Life Ostomy (COH-QoL-O) (ad hoc questionnaire): Items (no scale) on diet: 8 general diet (high protein, low carbohydrate, fast food, diabetic, vegetarian, vegan, vegan, heart-healthy, no special diet); 5 broad diet (fast food, vegetarian/vegan, therapeutic/health-promoting, gastrointestinal symptom modulating, and no special diet) and a scale with 43 items Health-Related QoL with Likert scale not reported Score: 0 (worst QoL) - 10 (best QoL). Reliability: not reported PA: Self-Efficacy (SE) to Perfom Self-Management Behaviors (ad hoc questionnaire): from the instrument (Godin Leisure-Time Exercise Questionnaire), contains 3 unscaled parts. 2 Items: “How confident do you feel you can perform gentle exercises for muscle strength and flexibility three to four times per week (range of motion, use of weights, etc.)?” and “How confident do you feel you can perform aerobic exercises such as walking, swimming or cycling three to four times per week?”. Likert scale: not reported. Score: 1 (not at all confident) - 10 (totally confident); Reliability: (α=0.83). Ad hoc questionnaire: One question with three parts on different PA intensities. Frequency and intensity of PA for one week. Measures: light (minimal exertion, no sweating), moderate (not strenuous, light sweating) and vigorous (heart beating fast, intense sweating). |
QoL: COH-QoL-O: Those who met or exceeded American Cancer Society (ACS) guidelines reported greater psychological well-being (Mean difference=1.03; 95% CI: 0.19-1.9); overall QoL (Mean difference=0.74; 95% CI: 0.04-1.4) and physical strength (Mean difference=1.29; 95% CI: 0.17- 2.4) compared to the non-active category. The group that met not exceeded the ACS PA guidelines had better psychological well-being and physical strength scores that exceeded the minimally important difference compared to the non-active. Total QoL score: (Non-active: Mean=6.32 (SD=0.18); Low active: Mean=6.71 (SD=0.26); Active: Mean=7.08 (SD=0.26)). Physical strength: (Non-active: Mean=6.15 (SD=0.30); Low active: Mean=6.89 (SD=0.40); Active: Mean=7.48 (SD=0.48). PA: SE: Self-efficacy for aerobic exercise accounted greater variance for PA time (4.9%) than ostomy type (2.5%). Patients with urostomies who met ACS PA guidelines had higher self-efficacy scores for aerobic exercise capacity (p=0.02). Patients who met ACS PA guidelines had higher self-efficacy scores for both gentle (8.1 points out of 10) and aerobic exercise (8.7 points out of 10) compared to those who did not meet guidelines. However, the latter group of patients reported moderate self-efficacy with respect to the ability to perform gentle (6.7 points) or aerobic (6.1 points) PA. Ad hoc questionnaire: No differences in PA intensity and type of ostomy: Intense PA (p=0.06): Colostomy: Mean=91.3 (SD=198.2); Ileostomy: Mean=38.6 (SD=79.6); Vigorous PA (p=0.08): Colostomy: Mean=16.2 (SD=63.3); Ileostomy: Mean=3.8 (SD=17.1); Moderate AF (p=0.32): Colostomy: Mean=59 (SD=122.3); Ileostomy: Mean=31 (SD=66.6). |
| Lowe, Alsaleh & Blake (2019) [20] Cross-sectional |
N=116 (completed questionnaire n=94) Male: 46 (49%); Female: 48 (51%) Colostomy, ileostomy and urostomy PA: Walking |
QoL: Patient Health Questionnaire (PHQ-9): Items: 9 criteria for depression (depressed mood or irritability, decreased interest or pleasure, significant weight loss or loss of appetite, changes in sleep pattern, changes in activity, fatigue or loss of energy, guilt or worthlessness, concentration, and suicidality; Likert scale: 0 (never) - 3 (almost every day); Score: 5-27 (higher score indicates depression, less than 4 indicates no depression) Reliability: Not reported. SQoL: Items: 20 in 5 domains (stoma device; sleep; sexual activity; relationships with family and friends and social relationships). Likert scale: 1 (always) - 4 (never); Score: 20-80 (higher score indicates optimal QoL). Reliability: Not reported. Social Physique Anxiety Scale (SPAS): Items: 12; Likert scale: 1 (not at all characteristic of me) - 5 (extremely characteristic of me). Score: Maximum 60 (low scores indicate reduced physical anxiety; Reliability: Not reported. PA: International PA Questionnaire (IPAQ): Short version. Measures of the amount of exercise in frequency (days per week) and duration (hours and minutes per day). Scale: Not reported; Score: Not reported; Reliability: Not reported. Self-efficacy for exercise (SEE): Items: 9 (environmental