Submitted:
05 August 2024
Posted:
06 August 2024
You are already at the latest version
Abstract
Keywords:
Introduction
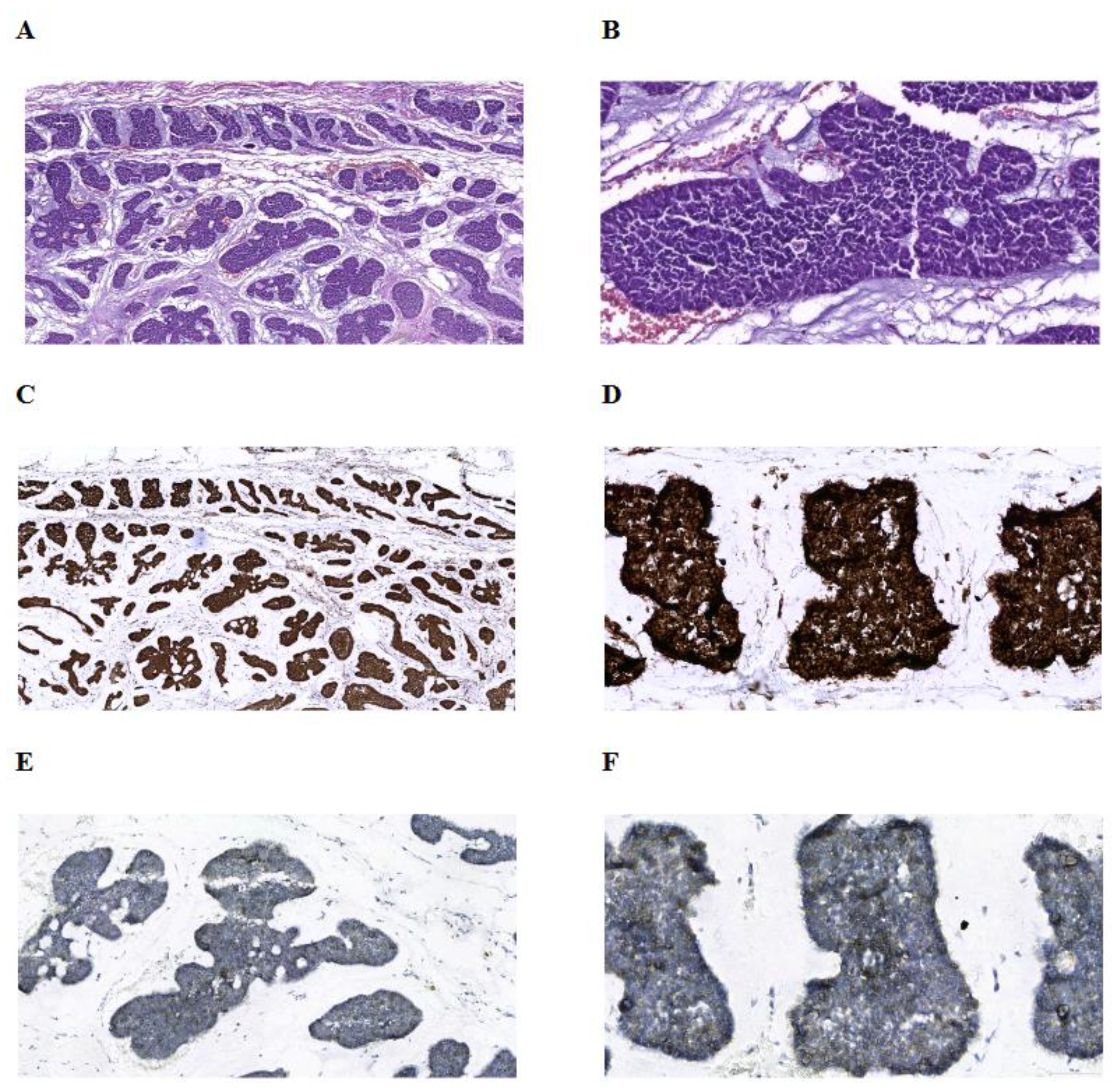
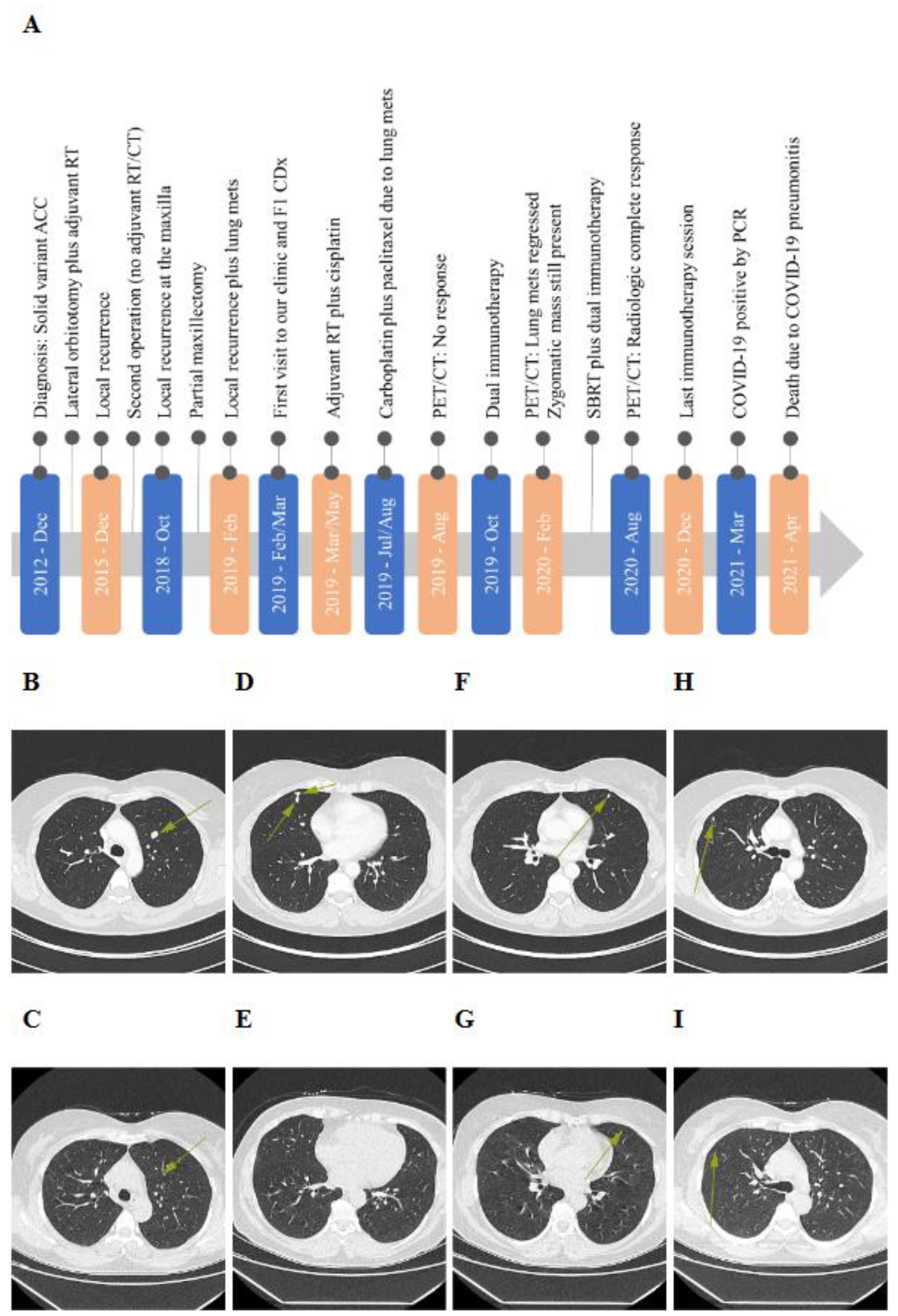
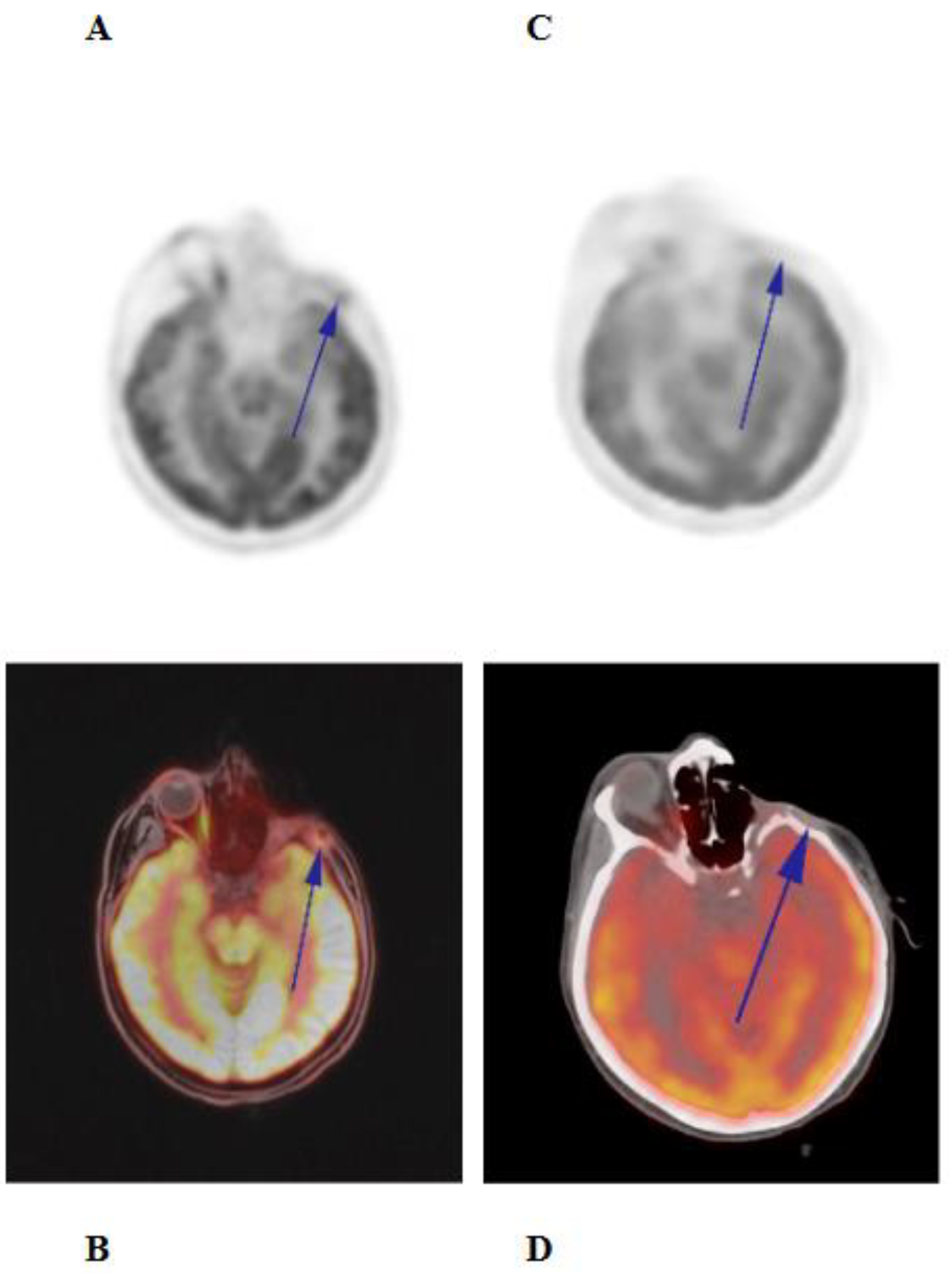
Case Presentation
Discussion
Informed Consent
Data Availability Statement
Acknowledgments
Conflicts of Interest Statement and Funding
References
- Steuer CE, Hanna GJ, Viswanathan K, et al. The evolving landscape of salivary gland tumors. CA Cancer J Clin 2023; 73: 597-619. 20230725. [CrossRef]
- Li N, Xu L, Zhao H, et al. A comparison of the demographics, clinical features, and survival of patients with adenoid cystic carcinoma of major and minor salivary glands versus less common sites within the Surveillance, Epidemiology, and End Results registry. Cancer 2012; 118: 3945-3953. 20111216. [CrossRef]
- Lesueur P, Rapeaud E, De Marzi L, et al. Adenoid Cystic Carcinoma of the Lacrimal Gland: High Dose Adjuvant Proton Therapy to Improve Patients Outcomes. Front Oncol 2020; 10: 135. 20200218. [CrossRef]
- Emerick C, Mariano FV, Vargas PA, et al. Adenoid Cystic Carcinoma from the salivary and lacrimal glands and the breast: Different clinical outcomes to the same tumor. Crit Rev Oncol Hematol 2022; 179: 103792. 20220813. [CrossRef]
