1. Introduction
Climate change has been described as “the biggest global health threat of the 21st century
”. [
1] WHO clearly states that climate change impacts health in many different ways, both directly (extreme weather events) and indirectly (for example it can lead to food, nutrition and water insecurity). [
2] Since environmental health is closely related to human health [
3] the urgency of global climate change demands that all sectors, including healthcare, adopt more sustainable practices. The healthcare sector itself contributes significantly to global greenhouse gas (GHG) emissions, accounting for approximately 4-5% of total emissions [
3,
4,
5]. If global healthcare were a country, it would be the fifth largest carbon emitter on the planet. [
6] Within this sector, anaesthesia is a major contributor due to the use of potent greenhouse gases and disposable materials, therefore the role of aneaesthesia providers is crucial in reducing the environmental impact of their practice [
7]. Anaesthetic agents such as isoflurane, desflurane, sevoflurane and nirous oxide have atmospheric lifetimes and global warming potentials far exceeding those of carbon dioxide [
8]. The environmental impact of these gases, along with the waste from single-use anesthesia equipment, highlights a critical yet often overlooked aspect of healthcare sustainability.
The transition towards greener anesthesia is not only an ethical imperative, aligning with the broader healthcare goal of 'Primum non nocere' (First do no harm), but also a pragmatic step towards future-proofing anaesthetic practice
[6,9]. As climate change drives policy and regulation, anaesthesiologists, like other healthcare professionals, will face increasing pressure to minimize the environmental impact of their practice.
This transition involves adopting less harmful anaesthetic agents, integrating novel technologies, and implementing systemic changes to reduce waste and promote recycling. The COVID-19 pandemic has further accelerated discussions around healthcare sustainability, emphasizing the need for resilient, adaptable, and eco-conscious medical practices. It has demonstrated the healthcare sector's ability to adapt swiftly, indicating that transitioning towards sustainable anesthesia is both realistic and achievable with concerted effort.
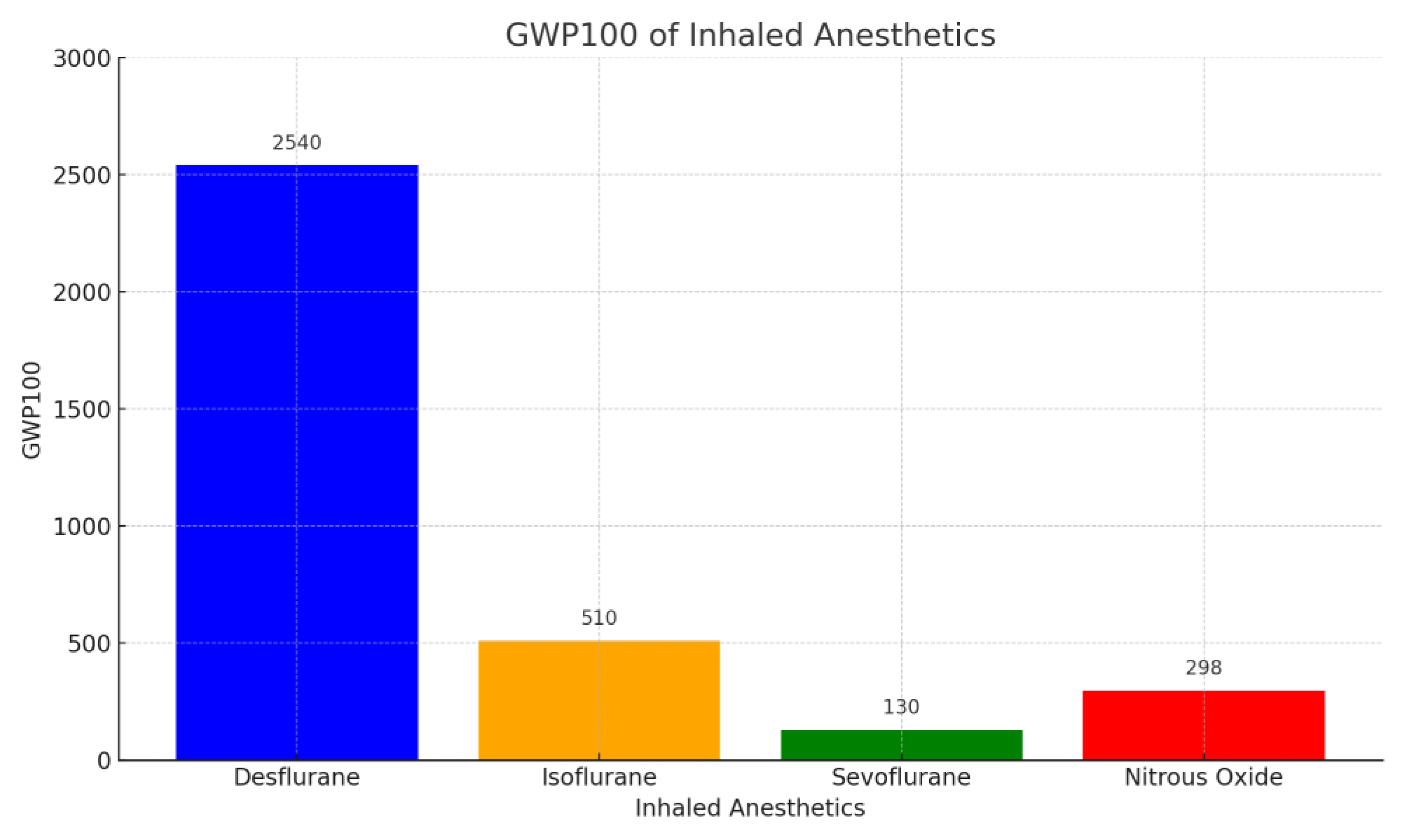
2. Environmental Impact of Inhaled Anaesthetics
Inhaled anaesthetics integral to contemporary anaesthesia practice present a profound environmental challenge primarily due to their high Global Warming Potential (GWP). These agents during the clinical usage undergo only to minimal metabolism and are exhaled almost unmodified and then released as waste anaesthetic gases (WAG) in the atmosphere. Here they act as GHGs contributing to global warming. Commonly used inhaled agents such as desflurane, sevoflurane, isoflurane and nitrous oxide exhibit GWPs of 2540, 130, 510 and 265 times that of carbon dioxide over a 100-year horizon [
6,
8] (
Figure 1).