climate, boredom, pain, exercising alone, pleasant or unpleasant exercise, being busy, tiredness, stress, and depression). Scale: 0 (no confidence) to 10 (high confidence); Score: 0-90 (Higher score indicates more self-efficacy for exercise); Reliability: Not reported. Excess Benefits and Barriers Scale (EBBS): 29 items to measure perceived benefits and barriers to PA (Benefits: improved life, physical performance, psychological outlook, social interaction, and preventive health. Barriers: exercise environment, time investment; physical effort; and family discouragement). Likert scale: Benefits score 1 (strongly disagree) to 4 (strongly agree); for barriers inverse score. Score: 43-172, higher values indicate greater perception of PA benefits; Reliability: Not reported. |
QoL: PHQ-9: Total PHQ-9: Mean=3.22 (SD=4.8). No differences for depression according to exercise intensity (F=3.05; p=0.53). SQoL: Total: Mean=19.3 (SD=12.9). No differences for exercise intensity (F=0.40; p=0.67). SPAS: No differences for physical anxiety according to exercise intensity (F=1.97; p=0.15). PA: IPAQ: Inactive (n=36; 42%), minimally active (n=35; 41%), active (n=15; 17%) participants. Differences favor to women (more active) than men (p=0.05). SEE: Total score (Mean=40.8; SD: 20.7) indicated moderate self-efficacy for exercise. Scores had significant effect for MET intensity (F=3.04, p<0.001). Mean score for inactive group (n=34, Mean=30.4) was significative lower than for the minimally active group (n=33; Mean=46; p=0.03) and the active group (n=17; Mean=49; p=0.01). There was no difference between the minimally active and active groups (p=0.61). EBBS: The greatest barriers to PA were physical effort, time, and accessibility. Scores were significative lower in inactive participants compared to minimally active and active (not reported p-value). Individuals with higher total score (higher perceived benefits) were more likely to be active or minimally active than inactive. Individuals with lower score (fewer perceived benefits) were more likely to be inactive than minimally active or active. No differences between the minimally active group and the active group (p=0.90). |
| Kindred et al. (2019) [21] RCT |
N=46 IG: N=20 Male: 8 (40%); Female: 12 (60%) CG: N=26 Male: 12 (46.2%); Female: 14 (53.8%) PA: Strength exercise; moderate intensity (12 weeks). Submaximal fitness test: Treadmill walking. Participants select the fastest steady pace walking one mile by estimating maximal oxygen consumption. Accelerometer data: Moderate to vigorous PA was measured with the Computer Science and Applications, Inc. monitor 3 consecutive days. |
PA: Body Esteem Scale (BES): 35 Items into subscales according to the sex of the individual (Men: physical attractiveness, upper body strength and physical condition. Women: sexual attractiveness, weight concern and physical condition). 5-point Likert scale: 1 (very negative feelings) 5 (very positive feelings). Score: Higher indicates positive body esteem. Reliability: Not reported. Body composition: Measured by electrical impedance with a single frequency current (50 kHz) produced by a Quantum II RJL analyzer (RJL Systems, Clinton Township, MI). |
BES: Significative associations on physical fitness (body esteem) in men (3 months: b=0.68; SD=0.35; p=0.04; 6 months: b=1.36; SD=0.66; p=0.04; and 12 months: b=0.84; SD=0.36; p=0.03). No statistical difference in women. Body composition: Among women there were positive associations between reductions in body fat and body size (3 months: b=3.71; SD=1.79; p=0.05; 12 months: b=5.99; SD=2.95; p=0.05). |
| Russell (2017) [22] Cross-sectional |
N=2631 Male: 46%; Female: 54%. Type of stoma: Not Specified PA: Not reported |
Instrument not reported. Ad hoc survey with open and closed questions using a 3 and 5-point likert scale. |
People declared QoL “a little worse” than before surgery (22.5% diagnosis/suspected hernia vs. 16% without hernia; p<0.05). 32% with hernia declare being “much less active” than before surgery compared to 19% without hernia (p<0.001). |
| Russell (2017) [23] Cross-sectional |
N=2631 Male: 46%; Female: 54%. Type of stoma: Not Specified PA: Not reported |
Ad hoc survey: “Living with a stoma, your experience” with open and closed questions, rating scales of 3 and 5-points likert scale. | People with stoma reported less active (24.8%) compared to other conditions (p<0.001). People who reported performing PA since intervention (38%) showed a higher perceived QoL (p<0.05). |