- Ferrarotto R, Mitani Y, McGrail DJ, et al. Proteogenomic Analysis of Salivary Adenoid Cystic Carcinomas Defines Molecular Subtypes and Identifies Therapeutic Targets. Clin Cancer Res 2021; 27: 852-864. 20201110. [CrossRef]
- Marabelle A, Fakih M, Lopez J, et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol 2020; 21: 1353-1365. 20200910. [CrossRef]
- Marcus L, Lemery SJ, Keegan P, et al. FDA Approval Summary: Pembrolizumab for the Treatment of Microsatellite Instability-High Solid Tumors. Clin Cancer Res 2019; 25: 3753-3758. 20190220. [CrossRef]
- Ho AS, Ochoa A, Jayakumaran G, et al. Genetic hallmarks of recurrent/metastatic adenoid cystic carcinoma. J Clin Invest 2019; 129: 4276-4289. [CrossRef]
- Mahmood U, Bang A, Chen YH, et al. A Randomized Phase 2 Study of Pembrolizumab With or Without Radiation in Patients With Recurrent or Metastatic Adenoid Cystic Carcinoma. Int J Radiat Oncol Biol Phys 2021; 109: 134-144. 20200808. [CrossRef]
- Schumacher TN and Schreiber RD. Neoantigens in cancer immunotherapy. Science 2015; 348: 69-74. [CrossRef]
- McGranahan N, Furness AJ, Rosenthal R, et al. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science 2016; 351: 1463-1469. 20160303. [CrossRef]
- Chen H, Chong W, Teng C, et al. The immune response-related mutational signatures and driver genes in non-small-cell lung cancer. Cancer Sci 2019; 110: 2348-2356. 20190723. [CrossRef]
