1. Introduction
Spinal Cord Injury (SCI) is a devastating condition with high morbidity and mortality, with an incidence rate of 12 and a prevalence of 263 per 100’000 people [
1]. This estimate corresponds to about 21 million cases and a consequent significant burden to healthcare systems and economies through high healthcare costs and lost productivity [
2]. Spinal cord syndromes are conventionally classified according to the Asia Impairment Scale (AIS) level, based on the International Standards for Neurological Classification of SCI (ISNCSCI) [
3], and a wide range of highly different clinical pictures can be identified. The cervical incomplete lesion is currently the most common injury, followed by incomplete paraplegia and complete paraplegia. Lastly, the cervical complete lesion is the least widespread [
4]. The severity of the injury is a key factor in the clinical evaluation of individuals with SCI since it is considered the main predictor of neurological recovery and it is strictly linked to the final level of independence that can be reached [
5].
The care of individuals with SCI is multidisciplinary and takes into account the heterogeneity of clinical pictures, the systems involved, and the presence of several secondary health conditions [
6]. The consequent overall managing costs are staggering and pose a significant burden to individuals with SCI, their families, and society [
7]. Neurorehabilitation is an essential element of the overall care process of individuals following a SCI [
8]. It is mainly based on the compensation of functional loss and on the usage of those functions of the sensorimotor system that are still intact, to maximally improve independence and facilitate the reintegration into the family, social and work environments [
9]. Therefore, the aim of rehabilitation procedures is the improvement of selected outcomes, by exploiting plasticity of neuronal centers through functional training [
10,
11,
12], to ultimately promote functional recovery and independence in Activities of Daily Living (ADLs) [
13].
Conventional rehabilitation strategies, manually performed by Physical Therapists (PTs), may include different approaches which must be tailored for each individual based on the severity and the level of the injury. In fact, individuals with an incomplete sensorimotor injury can perform a much wider range of activities than individuals with a complete SCI. The rehabilitation program may include:
i) joints mobilization, muscle tone modulation or muscle strength improvement;
ii) training on trunk control and transfers to improve postural control and enhance independence during ADLs;
iii) training for standing recovery, also including exercises for the control of weight shifting for static and dynamic balance or gait rehabilitation strategies [
14,
15].
In the last decades, due to the technological developments in rehabilitation bioengineering, which leverages on continuously evolving fields such as robotics [
16], wearable and environmental sensors [
17,
18,
19], virtual reality [
20,
21] and many others, new devices have been introduced in the clinical setting. Their use enabled the implementation of several technology-aided rehabilitation paradigms [
22,
23] currently mainly adopted as add-on to conventional treatment [
16,
24,
25,
26,
27]. Rehabilitation technologies for individuals with SCI available on the market range from simple tools for tone modulation [
28], to platforms for balance rehabilitation during both sitting and standing [
22,
29], up to advanced devices for the recovery of upper or lower limb functions (such as, but not limited to, overground and treadmill-based exoskeletons, with or without body weight support, and end-effector robots). Since literature recognizes that technological innovation has the potential to enhance rehabilitation paths [
30], several studies were aimed at:
i) evaluating the effectiveness of these technologies on specific aspects of patient performance, e.g. muscles force, balance, independence in ADLs, etc., often in comparison with conventional rehabilitation [
26,
31,
32];
ii) identifying possible barriers to rehabilitation technology adoption, by analyzing the perspectives of people with disability and of health service providers [
33,
34,
35,
36].
Nonetheless, the quantification of the daily actual adoption into clinical settings of SCI rehabilitation [
26,
31,
32] is missing [
37]. To fill this gap, we addressed two aspects that have not been investigated in current literature:
i) the quantification of the overall adoption of technologies in the clinical daily practice, compared to conventional treatment, and
ii) the analysis of the specific technological resources adopted in homogeneous groups of individuals with SCI characterized by different neurological and functional features.
Therefore, the main aim of this study is to quantify the distribution of conventional treatments (Treatment As Usual – TAU) and treatments with technologies (Treatment With Technologies – TWT), also assessing the usage of specific TWT or TAU categories in the neurorehabilitation program of a cohort of individuals with SCI arranged in groups with similar characteristics. Our hypothesis is that the adoption of technologies (type/aim and amount of usage) can change among different groups of individuals. To this aim TAU and TWT data were collected and individuals under analysis were grouped according to the conventional AIS level, based on the ISNCSCI [
3], and a new specifically developed MultiFactor (MF) clustering approach that considers the lesion level, the level of independence in the ADLs (before and after the rehabilitation path), and the hospitalization duration, besides the AIS level at admission and discharge.
The motivation for this dual analysis lies in the hypothesis that simply clustering individuals according to the conventional AIS-based classification can be not effective since individuals with SCI, apparently comparable when classified with the same AIS level, can actually pursue very different ranges of neurological and functional recovery, especially after incomplete lesions [
38].. It is then desirable to make it available a clustering method able to group SCI population in homogeneous subgroups considering not only the neurological aspect, but also the functional one, by addressing the level of independence in the ADLs reached within a defined time frame. We hence expect that individuals belonging to the same AIS category can be too heterogeneous for investigating the specific TAU/TWT distribution and that, contrarily, a MF clustering, accounting for additional variables not considered in the traditional AIS neurological classification, can provide more insightful results on technology use and on its relationship with individuals’ overall rehabilitation program and outcome.
For this study we have focused on a specific clinical setting, namely the Spinal Cord Unit within the Neurorehabilitation 1 Department of Fondazione Santa Lucia (FSL) IRCCS in Rome, where rehabilitation technological devices have been progressively introduced along the years in the daily treatments of individuals with SCI. Data has been collected and digitized by means of a newly developed database accessed by a dedicated local Web App.
3. Results
A total cohort of 106 individuals with SCI, 89 males and 17 females, aged 51.32 ± 19.92 years, with traumatic etiology in 60% of cases, was included in the study. The mean time elapsed between SCI event and admission at the Spinal Cord Unit was 96.22 ± 52.90 days. Data from 104 individuals were considered for the analysis because 2 individuals died during hospitalization.