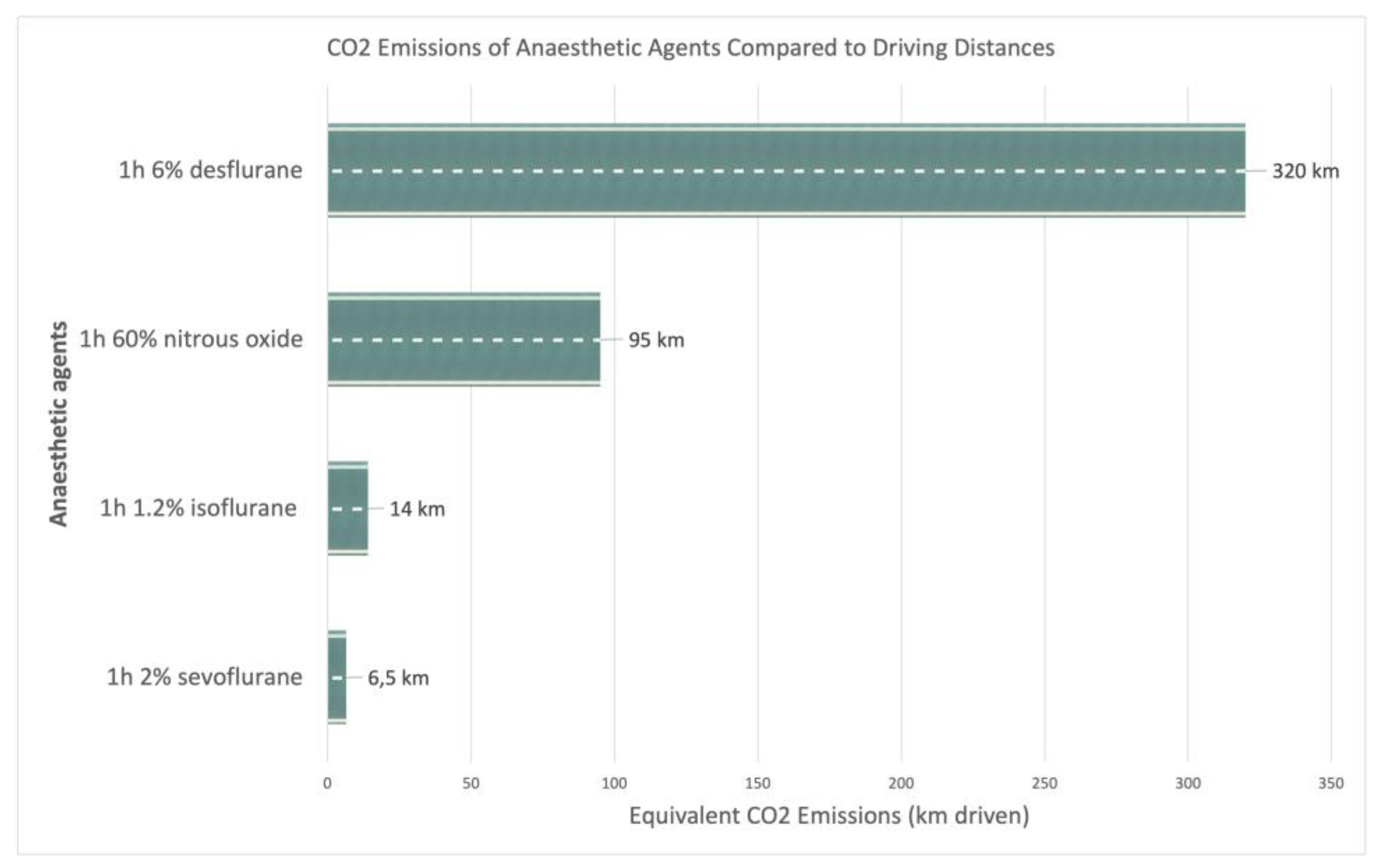
This stark contrast in GWP values underscores the critical need to mitigate their environmental impact. Various authors to better illustrate the magnitude of this problem, have compared the CO2 emissions per hour (CO2 equivalent, CDE) of these aneaesthetic agents used at 1MAC to those produced by driving different distances by car (
Figure 3):
- -
One hour of 2% sevoflurane emits a CDE similar to that driving 6.5 km
- -
One hour of 1.2% isoflurane emits a CDE similar to that driving 14 km;
- -
One hour of 60% nitrous oxide emits a CDE similar to that driving 95 km;
- -
One hour of 6% desflurane emits a CDE similar to that driving 320 km. [
10,
11]
Figure 2.