- Long J, Wang D, Wang A, et al. A mutation-based gene set predicts survival benefit after immunotherapy across multiple cancers and reveals the immune response landscape. Genome Med 2022; 14: 20. 20220224. [CrossRef]
- Chae YK, Viveiros P, Lopes G, et al. Clinical and Immunological Implications of Frameshift Mutations in Lung Cancer. J Thorac Oncol 2019; 14: 1807-1817. 20190622. [CrossRef]
- Cormedi MCV, Van Allen EM and Colli LM. Predicting immunotherapy response through genomics. Curr Opin Genet Dev 2021; 66: 1-9. 20201208. [CrossRef]
- Wei SC, Anang NAS, Sharma R, et al. Combination anti-CTLA-4 plus anti-PD-1 checkpoint blockade utilizes cellular mechanisms partially distinct from monotherapies. Proc Natl Acad Sci U S A 2019; 116: 22699-22709. 20191021. [CrossRef]
- Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N Engl J Med 2015; 373: 23-34. 20150531. [CrossRef]
- Magri A, Germano G, Lorenzato A, et al. High-dose vitamin C enhances cancer immunotherapy. Sci Transl Med 2020; 12. [CrossRef]
- Hoffer LJ, Levine M, Assouline S, et al. Phase I clinical trial of i.v. ascorbic acid in advanced malignancy. Ann Oncol 2008; 19: 1969-1974. 20080609. [CrossRef]
- Peng D, He A, He S, et al. Ascorbic acid induced TET2 enzyme activation enhances cancer immunotherapy efficacy in renal cell carcinoma. Int J Biol Sci 2022; 18: 995-1007. 20220101. [CrossRef]