| Krouse et al. (2017) [24] Cross-sectional |
N=1063 (target population) rectal cancer survivors (<5 years after diagnosis) during 2010-2011. N= 557 (sample) Type of stoma: Not specified PA: Not reported. |
QOL: City of Hope QoL Ostomy (COH-QoL-O) (Ad hoc questionnaire): Items: Not specified. Scale: Not specified. Score: 0-10; higher score indicates better QoL. Subscales (physical, psychological, social, and spiritual well-being); Reliability: Not reported. |
QOL: COH-QoL-O: Total QoL better in the group with guidelines respect to not active (Mean difference=0.43; 95% CI: 0.10-0.76). The group that followed the guidelines showed greater psychological well-being (Mean difference=0.55; 95% CI: 0.23-0.88). Association between increased PA time and physical component (Mean difference=6.0; 95% CI: 3.9-8.1), physical function (Mean difference=7.0; 95% CI: 4.8-9.3), physical role (Mean difference=4.5; 95% CI: 2.5-6.5), general health (Mean difference=5.8; 95% CI: 3.5-8.2), vitality (Mean difference=5.7; 95% CI: 3.6-7.8), social role (Mean difference=3.7; 95% CI: 1.4-5.9) and emotional role (Mean difference=3.8: 95% CI: 0.82-6.7). PA: GLTEQ: 34% (n=190) not active, 26% (n=145) insufficiently active, 13% (n=72) meeting guidelines and 27% (n=150) above guidelines. Relationship between PA time and being younger (p<0.001), years since surgery (p=0.02), college degree (p<0.001), higher income (p=0.004), married or partnered (p=0.003) and comorbidity less than 2 (p<0.001). No differences (p=0.08) between having an ostomy and time of PA. |
| Courneya et al. (1999) [28] Cohortes |
N= 53 Males: 60%. Mean age: 60.7 years Type of stoma: Colostomy, ileostomy and urostomy. PA: Not reported. |
QoL: Functional Assessment of Cancer Therapy- Colorectal (FACT-C): 6 dimensions: physical, functional, emotional, social, relationship with physician, additional aspects; Scale: Likert 0 (worst quality) - 4 (best quality); Score: Not reported; Reliability: α=0.85 (baseline); α= 0.91 (4 months). Satisfaction with Life scale (SWL): Items: 5 on unspecified aspects of life; Scale: Likert 1 (worst satisfaction) - 7 (best satisfaction); Score: Not reported; Reliability: α=0.91 (baseline); α=0.92 (4 months). PA: Godin Leisure Time Exercise Questionnaire (GLTEQ): Items: 3 questions on frequency of days per week performing light, moderate and strenuous exercise for 15 minutes. Scale: Open-ended. |
QoL: FACT-C: Total: Baseline (Mean=3.31; SD=0.40). 4 months (Mean=3.24; SD=0.52). Mean difference= -0.07 (SD= 0.35). Physical: Baseline (Mean=3.41; SD=2.48). 4 months (Mean=3.23; SD=0.81). Mean difference= -0.18 (SD= 0.66). Functional: Baseline (Mean=3.05; SD=0.66). 4 months (Mean=3.10; SD=0.70). Mean difference= 0.05 (SD= 0.63). Emotional: Baseline (Mean=3.37; SD=0.60). 4 months (Mean=3.49; SD=0.50). Mean difference= -0.07 (SD= 0.35). Social: Baseline (Mean=3.56; SD=0.57). 4 months (Mean=3.28; SD=0.76). Mean difference= -0.28 (SD=0.74). Changes in QoL at 4 months for social dimension (p<0.008). SWL: Baseline (Mean=4.98; SD=1.51). 4 months (Mean=5.00; SD=1.41). Mean difference=0.02 (SD=1.12). Baseline correlation between satisfaction and functional dimension (r=0.70). Multifactorial analysis indicated that functional dimension is the only one that explains 50% of variance: F(1.51)=50.20; p<0.001. Correlation at 4 months between satisfaction and functional (r=0.73), emotional (r=0.56), physical (r=0.54), additional aspects (r=0.49) and social (r=0.40) dimensions. Multifactorial analysis: functional (B=0.58), additional aspects (B=0.25) and social (B=0.19) dimensions explained 62% of variance: F(3.49)=26.64; p<0.001. Changes in satisfaction Baseline - 4 months for physical (r=0.38), functional (r=0.33) and additional aspects (r=0.31) explained 15% of variance: F(1.15)=8.71; p<0.005. PA: GLTEQ: Mild: Baseline (Mean=2.64; SD=2.48). 4 months (Mean=2.75; SD=2.52). Mean difference=0.11 (SD=2.77). Moderate: Baseline (Mean=1.53; SD=1.90). 4 months (Mean=1.78; SD=2.13). Mean difference=0.25 (SD=2.51). Extenuating: Baseline (Mean=0.53; SD=1.44). 4 months (Mean=0.17; SD=0.49). Mean difference= -0.36 (SD=1.26). Increases in mild to moderate PA associated in total QoL at 4 months (r=0.39; p<0.01). |
| 1 PA: Physical Activity; 2 QoL: Quality of Life; 3 SD: Standard Deviation | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