3.1. AIS-Based Clustering
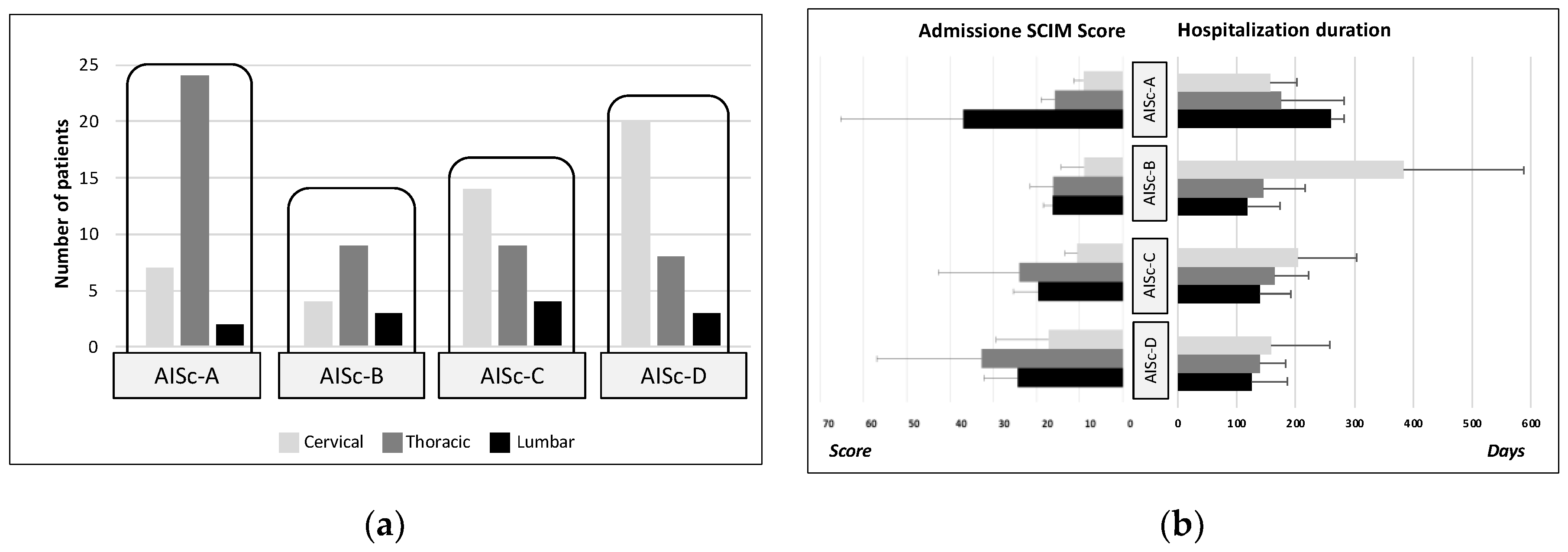
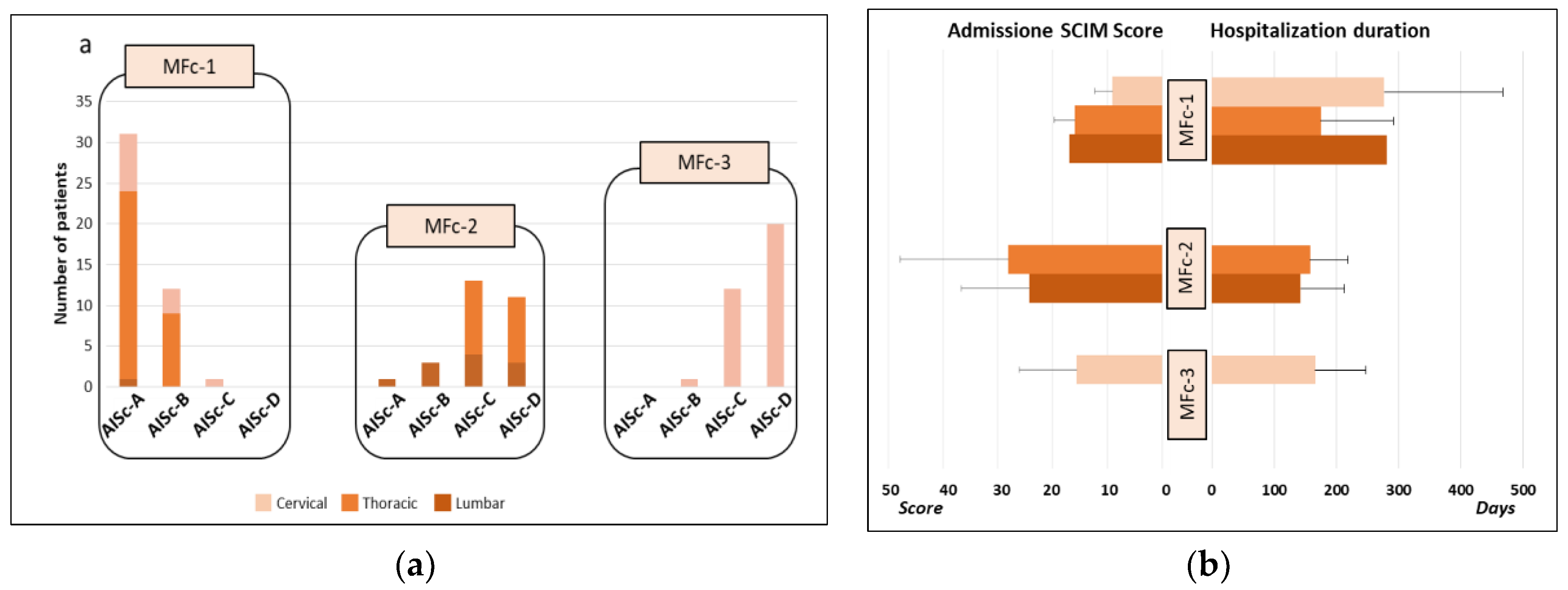
Four AIS-based clusters were created according to AIS level, i.e. including respectively individuals with SCI classified as AIS A, B, C and D levels (AISc-A, AISc-B, AISc-C, AISc-D). AIS-based clustering revealed that most individuals belonged to AISc-A (N=33) or AISc-D (N=30), with less individuals grouped into AISc-C (N=27) or AISc-B (N=16). The most represented lesion level was thoracic for AISc-A and AISc-B individuals, whereas lumbar lesion was the least frequent in all categories (
Figure 1.a). The mean SCIM score recorded at admission was 17.80 ± 12.37: AISc-A and AISc-B individuals had a lower score than individuals with incomplete motor lesion, with the only exception of AISc-A individuals with lumbar lesion. Those with the highest SCIM score were AISc-D individuals. Moreover, individuals with cervical lesion had the lowest SCIM values among all AIS-based categories (
Figure 1b).
The mean hospitalization duration was 172.37 ± 101.25 days. Among individuals with incomplete injury (AISc-B, AISc-C or AISc-D) those with cervical lesion had the longest hospital stay, whereas the earliest discharged individuals were those with lumbar SCI. This pattern was completely reversed in the case of individuals from AISc-A, for whom hospital stays in case of lumbar lesions were longer than in case of cervical injuries (
Figure 1.b).