- Luchtel RA, Bhagat T, Pradhan K, et al. High-dose ascorbic acid synergizes with anti-PD1 in a lymphoma mouse model. Proc Natl Acad Sci U S A 2020; 117: 1666-1677. 20200107. [CrossRef]
- Paul S and Sa G. Curcumin as an Adjuvant to Cancer Immunotherapy. Front Oncol 2021; 11: 675923. 20210816. [CrossRef]
- Demiray M, Sahinbas H, Atahan S, et al. Successful treatment of c-kit-positive metastatic Adenoid Cystic Carcinoma (ACC) with a combination of curcumin plus imatinib: A case report. Complement Ther Med 2016; 27: 108-113. 20160701. [CrossRef]
- Barroso-Sousa R, Barry WT, Garrido-Castro AC, et al. Incidence of Endocrine Dysfunction Following the Use of Different Immune Checkpoint Inhibitor Regimens: A Systematic Review and Meta-analysis. JAMA Oncol 2018; 4: 173-182. [CrossRef]
- Laurie SA, Ho AL, Fury MG, et al. Systemic therapy in the management of metastatic or locally recurrent adenoid cystic carcinoma of the salivary glands: a systematic review. Lancet Oncol 2011; 12: 815-824. 20101210. [CrossRef]
- Ho AS, Kannan K, Roy DM, et al. The mutational landscape of adenoid cystic carcinoma. Nat Genet 2013; 45: 791-798. 20130519. [CrossRef]
- Sahara S, Herzog AE and Nor JE. Systemic therapies for salivary gland adenoid cystic carcinoma. Am J Cancer Res 2021; 11: 4092-4110. 20210915.