CO2 equivalent for 1 MAC-hour of common anesthetic gases in kilometers driven.
Figure 2.
CO2 equivalent for 1 MAC-hour of common anesthetic gases in kilometers driven.
In 2010, Sulbaek Andersen., et al. estimated that yearly global emission from inhaled anesthetics is equivalent to gas emissions by 1 million passenger cars [
12]. The atmospheric lifetimes of these halogenated agents, ranging from approximately 1.1 to 14 years, amplify their long-lasting detrimental effects on the environment [
13]. The claim that operating anaesthesia machines are energy-intensive is incorrect; their energy consumption is negligible compared to the impact of anaesthetic gases and reusable/disposable equipment.
Nitrous oxide has a much longer atmospheric lifetimes, more than 100 years and it also depletes ozone layer [
8,
13]. Because of this double effect as GHG and ozone depleter the use of nitrous oxide as carrier gas can dramatically increases the global warming effects of other agents such as sevoflurane [
8].
Furthermore, while there is concern regarding the health risks posed to healthcare workers from occupational exposure to waste anaesthetic gases, these gases have been used safely for decades, with well-studied occupational risks. Ongoing research and development of effective mitigation strategies are necessary to safeguard both environmental and occupational health [
8,
14].
The regulatory and policy landscape is evolving in response to the environmental repercussions of anaesthetic gases. There is increasing recognition across healthcare sectors of the need for environmentally sustainable practices, with anaesthesia playing a leading role. Recent policy developments reflect a growing willingness to address the environmental impact of medical practices, signaling potential future shifts in anaesthesia practice. These changes are crucial in steering the field towards more sustainable and environmentally responsible methods, ensuring the healthcare sector contributes positively to global efforts in combating climate change.
3. Strategies for Sustainable Anaesthesia
Sustainable practices in anaesthesia are essential in mitigating the significant environmental impact of anaesthetic gases. The most simple and effective measures that anaesthesiologist can take to reduce their carbon footprint are:
- -
Choose the agent with the lower GWP: avoid desflurane and nitrous oxide, their use should be restricted to only specific cases [
6,
7,
15]. In clinically equivalent doses, ranked climate impacts: desflurane > nitrous oxide > isoflurane > sevoflurane.
- -
Utilize low fresh gas flow: using low flow anaestehesia (LFA) allows to reduce the total amount of gas required so there is a smaller environmental and operating room pollution and also a reduction of the costs. It also consent to preserve a better humidification and heat of the circuit, that is beneficial for the homeostasis of the patient [
14,
16]. There is no universal definition of LFA, according to Baker classification low flow is considered a FGF of 500-1000ml [
17].
- -
Prefer techniques that minimize the use of inhalation agents such as regional and total intravenous anaestehesia [
15,
18].
These recommendation are encouraged by the ASA Task Force on the Environment, when clinically appropriate [
18].
Another strategy to minimize the impact of WAGs is employing technologies like Sedaconda™ ACD-S to capture and recycle exhaled anaesthetics [
6,
19]. This device is designed for administering volatile anaesthetics like isoflurane and sevoflurane more efficiently, reducing gas consumption and consequently their GWP. It can be described as a small single-use anaesthetic vaporizer integrated with an HME filter in one airway component. Like an HME filter, the device returns moisture to the patient, but also reflects 90% of the anaesthetic by adsorbing and then releasing the drug using a special carbon filament reflecting medium. This recycling process lowers the overall amount of anesthetic required, reducing that which is exhausted or scavenged upon exhalation [
20]. The ASA sustainability checklists encourages research on anaesthetic gas trapping devices [
21].
Other practical measures include ensuring good seals with airway devices, using cuffed tubes in pediatrics and minimizing disconnections between the anaesthetic circuit and machine [
22].
Transitioning to Intravenous Anaesthesia
Transitioning to intravenous (IV) anaesthesia can significantly reduce the GWP associated with anaesthetic practices by eliminating the use of volatile gases with high GWPs. IV anaesthetics do not directly contribute to atmospheric greenhouse gases. The indirect environmental impact is a result of their manufacture, packaging, transportation but also the use of delivery systems, drug wastage and disposal [
23]. Despite involving the use of electrically powered pumps, their overall energy consumption is lower than that of anaesthesia machines for volatile gases. Considering the life-clycle assassement of propofol TIVA related GHG emissions are 4 times smaller than that from desflurane and nitrous oxide [
22,
24].