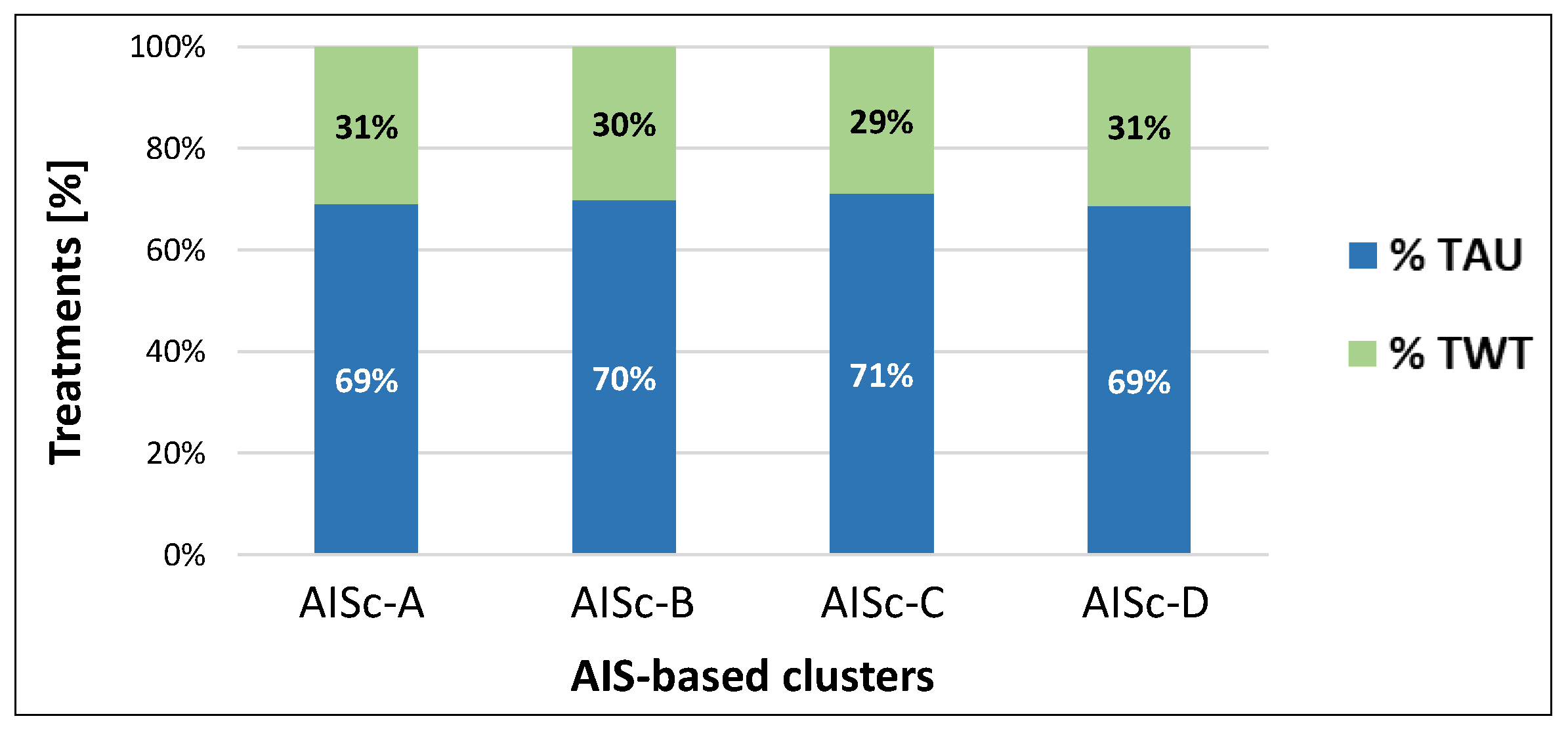
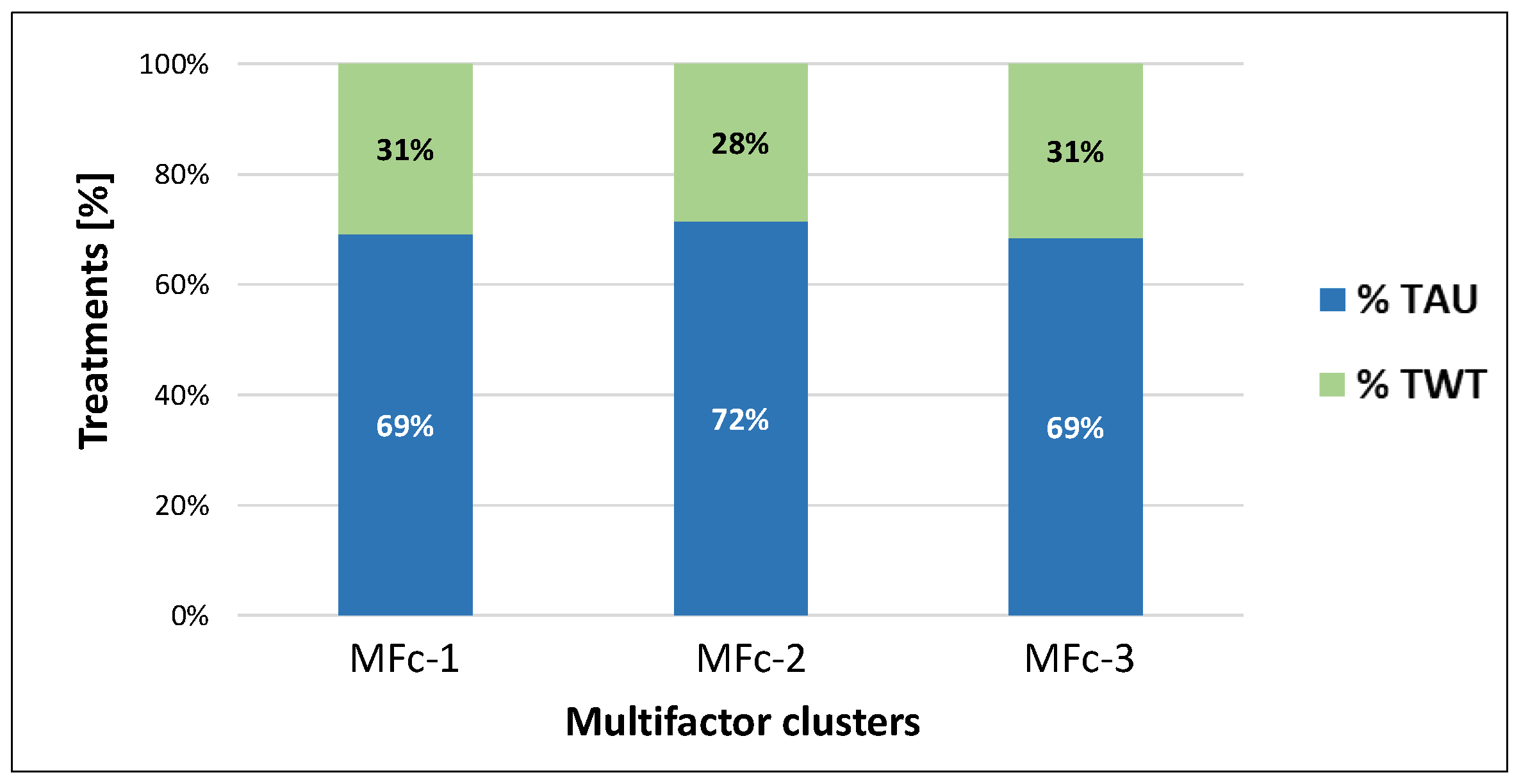
As regards the primary outcome of the study, TWT represented about 30% of the total treatments received by the sample. No substantial differences were reported among AIS-based categories, ranging from 29% for individuals grouped into AISc-C to 31% for AISc-A and AISc-D clusters (
Figure 2).