- Valkenburg KC, de Groot AE and Pienta KJ. Targeting the tumour stroma to improve cancer therapy. Nat Rev Clin Oncol 2018; 15: 366-381. [CrossRef]
- Schlauch D, Fu X, Jones SF, et al. Tumor-Specific and Tumor-Agnostic Molecular Signatures Associated With Response to Immune Checkpoint Inhibitors. JCO Precis Oncol 2021; 5: 1625-1638. [CrossRef]
- Patel SP and Kurzrock R. PD-L1 Expression as a Predictive Biomarker in Cancer Immunotherapy. Mol Cancer Ther 2015; 14: 847-856. 20150218. [CrossRef]
- Boyiadzis MM, Kirkwood JM, Marshall JL, et al. Significance and implications of FDA approval of pembrolizumab for biomarker-defined disease. J Immunother Cancer 2018; 6: 35. 20180514. [CrossRef]
- Gandini S, Massi D and Mandala M. PD-L1 expression in cancer patients receiving anti PD-1/PD-L1 antibodies: A systematic review and meta-analysis. Crit Rev Oncol Hematol 2016; 100: 88-98. 20160210. [CrossRef]
- McGrail DJ, Pilie PG, Rashid NU, et al. High tumor mutation burden fails to predict immune checkpoint blockade response across all cancer types. Ann Oncol 2021; 32: 661-672. 20210315. [CrossRef]
- Samstein RM, Lee CH, Shoushtari AN, et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat Genet 2019; 51: 202-206. 20190114. [CrossRef]
- Ross JS, Gay LM, Wang K, et al. Comprehensive genomic profiles of metastatic and relapsed salivary gland carcinomas are associated with tumor type and reveal new routes to targeted therapies. Ann Oncol 2017; 28: 2539-2546. [CrossRef]
- Davis AA and Patel VG. The role of PD-L1 expression as a predictive biomarker: an analysis of all US Food and Drug Administration (FDA) approvals of immune checkpoint inhibitors. J Immunother Cancer 2019; 7: 278. 20191026. [CrossRef]
- Chen W, Fung AS, McIntyre JB, et al. Assessment Of Tumour Infiltrating Lymphocytes And Pd-l1 Expression In Adenoid Cystic Carcinoma Of The Salivary Gland. Clin Invest Med 2021; 44: E38-41. 20210321. [CrossRef]
- Sridharan V, Gjini E, Liao X, et al. Immune Profiling of Adenoid Cystic Carcinoma: PD-L2 Expression and Associations with Tumor-Infiltrating Lymphocytes. Cancer Immunol Res 2016; 4: 679-687. 20160616. [CrossRef]
- Oliva M, Spreafico A, Taberna M, et al. Immune biomarkers of response to immune-checkpoint inhibitors in head and neck squamous cell carcinoma. Ann Oncol 2019; 30: 57-67. [CrossRef]
- Cohen RB, Delord JP, Doi T, et al. Pembrolizumab for the Treatment of Advanced Salivary Gland Carcinoma: Findings of the Phase 1b KEYNOTE-028 Study. Am J Clin Oncol 2018; 41: 1083-1088. [CrossRef]
- Fayette J, Even C, Digue L, et al. NISCAHN: a phase II trial of nivolumab in patients with salivary gland carcinoma (Unicancer ORL-08). BMJ Oncol 2023; 2. [CrossRef]
- Vos JL, Burman B, Jain S, et al. Nivolumab plus ipilimumab in advanced salivary gland cancer: a phase 2 trial. Nat Med 2023; 29: 3077-3089. 20230824. [CrossRef]
- Fumet JD, Truntzer C, Yarchoan M, et al. Tumour mutational burden as a biomarker for immunotherapy: Current data and emerging concepts. Eur J Cancer 2020; 131: 40-50. 20200409. [CrossRef]