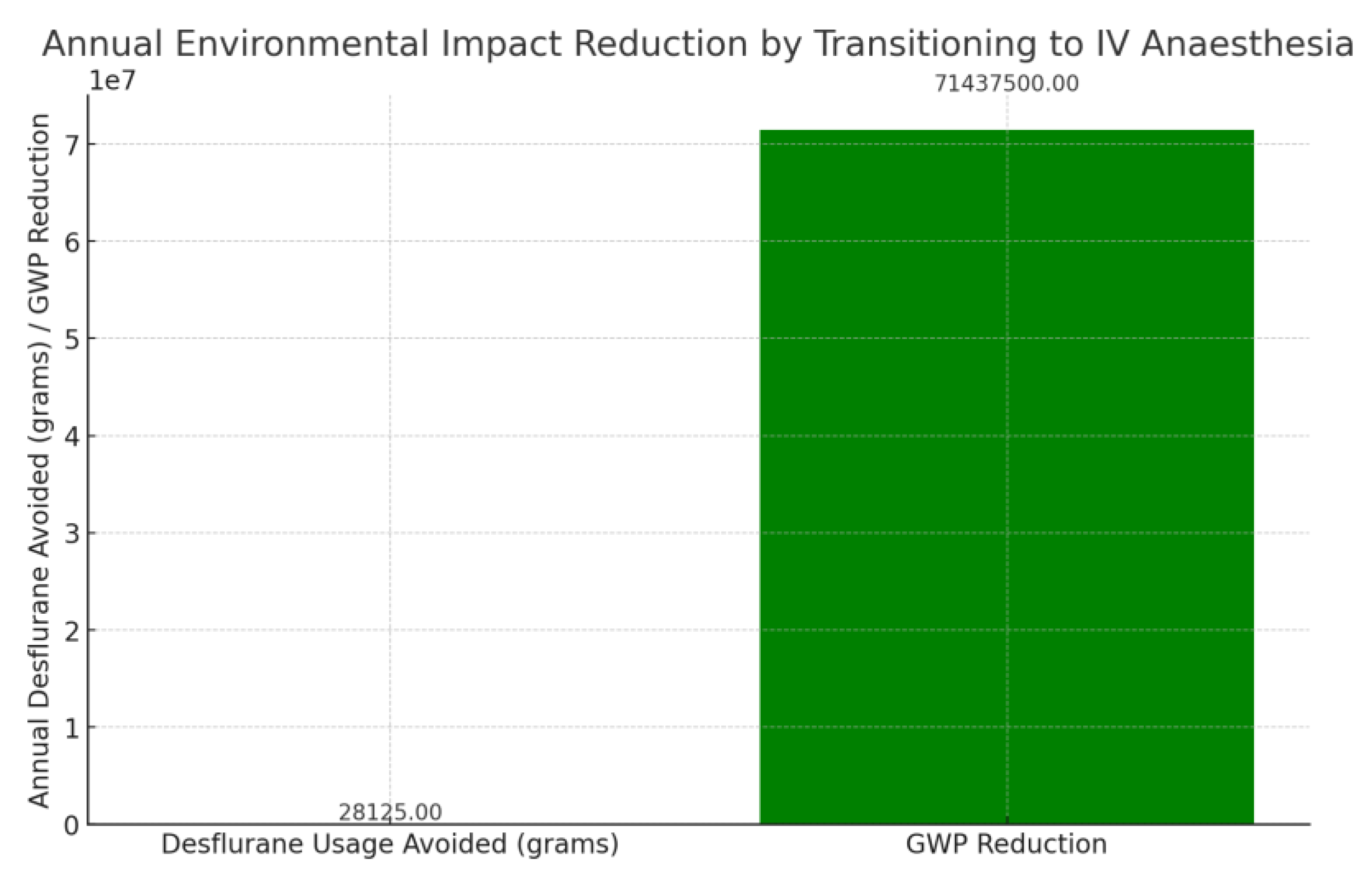
To quantify GWP reduction, consider a medium-sized hospital transitioning 50% of its anaesthetic procedures from desflurane to IV anaesthesia. If each procedure avoids the use of 15 mL of desflurane (density ~1.5 g/mL), the GWP reduction can be estimated as follows:
Daily desflurane usage avoided: 15 mL/procedure × 1.5 g/mL × number of procedures/day.
Annual usage avoided: Daily usage × number of operating days/year.
GWP reduction: Annual usage (in grams) × GWP of desflurane (2540 over 100 years).
Figure 3.
a graph representing the annual environmental impact reduction by transitioning 50% of anaesthetic procedures from desflurane to intravenous anaesthesia in a medium-sized hospital. The graph shows the annual desflurane usage avoided (in grams) and the corresponding GWP reduction. .
Figure 3.
a graph representing the annual environmental impact reduction by transitioning 50% of anaesthetic procedures from desflurane to intravenous anaesthesia in a medium-sized hospital. The graph shows the annual desflurane usage avoided (in grams) and the corresponding GWP reduction. .
To further reduce the environmental impact of propofol life-cycle is important to consider minimizing the requirement of single-use plastic and drug wastage. It has been found that within a small surgical suite wasted or discarded propofol accounted for 45% of all the drug waste. It is then recommended to avoid unnecessary drug preparation and prefer the use of small size vials of propofol 20ml versus 50 or 100ml in the operating room [
23,
25].