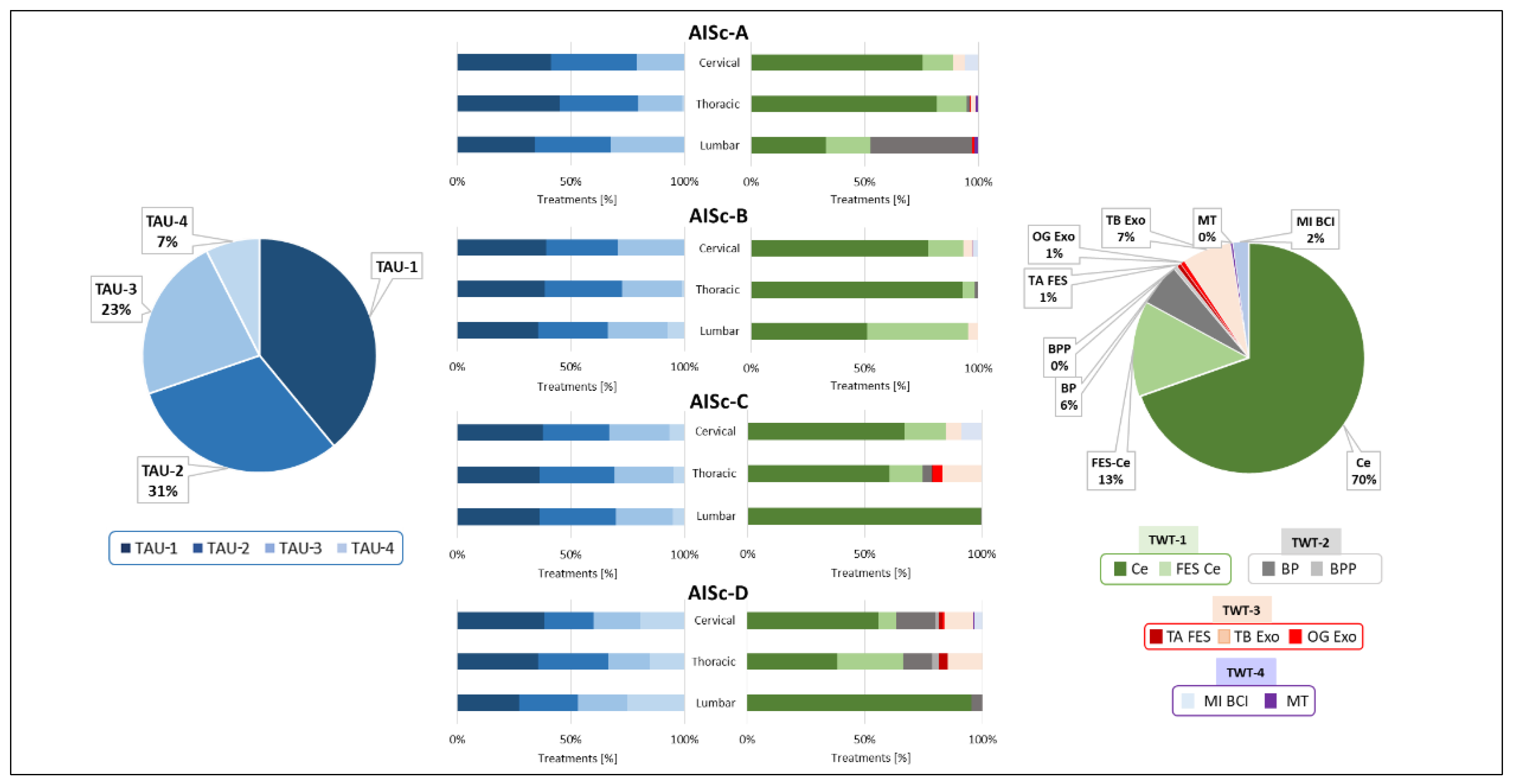
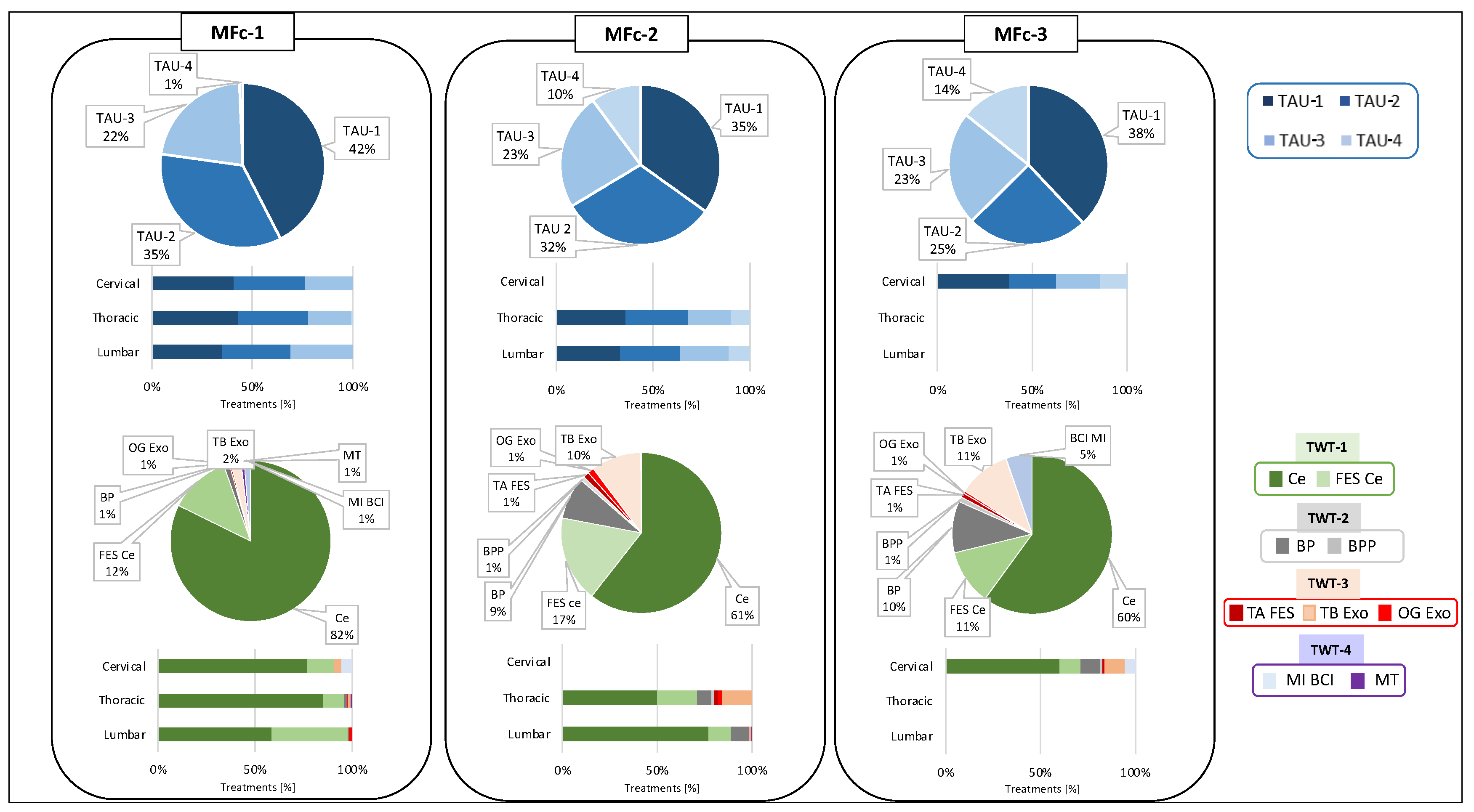
Looking in detail at the conventional treatments across AIS-based categories, TAU-1 was the most adopted one, followed by TAU-2, TAU-3 and TAU-4, respectively (
Figure 3).
Notably, TAU-1 is less adopted as the lesion level decreases. Regardless of the level of injury for AISc-A and AISc-B TAU-4 is almost never present, while its adoption increases as the severity of the injury decreases for individuals with motor incomplete SCI. In particular, TAU-4 was chosen at the expense of TAU-3 for AISc-D.
Considering the analysis of TWT data, TWT-1 adoption was the highest, especially for the Ce (70 %), followed by TWT-3, in particular the OG Exo device (7%), and TWT-2. Finally, TWT-4 devices were the least used (2%). A clear prevalence of a specific device was not found for TWT-2 and TWT-4. Ce (70%) was more commonly used than Ce FES (13%) among all AIS-based categories, regardless of the level of impairment. In case of complete motor lesions, TWT-2 devices were exclusively used for AISc-A individuals, in particular for those with lumbar SCI. For both AISc-A and AISc-B clusters, different TWT-3 and TWT-4 devices were used, but specifically the OG Exo and MT were used for individuals with the highest level of impairment only. In case of AISc-C and AISc-D, individuals received TWT-3 and TWT-4. The only exception was the exclusive use of the TA FES for individuals from AISc-D with cervical and thoracic SCI.