- Wolf Y, Bartok O, Patkar S, et al. UVB-Induced Tumor Heterogeneity Diminishes Immune Response in Melanoma. Cell 2019; 179: 219-235 e221. 20190912. [CrossRef]
- Litchfield K, Reading JL, Puttick C, et al. Meta-analysis of tumor- and T cell-intrinsic mechanisms of sensitization to checkpoint inhibition. Cell 2021; 184: 596-614 e514. 20210127. [CrossRef]
- Gajic ZZ, Deshpande A, Legut M, et al. Recurrent somatic mutations as predictors of immunotherapy response. Nat Commun 2022; 13: 3938. 20220708. [CrossRef]
- Martinez-Jimenez F, Priestley P, Shale C, et al. Genetic immune escape landscape in primary and metastatic cancer. Nat Genet 2023; 55: 820-831. 20230510. [CrossRef]
- Zhang K, Hong X, Song Z, et al. Identification of Deleterious NOTCH Mutation as Novel Predictor to Efficacious Immunotherapy in NSCLC. Clin Cancer Res 2020; 26: 3649-3661. 20200402. [CrossRef]
- Wang F, Long J, Li L, et al. Mutations in the notch signalling pathway are associated with enhanced anti-tumour immunity in colorectal cancer. J Cell Mol Med 2020; 24: 12176-12187. 20200914. [CrossRef]
- Roper N, Velez MJ, Chiappori A, et al. Notch signaling and efficacy of PD-1/PD-L1 blockade in relapsed small cell lung cancer. Nat Commun 2021; 12: 3880. 20210623. [CrossRef]
- Qiu H, Zmina PM, Huang AY, et al. Inhibiting Notch1 enhances immunotherapy efficacy in melanoma by preventing Notch1 dependent immune suppressive properties. Cancer Lett 2018; 434: 144-151. 20180721. [CrossRef]
- K. R. Reyes, L. Zhang, X. Zhu, et al. Association of biomarkers and outcomes in patients (pts) with metastatic urothelial carcinoma (mUC) treated with immune checkpoint inhibitors (ICIs). J Clin Oncol 2023. [CrossRef]
- T. Jindal, X. Zhu, L. Zhang, et al. Association of biomarkers and response to immune checkpoint inhibitors (ICIs) in patients with metastatic urothelial carcinoma (mUC) with high and low tumor mutation burden (TMB). J Clin Oncol 2023. [CrossRef]
- Bedhiafi T, Inchakalody VP, Fernandes Q, et al. The potential role of vitamin C in empowering cancer immunotherapy. Biomed Pharmacother 2022; 146: 112553. 20211220. [CrossRef]
- Sartore-Bianchi A, Amatu A, Nicolantonio FD, et al. High-dose vitamin C to enhance neoadjuvant immune checkpoint therapy in mismatch repair proficient colon cancer: The ALFEO pilot study. Journal of Clinical Oncology 2023. [CrossRef]
- Chen Q, Espey MG, Krishna MC, et al. Pharmacologic ascorbic acid concentrations selectively kill cancer cells: action as a pro-drug to deliver hydrogen peroxide to tissues. Proc Natl Acad Sci U S A 2005; 102: 13604-13609. 20050912. [CrossRef]
- Adibi A, Tokat UM, Ozgu E, et al. PARP inhibitor combinations with high-dose vitamin C in the treatment of Ewing sarcoma: two case reports and mechanistic overview. Ther Adv Med Oncol 2023; 15: 17588359231213841. 20231215. [CrossRef]
- Banerjee S, Ji C, Mayfield JE, et al. Ancient drug curcumin impedes 26S proteasome activity by direct inhibition of dual-specificity tyrosine-regulated kinase 2. Proc Natl Acad Sci U S A 2018; 115: 8155-8160. 20180709. [CrossRef]