Collaborative efforts with environmental scientists and policymakers are essential for developing guidelines and supporting research on alternative anaesthetic agents and innovative technologies. Community engagement through awareness campaigns is vital for public understanding and support for sustainable anaesthesia practice [
26,
27]
Environmental impact of the peri-operative assistance is relevant. Operating rooms are responsible for 20 to 30% of all hospital waste [
18,
28] and are highly energy-intensive, therefore all the members of the surgical equip should minimize the overuse and waste of drugs and equipment, along with the use of energy and water [
7]. Anaesthesia providers should use the approach of “reduce, reuse, recycle” to promote the reduction of unnecessary waste [
15].
Routinely drug waste is estimated to account for 25-30% of the total anaesthesia budget, therefore is both responsible for an environmental pollution and economic loss. The amount of propofol wasted is up to 49% [
29]; there is also a huge drug wastage of cardiac resuscitative medication such as ephedrine, atropine, phenylephrine but also paralytic agents, all these are being routinely prepared in advance but then remain unused and discarded up to 30-50% of the time [
30,
31].
Simple strategies to prevent waste could be keeping
emergency ampoules and syringes on hand so that they can be easily prepared when needed, usage of pre-filled syringes of commonly used anesthesia drugs [
15,
32] and prefer smaller vials such already mentioned above [
9].
More than one third of the waste produced by the operating room is generated before the arrival of the patient so it is composed of materials clean, that are not contaminated or infectious, therefore it can be considered almost all “general/domestic waste” that need to be discarded properly in recycling bin according to the type of materials [
9,
33].
Anesthesia-related waste representing as much as 25% of all trash produced during surgery and there are a lot of potentially recyclable products such as surgical instrument wraps (including blue wrap), forced-air warming blankets, saline and water ampoules and bottles, uncontaminated intravenous fluid bags and tubing , oxygen masks and tubing, suction tubing, uncontaminated syringes, hard plastic packaging (procedure equipment trays, ex. central line trays), boxboard, paper package inserts, rippable paper packaging, glass vials [
15].
Still there is no adequate information on the importance of recycling and on how to properly recycle intraoperatively [
34].
In the project “greening the operating room” the ASA Committee on Environmental Health proposes a sustainability checklist [
21].
Table 1.
3.1. Implementation Challenges and Proposed Solutions
Implementing sustainable strategies in anaesthesia faces several challenges, including a lack of awareness and education among providers, technological barriers, resistance to change, and policy limitations.
Lack of Awareness and Education
Many anaesthesiologists are not fully aware of the environmental impact of their practices or the available eco-friendly alternatives. Addressing this gap requires integrating sustainability-focused education into anaesthesia curriculums and regular professional development programs [
7,
35]. Simple free tools for estimate personal’s anaeshetic carbon footprint could be the Yale Gassing Greener and the Association of Anaesthetists Anaesthetic Gases Calculator [
6].
Technological Barriers
The limited availability or high cost of green technologies can hinder their adoption. Advocacy for increased research funding and incentives for manufacturers to develop affordable solutions is crucial. Overcoming these barriers involves strategic change management and engaging key opinion leaders to champion sustainable practices [
36].
Resistance to Change
Resistance to change in anaesthesia practice can be mitigated through strategic change management, including engaging key opinion leaders to champion sustainable practices and demonstrating the long-term cost-effectiveness of sustainable practices [
37].
Policy and Regulatory Limitations
The current policy and regulatory environment does not adequately support sustainable anaesthesia practices. Collaboration with relevant bodies to develop and advocate for supportive policies is necessary. Economic constraints within healthcare systems can be addressed by demonstrating the long-term cost-effectiveness of sustainable practices and exploring funding avenues for initial investments [
38]. Also NICE, in his program for 2021-2026, promotes an approach that should consider not only the health impact on economic but also on the environment and encourage the health and care system to reduce its carbon footprint [
39].
Standardized Systems and Monitoring
Standardized systems are needed to measure the environmental impact of anaesthesia practices accurately and monitor progress. Interdisciplinary collaboration is essential to understand the full spectrum of environmental impacts and develop comprehensive mitigation strategies [
40,
41].
Addressing Global Disparities
Addressing global disparities in resources and infrastructure is crucial for the widespread implementation of sustainable anaesthesia practices. This requires international collaboration and context-specific strategies [
42].
4. Monitoring and Evaluating Sustainable Anaesthesia Practices
In the quest for sustainability in anaesthesia, continuous monitoring and evaluation of eco-conscious practices are crucial. Establishing specific, measurable Key Performance Indicators (KPIs) aligned with broader healthcare sustainability goals is essential. These KPIs should encompass aspects such as GHG emissions reduction, waste minimization, and energy efficiency in anaesthesia departments [
40]. During 2023 ASA proposed the “inhaled anesthetic challenge” with the goal of reducing the carbon emissions produced by the inhaled anesthetic by 50% [
43]. Other KPIs could be the amount of plastic recycled or the amount of cardiovascular emergency drugs saved [
44].
An easy task could be also reducing the amount of unnecessary endo-venous paracetamol and promoting the oral route whenever is possible with a reduction of the carbon footprint of one of the most commonly prescribed drug for analgesia (CDE of 1 g of oral paracetamol are eight times less than those of the correspondent endo-venous dose in a plastic vial) [
45].