3.2. Multifactor Clustering
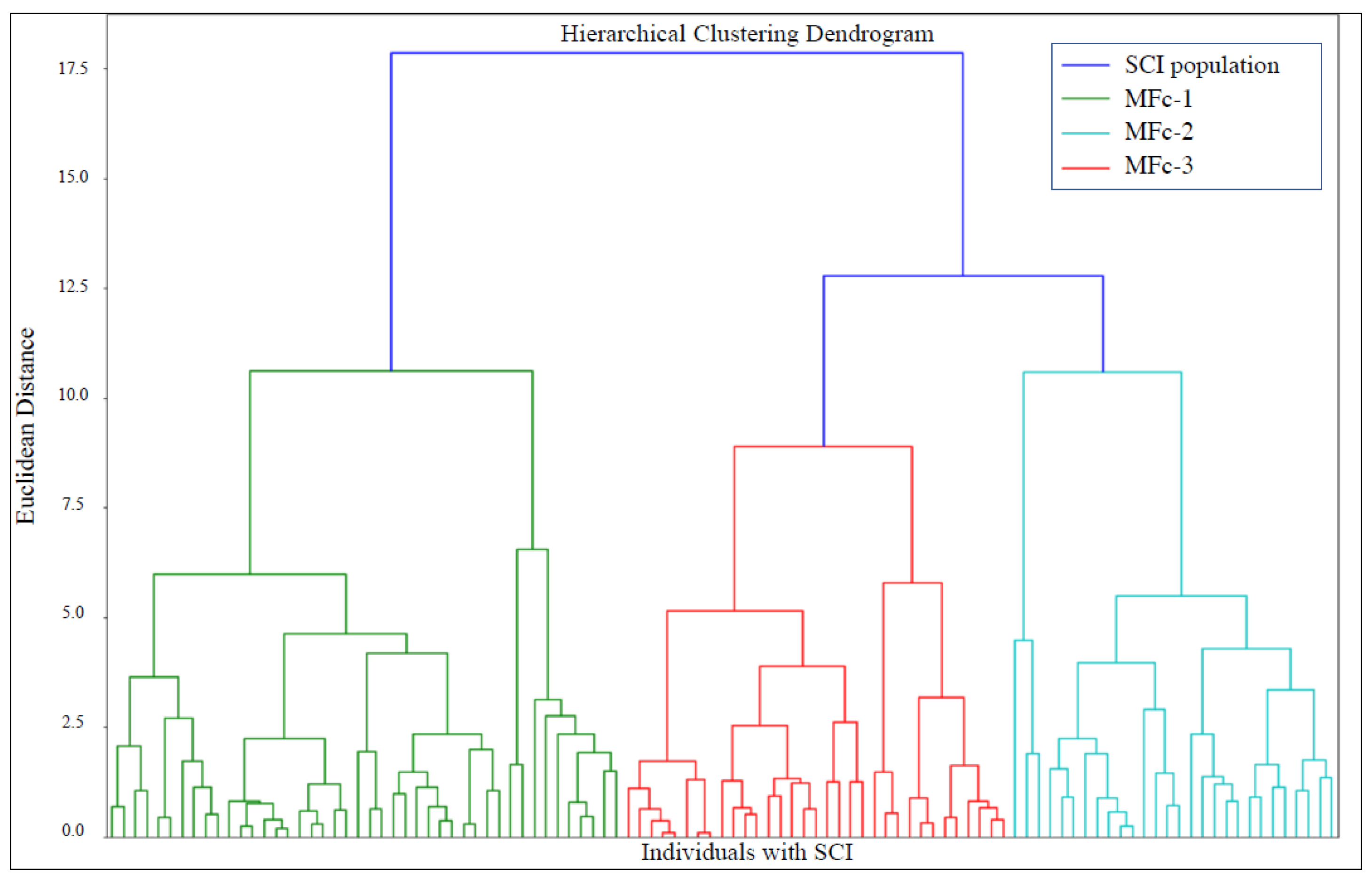
The MF clustering based on the method described in
Section 2.5 produced the dendrogram reported in
Figure 4, a tree-like representation of the clusters hierarchy. The Euclidean distance on the dendrogram represents the dissimilarity among clusters, with larger distances indicating more heterogeneity.
Three MF clusters (MFc-1, MFc-2, MFc-3) were extracted from the dendrogram considering the most relevant distinction among main groups of individuals with SCI. We considered inter-cluster variance among sub-clusters at a level below the selected three too small for a further useful distinction. By decreasing the Euclidean distance threshold in the dendrogram, more clusters can be found that show even greater overlap. Hence, individuals belonging to the final three clusters were considered to have homogeneous features.
MFc-1 was mainly composed of individuals with cervical or thoracic motor complete SCI (it contained no individuals classified as AISc-D and almost no AISc-C individuals). MFc-2 included individuals with a thoracic or lumbar lesion, mainly with motor incomplete SCI. MFc-3 consisted exclusively of individuals with incomplete cervical lesion and almost no AISc-A individuals (
Figure 5a). According to the MF analysis, data showed that the individuals in MFc-1 had the lowest SCIM score on admission and the higher duration of hospitalization. On the contrary, individuals belonging to MFc-2 had the highest SCIM score on admission and the shortest hospitalization (
Figure 5b).
As regards the primary outcome of the study, TWT adoption ranged from 28% to 31% of the total treatments received by the sample (
Figure 6). The three MF clusters presented a similar distribution between TAU and TWT, with a minor difference for cluster MFc-2 that received less TWT (28%) than the other clusters (31%).
Overall, considering the conventional rehabilitation, TAU-1 was the most adopted, followed by TAU-2, TAU-3 and TAU-4. Cluster MFc-1 presented the highest TAU-1 and the lowest TAU-4 adoption. Instead, for the other two clusters, TAU-4 covered more than 10% of the total TAU. The data on the TAU-3 was similar among the clusters, while TAU-2 was mainly proposed in cluster MFc-1. For these data, no substantial differences were noted when considering the lesion levels.
The data on TWT showed that for each of the three clusters, TWT-1 was the most adopted, whereas TWT-4 was the least used. TWT distribution between MFc-2 and MFc-3 was similar and different compared to MFc-1, with the only exception of the MI BCI device that was absent in MFc-2. Compared to MFc-1, MFc-2 and MFc-3 presented a higher adoption of TWT-2 and TWT-3, whereas the usage of TWT-1 was low (
Figure 7).
3.3. Statistical Analysis for AIS-Based and MF Clustering Approaches
The silhouette score [
57] for all the samples of the MF clusters was equal to 0.02, whereas AIS-based classification resulted in a worse silhouette value of -0.11 (the negative sign indicates closer similarity among clusters).
For the MF clustering the MANOVA test resulted in a p-value equal to 0.0013, indicating a strong statistical significance, whereas for the AIS-based clustering the p-value was equal to 0.0186. These results suggest that, even if both clustering methodologies revealed significant differences among groups of individuals, the MF clustering can better separate clusters, as evidenced by the lower p-value. This difference points out the MF clustering ability to capture a broader range of variables that influence the rehabilitation process, beyond the mere severity of the injury.