- Sun ZJ, Chen G, Zhang W, et al. Curcumin dually inhibits both mammalian target of rapamycin and nuclear factor-kappaB pathways through a crossed phosphatidylinositol 3-kinase/Akt/IkappaB kinase complex signaling axis in adenoid cystic carcinoma. Mol Pharmacol 2011; 79: 106-118. 20101019. [CrossRef]
- Sun ZJ, Chen G, Hu X, et al. Activation of PI3K/Akt/IKK-alpha/NF-kappaB signaling pathway is required for the apoptosis-evasion in human salivary adenoid cystic carcinoma: its inhibition by quercetin. Apoptosis 2010; 15: 850-863. [CrossRef]
- Phuchareon J, van Zante A, Overdevest JB, et al. c-Kit Expression is Rate-Limiting for Stem Cell Factor-Mediated Disease Progression in Adenoid Cystic Carcinoma of the Salivary Glands. Transl Oncol 2014; 7: 537-545. 20141024. [CrossRef]
- Argiris A, Ghebremichael M, Burtness B, et al. A phase 2 trial of bortezomib followed by the addition of doxorubicin at progression in patients with recurrent or metastatic adenoid cystic carcinoma of the head and neck: a trial of the Eastern Cooperative Oncology Group (E1303). Cancer 2011; 117: 3374-3382. 20110118. [CrossRef]
- Turajlic S, Litchfield K, Xu H, et al. Insertion-and-deletion-derived tumour-specific neoantigens and the immunogenic phenotype: a pan-cancer analysis. Lancet Oncol 2017; 18: 1009-1021. 20170707. [CrossRef]
- Schwitalle Y, Kloor M, Eiermann S, et al. Immune response against frameshift-induced neopeptides in HNPCC patients and healthy HNPCC mutation carriers. Gastroenterology 2008; 134: 988-997. 20080111. [CrossRef]
- Ballhausen A, Przybilla MJ, Jendrusch M, et al. The shared frameshift mutation landscape of microsatellite-unstable cancers suggests immunoediting during tumor evolution. Nat Commun 2020; 11: 4740. 20200921. [CrossRef]
- Roudko V, Bozkus CC, Orfanelli T, et al. Shared Immunogenic Poly-Epitope Frameshift Mutations in Microsatellite Unstable Tumors. Cell 2020; 183: 1634-1649 e1617. 20201130. [CrossRef]
- Florou V, Floudas CS, Maoz A, et al. Real-world pan-cancer landscape of frameshift mutations and their role in predicting responses to immune checkpoint inhibitors in cancers with low tumor mutational burden. J Immunother Cancer 2023; 11. [CrossRef]
- Lou Y, Asmann Y, Thomas M, et al. Integrating INDEL Mutations into Neoantigen Prediction in Lung Cancer: Developing Personalized Cancer Vaccines. J Thorac Oncol 2017; 12: 1814-1815. [CrossRef]
- Gebert J, Gelincik O, Oezcan-Wahlbrink M, et al. Recurrent Frameshift Neoantigen Vaccine Elicits Protective Immunity With Reduced Tumor Burden and Improved Overall Survival in a Lynch Syndrome Mouse Model. Gastroenterology 2021; 161: 1288-1302 e1213. 20210702. [CrossRef]
- Hanna GJ, Lizotte P, Cavanaugh M, et al. Frameshift events predict anti-PD-1/L1 response in head and neck cancer. JCI Insight 2018; 3 20180222. [CrossRef]
- Jayasinghe RG, Cao S, Gao Q, et al. Systematic Analysis of Splice-Site-Creating Mutations in Cancer. Cell Rep 2018; 23: 270-281 e273. [CrossRef]
- Maleki Vareki S. High and low mutational burden tumors versus immunologically hot and cold tumors and response to immune checkpoint inhibitors. J Immunother Cancer 2018; 6: 157. 20181227. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