Data Collection and Analysis
Rigorous data collection and analysis are instrumental in assessing KPIs. Utilizing advanced analytical tools to understand resource utilization patterns, waste generation, and emission levels is necessary. Simple methods for data collection and analysis can be implemented to assess personal and departmental performance without waiting for sophisticated tools [
46].
Benchmarking and Continuous Improvement
Benchmarking against national and international standards offers a framework for evaluating the success of sustainability efforts. Regularly scrutinizing collected data helps identify successes and areas needing improvement, fostering a culture of continuous improvement [
47].
Technological Advancements
Digital tracking systems and automated reporting tools offer real-time insights crucial for prompt adjustments and decision-making. Assessing the long-term impacts of sustainable practices on both the environment and healthcare outcomes ensures alignment with enduring sustainability objectives [
46].
5. Conclusions
The healthcare sector significantly contributes to global greenhouse gas emissions, and the role of anaesthesia, particularly through the use of high Global Warming Potential (GWP) gases like isoflurane, desflurane, sevoflurane and nitrous oxide, is a focal point for sustainable reform [
11].
The evidence underscores the urgent need for the healthcare community, especially within anaesthesia, to reassess and modify practices in line with environmental sustainability. Strategies such as optimizing delivery system efficiency, reducing waste, and transitioning to less harmful anaesthetic agents or techniques like intravenous anaesthesia or locoregional and low-flow methods are feasible and necessary steps towards reducing the specialty’s carbon footprint [
48,
49].
Incorporating lifecycle assessments in healthcare emissions accounting provides a comprehensive view of the environmental impact of anaesthetic drugs from production to disposal. This holistic approach is crucial for understanding and mitigating the climate impact of healthcare practices [
13].
Reducing climate impact contributes to public health but also is a way to saving health care system money that can be transformed in more resources for patient care and other goals [
50]. A more sustainable approach is therefore a benefit for our health, the planet’s health, and for the financial system [
51].
Advancing sustainable anaesthesia involves adopting greener anaesthetics and technologies and a systemic shift in education, policy-making, and clinical culture. By actively engaging in this transition, anaesthesiologists can significantly contribute to global efforts to curb climate change, aligning with the broader healthcare mission of 'Primum non nocere' – first do no harm [
4].
In conclusion, a concerted effort among clinicians, policymakers, and stakeholders is necessary to embrace sustainable anaesthesia practices, thereby reducing the environmental impact of healthcare and fostering a culture of ecological responsibility [
52].
Author Contributions
Conceptualization, E.S. and I.C.; methodology, I.C.; software, I.C.; validation, E.S., I.C..; formal analysis, I.C.; investigation, I.C.; resources, E.S.; data curation, I.C.; writing—original draft preparation, I.C.; writing—review and editing, E.S. and L. C.; visualization, E.S.; supervision, E.S. project administration, E.S.; funding acquisition, I.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Costello, A.; Abbas, M.; Allen, A.; Ball, S.; Bell, S.; Bellamy, R.; Friel, S.; Groce, N.; Johnson, A.; Kett, M.; et al. Managing the Health Effects of Climate Change. Lancet and University College London Institute for Global Health Commission. The Lancet 2009, 373, 1693–1733. [CrossRef]
-
Compendium of WHO and Other UN Guidance on Health and Environment, 2024 Update; 2024; ISBN 9789240088061.
- Sherman, J.D. The Perioperative Garden of Eden. A & A Case Reports 2016, 6, 183–185. [CrossRef]
- Romanello, M.; Di Napoli, C.; Drummond, P.; Green, C.; Kennard, H.; Lampard, P.; Scamman, D.; Arnell, N.; Ayeb-Karlsson, S.; Ford, L.B.; et al. The 2022 Report of the Lancet Countdown on Health and Climate Change: Health at the Mercy of Fossil Fuels. The Lancet 2022, 400, 1619–1654. [CrossRef]
- Lenzen, M.; Malik, A.; Li, M.; Fry, J.; Weisz, H.; Pichler, P.-P.; Chaves, L.S.M.; Capon, A.; Pencheon, D. The Environmental Footprint of Health Care: A Global Assessment. The Lancet Planetary Health 2020, 4, e271–e279. [CrossRef]