For both clustering methods the results from the Kruskal-Wallis test showed statistically significant differences when comparing the adoption of TWT-1, TWT-2, TWT-3 or TWT-4 across the four AIS-based clusters and across the three MF clusters with each other (p<0.01). Only two exceptions were found: i) for the AIS-based clustering, the median adoption of TWT-4 remained consistent across all clusters (p>0.05); ii) for the MF clustering approach, TWT-2 displayed a p-value of 0.056, marginally above the standard cutoff, suggesting a slight deviation from median uniformity. Specifically, for AIS-based clustering, statistical analysis revealed p>0.05 for the AISc-B and AISc-C clusters in the TWT-4 vs TWT-2/TWT-3 comparison, and for the AISc-D cluster in the TWT-2 vs TWT-3 comparison. Conversely, for the MF clustering, p>0.05 was reported only in the MFc-3, in the comparisons TWT-2 vs TWT-3/TWT-4 and TWT-3 vs TWT-4.
The results of the Kruskal-Wallis test for the analysis of TAU indicate statistically significant differences when comparing TAU-1, TAU-2, TAU-3, TAU-4 across the four AIS-based clusters and across the three MF clusters (p< 0.01). As for the TWT, an exception was found also in this case, but it was present for both clustering approaches. The median value of TAU-3 remained consistent across all clusters, with a p-value of 0.051.
4. Discussion
This study aimed to quantify the distribution of TAU and TWT adopted in neurorehabilitation programs of individuals with SCI with a specific focus on a selected Italian Spinal Cord Unit which includes PTs with at least three years of neurorehabilitation experience and who are trained and constantly updated in using technological devices. Results should be interpreted considering that they refer to a set of technologies specifically available in the setting under analysis and which clearly do not cover the full spectrum of solutions potentially available on the market or in other rehabilitation hospitals. Nonetheless, we think that our results can still be considered relevant for researchers and clinicians interested in the application of non-conventional solutions as add-on to rehabilitation paths.
The scientific literature on SCI neurorehabilitation states quite clearly that technologies should be considered as complementary aids to enhance the effectiveness of the conventional treatment [
60]. Anyhow, the quantification of the adoption of technologies in the clinical daily practice compared to conventional treatment has not been investigated in the field of SCI. Indeed, the scientific literature includes papers focusing on the analysis of devices effectiveness or seldomly on the barriers, advantages and disadvantaged for their use, but no data on the actual technology adoption in daily clinical practice are available at best of our knowledge. According to the results of our selected Italian Spinal Cord Unit, the amount of TWT is on average about 30% of the total therapies for all individuals with SCI, independently from the clustering approach. However, we cannot state if technologies can be considered underutilized or not because similar data on the actual adoption in daily rehabilitation is not easily traceable. Indeed, the only available data is mainly coming from mere indirect indications on market dimensions provided by manufacturers and market leaders related to their products [
60]. On this basis, literature generally suggests that the rate of technology adoption is quite limited due to a number of barriers [
60], despite TWTs present several advantages such as the possibility to perform intensive and task-oriented motor activities, to monitor and objectively quantify performance in real-time and/or along time or to take advantage of continuous feedback thus promoting motivation and engagement [
61,
62,
63].
The possible barriers that can contrast TWT adoption may include technological barriers such as the setup of the devices, the complexity of use, the level of training necessary for PTs to master the technology [
60]. Furthermore, the migration to technology-aided rehabilitation may be perceived as a de-personalization of treatment from the patient point of view, increasing the dislike and the impression to feel controlled by a machine. Users’ behaviors and motivations when using and interacting with rehabilitation devices may be considered key factors for the acceptance of individuals with SCI of the use of this technology. These factors include personal beliefs and perceptions of advantages and disadvantages of the use of a device [
36]. Besides the patient's point of view, the PTs may prefer long standing traditional rehabilitation methods or may be influenced by a limited knowledge of the available technologies and their potential functionalities. In fact, PTs should be constantly updated on innovations, which require learning new solutions and new characteristics and capabilities of the upgrades of the different devices [
60]. Besides, the presence of expert personnel was perceived positively by individuals with SCI, primarily due to the sense of safety and trust they provided during the delivery of TWT [
36]. This finding suggests that the involvement of skilled professionals is important in enhancing the overall experience and acceptance of technologies. From the organizational point of view, the introduction of technology-aided rehabilitation also requires dedicated training for the staff of PTs and especially an increase of the complexity in the management of therapeutic planning. Moreover, the adoption of new technologies often requires a reorganization of activities and redistribution of goals, interests and responsibilities within the clinical organization, thus potentially increasing the resistance from the clinical staff. In the care of individuals with SCI, also Medical Doctors play a key role. The heterogeneity of technologies adopted within a neurorehabilitation framework requires not only the PTs but also, and maybe especially, the prescribing Medical Doctors to have a clear awareness of the potentialities of each technology, as well as of any exclusion criteria that prevent their use for specific individuals with SCI. Unfortunately, the scientific proofs of the benefits of all the available technology-aided training, or even the superiority over conventional solutions, are sometimes not clearly stated or controversial for the overall spectrum of SCI neurological features. Furthermore, there is a lack of well-defined guidelines to implement specific and effective protocols. To this aim periodic team meetings are held in the FSL Spinal Cord Unit, in which the team, including medical doctors and PTs, evaluates the progress in using technological devices and make decisions about continuing, modifying or discarding ongoing therapies. Other possible limitations for many rehabilitation centers may be the overall costs for the purchase and maintenance of technologies or the questionable benefit-cost ratio. These uncertainties might support the preference of conventional therapy and possibly discourage investment in technologies.
In this study, individuals with SCI were grouped according to two different approaches: a conventional method based on the AIS [
3] level classification (AIS-based clustering) and a newly developed method that classifies individuals by taking multiple characteristics into account (MF clustering). This second approach was conceived by considering that besides neurological features, the range of functional improvements following SCI [
38], as well as the rehabilitation goals and hospitalization duration may vary even among individuals with the same AIS classification [
64]. Indeed, even if individuals with SCI apparently can be considered comparable when classified according to the AIS level, they may actually achieve different ranges of functional recovery, also because they start from a different level of independence in the ADLs, especially after incomplete SCI [
38]. The purpose of multifactor clustering was not to propose a new classification of neurological impairment that can replace the AIS-based approach, but rather to provide better insights on technology adoption in the neurorehabilitation treatments of individuals with SCI by considering both neurological and functional recovery. As mentioned above, results showed that the amount of TWT is on average about 30% of the total therapies for all individuals, independently from the clustering approach. Although the overall percentage of technology adoption did not differ substantially among the clusters, some interesting differences may be highlighted by analyzing technology distribution on the basis of rehabilitation goals, i.e. by comparing TWT-1, TWT-2, TWT-3 and TWT-4. Considering AIS-based approach, for AISc-A and AISc-B the most selected treatment goal was muscle tone control and modulation (TWT-1) while the other types of TWT were seldom adopted. Even for AISc-C and AISc-D, TWT-1 was the most frequent strategy since muscle tone modulation is pursued regardless of the AIS level. TWT-3 and mainly TWT-2 were proposed respectively to improve walking ability and balance control, particularly for individuals with thoracic or lumbar SCI. The main difference between AISc-C and AISc-D categories was that in case of AISc-D a higher level of BP and BPP adoption for balance rehabilitation, and of TB Exo and TA FES for gait rehabilitation, was observed. No statistical differences were noted across AIS-based clusters for TWT-4, suggesting a similar level of adoption of this category of technologies in the neurorehabilitation program. The deeper analysis of TWT adoption based on the MF clustering allows for a more insightful tuning of the neurorehabilitation (technology-aided or conventional) proposed to individuals with SCI, by taking into account not only AIS level but also richer data. Indeed, AIS-based classification flattens important information on the functional status and on the independence in performing ADLs of each individual with SCI, because it disregards the concrete possibility to have heterogeneous clinical and functional conditions within the same AIS level. In the case of MFc-1 there is almost exclusive use of TWT-1 technologies (about 94%), particularly the Ce device, and TWT-2 is the least utilized. Technologies deputed to gait recovery are slightly more utilized than those for upper limbs. For MFc-2 and MFc-3, there is an almost similar use of technologies for muscle tone modulation (Ce device). On the contrary, FES Ce was more adopted and TWT-4 was never used for MFc-2. TWT-3 devices were more widely used in cluster MFc-3. All these differences were statistically significant whereas no statistically significant difference among MF clusters were noted for TWT-2. The technology use for muscle tone modulation, gait recovery and upper limb function, was higher in individuals belonging to MFc-3, with respect to the ones of MFc-2, since they have a greater functional deficit. Moreover, individuals with cervical injury can benefit from a greater spectrum of technological solutions because of the possibility of taking advantage of tools for the upper limbs in addition to those for the lower limbs. Furthermore, individuals with cervical lesion remained hospitalized longer than individuals with thoracic or lumbar lesions belonging to AISc-B, AISc-C and AISc-D. The lower the injury level, the shorter the average hospitalization duration in case of sensorimotor incomplete lesions. This pattern is totally reversed only for AISc-A for which longer stays are reported for lumbar lesions with respect to the cervical ones (
Figure 1.b). This may depend on the potential recovery and related functional goals planned to manage the discharge from the Spinal Cord Unit. For example, an individual with a complete cervical injury might have a relatively easy to reach rehabilitation goal, such as the autonomous management of a powered wheelchair. This goal might be achieved faster than the target of an individual with lumbar complete lesion, who aims to regain functional ambulation by using walking aids and braces. Moreover, for the MF clustering in case of sensorimotor incomplete SCI (MFc-2 and MFc-3), individuals with cervical lesion (lower SCIM score) stay longer than thoraco-lumbar ones (higher SCIM score) into the Spinal Cord Unit. Overall, the individuals included in MFc-1 showed the lowest SCIM score at admission and remained hospitalized longer than the other two groups of individuals with incomplete injuries.
Analyzing TWT categories, the most frequently adopted device was the Ce, followed by FES Ce, independently from the clustering approach. The reason is probably due to the limited number of contraindications of these systems (almost all individuals are suitable for their adoption) and to their ease of application. These tools can be used without a direct intervention from PTs (i.e. by just relying on their supervision), thus also ensuring longer rehabilitation sessions. On the contrary, TWT-2, TWT-3 and TWT-4 were largely less utilized since they required the direct intervention from the PT. Indeed, not everyone was able to perform tasks more complex than those faced with TWT-1 devices, which simply required the patient to be sitting in the wheelchair or lying on the bed. Among the TWT-2 devices, the BP was used much more than the BPP, even though they both had quite similar functionalities when working in a standing position. This may be because BP can also be used in a seated position or even directly in the wheelchair in case of individuals unable to maintain standing. Hence, BP can be considered to have a greater usability compared to the BPP. For technologies included in TWT-3, the TB Exo was more used than both OG Exo and TA FES. Factors that may reduce the adoption of these two devices include the long time required for system setting and patient’s preparation, the non-negligible spectrum of contraindications inherent in the type of device and, consequently, the reduced number of individuals who could benefit from them. Moreover, for OG Exo two PTs are simultaneously required to safely manage the user, whereas TA FES can be used in a reduced number of individuals since ambulation is not feasible for everybody and since its usage is quite specific for deficits to ankle dorsiflexor muscles. Regarding upper limb technologies, the MI BCI device was used more extensively than MT because it does not require motor engagement and thus allows all individuals, even those with severe upper limb impairments, to take advantage of it. For the sake of completeness, it is worth adding that actually the validity of MI BCI for recovery of upper limb function has been demonstrated for stroke survivors and it is currently under investigation for individuals with SCI [
55]. It is worth to specify that no difficulties or delays were encountered in the delivery of the above-mentioned TWT, since FSL clinical engineering department was constantly engaged in the maintenance of the devices to make them constantly working.
Although the main focus of the study was on quantifying technology adoption, the categorization of TAUs and related analysis provides interesting information. For both clustering methods, significant differences were found for TAU-1, TAU-2 and TAU-4 in the comparison among MF clusters and among AIS-based clusters. This indicates differences in the adoption of exercises focused on joint range of motion maintenance, muscle tone modulation and force control (TAU-1), transfers and trunk control (TAU-2) or gait ability (TAU-4).
Indeed, conventional SCI rehabilitation is typically well addressed in many literature studies but no clear data on the rehabilitation programs categorized by functional goals during hospitalization are available. The AIS-based clustering showed that for individuals grouped in AISc-A and AISc-B a wide administration of TAU-1 and TAU-2 emerged. In this case, TAU-1 was proposed mainly to prevent the onset of secondary complications due to SCI [
6], such as muscle shortenings or tone alterations, decreased range of motion, pressure sores or neurogenic heterotopic ossification onset and to only strengthen uninjured motor districts above the level of injury [
65,
66]. Moreover, TAU-2 was proposed to train transfers and trunk control with the purpose of promoting as much autonomy as possible. Besides TAU-1 and TAU-2, mainly TAU-3 was proposed to train individuals to reach and maintain standing position and to facilitate orthostatic hypotension control, promote bowel functionality and improve bone mineralization by reducing the risk of severe osteoporosis and the occurrence of spontaneous fractures [
67]. The amount of TAU-4 was very limited, since only few individuals classified as AISc-A with low thoracic or lumbar injury can recover walking function by using braces, walking aids and physical assistance, and only a small proportion of AISc-B individuals can recover walking function [
68]. Even in the case of AISc-C and AISc-D, there was a prevalence of TAU-1, less than AISc-A and AISc-B clusters, which was mainly oriented towards strengthening the unimpaired districts and promoting the best motor recovery achievable below the lesion level. The second most frequently administered therapy was TAU-2, delivered to promote independence and to prepare the trunk control during most complex activities like standing or walking, followed by TAU-3. Individuals with SCI usually begin to experience upright standing position maintenance within parallel bars to ensure upper limb support in maintaining standing position, to allow the musculoskeletal system to accept the load progressively, and to promote proper bowel and bladder functions. TAU-4 was proposed more frequently to individuals in AISc-D than to those in AISc-C, since the former ones have the motor skills needed to walk again (with or without an aid, depending on the lesion) more suitable than all the other individuals [
68]. Also for TAU, the analysis of MF clustering provides additional broader information. Overall, the highest level of TAU-1 adoption was reported for MFc-1, where almost no TAU-4 was noted. In MFc-3 there was a greater use of TAU-1 and TAU-4, at the expense of TAU-2, than in MFc-2. Hence, there is a greater focus on muscle tone and recruitment in addition to walking than on balance training, even if in MFc-3 there are only individuals with cervical SCI. No differences across MF clusters were observed for TAU-3, suggesting no specific differences in the balance conventional rehabilitation.