- McGain, F.; Muret, J.; Lawson, C.; Sherman, J.D. Environmental Sustainability in Anaesthesia and Critical Care. British Journal of Anaesthesia 2020, 125, 680–692. [CrossRef]
- White, S.M.; Shelton, C.L.; Gelb, A.W.; Lawson, C.; Mcgain, F.; Muret, J.; Sherman, J.D. Principles of Environmentally-Sustainable Anaesthesia: A Global Consensus Statement from the World Federation of Societies of Anaesthesiologists Representing the World Federation of Societies of Anaesthesiologists Global Working Group on Environmental Sustainability in Anaesthesia*. 2021. [CrossRef]
- Varughese, S.; Ahmed, R. Environmental and Occupational Considerations of Anesthesia: A Narrative Review and Update. Anesthesia and Analgesia 2021, 133, 826–835. [CrossRef]
- Sherman, J.; McGain, F. Environmental Sustainability in Anesthesia: Pollution Prevention and Patient Safety. Advances in Anesthesia 2016, 34, 47–61. [CrossRef]
- Hanna, M.; Bryson, G.L. A Long Way to Go: Minimizing the Carbon Footprint from Anesthetic Gases. Canadian Journal of Anesthesia 2019, 66, 838–839. [CrossRef]
- Ryan, S.M.; Nielsen, C.J. Global Warming Potential of Inhaled Anesthetics. Anesthesia & Analgesia 2010, 111, 92–98. [CrossRef]
- Sulbaek Andersen, M.P.; Sander, S.P.; Nielsen, O.J.; Wagner, D.S.; Sanford, T.J.; Wallington, T.J. Inhalation Anaesthetics and Climate Change. British Journal of Anaesthesia 2010, 105, 760–766. [CrossRef]
- Andersen, S.; Nielsen, O.J.; Prof, A.; Peter, M.; Nielsen, O.J.; Sherman, J.D. Assessing the Potential Climate Impact of Anaesthetic Gases. Personal View Lancet Planet Health 2023. [CrossRef]
- Gaya da Costa, M.; Kalmar, A.F.; Struys, M.M.R.F. Inhaled Anesthetics: Environmental Role, Occupational Risk, and Clinical Use. Journal of Clinical Medicine 2021, 10, 1–23. [CrossRef]
- Petre, M.A.; Malherbe, S. Environmentally Sustainable Perioperative Medicine: Simple Strategies for Anesthetic Practice. Canadian Journal of Anesthesia 2020, 67, 1044–1063. [CrossRef]
- Brattwall, M.; Warrén-Stomberg, M.; Hesselvik, F.; Jakobsson, J. Brief Review: Theory and Practice of Minimal Fresh Gas Flow Anesthesia. Canadian Journal of Anesthesia 2012, 59, 785–797. [CrossRef]
- Baker, A.B. Back to Basics - A Simplified Non-Mathematical Approach to Low Flow Techniques in Anaesthesia. Anaesthesia and Intensive Care 1994, 22, 394–395. [CrossRef]
- Sherman, J.D. Committee on Environmental Health Releases New Edition of ‘Greening the Operating Room and Perioperative Arena.’ ASA Monitor 2024, 88, 9–10. [CrossRef]
- Soro, M.; Badenes, R.; Garcia-Perez, M.L.; Gallego-Ligorit, L.; Martí, F.J.; Aguilar, G.; Belda, F.J. The Accuracy of the Anesthetic Conserving Device (Anaconda©) as an Alternative to the Classical Vaporizer in Anesthesia. Anesthesia and Analgesia 2010, 111, 1176–1179. [CrossRef]
- Farrell, R.; Oomen, G.; Carey, P. A Technical Review of the History, Development and Performance of the Anaesthetic Conserving Device “AnaConDa” for Delivering Volatile Anaesthetic in Intensive and Post-Operative Critical Care. Journal of Clinical Monitoring and Computing 2018, 32, 595–604. [CrossRef]
- the ASA Committee on Environmental Health Sustainability Checklists Available online: https://www.asahq.org/about-asa/governance-and-committees/asa-committees/environmental-sustainability/greening-the-operating-room/checklists (accessed on 23 July 2024).
- Campbell, M.; Pierce, J.M.T. Atmospheric Science, Anaesthesia, and the Environment. BJA Education 2015, 15, 173–179. [CrossRef]
- Lane, S.F. The Environmental Sustainability of Propofol Use in Daily Practice. British Journal of Anaesthesia 2020, 124, e221–e222. [CrossRef]
- Sherman, J.; Le, C.; Lamers, V.; Eckelman, M. Life Cycle Greenhouse Gas Emissions of Anesthetic Drugs. Anesthesia and Analgesia 2012, 114, 1086–1090. [CrossRef]
- Mankes, R.F. Propofol Wastage in Anesthesia. Anesthesia and Analgesia 2012, 114, 1091–1092. [CrossRef]
- Bouvet, L.; Chasseigne, V.; Bonnet, L.; d’Aranda, E.; Zieleskiewicz, L. Sustainability in Anesthesia and Critical Care: Achievements, Needs and Barriers. Anaesthesia Critical Care & Pain Medicine 2023, 42, 101297. [CrossRef]
- Gasciauskaite, G.; Lunkiewicz, J.; Spahn, D.R.; Von Deschwanden, C.; Nöthiger, C.B.; Tscholl, D.W. Environmental Sustainability from Anesthesia Providers’ Perspective: A Qualitative Study. BMC Anesthesiology 2023, 23, 377. [CrossRef]
- McGain, F.; White, S.; Mossenson, S.; Kayak, E.; Story, D. A Survey of Anesthesiologists’ Views of Operating Room Recycling. Anesthesia and Analgesia 2012, 114, 1049–1054. [CrossRef]
- Gillerman, R.G.; Browning, R.A. Drug Use Inefficiency: A Hidden Source of Wasted Health Care Dollars. Anesthesia & Analgesia 2000, 91, 921–924. [CrossRef]
- Lejus, C.; Blanloeil, Y.; Oudot, M.; Le Teurnier, Y.; Lepage, J.Y.; Loutrel, O.; Asehnoune, K. Atropine and Ephedrine: A Significant Waste in the Operating Theatre. Anaesthesia 2012, 67, 300–301. [CrossRef]
- Barbariol, F.; Deana, C.; Lucchese, F.; Cataldi, G.; Bassi, F.; Bove, T.; Vetrugno, L.; De Monte, A. Evaluation of Drug Wastage in the Operating Rooms and Intensive Care Units of a Regional Health Service. Anesthesia and Analgesia 2021, 132, 1450–1456. [CrossRef]
- Ingle, R.G.; Agarwal, A.S. Pre-Filled Syringe – a Ready-to-Use Drug Delivery System: A Review. Expert Opinion on Drug Delivery 2014, 11, 1391–1399. [CrossRef]
- Wyssusek, K.H.; Keys, M.T.; van Zundert, A.A.J. Operating Room Greening Initiatives – the Old, the New, and the Way Forward: A Narrative Review. Waste Management and Research 2019, 37, 3–19. [CrossRef]
- Ard, J.L.; Tobin, K.; Huncke, T.; Kline, R.; Ryan, S.M.; Bell, C. A Survey of the American Society of Anesthesiologists Regarding Environmental Attitudes, Knowledge, and Organization. A & A Case Reports 2016, 6, 208–216. [CrossRef]
- Lees, N.; Hall, R. Information Technology in Anaesthesia and Critical Care. Continuing Education in Anaesthesia Critical Care & Pain 2011, 11, 104–107. [CrossRef]
- Khan, F.A.; Merry, A.F. Improving Anesthesia Safety in Low-Resource Settings. Anesthesia and Analgesia 2018, 126, 1312–1320. [CrossRef]
- Bocskai, T.; Loibl, C.; Vamos, Z.; Woth, G.; Molnar, T.; Bogar, L.; Lujber, L. Cost-Effectiveness of Anesthesia Maintained with Sevoflurane or Propofol with and without Additional Monitoring: A Prospective, Randomized Controlled Trial. BMC Anesthesiology 2018, 18. [CrossRef]
- Klar, G.; Zalan, J.; Roche, A.M.; Phelan, R. Ethical Dilemmas in Global Anesthesia and Surgery. Canadian Journal of Anesthesia 2018, 65, 861–867.
- National Institute for Health and Care Excellence The NICE Strategy 2021 to 2026. 2021.
- Wacker, J. Quality Indicators for Anesthesia and Perioperative Medicine. Current Opinion in Anaesthesiology 2023, 36, 208–215.
- Herrmann, A.; Lenzer, B.; Müller, B.S.; Danquah, I.; Nadeau, K.C.; Muche-Borowski, C.; Traidl-Hoffmann, C. Integrating Planetary Health into Clinical Guidelines to Sustainably Transform Health Care. The Lancet Planetary Health 2022, 6, e184–e185. [CrossRef]
- Perret, L.; Paquin-Lanthier, G.; Williams, S. Urgence Climatique et Anesthésie Carboneutre. Revue Médicale Suisse 2023, 19, 1513–1516. [CrossRef]
- American society of anesthesiologists Inhaled Anesthetic 2023 Challenge Available online: https://www.asahq.org/about-asa/governance-and-committees/asa-committees/environmental-sustainability/inhaled-anesthetic-challenge.
- Xiao, M.Z.X.; Abbass, S.A.A.; Bahrey, L.; Rubinstein, E.; Chan, V.W.S. A Roadmap for Environmental Sustainability of Plastic Use in Anesthesia and the Perioperative Arena. Anesthesiology 2021, 135, 729–737. [CrossRef]
- Gisbert-Mora, C.; Sablé, S.; Vinclair, C.; Pillot, J.; Rozé, H. How a Green Team Can Rapidly Lower the Carbon Footprint of Paracetamol Route Use in Intensive Care. Intensive Care Medicine 2024, 10–11. [CrossRef]
- Seger, C.; Cannesson, M.; Hemmerling Montreal, T.M.; Lieve Vrouw Jan A Hendrickx, O.F. Open Peer Review Recent Advances in the Technology of Anesthesia [Version 1; Peer Review: 2 Approved]. 2020. [CrossRef]
- Yeoh, C.B.; Lee, K.J.; Coric, V.; Tollinche, L.E. Simple Green Changes for Anesthesia Practices to Make a Difference. EC clinical and medical case reports 2020, 3, 1–6.
- Yasny, J.S.; White, J. Environmental Implications of Anesthetic Gases. Anesthesia Progress 2012, 59, 154–158. [CrossRef]
- Pratt, B. Sustainable Global Health Practice: An Ethical Imperative? Bioethics 2022, 36, 874–882. [CrossRef]
- World Health Organization Healthy Hospitals, Healthy Planet, Healthy People: Addressing Climate Change in Health Care Settings: Discussion Draft. Healthy Hospitals, Healthy Planet, Healthy people: Addressing climate change in health care settings: Discussion Draft 2010, 30.
- Health Research & Educational Trust. Environmental Sustainability in Hospitals: The Value of Efficiency. 2014, 1–34.
- Hussain, A.; Umair, M.; Khan, S.; Alonazi, W.B.; Almutairi, S.S.; Malik, A. Exploring Sustainable Healthcare: Innovations in Health Economics, Social Policy, and Management. Heliyon 2024, 10, e33186. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).