From a statistical point of view, the analysis of the silhouette reveals a positive value for the MF clustering suggesting a higher level of separation across the clusters, in comparison to the negative score obtained for the four AIS-based clusters. This data is interesting since the AIS-based classification considers the neurological lesion in terms of completeness of the damage to the motor and/or sensory system (i.e. AIS level A, B, C or D) [
64]. Results indicate that MFc-1 includes almost all individuals with cervical or thoracic lesions classified as AIS A and B, whereas the individuals with lumbar complete lesions and with sensorimotor incomplete lesions were merged in the other two clusters: MFc-2 grouped thoracic and lumbar lesions, while MFc-3 included cervical ones. Therefore, in line with our initial hypothesis, the MF clustering was demonstrated to be capable of grouping the individuals based on neurological features and functional abilities. Individuals classified as AIS A and B, merged into the MFc-1, presented more severe functional injuries and less room for improvement whereas individuals with sensorimotor incomplete SCI (AIS C and D) were grouped separately based on the lesion level. Indeed, considering that the lower the level of the injury the greater the residual functional capacity, MFc-2 encloses less impaired individuals with respect to MFc-3. As reported above, this result does not claim to indicate that the proposed clustering approach can replace the worldwide adopted AIS classification. Rather, it suggests that a more thorough analysis can be conducted on technology adoption in case functional capabilities and hospitalization length are taken into account besides strictly analyzing neurological state. Identifying homogeneous subgroups for clinical trials can help to more accurately determine whether a therapeutic intervention is actually effective [
69]. The possibility in future works to potentially develop a classification method able to group an intrinsically heterogeneous population in homogeneous subgroups, considering both neurological and functional information, can be advantageous for studies on SCI, where difficulties can arise due to the significant differences in the participants [
64].
Our study provided useful information to identify technologies adopted for the treatment of specific groups of individuals with SCI, at least according to what commonly pursued during typical practice. Nonetheless, as anticipated, our results cannot be fully generalized since they are restricted only to a selected Italian Spinal Cord Unit with specific characteristics (number of PTs, years of experience in neurorehabilitation and in technology devices usage, internal scheduling procedures, etc.) and they do not cover a broad range of technologies available for clinical use. Moreover, the sample of individuals under analysis and the time window of observation can be considered relatively small. Hence, further studies are needed to deepen the topic of technology adoption. It would be interesting to reproduce this analysis in other SCI neurorehabilitation institutions to compare different Spinal Cord Unit in the same country, or even in different countries, considering the specificity of each environment. This would help understanding whether there are differences in technology adoption, which could be attributed not to the complexity of the technology itself but rather to the difficulty in the usage or management for a specific pathology. Further investigations could be devoted to analyze possible relationships between the amount of technology adoption and the actual effectiveness. The combination of data on the actual adoption of technologies in daily clinical practice coupled with effectiveness data could help for the selection of technologies to be acquired in a the Spinal Cord Unit with related training courses for the professionals who will use them. Another possible interesting aspect to be investigated is the potential influence of TWT adoption on the hospitalization duration, given that that the days of recovery are commonly used to measure the performance and efficiency of healthcare systems.
Figure 1.
Grouping of the cohort of individuals with SCI according to the AIS-based clustering: (a) Number of individuals for each cluster (AISc-A, AISc-B, AISc-C or AISc-D) grouped according to the lesion level; (b) SCIM score at the admission and hospitalization duration. Error bars in the bar graphs indicate standard deviation.
Figure 1.
Grouping of the cohort of individuals with SCI according to the AIS-based clustering: (a) Number of individuals for each cluster (AISc-A, AISc-B, AISc-C or AISc-D) grouped according to the lesion level; (b) SCIM score at the admission and hospitalization duration. Error bars in the bar graphs indicate standard deviation.
Figure 2.
Percentage of TAU or TWT adoption on the total amount of treatments administered for the individuals with SCI classified according to the AIS-based clustering.
Figure 2.
Percentage of TAU or TWT adoption on the total amount of treatments administered for the individuals with SCI classified according to the AIS-based clustering.
Figure 3.
Distribution of TAU-1, TAU-2, TAU-3, TAU-4 and TWT-1, TWT-2, TWT-3, TWT-4 for the total cohort of individuals with SCI (pie charts) and for each AIS-based clustering, classified according to the lesion level (cervical, thoracic or lumbar lesion).
Figure 3.
Distribution of TAU-1, TAU-2, TAU-3, TAU-4 and TWT-1, TWT-2, TWT-3, TWT-4 for the total cohort of individuals with SCI (pie charts) and for each AIS-based clustering, classified according to the lesion level (cervical, thoracic or lumbar lesion).
Figure 4.
Dendrogram obtained from the hierarchical clustering approach visually representing the arrangement of MF clusters produced by the analysis. Each cluster is represented by a specific color (blue for the whole SCI population, green for MFc-1, light blue for MFc-2, and red for MFc-3).
Figure 4.
Dendrogram obtained from the hierarchical clustering approach visually representing the arrangement of MF clusters produced by the analysis. Each cluster is represented by a specific color (blue for the whole SCI population, green for MFc-1, light blue for MFc-2, and red for MFc-3).
Figure 5.
Grouping of the cohort of individuals with SCI according to the MF clustering: (a) Number of individuals for each cluster (MFc-1, MFc-2, MFc-3) grouped according to the lesion level and AIS-based classification; (b) SCIM score at the admission and hospitalization duration.
Figure 5.
Grouping of the cohort of individuals with SCI according to the MF clustering: (a) Number of individuals for each cluster (MFc-1, MFc-2, MFc-3) grouped according to the lesion level and AIS-based classification; (b) SCIM score at the admission and hospitalization duration.
Figure 6.
Percentage of TAU or TWT adoption on the total amount of treatments administered for the individuals with SCI, classified according to the MF clustering.
Figure 6.
Percentage of TAU or TWT adoption on the total amount of treatments administered for the individuals with SCI, classified according to the MF clustering.
Figure 7.
Distribution of TAU-1, TAU-2, TAU-3, TAU-4 and TWT-1, TWT-2, TWT-3, TWT-4 for each MF clusters MFc-1, MFc-2, MFc-3 (pie charts), classified according to the lesion level (bar graphs).
Figure 7.
Distribution of TAU-1, TAU-2, TAU-3, TAU-4 and TWT-1, TWT-2, TWT-3, TWT-4 for each MF clusters MFc-1, MFc-2, MFc-3 (pie charts), classified according to the lesion level (bar graphs).
Table 1.
Available technologies at FSL Spinal Cord Unit classified into Treatment With Technologies (TWT) categories.
Table 1.
Available technologies at FSL Spinal Cord Unit classified into Treatment With Technologies (TWT) categories.
| Treatment With Technologies (TWT) category |
Device |
Device acronym |
| TWT-1 |
Cycloergometer |
Ce |
| Functional Electrical Stimulation-aided Cycloergometer |
FES Ce |
| TWT-2 |
Balance Plate |
BP |
| Balance Perturbation Plate |
BPP |
| TWT-3 |
Tibialis Anterior Functional Electrical Stimulation |
TA FES |
| Lower limb Treadmill-Based exoskeleton |
TB exo |
| Lower limb OverGround exoskeleton |
OG exo |
| TWT-4 |
Upper limb Motor Imagery Brain Computer Interface |
MI BCI |
| Upper limb Game based Motor Trainer |
MT |